Professional Documents
Culture Documents
DIT SoniyaR
DIT SoniyaR
Uploaded by
Laelannie MagpayoCopyright:
Available Formats
You might also like
- UEENEEI157A+Inotech Controls+Handbook - V2 - 3Document142 pagesUEENEEI157A+Inotech Controls+Handbook - V2 - 3Kim N Lewis100% (3)
- Poem AnalysisDocument4 pagesPoem AnalysisCharles Ting67% (3)
- Nur 403 Tni PaperDocument11 pagesNur 403 Tni Paperapi-369824515No ratings yet
- Dietplan Type2B Balanceddiet PDFDocument5 pagesDietplan Type2B Balanceddiet PDFMario The Coach100% (2)
- Guler Et Coll (2020) - DONEDocument8 pagesGuler Et Coll (2020) - DONEMaya HammoudNo ratings yet
- The Effectiveness of Quarter Turn From Prone in Maintaining Respiratory Function in Premature InfantsDocument7 pagesThe Effectiveness of Quarter Turn From Prone in Maintaining Respiratory Function in Premature InfantsAkmal ThariqNo ratings yet
- Thesis On Neonatal ResuscitationDocument5 pagesThesis On Neonatal Resuscitationtarasmithbaltimore100% (2)
- Neonatal NursingDocument5 pagesNeonatal Nursingmutmainatul mardiyah100% (1)
- The Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialDocument8 pagesThe Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialAndreas Arie WidiadiaksaNo ratings yet
- Doyle & Bradshaw - Sixty Golden MinutesDocument6 pagesDoyle & Bradshaw - Sixty Golden MinutesVillia DamayantieNo ratings yet
- Pain Relief During Labor and Delivery: A Brief 2013 UpdateDocument5 pagesPain Relief During Labor and Delivery: A Brief 2013 UpdateJheiczhietoot KibasNo ratings yet
- Going Home: Facilitating Discharge of The Preterm InfantDocument14 pagesGoing Home: Facilitating Discharge of The Preterm InfantYohanes DokaNo ratings yet
- Journal NicuDocument4 pagesJournal NicuMargaret LlavorNo ratings yet
- SA PerformanceDocument8 pagesSA Performancefernin96No ratings yet
- Problem StatementDocument15 pagesProblem StatementhuylimalaNo ratings yet
- Chapter 40 - Abril - CJDocument16 pagesChapter 40 - Abril - CJcarms abrilNo ratings yet
- Lung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFDocument8 pagesLung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFcesar juarezNo ratings yet
- 2017-Journal of Paediatrics and Child HealthDocument1 page2017-Journal of Paediatrics and Child HealthAna SopaNo ratings yet
- Delivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadDocument10 pagesDelivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadRaja SekarNo ratings yet
- MODEL OF PRACTICE TsaarDocument6 pagesMODEL OF PRACTICE TsaarCrystal Ann TadiamonNo ratings yet
- Basic EcgDocument19 pagesBasic EcgIrma SihotangNo ratings yet
- High-Flow Nasal Cannulae in Very Preterm Infants After ExtubationDocument9 pagesHigh-Flow Nasal Cannulae in Very Preterm Infants After ExtubationRiska Diene PratiwiNo ratings yet
- The Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesDocument5 pagesThe Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesJehangir AllamNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- Brief Resume of The Intended Work: "The Nation Walks On The Feet of Little Children."Document11 pagesBrief Resume of The Intended Work: "The Nation Walks On The Feet of Little Children."sr.kumariNo ratings yet
- Circulation 2015 Wyckoff S543 60Document18 pagesCirculation 2015 Wyckoff S543 60Kahfi Rakhmadian KiraNo ratings yet
- Neonatal Research PaperDocument5 pagesNeonatal Research Paperkrqovxbnd100% (1)
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Nursing Crib ThesisDocument8 pagesNursing Crib ThesisProfessionalCollegePaperWritersMcAllen100% (1)
- 2015 Neonatal Resuscitation AHADocument19 pages2015 Neonatal Resuscitation AHAJoyceAltamiranoEncisoNo ratings yet
- ResuscitationDocument18 pagesResuscitationIva NurilNo ratings yet
- Assessment of Initial Morbidity Patterns in Late Preterm Infants Relative To Those at TermDocument6 pagesAssessment of Initial Morbidity Patterns in Late Preterm Infants Relative To Those at TermInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 3 Killers Complications During Childbirth BriefDocument2 pages3 Killers Complications During Childbirth BriefAraz MuhammadaminNo ratings yet
- Effectiveness of Nesting On Posture and Movements Among Preterm BabiesDocument7 pagesEffectiveness of Nesting On Posture and Movements Among Preterm BabiesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Study of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Document6 pagesStudy of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Elison J PanggaloNo ratings yet
- 26 Device Improves Swallowing in Newborns: CommentDocument33 pages26 Device Improves Swallowing in Newborns: CommentWahyuni M. Ali MreNo ratings yet
- ObjectivesDocument73 pagesObjectivesJoanna Bee Rose MagyawiNo ratings yet
- Differences in The Swallowing Process of Newborns and HealthyDocument12 pagesDifferences in The Swallowing Process of Newborns and Healthysiramliw3No ratings yet
- Research Proposal - SammyDocument24 pagesResearch Proposal - SammyOfosu AugustineNo ratings yet
- Initial Resuscitation and Stabilization of The Periviable Neonate: The Golden-Hour ApproachDocument5 pagesInitial Resuscitation and Stabilization of The Periviable Neonate: The Golden-Hour ApproachwilmaNo ratings yet
- ProneDocument8 pagesPronesophiaNo ratings yet
