Professional Documents
Culture Documents
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Uploaded by
Hotdo SitumorangCopyright:
Available Formats
You might also like
- Surgery OSCE QuestionsDocument0 pagesSurgery OSCE QuestionsSinginiD86% (7)
- Post Test - CHNDocument13 pagesPost Test - CHNNaomi VirtudazoNo ratings yet
- Qualitative Article CritiqueDocument9 pagesQualitative Article CritiqueJohn Smith100% (2)
- Medication Incompatibility in Intravenous Lines in A Paediatric Intensive Care Unit (PICU) of Indonesian Hospital (Kel.8)Document11 pagesMedication Incompatibility in Intravenous Lines in A Paediatric Intensive Care Unit (PICU) of Indonesian Hospital (Kel.8)Rotama GurningNo ratings yet
- Adherence 4Document10 pagesAdherence 4NajeebNo ratings yet
- 2019 - KarttunenDocument10 pages2019 - KarttunenazeemathmariyamNo ratings yet
- CF Rca TemplateDocument8 pagesCF Rca TemplateEsteban García EcheverryNo ratings yet
- Background. Registered Nurses (RNS) Have A Role in The Medication Administration ProcessDocument4 pagesBackground. Registered Nurses (RNS) Have A Role in The Medication Administration ProcessEdmarkmoises ValdezNo ratings yet
- Enteral Tube Administration of Oral Chemotherapy DrugsDocument15 pagesEnteral Tube Administration of Oral Chemotherapy DrugsCoté HuertaNo ratings yet
- Farmaceuticos Instruindo EnfermagemDocument8 pagesFarmaceuticos Instruindo EnfermagemPhilipe VieiraNo ratings yet
- Fs 2Document13 pagesFs 2Muhamad Taufiq AliNo ratings yet
- How To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalDocument10 pagesHow To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalyyNo ratings yet
- False-Positive Interferences of Common Urine Drug Screen Immunoassays: A ReviewDocument10 pagesFalse-Positive Interferences of Common Urine Drug Screen Immunoassays: A ReviewJesse SonnenscheinNo ratings yet
- Article - False Positive Interferences of Common UDS ImmunoassaysDocument10 pagesArticle - False Positive Interferences of Common UDS ImmunoassayshmNo ratings yet
- 2019 - Darbishire Et AlDocument5 pages2019 - Darbishire Et AlazeemathmariyamNo ratings yet
- 1642-Article Text-7699-1-10-20200623Document5 pages1642-Article Text-7699-1-10-20200623mtgnzgaNo ratings yet
- NHS-FPX 4000 Applying Library Research SkillsDocument7 pagesNHS-FPX 4000 Applying Library Research SkillsIrene WafulaNo ratings yet
- Jurnal KesehatanDocument8 pagesJurnal KesehatanwildaNo ratings yet
- Jurnal PsDocument19 pagesJurnal PsIkeSintiaSuciNo ratings yet
- Preventing Ventilator-Associated ICHEDocument8 pagesPreventing Ventilator-Associated ICHEFelix Brian FelixNo ratings yet
- Quasi-Experimentos Infect DeseaseDocument8 pagesQuasi-Experimentos Infect DeseaseAlan MoraesNo ratings yet
- Robinson 2021Document12 pagesRobinson 2021Ami R. VirueteNo ratings yet
- Exploring The Knowledge and Attitude of Medical and Pharmacy Students About Generic Medicine in Lahore, PakistanDocument7 pagesExploring The Knowledge and Attitude of Medical and Pharmacy Students About Generic Medicine in Lahore, PakistanMathilda UllyNo ratings yet
- Research Article: Self-Medication in University Students From The City of Mansoura, EgyptDocument7 pagesResearch Article: Self-Medication in University Students From The City of Mansoura, EgyptyunitakajahNo ratings yet
- Implementation of Pharmacists' Monitoring for Intravenous Drug Compatibility - Ngọc DiệuDocument6 pagesImplementation of Pharmacists' Monitoring for Intravenous Drug Compatibility - Ngọc DiệuJolie Thao NgôNo ratings yet
- Original Paper: Pediatric Suspension Usage & Reconstitution Practices of Mothers in Zaria, Northwestern NigeriaDocument8 pagesOriginal Paper: Pediatric Suspension Usage & Reconstitution Practices of Mothers in Zaria, Northwestern Nigeriaeinas omerNo ratings yet
- Roughead 2016Document10 pagesRoughead 2016Armando cortezNo ratings yet
- PPhA NatCon 2024 Presentations Book of AbstractsDocument53 pagesPPhA NatCon 2024 Presentations Book of AbstractsRey TabayNo ratings yet
- Medication Error Factors, Safety Guideline System, Flow of Drug Usage, and Code of Conduct To Prevent Medication ErrorDocument5 pagesMedication Error Factors, Safety Guideline System, Flow of Drug Usage, and Code of Conduct To Prevent Medication ErrorskyNo ratings yet
- A Retrospective Observational Study To Determine The Percentage of Drugs Prescribed by Generic Names in ICU of A Tertiary Care Hospital in Dakshina KannadaDocument6 pagesA Retrospective Observational Study To Determine The Percentage of Drugs Prescribed by Generic Names in ICU of A Tertiary Care Hospital in Dakshina KannadaIJPS : A Pharmaceutical JournalNo ratings yet
- The Need For Pharmaceutical Care in An Intensive Care Unit at A Teaching Hospital in South AfricaDocument4 pagesThe Need For Pharmaceutical Care in An Intensive Care Unit at A Teaching Hospital in South AfricaAdibaNo ratings yet
- Improving Safety On High-Alert MedicationDocument48 pagesImproving Safety On High-Alert MedicationLenny SucalditoNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- Reconciliacao MedicamentosaDocument22 pagesReconciliacao MedicamentosapchrispimNo ratings yet
- Frisk 2013Document12 pagesFrisk 2013Andres Felipe Narvaez PastranaNo ratings yet
- Artikel 3 Evaluation of Cart Fill Drug Distribution System For Inpatients at A South Indian Tertiary Care Teaching HospitalDocument5 pagesArtikel 3 Evaluation of Cart Fill Drug Distribution System For Inpatients at A South Indian Tertiary Care Teaching HospitalPuTri BerutuNo ratings yet
- The Causes of Prescribing Errors in English General PracticesDocument8 pagesThe Causes of Prescribing Errors in English General PracticesrosianaNo ratings yet
- 10 1093@ajhp@zxz236Document13 pages10 1093@ajhp@zxz236pymb6gt7jbNo ratings yet
- 5DCAA8961360Document5 pages5DCAA8961360Usama SpiffyNo ratings yet
- Adherence To MedicationDocument11 pagesAdherence To Medicationwillie2210100% (1)
- Hummael (2010)Document6 pagesHummael (2010)dewiNo ratings yet
- Factors Associated With Patients' Incomplete Understanding of PrescriptionsDocument9 pagesFactors Associated With Patients' Incomplete Understanding of PrescriptionsCanlas John MichaelNo ratings yet
- Knowledge About The Administration and Regulation of High Alert Medications Among Nurses in Palestine: A Cross-Sectional StudyDocument17 pagesKnowledge About The Administration and Regulation of High Alert Medications Among Nurses in Palestine: A Cross-Sectional StudyRachel CalditoNo ratings yet
- Incidence of Intravenous Drug Incompatibilities in Intensive Care UnitsDocument5 pagesIncidence of Intravenous Drug Incompatibilities in Intensive Care UnitsNeliydaMayantiNo ratings yet
- Adverse Event or Near-Miss Analysis (Nursing) .EditedDocument10 pagesAdverse Event or Near-Miss Analysis (Nursing) .EditedMaina PeterNo ratings yet
- Presentation RTA, DM, Rheumatoid ArthritisDocument26 pagesPresentation RTA, DM, Rheumatoid ArthritisShah MohammedNo ratings yet
- Morris 1992Document13 pagesMorris 1992Lorena PăduraruNo ratings yet
