Professional Documents
Culture Documents
Metachromatic Leukodystrophy Pediatric Presentatio
Metachromatic Leukodystrophy Pediatric Presentatio
Uploaded by
Mike SihombingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metachromatic Leukodystrophy Pediatric Presentatio
Metachromatic Leukodystrophy Pediatric Presentatio
Uploaded by
Mike SihombingCopyright:
Available Formats
RAPID COMMUNICATIONS
Metachromatic leukodystrophy: pediatric
presentation and the challenges of early diagnosis
Frederico Mendes Borges1
Maria Júlia Gonzalez da Costa1
Zumira Aparecida Carneiro1
Charles Marques Lourenço1,2
1. Faculdade de Medicina - Centro Universitário Estácio de Ribeirão Preto, Ribeirão Preto, SP, Brasil.
2. CPDP - Centro Paulista de Diagnóstico, Pesquisa e Treinamento, Ribeirão Preto, SP, Brasil.
http://dx.doi.org/10.1590/1806-9282.66.10.1344
KEYWORDS: Leukodystrophy, Metachromatic/diagnosis. Child. Hereditary Central Nervous System Demyelinating Diseases.
PALAVRAS-CHAVE: Leucodistrofia Metacromática/diagnóstico. Criança. Doenças Desmielinizantes Hereditárias do Sistema Nervoso Central.
INTRODUCTION
Metachromatic leukodystrophy (MLD; OMIM FIGURE 1. CHEMICAL STRUCTURE OF THE SULFATIDE
250100) is an autosomal recessive hereditary dis- (3-O-SULFOGALACTOSYLCERAMIDE).
ease caused by a deficiency of the Arylsulfatase A
(ARSA) enzyme and, more rarely, of Saposin B, which
is responsible for the interaction with the sulfatide,
allowing the ARSA to degrade it. Therefore, it is clas-
sified as a hereditary metabolic disorder that evolves
with a reduction of sulfatide degradation. Initially, SOURCE: The authors, 2019.
the disease was known as “diffuse cerebral sclero-
sis” and, in 1938, it was named “metachromatic leu- such as the kidneys, gall bladder, spleen, and other
kodystrophy” and classified as a lipidosis in 1958 and visceral ones1-3. There are different variants (leading to
1959, based on the discovery of a high concentration different levels of residual enzymatic activity) and vari-
of sulfatídes (3-O-Sulfogalactosylceramide) (Figure 1) ations regarding the age of onset of the first symptoms
demonstrated by Jatzkewitz and Austin1.2. and speed of disease progression, thus, it has been
ARSA deficiency causes metachromatic lipids to classified as: infantile (late infantile, 0 to 4 years), juve-
accumulate on the white matter of the central and nile (4 to 15 years), and adult (over 15 years) (Annex
peripheral nervous system, which is responsible for 1)3.4. In addition, the diagnosis can be suspected when
causing demyelination and may also affect organs the patient begins to show signs of loss of intellectual,
DATE OF SUBMISSION: 23-Apr-2020
DATE OF ACCEPTANCE: 01-Jun-2020
CORRESPONDING AUTHOR: Charles Marques Lourenço
Faculdade de Medicina, Centro Universitário Estácio de Ribeirão Preto, Rua Abrahão Issa Halach, 980, Ribeirânia, SP, Brasil – 14096-160
Tel/Fax: +55 16 3603-9942
E-mail: charlesgenetica@gmail.com, charles.lourenco@estacio.br
REV ASSOC MED BRAS 2020; 66(10):1344-1350 1344
BORGES, F. M. ET AL
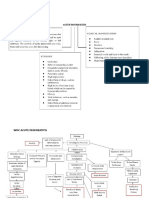
cognitive, and/or motor abilities, and it is possible to The juvenile form, sometimes, can be divided into
confirm it based on the dosage of the ARSA enzyme early and late10. The first is manifested between 4 to
and sulfatídes (Diagram 1)3.5. 6 years with abnormal gait and posture, emotional
The infantile type (late infantile) usually manifests and behavioral disorders, ocular atrophy, and pro-
during the second year of life, with a gait disorder of gressive spastic tetraparesis. The late juvenile type
sudden onset as well when the child begins to learn to appears between the ages of 4 and 15 years, starting
walk6. Often, an orthopaedist is sought before the neu- with more prominent behavioral abnormalities, poor
rological manifestations appear. Strabismus, dysar- school performance, and regression of language, fol-
thria, spasticity, and intellectual deterioration appear lowed by motor disorders and spastic tetraparesis that
gradually. Coarse tremors or coarse abnormal move- progresses more slowly3.10. Whereas in the adult type,
ments (athetosis) of the extremities may appear. The two clinical presentations have been described: one
deep tendon reflexes of the lower limbs are reduced was characterized mainly by signals from the central
or absent7. In addition, spasticity episodes may be nervous system (pyramidal and cerebellar dystonia)
triggered by any feeling of discomfort (including con- and peripheral neuropathy, whereas the other clin-
stipation or cholecystopathy) and may result in severe ical presentation begins with behavioral abnormali-
episodes of stiffness and shaking, crying, sweating, ties, i.e., mood disorders, peculiar reactions in social
and fever of unknown origin. During the third and interactions, progressive mental deterioration, and
fourth years of life, there is a rapid progression of the the presence of peripheral neuropathy may or may
disease with the onset of visual abnormalities, such not be identified11. In these cases, an initial diagnosis
as optic atrophy and progressive amblyopia8.9. of schizophrenia is established. Most of these patients
DIAGRAM 1. FLOWCHART FOR THE DIAGNOSIS OF METACHROMATIC LEUKODYSTROPHY.
