Professional Documents
Culture Documents
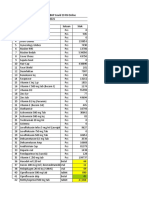
PVC Drugstudy
PVC Drugstudy
Uploaded by
freejorgeeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PVC Drugstudy
PVC Drugstudy
Uploaded by
freejorgeeCopyright:
Available Formats
Angiozem
Content
s Diltiazem HCl
Indicatio Management of chronic stable angina and angina
ns artery spasm. Alone or in combination, it is also used for the
treatment of hypertension.
Dosag Initially, 30 mg 3 or 4 times a day, the dosage being increased
e gradually at 1- or 2-day intervals as needed and tolerated, or as
prescribed by the physician.
Administrati
May be taken with or without food
on
Contraindicati Patients with sick sinus syndrome except in the presence of a
ons functioning ventricular pacemaker; 2nd- or 3rd-degree AV block
except in the presence of a functioning ventricular pacemaker;
hypotension (<90 mm Hg systolic); hypersensitivity to
and acute myocardial infarction and pulmonary congestion
documented by x-ray on admission.
Use in lactation: Diltiazem should not be given to nursing women
until more information becomes available concerning its safety on
infants.
Warning Cardiac Conduction: Diltiazem prolongs AV node refractory period
s without significantly prolonging sinus node recovery time, except in
patients with sick sinus syndrome. This effect may rarely result in
abnormal slow heart rates (particularly in patients with sick sinus
syndrome) or 2nd- or 3rd-degree AV block (13 of 3290 patients or
0.4%). Concomitant use of diltiazem with β-blockers or digitalis may
result in additive effects on cardiac conduction. A patient with
Prinzmetal's angina developed periods asystole (2-5 sec) after a
single dose of 60 mg of diltiazem. (See Adverse Reactions.)
Congestive Heart Failure: Although diltiazem has a negative
inotropic effect in isolated animal tissue preparations, hemodynamic
studies in humans with normal ventricular function have not shown
a reduction in cardiac index nor consistent negative effects on
contractility (dp/dt). An acute study of oral diltiazem
impaired ventricular function (ejection fraction 24±6%) showed
improvement in indices of ventricular function without significant
decrease in contractile function (dp/dt). Worsening of congestive
heart failure has been reported in patients with preexisting
impairment of ventricular function. Hypotension: Decreases in blood
pressure associated with diltiazem therapy may occasionally result
in symptomatic hypotension.
Special General: Diltiazem is extensively metabolized by the liver and
Precautions excreted by the kidneys and in bile. As with any drug given over
prolonged periods, laboratory parameter 8 of renal and hepatic
functions should be monitored at regular intervals.
Angiozem should be used with caution in patients with impaired
renal or hepatic function. In subacute and chronic dog and rat
studies designed to produce toxicity, high doses of
associated with hepatic damage. In special subacute
studies, oral doses of ≥125 mg/kg in rats were associated with
histological changes in the liver which were reversible when the
drug was discontinued. In dogs, doses of 20 mg/kg were also
associated with hepatic changes; however, these changes were
reversible with continued dosing.
Dermatological events (see Adverse Reactions) may be transient
and may disappear despite continued use of diltiazem
skin eruptions progressing to erythema multiforme
exfoliative dermatitis have also been infrequently reported. Should a
dermatologic reaction persist, Angiozem should be discontinued.
Adverse Drug The following represent occurrences observed in clinical studies of
Reactions angina patients. In many cases, the relationship to
been established. The most common occurrences from these
studies as well as their frequency of presentation are: Edema
(2.4%), headache (2.1%), nausea (1.9%) dizziness (1.5%), rashes
(1.3%), asthenia (1.2%). Ankle edema, hypotension, flushing and
gastrointestinal disturbances (including anorexia, vomiting,
constipation or diarrhea, taste disturbances and weight gain) may
occur. Rashes, possibly due to hypersensitivity, are normally mild
and transient, but in a few cases, erythema multiforme
dermatitis has developed. Transient elevations in liver enzyme
values, and occasionally hepatitis, have been reported.