- Research in Hospital PharmacyDocument5 pagesResearch in Hospital Pharmacysyedamaryamali19No ratings yet
- Knowledge and Perception About Epidemiology Among Pharmacy StudentsDocument7 pagesKnowledge and Perception About Epidemiology Among Pharmacy StudentsArwinda NugraheniNo ratings yet
- Drug Prescribing and Dispensing Pattern in PediatrDocument6 pagesDrug Prescribing and Dispensing Pattern in PediatrAestherielle SeraphineNo ratings yet
- Avoiding Medication Errors Caused by Nurses in The Emergency Department in Saudi ArabiaDocument5 pagesAvoiding Medication Errors Caused by Nurses in The Emergency Department in Saudi Arabiaeditorial.boardNo ratings yet
- 2005-Adherence To Medication PDFDocument11 pages2005-Adherence To Medication PDFRizki RomadhonNo ratings yet
- OsterbergDocument11 pagesOsterbergMurti Apsari DewiNo ratings yet
- Evaluation of Drug Administration Errors in A Teaching HospitalDocument8 pagesEvaluation of Drug Administration Errors in A Teaching Hospitalmatin5No ratings yet
- Medication AssignmentDocument5 pagesMedication Assignmentapi-525323558No ratings yet
- Carpio Value To PracticeDocument4 pagesCarpio Value To Practiceapi-687505120No ratings yet
- Kejadian Eror Medikasi Di Ruang ICU JurnalDocument11 pagesKejadian Eror Medikasi Di Ruang ICU JurnalindriNo ratings yet
- Assessment 2 Medication ErrorsDocument9 pagesAssessment 2 Medication Errorsakko aliNo ratings yet
- 1 s2.0 S0002945923032072 MainDocument8 pages1 s2.0 S0002945923032072 Mainsoam.nadeem23No ratings yet
- Jurnal 1 PPKDocument7 pagesJurnal 1 PPKIndra Ressy OctavianiNo ratings yet
- Chibueze 2018Document8 pagesChibueze 2018AyuNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- Alumni Certificate of AppreciationDocument3 pagesAlumni Certificate of Appreciation1234 dhwani CHANPURANo ratings yet
- PICO & Search Strategy Worksheet: Name: Macayla GreinerDocument6 pagesPICO & Search Strategy Worksheet: Name: Macayla Greinerapi-407402630No ratings yet
- 1.3.FOUNDATIONS FOR Nursing Education PDFDocument23 pages1.3.FOUNDATIONS FOR Nursing Education PDFbereketNo ratings yet
- Molecular Ecology - 2023 - Velsko - High Conservation of The Dental Plaque Microbiome Across Populations With DifferingDocument20 pagesMolecular Ecology - 2023 - Velsko - High Conservation of The Dental Plaque Microbiome Across Populations With Differingloayza55No ratings yet
- Respiratory and Circulatory Systems: Activity Sheet No. 1Document7 pagesRespiratory and Circulatory Systems: Activity Sheet No. 1alexNo ratings yet
- 611 1199 1 SMDocument15 pages611 1199 1 SMTata TNo ratings yet
- NLM Classification: Worldwide Source of Medical Library ClassificationDocument1 pageNLM Classification: Worldwide Source of Medical Library ClassificationFrancisca CuellarNo ratings yet
- WAC 110 - 60A CHAPTER - FMDocument28 pagesWAC 110 - 60A CHAPTER - FMroger degreeNo ratings yet
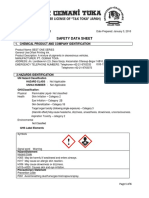
- SDS 175 BEST ONE SeriesDocument6 pagesSDS 175 BEST ONE SeriesWitara SajaNo ratings yet
- Nursing Assessment Template 11Document48 pagesNursing Assessment Template 11metrohealth shankarappasNo ratings yet
- Naturopathic Nutrition: Folate / Folic Acid, B12 and Biotin & OthersDocument29 pagesNaturopathic Nutrition: Folate / Folic Acid, B12 and Biotin & Othersglenn johnstonNo ratings yet
- Can Amitriptyline Makes You Feel More Awake Instead of DrowsyDocument3 pagesCan Amitriptyline Makes You Feel More Awake Instead of Drowsyteddypol100% (1)
- Sen (2017) What Stays Unsaid in Therapeutic RelationshipsDocument6 pagesSen (2017) What Stays Unsaid in Therapeutic RelationshipsnuriasegarramarNo ratings yet
- Lo3 - QUESTIONS AND ANSWERSDocument29 pagesLo3 - QUESTIONS AND ANSWERSisraaNo ratings yet
- Putu Yudi Pradnyana - 173212761 - A11b - Literature Review - Patient SafetyDocument5 pagesPutu Yudi Pradnyana - 173212761 - A11b - Literature Review - Patient SafetyKetut AdipaNo ratings yet
- Introducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionDocument9 pagesIntroducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionJhónatan CarranzaNo ratings yet
- Lab SafetyDocument75 pagesLab SafetyAskYahGirl ChannelNo ratings yet
- 2181-Article Text-4435-1-10-20190829Document18 pages2181-Article Text-4435-1-10-20190829shaniaNo ratings yet
- 60-SGC-HSE-F-007 Task Risk Assesement - Rev00 (En+Az) - ApprovedDocument11 pages60-SGC-HSE-F-007 Task Risk Assesement - Rev00 (En+Az) - ApprovedРашад ИбрагимовNo ratings yet
- MQ BDS 2nd Phase Web Options Notfication 2021Document2 pagesMQ BDS 2nd Phase Web Options Notfication 2021Feroz FerozNo ratings yet
- TeamBodyProject Quickstart GuideDocument15 pagesTeamBodyProject Quickstart GuideAbh ParNo ratings yet
- Psychology FullDocument151 pagesPsychology Fullraghuveer ula akNo ratings yet
- Your College Experience Transformation - Instructions and Grading RubricDocument5 pagesYour College Experience Transformation - Instructions and Grading Rubricapi-535279488No ratings yet
- Assessment of Knowledge and Attitude of Pharmacists Toward The Side Effects of Anesthetics in Patients With Hypertension: A Cross-Sectional StudyDocument9 pagesAssessment of Knowledge and Attitude of Pharmacists Toward The Side Effects of Anesthetics in Patients With Hypertension: A Cross-Sectional StudyMediterr J Pharm Pharm SciNo ratings yet
- There Are Three Types of AssessmentDocument6 pagesThere Are Three Types of Assessmentapi-316564284No ratings yet
- Veneers - Fantasy, Risk, SuccessDocument990 pagesVeneers - Fantasy, Risk, SuccessflaysminNo ratings yet
- ReflectionDocument3 pagesReflectionERLI CADUNGOGNo ratings yet
- Propranolol For AkitishiaDocument11 pagesPropranolol For AkitishiaPsikiatri 76 UndipNo ratings yet
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Uploaded by
Hotdo SitumorangOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Medication Incompatibility in Intravenous Lines in A Paediatric Inten-Sive Care Unit (PICU) of Indonesian Hospital
Uploaded by
Hotdo SitumorangCopyright:
Available Formats
Crit Care Shock (2018) 21:114-123
Medication incompatibility in intravenous lines in a Paediatric Inten-
sive Care Unit (PICU) of Indonesian hospital
Suci Hanifah, Patrick Ball, Ross Kennedy
Abstract mine, and midazolam+dobutamine+norepineph-
Objectives: Currently, little is documented con- rine. Compatibility data covering simultaneous
cerning the patterns of multiple concurrent med- administration of three-or-more intravenous
ication use utilising single intravenous line. The drugs was not found in 97.5% (n=120) of the
in-line compatibility issues in Paediatric Inten- cases. Most practitioners (92.9%) recognized in-
sive Care Units (PICUs) are not as well docu- compatibility. Many (46.4%) said they observed
mented as in adult patients either. This study >3-10 in-line incompatibilities in a month. Most
closely examined the combination of medications nurses (78.5%) reported using the manufacturer
used concurrently in a PICU, recorded how med- as their reference source for compatibility data.