- PAPER (ENG) - (Kelly B., 2007 NEZ) The First Year of Human Life Coordinating Respiration and NutritiveDocument7 pagesPAPER (ENG) - (Kelly B., 2007 NEZ) The First Year of Human Life Coordinating Respiration and NutritiveAldo Hip NaranjoNo ratings yet
- Clinical Outcomes of Snuggle Up Position Using Positioning Aids For Preterm (27-32 Weeks) InfantsDocument6 pagesClinical Outcomes of Snuggle Up Position Using Positioning Aids For Preterm (27-32 Weeks) InfantsMastifa HanasitaNo ratings yet
- Weight Gain in Preterm Low Birth Weight Infants With Multisensory InterventionDocument5 pagesWeight Gain in Preterm Low Birth Weight Infants With Multisensory Interventionagung setiawanNo ratings yet
- Assess The Effectiveness of Sensory Nursing Interventions On Neonatal Reflex and Reactivity Among Preterm Infants in Selected Setting, Nagercoil, K.K. DistrictDocument12 pagesAssess The Effectiveness of Sensory Nursing Interventions On Neonatal Reflex and Reactivity Among Preterm Infants in Selected Setting, Nagercoil, K.K. DistrictImpact JournalsNo ratings yet
- The Importance of The Right Factory Fake Bundle Management On The Fetal Distress CaseDocument7 pagesThe Importance of The Right Factory Fake Bundle Management On The Fetal Distress CaseAnnis Laella MegassariNo ratings yet
- Effect of CupDocument9 pagesEffect of CupInés Valero ArredondoNo ratings yet
- Pioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Document13 pagesPioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Kinjal Vasava100% (1)
- Skin To SkinDocument9 pagesSkin To SkinAsiatiNo ratings yet
- The Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUDocument11 pagesThe Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Surfactant For Respiratory Distress SyndromeDocument12 pagesSurfactant For Respiratory Distress Syndromesanjuy_garzaNo ratings yet
- The Effectiveness of Combination of Kangaroo Mother Care Method and Lullaby Music Therapy On Vital Sign Change in Infants With Low Birth WeightDocument8 pagesThe Effectiveness of Combination of Kangaroo Mother Care Method and Lullaby Music Therapy On Vital Sign Change in Infants With Low Birth Weightzaenab anissaNo ratings yet
- Baby Sleep Incidental Aspiration Case ReportDocument4 pagesBaby Sleep Incidental Aspiration Case ReportSebastian Jaén Vinueza SoteloNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- Nesting DN O2Document9 pagesNesting DN O2septiana dwi lestariNo ratings yet
- A Quasi Experimental Study To Evaluate The Effect of Prefeeding Oral Stimulation Program On Oral Feeding Skills Among Preterm Infants in Selected Hospitals, PunjabDocument29 pagesA Quasi Experimental Study To Evaluate The Effect of Prefeeding Oral Stimulation Program On Oral Feeding Skills Among Preterm Infants in Selected Hospitals, PunjabEditor IJTSRD100% (1)
- Intervencion Temprana SuccionDocument13 pagesIntervencion Temprana Succionjulianamd87No ratings yet
- BBLR 2Document6 pagesBBLR 2refiNo ratings yet
- Human Milk: Composition, Clinical Benefits and Future Opportunities: 90th Nestlé Nutrition Institute Workshop, Lausanne, October-November 2017From EverandHuman Milk: Composition, Clinical Benefits and Future Opportunities: 90th Nestlé Nutrition Institute Workshop, Lausanne, October-November 2017No ratings yet
- Menu and Product Knowledge Managemen TDocument55 pagesMenu and Product Knowledge Managemen TLaelannie Magpayo100% (1)
- Literature Review: Effect of Benson's Relaxation Therapy (BRT) On Post Caesarean Section Pain and StressDocument6 pagesLiterature Review: Effect of Benson's Relaxation Therapy (BRT) On Post Caesarean Section Pain and StressLaelannie MagpayoNo ratings yet
- Solution Brown Solution: Sample Used Time Oxidized Apple Banana Potato GuavaDocument7 pagesSolution Brown Solution: Sample Used Time Oxidized Apple Banana Potato GuavaLaelannie MagpayoNo ratings yet
- The Oath: Permissible Medical ExperimentsDocument3 pagesThe Oath: Permissible Medical ExperimentsLaelannie MagpayoNo ratings yet
- The Effect of Progressive Muscle Relaxation On PosDocument16 pagesThe Effect of Progressive Muscle Relaxation On PosLaelannie MagpayoNo ratings yet
- World Teachers' Day 2020: Teachers: Leading in Crisis, Reimagining The Future Concept NoteDocument5 pagesWorld Teachers' Day 2020: Teachers: Leading in Crisis, Reimagining The Future Concept NoteLaelannie MagpayoNo ratings yet
- Education in A BoxDocument3 pagesEducation in A BoxLaelannie MagpayoNo ratings yet
- Insights Into Digestion and Absorption of Major Nutrients in HumansDocument10 pagesInsights Into Digestion and Absorption of Major Nutrients in HumansLaelannie MagpayoNo ratings yet
- Nitrogenous Compounds in Blood and Urine-I: NPN and Urea: ArticleDocument3 pagesNitrogenous Compounds in Blood and Urine-I: NPN and Urea: ArticleLaelannie MagpayoNo ratings yet
- Questions For Discussion: (Financial Literacy) : Group TaskDocument3 pagesQuestions For Discussion: (Financial Literacy) : Group TaskLaelannie MagpayoNo ratings yet
- Media 49768e6 ccq6 4-0283Document12 pagesMedia 49768e6 ccq6 4-0283Laelannie MagpayoNo ratings yet
- Msds-Exp-09 CCLDocument2 pagesMsds-Exp-09 CCLLaelannie MagpayoNo ratings yet
- Experiment 3 LipidsDocument4 pagesExperiment 3 LipidsLaelannie MagpayoNo ratings yet
