Professional Documents
Culture Documents
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
Uploaded by
Man Tue ThaiCopyright:
Available Formats
You might also like
- Raheel OSCE Notes January 2023Document453 pagesRaheel OSCE Notes January 2023KamleshKumar100% (2)
- Varicocele Secrets: The Underground Solution for Getting Rid of Varicocele for The Rest of Your Life [EN]From EverandVaricocele Secrets: The Underground Solution for Getting Rid of Varicocele for The Rest of Your Life [EN]No ratings yet
- CrackTheNac 8 Case For The NAC OSCEDocument19 pagesCrackTheNac 8 Case For The NAC OSCEEmad Mergan100% (6)
- Station 5 Example ScenariosDocument12 pagesStation 5 Example ScenariosDavidJohnsonNo ratings yet
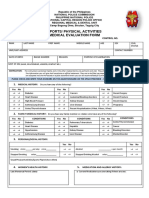
- Medical Evaluation Form 2022Document2 pagesMedical Evaluation Form 2022jimmy p. lamhi50% (2)
- Step 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionFrom EverandStep 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionNo ratings yet
- 2 CA - Health Profile - 2014-12-19 PDFDocument9 pages2 CA - Health Profile - 2014-12-19 PDFLiamNo ratings yet
- Health Unit Coordinator CoursesDocument13 pagesHealth Unit Coordinator CoursesMan Tue ThaiNo ratings yet
- PFT Medical Evaluation Form 1Document3 pagesPFT Medical Evaluation Form 1Dexter VenguaNo ratings yet
- Template - 2020 PAR-QDocument9 pagesTemplate - 2020 PAR-QJairo OntongNo ratings yet
- Pharmacotherapeutics Soft Copy DIIDocument95 pagesPharmacotherapeutics Soft Copy DIILiyakath AliNo ratings yet
- Detoxification Questionnaire: I. Medical Symptoms Questionnaire (MSQ)Document2 pagesDetoxification Questionnaire: I. Medical Symptoms Questionnaire (MSQ)ddddNo ratings yet
- Family Medicine - General Practice MEQ 2006Document6 pagesFamily Medicine - General Practice MEQ 2006jermie22100% (1)
- 11mastering Medical Long CaseDocument42 pages11mastering Medical Long CaseAthirahRaraNo ratings yet
- January2020PARQPlusFillable 1Document6 pagesJanuary2020PARQPlusFillable 1ssamyang92No ratings yet
- Pharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordDocument20 pagesPharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordNurwahidah Moh WahiNo ratings yet
- All CasesDocument32 pagesAll CasesMona NasrNo ratings yet
- ParQ Plus Jan 2023Document6 pagesParQ Plus Jan 2023troy montarilNo ratings yet
- Par QPlus 2022Document7 pagesPar QPlus 2022MARIKA BALONDONo ratings yet
- Opening The Consultation: Ideas, Concerns and Expectations (ICE)Document8 pagesOpening The Consultation: Ideas, Concerns and Expectations (ICE)Toria053No ratings yet
- ParQ Plus Jan 2022 FillableDocument5 pagesParQ Plus Jan 2022 FillableRaechelle DizonNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneJacquelynne Amba100% (1)
- Drug Study MedicineDocument24 pagesDrug Study MedicineLutzie PagulaNo ratings yet
- SkinDocument6 pagesSkinKrishna Faith P. DelaraNo ratings yet
- Physical Health CheckDocument9 pagesPhysical Health CheckDivya ThanlaeNo ratings yet
- LMCC II GuideDocument79 pagesLMCC II GuideSoleil DaddouNo ratings yet
- Parqplus 2020Document6 pagesParqplus 2020klinikcitrautamapalembangNo ratings yet
- At the Precipice: My Three-Year Journey from Stroke to Good Health with Type 2 DiabetesFrom EverandAt the Precipice: My Three-Year Journey from Stroke to Good Health with Type 2 DiabetesNo ratings yet
