Professional Documents
Culture Documents
Management of Antithrombotic Therapy For Neuraxial and Peripheral Nerve Procedures
Management of Antithrombotic Therapy For Neuraxial and Peripheral Nerve Procedures
Uploaded by
jojobodOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Antithrombotic Therapy For Neuraxial and Peripheral Nerve Procedures
Management of Antithrombotic Therapy For Neuraxial and Peripheral Nerve Procedures
Uploaded by
jojobodCopyright:
Available Formats
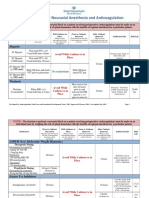
MANAGEMENT OF ANTITHROMBOTIC THERAPY
FOR NEURAXIAL AND PERIPHERAL NERVE PROCEDURES1
Guidelines to Prevent Neuraxial Hematoma after Epidural/Intrathecal/Spinal Injections and
Perineural Hematoma following Peripheral Nerve procedures, excluding Chronic Pain Procedures ONLY
These guidelines are not intended to supersede clinical judgement.
ATTENTION! WHEN CAN YOU SAFELY DO NEURAXIAL/PERIPHERAL NERVE PROCEDURES OR GIVE ANTITHROMBOTIC AGENTS?
NOTE: For concerns related to bleeding or traumatic procedures, contact Pain Service.
PRECAUTIONS:
Do NOT give MULTIPLE anticoagulants, including antiplatelet agents, concurrently in patients undergoing Neuraxial/Nerve Procedures.
Delay restarting anticoagulants for 24 hours after traumatic needle placement.
A. PRIOR TO B. WHILE C. AFTER
NEURAXIAL/NERVE NEURAXIAL/NERVE NEURAXIAL/NERVE
PROCEDURE CATHETER IN PLACE PROCEDURE
Minimum time between last Restrictions on use of antithrombotic Minimum time between
MEDICATION dose of antithrombotic agent agents while neuraxial/nerve catheters neuraxial injection or
AND neuraxial injection or are in place and prior to their removal neuraxial/nerve catheter
neuraxial/nerve catheter removal AND next dose of
placement antithrombotic agent
ANTICOAGULANTS FOR VTE PROPHYLAXIS
heparin unfractionated May be given; no time restrictions for neuraxial injection or neuraxial/nerve catheter placement
5000 units SQ Q8H or Q12H Does not require Pain Service approval.
CONTRAINDICATED
while catheter in place.
* heparin unfractionated 12 hours 4 hours
May NOT be given unless approve by
7500 units SQ Q8H
Pain Service Attending
* dalteparin (Fragmin)
5000 units SQ QDay May be given BUT:
•Must wait 8 hours after catheter
12 hours – CrCl ≥ 30 ml/min
PLACEMENT before giving dose 4 hours
24 hours – CrCl < 30 ml/min
•Must wait 12 hours after last dose
* enoxaparin (Lovenox) before REMOVING catheter
40mg SQ QDay
* enoxaparin (Lovenox)
12 hours – CrCl ≥ 30 ml/min
30mg SQ Q12H or 4 hours
24 hours – CrCl < 30 ml/min CONTRAINDICATED
40mg SQ Q12H
while catheter in place.
May NOT be given unless approved by
fondaparinux (Arixtra) 48 hours – CrCl ≥ 30 ml/min Pain Service Attending
6 hours
2.5mg SQ QDay CrCl < 30 ml/min: Call Hematology
48 hours – CrCl ≥ 50 ml/min
apixaban (Eliquis)
72 hours – CrCl 30-50 ml/min
2.5mg bid (prophylaxis)
CrCl < 30 ml/min: Call Hematology
May be given BUT:
48 hours – CrCl ≥ 50 ml/min •Must wait 8 hours after catheter
rivaroxaban (Xarelto)
72 hours – CrCl 30-50 ml/min PLACEMENT before giving dose 6 hours
10mg po QDay (prophylaxis)
CrCl < 30 ml/min: Call Hematology •Must wait 12 hours after last dose
before REMOVING catheter
72 hours – CrCl ≥ 30 ml/min
betrixaban (Bevyxxa)
96 hours – CrCl 15-30 ml/min
80mg QDay (prophylaxis)
CrCl < 15 ml/min: Call Hematology
* for use of these specific agents/doses with select superficial, lower extremity PNCs at Harborview Medical Center only, see internal
recommendations available on HMC Integrated Pain Care Program website:
https://hmc.uwmedicine.org/BU/pain/Documents/Anticoagulation%20for%20select%20PNCs.pdf
JUNE 2021 Page 1
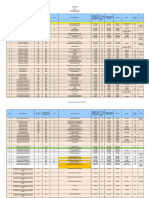
MANAGEMENT OF ANTITHROMBOTIC THERAPY
FOR NEURAXIAL AND PERIPHERAL NERVE PROCEDURES1
Guidelines to Prevent Neuraxial Hematoma after Epidural/Intrathecal/Spinal Injections and
Perineural Hematoma following Peripheral Nerve procedures, excluding Chronic Pain Procedures ONLY
These guidelines are not intended to supersede clinical judgement.