- Current Status, Research Trends, and ChallengesDocument23 pagesCurrent Status, Research Trends, and Challengesqgi-tanyaNo ratings yet
- Chapter 8 Supplemental Questions: E8-1 (Inventoriable Costs)Document7 pagesChapter 8 Supplemental Questions: E8-1 (Inventoriable Costs)Dyan NoviaNo ratings yet
- Decribing Connections Between Historical EventsDocument4 pagesDecribing Connections Between Historical Eventsapi-334916201No ratings yet
- KB Shape CodesDocument9 pagesKB Shape CodesPrashanth TNo ratings yet
- The 1 Catholic Mass in The PhilippinesDocument16 pagesThe 1 Catholic Mass in The PhilippinesRosalie AlitaoNo ratings yet
- Ics Lab Manual PDFDocument46 pagesIcs Lab Manual PDFEyes FlikerNo ratings yet
- Accounting Unit Additional Execerses AA025 Sem 2, 2019/2020Document5 pagesAccounting Unit Additional Execerses AA025 Sem 2, 2019/2020nur athirahNo ratings yet
- ARTI Refrigerant Database - Volume Two PDFDocument578 pagesARTI Refrigerant Database - Volume Two PDFAymanNo ratings yet
- Hopkins Verbal Learning Test Revised NorDocument13 pagesHopkins Verbal Learning Test Revised NorOscar Ariza CaroNo ratings yet
- English Chapter 5Document20 pagesEnglish Chapter 5Kumar sankar SNo ratings yet
- v2 SDO ISABELA LEARNING RECOVERY PLANDocument16 pagesv2 SDO ISABELA LEARNING RECOVERY PLANRoland Mark DumaliangNo ratings yet
- Windows Server ChecklistDocument116 pagesWindows Server Checklistravichandran_mcpNo ratings yet
- I04 U11 Conditionals & Reported SpeechDocument4 pagesI04 U11 Conditionals & Reported Speechmelgarejo1111No ratings yet
- 17 Reg-TocDocument1 page17 Reg-TocvanithaNo ratings yet
- Personal Nutrition 9th Edition Boyle Solutions ManualDocument32 pagesPersonal Nutrition 9th Edition Boyle Solutions Manualthoabangt69100% (29)
- CPAR LessonDocument2 pagesCPAR LessonAnabelle MoyamoyNo ratings yet
- Research and Innovation in Higher Education-EPP-1-2018-1-AT-EPPKA1-JMD-MOBDocument2 pagesResearch and Innovation in Higher Education-EPP-1-2018-1-AT-EPPKA1-JMD-MOBTabah Ghifary Diniya (Ghif)No ratings yet
- March 6 - Artificial Selection PresentationsDocument3 pagesMarch 6 - Artificial Selection Presentationsapi-503273730No ratings yet
- ShowPDF Paper - AspxDocument14 pagesShowPDF Paper - AspxShawkat AhmadNo ratings yet
- NIV Excerpt PDFDocument57 pagesNIV Excerpt PDFAnonymous tSYkkHToBPNo ratings yet
- Cetirizine Degradation ProductsDocument7 pagesCetirizine Degradation ProductsASHOK KUMAR LENKANo ratings yet
- P Block Elements Group 15Document79 pagesP Block Elements Group 1515 Kabir Sharma 10 HNo ratings yet
- Yak 52 Maitenance ManualDocument36 pagesYak 52 Maitenance ManualAvionicsfNo ratings yet
- Individual Assignment: Retail ManagementDocument11 pagesIndividual Assignment: Retail ManagementTijo ThomasNo ratings yet
- +english Test Prac Poison Tree-AnswersDocument5 pages+english Test Prac Poison Tree-AnswersLouise Francis100% (1)
DIT SoniyaR
DIT SoniyaR
Uploaded by
Laelannie MagpayoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DIT SoniyaR
DIT SoniyaR
Uploaded by
Laelannie MagpayoCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/342160774
Effectiveness of prone and supine position on respiratory pattern among
neonates
Article in Drug Invention Today · June 2020
CITATIONS READS
0 192
3 authors, including:
Jagadeeswari Jayaseelan
Saveetha University
16 PUBLICATIONS 1 CITATION
SEE PROFILE
All content following this page was uploaded by Jagadeeswari Jayaseelan on 14 June 2020.
The user has requested enhancement of the downloaded file.
Research Article
Effectiveness of prone and supine position on respiratory
pattern among neonates
J. Jagadeeswari*, R. Soniya
ABSTRACT
Background: Newborns have irregular breathing patterns that concern new parents. They can breathe fast, take long pauses
between breaths, and make unusual noises. A newborn takes 30–60 breaths per minute. This can slow down to 20 times per
minute while they sleep. At 6 months, babies breathe about 25–40 times per minute. Newborns can also take rapid breaths
and then pause for up to 10 s at a time. Aim: The present study aims are to assess the effectiveness of prone and supine
position on a respiratory pattern among of neonates with respiratory problems. Materials and Methods: The research design
for the study is pre-experimental research design with two group pre-test post-test design. Convenient sampling technique
was used to select samples. Semi-structured interview was used to collect demographic data and bio-physiological method
was to assess the respiratory pattern such as respiratory rate, respiratory depth, retraction, nasal flaring, and chest in drawing,
wheezing, and oxygen saturation. The babies in experimental group were divided into two groups and placed in supine and
prone position. After an hour, the respiratory pattern was re-assessed. Results: The study results show that the respiratory
pattern variable wheezing had shown a statistically significant difference between the prone and supine position with a Chi-
square value of 3.968 which was found to be statistically significant at P < 0.05. This indicates that prone position is more
effective than supine position among neonates. Conclusion: Prone position also helps in maintaining respiratory pattern,
especially oxygen saturation and helps in prompt recovery of the neonates from respiratory diseases.