SOURCE: Adapted from Artigalas3.
1345 REV ASSOC MED BRAS 2020; 66(10):1344-1350
Metachromatic leukodystrophy: pediatric presentation and the challenges of early diagnosis
remain for several years without any other neurolog- intercurrences. G1P1A0C1. Born by cesarean delivery
ical symptom11.12. due to pelvic fetal presentation. Presented, at birth,
We report a case series of patients with infantile APGAR 9 in the 1st minute and 10 in the 5th minute,
MLD whose diagnosis was late due to little knowl- weighed 3210g (P50), measured 47 cm, and 35 cm
edge about the signs and symptoms of this group of (P15) of head circumference. According to the curve
diseases by the medical community. of head circumference for the first 2 years of age, all
markings were close to the P50 line. At 1 year and
9 months, upon presenting progressive difficulty in
METHODS
ambulation, a magnetic resonance imaging of the skull
Review of clinical, laboratory, and neuroradiologic (Figure 2A) was completed, which showed no evidence
data of the sample of patients affected by metachro- of demyelination and presented all other parameters
matic leukodystrophy at a referral center for the treat- within normality. The mother reported that, at 2 years
ment of rare diseases in the state of São Paulo. and 1 month, there was asthenia and regression of
the ability to ambulate, even with assistance, and a
gradual reduction of the volume of speech until it was
RESULTS
completely lost. At 2 years and 3 months, there was
Case 1
asthenia of the cervical muscles and the onset of limb
Male patient, 6 years old, son of non-consanguin- spasticity. Therapy with Sodium Valproate was pre-
eous parents. Born by cesarean delivery, at full-term. scribed, and the onset of frequent choking with liquids
Presented, at birth, APGAR 9 in the 1st minute and 10 (water and medicines) was noticed. Thus, a diet of food
in the 5th minute, weighed 2700g and head circumfer- pastes was started and, finally, a nasoenteral tube was
ence of 35 cm (P50). At 2 years and 3 months, sought used for 11 months. Frequent episodes of gastroesoph-
treatment with an orthopedist due to regression of gait ageal reflux and aspiration pneumonia were reported
associated with frequent falls and, at 3 years, started in the following 3 months. At 3 years and 3 months, a
presenting regression of language and a complete Nissen surgery was carried out for the correction of
inability to ambulate. Magnetic resonance imaging reflux and gastrostomy. At 3 years and 9 months, a
of the skull and an electroencephalogram (EEG) were new magnetic resonance imaging of the skull (Figure
requested, which presented the following abnormali- 2B) was completed, which showed abnormal bilateral
ties: abnormal white matter (diffuse alteration of mye- signal and symmetrical periventricular and subcortical
linization with signs of axonal dysfunction and active white matter, supra- and infratentorial, conferring it a
myelin damage) and GEE compatible with diffuse striped/tiger pattern appearance. Currently, the child
encephalopathy. There was a suspicion of neuromet- weighs 17 kg, is 105 cm tall, has a BMI of 15.419 kg/m2,
abolic disease and, thereafter, exams were requested and takes Baclofen, Ranitidine, Levetiracetam, Risper-
for the enzyme dosage of blood ARSA and the dosage idone, N-acetylcysteine, Phenobarbital, Beclometha-
of urine sulfatídes, which showed reduced activity of sone, Montelukast, Lactulose, Budesonide. Diagram 2
the ARSA enzyme and high concentrations of sulfatídes
in urine, respectively. At 4 years and 4 months, the Case 3
parents reported the onset of anorexia as a result of Female patient, 3 years and 9 months old, child
pneumonia, with the need for using gastrostomy in an of non-consanguineous parents. Presented, at birth,
attempt to improve the condition. Currently, the child APGAR 9 in the 1st minute and 10 in the 5th minute,
weighs 11.3 kg and measures 93 cm, BMI of 13.06 kg/ weighed 3400g and measured 49 cm, which placed her
m2 (P15), undergoes follow-up with a speech therapist at the percentile 50 of age and height based on age.
and physiotherapist, and takes Carbamazepine, Oxcar- She was born with hypoglycemia, with suspected early
bazepine, Simvastatin, Phenobarbital, N-acetylcysteine, sepsis, and was hospitalized in the ICU for 7 days. She
Phosphoethanolamine,’1 Botulinum Toxin. Diagram 2. was exclusively breastfed on free demand during the
first six months. The patient presented normal neu-
Case 2 rological, psychological, and motor development up
A female patient, 5 years old, daughter of consan- to the age of 2 years. She evolved to the inability to
guineous parents, was referred for neurologic eval- ambulate at 2 years and 4 months. At 2 years and 7
uation due to a gait dysfunction. Pregnancy without months, magnetic resonance imaging was completed,
REV ASSOC MED BRAS 2020; 66(10):1344-1350 1346
BORGES, F. M. ET AL
FIGURE 2. (A) MAGNETIC RESONANCE OF THE SKULL WITH NO SIGNS OF ABNORMALITIES. (B) MAGNETIC
RESONANCE OF THE SKULL FROM THE SAME PATIENT SHOWING A STRIPED/TIGER PATTERN (RED ARROW).
