Professional Documents
Culture Documents
Empiric Antibiotic List
Empiric Antibiotic List
Uploaded by
password0 ratings0% found this document useful (0 votes)
37 views2 pagesThis document provides guidelines for diagnosing and treating various infections including:
1) Neutropenic fever - obtain blood cultures before antibiotics and treat with ceftazidime or cefepime for suspected gram-negative infections or add vancomycin for suspected MRSA.
2) C. difficile diarrhea - test stool with PCR and treat mild cases with metronidazole or severe cases with vancomycin.
3) Suspected fungemia - empirically treat with micafungin and de-escalate to fluconazole if C. albicans is identified, consulting infectious diseases.
Original Description:
Original Title
Empiric-antibiotic-list
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidelines for diagnosing and treating various infections including:
1) Neutropenic fever - obtain blood cultures before antibiotics and treat with ceftazidime or cefepime for suspected gram-negative infections or add vancomycin for suspected MRSA.
2) C. difficile diarrhea - test stool with PCR and treat mild cases with metronidazole or severe cases with vancomycin.
3) Suspected fungemia - empirically treat with micafungin and de-escalate to fluconazole if C. albicans is identified, consulting infectious diseases.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
37 views2 pagesEmpiric Antibiotic List
Empiric Antibiotic List
Uploaded by
passwordThis document provides guidelines for diagnosing and treating various infections including:
1) Neutropenic fever - obtain blood cultures before antibiotics and treat with ceftazidime or cefepime for suspected gram-negative infections or add vancomycin for suspected MRSA.
2) C. difficile diarrhea - test stool with PCR and treat mild cases with metronidazole or severe cases with vancomycin.
3) Suspected fungemia - empirically treat with micafungin and de-escalate to fluconazole if C. albicans is identified, consulting infectious diseases.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
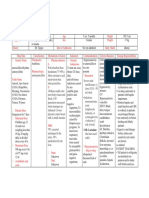
NEUTROPENIC FEVER C.
DIFFICILE DIARRHEA SUSPECTED FUNGEMIA
Diagnosis: Only loose stools will be accepted by
Diagnosis: If possible, obtain blood culture x 2 (1 the lab for C.diff testing. Order C.diff testing Risk factors: Septic pts on TPN, prolonged abx
peripheral and 1 central) before antibiotics are
infused. Do NOT delay antibiotics while waiting for cultures
(Toxigenic by PCR, not toxin assay) in CPOE. therapy, malignancy, femoral catheterization
or Candida colonization at multiple sites.
Empiric Antimicrobial
Mild to Moderate disease: Metronidazole 500mg PO TID
to be drawn. Review past microbiology for known
colonization or infections with resistant organisms.
Typical duration: 10-14 days, do not send stool for test of
cure
Micafungin 100 mg IV q24 hours Therapy
De-Escalate to Fluconazole 400 mg-800mg IV Daily if
Severe disease (WBC > 15K, SCr 1.5 X baseline or ICU C.albicans or if susceptible by MIC testing.
Typical Duration: until pt is afebrile and has ANC > 500 status): Vancomycin Solution 125mg PO q 6 hours Consult Infectious Diseases for line management.
A. Stable with NO sepsis, NO history of resistant (Preferred agent for ICU) Typical Duration: 14 days;
organisms, NO specific abdominal findings: (susceptible
Typical Duration: 14 days after blood culture clearance UW Medicine Sepsis Guidelines
DO NOT send stool for test of cure
gram-negative rods including Pseudomonas, Acinetobacter, Severe Complicated (hypotension or shock, ileus, mega SEPSIS: SITE UNKNOWN
E.coli, Klebsiella, etc) colon): Vancomycin 500mg PO/NG q 6 hours PLUS Met-
(MRSA, resistant Gram-negative bacilli)
Ceftazidime or Cefepime 2gm IV q8 hours ronidazole 500mg IV q8 hours. Consider adding rectal
instillation of vancomycin (500mg PR q6h) if complete Diagnosis: Culture blood (all lumens), urine & Antimicrobial Stewardship Teams
Consider Vancomycin IF suspected line infection, ileus.
sputum. Tailor antimicrobial within 48 hours
mucositis, sepsis, h/o colonization or infection with Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm These recommendations are based on local microbiology,
Also consider consulting GI, ID, and Surgery. if <70kg), then 15 mg/kg IV q12 hours PLUS
MRSA antimicrobial resistance patterns, and national guidelines.