KEY WORDS: Neonates, Prone position, Respiratory pattern, Supine position
INTRODUCTION care. Newborns have irregular breathing patterns that
concern new parents. They can breathe fast, take long
An infant whose birth weight <2500 g regardless of pauses between breaths, and make unusual noises. A
their gestational age is called low birth weight infants. newborn takes 30–60 times per minute. This can slow
Reduction in infant and child mortality is a major down to 20 times per minute while they sleep. At 6
goal of strategy to achieve health for all.[1] The major months, babies breathe about 25–40 times per minute.
contribution of infant death is by neonates which are
An adult, meanwhile, takes about 12–20 breaths per
a serious concern since nearly 5 million neonates
minute. Newborns can also take rapid breaths and then
die each year in the world, of which 96% are in the
pause for up to 10 s at a time.[5,6]
developing countries, effective reduction of such high
neonatal death rate remains a major global challenge Breathing difficulties are common immediately after
in 21st century.[2-4]
birth and during the first few hours of a baby’s life. More
Birth is a transition from a fluid environment to complex breathing problems a baby can experience
one where we breathe air. Breathing difficulties are are asphyxia, transient tachypnea, respiratory distress
common immediately after birth and during the first few syndrome, meconium aspiration, pneumothorax,
hours of life. However, some babies may experience pneumonia, and congenital lung malformations.
more complex breathing problems that require special Neonates have clinical symptoms breathing difficulties
displays classic clinical signs of respiratory distress
Access this article online regardless of the underlying cause. These consist
of tachypnea (respiratory rate >60 breaths⋅min−1),
Website: jprsolutions.info ISSN: 0975-7619
tachycardia (heart rate >160 beats⋅min−1), nasal
Department of Obstetrics and Gynecological Nursing, Saveetha College of Nursing, Saveetha Institute of Medical and
Technical Sciences, Saveetha University, Chennai, Tamil Nadu, India
*Corresponding author: J. Jagadeeswari, Department of Obstetrics and Gynecological Nursing, Saveetha College
of Nursing, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, Tamil Nadu, India.
Phone: +91-8056474788. E-mail: j.jagadeeswari@gmil.com
Received on: 12-01-2020; Revised on: 10-02-2020; Accepted on: 18-03-2020
Drug Invention Today | Vol 13 • Issue 7 • 2020 983
J. Jagadeeswari and R. Soniya
flaring, grunting, chest wall recessions (suprasternal, respiratory pattern among of neonates with respiratory
intercostal, and subcostal), cyanosis, and apnoea.[7] problems, and (3) to compare the effectiveness of
prone and supine position on a respiratory pattern
As nurses it’s our responsibility to maintain good among neonates.
respiratory and breathing pattern among the neonates.
Hence, the researcher felt the need to contribute MATERIALS AND METHODS
positioning practices in neonates to improve breathing
pattern. This study is to find out the effectiveness of A quantitative approach with a quasi-experimental
prone and supine position of newborns.[8] research design was used to conduct the study
in the neonatal ICU of Thiruvallur District Head
As newborn infants exhibit physiological and Quarter Government Hospital. Thirty samples were
behavioral signs of pain and stress that can selected using a convenience sampling technique.
be recognized by health-care professionals, The criteria for sample selection were low birth
pharmacological, and nonpharmacological resources weight infants with a weight between 1200 and
may be employed in the neonatal intensive care unit 2500, neonates admitted in NICU with spontaneous
(NICU) to manage such conditions. In this regard,
breathing with no need of assisting devices,
appropriate positioning is considered an important
neonates not treated with sedatives 24 h before the
nonpharmacological intervention in premature
intervention and neonates whose mothers who are
newborns admitted to NICU, and according to some
willing to participate in the study. The exclusion
studies, the frequency of stress behaviors is lower
criteria for the samples were neonates with no
when infants are placed in the prone position.[9]
major congenital defects or abnormal neurological
The positioning of infants is a simple and safe findings, including intraventricular hemorrhage;
therapeutic maneuver with prompt and demonstrable neonates should not have any birth complications
benefit. Early hospitalization, the prone position such as RDS and neurological problems in low
is best for pre-term infants and result in improved birth weight babies. The data collection period
oxygenation, better-tolerated feedings, and more was done with prior permission from the HOD of
organized sleep rest patterns. Infants exhibit less the Neonatology Department and ethical clearance
physical activity and energy expenditure when placed was obtained from the institution. The purpose of
in a prone position. Concluded that oxygenation was the study was explained to the samples with written
found to be significantly superior in the prone position informed consent was obtained from them. The
than in the supine position. They justified that prone demographic data were collected by using structured
ventilation, however, is not yet a standard practice questionnaire. The bio-physiological parameters
and it is reasonable to assume that optimized initial were assessed before position among both the
ventilation would lead to improve results in terms experimental groups. Then, babies in experimental
of shortened duration of ventilation and improved Group 1 were placed in supine and experimental and
survival.[10] Group 2 in prone position. After an hour, the bio-
physiological parameters were assessed among both
In 2001, Kornecki et al. concluded that oxygenation experimental groups. The data were analyzed using
was found to be significantly superior in the prone descriptive and inferential statistics. The sample
position than in the supine position. They justified characteristics were described using frequency and
that prone ventilation, however, is not yet a standard percentage. Pearson’s correlation coefficient was
practice and it is reasonable to assume that optimized used to assess the effectiveness of prone and supine
initial ventilation would lead to improved results position in the experimental groups. Chi-square used
in terms of shortened duration of ventilation and to associate the post-test level of posture comfort
improved survival.[11] with the selected demographic variables.
