Professional Documents
Culture Documents
Anaphylaxis The Facts Feb 2019
Anaphylaxis The Facts Feb 2019
Uploaded by
Syed AbdulCopyright:
Available Formats
You might also like
- VHA Code of IntegrityDocument28 pagesVHA Code of IntegrityFedSmith Inc.No ratings yet
- FAMILY NURSING CARE PLAN - AsthmaDocument1 pageFAMILY NURSING CARE PLAN - AsthmaJULIANNE BAYHON80% (5)
- Hypoglycaemia Acute Management ABCDEDocument11 pagesHypoglycaemia Acute Management ABCDESSNo ratings yet
- Ryan M. Carvalho: Career Objective: EducationDocument3 pagesRyan M. Carvalho: Career Objective: EducationddadNo ratings yet
- Nursing CatalogDocument27 pagesNursing Catalogrrockel100% (1)
- Critical Care NursingDocument12 pagesCritical Care NursingMoni Mbumba MelekeNo ratings yet
- Idiopathic Anaphylaxis 2021 v4Document10 pagesIdiopathic Anaphylaxis 2021 v4Cheyenne KruseNo ratings yet
- Idiopathic Anaphylaxis 2021 v5Document10 pagesIdiopathic Anaphylaxis 2021 v5RoundaboutNo ratings yet
- Exercise Induced Anaphylaxis-2019-V4Document6 pagesExercise Induced Anaphylaxis-2019-V4RoundaboutNo ratings yet
- Xis November 6, 2010Document61 pagesXis November 6, 2010bampugoNo ratings yet
- Anaphylaxis Resource Information and Lesson Plan Grades 4-6: Safe S A F EDocument10 pagesAnaphylaxis Resource Information and Lesson Plan Grades 4-6: Safe S A F EJefferson F. IberaNo ratings yet
- When To See A Doctor: Seek Emergency Medical HelpDocument4 pagesWhen To See A Doctor: Seek Emergency Medical HelpMaria Virginia FernandezNo ratings yet
- 1 Anaphylaxis Anaphylaxis Is A Life-Threatening TypeDocument9 pages1 Anaphylaxis Anaphylaxis Is A Life-Threatening TypeCraigNo ratings yet
- Clinical Aspects of Anaphlyaxis: DiagnosisDocument4 pagesClinical Aspects of Anaphlyaxis: Diagnosismaheen akramNo ratings yet
- AllergiesDocument9 pagesAllergiesClark Angelo JuanNo ratings yet
- What Is Allergy?: Ascia Information For Patients, Consumers and CarersDocument2 pagesWhat Is Allergy?: Ascia Information For Patients, Consumers and Carersvineeth84No ratings yet
- What Is AnaphylaxisDocument13 pagesWhat Is AnaphylaxisJohn SolivenNo ratings yet
- Anaphylactic ShockDocument29 pagesAnaphylactic ShockHIND100% (7)
- Emergency Medical Services Agency Lessons Learned: To: AlDocument4 pagesEmergency Medical Services Agency Lessons Learned: To: AlMega MuzdalifahNo ratings yet
- Anaphylaxis Part ADocument4 pagesAnaphylaxis Part ASojiNo ratings yet
- AnaphyDocument6 pagesAnaphyJefferson PaloyoNo ratings yet
- Shock Concept MapDocument2 pagesShock Concept MapElizabeth GarretsonNo ratings yet
- How Common Is Anaphylaxis?Document1 pageHow Common Is Anaphylaxis?Choong Cheng LounNo ratings yet
- Anaphylactic ShockDocument7 pagesAnaphylactic Shockapi-302126807No ratings yet
- Allergic Reaction: Under Supervision Prof. Nagwa Mahmoud El KobbiaDocument24 pagesAllergic Reaction: Under Supervision Prof. Nagwa Mahmoud El KobbiamorsiNo ratings yet
- Sudden IllnessesDocument26 pagesSudden IllnessesHesedh Jireh MartinNo ratings yet
- Allergies 1Document75 pagesAllergies 1asdfNo ratings yet
- Board Prep Emergency Ingestions Dec.2018Document46 pagesBoard Prep Emergency Ingestions Dec.2018Emily EresumaNo ratings yet
- Anaphylaxis Copy1Document22 pagesAnaphylaxis Copy1MunishNo ratings yet
- Symptoms: Allergic Reaction Medications Epinephrine Anaphylaxis Allergic Reaction Blood PressureDocument3 pagesSymptoms: Allergic Reaction Medications Epinephrine Anaphylaxis Allergic Reaction Blood Pressurejohn mendozaNo ratings yet
- First Aid For Allergic ReactionsDocument4 pagesFirst Aid For Allergic ReactionsIwan SetiawanNo ratings yet
- AnaphylaxisDocument10 pagesAnaphylaxisMadyline VictoryaNo ratings yet
- The Healthy Baby Gut Guide: Prevent Allergies, Build Immunity and Strengthen Microbiome Health From Day OneFrom EverandThe Healthy Baby Gut Guide: Prevent Allergies, Build Immunity and Strengthen Microbiome Health From Day OneNo ratings yet
- 5 Common Allergy MythsDocument2 pages5 Common Allergy MythsAbigail CoNo ratings yet
- ASCIA Anaphylaxis Training Resources NOV05Document23 pagesASCIA Anaphylaxis Training Resources NOV05keziahmaterschl2023No ratings yet
- FoodallergyDocument40 pagesFoodallergyapi-309082881No ratings yet
- AllergiesDocument12 pagesAllergiesKhushbu JainNo ratings yet
- Mustard Allergy: The FactsDocument5 pagesMustard Allergy: The FactsAnonymous GBge2ED1ONo ratings yet
- Drug AllergiesDocument3 pagesDrug AllergiesakbarNo ratings yet
- IMMUNOLOGYDocument11 pagesIMMUNOLOGYKiran ShahNo ratings yet
- Anaphylaxis TADocument54 pagesAnaphylaxis TAUriko ZoeNo ratings yet