Duration variable Meropenem 1gm IV q8 hours (requires ID consult > They should not replace clinical judgment, and may be mod-
72hrs)
ified depending on individual patient. Consult pharmacy for
B. Stable with h/o MDR infection or colonization, or MENINGITIS If previous colonization or concerns for highly re-
abdominal findings: (susceptible gram-negative rods sistant Gram-negative pathogen such as Acinetobac- renal dosing.
(S.pneumoniae, N.meningitidis and H.influenzae ter, Pseudomonas, or ESBL, consider adding:
including Pseudomonas, Acinetobacter, E.coli, Klebsiella, Conversion from IV to PO may be appropriate once patient
Consider Listeria and HSV in patients age > 50, immuno- Ciprofloxacin 400 mg IV q8 hours OR
and anaerobes) hemodynamically stable and/or tolerating medications by
compromised or alcoholic.) Tobramycin 7mg/kg IV x1
Meropenem 1g IV q8 hours (requires ID consult > 72hrs) Diagnosis: Order antibiotics immediately; Do not wait for Typical Duration: 14 days mouth.
ADD Vancomycin IF suspected line infection, mucositis, results of LP to initiate antimicrobials. LP for opening
Order the first dose of antibiotics as STAT.
pressure, gram stain, culture, HSV PCR, cell count, glu-
sepsis, h/o colonization or infection with MRSA cose, and protein. Add cryptococcal antigen for HIV pa- SIGNIFICANT PENICILLIN ALLERGY
Consider Daptomycin 8mg/kg q24h instead of tients. Example - anaphylaxis, airway compromise,
Vancomycin IF history of VRE colonization or infection Non-surgical, community-acquired: etc Version 8: September 2016
but discontinue when culture negative for VRE. Consider Dexamethasone 0.15mg/kg IV q6 hours for 2 CONSULT ALLERGY for evaluation and possi-
-4 days, give 15 minutes prior to abx if possible ble skin testing HMC: Jeannie Chan & John Lynch (Pager: 206-744-3000)
Ceftriaxone 2g IV q 12 hours PLUS For all infections except hospital-acquired intra-
C. Sepsis without focal findings: (susceptible gram-negative Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm abdominal infection: UWMC: Rupali Jain & Paul Pottinger (Pager: 206-598-6190)
rods including Pseudomonas, Acinetobacter, E.coli, if <70kg) STAT, then 15 mg/kg IV q8 hours Replace Meropenem, Ceftazidime, Cefepime, or Pipe-
Klebsiella, and anaerobes) ADD Ampicillin 2g IV q4 hours for Listeria coverage racillin-Tazobactam with Ciprofloxacin 400mg IV q8h
Meropenem 1gm IV q8 hours STAT PLUS ADD Acyclovir 10mg/kg IV q8h for HSV coverage +/- Aztreonam 2gm IV q 8 hours
Online: https://occam.uwmedicine.org
when appropriate For intra-abdominal infections:
Tobramycin 5 mg/kg IV x1 STAT, based on ideal body Replace Ceftriaxone or Piperacillin-Tazobactam or
Typical duration: 14 days
weight, unless underweight or obese or renal dysfunction Ertapenem with Levofloxacin 750mg PO/IV q24h +
(call pharmacy) PLUS Post-surgical meningitis: (S.epidermidis, S.aureus, Metronidazole 500mg PO/IV q8h.
P.acnes, gram-negative rods (including P.aeruginosa) For CAP: Replace Ceftriaxone or Ampicillin-Sulbactam
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm if Cefepime 2g IV q8 hours PLUS with Moxifloxacin 400mg PO/IV q24h
<70kg) STAT, then 15 mg/kg IV q12 hours
Metronidazole 500mg IV q8 hours PLUS For NSTI: Omit Penicillin.