SOURCE: The authors, 2019.
which showed extensive abnormal areas in the white therefore, has recently undergone surgery to correct
matter of the brain hemispheres, suggestive of cere- the shortening of the Achilles tendons in both lower
bral metabolic disease. After imaging examination, limbs, associated with the use of Botox and orthoses.
CSF was collected, which showed demyelination. At 3 Currently, the child weighs 12.98 kg, is 98 cm tall,
years, there was the onset of dysphagia for solid foods. is in the percentile 15 for height/age and below the
Currently, the diet consists of food pastes. The mother percentile 5 for weight/age, has a BMI of 13.51 kg/
reports that she underwent cesarean delivery, at 37 m2 and takes Simvastatin, Vitamin D, Vitamin B12,
weeks, due to maternal diabetes and that there were Baclofen, Clonazepam, N-Acetylcysteine, Curcuma
no complications. The patient presents spasticity and, Longa (Zingiberaceae). Diagram 2
DIAGRAM 2. COMPARISON BETWEEN THE
PATIENTS REPORTED, BASED ON THE LEVEL OF DISCUSSION
CONSANGUINITY, ENZYME LEVEL OF BLOOD
ARYLSULFATASE A, PATHOGENIC VARIANT, AGE OF MLD is characterized by metachromatic granules
INITIAL SYMPTOM, INITIAL SYMPTOM, AND AGE AT produced by the accumulation of sulfatídes13. In this
DIAGNOSIS. condition, the ARSA enzyme, which is coded by the
ARSA gene, is abnormally present14. Patients with this
condition can be classified based on the age of onset of
the disorder. Up to 4 years of age, MLD is called “late
infantile”, at ages 4-15 years is referred to as “juve-
nile”, and after the age of 15 years of age, as “adult”15.
The three patients reported are classified as the late
infantile presentation. Initially, MLD presents with
focal neurological deficits, behavior disorders, and
several other nonspecific signs and symptoms that
make its early diagnosis a challenge16.
In the late infantile presentation, at least 75% of
the cases present the onset of symptoms, on average,
prior to 18 months of age, while our study found that
SOURCE: The authors, 2019. the first symptoms appeared only at 24 months on
1347 REV ASSOC MED BRAS 2020; 66(10):1344-1350
Metachromatic leukodystrophy: pediatric presentation and the challenges of early diagnosis
average17. According to Kehrer et al.18, the initial clin- all possible ways, which will contribute to an early
ical manifestations commonly described in the late diagnosis and improvement of their quality of life.
infantile presentation are changes in muscle tonus, in Even though there is still no curative treatment
particular in the lower limbs, which evolves to motor for this disease, new therapeutic possibilities are
regression, present in 70% of the late infantile cases emerging, such as intrathecal enzyme replacement
and in all 3 patients described in our study. In addition, and hematopoietic stem-cell transplantation (HSCT)
the regression of speech and language is present in ⅔ associated with gene therapy.
of our patients, compared to 48% of those affected by HSCT aims to treat the manifestations of MLD in
the late infantile presentation in the study analyzed. the central nervous system; however, there are obsta-
Another important factor to be emphasized is the time cles that still prevent it from being timely offered to
between the first symptoms and the date of the diag- patients because it preferably should be performed in
nosis. According to this same author, the average time a pre-symptomatic or oligosymptomatic phase with
between these parameters was 12 months in patients an allogeneic donor. Other obstacles consist in the
with the late infantile presentation, which was also identification of a HLA-compatible donor to minimize
observed in the present study. However, a greater time the risks of the procedure, such as graft-versus-host
interval stands out in the patient of the second report, disease, and who should not be a carrier of pathogenic
i.e., 2 years and 3 months from the initial symptoms variants of MLD2. Although there has been a signifi-
until the diagnosis, which may affect the prognosis. cant improvement in allogeneic transplantation, the
In the study by Barboura et al.19, two patients with therapy is still controversial since data from results
the late infantile presentation showed MLD-charac- are limited and difficult to generalize to the public
teristic lesions on the white matter of the periven- affected due to the use of different eligibility criteria
tricular region on magnetic resonance, similar to the and transplantation protocols and different responses
findings of the study by Groeschel et al.20, which also to its deployment with different presentations of MLD.
identified the same abnormality in their patients. In addition, transplantation cannot be offered to indi-
We emphasize that, in addition to the demyelination viduals with significant neurological involvement17.22.
affecting predominantly the periventricular region, Recently, advances have allowed combining HSCT
it spares the subcortical area (U-fibers) of the white with gene therapy. Gene therapy is the delivery of
matter, as observed in the study by Barboura I and the genetic material, using viral vectors, to the cells or
present one. In addition, Groeschel et al.20 mention tissues of an individual for therapeutic purposes.
that the MRI images in the late infantile presentation It is possible to modify stem cells and autologous
are normal until the onset of the first symptoms. The hematopoietic progenitor cells using a lentivirus that
same can be seen in the case of patient number 2, expresses a functional ARSA enzyme, this is currently
who showed no signs of demyelination and other being tested in clinical trials with promising results.
MLD patterns in the first magnetic resonance imag- Studies have shown a reconstitution of ARSA activity
ing completed. in hematopoietic cells and in the cerebrospinal fluid.
