Professional Documents
Culture Documents
Administering An Intradermal Injection.16
Administering An Intradermal Injection.16
Uploaded by
Fazil BilalOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Administering An Intradermal Injection.16
Administering An Intradermal Injection.16
Uploaded by
Fazil BilalCopyright:
Available Formats
CLINICAL
DO’S & DON’TS
Administering an intradermal injection
BY GAYLA H. LOVE, RN, CCM, BSN
AN INTRADERMAL injection may be given for diagnostic purposes, such as allergy or tuberculosis testing. Medica-
tion injected into the dermis is absorbed slowly because of this skin layer’s limited blood supply.
DO
• Gather equipment, including the ordered medication and a tuberculin syringe with a
Downloaded from http://journals.lww.com/nursing by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdgGj2MwlZLeI= on 07/09/2021
26- or 27-gauge, 1⁄2” to 3⁄8” needle.
• Verify the order. Check the medication expiration date and assess the patient for con-
traindications, including allergies. Ask her if she’s ever had an injection reaction.
• Draw up the correct medication dose aseptically in a syringe.
• Perform hand hygiene, explain the procedure to the patient, and put on gloves.
• Select an appropriate injection site, rotating the site if necessary. The first
choice is usually the ventral aspect of the forearm because it’s relatively
hairless. If you can’t use the forearm, consider the upper back or a subcu-
taneous injection site.
• Instruct your patient to extend her arm if you use the ventral aspect of
the forearm. Support her elbow and forearm on a flat surface and clean the
injection site.
§ Pull the skin taut with your nondominant hand and slowly insert the
needle, bevel up, at a 5- to 15-degree angle, until the bevel is just under
the epidermis.
§ Inject the medication slowly. You’ll immediately see a wheal or bubble-
like area on the skin’s surface.
• Remove the needle and apply gentle pressure to the site with an alcohol
swab or 2x2 gauze pad. Using a skin marker, draw a circle around the in-
jection site.
• Assess the injection site and observe the patient for adverse drug events
(ADEs), such as difficulty breathing.
BIRCK COX
• Discard equipment properly, remove your gloves, and perform hand hy-
giene.
• Document the medication administration and the patient’s response according to facility
policy. Note any ADEs and actions taken.
• Reassess the reaction at the site according to facility policy; for example, 48 to 72 hours
after injection.
DON’T
• Don’t choose an injection site that’s inflamed, burned, or hairy, or that has a lesion
or traumatic injury.
• Don’t administer more than 0.1 ml intradermally without questioning and confirm-
ing the order.
• Don’t massage the site after giving the injection because doing so can cause a false-
positive result.‹›
SELECTED REFERENCES
Rice J. Medications and Mathematics for the Nurse, 9th edition. Clifton Park, N.Y., Thomson Delmar Learning, 2002.
White L. Foundations of Nursing, 2nd edition. Clifton Park, N.Y., Thomson Delmar Learning, 2005.
Gayla H. Love is a practical-nursing instructor at Griffin (Ga.) Technical College, and she’s also a nurse for Medical Staffing Network in
Atlanta, Ga. Richard L. Pullen, Jr., RN, EdD, coordinates Clinical Do’s & Don’ts, which illustrates key clinical points for a common nursing pro-
cedure. Because of space constraints, it’s not comprehensive.