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Document49 pagesLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNo ratings yet
- Reading Test - 3 Clinical Depression Text ADocument17 pagesReading Test - 3 Clinical Depression Text AJisha JanardhanNo ratings yet
- The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesThe Physical Activity Readiness Questionnaire For EveryoneFrances RedNo ratings yet
- P Drugs - Personal Drugs For PatientsDocument30 pagesP Drugs - Personal Drugs For Patientsjco jac100% (1)
- Personal Health AssessmentDocument8 pagesPersonal Health AssessmenthelloNo ratings yet
- Coumadin Dosing GuideDocument3 pagesCoumadin Dosing Guidemorale28No ratings yet
- Multitable New Patient FormDocument8 pagesMultitable New Patient Forme-MedTools100% (9)
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- PatientDocument9 pagesPatientkcquitorianoNo ratings yet
- Soap FormsDocument6 pagesSoap FormsJunJieNo ratings yet
- Pharmaceutical Care Plan IIIDocument20 pagesPharmaceutical Care Plan IIIAdemilola AdekoyaNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument6 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneArnel Bagalawis100% (1)
- PAR-Q+: Oo Oo Oo OoDocument6 pagesPAR-Q+: Oo Oo Oo OoRoxyNo ratings yet
- Pre Employment Medical - Declaration - HMCL DOCTORSDocument2 pagesPre Employment Medical - Declaration - HMCL DOCTORSabhishek vermaNo ratings yet
- Self Report MedicationDocument3 pagesSelf Report MedicationMarjhun Flores GuingayanNo ratings yet
- Advance Care or Health Directive. July 2013: With YOUTUBE VIDEODocument2 pagesAdvance Care or Health Directive. July 2013: With YOUTUBE VIDEODr Jerome MellorNo ratings yet
- PFT Form 2023Document2 pagesPFT Form 2023Custodial Facility Pasig CPSNo ratings yet
- Pharmacy CounsellingDocument8 pagesPharmacy CounsellingChrissieNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneLenard PagsisihanNo ratings yet
- 1992-1997 and 2004 Questions and AnswersDocument56 pages1992-1997 and 2004 Questions and AnswersEmad MerganNo ratings yet
- Dominic Pathfit 1&2Document6 pagesDominic Pathfit 1&2Milbert Patun-ogNo ratings yet
- Botulism Toolkit: Emergency Recognition, Response and Anti Terrorism Training Associates (ERRATA, LLC.)Document18 pagesBotulism Toolkit: Emergency Recognition, Response and Anti Terrorism Training Associates (ERRATA, LLC.)Joko YantoNo ratings yet
- Groups ABCD - Family Medicine End Block QuestionsDocument10 pagesGroups ABCD - Family Medicine End Block QuestionsHisham ChomanyNo ratings yet
- FMcase 2Document27 pagesFMcase 2Ryan Townsend100% (3)
- CPS2 MED20 Scenario 1Document7 pagesCPS2 MED20 Scenario 1mNo ratings yet
- Clinical Document 1Document7 pagesClinical Document 1api-253709303No ratings yet
- Patient Education PlanDocument4 pagesPatient Education Planapi-248022066No ratings yet
- 2021 Revalida - Adult IMDocument11 pages2021 Revalida - Adult IMJv MataNo ratings yet
- Use of Antibiotics For Respiratory Tract Infections in Adults and ChildrenDocument7 pagesUse of Antibiotics For Respiratory Tract Infections in Adults and Childrendokter Hewan AdhonaNo ratings yet
- Measure Blood Pressure Accurately. Healthy Living Solutions Book 3 (for Professionals)From EverandMeasure Blood Pressure Accurately. Healthy Living Solutions Book 3 (for Professionals)Rating: 4 out of 5 stars4/5 (1)