In terms of laboratory exams, according to Van There is evidence of prevention of disease onset or
Rappard et al.21, the examination of the Arylsulfatase interruption of its progression with the restoration
A enzyme activity should not be the only parameter of normal levels regarding motor function and the
since this may be low in cases of pseudo-deficiency of conduction of impulses in the peripheral nerves17.22.
MLD alleles, which is caused by low enzyme activity Enzyme replacement therapy (ERT) is an alterna-
but the patient presents no symptoms. With the exam- tive that benefits from the enzyme provision via the
ination of urine sulfatídes it is possible to distinguish intrathecal route in patients with the late infantile
it from actual ARSA deficiency since, if the results are presentation; it requires a trained neurosurgery team
positive, MLD is confirmed. In the study presented, for the procedure to be performed and this method
the first two patients had reduced activity of the Aryl- is not capable of enabling the patient to produce
sulfatase enzyme and in the examination of the third the enzyme23.
patient, the activity is undetectable. The statement by Unfortunately; none of the patients described could
Van Rappard et al.21 corroborates the present study, participate in the clinical studies previously described
supporting the understanding that complementary due to the late diagnosis when they already presented
examinations are necessary to evaluate patients in advanced and irreversible sequelae from the disease.
REV ASSOC MED BRAS 2020; 66(10):1344-1350 1348
BORGES, F. M. ET AL
CONCLUSION
In short, Metachromatic Leukodystrophy is a rare, Author’s Contribution
devastating, and progressive hereditary disease. Given All authors participated in the study design with
the possibility of emerging treatments specific to this substantial contributions to the concept and design,
illness, it is vital to obtain an early diagnosis. Even in data acquisition, analysis, and interpretation, and
the absence of specific therapies, the correct diagno- drafting of the paper, with final approval of the ver-
sis allows the family genetic counseling and better sion to be published, thus conforming to the uniform
therapeutic follow-up of patients to manage the com- requirements of the International Committee of Med-
plications from the disease. ical Journal Editors.
ANNEX 1. MLD PRESENTATIONS: CLINICAL MANIFESTATIONS, DIFFERENTIAL DIAGNOSES, AND LABORATORY
TESTS.
Findings Late Infantile Presentation Juvenile Presentation Adult Presentation
Age of onset Between 0 and 4 years Between 4 and 15 years From 15 years onward
Main clinical -Developmental delay (gait, speech, etc.) -Behavioral changes -Behavioral changes (depression,
manifestations -Frequent falls -Learning difficulties anxiety, etc.)
-Hypotonia -Ataxia and frequent falls -Progressive dementia
-Decreased or absent tendon reflexes -Extrapyramidal involvement -Ataxia
-Optic atrophy and nystagmus -Epileptic seizures -Epileptic seizures
-Epileptic seizures
Survival From 6 months to 8 years From 10 to 20 years From 10 to 30 years
Main differential -Krabbe Disease -X-Linked Adrenoleukodystrophy -Psychosis
diagnoses -Mitochondrial Encephalopathy -Mitochondrial Encephalopathy -Neuropathies with a motor
-Canavan Disease -Neuroaxonal Dystrophy predominance
-Alexander Disease -Juvenile Krabbe Disease -Adult Krabbe Disease
-Neuroaxonal Dystrophy -Juvenile Gangliosidoses (GM1 and -Neuropathy, ataxia, and retinitis
GM2) pigmentosa (NARP)
-Adrenomyeloneuropathy
Image of the CNS -Abnormalities in the periventricular and -Abnormalities in the centrum -Abnormalities in the centrum
(MRI or CT) centrum semiovale white matter semiovale white matter semiovale white matter
-U-Fibers are spared -Beginning of the anterior pole in -Beginning of the anterior pole in
-Beginning of the posterior pole in the the posterior direction the posterior direction
anterior direction
SOURCE: Adapted from Artigalas3
REFERENCES
1. Black JW, Cumings JN. Infantile metachromatic leucodystrophy. J Neurol 9. Yavuz H, Yüksekkaya HA. Intestinal involvement in metachromatic leuko-
Neurosurg Psychiatry. 1961;24(3):233-9. dystrophy. J Child Neurol. 2011;26(1):117-20.
2. The online metabolic and molecular bases of inherited disease. McGraw-
10. IOS Press [Internet]. [citado 23 de abril de 2019]. Disponível em: https://
Hill Medical [Internet]. [citado 24 de abril de 2019]. Disponível em: https://
www.iospress.nl/book/differential-diagnosis-in-neurology/
ommbid.mhmedical.com/book.aspx?bookID=971
3. Artigalas OAP. Leucodistrofia metacromática: caracterização epidemiológica, 11. van Rappard DF, de Vries ALC, Oostrom KJ, Boelens JJ, Hollak CE, van der
bioquímica e clínica de pacientes brasileiros [Dissertação de Mestrado]. Knaap MS, et al. Slowly progressive psychiatric symptoms: think metachro-
Porto Alegre: Universidade Federal do Rio Grande do Sul; 2009. [cited 2019 matic leukodystrophy. J Am Acad Child Adolesc Psychiatry. 2018;57(2):74-6.