AGENTS USED FOR FULL SYSTEMIC ANTICOAGULATION
48 hours – CrCl ≥ 50 ml/min
apixaban (Eliquis) 72 hours – CrCl 30-50 ml/min
CrCl < 30 ml/min: Call Hematology
2.5mg bid – 10mg bid
*If neuraxial needed sooner, check
apixaban level
rivaroxaban (Xarelto) 48 hours – CrCl >50 ml/min
15-20mg po qday or 15mg bid CrCl < 50 ml/min: Call Hematology
CONTRAINDICATED
while catheter in place.
edoxaban (Savaysa) 48 hours – CrCl ≥ 50 ml/min May NOT be given unless approved by 6 hours
30-60mg QDay CrCl < 50 mL/min: Call Hematology
Pain Service Attending
72 hours – CrCl 50 ml/min
dabigatran (Pradaxa)
120 hours – CrCl 30-50 ml/min
75mg bid – 150mg bid
CrCl < 30 ml/min: Call Hematology
fondaparinux (Arixtra) 72 hours – CrCl ≥ 30 ml/min
5-10mg SQ QDay CrCl < 30 ml/min: Call Hematology
dalteparin (Fragmin)
24 hours – CrCl ≥ 30 ml/min
200 Units/kg SQ QDay or
48 hours – CrCl < 30 ml/min
100 Units/kg SQ Q12H
enoxaparin (Lovenox)
24 hours – CrCl ≥ 30 ml/min
1.0 - 1.5mg/kg SQ QDay or
48 hours – CrCl < 30 ml/min
1mg/kg SQ Q12H
CONTRAINDICATED
while catheter in place.
heparin unfractionated when aPTT normal or anti-Xa
May NOT be given unless approved by 4 hours
IV infusion activity undetectable
Pain Service Attending
heparin unfractionated when aPTT normal or anti-Xa
full dose SQ activity undetectable
warfarin (Coumadin) when INR ≤ 1.5
DIRECT THROMBIN INHIBITORS, INJECTABLE
when DTI assay < 40 CONTRAINDICATED
argatroban or aPTT < 40 sec while catheter in place.
IV continuous infusion May NOT be given unless approved by
Pain Service Attending
when DTI assay < 40 4 hours
or aPTT < 40 sec
bivalirudin (Angiomax)
IV continuous infusion
JUNE 2021 Page 2
MANAGEMENT OF ANTITHROMBOTIC THERAPY
FOR NEURAXIAL AND PERIPHERAL NERVE PROCEDURES1
Guidelines to Prevent Neuraxial Hematoma after Epidural/Intrathecal/Spinal Injections and
Perineural Hematoma following Peripheral Nerve procedures, excluding Chronic Pain Procedures ONLY
These guidelines are not intended to supersede clinical judgement.
ANTIPLATELET AGENTS pages 285-286
aspirin or NSAIDS May be given; no time restrictions for neuraxial injection or neuraxial/nerve catheter placement
Does not require Pain Service approval
abciximab (Reopro)
48 hours
IV continuous infusion
aspirin/dipyridamole
24 hours
(Aggrenox)
cangrelor (Kengreal)
3 hours
IV continuous infusion
clopidogrel (Plavix) CONTRAINDICATED
while catheter in place.
6 hours
May NOT be given unless approved by
prasugrel (Effient) 7 days Pain Service Attending
ticagrelor (Brilinta)
tirofiban (Aggrastat)
IV continuous infusion
8 hours– CrCl > 50 ml/min
CrCl < 50 Call Hematology
eptifibatide (Integrelin)
IV continuous infusion
THROMBOLYTIC AGENTS
alteplase (TPA) May be given; no time restrictions for neuraxial injection or neuraxial/nerve catheter placement
1mg dose for catheter Does not require Pain Service approval
clearance (Maximum dose 4mg/24 hours)
alteplase (TPA) CONTRAINDICATED
full dose for stroke, MI, etc while catheter in place.
48 hours 10 days
May NOT be given unless approved by
Pain Service Attending
References
Horlocker TT et al. Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence Based Guidelines (4th ed).