ications were used, and then investigated the in- Flushing with clear fluid between doses was the
line potential compatibility. most used method to prevent incompatibility
Methods: This study was a mixed model designed (45.5%).
first to identify retrospectively the patterns of Conclusions: It was a common practice to con-
multiple medication use at any single time of ad- currently administer three or more medications:
ministration (STA). Secondly, a questionnaire analgesics, sedatives, inotropes, and others,
was distributed to practitioners to elucidate their through the same port with major potential for
perceptions about incompatibility. incompatibility issues. Most of the literature is
Results: From a single lumen peripheral line in- based on two drug comparisons with minimal in-
vitro simulation, it was observed that three infu- formation on using combinations of three or
sions typically met in sequential Y-sites and had more. Most practitioners’ understanding of the
the potential to interact. The combinations iden- implications of the terminology of “incompatibil-
tified were morphine+midazolam, midazo- ity not known or possible” for their patients ap-
lam+fentanyl+morphine, morphine+fenta- peared lacking.
nyl+dobutamine, morphine+midazolam+keta-
.
Key words: Intravenous, drug utilization, drug incompatibility, critical care, paediatrics.
Introduction a single admission. (1) In paediatric practice, the re-
In critical care, the majority of medications (>70%) quirement for multiple parenteral medications with
are administered parenterally for faster action or due limited venous access and fluid volume restriction
to patient’s inability to swallow oral medications. It frequently leads to concurrent administration of
is known that many patients will receive an average combinations of intravenous (IV) medications
of 10 different medications in multiple doses during through a single line. Based on pharmaceutical for-
. mulation principles, this has the potential for physi-
cal and chemical reactions, which when occurring
in-line and directly entering the patient circulation,
From Pharmacy Department, Faculty of Science, Universitas may lead to morbidity or mortality. (2,3) Anecdotal
Islam Indonesia (UII), Yogyakarta, Indonesia (Suci Hanifah), evidence suggests that insufficient attention is paid
School of Pharmacy, Faculty of Science and Engineering, Wol-
to this, which seems to be multifactorial and may
verhampton University, England, UK (Patrick Ball), and
School of Biomedical Science, Charles Sturt University, New include knowledge, time, workforce, and cost con-
South Wales, Australia (Ross Kennedy). straints. (4)
Literature reports on medication use have concen-
trated on a single agent and infusion fluids or per-
Address for correspondence:
Suci Hanifah
haps in combination with another, making it diffi-
Jalan Kaliurang Km 14.4 Sleman, Yogyakarta 55582, Indonesia cult to evaluate in the context of multiple medica-
Tel: +6285643958700 tions being added at different access points into a
Emails: suci.hanifah@gmail.com, suci.hanifah@uii.ac.id single infusion system. (5,6) Also, laboratory mod-
.
114 Crit Care Shock 2018 Vol. 21 No. 3
els where two medications have been mixed to- viewed to gain an adequate sample of medication
gether at fixed concentrations in a test tube poorly usage patterns in the PICU and any recorded issues
reflect the way in which medications may also in- regarding incompatibility. Then, bedside observa-
teract with residuals of another before or after, the tions were undertaken for one month to confirm pat-
IV fluids, and the infusion system (tubing, connect- terns of how medications were prescribed, prepared
ors, etc.), or for various periods of time at variable and administered as well as where medications were
concentration gradients resulted from flow effects. administered simultaneously. No staff information
Also, the role of pharmaceutical excipients in the or identifiers were collected, and only the process
formulation makes it impossible to extrapolate in- sequence was recorded. Thirdly, a questionnaire
formation from one manufacturer’s formulation to was administered to nurses and resident doctors in-
an alternative product from a different manufac- volved in drug preparation and administration. This
turer. (7) A recent study has suggested that pharma- was used to understand their perspective on incom-
cists, who are usually consulted when information patibilities and to identify whether they perceived
about incompatibility is not available, need to be them as serious problems. The collected infor-
aware of medication compatibility issues and that mation was then analysed to establish an under-
“no data available” should not be interpreted as safe standing of the level of incompatibility problem and
to minimize such errors in their hospitals. (8) current prevention strategies in the PICU facility.
This preliminary study was used as the basis for All data collected in this phase was anonymous and
identifying the problem of incompatibility in paedi- no personal identifiers were used.
atric critical care setting in in-vitro real time simu-
lated IV lines by closely observing and recording Operational definitions adopted for drug admin-
the practice and gathering information about ward istration
staff experiences and reactions to what has been ob- “Single time of administration (STA)” refers to the
served by pharmacists as incompatibility. administration of more than one medication at a spe-
cific timing, such as 8.00 o’clock in the morning or
Methods in the evening. The term “infusion-infusion” refers
Study approach to the simultaneous administration of two medica-
The setting of this research was the PICU in a teach- tions by infusion via a two-way connector. At any
ing hospital in Java, Indonesia, which is considered STA, if an intermittent or single bolus IV medica-
a centre of excellence within the province. It is a tion is injected sequentially through a port into infu-
leading centre from which other hospitals look for sion tubing, the term “infusion-injection” will be
guidance. After a comprehensive review of litera- used.
ture, a retrospective prescription chart review was
conducted to establish the most common combina- Data analysis
tions of medications and the problems incurring Data collected from the medical records was tran-
during their administration. This was followed by a scribed into a Microsoft Excel™ spreadsheet. To
prospective observational study of medication ad- ensure that there was no missing data, the spread-
ministration practice and administration of a simple sheet was crosschecked several times in sequence
questionnaire on the perceptions of nursing and and randomly. The data regarding medication use
medical staff in relation to the problem of drug in- and questionnaire responses were qualitatively ana-
compatibility. lysed.