- Staying Alive: The Signs That You Have to See a Doctor Right Now (and the Ways to Avoid Having to See One Again)From EverandStaying Alive: The Signs That You Have to See a Doctor Right Now (and the Ways to Avoid Having to See One Again)No ratings yet
- 2022 Oregon EITC NoticeDocument1 page2022 Oregon EITC NoticeMan Tue ThaiNo ratings yet
- PTO PolicyDocument5 pagesPTO PolicyMan Tue Thai100% (1)
- Mat Act Fact Sheet 117thDocument1 pageMat Act Fact Sheet 117thMan Tue ThaiNo ratings yet
- PA Prescription Requirements 12 18Document8 pagesPA Prescription Requirements 12 18Man Tue ThaiNo ratings yet
- Downtown STREETCAR MapDocument1 pageDowntown STREETCAR MapMan Tue ThaiNo ratings yet
- DumplingWeek 2023 PassportDocument1 pageDumplingWeek 2023 PassportMan Tue ThaiNo ratings yet
- K-ETA FAQ - (Eng)Document9 pagesK-ETA FAQ - (Eng)Man Tue ThaiNo ratings yet
- 2005 National Future Stars Developmental TeamDocument3 pages2005 National Future Stars Developmental TeamMan Tue ThaiNo ratings yet
- Wellness DiscountDocument1 pageWellness DiscountMan Tue ThaiNo ratings yet
- Micronutrients Assignment-14th EdDocument3 pagesMicronutrients Assignment-14th EdMan Tue ThaiNo ratings yet
- Spring 2016: Mon Tues Wed Thu FriDocument2 pagesSpring 2016: Mon Tues Wed Thu FriMan Tue ThaiNo ratings yet
- Associate Cover LetterDocument2 pagesAssociate Cover LetterMan Tue ThaiNo ratings yet
- The Crucial Acquisition of KnowledgeDocument5 pagesThe Crucial Acquisition of KnowledgeMan Tue ThaiNo ratings yet
- Fundamentals of Visualization With TableauDocument1 pageFundamentals of Visualization With TableauMan Tue ThaiNo ratings yet
- MT ThesisDocument19 pagesMT ThesisMan Tue ThaiNo ratings yet
- GraduationChecklist 003Document1 pageGraduationChecklist 003Man Tue ThaiNo ratings yet
- Eng/Npd Girish Comprehen Sive Charan Marketing: Internal Quality Audit Schedule No:Qms Ia-1Document1 pageEng/Npd Girish Comprehen Sive Charan Marketing: Internal Quality Audit Schedule No:Qms Ia-1DhinakaranNo ratings yet
- Migrating and Installing Avaya Appliance Virtualization PlatformDocument68 pagesMigrating and Installing Avaya Appliance Virtualization PlatformSathish RajanNo ratings yet
- MBA Course StructureDocument2 pagesMBA Course StructureAnupama JampaniNo ratings yet
- Math 8 Q3 Module 5 With Answer KeyDocument13 pagesMath 8 Q3 Module 5 With Answer KeyJimcris villamorNo ratings yet
- Electrical Engineering Software PDFDocument12 pagesElectrical Engineering Software PDFAkd Deshmukh50% (2)
- Plants and Animals Live Together Lesson PlanDocument3 pagesPlants and Animals Live Together Lesson Planapi-374921894No ratings yet
- Fundamentals of Thermal Sensors: Thu HuynhDocument39 pagesFundamentals of Thermal Sensors: Thu HuynhsamcaridoNo ratings yet
- Experiment 7: Investigating The Change of Volume in The Change of Temperature (Document2 pagesExperiment 7: Investigating The Change of Volume in The Change of Temperature (EDWIN SIMBARASHE MASUNUNGURENo ratings yet
- Ongc V Saw PipesDocument9 pagesOngc V Saw PipesManisha SinghNo ratings yet
- HT Motors Data SheetDocument3 pagesHT Motors Data SheetSE ESTNo ratings yet