- Anaphylaxis - First AidDocument3 pagesAnaphylaxis - First Aidsamanthafcooper_2753No ratings yet
- Hypoglycaemia - Acute Management - AbcdeDocument8 pagesHypoglycaemia - Acute Management - Abcderjohn 7No ratings yet
- Case Study For AllergyDocument3 pagesCase Study For AllergyGabbii CincoNo ratings yet
- BeSAFEBrochure PDFDocument2 pagesBeSAFEBrochure PDFPelmark G BalidiongNo ratings yet
- Allergies - Illnesses & Conditions - NHS InformDocument20 pagesAllergies - Illnesses & Conditions - NHS Informdavid gwyenrpNo ratings yet
- 2.first Aid Chapter-2Document7 pages2.first Aid Chapter-2Mohamed BinNo ratings yet
- Allergies Takunda Makondo 5th SemesterDocument11 pagesAllergies Takunda Makondo 5th SemestermakondotakundaNo ratings yet
- Guia Anafilaxia Niños y Adolescentes PacientesDocument8 pagesGuia Anafilaxia Niños y Adolescentes PacientesMariana Martinez LechugaNo ratings yet
- MaceeDocument40 pagesMaceeKaryl Anne LantingNo ratings yet
- Oral Allergy Version 8 Formatted With AC Logo and Name UpdatedDocument6 pagesOral Allergy Version 8 Formatted With AC Logo and Name UpdatedGlowstarNo ratings yet
- Paeds Complete PDFDocument176 pagesPaeds Complete PDFjljoioiuNo ratings yet
- Boado, M.A (Common Allergic Reaction and Stinging Insect)Document8 pagesBoado, M.A (Common Allergic Reaction and Stinging Insect)Melody BoadoNo ratings yet
- Allergies: A Protective Mechanism Out of ControlDocument29 pagesAllergies: A Protective Mechanism Out of Controlडा. सत्यदेव त्यागी आर्यNo ratings yet
- Allergies and HypersensitivityDocument14 pagesAllergies and HypersensitivityBabar MushtaqNo ratings yet
- By Mayo Clinic StaffDocument5 pagesBy Mayo Clinic StaffTry Febriani SiregarNo ratings yet
- Allergic ReactionsDocument12 pagesAllergic Reactionsvorticella12No ratings yet
- Anaphylaxis Articulo CompletoDocument6 pagesAnaphylaxis Articulo CompletoFrancelia Quiñonez RuvalcabaNo ratings yet
- Anaphylaxis (Case)Document4 pagesAnaphylaxis (Case)drkmwaiNo ratings yet
- ДокументDocument3 pagesДокументNura지민No ratings yet
- Allergies and Asthma TempDocument3 pagesAllergies and Asthma TempKonie LappinNo ratings yet
- Food Allergies and Pollen AllergiesDocument8 pagesFood Allergies and Pollen AllergiesYujenNo ratings yet
- Allergies: Understand and Manage Your AllergiesDocument44 pagesAllergies: Understand and Manage Your AllergieseeeNo ratings yet
- 3E Food AllergiesDocument12 pages3E Food Allergiesngd03122007No ratings yet
- Medical Emergencies AnaphylaxisDocument8 pagesMedical Emergencies AnaphylaxisLina Na'ilahNo ratings yet
- Materi PerkuliahanDocument69 pagesMateri PerkuliahanRirin RiriNo ratings yet
- The Gemini Virtual ClinicDocument19 pagesThe Gemini Virtual ClinicKritika SoniNo ratings yet
- Surgical Nursing Final PDFDocument26 pagesSurgical Nursing Final PDFAnuj Misra100% (2)
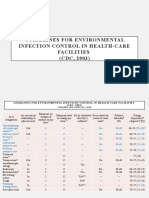
- CDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Document9 pagesCDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Kesehatan LingkunganNo ratings yet
- OTC wv1Document42 pagesOTC wv1Sheena GagarinNo ratings yet
- What Is EHealthDocument64 pagesWhat Is EHealthAshvini GoelNo ratings yet
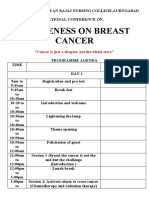
- National ConferenceDocument3 pagesNational Conferencelaveena aswaleNo ratings yet
- Project Proposal Purchase of CBRDocument3 pagesProject Proposal Purchase of CBRAida Potacag BuasenNo ratings yet
- Ah102 Syllabus 20171109Document7 pagesAh102 Syllabus 20171109api-384628971No ratings yet
- 2019 JSNA FinalDocument92 pages2019 JSNA Finalhiruni01No ratings yet
- Comparative Table Low Molecular Weight Heparins 1 2Document2 pagesComparative Table Low Molecular Weight Heparins 1 2Cosmin RazvanNo ratings yet
- FNCP (Hypertension)Document3 pagesFNCP (Hypertension)Jose Emmanuel Ribaya RuivivarNo ratings yet
- QUALISDocument31 pagesQUALISjopepinho5796No ratings yet
- Atfm Logbook m01cvs - Shrirajeswariintake13Document18 pagesAtfm Logbook m01cvs - Shrirajeswariintake13Shri VKNo ratings yet
- Prophetic Medicine Is The Cheapest, Safest and The Best Remedy in The Prevention and Treatment of Hypertension (High Blood Pressure) - A Mini ReviewDocument6 pagesProphetic Medicine Is The Cheapest, Safest and The Best Remedy in The Prevention and Treatment of Hypertension (High Blood Pressure) - A Mini ReviewCoronavirus COVID-19No ratings yet
- English For Informatics EngineeringDocument32 pagesEnglish For Informatics EngineeringDiana Urian100% (1)
- Introduction To Implant DentistryDocument106 pagesIntroduction To Implant DentistryFed Espiritu Santo GNo ratings yet