Apr 23]. Available from: https://lume.ufrgs.br/handle/10183/29560
12. Kumperscak HG, Paschke E, Gradisnik P, Vidmar J, Bradac SU. Adult meta-
4. Marcão AM, Wiest R, Schindler K, Wiesmann U, Weis J, Schroth G, et al. chromatic leukodystrophy: disorganized schizophrenia–like symptoms and
Adult onset metachromatic leukodystrophy without electroclinical periph- postpartum depression in 2 sisters. J Psychiatry Neurosci. 2005;30(1):33-6.
eral nervous system involvement: a new mutation in the ARSA gene. Arch
Neurol. 2005;62(2):309-13. 13. Mancini GM, van Diggelen OP, Huijmans JG, Stroink H, de Coo RF. Pit-
5. Ribeiro E, Ribeiro M. Leucodistrofia metacromática: relato de caso de dois falls in the diagnosis of multiple sulfatase deficiency. Neuropediatrics.
irmãos cosanguíneos. Rev Neurociências. 2014;21:580-6. 2001;32(1):38-40.
6. Artigalás O, Lagranha VL, Saraiva-Pereira ML, Burin MG, Lourenço CM, van 14. Ozkara HA, Topçu M. Sphingolipidoses in Turkey. Brain Dev.
der Linden H Jr, et al. Clinical and biochemical study of 29 Brazilian patients 2004;26(6):363–6.
with metachromatic leukodystrophy. J Inherit Metab Dis. 2010;33(Suppl
3):S257-62. 15. Developing Therapeutic Approaches for Metachromatic Leukodystrophy.
Drug Des Devel Ther. 2013;7:729-45.
7. Kohlschütter A. Lysosomal leukodystrophies: krabbe disease and metachro-
matic leukodystrophy. Handb Clin Neurol. 2013;113;1611-8. 16. Mahmood A, Berry J, Wenger DA, Escolar M, Sobeih M, Raymond G, et
8. Oak S, Rao S, Karmarkar S, Kulkarui B, Kalgutkar A, Malde A, et al. Papillo- al. Metachromatic leukodystrophy: a case of triplets with the late infan-
matosis of the gallbladder in metachromatic leukodystrophy. Pediatr Surg tile variant and a systematic review of the literature. J Child Neurol.
Int. 1997;12(5-6):424-5. 2010;25(5):572-80.
1349 REV ASSOC MED BRAS 2020; 66(10):1344-1350
Metachromatic leukodystrophy: pediatric presentation and the challenges of early diagnosis
17. Gomez-Ospina N. Arylsulfatase A deficiency. 2006 May 30 [Updated 2017 20. Groeschel S, Kehrer C, Engel C, Dali CI, Bley A, Steinfeld R, et al. Metachro-
Dec 14]. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews® matic leukodystrophy: natural course of cerebral MRI changes in relation to
[Internet]. Seattle: University of Washington, Seattle; 1993-2019. Available clinical course. J Inherit Metab Dis. 2011;34(5):1095-102.
from: https://www.ncbi.nlm.nih.gov/books/NBK1130/ 21. van Rappard DF, Boelens JJ, Wolf NI. Metachromatic leukodystrophy: dis-
ease spectrum and approaches for treatment. Best Pract Res Clin Endocrinol
18. Kehrer C, Groeschel S, Kustermann-Kuhn B, Bürger F, Köhler W, Kohlschüt- Metab. 2015;29(2):261-73.
ter A, et al; German LEUKONET. Language and cognition in children with
metachromatic leukodystrophy: onset and natural course in a nationwide 22. Sessa M, Lorioli L, Fumagalli F, Acquati S, Redaelli D, Baldoli C, et al. Len-
cohort. Orphanet J Rare Dis. 2014;9:18. tiviral haemopoietic stem-cell gene therapy in early-onset metachromatic
leukodystrophy: an ad-hoc analysis of a non-randomized, open-label, phase
19. Barboura I, Hadded S, Chebel S, Mansour RB, Chahed H, Gueddiche MN, 1/2 trial. Lancet. 2016;388(10043):476-87.
et al. Brain MRI and biological diagnosis in five Tunisians MLD patients. 23. Rosenberg JB, Kaminsky SM, Aubourg P, Crystal RG, Sondhi D. Gene ther-
Diagn Pathol. 2012;7:11. apy for metachromatic leukodystrophy. J Neurosci Res. 2016;94(11):1169-79.