Ethics approval for this study was obtained from the
Charles Sturt University Human Research Ethics Results
Committee (CSU HREC) on 18 September 2013 The retrospective medical record search yielded in-
(2013/173). In addition, approval was also granted formation on 231 patients. There were 19 patients
by Universitas Gadjah Mada Human Ethics Com- excluded due to missing measurable data fields in
mittee (GMU HEC) on 31 July 2013 their records, and 212 patient records were consid-
(KE/FK/733/EC). Hospital staff participation was ered for further analysis, including the name of the
voluntarily, and the return of completed question- medication, route, dose, administration time, and
naire was considered as an implied consent to par- any reported incompatibility medication-related
ticipate. problems.
Data collection Profile of multiple intravenous
As an initial step, medical records for the period be- Patients in this PICU were administered an average
tween 1 June 2012 and 30 September 2013 were re- of 1-6 drugs at one STA, mostly (89%) through a
. .
Crit Care Shock 2018 Vol. 21 No. 3 115
peripheral venous cannula (PVC). Over one third of tion of practitioners’ practice in administering par-
the patients (32.5%) received three infused medica- enteral infusion, it was found that practitioners did
tions concurrently through one line with other med- not appear to pre-consider IV drug compatibility, in-
ications administered by a bolus injection merged cluding definitions, prior to commencing admin-
into the infusion line at a ‘Y’-site. Therefore, a med- istration. Some nurses asked for an explanation of
ication group was defined as the combination of what incompatibility is and how it occurs. Other
medications administered simultaneously through nurses asked how to distinguish incompatibility
one line (infusion-infusion) or consecutively at one from thrombophlebitis and the differences between
STA through one extension (infusion-injection). incompatibility and drug interaction. There were
From a review of the medical records, it was found also questions about when flushing should be used
that there were more than 100 different groups of in relation to medication administration.
infusion-infusion and infusion-injection amongst The questionnaire was administered to nurses
the 212 sample patients. Figure 1 shows the fre- (n=22) and resident medical doctors (n=6) who
quency of the top 20 groups of drugs by frequency were in charge of the preparation and administration
of occurrence among the study samples. of IV drugs in PICU for more than a month, and all
The top 20 medication groups included various an- staff (n=28) returned the completed survey. There
algesic, sedative, and inotropic drugs. The most fre- was no consultation with or input from clinical phar-
quent groups were morphine+midazolam (15.6% macists in the ward on the preparation or admin-
frequency), morphine+fentanyl+midazolam (9.4% istration of drugs. The answers from nursing staff
frequency), and morphine+fentanyl+dobutamine and resident medical doctors to the questionnaire
(6.6% frequency). are shown in Table 2.
In one STA, infusions met injections (intermittent All the nurses reported that they had observed drug
medications) in the following descending order of incompatibilities during their employment at PICU.
frequency: paracetamol, cefotaxime, furosemide, Only four of the doctors reported observing incom-
ranitidine, meropenem, ampicillin, phenobarbital, patibilities. The doctors reported that they had ob-
phenytoin, metronidazole, chloramphenicol, acy- served less than three incompatibilities in the month
clovir, fluconazole, gentamicin, and methylpredni- prior to the survey, whereas about 59% of nurses re-
solone. ported observing 3-10 incompatibilities in the same
period. In this context, incompatibility refers to a
Potential problem of incompatibility visible colour change in the line or the appearance
Incompatibility is defined as the potential for a of a ‘flash’ of powder, as medications come to-
chemical reaction, displacement of particles, precip- gether, but not other possible incompatibility, which
itation, jell formation, or other interactions arising does not cause physical characteristic changes.
from medications coming together in the tubing, Although the doctors reported observing less than
such as drug-solution or drug-drug including infu- three occlusions in the previous month, about 45.5%
sion-infusion and infusion-injection or drug-equip- of nurses observed 3-10 occlusions and about
ment. Using recent literature, a two-dimensional 54.5% observed more than 10 occlusions. However,
compatibility chart could be developed (Figure 2), all the doctors and nurses had reported that their per-
which shows that 73.6% of medications had their ceived occlusions were not due to drug incompati-
information available on the PICU hospital website bilities. The staff had linked the occlusion to having
database; of these, 57.3% appeared compatible, been caused by a technical problem or blood clot-
while 16.2% were incompatible in solution. ting occlusion.
To identify the compatibility of co-infusions with With respect to prevention of incompatibility, prac-
simultaneous administration in a ‘Y’-site, a chart titioners (78.6%) usually referred to pharmaceutical
was developed which more closely resembled the manufacturers although some (21.4%) reported that
practice. Table 1 was developed to represent a pos- they used the “Handbook on Injectable Drugs”
sible compatibility chart (infusion-injection) based (Trissel, 2014) instead; however, on investigation,
on actual experience in practice. Unlike the two-di- the book was found to be located in the pharmacy
mensional chart, using recent literature, many not readily accessible in the ward. Most (45.5%)
frames were missing (97.5%; n=120) from this managed incompatibility by flushing with sodium
chart. chloride 0.9%. However, most nurses (68%) and all
the medical doctors reported that they considered
Problem of IV drug incompatibility faced by health drug incompatibility issues as beyond their respon-
practitioners sibilities.
During the one-month period of bedside observa- A range of drugs was reported to be involved in the
. .
116 Crit Care Shock 2018 Vol. 21 No. 3
incompatibilities observed (Figure 3). The most as this is an inherent part of their practice responsi-
frequent medications involved, reported by both bilities as drug administration specialists. However,
doctors and nurses, were phenytoin and phenobar- most of the nurses felt that, even though they are
bital. Interestingly, inotropic drugs were also drug administration specialists, managing compati-
viewed as problematic by the doctors (66.7%) but bility is beyond their expertise and responsibility.