- Guideline AnesthesiaDocument31 pagesGuideline AnesthesiaMuhammad Izzatul Naim ZainuddinNo ratings yet
- Test Bank For 3 2 1 Code It 2020 8th Edition Michelle GreenDocument37 pagesTest Bank For 3 2 1 Code It 2020 8th Edition Michelle Greengeorgiannawiegardpro100% (17)
- Case StudyDocument5 pagesCase StudyKadiah KamaraNo ratings yet
- MH Assessment TemplateDocument2 pagesMH Assessment TemplatetakemebrickNo ratings yet
- Skills For Normal Vaginal Delivery NSVD 1Document1 pageSkills For Normal Vaginal Delivery NSVD 1Jewel Ann NuñezNo ratings yet
- Bacteriological Profile of Infections in Burns Unit - Plastic and Reconstructive Surgery Department - Mohammed Vi Chu MarrakechDocument7 pagesBacteriological Profile of Infections in Burns Unit - Plastic and Reconstructive Surgery Department - Mohammed Vi Chu MarrakechIJAR JOURNALNo ratings yet
- Physical Activity and Mental Health: Current ConceptsDocument14 pagesPhysical Activity and Mental Health: Current ConceptsCamilo RinconNo ratings yet
- Chapter 25 (Caring) ReviewerDocument7 pagesChapter 25 (Caring) ReviewerCarolyn Moquerio-serniculaNo ratings yet
Anaphylaxis The Facts Feb 2019
Anaphylaxis The Facts Feb 2019
Uploaded by
Syed AbdulOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaphylaxis The Facts Feb 2019
Anaphylaxis The Facts Feb 2019
Uploaded by
Syed AbdulCopyright:
Available Formats
Anaphylaxis: The Facts
The aim of this Factsheet
Anaphylaxis (pronounced ana-fil-ax-is) is a severe and often sudden allergic reaction. It can occur when
someone with allergies is exposed to something, they are allergic to (known as an allergen). Reactions usually
begin within minutes and rapidly progress but can occur up to 2-3 hours later.
Anaphylaxis is potentially life-threatening, and always requires an immediate emergency response.
If you or your child have had anaphylaxis, this Factsheet will help you understand more about the condition:
what anaphylaxis is, what causes it, the treatments and other vital facts. If you have experienced a sudden
allergic reaction in the past, then you may be at risk of anaphylaxis even if you have not had anaphylaxis
before. We advise that you see your GP and ask for a referral to an allergy clinic.
A diagnosis of anaphylaxis can be daunting at first, but by becoming well-informed, thinking ahead and
employing daily coping strategies, people affected find that life can return, almost, to normal.
Throughout the text you will see brief medical references given in brackets. Full references to these
documents are listed at the end of the Factsheet.
What are the causes of anaphylaxis?
The common causes of anaphylaxis include foods such as peanuts, tree nuts, milk, eggs, shellfish, fish,
sesame seeds and kiwi fruit, although many other foods have also been known to trigger anaphylaxis. Some
people can react to tiny amounts of food, although this rarely causes a very severe reaction. Non-food causes
include wasp or bee stings, natural latex (rubber), and certain drugs such as penicillin. In some people exercise
can trigger a severe reaction – either on its own or in combination with other factors such as food or drugs (for
example, aspirin).
Sometimes the cause of the reaction is not found. Such reactions may be labelled “idiopathic anaphylaxis”
(cause unknown). This does not mean the condition is psychological, though emotional stress can sometimes
worsen a reaction.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 1
What are the symptoms of anaphylaxis?
Most healthcare professionals consider an allergic reaction to be anaphylaxis when it involves a difficulty in
breathing or affects the heart rhythm or blood pressure. Any one or more of the following symptoms may be
present. These are often referred to as the ABC symptoms:
Airway Breathing Consciousness/Circulation
• Persistent cough • Difficult or noisy breathing • Feeling lightheaded or faint.
• Vocal changes (hoarse voice) • Wheezing (like an asthma • Clammy skin
• Difficulty in swallowing attack) • Confusion
• Swollen tongue • Unresponsive/unconscious
(due to a drop-in blood
pressure)
If there is a dramatic fall in blood pressure (anaphylactic shock) the person may become weak and floppy and
may have a sense of something terrible happening. This may lead to collapse, unconsciousness and – on rare
occasions – death.
In addition to the ABC symptoms listed above, the following, less severe symptoms may occur:
• Widespread flushing of the skin
• Nettle rash (otherwise known as hives or urticaria)
• Swelling of the skin (known as angioedema) anywhere on the body (for example, lips, face).