The following events were reported infrequently (<1%):
Cardiovascular: Angina, arrhythmia, AV block (1st degree), AV block
(2nd or 3rd degree, see Warnings), bradycardia, bundle-branch
block, congestive heart failure, ECG abnormality, flushing,
hypotension, palpitations, syncope.
CNS: Abnormal dreams, amnesia, depression, gait abnormality,
hallucinations, insomnia, nervousness, paresthesia
change, somnolence, tremor.
Gastrointestinal: Anorexia, constipation, diarrhea,
dyspepsia, mild elevations of alkaline phosphatase
LDH.
Dermatological: Petechiae, photosensitivity, pruritus
Others: Amblyopia, CPK elevation, dry mouth, dyspnea
eye irritation, hyperglycemia, hyperuricemia, impotence and muscle
cramps, nasal congestion, nocturia, osteoarticular
sexual difficulties, tinnitus.
Click to view ADR Monitoring Website
Drug Due to the potential for additive effects, caution and careful titration
Interactions are warranted in patients receiving diltiazem concomitantly with
other agents known to affect the cardiac contractility and/or
conduction (see Warnings). Pharmacologic studies indicate that
there may be additive effects in prolonging AV conduction when
using β-blockers or digitalis concomitantly with diltiazem
Warnings). As with all drugs, care should be exercised when treating
patients with multiple medications. Diltiazem undergoes
biotransformation by cytochrome P-450 mixed function
administration of diltiazem with other agents which follow the same
route of biotransformation may result in the competitive inhibition of
metabolism. Especially in patients with renal and/or hepatic
impairment, dosage of similarly metabolized drugs, particularly
those of low therapeutic ratio, may require adjustment when
starting or stopping concomitantly administered diltiazem
maintain optimum therapeutic blood levels.
Beta-Blockers: Controlled and uncontrolled domestic studies suggest
that concomitant use of diltiazem and β-blockers is usually well
tolerated. But available data are not sufficient to predict the effects
of concomitant treatment in patients with left ventricular
dysfunction or cardiac conduction abnormalities. Administration of
diltiazem concomitantly with propranolol in 5 normal volunteers
resulted in increased propranolol levels in all subjects and
bioavailability of propranolol was increased approximately by
50%. In vitro, propranolol appears to be displaced from its binding
sites by diltiazem. If combination therapy is initiated or withdrawn in
conjunction with propranolol, an adjustment in the
may be warranted.
Cimetidine: A study in 6 healthy volunteers has shown a significant
increase in peak diltiazem plasma levels (58%) and AUC (53%) after
a 1-week course of cimetidine at 1200 mg/day and a single dose of
diltiazem 60 mg. Ranitidine produced smaller, nonsignificant
increases. The effect may be mediated by cimetidine's
inhibition of hepatic cytochrome P-450, the enzyme system
responsible for the first-pass metabolism of diltiazem
currently receiving diltiazem therapy should be carefully monitored
for a change in pharmacological effect when initiating and
discontinuing therapy with cimetidine. An adjustment in
dose may be warranted.
Anesthetics: The depression of cardiac contractility, conductivity
and automaticity as well as the vascular dilation associated with
anesthetics may be potentiated by calcium-channel blockers. When
used concomitantly, anesthetics and calcium blockers should be
titrated carefully.
Cyclosporin: A pharmacokinetic interaction between
cyclosporin has been observed during studies involving renal and
cardiac transplant patients. In renal and cardiac transplant
recipients, a reduction of cyclosporin dose ranging from 15-48% was
necessary to maintain cyclosporin through concentrations similar to
those seen prior to the addition of diltiazem. If these agents are to
be administered concurrently, cyclosporin concentrations should be
monitored especially when diltiazem therapy is initiated, adjusted or
discontinued. The effect of cyclosporin-diltiazem plasma
concentrations has not been evaluated.
Carbamazepine: Concomitant administration of diltiazem
carbamazepine has been reported to result in elevated serum levels
of carbamazepine (40-72% increase), resulting in toxicity in some
cases. Patients receiving these drugs concurrently should be
monitored for a potential drug interaction.