less so by the nurses (22.7%). Therefore, the lack of ward pharmacy services in
this PICU appears to be an integrated part of the in-
Discussion compatibility problems. Fahimi (2015) found that
The likelihood of incompatibility increases with the drug incompatibility problems are frequent and
increasing number of medications at any STA. Re- need to be dealt with as they are one of the leading
ducing the number of drugs per STA may be possi- medication errors. (11)
ble by spacing the administration of injections, but On further investigation, it was found that manufac-
this may fit poorly into nursing routines and is com- turer information sheets were commonly used as a
plicated for slow or continuous concurrent infu- reference by nurses though they actually provided
sions. This is more complicated in paediatrics pop- insufficient information on compatibility. This is
ulation when only a small volume of fluids can be also in accordance with a previous study which dis-
infused and multiple access sites are not possible covered that many practitioners lacked awareness of
due to the age of patients. This may increase cost compatibility and how to source trusted information
and workload of ward staff and lead to medication about it. (8) In addition, Kanji (2010) stated that
errors. (9) nurses often ran concomitant drugs without suffi-
When a single lumen PVC is utilized, a rule to use cient understanding of drug compatibility. (12)
separate lumen for each drug may become impossi- Another finding was that the PICU practitioners
ble. Additionally, in one single PVC, several infu- have insufficient training on how to manage incom-
sions flow in each piece of tubing and meet with the patibility issues effectively. This study also identi-
other infusions or injections at a 3-way stopcock or fied vast variation in medication groups and admin-
other connector where incompatibility reactions can istration protocols, which seems to be confusing for
occur. In contrast, incompatibility seems rarely to nurses, leaving them at the risk of causing admin-
be reported when two IV drugs are administered istration errors. Camire (2010) found a correlation
concurrently in critical care. The potential for in- between a higher level of knowledge and a reduc-
compatibility between consecutive IV injections ap- tion in errors. (13)
pears to be avoidable if practitioners are accustomed Incompatibility is commonly classified by nurses as
to flushing with clear fluid before and after medica- relating to the medication injected rather than the
tion delivery provided that the solution and volume process. Most injections, such as acyclovir, ampicil-
used have been validated for the system in use; how- lin, furosemide, phenobarbital, phenytoin and mero-
ever, in small infants, the volume and electrolyte ad- penem, have a basic pH (>7) or high pKa and will
ministered with the flushes may be significant. theoretically cause precipitation when in low pH so-
Though rare, it may still occur as a fixed route for lutions such as 5% glucose (pH 4-4.5). It is well
three common groups: amine/cardioactive drugs, known that the high pKa of these drugs means that
analgesic/sedative, and parenteral nutrition in sepa- relatively high pH levels are required to sustain
rated lumen that cannot be implemented because of drugs in solution and they are very prone to precip-
the non-availability of multi lumen catheters in this itation during dilution if the pH is allowed to drift
unit. However, the frequency of this occurrence is too low. (14) Considering this, it is deemed neces-
not known and missing from the chart mimicking sary to undertake assays of compatibility to fill in
practice (Table 1). This study’s finding regarding the missing frame of the chart (Table 1). Bertsche
the increased risk of incompatibility between three (2008) found that having a protocol reduced incom-
or more medications concurs with that of other patibility from 5.8% to 2.4%. (8) Thus, the provi-
works being understudied. (7,10) Therefore, the de- sion of IV compatibility data is a fundamental phar-
velopment of a three-dimensional (or more) chart macy service in critical care. (15)
for each infusion group administered in conjunction Overall, these present findings have illustrated the
with an injection is a benefit to the current body of recurrent problems of incompatibility and lacked
knowledge in the area of parenteral therapy for pae- recognition and understanding. The lack of a ward
diatric patients. pharmacist in PICU may contribute to the low
Based on the questionnaires, nurses were more awareness level. This appears to differ from hospi-
likely to encounter and observe drug incompatibili- tals in some developed countries where pharmacist
ties and occlusion of the infusion line than doctors contribution is considered helpful in two-thirds of
. .
Crit Care Shock 2018 Vol. 21 No. 3 117
compatibility cases (16) and can reduce errors by Conclusions
66%. (17) Accordingly, the current study supports Based on the medical records of 212 paediatric pa-
the need for clinical pharmacists to be involved in tients, the majority were administered multiple
the development of infusion protocols in PICU. The medications using three simultaneous infusions and
role of pharmacists should be extended to critical an injection. The five main drug groups in this PICU
care services. (18,19) According to the international were morphine+midazolam, midazolam+fenta-
guidance on competency from the Society of Criti- nyl+morphine, morphine+fentanyl+dobutamine,
cal Care Medicine, the prevention of incompatibil- morphine+midazolam+ketamine, and midazo-
ity falls within the competency and responsibility of lam+dobutamine+norepinephrine. Additional med-
clinical pharmacists. (20) ications may also be administered as bolus or inter-
This study has provided preliminary information on mittent, including ampicillin, acyclovir, cefotaxime,
the incompatibility problems in PICU and ad- chloramphenicol, gentamicin, phenytoin,
dressed the urgency of incompatibility assays for methylprednisolone, metronidazole, meropenem,
three and more concurrent medications. The identi- phenobarbital, phenytoin, and ranitidine.
fication of incompatibility must be interpreted with ‘Y’-site incompatibility occurred during the dwell
caution as the numbers and percentages do not ex- time with other infusions and injections as they were
press the actual frequency of incompatibility in administered with a one-lumen catheter (no separate
every single case, but they are based on the most line). Based on a review of the literature, much in-
frequently listed medications and conditions, which formation (97.5%, n=120) is missing from the infu-
have the potential for incompatibility. This study sions-injections compatibility chart with regard to
may be limited to reflect incompatibility problems the most frequently administered combinations.
in Indonesia, which can be different from other The responses from the questionnaires have shown
countries. that most practitioners (92.9%) encountered incom-
Based on the findings, the current study proposes patibility during observation, mainly with pheny-
that hospitals should provide staff with education toin, although most did not have sufficient under-
sessions in the area of parenteral drug compatibility standing of incompatibility problems and manage-
to raise the level of awareness regarding this critical ment. The 78.5% practitioners used manufacturer
issue. Appropriate professional development short information to check the compatibility data. To pre-
courses can also relay information, refresh the vent incompatibility, flushing was used by 45.5%
knowledge, and increase awareness of practitioners nurses, while 39.3% chose to change drugs, and
concerning incompatibility. (21) 17.9% reported to the doctors.
118 Crit Care Shock 2018 Vol. 21 No. 3
Table 1. Compatibility amongst medication groups, infusion with injection
Infusion Injection drugs Intermittent
Drug groups
Without injection
Chloramphenicol
Dexamethasone
Metronidazole
Phenobarbital
Paracetamol
Fluconazole
Meropenem
Furosemide
Cefotaxime
Gentamicin
Ampicillin
Ranitidine
Phenytoin
Acyclovir
Midazolam, morphine C ? ? ? ? ? ? ? ? ? ? ? ? ? ?
Morphine, midazolam, C ? ? ? ? ? ? ? ? ? ? ? ? ? ?
fentanyl
Morphine, fentanyl, do- ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
butamine
Midazolam, morphine, C ? ? ? ? ? ? ? ? ? ? ? ? ? ?
ketamine
Fentanyl, dobutamine, ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
norepinephrine
Midazolam, dobuta- ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
mine, norepinephrine
Legend: C=compatible; ?=no data available (no recent compatibility study or information in the literature
to answer).
Crit Care Shock 2018 Vol. 21 No. 3 119
Table 2. Incompatibility problem according to health practitioners based on questionnaires
Questions and choice of answers Responses to questions
Nurses (n=22) Doctors (n=6)
Duration of work in PICU
- <1 year 0 6
- 1 to <5 years 2 0
- 5 to <10 years 13 0
- ³10 years 7 0
Occurrence of incompatibility
- Have you ever observed drug incompabilities at PICU Sardjito?
• Yes 22 4
• No 0 2
- How often have you observed drug incompatibilities within the last month?
• <3 4 6
• 3-10 13 0
• >10 4 0
• No answer 1 0
- Have you observed an infusion line occlusion?
• Yes 22 5
• No 0 1
- How often did you observe an occlusion within last month?
• <3 0 6
• 3-10 10 0
• >10 12 0
- Were those occlusions associated with incompatibility?
• Yes 0 0
• No 22 6
- What medications have you observed Various answers given; see Figure 3
drug incompatibilities with?
- What incompatibilities have proved hard Phenytoin (22) Phenytoin (4)
to manage? Phenobarbital (20) No answer (2)
Diazepam (2)
Prevention of incompatibility
- Is there any protocol for preventing in- Yes (10), flushing Yes (0)
compatibility? No (12) No (6)
Did not know (0) Did not know (0)
- What reference do you use to have a look Manufacturers (16) Manufacturers (6)
at information regarding incompatibility? Book* (6)
- How can you manage the incompatibility Spooling or aspira- Spooling or aspira-
or line occlusion? tion (10) tion (0)
Changing with the Changing with the
other (8) other (3)
Reporting to senior Reporting to senior
or doctor (4) or doctor (1)
No answer (2)
Legend: *=Trissel’s “Handbook on Injectable Drugs”.