A study performed by Taccone et al. suggests a
nonsignificant 10% difference in mortality favoring RESULTS AND DISCUSSION
the prone group and a significantly greater proportion Section A: Sample Characteristics
of infants in the prone group experienced at least one
complication as compared to the supine group. They Among 15 samples in experimental Group 1 (prone
concluded that the rate of complications was almost position), most of them 7 (46.7%) were 11–20 months
3 times greater in the prone group than in the supine old, 8 (53.3%) were baby boy, 10 (66.7%) were
group.[12] weighing 1500–2001 g, 8 (53.3%) had an APGAR
score of 9–10, 10 (66.77%) were pre-term, 10 (66.7%)
A purpose of the study was (1) to assess the were born by cesarean section, 8 (53.3%) were second
respiratory pattern among of neonates, (2) to assess child, and 8 (53.3%) had no history of respiratory
the effectiveness of prone and supine position on a distress at birth.
984 Drug Invention Today | Vol 13 • Issue 7 • 2020
J. Jagadeeswari and R. Soniya
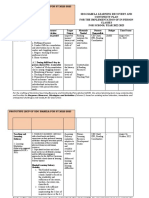
Table 1: Comparison of respiratory pattern among neonates in supine and prone position
Respiratory pattern Prone position Supine position Chi-square test
(f) (%) (f) (%)
Wheezing χ2=3.968
Absent 13 86.7 8 53.3 d.f=1
Minimal audible with stethoscope 2 13.3 7 46.7 P=0.046
Marked audible with stethoscope - - - - S*
*P<0.05, S: Significant
Among 15 samples in experimental Group 2 (supine Positioning according to a standard operating procedure
position), most of them 6 (40%) were 11–20 months was able to produce more positive responses in prone
old, 9 (60%) were baby girl, 8 (53.3%) were weighing and supine position groups during the intervention.[13]
2001–2500 g, 12 (80%) had an APGAR score of 9–10,
6 (40%) were term babies, 8 (53.3%) were born by CONCLUSION
normal delivery, 8 (53.3%) were a second child, and 8
(53.3%) had a history of respiratory distress at birth. This indicates that prone position is more effective than
supine position among neonates. Prone position also
Section B: Effectiveness of Prone and Supine helps in maintaining respiratory pattern, especially
Position on Respiratory Pattern among Neonates oxygen saturation, and helps in prompt recovery of
the neonates from respiratory diseases.
The present study results related to prone position
shows that among neonates, most of them 7 (46.7%)
were 11–20 months old, 8 (53.3%) were baby boy, 10 REFERENCES
(66.7%) were weighing 1500–2001 g, 8 (53.3%) had 1. Ahmed K, Malik A, Yousef W. Perinatal morbidity and mortality
an APGAR score of 9–10, 10 (66.77%) were pre-term, in case of preterm labour, an antegrade study conducted at lady
Willingdon hospitals, labour. Biomedical 2000;1:74-7.
10 (66.7%) were born by cesarean section, 8 (53.3%)
2. Korejo R, Butta S, Noorani KJ, Butta ZA. An audit and trends
were second child, and 8 (53.3%) had no history of of perinatal mortality at the jinnash postgraduate medical centre
respiratory distress at birth. Karachi. J Pak Med Assoc 2007;57:168-72.
3. Aly H. Respiratory disorders in the newborn: Identification and
The present study results related to supine position show diagnosis. Paediatr Rev 2004;25:201-8.
4. Gouna G, Rakza T, Kuissi E, Pennaforte T, Mur S, Storme L.
that among neonates, most of them 6 (40%) were 11–20 Positioning effects on lung function and breathing pattern in
months old, 9 (60%) were baby girl, 8 (53.3%) were premature newborns. J Pediatr 2013;162:1133-7.
weighing 2001–2500 g, 12 (80%) had an APGAR score 5. Eghbalian F. A comparison of supine and prone positioning
of 9–10, 6 (40%) were term babies, 8 (53.3%) were born on improves arterial oxygenation in premature neonates. J
Neonatal Perinatal Med 2014;7:273-7.
by normal delivery, 8 (53.3%) were second child, and 6. Ellsworth MA, Ulrich TJ, Carey WA, Colby CE, Ackerman MJ.
8 (53.3%) had a history of respiratory distress at birth. QTc interval prolongation and severe apneas associated with a
change in infant positioning. Pediatrics 2013;132:e1690-3.
Section C: Comparing the Effectiveness of Prone 7. Das H, Shaikh S, Kella N. Effect of prone versus supine
and Supine Position on Respiratory Pattern among position on oxygen saturation in patients with respiratory
distress in neonates. Pak J Med Sci 2011;27:1098-101.