View more drug interactions for Angiozem
Pregnancy
Category (US
FDA)
Category C: Either studies in animals have revealed adverse
effects on the foetus (teratogenic or embryocidal or other) and
there are no controlled studies in women or studies in women and
animals are not available. Drugs should be given only if the
potential benefit justifies the potential risk to the
Storag
Store at temperatures not exceeding 30°C.
e
Mechanism of Antiangina.
Action Pharmacology: The therapeutic benefits achieved with
are related to its ability to inhibit the influx of calcium ions during
membrane depolarization of cardiac and vascular smooth muscle.
Mechanism of Action: Diltiazem acts in the following ways: Angina
Due to Coronary Artery Spasm: Diltiazem has been shown to be a
potent dilator of coronary arteries both epicardial
subendocardial. Spontaneous and ergonovine-induced coronary
artery spasms are inhibited by diltiazem.
Exertional Angina: Diltiazem has been shown to produce increase in
exercise tolerance, probably due to its ability to reduce myocardial
oxygen demand. This is accomplished via reductions in heart rate
and systemic blood pressure at submaximal and maximal exercise
workloads. In animal models, diltiazem interferes with the slow
inward (depolarizing) current in excitable tissue. It causes
excitation-contraction uncoupling in various myocardial tissues
without changes in the configuration of the action potential.
Diltiazem produces relaxation of coronary vascular smooth muscle
and dilation of both large and small coronary arteries. The resultant
increases in coronary blood flow (epicardial and subendocardial
occur in ischemic and non-ischemic models, and are accompanied
by dose-dependent decreases in blood pressure and decreases in
peripheral resistance.
MIMS
Calcium Antagonists
Class
ATC C08DB01 - Diltiazem ; Belongs to the class of benzothiazepine
Classification derivative selective calcium-channel blockers with direct cardiac
effects. Used in the treatment of cardiovascular diseases.
Poison
Rx
Schedule
Presentation/Pack
Tab 30 mg x 100's. 60 mg x 100's.
ing
Amiodarone
Indication & Oral
Dosage Ventricular arrhythmias
Adult: 800-1,600 mg/day in 1-2 divided doses for 1-3 wk until initial
therapeutic response is achieved, then reduce dose to 600-800
mg/day in 1-2 divided doses for 1 mth. Maintenance: 400 mg/day;
lower doses may be used for supraventricular arrhythmias. Daily
doses may be divided. Close monitoring of the patient is
recommended. Use the minimum effective dose.
Hepatic impairment: Dosage reduction may be necessary.
Intravenous
Life-threatening ventricular arrhythmias
Adult: Recommended starting dose: About 1 g over 1st 24 hr. Dose
is given in a 3-phase sequence. Initial rapid loading dose: Infuse 150
mg at a rate of 15 mg/minute (initial infusion rate should not exceed
30 mg/minute); followed by the slow loading phase: Infuse 360 mg
at a rate of 1 mg/minute; followed by the first maintenance phase:
Infuse 540 mg at a rate of 0.5 mg/minute. After the 1st 24 hr,
maintain infusion rate at 0.5 mg/minute (i.e. 720 mg over 24 hr);
rate may be increased to achieve effective suppression of
arrhythmia. For breakthrough episodes, supplemental doses of 150
mg may be given at 15 mg/minute; may repeat supplemental doses
up to a max IV dose of 2.2 g/24 hr. Maintenance infusion at up to 0.5
mg/minute may be continued for up to 2-3 wk with caution.
Concentrate for inj should be diluted prior to admin. Conversion to
oral therapy will depend on the administered dose of the IV therapy
and the bioavailability of the oral drug.
Hepatic impairment: Dosage reduction may be necessary.
Intravenous
Pulseless ventricular fibrillation or ventricular tachycardia
Adult: Initial: 300 mg (diluted in 20-30 ml dextrose 5% or normal
saline) if VF or VT recurs, to be given as a single dose by rapid IV inj.