• Abdominal pain, nausea and vomiting
Those symptoms can also occur on their own. In the absence of the more serious ABC symptoms listed above,
the allergic reaction is likely to be less severe, but you should watch carefully in case ABC symptoms develop.
Why does anaphylaxis occur?
An allergic reaction (including anaphylaxis) occurs because the body’s immune system reacts inappropriately
in response to the presence of a food or substance that it wrongly perceives to be a threat. When this
happens, chemicals such as histamine are released from cells in the blood and tissues. These can cause
swelling in the skin, lips, mouth, throat or lower airway causing difficulty in swallowing and/or breathing.
What should I do if I’m worried that my allergy may be severe?
See your GP as soon as possible. Many GPs are well informed about allergy and can make a thorough
diagnosis. In most cases, the GP will need to refer you to an NHS allergy clinic.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 2
If the allergy affects your child your GP should be guided by the clinical guideline issued by NICE (the National
Institute for Health and Care Excellence) on the subject of “Food allergy in children and young people”
(CG116). This makes it clear which cases should be referred. The guidance can be accessed here:
http://guidance.nice.org.uk/CG116
Your GP can find information about the nearest children’s allergy clinic from the website of the BSACI (British
Society for Allergy and Clinical Immunology): www.bsaci.org.
If you are unsure about the potential severity of your allergy, don’t let that deter you from seeking your
doctor’s advice. It’s better to be safe than sorry.
What will an allergy clinic do?
The clinic will take a detailed history of previous reactions and other allergic conditions you or your child may
have, such as asthma, eczema or hay fever. Valuable information can also be provided through allergy tests,
such as skin prick tests and blood tests. Together, this can help the doctor or specialist nurse predict the
likelihood that a specific food or substance will cause an allergic reaction. They do not predict how severe
such a reaction might be, but the history can help the doctor decide whether to prescribe “rescue” medicines
such as adrenaline auto-injector “pen”.
Occasionally a “food challenge” may be offered to confirm diagnosis of allergy to a specific food or to rule out
food allergy. The person will be asked to eat small amounts of the suspect allergen, gradually increasing the
amount until it is clear that he or she is not allergic, or else a reaction occurs. Such tests should only be done
in an allergy clinic under controlled conditions.
Similarly, a challenge, under carefully supervised conditions, may be needed if you are suspected to be
allergic to a prescribed drug. This is because currently available tests may often not provide a reliable
diagnosis.
In our opinion, any allergy diagnosis using questionable techniques such as those advertised on the Internet
should be viewed with caution (see Royal College of Pathologists’ report, 2002, and NICE guideline CG 116 on
the diagnosis and assessment of food allergy in children and young people). The NICE guideline specifically
warns against Vega testing, applied kinesiology and hair analysis in the diagnosis of food allergy.
What is the treatment for a severe reaction?
Pre-loaded auto-injectors containing adrenaline are prescribed for people believed to be at risk of
anaphylaxis. Adrenaline is referred to in some countries as epinephrine, which is the internationally
recognised term for adrenaline.
Because severe allergic reactions can occur rapidly, the prescribed auto-injector must be readily available at
all times. The injection should be given as soon as any symptoms of anaphylaxis are present. If in doubt, give
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 3
adrenaline. A second dose should be given after 5-10 minutes if symptoms of anaphylaxis remain, or if there
is any doubt about whether the symptoms have improved.
An ambulance must be called immediately following an injection of adrenaline, even if there is immediate
improvement. The emergency service operator must be told the person is suffering from anaphylaxis and
needs to be attended by paramedics.
If the person’s condition deteriorates after making the initial 999 call, a second call to the emergency services
should be made to ensure an ambulance has been dispatched.
The matter of how many auto-injectors you should carry is addressed later in this Factsheet (“How many
auto-injectors should I carry?”).
How does adrenaline work?
Adrenaline acts quickly to open up the airways, stop swelling and raise the blood pressure. To allow it to work
most effectively, it should be administered as soon as anaphylaxis is suspected.
It is difficult to prove categorically that adrenaline saves lives and studying severe reactions in research is
difficult because of the speed with which anaphylaxis can occur. This uncertainty was acknowledged in a
major review of the medical literature on the use of adrenaline for anaphylaxis (Sheikh et al, Cochrane
Collaboration, 2011). Nevertheless, we are aware of a large amount of anecdotal evidence showing that most
people dying from anaphylaxis did not receive prompt treatment with adrenaline and further evidence
showing that people have recovered quickly when adrenaline was given. In our opinion, this provides strong
evidence for the effectiveness of adrenaline.
What auto-injectors are available?
Pre-loaded adrenaline auto-injectors – Emerade®, EpiPen® or Jext® – are available on prescription for those
thought to be at risk of a severe reaction.
You can visit their individual websites for information:
www.emerade-bausch.co.uk
www.epipen.co.uk
www.jext.co.uk
If you carry adrenaline you should check the expiry dates of your auto-injector at regular intervals. The three
injector companies listed above all send out expiry date reminders to anyone who registers for this.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 4
In the case of children, you should check whether a growth spurt means the child should move up from a
“Junior” device (0.15mg) to a standard strength one (0.3mg). This is necessary once the child reaches 25kg.
How many auto-injectors should I carry?