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm For meningitis: Replace Ceftriaxone or Ampicillin with
D. For all pts: During flu seasons, send Flu testing and Trimethoprim-Sulfamethoxazole 5mg/kg IV q8h PLUS
then give oseltamivir 75mg - 150mg PO/NGT q12. if <70kg) STAT, then 15 mg/kg IV q8 hours Aztreonam 2g IV q8h PLUS Vancomycin
PNEUMONIA BLOODSTREAM NECROTIZING SOFT TISSUE URINARY
A. Community-acquired pneumonia [non- A. Suspected Line infection (MRSA, Gram- INFECTION A. Community Acquired Pyelonephritis
aspiration risk] (S. pneumoniae, atypicals) negative rods) (Enteric Gram-negative rods)
(MRSA, Group A strep, Clostridium sp and
Diagnosis: Send sputum gram stain & culture, Diagnosis: Order antibiotics immediately and
CXR, and blood cultures. mixed anaerobes, Gram-negative rods) Diagnosis: Clean catch midstream U/A with reflexive
draw paired, simultaneous, quantitative blood cultures Typical Duration: 14 days after debridement gram stain and culture (UACRC). Neutropenic and
Ceftriaxone 1 gm IV q24 hours PLUS from all central line lumens AND one peripheral site. Diagnosis: Suspect NSTI in septic patients, rapid skin transplant patients may not mount WBC response;
Azithromycin 500 mg PO/IV q24 hours Central line CFU x2 more than peripheral site CFU lesion progression, pain out of proportion to physical appropriate to cover these patients empirically even
If previous MRSA colonization or infection, consider strongly suggests line infection. findings & hyponatremia. STAT surgery and Infectious without positive U/A if presentation suggests pyelo-
adding: Vancomycin loading dose IV x1 (2 gm if >70 kg, Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm Diseases consult. Focus therapy based on culture results nephritis.
1.5 gm if <70kg), then 15 mg/kg IV q12 hours and patient response.
if <70kg), then 15 mg/kg IV q12 hours PLUS
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm if Ceftriaxone 1 gm IV q 24 hours
Typical Duration: 7 days Cefepime 2gm IV q8 hours <70kg), then 15 mg/kg IV q12 hours PLUS If patient hemodynamically unstable or history
Please consult Infectious Diseases if considering line Penicillin 4 million units IV q4 hours PLUS MDRO, change to: Ertapenem 1g q 24 hours
B. CAP with cavitary lesion(s) (Oral anaerobes and MRSA)
Ampicillin/Sulbactam 3 gm IV q6 hours PLUS
salvage Clindamycin 1200 mg IV q6 hours PLUS EITHER
Typical Duration: 14 days
Azithromycin 500 mg PO/IV q24 hours PLUS
B. Suspected endocarditis, hemodynamically stable, no Levofloxacin 750mg IV daily OR
valve insufficiency: For Neutropenic pts: Gentamicin 7 mg /kg IV q24 hours B. Catheter-associated UTI or Hospital- acquired:
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm if Diagnosis: Draw 3 sets of blood cultures prior to antibi- (replace Levofloxacin)
<70kg), then 15 mg/kg IV q12 hours (Resistant Gram-negative rods)
otics and consult Infectious Diseases. For Fournier’s: replace Penicillin with Piperacillin-
Diagnosis: Obtain specimen from new foley, or from
Typical Duration: 10-21 days
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 gm tazobactam: 4.5g x1, then 3.375g IV q8h infused over 4 hrs
sterilized port on existing foley, not from collection
if <70kg), then 15 mg/kg IV q12 hours PLUS bag or urimeter. Send U/A with reflexive gram stain
CF or Lung transplant patients: Call Pulmonary Transplant INTRA-ABDOMINAL
and Transplant Infectious Diseases Consult. Ceftriaxone 2gm IV q24 hours and culture (UACRC). WBCs and Bacteria on direct
Consult Infectious Diseases A. Community-acquired, mild-moderate stain suggests infection, but colonization also very