20 Nursing2006, Volume 36, Number 6 www.nursing2006.com
You might also like
- Nursing Care Plan - BronchitisDocument2 pagesNursing Care Plan - Bronchitisderic94% (36)
- Clinical Case Scenario 6Document17 pagesClinical Case Scenario 6Sean Menard Flores100% (1)
- Health Teaching Plan For Dengue Hemorrhagic FeverDocument3 pagesHealth Teaching Plan For Dengue Hemorrhagic Fevershiramu100% (5)
- Skill Checklist Applying An Extremity RestraintDocument2 pagesSkill Checklist Applying An Extremity RestraintAsep BageurNo ratings yet
- Basic Microblading ManualDocument12 pagesBasic Microblading ManualMaria Rina100% (6)
- Anatomical Landmarks For Injecting With Botulinum ToxinsDocument6 pagesAnatomical Landmarks For Injecting With Botulinum ToxinsAnna0% (1)
- Day 3 Activity: Nursing Care Plan: College of Health SciencesDocument6 pagesDay 3 Activity: Nursing Care Plan: College of Health SciencesAngelica Charisse BuliganNo ratings yet
- OxacillDocument1 pageOxacillnerissa_villanueva3523No ratings yet
- Symbols Glossary: S S T E T S R S TDocument9 pagesSymbols Glossary: S S T E T S R S TFirman UmatiNo ratings yet
- Ncm103rle - Midterm ReviewerDocument16 pagesNcm103rle - Midterm RevieweraragonjonathanryanabcomNo ratings yet
- Discharge PlanDocument4 pagesDischarge PlanVillanueva NiñaNo ratings yet
- Midterm NGT InsertionDocument5 pagesMidterm NGT InsertionMaria Kyla VicenteNo ratings yet
- Administering IntradermalDocument28 pagesAdministering IntradermalSaul Remus Q. DasmariñasNo ratings yet
- Subcutaneous InjectionDocument16 pagesSubcutaneous InjectionNani KicchaNo ratings yet
- Hep BDocument4 pagesHep BHanniel MontecalboNo ratings yet
- IV InjectionDocument13 pagesIV Injectionnileshgarje555No ratings yet
- OSCE ProceduresDocument16 pagesOSCE ProceduresQueen ShNo ratings yet
- Group 1 - Nebulizations PDFDocument23 pagesGroup 1 - Nebulizations PDFScribdTranslationsNo ratings yet
- Nursing Process Focus: Patients Receiving Fluticasone (Flonase) Assessment Potential Nursing DiagnosesDocument2 pagesNursing Process Focus: Patients Receiving Fluticasone (Flonase) Assessment Potential Nursing DiagnosesHannah Lorraine GamayonNo ratings yet
- Removing Medication From An AmpuleDocument2 pagesRemoving Medication From An AmpuleMichael Bon MargajaNo ratings yet
- Parenteral InjectionsDocument42 pagesParenteral InjectionsAngelica AmandoNo ratings yet
- Administering An Intramuscular InjectionDocument11 pagesAdministering An Intramuscular InjectionRalf FiedalinoNo ratings yet
- NCP Med WingDocument4 pagesNCP Med WingACOB, Jamil C.No ratings yet
- Impaired Gas Exchange Related To Collection of Mucus in The Airways (Pneumonia) andDocument2 pagesImpaired Gas Exchange Related To Collection of Mucus in The Airways (Pneumonia) andBetina De JesusNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Objectives: Nursing Intervention Rationale: EvaluationDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Objectives: Nursing Intervention Rationale: EvaluationMaria Eliza AgustinoNo ratings yet
- Asthma NCPDocument4 pagesAsthma NCPMonique Sacherow BacherNo ratings yet
- Patient-Controlled Analgesia (PCA) Is An Interactive MethodDocument10 pagesPatient-Controlled Analgesia (PCA) Is An Interactive Methodrahtu suzi ameliaNo ratings yet
- NCP OperañaDocument3 pagesNCP OperañaOPERAñA ELLAYZA RB DECANONo ratings yet
- Brown and Yellow Scrapbook Brainstorm PresentationDocument17 pagesBrown and Yellow Scrapbook Brainstorm Presentationdh4rk08No ratings yet
- Suctioning Trache Care NebuDocument11 pagesSuctioning Trache Care NebuROLAND LAURENCE BARGO JARDIOLINNo ratings yet
- Diagnostic Studies For Musculoskeletal DisordersDocument16 pagesDiagnostic Studies For Musculoskeletal DisordersClarisse Anne QuinonesNo ratings yet
- Injection TechniquesDocument7 pagesInjection TechniquesLheo AngelesNo ratings yet