In 2014, the UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) advised that anyone who is
at risk of suffering anaphylaxis should always have at least two adrenaline auto-injector devices immediately
available. The MHRA report said: “It is acknowledged that in some cases, a single injection is not sufficient to
achieve a response for a number of reasons, including severity of attack as well as the possibility that a dose
has not been effectively administered; a second injection may therefore be needed.” The Anaphylaxis
Campaign supports this view.
In cases where the risk of anaphylaxis is thought to be low, there is a difference of opinion among members of
the medical community. While some allergy specialists agree that two auto-injectors must always be
immediately available (in line with the MHRA report), others believe it is sufficient to have one device
available, arguing that one injection is likely to be enough to treat the symptoms until emergency medical
help arrives.
This is a matter that you should discuss with your allergy specialist. To read the MHRA’s 2014 review, see the
references near the bottom of this page.
What increases the risk of a severe reaction?
Although it does not necessarily follow that each reaction is worse than the one before, there are times when
you may be particularly vulnerable and at increased risk of a severe reaction. Times when you need to be
particularly careful to avoid the trigger allergen include:
• If you have asthma that is poorly controlled
• If you are suffering from an infection, or have recently had one
• If you exercise just before or just after contact with the allergen
• If you are also suffering from aeroallergen symptoms, such as hay fever (see Vetander et al 2012)
• During times of emotional stress
• If you have been drinking alcohol
If you are allergic to a food, the amount eaten is also important as the more you consume, the worse the
reaction is likely to be.
The way the allergen is presented in the food is also important. For example, peanut allergens already
dissolved in Satay sauce, curry sauce or mayonnaise (or plant allergens in smoothies) can cause much worse
throat swelling than when the whole food needs to be chewed first to extract the allergen.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 5
Make sure you remain vigilant on special occasions including holidays or times of celebration, such as
weddings, buffets, parties or religious festivals.
What can I do to protect myself?
1. If you have asthma as well as allergies, make sure your asthma is well managed. If you have poorly
controlled asthma, there is a higher likelihood of any allergic reaction becoming severe, (Pumphrey
and Gowland, 2007, and Noimark et al, 2012). You can take control of your asthma by knowing what
medicines to take, how much to take and when to take them. See your GP or asthma nurse for advice
on this crucial point and to obtain an asthma management plan to help you self-manage.
2. If you have been prescribed adrenaline, carry it at all times – no exceptions.
3. Think ahead. Write out an emergency allergy action plan in advance. Make sure those around you
know how and when to administer the adrenaline. Practise regularly with a trainer device. The BSACI
has Allergy Action Plans for children available to download from its website. Information for
anaphylaxis in school children can be found at www.sparepensinschools.uk.
What should I do if I think I am having a severe reaction?
Use your adrenaline device without delay if you believe the reaction could be anaphylaxis. If you can’t breathe
or can’t stand you should sit or lie on the floor – whichever is the most comfortable position for you at the
time – and administer adrenaline as you should have been shown. Then dial 999 immediately or get someone
else to do it. If feeling very faint it may help to raise your legs against a wall. If vomiting you should lie on your
side.
Your allergist should help you understand in advance what symptoms provide a signal that a severe reaction
is occurring. Some people worry that adrenaline may be harmful, but evidence supports the safety of
prescribed adrenaline devices so long as they are used correctly (Sheikh et al, Cochrane Collaboration, 2011).
Always consider anaphylaxis as a possibility in someone with known food allergy who has sudden breathing
difficulty.
Click here to read our separate Factsheet on adrenaline.
Biphasic anaphylaxis
If you have anaphylaxis, you will need to be observed in hospital after you have recovered. This is because in
around 1 in 20 cases, a second ‘wave’ of symptoms can develop. This is referred to as a biphasic reaction.
Around half of biphasic reactions occur within 6-12 hours of the initial reaction (Lee et al, 2015). The length of
the observation period should be determined by the treating doctor.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 6
Does the risk of anaphylaxis get less over time?
There is no evidence that the risk of anaphylaxis gets less over time; however, some people will outgrow their
allergies over time. This is more common in young children, particularly those allergic to cow’s milk, egg and
wheat.
What is Mastocytosis?
In most cases of anaphylaxis there is a trigger such as a food, drug, insect sting or some other agent, but
anaphylaxis can also occur in people who have a very rare condition called Mastocytosis, which is caused by
too many ‘mast cells’ gathering in the tissues of the body. These are the main cells that release histamine and
other chemicals involved in allergic reactions, causing symptoms such as a skin rash, itchy skin and
anaphylaxis. If you have this very rare condition, it’s important that your doctor identifies Mastocytosis as the
cause of your symptoms. Further information:
http://www.nhs.uk/conditions/Mastocytosis/Pages/Introduction.aspx
Anaphylaxis: the key messages
Anaphylaxis is serious but, in our view, it is manageable. With a calm but committed attitude you will
certainly cope. Remember these important points:
• If you are at risk, see your GP and ask for a referral to an allergy clinic. Guidelines have been issued by
NICE showing what should be expected from your doctor. See www.nice.org.uk/guidance/cg134
• If you are prescribed an adrenaline injector, learn how to use it and carry it everywhere at all times.
• Do your research. If the allergen that affects you is a food, read food labels scrupulously and ask
direct questions wherever food is served.