C. High-risk for MDRO pneumonia [i.e.from skilled nursing (Enteric Gram-negative rods, anaerobes) common.
CELLULITIS HMC: Ertapenem 1g IV q24h Ceftazidime 2g IV q8 hours
facility, etc](MRSA, resistant Gram-negative rods including
Acinetobacter, Pseudomonas, ESBL) Not-applicable to device-related infections UWMC: Ceftriaxone 2g IV q24 hours PLUS Metroni- If previous colonization with highly resistant Gram-
Cefepime 2g IV q8 hours +/- Vancomycin loading dose IV (eg ICD, pacemakers,VADs, etc): Consult dazole 500mg PO/IV q 8 hours
negative pathogen such as Acinetobacter, Pseudo-
x1 (2 gm if >70 kg, 1.5 gm if <70kg), then 15 mg/kg IV q12 Infectious Diseases For uncomplicated biliary infections, anaerobic cover-
hours if h/o MRSA infection/colonization A. Non-purulent skin/soft tissue infection: age usually not necessary, use Ceftriaxone alone. monas, or ESBL, consider: Meropenem 1 gm IV q8
Typical Duration: 7 days (Streptococcus species) Typical Duration: 4 days following source control hours (requires ID consult > 72hrs) instead of
D. UWMC only: Ventilator-associated Pneumonia (VAP) Cefazolin 2g IV q8h B. Hospital-acquired, severe physiological disturbance, ceftazidime
regardless of hospitalization day PO option for Strep/MSSA: Cephalexin 500mg QID advanced age, immunocompromised (Resistant Gram- If GPC seen on gram stain, add: Vancomycin load-
Treat as High-risk for MDROs (see section C) negative rods, anaerobes)
ing dose IV x1 (2 gm if >70 kg, 1.5 gm if <70kg),
E. HMC only: B. Purulent/abscess forming skin/soft tissue infection: Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5
Early onset VAP (i.e. < 4 days of hospitalization or venti- (S.aureus: MSSA or MRSA) gm if <70kg), then 15 mg/kg IV q12 hrs PLUS EITHER then 15 mg/kg IV q12 hrs
lation) or aspiration: Ceftriaxone 1g IV daily OR Diagnosis: I&D abscess; send pus (not wound swab) for Piperacillin-tazobactam 4.5gm X 1, then 4 hours De-escalate or discontinue coverage if alternate
Ampicillin-sulbactam 3g IV q6h gram stain and culture. later start 3.375g IV q8h infused over 4 hours OR
Vancomycin loading dose IV x1 (2 gm if >70 kg, 1.5 source found for patient symptoms.
Late-onset [> 4 days inpatient], Treat as High-risk for If previous colonization or concerns for highly re-
MDROs (see section C) gm if <70kg), then 15 mg/kg IV q12 hrs Typical Duration: 7-14 days
sistant Gram-negative pathogen such as Acinetobac-
De-escalate when culture data available ter, Pseudomonas, or ESBL, consider: Meropenem 1 C. UTIs in abdominal Transplant patients: Same as
F. For all Pneumonia pts: PO options for MRSA: Bactrim or Doxycycline gm IV q8 hours (requires ID consult > 72hrs) instead
Typical Duration: 5-7 days; Consult Infectious Diseases above and consult Transplant Infectious Diseases
During flu seasons, send Flu testing and then give for PO step-down options
of Piperacillin-tazobactam
Typical Duration: 4-7 days from source control; if source
oseltamivir 75mg - 150mg PO/NGT q12. control is not attained, then duration is variable.