- Normalized Impedance and Admittance Coordinates: Name Title Dwg. NoDocument1 pageNormalized Impedance and Admittance Coordinates: Name Title Dwg. NoJayeng WidiatmokoNo ratings yet
- Final Report: Simulation Using Star CCM+ Theory and Practice in Marine CFD BenaoeDocument10 pagesFinal Report: Simulation Using Star CCM+ Theory and Practice in Marine CFD BenaoeRaviindra singhNo ratings yet
- 2012 GR 7 Maths PDFDocument8 pages2012 GR 7 Maths PDFmarshy bindaNo ratings yet
- Değişim Sınavı 2020Document29 pagesDeğişim Sınavı 2020Mustafa CinNo ratings yet
- MRD Carotid StentDocument5 pagesMRD Carotid StentKhushboo WarhadeNo ratings yet
- 11thsamplebooklet PDFDocument200 pages11thsamplebooklet PDFSoumyodeep ChowdhuryNo ratings yet
- S17.s1 - Final Project - Inglés 3 - MANUEL LAURA MAMANIDocument3 pagesS17.s1 - Final Project - Inglés 3 - MANUEL LAURA MAMANIManuel Sebastian Laura MamaniNo ratings yet
- R1600H Sistema ImplementosDocument31 pagesR1600H Sistema ImplementosLuis Angel Pablo Juan de Dios100% (1)
- Digital NativesDocument10 pagesDigital NativesJonathan Blanco Sa RiyadhNo ratings yet
- Solucionario Ingenieria en Control Moderna OGATADocument240 pagesSolucionario Ingenieria en Control Moderna OGATAanandpj444471% (7)
- FMCG Organisation Chart: Board of DirectorsDocument1 pageFMCG Organisation Chart: Board of DirectorsKumar Panchal0% (1)
- Jadual BerkalaDocument2 pagesJadual BerkalaRohani Yusof75% (4)
- CMP 1 1 CDPDocument11 pagesCMP 1 1 CDPSachin NakadeNo ratings yet
- Philippine Notices To MarinersDocument42 pagesPhilippine Notices To MarinersTaneo Prince CalebNo ratings yet
- Name of Customer - Name of Project - TE-112045 - WFC - Print - OutDocument1 pageName of Customer - Name of Project - TE-112045 - WFC - Print - OutJavier EspinosaNo ratings yet
- Heat Exchanger Design CHE 311 Final Project MSUDocument15 pagesHeat Exchanger Design CHE 311 Final Project MSUnefoussiNo ratings yet
- 2018 Trial 1 Biology Questions and Marking SchemeDocument11 pages2018 Trial 1 Biology Questions and Marking SchemeKodhekNo ratings yet
- Beyond Locative Media - Mark Tuters and Kazys VarnelisDocument6 pagesBeyond Locative Media - Mark Tuters and Kazys VarnelisEduardoNo ratings yet
- Physics Notes Class 11 CHAPTER 13 KINETIC THEORY With SOLUTIONSDocument6 pagesPhysics Notes Class 11 CHAPTER 13 KINETIC THEORY With SOLUTIONSSk ShivamNo ratings yet
- Cyber CrimeDocument366 pagesCyber CrimeRufino Gerard MorenoNo ratings yet
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
Uploaded by
Man Tue ThaiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
TOBACCO CESSATION - NRT (Nicotine Replacement Therapy) and Non-NRT
Uploaded by
Man Tue ThaiCopyright:
Available Formats
PREVENTIVE CARE
TOBACCO CESSATION – NRT (Nicotine Replacement Therapy) and Non-NRT
STATEWIDE DRUG THERAPY MANAGEMENT PROTOCOL for the OREGON PHARMACIST
AUTHORITY and PURPOSE: Per ORS 689.645, a pharmacist may provide patient care services
pursuant to a statewide drug therapy management protocol.
Following all elements outlined in OAR 855-020-0110, a pharmacist licensed and located in
Oregon may prescribe individual or multiple Nicotine Replacement Therapy (NRT) OTC and Rx
for tobacco cessation.
Following all elements outlined in OAR 855-020-0110, a pharmacist licensed and located in
Oregon may prescribe non-NRT medications for tobacco cessation.