Supplemental dose: 150 mg followed by an infusion of 1 mg/minute
for 6 hr, then 0.5 mg/minute. Max: 2.1 g daily.
Hepatic impairment: Dosage reduction may be necessary.
Reconstitution: To make solution for 1st rapid loading infusion or
supplemental infusion: Add 3 ml of amiodarone HCl concentrate (50
mg/ml) to 100 ml of dextrose 5% to give a final conc of 1.5 g/ml; for
slow infusion: Add 18 ml of amiodarone HCl concentrate (50 mg/ml)
to 500 ml of dextrose 5% to give a final conc of 1.8 mg/ml; for
subsequent maintenance infusions, diluted solutions with conc
ranging from 1-6 mg/ml may be used. Solutions with conc ≥ 2 mg/ml
should be administered via a central venous catheter.
Incompatibility: Y-site incompatibility: Cefamandole, sodium
bicarbonate, heparin, aminophylline. Syringe incompatibility:
Heparin. Admixture incompatibility (amiodarone conc: 4 mg/ml):
Cefazolin sodium, cefamandole, mezlocillin sodium, sodium
bicarbonate, heparin sodium, aminophylline.
Administrati May be taken with or without food. (Take consistently w/ or without
on meals. Take w/ meals if high dose or to reduce GI discomfort.)
Overdosa Symptoms include hypotension, cardiogenic shock, bradycardia, AV
ge block and hepatotoxicity. Hypotension and cardiogenic shock should
be treated by slowing the infusion rate or with vasopressor drugs,
positive inotropic agents and volume expansion. Bradycardia and AV
block may require temporary pacing. Monitor hepatic enzyme
concentrations. Amiodarone is not dialyzable.
Contraindicati Hypersensitivity to amiodarone or iodine. Severe sinus node
ons dysfunction, 2nd and 3rd degree heart block (except in patients with
a functioning artificial pacemaker), cardiogenic shock, pregnancy.
Special Close monitoring is recommended as amiodarone may worsen
Precautions arrhythmia especially when used concurrently with other anti-
arrhythmic drugs or drugs that prolong QT interval. May cause
hypotension and bradycardia. May increase risk of liver toxicity. May
cause visual disturbance/impairment; corneal refractive laser
surgery is not recommended in patients on amiodarone treatment.
May cause lung damage; monitor for pulmonary toxicity e.g. acute
respiratory distress syndrome. Monitor liver functions regularly. May
affect defibrillation or pacing thresholds of cardiac devices. Correct
electrolyte imbalance before starting treatment. Caution when used
in patients undergoing surgery. Avoid excessive sunlight exposure
due to increased risk of photosensitivity. Hepatic impairment,
thyroid disease, elderly. Lactation.
Adverse Drug Blue-grey discolouration of skin, photosensitivity, peripheral
Reactions neuropathy, paraesthesia, myopathy, ataxia, tremor, nausea,
vomiting, metallic taste, hypothyroidism, hyperthyroidism,
alopoecia, sleep disturbances, corneal microdeposits, hot flushes,
sweating. Heart block, bradycardia, sinus arrest, hepatotoxicity,
heart failure.
Potentially Fatal: Pulmonary toxicity including pulmonary fibrosis
and interstitial pneumonitis, hepatotoxicity, thyrotoxicity. Ventricular
arrhythmias, pulmonary alveolitis, exacerbation of arrhythmias and
rare serious liver injury. Generally in patients with high doses and
having preexisting abnormalities of diffusion capacity.
Drug Potentiation of antiarrhythmic drugs. Possible increased risk of
Interactions adverse effects when used with anaesthetic agents. Monitor plasma
levels of amiodarone when used with HIV protease
inhibitors. Cimetidine may increase serum levels of amiodarone.
Concurrent use may increase serum levels of ciclosporin. May
increase risk of myopathy or rhabdomyolysis when used with HMG-
CoA reductase inhibitors.Rifampin may reduce the serum levels of
amiodarone.
Potentially Fatal: Potentiates the effect of warfarin and other
anticoagulants hence dose of warfarin generally needs to be
reduced approx half. Raised plasma concentrations
of digoxin, phenytoin and quinidine. Additive effect with beta-
blockers and calcium-channel blockers (e.g. verapamil and
diltiazem).