Yeast in the sputum rarely represents true infection. C. Abdominal Transplant patients: Same as above and consult
Transplant Infectious Diseases
You might also like
- PSYCH 505 Case Study Core FunctionsDocument8 pagesPSYCH 505 Case Study Core FunctionsHugsNo ratings yet
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- VancomycinDocument3 pagesVancomycinGwyn Rosales100% (3)
- Genentech - Capacity PlanningDocument7 pagesGenentech - Capacity PlanningTejas MahajanNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- 04.the Cleveland Clinic Intensive Review of Pediatrics 2nd EdDocument513 pages04.the Cleveland Clinic Intensive Review of Pediatrics 2nd EdSav GaNo ratings yet
- Introduction To PeriodontologyDocument33 pagesIntroduction To PeriodontologyEmine Alaaddinoglu100% (1)
- Ob Gyn AdultDocument3 pagesOb Gyn AdultHarshit RastogiNo ratings yet
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- Empiric Treatment Guidelines Common InfectionsDocument9 pagesEmpiric Treatment Guidelines Common InfectionsShiza Batool100% (1)
- NICU ABX ChartDocument11 pagesNICU ABX ChartdrchiNo ratings yet
- Antibiotic Guidelines For BONE AND JOINT INFECTIONSDocument3 pagesAntibiotic Guidelines For BONE AND JOINT INFECTIONSKhurram NadeemNo ratings yet
- Pocket Guide June2013 PDFDocument2 pagesPocket Guide June2013 PDFSergeyGruntov100% (1)
- Management of CAP in Adults - Ontario GovernmentDocument2 pagesManagement of CAP in Adults - Ontario GovernmentSukhvir AujlaNo ratings yet
- Antibiotic Guidelines For SKIN AND SOFT TISSUE INFECTIONSDocument11 pagesAntibiotic Guidelines For SKIN AND SOFT TISSUE INFECTIONSlaptopgreyNo ratings yet
- Vancomycin DRUGSTUDYDocument3 pagesVancomycin DRUGSTUDYEmagra AzilNo ratings yet
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- SHC Intra Abdominal GuidelinesDocument13 pagesSHC Intra Abdominal GuidelinesNguyễn Mạnh CườngNo ratings yet
- Solid Tumor Febrile NeutropeniaDocument12 pagesSolid Tumor Febrile NeutropeniaSimonNo ratings yet
- Escalation Guide For Gram-Negative Bacteremia StanfordDocument3 pagesEscalation Guide For Gram-Negative Bacteremia StanfordLuis MedinaNo ratings yet
- Antibiotic ProtocolDocument37 pagesAntibiotic ProtocolSrinivas VadtheNo ratings yet
- Antibiotic Protocol 2018Document10 pagesAntibiotic Protocol 2018sumayyah995No ratings yet
- CNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Document1 pageCNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Fitri RachmadaniNo ratings yet
- Drug Name Mechanism of Action Indication / Contraindication Adverse Effect Nursing Responsibilities Telavancin Indications: DXDocument2 pagesDrug Name Mechanism of Action Indication / Contraindication Adverse Effect Nursing Responsibilities Telavancin Indications: DXEmilie CajaNo ratings yet
- Valgancyclovir MOA: Uses Pharmacokinetics Dosage Side Effects ContraindicationsDocument2 pagesValgancyclovir MOA: Uses Pharmacokinetics Dosage Side Effects ContraindicationsiSmayli (smyle-smayl)No ratings yet
- Bone and Joint Infections BNHFT 2010 PDFDocument3 pagesBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNo ratings yet
- Classification: Cefditoren, As This Agent May CauseDocument3 pagesClassification: Cefditoren, As This Agent May CauseHavier EsparagueraNo ratings yet
- Vancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., PharmDocument78 pagesVancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., Pharmkharbosham100% (1)
- Antibiotic Hospital ManDocument1 pageAntibiotic Hospital Manarshiya.manasekiNo ratings yet