References
Lee, S., Bellolio, M.F., Hess, E.P., Erwin, P., Murad, M.H., Campbell, R.L. (2015) Time of Onset and Predictors
of Biphasic Anaphylactic Reactions: A Systematic Review and Meta-analysis. J Allergy Clin Immunol Pract. 3
(3). p. 408-416
Medicines & Healthcare Products Regulatory Agency (2014) ‘Adrenaline auto-injectors: a review of clinical
and quality considerations’ Available from http://www.mhra.gov.uk/home/groups/comms-
ic/documents/websiteresources/con423091.pdf
Noimark, L., Wales, J., Du Toit, G., Pastacaldi, C., Haddad, D., Gardner, J., Hyer, W., Vance, G., Townshend,
C., Alfaham, M., Arkwrigh, P.D., Rao, R., Kapoor, S., Summerfield, A., Warner, J.O., Roberts G. (2012) The use
of adrenaline auto-injectors by children and teenagers. Clinical and Experimental Allergy. 42 (2). p.284-292.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 7
Pumphrey, R.S. & Gowland, M.H (2007). Further fatal allergic reactions to food in the United Kingdom.
Journal of Allergy and Clinical Immunology. 119. (4). 1018-1019.
Royal College of Pathologists, Lay Advisory Committee. (2002). Allergy and Allergy Tests: A Guide for
Patients and Relatives.
Sheikh, A., Shehata,Y.A., Brown, S.G.A., Simons, F.E.R. (2011) Adrenaline (epinephrine) for the treatment of
anaphylaxis with and without shock (review). The Cochrane Collaboration
Vetander, M., Helander, D., Flodstrom, C., Ostblom, E., Alfven, T., Ly, D.H., Hedlin, G., Lilja, G., Nilsson, C.,
Wickman, M. (2012) Anaphylaxis and reactions to foods in children: a population-based case study of
emergency department visits. Clinical and Experimental Allergy. 42 (4):p.568-577.
NICE guidelines
NICE (2011). Diagnosis and assessment of food allergy in children and young people in primary care and
community settings (CG116). http://guidance.nice.org.uk/CG116
NICE (2014). Anaphylaxis: assessment to confirm an anaphylactic episode and the decision to refer after
emergency treatment for a suspected anaphylactic episode (CG134). www.nice.org.uk/guidance/cg134
Reviewers
This Factsheet has been peer reviewed by Dr Paul Turner, Clinical Senior Lecturer in the Section of Peadiatrics
(Department of Medicine), Imperial College, London; and Dr Paul Williams, Consultant Clinical Immunologist,
Department of Immunology, University Hospital of Wales. We are not aware of any relevant disclosures that
would need to be made in respect of their reviews of this Factsheet.
Disclaimer – The information provided in this Factsheet is given in good faith. Every effort has been taken
to ensure accuracy. All patients are different, and specific cases need specific advice. There is no
substitute for good medical advice provided by a medical professional.
About the Anaphylaxis Campaign: Supporting people at risk of severe allergies
The Anaphylaxis Campaign is the only UK wide charity to exclusively meet the needs of the growing numbers
of people at risk from severe allergic reactions (anaphylaxis) by providing information and support relating to
foods and other triggers such as latex, drugs and insect stings. Our focus is on medical facts, food labelling,
risk reduction and allergen management. The Campaign offers tailored services for individual, clinical
professional and corporate members.
Visit our website www.anaphylaxis.org.uk and follow us on Twitter @Anaphylaxiscoms.
Anaphylaxis the Basic Facts Factsheet February 2019
Document Reference ACFS22 2019V4
Next review date February 2022
© Anaphylaxis Campaign 2019 8
You might also like
- VHA Code of IntegrityDocument28 pagesVHA Code of IntegrityFedSmith Inc.No ratings yet
- FAMILY NURSING CARE PLAN - AsthmaDocument1 pageFAMILY NURSING CARE PLAN - AsthmaJULIANNE BAYHON80% (5)
- Hypoglycaemia Acute Management ABCDEDocument11 pagesHypoglycaemia Acute Management ABCDESSNo ratings yet
- Ryan M. Carvalho: Career Objective: EducationDocument3 pagesRyan M. Carvalho: Career Objective: EducationddadNo ratings yet
- Nursing CatalogDocument27 pagesNursing Catalogrrockel100% (1)
- Critical Care NursingDocument12 pagesCritical Care NursingMoni Mbumba MelekeNo ratings yet
- Idiopathic Anaphylaxis 2021 v4Document10 pagesIdiopathic Anaphylaxis 2021 v4Cheyenne KruseNo ratings yet
- Idiopathic Anaphylaxis 2021 v5Document10 pagesIdiopathic Anaphylaxis 2021 v5RoundaboutNo ratings yet
- Exercise Induced Anaphylaxis-2019-V4Document6 pagesExercise Induced Anaphylaxis-2019-V4RoundaboutNo ratings yet
- Xis November 6, 2010Document61 pagesXis November 6, 2010bampugoNo ratings yet