120 Crit Care Shock 2018 Vol. 21 No. 3
Figure 1. Top 20 simultaneous infusions in PICU
Morphine+Norepinephrine+Ketamine
Morphine+Ketamine
Morphine+Midazolam+Ketamine+Epinephrine
Morphine+Midazolam+Dopamine+Norepinephrine
Morphine+Fentanyl
Morphine+Dobutamine+Norepinephrine
Morphine+Dopamine
Morphine+Midazolam+Dobutamine+Epinephrine
Fentanyl+Midazolam+Ketamine
Fentanyl+Midazolam
Midazolam+Dopamine
Morphine+Dobutamine+Norepinephrine
Morphine+Fentanyl
Morphine+Midazolam+Dopamine
Fentanyl+Dobutamine+Norepinephrine
Midazolam+Dobutamine+Norepinephrine
Morphine+Midazolam+Ketamine
Morphine+Fentanyl+Dobutamine
Morphine+Fentanyl+Midazolam
Morphine+Midazolam
0 5 10 15 20 25 30 35
Number of Patients
Crit Care Shock 2018 Vol. 21 No. 3 121
Figure 2. Two-dimensional compatibility chart of the 22 top drugs in PICU
Legend: C=compatible; I=incompatible; ?=no data available.
Figure 3. Frequency of reported drug incompatibility occurrences
120,0
Frequency of reporting (%)
100,0
Nurses Doctors
80,0
60,0
40,0
20,0
0,0
em
l
lin
Am e
e
lin
/Im cin
ol
am
id
in
ita
id
ru
at
of
to
lip
su
cil
y
m
rb
en
ep
on
cD
op
am
ny
tra
pi
In
se
ba
ip
az
uc
e
pi
Pr
nt
ro
In
Ph
no
Di
Gl
ro
Ge
Fu
e
ot
um
em
Ph
In
lci
en
Ca
op
er
M
122 Crit Care Shock 2018 Vol. 21 No. 3
References
1. Di Paolo ER, Hirschi B, Pannatier A. Quantita- Res 2015;14:87-93.
tive Determination of Particulate Contamina- 12. Kanji S, Goddard R, Donnelly R, McIntyre L,
tion in Intravenous Administration Sets. Pharm Turgeon A, Coons P, et al. Physical Compati-
Weekbl Sci 1990;12(5):190-5. bility of Drug Infusion used in Canadian Inten-
2. Taxis K, Barber N. Incidence and Severity of sive Care Units: A Program of Research. Can-
Intravenous Drug Errors in a German Hospital. ada: Canadian Patient Safety Institute and Insti-
Eur J Clin Pharmacol 2004;59(11):815-7. tut Canadien pour la securite des patients; 2010
3. Bradley JS, Wassel RT, Lee L, Nambiar S. In- May 31. 32 p.
travenous Ceftriaxone and Calcium in the Neo- 13. Camiré E, Moyen E, Stelfox HT. Medication
nate: Assessing the Risk for Cardiopulmonary Errors in Critical Care: Risk Factors, Prevention
Adverse Events. Paediatrics. 2009;123(4): and Disclosure. CMAJ 2009;180(9):936-43.
e609-13. 14. Newton DW. Drug Incompatibility Chemistry.
4. Almasdy D, Siregar CJP. Evaluasi Teknik Am J Health Syst Pharm 2009;66(4):348-57.
Penggunaan Sediaan Parenteral dan Pencam- 15. Mühlebach S. Incompatibility Reactions in IV
puran Intravena pada Ruangan Rawat bedah di Drug Therapy: Preventable Medication Errors.
Suatu Rumah Sakit Pemerintah. Jurnal Sains Paper presented at: The 12th EAHP Congress;
dan Teknologi Farmasi 2002;7:36-43. 2007 Mar 21-23; Bordeaux, France.
5. Biswal S, Mishra P, Malhotra S, Puri G, Pandhi 16. Delestras S, Kabiche S, Guignard B, Sigrist T,
P. Drug Utilization Pattern in the Intensive Care Fonzo-Christe C, Bonnabry P. CP-049 Are
Unit of a Tertiary Care Hospital. J Clin Pharma- Pharmacist's Recommendations on Drug Com-
col 2006;46(8):945-51. patibility Applied by Healthcare Professionals?
6. Tavallaee M, Fahimi F, Kiani S. Drug-Use Pat- A Randomised Controlled Study. Eur J Hosp
terns in an Intensive Care Unit of a Hospital in Pharm Sci Pract 2014;21:A20.
Iran: an Observational Prospective Study. Int J 17. Leape LL. Errors in Medicine. Clin Chim Acta.
Pharm Pract 2010;18(6):370-6. 2009;404(1):2-5.
7. Hanifah S, Ball P, Kennedy R, Lambert K. 18. Chuang L, Sutton JD, Henderson GT. Impact of
Mapping of Incompatibility Assay: Bringing a Clinical Pharmacist on Cost Saving and Cost
Method to Problem in Critical Care. Int J Pharm Avoidance in Drug Therapy in an Intensive
Pharm Sci 2014;6(4):171-3. Care Unit. Hosp Pharm 1994;29(3):215-8, 21.
8. Bertsche T, Mayer Y, Stahl R, Hoppe-Tichy T, 19. LaRochelle JM, Desselle B. Critical Care Phar-
Encke J, Haefeli WE. Prevention of Intravenous macotherapy: Description of an Innovative Pe-
Drug Incompatibilities in an Intensive Care diatric Residency Elective Experience Unitliz-
Unit. Am J Health Syst Pharm 2008;65(19): ing Clinical Pharmacy Faculty as Preceptor.
1834-40. Crit Care Shock. 2015;18:52-4.
9. Dabaghzadeh F, Rashidian A, Torkamandi H, 20. Rudis MI, Brandl KM. Position Paper on Criti-
Alahyari S, Hanafi S, Farsaei S, et al. Medica- cal Care Pharmacy Services. Society of Critical
tion Errors in an Emergency Department in a Care Medicine and American College of Clini-
Large Teaching Hospital in Tehran. Iran J cal Pharmacy Task Force on Critical Care Phar-
Pharm Res 2013;12(4):937-42. macy Services. Crit Care Med 2000;28(11):
10. Trissel LA. Handbook on Injectable Drugs. 3746-50.
16th ed. Maryland: Bethesda MD, American 21. Shah A. Pharmacy Intervention in the Medica-
Society of Health-System Pharmacists; 2011. tion-use Process. The Role of Pharmacist in Im-
11. Fahimi F, Forough AS, Taghikhani S, proving Patient Safety. Den Haag, The Nether-
Saliminejad L. The Rate of Physicochemical In- lands: International Pharmaceutical Federation
compatibilities, Administration Errors. Factors (FIP); 2009.
Correlating with Nurses᾽ Errors. Iran J Pharm
.