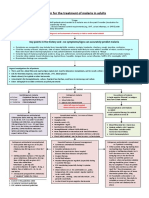
- Algorithm For The Treatment of Malaria in AdultsDocument1 pageAlgorithm For The Treatment of Malaria in AdultsRihab IsmaeelNo ratings yet
- Medicine RotatationbookletDocument20 pagesMedicine RotatationbookletJanelle JosephsNo ratings yet
- Candidiasis IDSA 2016Document23 pagesCandidiasis IDSA 2016Shihan HuqNo ratings yet
- DRUGSTUDYDocument8 pagesDRUGSTUDYWinnie Salazar AriolaNo ratings yet
- LevofloxacinDocument3 pagesLevofloxacinLIEZEL GRACE VELAYO100% (1)
- GNR Bacteremia De-Escalation Guide Final PDFDocument2 pagesGNR Bacteremia De-Escalation Guide Final PDFAbu Hammoud AlyazeediNo ratings yet
- 30 Glycopeptides Vancomycin and Teicoplanin 2015 Mandell Douglas and BDocument29 pages30 Glycopeptides Vancomycin and Teicoplanin 2015 Mandell Douglas and BHelen DyNo ratings yet
- NAG Sexually Transmitted InfectionsDocument24 pagesNAG Sexually Transmitted InfectionsJun JimenezNo ratings yet
- Drug Study: Adult: ChildDocument4 pagesDrug Study: Adult: ChildKristian Karl Bautista Kiw-isNo ratings yet
- Drug Study SPRDocument9 pagesDrug Study SPRKate WeyganNo ratings yet
- AmikinDocument2 pagesAmikinLIEZEL GRACE VELAYONo ratings yet
- Ampicillin DRUG STUDYDocument2 pagesAmpicillin DRUG STUDYJuliana CarpinteroNo ratings yet
- NAG Central Nervous System Infections As of Nov 2017Document9 pagesNAG Central Nervous System Infections As of Nov 2017Rhod Bernaldez EstaNo ratings yet
- Drug Study Amoxicillin PDFDocument4 pagesDrug Study Amoxicillin PDFMc SantosNo ratings yet
- 2012 Aug IMG Poster 165760a SepsisDocument1 page2012 Aug IMG Poster 165760a SepsisTeng Huei LeeNo ratings yet
- Antibiotic Pocket GuideDocument19 pagesAntibiotic Pocket GuideNaomi Liang100% (1)
- Antibiotka PicuDocument4 pagesAntibiotka Picusunu rachmat100% (1)
- AminoglycosideDocument16 pagesAminoglycosideDr. ChihiroNo ratings yet
- Gentamicin Sulfate-Drug StudyDocument3 pagesGentamicin Sulfate-Drug StudyDaisy Palisoc82% (11)
- CNS Infection GuidanceDocument2 pagesCNS Infection GuidanceGus LionsNo ratings yet
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocument1 pageGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxNo ratings yet
- Any Up-Dates Are To Be Completed in Different Color Ink. The Student Is Expected To Document All Meds The Client Is Currently ReceivingDocument1 pageAny Up-Dates Are To Be Completed in Different Color Ink. The Student Is Expected To Document All Meds The Client Is Currently Receivinggeorgeloto12No ratings yet
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Severe Sepsis and Septic Shock Antibiotic Guide: Community AcquiredDocument6 pagesSevere Sepsis and Septic Shock Antibiotic Guide: Community AcquiredAnonymous G6zDTD2yNo ratings yet
- TASH Empirical Antibiotic Treatment Guidelines - 2018 Hospital and Ventilator Associated Pneumonia (HAP and VAP)Document2 pagesTASH Empirical Antibiotic Treatment Guidelines - 2018 Hospital and Ventilator Associated Pneumonia (HAP and VAP)ጉራማይሌ TubeNo ratings yet
- Pediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic DiscussionDocument5 pagesPediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic Discussionapi-602288180No ratings yet
- Acyclovir (Acycloguanosi Ne) : Systemic Administration History: AllergyDocument3 pagesAcyclovir (Acycloguanosi Ne) : Systemic Administration History: AllergyAnnahNo ratings yet
- Drug StudyDocument1 pageDrug StudyBtob meloNo ratings yet
- Febrile Neutropenia Care GuidelineDocument2 pagesFebrile Neutropenia Care GuidelinedenokayuMRNo ratings yet