- Anaphylaxis Resource Information and Lesson Plan Grades 4-6: Safe S A F EDocument10 pagesAnaphylaxis Resource Information and Lesson Plan Grades 4-6: Safe S A F EJefferson F. IberaNo ratings yet
- When To See A Doctor: Seek Emergency Medical HelpDocument4 pagesWhen To See A Doctor: Seek Emergency Medical HelpMaria Virginia FernandezNo ratings yet
- 1 Anaphylaxis Anaphylaxis Is A Life-Threatening TypeDocument9 pages1 Anaphylaxis Anaphylaxis Is A Life-Threatening TypeCraigNo ratings yet
- Clinical Aspects of Anaphlyaxis: DiagnosisDocument4 pagesClinical Aspects of Anaphlyaxis: Diagnosismaheen akramNo ratings yet
- AllergiesDocument9 pagesAllergiesClark Angelo JuanNo ratings yet
- What Is Allergy?: Ascia Information For Patients, Consumers and CarersDocument2 pagesWhat Is Allergy?: Ascia Information For Patients, Consumers and Carersvineeth84No ratings yet
- What Is AnaphylaxisDocument13 pagesWhat Is AnaphylaxisJohn SolivenNo ratings yet
- Anaphylactic ShockDocument29 pagesAnaphylactic ShockHIND100% (7)
- Emergency Medical Services Agency Lessons Learned: To: AlDocument4 pagesEmergency Medical Services Agency Lessons Learned: To: AlMega MuzdalifahNo ratings yet
- Anaphylaxis Part ADocument4 pagesAnaphylaxis Part ASojiNo ratings yet
- AnaphyDocument6 pagesAnaphyJefferson PaloyoNo ratings yet
- Shock Concept MapDocument2 pagesShock Concept MapElizabeth GarretsonNo ratings yet
- How Common Is Anaphylaxis?Document1 pageHow Common Is Anaphylaxis?Choong Cheng LounNo ratings yet
- Anaphylactic ShockDocument7 pagesAnaphylactic Shockapi-302126807No ratings yet
- Allergic Reaction: Under Supervision Prof. Nagwa Mahmoud El KobbiaDocument24 pagesAllergic Reaction: Under Supervision Prof. Nagwa Mahmoud El KobbiamorsiNo ratings yet
- Sudden IllnessesDocument26 pagesSudden IllnessesHesedh Jireh MartinNo ratings yet
- Allergies 1Document75 pagesAllergies 1asdfNo ratings yet
- Board Prep Emergency Ingestions Dec.2018Document46 pagesBoard Prep Emergency Ingestions Dec.2018Emily EresumaNo ratings yet
- Anaphylaxis Copy1Document22 pagesAnaphylaxis Copy1MunishNo ratings yet
- Symptoms: Allergic Reaction Medications Epinephrine Anaphylaxis Allergic Reaction Blood PressureDocument3 pagesSymptoms: Allergic Reaction Medications Epinephrine Anaphylaxis Allergic Reaction Blood Pressurejohn mendozaNo ratings yet
- First Aid For Allergic ReactionsDocument4 pagesFirst Aid For Allergic ReactionsIwan SetiawanNo ratings yet
- AnaphylaxisDocument10 pagesAnaphylaxisMadyline VictoryaNo ratings yet
- The Healthy Baby Gut Guide: Prevent Allergies, Build Immunity and Strengthen Microbiome Health From Day OneFrom EverandThe Healthy Baby Gut Guide: Prevent Allergies, Build Immunity and Strengthen Microbiome Health From Day OneNo ratings yet
- 5 Common Allergy MythsDocument2 pages5 Common Allergy MythsAbigail CoNo ratings yet
- ASCIA Anaphylaxis Training Resources NOV05Document23 pagesASCIA Anaphylaxis Training Resources NOV05keziahmaterschl2023No ratings yet
- FoodallergyDocument40 pagesFoodallergyapi-309082881No ratings yet
- AllergiesDocument12 pagesAllergiesKhushbu JainNo ratings yet
- Mustard Allergy: The FactsDocument5 pagesMustard Allergy: The FactsAnonymous GBge2ED1ONo ratings yet
- Drug AllergiesDocument3 pagesDrug AllergiesakbarNo ratings yet
- IMMUNOLOGYDocument11 pagesIMMUNOLOGYKiran ShahNo ratings yet
- Anaphylaxis TADocument54 pagesAnaphylaxis TAUriko ZoeNo ratings yet
- Anaphylaxis - First AidDocument3 pagesAnaphylaxis - First Aidsamanthafcooper_2753No ratings yet
- Hypoglycaemia - Acute Management - AbcdeDocument8 pagesHypoglycaemia - Acute Management - Abcderjohn 7No ratings yet
- Case Study For AllergyDocument3 pagesCase Study For AllergyGabbii CincoNo ratings yet
- BeSAFEBrochure PDFDocument2 pagesBeSAFEBrochure PDFPelmark G BalidiongNo ratings yet
- Allergies - Illnesses & Conditions - NHS InformDocument20 pagesAllergies - Illnesses & Conditions - NHS Informdavid gwyenrpNo ratings yet
- 2.first Aid Chapter-2Document7 pages2.first Aid Chapter-2Mohamed BinNo ratings yet
- Allergies Takunda Makondo 5th SemesterDocument11 pagesAllergies Takunda Makondo 5th SemestermakondotakundaNo ratings yet
- Guia Anafilaxia Niños y Adolescentes PacientesDocument8 pagesGuia Anafilaxia Niños y Adolescentes PacientesMariana Martinez LechugaNo ratings yet
- MaceeDocument40 pagesMaceeKaryl Anne LantingNo ratings yet
- Oral Allergy Version 8 Formatted With AC Logo and Name UpdatedDocument6 pagesOral Allergy Version 8 Formatted With AC Logo and Name UpdatedGlowstarNo ratings yet