Reg Anesth Pain Med 2018; 43(3):263-309
Burnett AE, et al. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis (2016) 41:206–232. DOI 10.1007/s11239-015-1310-7.
Each recommendation was reviewed by members of anesthesiology, hematology and pharmacy to determine the
class (strength of recommendation) and level (quality of the evidence) using the 2018 American Society of
Regional Anesthesia and Pain Medicine (ASRA) Guidelines. These recommendations were approved by the
UW Medicine Thrombosis and Anticoagulation Safety Committee. In any case of discrepancy from the ASRA
2018 Regional and Antithrombotic Guidelines, a final decision was reached after consideration of medication
pharmacokinetics, procedure and thrombosis risk and clinical experience. These guidelines are not intended to
set out a legal standard of care and do not replace medical care or the judgment of the responsible medical
professional considering all the circumstances presented by an individual patient. This consensus statement is
not intended to ensure a successful patient outcome in every situation and is not a guarantee of any specific
outcome.
JUNE 2021 Page 3
You might also like
- Anesthesia Oral Board Review - Jessica A Lovich-SapolaDocument497 pagesAnesthesia Oral Board Review - Jessica A Lovich-Sapolazeispaul23No ratings yet
- Westmead Obstetric Anaesthesia Manual 2020Document72 pagesWestmead Obstetric Anaesthesia Manual 2020DavidNo ratings yet
- Medicine AnswersDocument6 pagesMedicine AnswersHarsha Vipin100% (5)
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideFrom EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuideNo ratings yet
- A Sample Report of Pharmacy TrainingDocument34 pagesA Sample Report of Pharmacy Trainingsaransh misra100% (2)
- BASIC Exam Blueprint PDFDocument3 pagesBASIC Exam Blueprint PDFmichael100% (1)
- Obestetrics GynecologyDocument203 pagesObestetrics GynecologySwamynadh Gandhi ReddiNo ratings yet
- Complications of Spinal and Epidural AnesthesiaDocument45 pagesComplications of Spinal and Epidural AnesthesiashikhaNo ratings yet
- Developments in High Potency API ManufacturingDocument1 pageDevelopments in High Potency API Manufacturingraju1559405100% (1)
- Breast CancerDocument18 pagesBreast CancerJohn AlcantaraNo ratings yet
- Document PDFDocument4 pagesDocument PDFDebasis SahooNo ratings yet
- General-Anesthesia Part 5Document4 pagesGeneral-Anesthesia Part 5Dianne GalangNo ratings yet
- TIVA - Copy (2) - Copy-1Document34 pagesTIVA - Copy (2) - Copy-1Keerthikumar Parvatha100% (2)
- Awareness Under AnesthesiaDocument27 pagesAwareness Under AnesthesiaagatakassaNo ratings yet
- 4.muscle RelaxantsDocument23 pages4.muscle Relaxantskarim hassanNo ratings yet
- Anesthesia For Kidney TransplantDocument6 pagesAnesthesia For Kidney TransplantachyutsharmaNo ratings yet
- Stoelting Anasthesia and Co Existing Disease PDFDocument28 pagesStoelting Anasthesia and Co Existing Disease PDFEgidia SetyaNo ratings yet
- CCCDocument487 pagesCCCSlaviša KovačevićNo ratings yet
- Anesthesia For Genitourinary SurgeryDocument76 pagesAnesthesia For Genitourinary SurgeryWenny Eka FildayantiNo ratings yet
- General-Anesthesia Part 3Document5 pagesGeneral-Anesthesia Part 3Dianne GalangNo ratings yet
- ANESTHESIA-Pediatrics Airway SyndromesDocument12 pagesANESTHESIA-Pediatrics Airway SyndromeshollyuNo ratings yet
- 100HRS of Online Anaesthesia All SessionDocument17 pages100HRS of Online Anaesthesia All SessionJagannath HansdaNo ratings yet
- Awareness in Anesthesia FinalisedDocument42 pagesAwareness in Anesthesia FinalisedLean CyNo ratings yet
- General Anesthesia: Presented By: Shalakha Bhardwaj BDS Final Year (2007-2011)Document85 pagesGeneral Anesthesia: Presented By: Shalakha Bhardwaj BDS Final Year (2007-2011)KrishnaBihariShuklaNo ratings yet