REV ASSOC MED BRAS 2020; 66(10):1344-1350 1350
You might also like
- Module Five Wellness Plan HOPEDocument15 pagesModule Five Wellness Plan HOPEZelda Raniblanket100% (1)
- Invitation To Health Canadian 4th Edition Hales Solutions ManualDocument18 pagesInvitation To Health Canadian 4th Edition Hales Solutions ManualJosephGlasswosmr100% (15)
- Communication Skills For Pharmacists.Document153 pagesCommunication Skills For Pharmacists.SalahadinNo ratings yet
- Case Study No.8Document7 pagesCase Study No.8Tahira Zehra0% (1)
- Leukodystrophy Paper August 27thDocument7 pagesLeukodystrophy Paper August 27thZorbey TurkalpNo ratings yet
- Wolcott-Rallison Syndrome: Review Open AccessDocument13 pagesWolcott-Rallison Syndrome: Review Open AccessMazen BarhoushNo ratings yet
- Sdarticle PDFDocument9 pagesSdarticle PDFManjeev GuragainNo ratings yet
- American Academy of Neurology Key PointsDocument193 pagesAmerican Academy of Neurology Key Pointszayat13No ratings yet
- Spinocerebellar AtaxiaDocument22 pagesSpinocerebellar Ataxiatbuyinza21apNo ratings yet
- Juvenile Metachromatic Leucodystrophy A Rare Case ReportDocument2 pagesJuvenile Metachromatic Leucodystrophy A Rare Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical Cases in Pediatric Peripheral NeuropathyDocument23 pagesClinical Cases in Pediatric Peripheral NeuropathyMateen ShukriNo ratings yet
- The Rare and The Unexpected Miller Fisher SyndromeDocument4 pagesThe Rare and The Unexpected Miller Fisher SyndromedoctorebrahimNo ratings yet
- Neuroradiological Findings of Trisomy 13 in A Rare Long-Term SurvivorDocument3 pagesNeuroradiological Findings of Trisomy 13 in A Rare Long-Term Survivorchristian roblesNo ratings yet
- Pascual Child Dystonias Management Review 2006Document8 pagesPascual Child Dystonias Management Review 2006leslyjanetNo ratings yet
- Camargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Document6 pagesCamargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Rizki Muhammad RanandaNo ratings yet
- A Case of Pervasive Developmental Disorder With Chromosomal Translocation 1-4Document14 pagesA Case of Pervasive Developmental Disorder With Chromosomal Translocation 1-4Agustia Pratiwi AhmadNo ratings yet
- MR Findings in Leigh Syndrome With COX Deficiency and SURF-1 MutationsDocument6 pagesMR Findings in Leigh Syndrome With COX Deficiency and SURF-1 MutationsDrsandy SandyNo ratings yet
- A Magnetic Resonance Approach To Metabolic Disorders in ChildhoodDocument12 pagesA Magnetic Resonance Approach To Metabolic Disorders in ChildhoodAna TelloNo ratings yet
- Johnson 1996Document11 pagesJohnson 1996Ali AmokraneNo ratings yet
- EFNS-guideline ALS PDFDocument22 pagesEFNS-guideline ALS PDFAhmad ShokryNo ratings yet
- Animal Model of EADocument13 pagesAnimal Model of EAzigurat00No ratings yet
- Senior-Loken Syndrome With Rare Manifestations: A Case ReportDocument5 pagesSenior-Loken Syndrome With Rare Manifestations: A Case ReportAndrie GunawanNo ratings yet
- A Sonographic Approach To The Prenatal Diagnosis of Skeletal DysplasiasDocument19 pagesA Sonographic Approach To The Prenatal Diagnosis of Skeletal DysplasiasminhhaiNo ratings yet
- Tolosa-Hunt Syndrome: A Rare Cause For An Isolated Ocular Nerve Palsy in An Elderly MaleDocument3 pagesTolosa-Hunt Syndrome: A Rare Cause For An Isolated Ocular Nerve Palsy in An Elderly MaleElisabeth TikalakaNo ratings yet
- BAAPSDocument147 pagesBAAPSGaurav Patodia100% (1)
- LDM - Bionature 2021-06-03-32Document8 pagesLDM - Bionature 2021-06-03-32JUAN CAMILO GONZALEZ JULIONo ratings yet
- Laporan Tutorial Edit 2Document21 pagesLaporan Tutorial Edit 2Magenda BismaNo ratings yet
- 1 s2.0 S1071909198800077 MainDocument8 pages1 s2.0 S1071909198800077 MainamandaribeirouNo ratings yet
- Spinal Muscular Atrophy: Stephen J. Kolb,, John T. KisselDocument16 pagesSpinal Muscular Atrophy: Stephen J. Kolb,, John T. KisselZouhour MiladiNo ratings yet
- A Rare Case Report On Metachromatic Leukodystrophy Presenting With Regression of MilestoneDocument3 pagesA Rare Case Report On Metachromatic Leukodystrophy Presenting With Regression of MilestoneBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Marfan Syndrome With Atypical PresentationDocument4 pagesMarfan Syndrome With Atypical PresentationaiNo ratings yet
- Enfermedades LisosomalesDocument32 pagesEnfermedades LisosomalesJonathanOmarLaraAcevedoNo ratings yet
- Ehara 1997Document9 pagesEhara 1997jahfdfgsdjad asdhsajhajdkNo ratings yet
- Transient Idiopathic Dystonia Infancy PDF Acta Paediatrica 2011Document4 pagesTransient Idiopathic Dystonia Infancy PDF Acta Paediatrica 2011Ana SopaNo ratings yet