Neonates 8. Ghorbani F, Asadollahi M, Valizadeh S. Comparison the effect
The study results show that the respiratory pattern of sleep positioning on cardiorespiratory rate in noninvasive
ventilated premature infants. Nurs Midwifery Stud 2013;2:182-7.
variable wheezing had shown a statistically significant 9. Alsaghir AH, Martin CM. Effect of prone positioning in patients
difference between the prone and supine position with with acute respiratory distress syndrome: A meta-analysis. Crit
a Chi-square value of 3.968 which was found to be Care Med 2008;36:603-9.
statistically significant at P < 0.05 level [Table 1]. 10. Sharma P, Arora S, Sarkar S, Puliyel J. A randomized
clinical trial to assess the effectiveness of prone position on
cardiorespiratory outcomes among infants with respiratory
This study is supported by Santos et al. (2017) conducted distress. MAMC J Med Sci 2016;2:81-8.
a study on “Physiological and behavioral effects of pre- 11. Kornecki A, Frndova H, Coates AL, Shemie SD. Prone position
term infant positioning in a neonatal intensive care is best for acute respiratory failure. AAP Grand Rounds
2001;5:48-9.
unit.” Twenty-four pre-term newborns with gestational
12. Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C,
age ≤32 weeks, who were randomly separated into four et al. Prone positioning in patients with moderate and severe
groups: Right side position, supine position, left side acute respiratory distress syndrome: A randomized controlled
position, and prone position during the intervention, trial. JAMA 2009;302:1977-84.
13. Alessandra S, Claudia V, Gladson B, Erica O, Claudia C,
heart rate decreased in the right side position, supine Ana G. Physiological and behavioural effects of preterm infant
position, and prone position. The respiratory rate positioning in a neonatal intensive care unit. Br J Midwifery
reduced in all positions and peripheral oxygen saturation 2017;25:647-54.
remained stable in most positions. Behavioral scores
Source of support: Nil; Conflicts of interest: None Declared
were reduced in supine, left side, and prone positions.
Drug Invention Today | Vol 13 • Issue 7 • 2020 985
View publication stats
You might also like
- UEENEEI157A+Inotech Controls+Handbook - V2 - 3Document142 pagesUEENEEI157A+Inotech Controls+Handbook - V2 - 3Kim N Lewis100% (3)
- Poem AnalysisDocument4 pagesPoem AnalysisCharles Ting67% (3)
- Nur 403 Tni PaperDocument11 pagesNur 403 Tni Paperapi-369824515No ratings yet
- Dietplan Type2B Balanceddiet PDFDocument5 pagesDietplan Type2B Balanceddiet PDFMario The Coach100% (2)
- Guler Et Coll (2020) - DONEDocument8 pagesGuler Et Coll (2020) - DONEMaya HammoudNo ratings yet
- The Effectiveness of Quarter Turn From Prone in Maintaining Respiratory Function in Premature InfantsDocument7 pagesThe Effectiveness of Quarter Turn From Prone in Maintaining Respiratory Function in Premature InfantsAkmal ThariqNo ratings yet
- Thesis On Neonatal ResuscitationDocument5 pagesThesis On Neonatal Resuscitationtarasmithbaltimore100% (2)
- Neonatal NursingDocument5 pagesNeonatal Nursingmutmainatul mardiyah100% (1)
- The Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialDocument8 pagesThe Effects of Premature Infant Oral Motor Intervention (PIOMI) On Oral Feeding of Preterm Infants - A Randomized Clinical TrialAndreas Arie WidiadiaksaNo ratings yet
- Doyle & Bradshaw - Sixty Golden MinutesDocument6 pagesDoyle & Bradshaw - Sixty Golden MinutesVillia DamayantieNo ratings yet
- Pain Relief During Labor and Delivery: A Brief 2013 UpdateDocument5 pagesPain Relief During Labor and Delivery: A Brief 2013 UpdateJheiczhietoot KibasNo ratings yet
- Going Home: Facilitating Discharge of The Preterm InfantDocument14 pagesGoing Home: Facilitating Discharge of The Preterm InfantYohanes DokaNo ratings yet
- Journal NicuDocument4 pagesJournal NicuMargaret LlavorNo ratings yet
- SA PerformanceDocument8 pagesSA Performancefernin96No ratings yet
- Problem StatementDocument15 pagesProblem StatementhuylimalaNo ratings yet
- Chapter 40 - Abril - CJDocument16 pagesChapter 40 - Abril - CJcarms abrilNo ratings yet
- Lung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFDocument8 pagesLung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFcesar juarezNo ratings yet
- 2017-Journal of Paediatrics and Child HealthDocument1 page2017-Journal of Paediatrics and Child HealthAna SopaNo ratings yet
- Delivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadDocument10 pagesDelivery Room Handling of The Newborn: Stephanie Marshall, Asta Maria Lang, Marta Perez and Ola D. SaugstadRaja SekarNo ratings yet
- MODEL OF PRACTICE TsaarDocument6 pagesMODEL OF PRACTICE TsaarCrystal Ann TadiamonNo ratings yet
- Basic EcgDocument19 pagesBasic EcgIrma SihotangNo ratings yet
- High-Flow Nasal Cannulae in Very Preterm Infants After ExtubationDocument9 pagesHigh-Flow Nasal Cannulae in Very Preterm Infants After ExtubationRiska Diene PratiwiNo ratings yet
- The Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesDocument5 pagesThe Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesJehangir AllamNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- Brief Resume of The Intended Work: "The Nation Walks On The Feet of Little Children."Document11 pagesBrief Resume of The Intended Work: "The Nation Walks On The Feet of Little Children."sr.kumariNo ratings yet