Crit Care Shock 2018 Vol. 21 No. 3 123
You might also like
- Surgery OSCE QuestionsDocument0 pagesSurgery OSCE QuestionsSinginiD86% (7)
- Post Test - CHNDocument13 pagesPost Test - CHNNaomi VirtudazoNo ratings yet
- Qualitative Article CritiqueDocument9 pagesQualitative Article CritiqueJohn Smith100% (2)
- Medication Incompatibility in Intravenous Lines in A Paediatric Intensive Care Unit (PICU) of Indonesian Hospital (Kel.8)Document11 pagesMedication Incompatibility in Intravenous Lines in A Paediatric Intensive Care Unit (PICU) of Indonesian Hospital (Kel.8)Rotama GurningNo ratings yet
- Adherence 4Document10 pagesAdherence 4NajeebNo ratings yet
- 2019 - KarttunenDocument10 pages2019 - KarttunenazeemathmariyamNo ratings yet
- CF Rca TemplateDocument8 pagesCF Rca TemplateEsteban García EcheverryNo ratings yet
- Background. Registered Nurses (RNS) Have A Role in The Medication Administration ProcessDocument4 pagesBackground. Registered Nurses (RNS) Have A Role in The Medication Administration ProcessEdmarkmoises ValdezNo ratings yet
- Enteral Tube Administration of Oral Chemotherapy DrugsDocument15 pagesEnteral Tube Administration of Oral Chemotherapy DrugsCoté HuertaNo ratings yet
- Farmaceuticos Instruindo EnfermagemDocument8 pagesFarmaceuticos Instruindo EnfermagemPhilipe VieiraNo ratings yet
- Fs 2Document13 pagesFs 2Muhamad Taufiq AliNo ratings yet
- How To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalDocument10 pagesHow To Change Nurses' Behavior Leading To Medication Administration Errors Using A Survey Approach in United Christian HospitalyyNo ratings yet
- False-Positive Interferences of Common Urine Drug Screen Immunoassays: A ReviewDocument10 pagesFalse-Positive Interferences of Common Urine Drug Screen Immunoassays: A ReviewJesse SonnenscheinNo ratings yet
- Article - False Positive Interferences of Common UDS ImmunoassaysDocument10 pagesArticle - False Positive Interferences of Common UDS ImmunoassayshmNo ratings yet
- 2019 - Darbishire Et AlDocument5 pages2019 - Darbishire Et AlazeemathmariyamNo ratings yet
- 1642-Article Text-7699-1-10-20200623Document5 pages1642-Article Text-7699-1-10-20200623mtgnzgaNo ratings yet
- NHS-FPX 4000 Applying Library Research SkillsDocument7 pagesNHS-FPX 4000 Applying Library Research SkillsIrene WafulaNo ratings yet
- Jurnal KesehatanDocument8 pagesJurnal KesehatanwildaNo ratings yet
- Jurnal PsDocument19 pagesJurnal PsIkeSintiaSuciNo ratings yet
- Preventing Ventilator-Associated ICHEDocument8 pagesPreventing Ventilator-Associated ICHEFelix Brian FelixNo ratings yet
- Quasi-Experimentos Infect DeseaseDocument8 pagesQuasi-Experimentos Infect DeseaseAlan MoraesNo ratings yet
- Robinson 2021Document12 pagesRobinson 2021Ami R. VirueteNo ratings yet
- Exploring The Knowledge and Attitude of Medical and Pharmacy Students About Generic Medicine in Lahore, PakistanDocument7 pagesExploring The Knowledge and Attitude of Medical and Pharmacy Students About Generic Medicine in Lahore, PakistanMathilda UllyNo ratings yet
- Research Article: Self-Medication in University Students From The City of Mansoura, EgyptDocument7 pagesResearch Article: Self-Medication in University Students From The City of Mansoura, EgyptyunitakajahNo ratings yet
- Implementation of Pharmacists' Monitoring for Intravenous Drug Compatibility - Ngọc DiệuDocument6 pagesImplementation of Pharmacists' Monitoring for Intravenous Drug Compatibility - Ngọc DiệuJolie Thao NgôNo ratings yet
- Original Paper: Pediatric Suspension Usage & Reconstitution Practices of Mothers in Zaria, Northwestern NigeriaDocument8 pagesOriginal Paper: Pediatric Suspension Usage & Reconstitution Practices of Mothers in Zaria, Northwestern Nigeriaeinas omerNo ratings yet
- Roughead 2016Document10 pagesRoughead 2016Armando cortezNo ratings yet
- PPhA NatCon 2024 Presentations Book of AbstractsDocument53 pagesPPhA NatCon 2024 Presentations Book of AbstractsRey TabayNo ratings yet
- Medication Error Factors, Safety Guideline System, Flow of Drug Usage, and Code of Conduct To Prevent Medication ErrorDocument5 pagesMedication Error Factors, Safety Guideline System, Flow of Drug Usage, and Code of Conduct To Prevent Medication ErrorskyNo ratings yet
- A Retrospective Observational Study To Determine The Percentage of Drugs Prescribed by Generic Names in ICU of A Tertiary Care Hospital in Dakshina KannadaDocument6 pagesA Retrospective Observational Study To Determine The Percentage of Drugs Prescribed by Generic Names in ICU of A Tertiary Care Hospital in Dakshina KannadaIJPS : A Pharmaceutical JournalNo ratings yet
- The Need For Pharmaceutical Care in An Intensive Care Unit at A Teaching Hospital in South AfricaDocument4 pagesThe Need For Pharmaceutical Care in An Intensive Care Unit at A Teaching Hospital in South AfricaAdibaNo ratings yet
- Improving Safety On High-Alert MedicationDocument48 pagesImproving Safety On High-Alert MedicationLenny SucalditoNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- Reconciliacao MedicamentosaDocument22 pagesReconciliacao MedicamentosapchrispimNo ratings yet
- Frisk 2013Document12 pagesFrisk 2013Andres Felipe Narvaez PastranaNo ratings yet
- Artikel 3 Evaluation of Cart Fill Drug Distribution System For Inpatients at A South Indian Tertiary Care Teaching HospitalDocument5 pagesArtikel 3 Evaluation of Cart Fill Drug Distribution System For Inpatients at A South Indian Tertiary Care Teaching HospitalPuTri BerutuNo ratings yet
- The Causes of Prescribing Errors in English General PracticesDocument8 pagesThe Causes of Prescribing Errors in English General PracticesrosianaNo ratings yet
- 10 1093@ajhp@zxz236Document13 pages10 1093@ajhp@zxz236pymb6gt7jbNo ratings yet
- 5DCAA8961360Document5 pages5DCAA8961360Usama SpiffyNo ratings yet
- Adherence To MedicationDocument11 pagesAdherence To Medicationwillie2210100% (1)
- Hummael (2010)Document6 pagesHummael (2010)dewiNo ratings yet
- Factors Associated With Patients' Incomplete Understanding of PrescriptionsDocument9 pagesFactors Associated With Patients' Incomplete Understanding of PrescriptionsCanlas John MichaelNo ratings yet
- Knowledge About The Administration and Regulation of High Alert Medications Among Nurses in Palestine: A Cross-Sectional StudyDocument17 pagesKnowledge About The Administration and Regulation of High Alert Medications Among Nurses in Palestine: A Cross-Sectional StudyRachel CalditoNo ratings yet