- Paeds Complete PDFDocument176 pagesPaeds Complete PDFjljoioiuNo ratings yet
- Boado, M.A (Common Allergic Reaction and Stinging Insect)Document8 pagesBoado, M.A (Common Allergic Reaction and Stinging Insect)Melody BoadoNo ratings yet
- Allergies: A Protective Mechanism Out of ControlDocument29 pagesAllergies: A Protective Mechanism Out of Controlडा. सत्यदेव त्यागी आर्यNo ratings yet
- Allergies and HypersensitivityDocument14 pagesAllergies and HypersensitivityBabar MushtaqNo ratings yet
- By Mayo Clinic StaffDocument5 pagesBy Mayo Clinic StaffTry Febriani SiregarNo ratings yet
- Allergic ReactionsDocument12 pagesAllergic Reactionsvorticella12No ratings yet
- Anaphylaxis Articulo CompletoDocument6 pagesAnaphylaxis Articulo CompletoFrancelia Quiñonez RuvalcabaNo ratings yet
- Anaphylaxis (Case)Document4 pagesAnaphylaxis (Case)drkmwaiNo ratings yet
- ДокументDocument3 pagesДокументNura지민No ratings yet
- Allergies and Asthma TempDocument3 pagesAllergies and Asthma TempKonie LappinNo ratings yet
- Food Allergies and Pollen AllergiesDocument8 pagesFood Allergies and Pollen AllergiesYujenNo ratings yet
- Allergies: Understand and Manage Your AllergiesDocument44 pagesAllergies: Understand and Manage Your AllergieseeeNo ratings yet
- 3E Food AllergiesDocument12 pages3E Food Allergiesngd03122007No ratings yet
- Medical Emergencies AnaphylaxisDocument8 pagesMedical Emergencies AnaphylaxisLina Na'ilahNo ratings yet
- Materi PerkuliahanDocument69 pagesMateri PerkuliahanRirin RiriNo ratings yet
- The Gemini Virtual ClinicDocument19 pagesThe Gemini Virtual ClinicKritika SoniNo ratings yet
- Surgical Nursing Final PDFDocument26 pagesSurgical Nursing Final PDFAnuj Misra100% (2)
- CDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Document9 pagesCDC - Guidelines For Environmental Infection Control in Health-Care Facilities (CDC, 2003)Kesehatan LingkunganNo ratings yet
- OTC wv1Document42 pagesOTC wv1Sheena GagarinNo ratings yet
- What Is EHealthDocument64 pagesWhat Is EHealthAshvini GoelNo ratings yet
- National ConferenceDocument3 pagesNational Conferencelaveena aswaleNo ratings yet
- Project Proposal Purchase of CBRDocument3 pagesProject Proposal Purchase of CBRAida Potacag BuasenNo ratings yet
- Ah102 Syllabus 20171109Document7 pagesAh102 Syllabus 20171109api-384628971No ratings yet
- 2019 JSNA FinalDocument92 pages2019 JSNA Finalhiruni01No ratings yet
- Comparative Table Low Molecular Weight Heparins 1 2Document2 pagesComparative Table Low Molecular Weight Heparins 1 2Cosmin RazvanNo ratings yet
- FNCP (Hypertension)Document3 pagesFNCP (Hypertension)Jose Emmanuel Ribaya RuivivarNo ratings yet
- QUALISDocument31 pagesQUALISjopepinho5796No ratings yet
- Atfm Logbook m01cvs - Shrirajeswariintake13Document18 pagesAtfm Logbook m01cvs - Shrirajeswariintake13Shri VKNo ratings yet
- Prophetic Medicine Is The Cheapest, Safest and The Best Remedy in The Prevention and Treatment of Hypertension (High Blood Pressure) - A Mini ReviewDocument6 pagesProphetic Medicine Is The Cheapest, Safest and The Best Remedy in The Prevention and Treatment of Hypertension (High Blood Pressure) - A Mini ReviewCoronavirus COVID-19No ratings yet
- English For Informatics EngineeringDocument32 pagesEnglish For Informatics EngineeringDiana Urian100% (1)
- Introduction To Implant DentistryDocument106 pagesIntroduction To Implant DentistryFed Espiritu Santo GNo ratings yet
- Guideline AnesthesiaDocument31 pagesGuideline AnesthesiaMuhammad Izzatul Naim ZainuddinNo ratings yet
- Test Bank For 3 2 1 Code It 2020 8th Edition Michelle GreenDocument37 pagesTest Bank For 3 2 1 Code It 2020 8th Edition Michelle Greengeorgiannawiegardpro100% (17)
- Case StudyDocument5 pagesCase StudyKadiah KamaraNo ratings yet
- MH Assessment TemplateDocument2 pagesMH Assessment TemplatetakemebrickNo ratings yet
- Skills For Normal Vaginal Delivery NSVD 1Document1 pageSkills For Normal Vaginal Delivery NSVD 1Jewel Ann NuñezNo ratings yet
- Bacteriological Profile of Infections in Burns Unit - Plastic and Reconstructive Surgery Department - Mohammed Vi Chu MarrakechDocument7 pagesBacteriological Profile of Infections in Burns Unit - Plastic and Reconstructive Surgery Department - Mohammed Vi Chu MarrakechIJAR JOURNALNo ratings yet
- Physical Activity and Mental Health: Current ConceptsDocument14 pagesPhysical Activity and Mental Health: Current ConceptsCamilo RinconNo ratings yet
- Chapter 25 (Caring) ReviewerDocument7 pagesChapter 25 (Caring) ReviewerCarolyn Moquerio-serniculaNo ratings yet