- Circulation 2015 Wyckoff S543 60Document18 pagesCirculation 2015 Wyckoff S543 60Kahfi Rakhmadian KiraNo ratings yet
- Neonatal Research PaperDocument5 pagesNeonatal Research Paperkrqovxbnd100% (1)
- Study of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreDocument11 pagesStudy of Clinical Profile of Late Preterms at Tertiary Care Hospital, BangaloreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Nursing Crib ThesisDocument8 pagesNursing Crib ThesisProfessionalCollegePaperWritersMcAllen100% (1)
- 2015 Neonatal Resuscitation AHADocument19 pages2015 Neonatal Resuscitation AHAJoyceAltamiranoEncisoNo ratings yet
- ResuscitationDocument18 pagesResuscitationIva NurilNo ratings yet
- Assessment of Initial Morbidity Patterns in Late Preterm Infants Relative To Those at TermDocument6 pagesAssessment of Initial Morbidity Patterns in Late Preterm Infants Relative To Those at TermInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 3 Killers Complications During Childbirth BriefDocument2 pages3 Killers Complications During Childbirth BriefAraz MuhammadaminNo ratings yet
- Effectiveness of Nesting On Posture and Movements Among Preterm BabiesDocument7 pagesEffectiveness of Nesting On Posture and Movements Among Preterm BabiesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Study of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Document6 pagesStudy of Respiratory Distress in Newborn: International Journal of Contemporary Pediatrics March 2017Elison J PanggaloNo ratings yet
- 26 Device Improves Swallowing in Newborns: CommentDocument33 pages26 Device Improves Swallowing in Newborns: CommentWahyuni M. Ali MreNo ratings yet
- ObjectivesDocument73 pagesObjectivesJoanna Bee Rose MagyawiNo ratings yet
- Differences in The Swallowing Process of Newborns and HealthyDocument12 pagesDifferences in The Swallowing Process of Newborns and Healthysiramliw3No ratings yet
- Research Proposal - SammyDocument24 pagesResearch Proposal - SammyOfosu AugustineNo ratings yet
- Initial Resuscitation and Stabilization of The Periviable Neonate: The Golden-Hour ApproachDocument5 pagesInitial Resuscitation and Stabilization of The Periviable Neonate: The Golden-Hour ApproachwilmaNo ratings yet
- ProneDocument8 pagesPronesophiaNo ratings yet
- PAPER (ENG) - (Kelly B., 2007 NEZ) The First Year of Human Life Coordinating Respiration and NutritiveDocument7 pagesPAPER (ENG) - (Kelly B., 2007 NEZ) The First Year of Human Life Coordinating Respiration and NutritiveAldo Hip NaranjoNo ratings yet
- Clinical Outcomes of Snuggle Up Position Using Positioning Aids For Preterm (27-32 Weeks) InfantsDocument6 pagesClinical Outcomes of Snuggle Up Position Using Positioning Aids For Preterm (27-32 Weeks) InfantsMastifa HanasitaNo ratings yet
- Weight Gain in Preterm Low Birth Weight Infants With Multisensory InterventionDocument5 pagesWeight Gain in Preterm Low Birth Weight Infants With Multisensory Interventionagung setiawanNo ratings yet
- Assess The Effectiveness of Sensory Nursing Interventions On Neonatal Reflex and Reactivity Among Preterm Infants in Selected Setting, Nagercoil, K.K. DistrictDocument12 pagesAssess The Effectiveness of Sensory Nursing Interventions On Neonatal Reflex and Reactivity Among Preterm Infants in Selected Setting, Nagercoil, K.K. DistrictImpact JournalsNo ratings yet
- The Importance of The Right Factory Fake Bundle Management On The Fetal Distress CaseDocument7 pagesThe Importance of The Right Factory Fake Bundle Management On The Fetal Distress CaseAnnis Laella MegassariNo ratings yet
- Effect of CupDocument9 pagesEffect of CupInés Valero ArredondoNo ratings yet
- Pioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Document13 pagesPioneer Nursing College Vadodara: Subject: Child Health Nursing Topic: Observation Report (Nicu)Kinjal Vasava100% (1)
- Skin To SkinDocument9 pagesSkin To SkinAsiatiNo ratings yet
- The Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUDocument11 pagesThe Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Surfactant For Respiratory Distress SyndromeDocument12 pagesSurfactant For Respiratory Distress Syndromesanjuy_garzaNo ratings yet
- The Effectiveness of Combination of Kangaroo Mother Care Method and Lullaby Music Therapy On Vital Sign Change in Infants With Low Birth WeightDocument8 pagesThe Effectiveness of Combination of Kangaroo Mother Care Method and Lullaby Music Therapy On Vital Sign Change in Infants With Low Birth Weightzaenab anissaNo ratings yet
- Baby Sleep Incidental Aspiration Case ReportDocument4 pagesBaby Sleep Incidental Aspiration Case ReportSebastian Jaén Vinueza SoteloNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- Nesting DN O2Document9 pagesNesting DN O2septiana dwi lestariNo ratings yet
- A Quasi Experimental Study To Evaluate The Effect of Prefeeding Oral Stimulation Program On Oral Feeding Skills Among Preterm Infants in Selected Hospitals, PunjabDocument29 pagesA Quasi Experimental Study To Evaluate The Effect of Prefeeding Oral Stimulation Program On Oral Feeding Skills Among Preterm Infants in Selected Hospitals, PunjabEditor IJTSRD100% (1)