- NCM 109 Rle Procedure - NebulizationDocument6 pagesNCM 109 Rle Procedure - NebulizationRAZELLE JOY CATIAN RODRIGUEZNo ratings yet
- Routes of Drug Administration The Route of Administration Is Determined Primarily by The Properties of The DrugDocument6 pagesRoutes of Drug Administration The Route of Administration Is Determined Primarily by The Properties of The DrugNouman AsgharNo ratings yet
- NoskhaDocument4 pagesNoskhanoranhassanshams0No ratings yet
- Parenteral Medication - PPT 1Document78 pagesParenteral Medication - PPT 1Tatah Rasma A. HadjaliNo ratings yet
- Enteral Nutrition: Course OutlineDocument3 pagesEnteral Nutrition: Course OutlineAngeli IdrisNo ratings yet
- NCM 104 Rle Final TermDocument15 pagesNCM 104 Rle Final TermJiro Luis KatindigNo ratings yet
- Forms and Routes of Drug AdministrationDocument21 pagesForms and Routes of Drug AdministrationtabiNo ratings yet
- Name of Drugs Action Contraindication Adverse Effects Nursing ResponsibilitiesDocument8 pagesName of Drugs Action Contraindication Adverse Effects Nursing ResponsibilitiesReychelle ChecheNo ratings yet
- 3 Intravenous-TherapyDocument4 pages3 Intravenous-TherapyMarie Louise Nicole TuvillaNo ratings yet
- Removing A Nasogastric Tube22Document4 pagesRemoving A Nasogastric Tube22Ashraf QotmoshNo ratings yet
- Drug Study-Operating RoomDocument6 pagesDrug Study-Operating RoomkathzheinNo ratings yet
- Tucker 2018Document8 pagesTucker 2018kosikevinonuNo ratings yet
- Conceptual MapsDocument8 pagesConceptual MapsScribdTranslationsNo ratings yet
- Admin An IM InjectionsDocument2 pagesAdmin An IM InjectionsjepoiNo ratings yet
- Midterm ReviewerDocument16 pagesMidterm RevieweraragonjonathanryanabcomNo ratings yet
- Dave CourseworkDocument7 pagesDave CourseworkTrisha Isobel DaveNo ratings yet
- Administering Intramuscular InjectionDocument3 pagesAdministering Intramuscular InjectionJela Jane ArcalNo ratings yet
- Rle116gep - EentDocument10 pagesRle116gep - EentKM PanganibanNo ratings yet
- Complications of DMDocument8 pagesComplications of DMShem DelolaNo ratings yet
- Neonatal PneumoniaDocument1 pageNeonatal PneumoniaAlyssa Rose MacasiebNo ratings yet
- MOON Post-Operative Rotator Cuff Repair Immediate Therapy ProtocolDocument14 pagesMOON Post-Operative Rotator Cuff Repair Immediate Therapy ProtocolAhmed MashalyNo ratings yet
- Snippets in Surgery Vol 1: Illustrated Essentials of General SurgeryFrom EverandSnippets in Surgery Vol 1: Illustrated Essentials of General SurgeryRating: 5 out of 5 stars5/5 (1)
- Local Anesthesia Made Easy: Complete Guide on How to make your Local Anesthetic Procedure a Success (Including a List of Anesthetic Equipment and their Uses)From EverandLocal Anesthesia Made Easy: Complete Guide on How to make your Local Anesthetic Procedure a Success (Including a List of Anesthetic Equipment and their Uses)No ratings yet
- Differentiating Anesthesia Equipment: Identify and Understand Anesthesia Equipment in 1 Hour (Including the most popular manufacturers and suppliers to buy Anesthesia Equipment)From EverandDifferentiating Anesthesia Equipment: Identify and Understand Anesthesia Equipment in 1 Hour (Including the most popular manufacturers and suppliers to buy Anesthesia Equipment)No ratings yet
- Angioplasty, (Stent Dilatation) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAngioplasty, (Stent Dilatation) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Simulation To Practice: Developing Nursing Skills in Mental Health: An Australian PerspectiveDocument5 pagesSimulation To Practice: Developing Nursing Skills in Mental Health: An Australian PerspectiveFazil BilalNo ratings yet
- Germany (German: DeutschlandDocument44 pagesGermany (German: DeutschlandFazil BilalNo ratings yet
- European UnionDocument31 pagesEuropean UnionFazil BilalNo ratings yet
- West Germany: West Germany, Officially The Federal Republic of GermanyDocument38 pagesWest Germany: West Germany, Officially The Federal Republic of GermanyFazil BilalNo ratings yet