- Shivani PDFDocument3 pagesShivani PDFdeepukumarNo ratings yet
- VancomycinDocument1 pageVancomycinJUSTINE ALLYSA MAY CASTILLONo ratings yet
- Monkeypox, Diagnosis and TreatmentDocument55 pagesMonkeypox, Diagnosis and TreatmentsamiNo ratings yet
- Pneumonia ADULTDocument6 pagesPneumonia ADULTSebastian TjuwatjaNo ratings yet
- Concise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryFrom EverandConcise Guide to Clinical Dentistry: Common Prescriptions In Clinical DentistryNo ratings yet
- Opioid Equianalgesic ChartDocument1 pageOpioid Equianalgesic Chartdamondouglas100% (7)
- Why Black Women With Ovarian Cancer Require Greater FocusDocument1 pageWhy Black Women With Ovarian Cancer Require Greater FocusMicheleFontanaNo ratings yet
- Perry Chapter 7,8,9,10,11,12,14 Case Study & DefinitionsDocument15 pagesPerry Chapter 7,8,9,10,11,12,14 Case Study & Definitionstriddle1969100% (1)
- A Lens To Understand Sanitation Workers and Their Health Status in IndiaDocument3 pagesA Lens To Understand Sanitation Workers and Their Health Status in IndiaRejesh BoseNo ratings yet
- Abnormal Eye PositionDocument30 pagesAbnormal Eye PositionNimas Prita100% (1)
- Example of Health Technology Assessment (HTA) of A Therapy For The Reduction of Alcohol ConsumptionDocument18 pagesExample of Health Technology Assessment (HTA) of A Therapy For The Reduction of Alcohol ConsumptiontantanwyNo ratings yet
- FITE Primer 2021Document3 pagesFITE Primer 2021iya gerzonNo ratings yet
- Asphyxia in Forensic AspectDocument31 pagesAsphyxia in Forensic AspectSita SilastutiNo ratings yet
- Gestational Weight GainDocument3 pagesGestational Weight GainainindyaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument2 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Chorea Approach PDFDocument1 pageChorea Approach PDFdrsushmakNo ratings yet
- Tuffey ResumeDocument3 pagesTuffey Resumeapi-317208513No ratings yet
- Acute EkaDocument25 pagesAcute EkaranggaNo ratings yet
- Placenta Previa: View Media GalleryDocument7 pagesPlacenta Previa: View Media GalleryMargaret AssilasNo ratings yet
- Mock Exam 1 - 50Document9 pagesMock Exam 1 - 50charlotte macairan67% (3)
- Allergic Rhinitis: Dr. Fauziah Henny, SP - THT-KLDocument14 pagesAllergic Rhinitis: Dr. Fauziah Henny, SP - THT-KLIsra AbdiNo ratings yet
- Liver Abscess of Patient: Case Report and Review of The LiteratureDocument4 pagesLiver Abscess of Patient: Case Report and Review of The LiteratureReinhar RusliNo ratings yet
- Su Jok, Twist Therapy AND Smile MeditationDocument7 pagesSu Jok, Twist Therapy AND Smile MeditationprateekNo ratings yet
- Bài tập tiếng anh unit 2Document31 pagesBài tập tiếng anh unit 2Nok NokNo ratings yet
- Personal Injury Ire FormDocument2 pagesPersonal Injury Ire FormBioVeda Health and Wellness CentersNo ratings yet
- Zephrex-D National Launch News ReleaseDocument3 pagesZephrex-D National Launch News ReleaseSam LevinNo ratings yet
- Supersizeme WorksheetDocument5 pagesSupersizeme WorksheetPaola SoledadNo ratings yet
- Q-NCOV-01D STANDARD Q COVID-19 IgM-IgG Duo Test INSERTODocument2 pagesQ-NCOV-01D STANDARD Q COVID-19 IgM-IgG Duo Test INSERTOechegarayNo ratings yet
- Asia-Pacific Glaucoma Guidelines PDFDocument118 pagesAsia-Pacific Glaucoma Guidelines PDFAvilla Ane LukitoNo ratings yet
- What Is AphasiaDocument4 pagesWhat Is AphasiaValentina DubNo ratings yet
- Germany Health Benefits SummaryDocument6 pagesGermany Health Benefits Summarytracy leeNo ratings yet