- Total Agenesis of The Corpus Callosum in A Patient With Childhood-Onset SchizophreniaDocument4 pagesTotal Agenesis of The Corpus Callosum in A Patient With Childhood-Onset SchizophreniaBhagyaraj JeevangiNo ratings yet
- Amyotrophic Lateral Sclerosis A.: Excellent History But Was This Copy-Pasted?Document8 pagesAmyotrophic Lateral Sclerosis A.: Excellent History But Was This Copy-Pasted?Allan CastroNo ratings yet
- Alpers' DiseaseDocument5 pagesAlpers' DiseaseDANY PAUL BABYNo ratings yet
- Primary Progressive Apraxia: A Syndrome Difficult To CategorizeDocument2 pagesPrimary Progressive Apraxia: A Syndrome Difficult To CategorizeGuilherme AméricoNo ratings yet
- CUSTODIO Y MONTESINOS 2020 Frontotemporal IMAGENDocument8 pagesCUSTODIO Y MONTESINOS 2020 Frontotemporal IMAGENMAXIMILIANO HEREDIANo ratings yet
- Clínica de La Epilepsia en Los Trastornos Del Espectro AutistaDocument7 pagesClínica de La Epilepsia en Los Trastornos Del Espectro AutistaVanesa RodriguezNo ratings yet
- Noonan Syndrome: Clinical Aspects and Molecular PathogenesisDocument25 pagesNoonan Syndrome: Clinical Aspects and Molecular PathogenesisFlavia ChNo ratings yet
- Lipofuscinosis Neuronal Ceroidea Infantil Tardía. Reporte de Un CasoDocument6 pagesLipofuscinosis Neuronal Ceroidea Infantil Tardía. Reporte de Un Casomauro3022No ratings yet
- Spinal DisDocument32 pagesSpinal DisAkmal Niam FirdausiNo ratings yet
- PDF 01litvanDocument10 pagesPDF 01litvanmartinetti2013No ratings yet
- Deficiencias Iniciales en La Enfermedad de Alzheimer: Tres Ejemplos PrácticosDocument5 pagesDeficiencias Iniciales en La Enfermedad de Alzheimer: Tres Ejemplos PrácticosBM CNo ratings yet
- Case Report: de Morsier Syndrome Associated With Periventricular Nodular HeterotopiaDocument4 pagesCase Report: de Morsier Syndrome Associated With Periventricular Nodular HeterotopiahypnonautNo ratings yet
- 3 10 20 691 PDFDocument2 pages3 10 20 691 PDFVaisnaviNo ratings yet
- Full Text 01Document8 pagesFull Text 01Zunaira AmberNo ratings yet
- Schizophrenia: Overview and Treatment OptionsDocument18 pagesSchizophrenia: Overview and Treatment OptionsMeindayaniNo ratings yet
- Neuroimaging Comparison of Primary Progressive Apraxia of Speech and Progressive Supranuclear PalsyDocument9 pagesNeuroimaging Comparison of Primary Progressive Apraxia of Speech and Progressive Supranuclear PalsyJose Alonso Aguilar ValeraNo ratings yet
- Leighton Et Al 2001. Disordered Breathing During Sleep in Patients With MucopolysaccharidosesDocument12 pagesLeighton Et Al 2001. Disordered Breathing During Sleep in Patients With MucopolysaccharidosesBoNo ratings yet
- Multiple Sistem AtrofiDocument10 pagesMultiple Sistem AtrofiYehuda SimbiakNo ratings yet
- Ataxias EspasticasDocument12 pagesAtaxias EspasticasOsvaldo CortésNo ratings yet
- A Fatal Outcome of A Neonatal Dilated Cardiomyopathy: Evolutive Neonatal Lupus or Earlier Childhood - Onset Systemic Lupus? A Case ReportDocument14 pagesA Fatal Outcome of A Neonatal Dilated Cardiomyopathy: Evolutive Neonatal Lupus or Earlier Childhood - Onset Systemic Lupus? A Case ReportIJAR JOURNALNo ratings yet
- SCAR1Document17 pagesSCAR1ADRIANA DE FREITAS SOUSANo ratings yet
- Dapus Amok 18 PDFDocument18 pagesDapus Amok 18 PDFmuiNo ratings yet
- Cerebral Palsy Sumber AaprmDocument6 pagesCerebral Palsy Sumber AaprmBiandaNo ratings yet
- Myoclonus With DementiaDocument8 pagesMyoclonus With DementiaSantosh DashNo ratings yet
- Clorhidrato de Buspirona en El Tratamiento de La Ataxia CerebelosaDocument5 pagesClorhidrato de Buspirona en El Tratamiento de La Ataxia CerebelosaRenato Byrontt Letelier BernalNo ratings yet
- Cerebral PalsyDocument40 pagesCerebral PalsyStefan ChrisnawanNo ratings yet
- How Alcohol Damages Brain Development in ChildrenDocument14 pagesHow Alcohol Damages Brain Development in ChildrenBenjamin gutierrezNo ratings yet
- Ataxia AcutaDocument17 pagesAtaxia AcutaAlina AndreiNo ratings yet
- 5 Different Type of SyndromeDocument6 pages5 Different Type of SyndromeAdnan RezaNo ratings yet
- Teknik Pemeriksaan IodoterapiDocument8 pagesTeknik Pemeriksaan IodoterapiMike SihombingNo ratings yet
- Resistance of Haemonchus Spp. To Albendazole, Fenbendazole and Levamisole in 4 Goat Farms of Antioquia, ColombiaDocument5 pagesResistance of Haemonchus Spp. To Albendazole, Fenbendazole and Levamisole in 4 Goat Farms of Antioquia, ColombiaMike SihombingNo ratings yet
- Congenital Malformations Associated With Maternal DiabetesDocument7 pagesCongenital Malformations Associated With Maternal DiabetesMike SihombingNo ratings yet
- Aspek Neuroendokrin PubertasDocument38 pagesAspek Neuroendokrin PubertasMike SihombingNo ratings yet