Click to view more Drug Interactions
Food St John's wort may reduce serum levels of amiodarone. Grapefruit
Interaction juice may increase serum levels of amiodarone.
Pregnancy
Category (US
FDA)
Category D: There is positive evidence of human foetal risk, but
the benefits from use in pregnant women may be acceptable
despite the risk (e.g., if the drug is needed in a life-threatening
situation or for a serious disease for which safer drugs cannot be
used or are ineffective).
Storag
Intravenous: Store at 15-25°C. Oral: Store at 20-25°C.
e
Mechanism of Amiodarone is a class III antiarrhythmic agent which inhibits
Action stimulation, prolongs action potential and refractory period in
myocardial tissues. It also decreases AV conduction and sinus node
function. Sinus rate is reduced by 15-20%, PR and QT intervals are
increased. Amiodarone can cause marked sinus bradycardia or sinus
arrest and heart block. In acute IV doses, amiodarone may exert a
mild negative inotropic effect.
Onset: IV: 1-30 minutes.
Duration: IV: 1-3 hr.
Absorption: Oral admin: Variable and erratically absorbed from the
GI tract; average bioavailability is about 50%.
Distribution: Extensively distributed to body tissues; accumulates
in muscles and fats. Crosses the placenta and enters breast milk.
Protein-binding: 96%
Metabolism: Yields desethylamiodarone (also has antiarrhythmic
properties); may undergo enterohepatic recycling.
Excretion: Mainly in the faeces via bile; via urine (small amounts of
amiodarone and its metabolites). Terminal elimination half-life:
About 50 days; may range from 20-100 days due to extensive tissue
distribution.
MIMS
Cardiac Drugs
Class
ATC C01BD01 - amiodarone; Belongs to class III antiarrhythmics used in
Classification the treatment of arrhythmia.
Carisoprodol
Oral
Indication & Painful muscle spasm associated with musculoskeletal
Dosage conditions
Adult: 350 mg 3-4 times daily for up to 2-3 wk.
Elderly: Half of the usual dose.
Administrati
May be taken with or without food.
on
Contraindicati
Acute intermittent porphyria, hypersensitivity. Lactation.
ons
Special Renal and hepatic failure, childn <12 yrs. Pregnancy. Should be used
Precautions with caution in addiction prone individuals.
Adverse Drug Dizziness, drowsiness, nausea, epigastric distress, tachycardia,
Reactions orthostatic hypotension, Hypersensitivity reactions, rash.
Potentially Fatal: Idiosyncratic reaction (rare).
Pregnancy
Category (US
FDA)
Category C: Either studies in animals have revealed adverse
effects on the foetus (teratogenic or embryocidal or other) and
there are no controlled studies in women or studies in women and
animals are not available. Drugs should be given only if the
potential benefit justifies the potential risk to the foetus.
Storag
Oral: Store at 15-30°C.
e
Mechanism of Carisoprodol blocks interneuronal synaptic activity in the descending
Action reticular formation and spinal cord resulting in skeletal muscle
relaxation.
Duration: 4-6 hrs.
Absorption: Absorbed from the GIT (oral); peak plasma
concentrations after 30 min.
Distribution: Enters breast milk (significant amounts).
Metabolism: Hepatic; yields meprobamate.
Excretion: Via urine (as metabolites).