- Incidence of Intravenous Drug Incompatibilities in Intensive Care UnitsDocument5 pagesIncidence of Intravenous Drug Incompatibilities in Intensive Care UnitsNeliydaMayantiNo ratings yet
- Adverse Event or Near-Miss Analysis (Nursing) .EditedDocument10 pagesAdverse Event or Near-Miss Analysis (Nursing) .EditedMaina PeterNo ratings yet
- Presentation RTA, DM, Rheumatoid ArthritisDocument26 pagesPresentation RTA, DM, Rheumatoid ArthritisShah MohammedNo ratings yet
- Morris 1992Document13 pagesMorris 1992Lorena PăduraruNo ratings yet
- Research in Hospital PharmacyDocument5 pagesResearch in Hospital Pharmacysyedamaryamali19No ratings yet
- Knowledge and Perception About Epidemiology Among Pharmacy StudentsDocument7 pagesKnowledge and Perception About Epidemiology Among Pharmacy StudentsArwinda NugraheniNo ratings yet
- Drug Prescribing and Dispensing Pattern in PediatrDocument6 pagesDrug Prescribing and Dispensing Pattern in PediatrAestherielle SeraphineNo ratings yet
- Avoiding Medication Errors Caused by Nurses in The Emergency Department in Saudi ArabiaDocument5 pagesAvoiding Medication Errors Caused by Nurses in The Emergency Department in Saudi Arabiaeditorial.boardNo ratings yet
- 2005-Adherence To Medication PDFDocument11 pages2005-Adherence To Medication PDFRizki RomadhonNo ratings yet
- OsterbergDocument11 pagesOsterbergMurti Apsari DewiNo ratings yet
- Evaluation of Drug Administration Errors in A Teaching HospitalDocument8 pagesEvaluation of Drug Administration Errors in A Teaching Hospitalmatin5No ratings yet
- Medication AssignmentDocument5 pagesMedication Assignmentapi-525323558No ratings yet
- Carpio Value To PracticeDocument4 pagesCarpio Value To Practiceapi-687505120No ratings yet
- Kejadian Eror Medikasi Di Ruang ICU JurnalDocument11 pagesKejadian Eror Medikasi Di Ruang ICU JurnalindriNo ratings yet
- Assessment 2 Medication ErrorsDocument9 pagesAssessment 2 Medication Errorsakko aliNo ratings yet
- 1 s2.0 S0002945923032072 MainDocument8 pages1 s2.0 S0002945923032072 Mainsoam.nadeem23No ratings yet
- Jurnal 1 PPKDocument7 pagesJurnal 1 PPKIndra Ressy OctavianiNo ratings yet
- Chibueze 2018Document8 pagesChibueze 2018AyuNo ratings yet
- Renal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysFrom EverandRenal Pharmacotherapy: Dosage Adjustment of Medications Eliminated by the KidneysNo ratings yet
- Alumni Certificate of AppreciationDocument3 pagesAlumni Certificate of Appreciation1234 dhwani CHANPURANo ratings yet
- PICO & Search Strategy Worksheet: Name: Macayla GreinerDocument6 pagesPICO & Search Strategy Worksheet: Name: Macayla Greinerapi-407402630No ratings yet
- 1.3.FOUNDATIONS FOR Nursing Education PDFDocument23 pages1.3.FOUNDATIONS FOR Nursing Education PDFbereketNo ratings yet
- Molecular Ecology - 2023 - Velsko - High Conservation of The Dental Plaque Microbiome Across Populations With DifferingDocument20 pagesMolecular Ecology - 2023 - Velsko - High Conservation of The Dental Plaque Microbiome Across Populations With Differingloayza55No ratings yet
- Respiratory and Circulatory Systems: Activity Sheet No. 1Document7 pagesRespiratory and Circulatory Systems: Activity Sheet No. 1alexNo ratings yet
- 611 1199 1 SMDocument15 pages611 1199 1 SMTata TNo ratings yet
- NLM Classification: Worldwide Source of Medical Library ClassificationDocument1 pageNLM Classification: Worldwide Source of Medical Library ClassificationFrancisca CuellarNo ratings yet
- WAC 110 - 60A CHAPTER - FMDocument28 pagesWAC 110 - 60A CHAPTER - FMroger degreeNo ratings yet
- SDS 175 BEST ONE SeriesDocument6 pagesSDS 175 BEST ONE SeriesWitara SajaNo ratings yet
- Nursing Assessment Template 11Document48 pagesNursing Assessment Template 11metrohealth shankarappasNo ratings yet
- Naturopathic Nutrition: Folate / Folic Acid, B12 and Biotin & OthersDocument29 pagesNaturopathic Nutrition: Folate / Folic Acid, B12 and Biotin & Othersglenn johnstonNo ratings yet
- Can Amitriptyline Makes You Feel More Awake Instead of DrowsyDocument3 pagesCan Amitriptyline Makes You Feel More Awake Instead of Drowsyteddypol100% (1)
- Sen (2017) What Stays Unsaid in Therapeutic RelationshipsDocument6 pagesSen (2017) What Stays Unsaid in Therapeutic RelationshipsnuriasegarramarNo ratings yet
- Lo3 - QUESTIONS AND ANSWERSDocument29 pagesLo3 - QUESTIONS AND ANSWERSisraaNo ratings yet
- Putu Yudi Pradnyana - 173212761 - A11b - Literature Review - Patient SafetyDocument5 pagesPutu Yudi Pradnyana - 173212761 - A11b - Literature Review - Patient SafetyKetut AdipaNo ratings yet
- Introducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionDocument9 pagesIntroducing WESAD, A Multimodal Dataset For Wearable Stress and Affect DetectionJhónatan CarranzaNo ratings yet
- Lab SafetyDocument75 pagesLab SafetyAskYahGirl ChannelNo ratings yet
- 2181-Article Text-4435-1-10-20190829Document18 pages2181-Article Text-4435-1-10-20190829shaniaNo ratings yet
- 60-SGC-HSE-F-007 Task Risk Assesement - Rev00 (En+Az) - ApprovedDocument11 pages60-SGC-HSE-F-007 Task Risk Assesement - Rev00 (En+Az) - ApprovedРашад ИбрагимовNo ratings yet
- MQ BDS 2nd Phase Web Options Notfication 2021Document2 pagesMQ BDS 2nd Phase Web Options Notfication 2021Feroz FerozNo ratings yet
- TeamBodyProject Quickstart GuideDocument15 pagesTeamBodyProject Quickstart GuideAbh ParNo ratings yet
- Psychology FullDocument151 pagesPsychology Fullraghuveer ula akNo ratings yet
- Your College Experience Transformation - Instructions and Grading RubricDocument5 pagesYour College Experience Transformation - Instructions and Grading Rubricapi-535279488No ratings yet
- Assessment of Knowledge and Attitude of Pharmacists Toward The Side Effects of Anesthetics in Patients With Hypertension: A Cross-Sectional StudyDocument9 pagesAssessment of Knowledge and Attitude of Pharmacists Toward The Side Effects of Anesthetics in Patients With Hypertension: A Cross-Sectional StudyMediterr J Pharm Pharm SciNo ratings yet
- There Are Three Types of AssessmentDocument6 pagesThere Are Three Types of Assessmentapi-316564284No ratings yet
- Veneers - Fantasy, Risk, SuccessDocument990 pagesVeneers - Fantasy, Risk, SuccessflaysminNo ratings yet
- ReflectionDocument3 pagesReflectionERLI CADUNGOGNo ratings yet
- Propranolol For AkitishiaDocument11 pagesPropranolol For AkitishiaPsikiatri 76 UndipNo ratings yet