- Reagen Dan Instrumen Pendukung Untuk Laboratorium Pengujian COVID-19Document14 pagesReagen Dan Instrumen Pendukung Untuk Laboratorium Pengujian COVID-19Mike SihombingNo ratings yet
- DIabetesinsipidus TB ARDocument5 pagesDIabetesinsipidus TB ARMike SihombingNo ratings yet
- Hospital Malnutrition in Pediatric Surgery at Dr. Cipto Mangunkusumo General Hospital 2015 and Its Associated FactorsDocument5 pagesHospital Malnutrition in Pediatric Surgery at Dr. Cipto Mangunkusumo General Hospital 2015 and Its Associated FactorsMike SihombingNo ratings yet
- Bedside Pediatric Early Warning SystemDocument38 pagesBedside Pediatric Early Warning SystemMike SihombingNo ratings yet
- 1.10. Follow Up: S Keluhan: BAB Hitam (-), Nyeri Ulu Hati Dan Perut Kanan Atas (-) ODocument8 pages1.10. Follow Up: S Keluhan: BAB Hitam (-), Nyeri Ulu Hati Dan Perut Kanan Atas (-) OMike SihombingNo ratings yet
- Characteristics and Prognosis in Women and Men With Type 1 Diabetes Undergoing Coronary Angiography: A Nationwide Registry ReportDocument8 pagesCharacteristics and Prognosis in Women and Men With Type 1 Diabetes Undergoing Coronary Angiography: A Nationwide Registry ReportMike SihombingNo ratings yet
- Pendekatan Farmakogenomik Dalam Pengembangan Obat Baru: April 2005Document12 pagesPendekatan Farmakogenomik Dalam Pengembangan Obat Baru: April 2005Mike SihombingNo ratings yet
- SFT WFH Girls P 2 5Document4 pagesSFT WFH Girls P 2 5Mike SihombingNo ratings yet
- Occupational English Test Listening Test - 2Document6 pagesOccupational English Test Listening Test - 2Jojelyn Yanez BaliliNo ratings yet
- Mono Bilberry - Oral EnglishDocument5 pagesMono Bilberry - Oral EnglishTom DelongeNo ratings yet
- PPE-25-Case Report of Aquagenic UrticariaDocument2 pagesPPE-25-Case Report of Aquagenic UrticariaSajin AlexanderNo ratings yet
- Canine OA Recognition and ManagementDocument10 pagesCanine OA Recognition and ManagementAngeles MerinoNo ratings yet
- Complications of Orthognathic SurgeryDocument39 pagesComplications of Orthognathic SurgeryAME DENTAL COLLEGE RAICHUR, KARNATAKANo ratings yet
- Case 2Document155 pagesCase 2Jade HemmingsNo ratings yet
- Cilia 2018Document1 pageCilia 2018Anna Beatriz Silva EspindolaNo ratings yet
- DNB Final Theory Papers Ophthalmology 2011 2020Document160 pagesDNB Final Theory Papers Ophthalmology 2011 2020Rekha JakharNo ratings yet
- Eli LillyDocument11 pagesEli LillyvemaNo ratings yet
- From The AcademyDocument13 pagesFrom The AcademySrinivas PingaliNo ratings yet
- Facility-Onset Infections(s) Device-Or Care-Related: Clostridioides DifficileDocument2 pagesFacility-Onset Infections(s) Device-Or Care-Related: Clostridioides DifficileHeba HanyNo ratings yet
- Pathology Chanting 230711 104344Document35 pagesPathology Chanting 230711 104344Smile forever100% (1)
- Product and Company Identification: SIFCO Process Solution Cadmium LHEDocument7 pagesProduct and Company Identification: SIFCO Process Solution Cadmium LHEshaotao guoNo ratings yet
- 7.stool Examination - Morphology of Eggs, Cysts, LarvaeDocument9 pages7.stool Examination - Morphology of Eggs, Cysts, LarvaeKowshik AvulaNo ratings yet
- Safety and Operating Instructions: Trench CompactorDocument40 pagesSafety and Operating Instructions: Trench CompactoralmirNo ratings yet
- Vitiligo A Review 2020 PDFDocument22 pagesVitiligo A Review 2020 PDFhannah khumairahNo ratings yet
- VV 1222 02Document5 pagesVV 1222 02Vy CaoNo ratings yet
- Roxana M. Culcer, M.D., FRACP - Aproach To A Collapsed NeonateDocument32 pagesRoxana M. Culcer, M.D., FRACP - Aproach To A Collapsed Neonatenicu 2021No ratings yet
- Periodontitis y Enfermedad CardiovascularDocument8 pagesPeriodontitis y Enfermedad CardiovascularDafne MendozaNo ratings yet
- Yellow Perils and Hate CrimesDocument21 pagesYellow Perils and Hate CrimesBach ĐứcNo ratings yet
- The World Health Organization A History: April 2019Document25 pagesThe World Health Organization A History: April 2019gkoutzioNo ratings yet
- Nosocomial Infections: Causes, Controls, Preventions and Future ChallengesDocument11 pagesNosocomial Infections: Causes, Controls, Preventions and Future ChallengesAy GlassesNo ratings yet
- Holographic Memory ResolutionDocument4 pagesHolographic Memory ResolutionDarnellNo ratings yet
- Rapidly Establishing A Hospital Based Convalescent Plasma Col - 2021 - AcademicDocument6 pagesRapidly Establishing A Hospital Based Convalescent Plasma Col - 2021 - AcademicdanielwongtsNo ratings yet
- HDU AuditDocument3 pagesHDU AuditAsdf DgfhgNo ratings yet
- Woc Acute Pancreatitis EngDocument10 pagesWoc Acute Pancreatitis EngMuhammad Alvin Fuzail IyazNo ratings yet