MIMS
Muscle Relaxants
Class
ATC M03BA02 - carisoprodol; Belongs to the class of carbamic esters
Classification used as centrally-acting muscle relaxants.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Current UIP (Universal Immunization Programme) Schedule in Our StateDocument35 pagesCurrent UIP (Universal Immunization Programme) Schedule in Our StateGopireddy Sivakarthik ReddyNo ratings yet
- Famotidine (Pepcid)Document1 pageFamotidine (Pepcid)E100% (1)
- Anthony Green Toxicology ReportDocument4 pagesAnthony Green Toxicology ReportGlennKesslerWPNo ratings yet
- PHESGO Nurse Administration Brochure Final Version - 210916 - 065152Document11 pagesPHESGO Nurse Administration Brochure Final Version - 210916 - 065152amyostNo ratings yet
- Characteristics of MetamizoleDocument9 pagesCharacteristics of MetamizoleLisa NPNo ratings yet
- Minutes of 281st Meeting of Registration BoardDocument755 pagesMinutes of 281st Meeting of Registration BoardSaheefaNo ratings yet
- Usp Review AlbuterolDocument82 pagesUsp Review Albuterolsrayu2603No ratings yet
- Case Study - DrugsDocument4 pagesCase Study - DrugsYza DizaNo ratings yet
- Laporan RS Online Dan IFRS (Stok Obat&BHP Covid) 1Document38 pagesLaporan RS Online Dan IFRS (Stok Obat&BHP Covid) 1zexindeathNo ratings yet
- Nursing Management of GI MedicationsDocument2 pagesNursing Management of GI MedicationsNil GyiNo ratings yet
- Sro 713 (I) 2018Document18 pagesSro 713 (I) 2018mazhar iqbalNo ratings yet
- Amitriptyline PDFDocument3 pagesAmitriptyline PDFscribdseewalNo ratings yet
- BK0131 Patterns and Trends of Amphetamine Type Stimulants ATS and ODocument96 pagesBK0131 Patterns and Trends of Amphetamine Type Stimulants ATS and OAnti NarkobaNo ratings yet
- Drugs Acting On The KidneysDocument56 pagesDrugs Acting On The Kidneysbetu tufaNo ratings yet
- PGX Guided Dosing of Antidepressant and Antipsychotic TherapyDocument1 pagePGX Guided Dosing of Antidepressant and Antipsychotic TherapyMichelle Kristine DonnellyNo ratings yet
- Nursing-Math Practice Set 1 PDFDocument3 pagesNursing-Math Practice Set 1 PDFSanaz NikiNo ratings yet
- Inventario Noviembre06Document13 pagesInventario Noviembre06luis davidNo ratings yet
- Department Memorandum No. 2022-0154Document41 pagesDepartment Memorandum No. 2022-0154Edrheyl Limbaga BiadnesNo ratings yet
- Urn Uvci 01 Ro M4q6dre9p31zg8ekv5zv705oygk8w2bDocument2 pagesUrn Uvci 01 Ro M4q6dre9p31zg8ekv5zv705oygk8w2bReni FerencziNo ratings yet
- Dosage: Route:: Mycobacterium TuberculosisDocument21 pagesDosage: Route:: Mycobacterium TuberculosisLyn ConsingNo ratings yet
- Case Parade Dr. VY - BaritoDocument11 pagesCase Parade Dr. VY - BaritoFADHILA SANDYNo ratings yet
- Cap 4-5-6 Painkillers, Local and Gen Anest - 2020Document15 pagesCap 4-5-6 Painkillers, Local and Gen Anest - 2020Irina Panciu StefanNo ratings yet
- M Pharma Projects Guides TitleDocument5 pagesM Pharma Projects Guides TitleRaviteja KondaNo ratings yet
- Alkaloidal AminesDocument55 pagesAlkaloidal Aminesakita dimaaalaNo ratings yet
- Formulary For VeterinariesDocument245 pagesFormulary For VeterinariesAhmad Raza100% (4)
- Inhaled SteriodsDocument7 pagesInhaled SteriodsEjie Boy IsagaNo ratings yet
- Formulary SaverDocument96 pagesFormulary SaverAhmad ANo ratings yet
- PHM 3471 Merged Week (1-6)Document303 pagesPHM 3471 Merged Week (1-6)Lisa MuthiniNo ratings yet
- Unit 3 Gastrointestinal Disorders P2 Peptic UlcerDocument43 pagesUnit 3 Gastrointestinal Disorders P2 Peptic UlcerShashidharan MenonNo ratings yet
- Lovenox (Enoxaparin) 80mgDocument1 pageLovenox (Enoxaparin) 80mgAdrianne BazoNo ratings yet