- William Hawes (Physician)Document3 pagesWilliam Hawes (Physician)Fazil BilalNo ratings yet
- Hazard System v0.3Document2 pagesHazard System v0.3akikumonNo ratings yet
- Ficha en Casa 03 de Junio-5°Document1 pageFicha en Casa 03 de Junio-5°Luis BarranzuelaNo ratings yet
- Robert Smith: Sr. Medical Sales RepresentativeDocument2 pagesRobert Smith: Sr. Medical Sales RepresentativeMukesh YadavNo ratings yet
- Folic Acid During COVID-19Document1 pageFolic Acid During COVID-19Muhammad HaneefNo ratings yet
- Curragh Post Primary School - Procedures 09Document4 pagesCurragh Post Primary School - Procedures 09api-161343455No ratings yet
- Statement of Account Revised For PcsoDocument1 pageStatement of Account Revised For PcsoST. AUGUSTINE HOSPITAL100% (1)
- Activity 2Document1 pageActivity 2Charlote Jennifer FetalinoNo ratings yet
- Woodhaven Senior Living Inspection Report - 9.24.19Document14 pagesWoodhaven Senior Living Inspection Report - 9.24.19NewsChannel 9 StaffNo ratings yet
- Development: Income and Other GoalsDocument3 pagesDevelopment: Income and Other GoalsRounak BasuNo ratings yet
- Lions Lub of Kathmandu Regency, President Report To Governor's First Advisory CommitteeDocument3 pagesLions Lub of Kathmandu Regency, President Report To Governor's First Advisory CommitteerajuNo ratings yet
- Ahmad Hasanul Fikri Mohd Yusoff ReportDocument8 pagesAhmad Hasanul Fikri Mohd Yusoff ReporthasanulfiqryNo ratings yet
- Specimen Collection & Handling Instructions: Combined Buccal/Bilateral Anterior Nasal CollectionDocument2 pagesSpecimen Collection & Handling Instructions: Combined Buccal/Bilateral Anterior Nasal CollectionLong NguyenNo ratings yet
- RLE Checklist Evaluation (Leopold's Maneuver)Document4 pagesRLE Checklist Evaluation (Leopold's Maneuver)Cameron De Guzman100% (1)
- Hifat 80a (Estandar) - Ficha TecnicaDocument6 pagesHifat 80a (Estandar) - Ficha TecnicaCamila CajicaNo ratings yet
- Perform Preventive Maintenance: Evidence GuideDocument6 pagesPerform Preventive Maintenance: Evidence GuidehamayunNo ratings yet
- ACI Formulations Limited: Nur Mohammad FerozDocument2 pagesACI Formulations Limited: Nur Mohammad FerozmahmudNo ratings yet
- ACC BCP COvid19 ImplementationDocument4 pagesACC BCP COvid19 ImplementationAnisa FauziahNo ratings yet
- Hse-Dvis-8 (2020 R1)Document2 pagesHse-Dvis-8 (2020 R1)JDNo ratings yet
- General Infection Control Audit Checklist - SafetyCultureDocument21 pagesGeneral Infection Control Audit Checklist - SafetyCultureHosam Gomaa100% (1)
- Dilg, Doh Launch Bida Ang May Disiplina' Campaign Urge Lgus To Organize Barangay Disiplina BrigadesDocument3 pagesDilg, Doh Launch Bida Ang May Disiplina' Campaign Urge Lgus To Organize Barangay Disiplina Brigadesjulnaser s. akmadNo ratings yet
- Revaclear: HFHD (High Flux) Convective (HDF) Poracton (Paes/Pvp, Bpa-Free)Document2 pagesRevaclear: HFHD (High Flux) Convective (HDF) Poracton (Paes/Pvp, Bpa-Free)AFRIANSYAHNo ratings yet
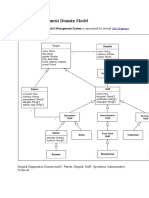
- Hospital Management Domain ModelDocument4 pagesHospital Management Domain Modelvinod kapateNo ratings yet
- Ntungamo District Service Commission: External Advert No. 1 of 2020Document1 pageNtungamo District Service Commission: External Advert No. 1 of 2020Stephen Odongo100% (1)
- Mock Test To Grade 10 Vietnam 2Document4 pagesMock Test To Grade 10 Vietnam 2Elvis TranNo ratings yet
- The International Journal of Periodontics & Restorative DentistryDocument7 pagesThe International Journal of Periodontics & Restorative DentistrytaniaNo ratings yet
- 004 Piling JSADocument4 pages004 Piling JSAIdada EzekielNo ratings yet
- Teaching Plan First Semester A.Y. 2020-2021: Indang, Cavite WWW - Cvsu.edu - PHDocument2 pagesTeaching Plan First Semester A.Y. 2020-2021: Indang, Cavite WWW - Cvsu.edu - PHYanis Emmanuelle LimNo ratings yet