- Anesthesia For Patients With Thyroid Disease - UpToDateDocument12 pagesAnesthesia For Patients With Thyroid Disease - UpToDateJavier GlezqNo ratings yet
- Journal of Anesthesiology MP State Vol 1Document37 pagesJournal of Anesthesiology MP State Vol 1cardiacanesthesiaNo ratings yet
- Regional Anesthesia Made Easy 2015Document35 pagesRegional Anesthesia Made Easy 2015Jeff GulitisNo ratings yet
- Anesthesia ManualDocument21 pagesAnesthesia ManualDocFrankNo ratings yet
- Anaesthesia 2022 Mcq'sDocument16 pagesAnaesthesia 2022 Mcq'sMiss IbrahimNo ratings yet
- Preoperative Patient Assessment and Management: Roxanne Jeen L. FornollesDocument61 pagesPreoperative Patient Assessment and Management: Roxanne Jeen L. FornollesRyan FornollesNo ratings yet
- Management of High Spinal AnesthesiaDocument8 pagesManagement of High Spinal AnesthesiaYeni TriastutikNo ratings yet
- AnaesthesiaDocument5 pagesAnaesthesiaAnonymous 4jkFIRalKNo ratings yet
- Regional Anesthesia Part 2Document9 pagesRegional Anesthesia Part 2Dianne GalangNo ratings yet
- Anesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaDocument3 pagesAnesthesia - State of Narcosis, Analgesia, Relaxation, and Loss of Reflex. Effects of AnesthesiaJhevilin RMNo ratings yet
- Royal College X AnesthesiaDocument66 pagesRoyal College X AnesthesiaManuela CormioNo ratings yet
- Regional Anesthesia Part 3Document5 pagesRegional Anesthesia Part 3Dianne GalangNo ratings yet
- MsmaidsDocument31 pagesMsmaidsnbrassarNo ratings yet
- Anesthesia TechnicianDocument1 pageAnesthesia TechnicianmahbbobNo ratings yet
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Physiology 20 21 22Document2 pages1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Physiology 20 21 22rkNo ratings yet
- 1095 Preoperative Risk Stratification and OptimizationDocument99 pages1095 Preoperative Risk Stratification and OptimizationHening Tirta KusumawardaniNo ratings yet
- Regional Anesthesia Part 1Document5 pagesRegional Anesthesia Part 1Dianne GalangNo ratings yet
- Anaesthetic Drug Crib Sheet-8Document1 pageAnaesthetic Drug Crib Sheet-8Tiarnán Byrne0% (2)
- Comparison of Two Approaches ofDocument96 pagesComparison of Two Approaches ofJacob OrtizNo ratings yet
- Anesthesia: A Comprehensive Review (5th Edition)Document1 pageAnesthesia: A Comprehensive Review (5th Edition)brakim23No ratings yet
- Fred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008Document53 pagesFred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008lmjeksoreNo ratings yet
- 9780190685157Document639 pages9780190685157Jaber AlhaizaeyNo ratings yet
- General-Anesthesia Part 1Document5 pagesGeneral-Anesthesia Part 1Dianne GalangNo ratings yet
- Update EmergenciesDocument84 pagesUpdate EmergenciesElaineNo ratings yet
- Anaesthesia For Neuroradiological Procedures Premalatha SDocument48 pagesAnaesthesia For Neuroradiological Procedures Premalatha SPrema LathaNo ratings yet
- Fundamentals of Anaesthesia and QBase Anesthesia 6Document2 pagesFundamentals of Anaesthesia and QBase Anesthesia 6Ch AhmedNo ratings yet
- Anesthesia For Multiple Trauma IntroductionDocument126 pagesAnesthesia For Multiple Trauma IntroductionabdishakurNo ratings yet
- Anaesthesia and Sedation Outside TheatresDocument15 pagesAnaesthesia and Sedation Outside Theatresمحمد زينNo ratings yet
- Journal ClubDocument26 pagesJournal Clubysindhura23gmailcom100% (1)
- C-Section Room Setup:: OB Rotation NotesDocument5 pagesC-Section Room Setup:: OB Rotation NotesEricNo ratings yet
- Regional Anesthesia and Acute Pain Medicine A Problem Based LearningDocument617 pagesRegional Anesthesia and Acute Pain Medicine A Problem Based LearningDAMIAN MERCADO BENTNo ratings yet
- Epidural AnaesthesiaDocument99 pagesEpidural AnaesthesiaabhinavguttikondaNo ratings yet