- Intervencion Temprana SuccionDocument13 pagesIntervencion Temprana Succionjulianamd87No ratings yet
- BBLR 2Document6 pagesBBLR 2refiNo ratings yet
- Human Milk: Composition, Clinical Benefits and Future Opportunities: 90th Nestlé Nutrition Institute Workshop, Lausanne, October-November 2017From EverandHuman Milk: Composition, Clinical Benefits and Future Opportunities: 90th Nestlé Nutrition Institute Workshop, Lausanne, October-November 2017No ratings yet
- Menu and Product Knowledge Managemen TDocument55 pagesMenu and Product Knowledge Managemen TLaelannie Magpayo100% (1)
- Literature Review: Effect of Benson's Relaxation Therapy (BRT) On Post Caesarean Section Pain and StressDocument6 pagesLiterature Review: Effect of Benson's Relaxation Therapy (BRT) On Post Caesarean Section Pain and StressLaelannie MagpayoNo ratings yet
- Solution Brown Solution: Sample Used Time Oxidized Apple Banana Potato GuavaDocument7 pagesSolution Brown Solution: Sample Used Time Oxidized Apple Banana Potato GuavaLaelannie MagpayoNo ratings yet
- The Oath: Permissible Medical ExperimentsDocument3 pagesThe Oath: Permissible Medical ExperimentsLaelannie MagpayoNo ratings yet
- The Effect of Progressive Muscle Relaxation On PosDocument16 pagesThe Effect of Progressive Muscle Relaxation On PosLaelannie MagpayoNo ratings yet
- World Teachers' Day 2020: Teachers: Leading in Crisis, Reimagining The Future Concept NoteDocument5 pagesWorld Teachers' Day 2020: Teachers: Leading in Crisis, Reimagining The Future Concept NoteLaelannie MagpayoNo ratings yet
- Education in A BoxDocument3 pagesEducation in A BoxLaelannie MagpayoNo ratings yet
- Insights Into Digestion and Absorption of Major Nutrients in HumansDocument10 pagesInsights Into Digestion and Absorption of Major Nutrients in HumansLaelannie MagpayoNo ratings yet
- Nitrogenous Compounds in Blood and Urine-I: NPN and Urea: ArticleDocument3 pagesNitrogenous Compounds in Blood and Urine-I: NPN and Urea: ArticleLaelannie MagpayoNo ratings yet
- Questions For Discussion: (Financial Literacy) : Group TaskDocument3 pagesQuestions For Discussion: (Financial Literacy) : Group TaskLaelannie MagpayoNo ratings yet
- Media 49768e6 ccq6 4-0283Document12 pagesMedia 49768e6 ccq6 4-0283Laelannie MagpayoNo ratings yet
- Msds-Exp-09 CCLDocument2 pagesMsds-Exp-09 CCLLaelannie MagpayoNo ratings yet
- Experiment 3 LipidsDocument4 pagesExperiment 3 LipidsLaelannie MagpayoNo ratings yet
- Current Status, Research Trends, and ChallengesDocument23 pagesCurrent Status, Research Trends, and Challengesqgi-tanyaNo ratings yet
- Chapter 8 Supplemental Questions: E8-1 (Inventoriable Costs)Document7 pagesChapter 8 Supplemental Questions: E8-1 (Inventoriable Costs)Dyan NoviaNo ratings yet
- Decribing Connections Between Historical EventsDocument4 pagesDecribing Connections Between Historical Eventsapi-334916201No ratings yet
- KB Shape CodesDocument9 pagesKB Shape CodesPrashanth TNo ratings yet
- The 1 Catholic Mass in The PhilippinesDocument16 pagesThe 1 Catholic Mass in The PhilippinesRosalie AlitaoNo ratings yet
- Ics Lab Manual PDFDocument46 pagesIcs Lab Manual PDFEyes FlikerNo ratings yet
- Accounting Unit Additional Execerses AA025 Sem 2, 2019/2020Document5 pagesAccounting Unit Additional Execerses AA025 Sem 2, 2019/2020nur athirahNo ratings yet
- ARTI Refrigerant Database - Volume Two PDFDocument578 pagesARTI Refrigerant Database - Volume Two PDFAymanNo ratings yet
- Hopkins Verbal Learning Test Revised NorDocument13 pagesHopkins Verbal Learning Test Revised NorOscar Ariza CaroNo ratings yet
- English Chapter 5Document20 pagesEnglish Chapter 5Kumar sankar SNo ratings yet
- v2 SDO ISABELA LEARNING RECOVERY PLANDocument16 pagesv2 SDO ISABELA LEARNING RECOVERY PLANRoland Mark DumaliangNo ratings yet
- Windows Server ChecklistDocument116 pagesWindows Server Checklistravichandran_mcpNo ratings yet
- I04 U11 Conditionals & Reported SpeechDocument4 pagesI04 U11 Conditionals & Reported Speechmelgarejo1111No ratings yet
- 17 Reg-TocDocument1 page17 Reg-TocvanithaNo ratings yet
- Personal Nutrition 9th Edition Boyle Solutions ManualDocument32 pagesPersonal Nutrition 9th Edition Boyle Solutions Manualthoabangt69100% (29)
- CPAR LessonDocument2 pagesCPAR LessonAnabelle MoyamoyNo ratings yet
- Research and Innovation in Higher Education-EPP-1-2018-1-AT-EPPKA1-JMD-MOBDocument2 pagesResearch and Innovation in Higher Education-EPP-1-2018-1-AT-EPPKA1-JMD-MOBTabah Ghifary Diniya (Ghif)No ratings yet
- March 6 - Artificial Selection PresentationsDocument3 pagesMarch 6 - Artificial Selection Presentationsapi-503273730No ratings yet
- ShowPDF Paper - AspxDocument14 pagesShowPDF Paper - AspxShawkat AhmadNo ratings yet
- NIV Excerpt PDFDocument57 pagesNIV Excerpt PDFAnonymous tSYkkHToBPNo ratings yet
- Cetirizine Degradation ProductsDocument7 pagesCetirizine Degradation ProductsASHOK KUMAR LENKANo ratings yet
- P Block Elements Group 15Document79 pagesP Block Elements Group 1515 Kabir Sharma 10 HNo ratings yet
- Yak 52 Maitenance ManualDocument36 pagesYak 52 Maitenance ManualAvionicsfNo ratings yet
- Individual Assignment: Retail ManagementDocument11 pagesIndividual Assignment: Retail ManagementTijo ThomasNo ratings yet
- +english Test Prac Poison Tree-AnswersDocument5 pages+english Test Prac Poison Tree-AnswersLouise Francis100% (1)