- Race 2007 PDFDocument236 pagesRace 2007 PDFRois Hasyim100% (1)
- Anesthesia For The Patient With Preeclampsia - UpToDateDocument31 pagesAnesthesia For The Patient With Preeclampsia - UpToDateJazivi AlejoNo ratings yet
- Checklist For Anaesthetic Equipment 2012Document2 pagesChecklist For Anaesthetic Equipment 2012that dude in duettesNo ratings yet
- Stanford Department of Anesthesiology Regional Anesthesia Syllabus Introduction (PDFDrive)Document335 pagesStanford Department of Anesthesiology Regional Anesthesia Syllabus Introduction (PDFDrive)Adam ForshawNo ratings yet
- Anesthetic Machine For StudentDocument76 pagesAnesthetic Machine For StudentMohmmed MousaNo ratings yet
- Failed Spinal AnaesthesiaDocument10 pagesFailed Spinal Anaesthesian12345678n100% (1)
- Obs QuestionsDocument14 pagesObs QuestionsMasseh YakubiNo ratings yet
- Evidence-Based Obstetric AnesthesiaFrom EverandEvidence-Based Obstetric AnesthesiaStephen H. HalpernNo ratings yet
- Sku Descripcion Fabricante Stoc KDocument35 pagesSku Descripcion Fabricante Stoc Kleidy andrea serrano caceresNo ratings yet
- Form Gdoc Febuari 2024Document84 pagesForm Gdoc Febuari 2024apotekcahayapakalNo ratings yet
- AeknilDocument2 pagesAekniljaycey24No ratings yet
- General Pharmacology MCQs (Edited)Document47 pagesGeneral Pharmacology MCQs (Edited)M7md AllahhamNo ratings yet
- AC200613 Full Answer KeyDocument26 pagesAC200613 Full Answer KeySuganya BalachandranNo ratings yet
- NithaDocument30 pagesNithaALINo ratings yet
- Peg & TPNDocument23 pagesPeg & TPNapi-3722454100% (1)
- Biowaiver Monograph For Immediate Release Solid Oral Dosage Forms OfloxacinDocument6 pagesBiowaiver Monograph For Immediate Release Solid Oral Dosage Forms Ofloxacinaanaal0% (1)
- UiuDocument3 pagesUiuleandro__scribdNo ratings yet
- Obat Topical2Document43 pagesObat Topical2nurwahidaNo ratings yet
- Medication Administration: BY Thomas PetriciniDocument204 pagesMedication Administration: BY Thomas PetricinisaheedvkNo ratings yet
- E Tender 20-03-18Document132 pagesE Tender 20-03-18gomathi ShankarNo ratings yet
- Respiratory Drugs Midterm ExamDocument10 pagesRespiratory Drugs Midterm ExamKevin VillaranteNo ratings yet
- BLS For Healthcare Providers Student ManualDocument2 pagesBLS For Healthcare Providers Student ManualdrsmiNo ratings yet
- Ampicillin PDFDocument3 pagesAmpicillin PDFandriNo ratings yet
- Drug Utilization Study of Antiepileptic Drugs In.21Document6 pagesDrug Utilization Study of Antiepileptic Drugs In.21Ramo EdumNo ratings yet
- Prometric Mcqs Plus CaculationsDocument147 pagesPrometric Mcqs Plus CaculationsShanaz KhanNo ratings yet
- Ace InhibitorsDocument15 pagesAce InhibitorsCarolyn Conn EdwardsNo ratings yet
- SJT Practice Paper With Rationales (NHS) PDFDocument74 pagesSJT Practice Paper With Rationales (NHS) PDFDorothea TangNo ratings yet
- Introduction To Pharmacoepidemiology PDFDocument17 pagesIntroduction To Pharmacoepidemiology PDFRhiny Erfiah RhindaNo ratings yet
- Cesarean Section Under Spinal Anesthesia in A Patient With Ankylosing SpondylitisDocument4 pagesCesarean Section Under Spinal Anesthesia in A Patient With Ankylosing SpondylitisFendy PrasetyoNo ratings yet
- Simply Better.: Innovation in Ultrasound-Guided Breast BiopsyDocument2 pagesSimply Better.: Innovation in Ultrasound-Guided Breast Biopsymarian.andrei.sebiNo ratings yet
- Injection Technique 1: Administering Drugs Via The Intramuscular RouteDocument3 pagesInjection Technique 1: Administering Drugs Via The Intramuscular RouteNur FaizahNo ratings yet
- Pharma Book ListDocument6 pagesPharma Book ListMedBook DokanNo ratings yet
- Antipsychotic DrugsDocument23 pagesAntipsychotic DrugsASHLEY DAWN BUENAFENo ratings yet
- QUIZ Classification of Surgery in TableDocument1 pageQUIZ Classification of Surgery in TableMaria Sheila BelzaNo ratings yet