STANDARDIZED PATIENT ASSESSMENT PROCESS ELEMENTS:
• Utilize the standardized Tobacco Cessation Patient Intake Form (pg. 2-4)
• Utilize the standardized Tobacco Cessation Assessment and Treatment Care Pathway (pg.
5-6)
PHARMACIST TRAINING/EDUCATION:
• Minimum 2 hours of documented ACPE CE related to pharmacist prescribing of tobacco
cessation products
Oregon Board of Pharmacy 1 of 6 v. 06/2021
Tobacco Cessation Self-Screening Patient Intake Form
(CONFIDENTIAL-Protected Health Information)
Date _____/_____/________ Date of Birth _____/_____/________ Age_____
Legal Name______________________________________________ Preferred Name __________________________
Sex Assigned at Birth (circle) M / F Gender Identification (circle) M / F / Other____
Preferred Pronouns (circle) She/Her/Hers, He/Him/His, They/Them/Their, Ze/Hir/Hirs, Other____________
Street Address ____________________________________________________________________________________
Phone ( ) _______________________ Email Address ______________________________________
Healthcare Provider Name _______________________ Phone ( ) ______________ Fax ( ) _______________
Do you have health insurance? Yes / No Insurance Provider Name _____________________________
Any allergies to medications? Yes / No If yes, please list ____________________________________
Any allergies to foods (ex. menthol/soy)? Yes / No If yes, please list ____________________________________
List of medicine(s) you take:___________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Do you have a preferred tobacco cessation product you would like to use?_____________________________________
Have you tried quitting smoking in the past? If so, please describe ___________________________________________
What best describes how you have tried to stop smoking in the past?
“Cold turkey”
Tapering or slowly reducing the number of cigarettes you smoke a day
Medicine
o Nicotine replacement (like patches, gum, inhalers, lozenges, etc.)
o Prescription medications (ex. bupropion [Zyban®, Wellbutrin®], varenicline [Chantix®])
Other___________________________________________
Health and History Screen – Background Information:
1. Are you under 18 years old? □ Yes □ No
2. Are you pregnant, nursing, or planning on getting pregnant or nursing in the next 6 □ Yes □ No □ Not sure
months?
3. Are you currently using and trying to quit non-cigarette products (ex. Chewing tobacco, □ Yes □ No
vaping, e-cigarettes, Juul)?
Medical History:
4. Have you ever had a heart attack, irregular heartbeat or angina, or chest pains in the past □ Yes □ No □ Not sure
two weeks?
5. Do you have stomach ulcers? □ Yes □ No □ Not sure
6. Do you wear dentures or have TMJ (temporomandibular joint disease)? □ Yes □ No □ Not sure
7. Do you have a chronic nasal disorder (ex. nasal polyps, sinusitis, rhinitis)? □ Yes □ No □ Not sure
8. Do you have asthma or another chronic lung disorder (ex. COPD, emphysema, chronic □ Yes □ No □ Not sure
bronchitis)?
Tobacco History:
9. Do you smoke fewer than 10 cigarettes a day? □ Yes □ No
Blood Pressure Reading _____/______ mmHg (*Note: Must be taken by a pharmacist)
Stop here if patient and pharmacist are considering nicotine replacement therapy or blood pressure
is ≥ 160/100 mmHg.
If patient and pharmacist are considering non-nicotine replacement therapy (ex. varenicline or
KEEP
bupropion) and blood pressure is < 160/100mmHg continue to answer the questions below.
GOING
Oregon Board of Pharmacy 2 of 6 v. 06/2021
Tobacco Cessation Self-Screening Patient Intake Form
(CONFIDENTIAL-Protected Health Information)
Medical History Continued:
10. Have you ever had an eating disorder such as anorexia or bulimia? □ Yes □ No □ Not sure
11. Have you ever had a seizure, convulsion, significant head trauma, brain surgery, history □ Yes □ No □ Not sure
of stroke, or a diagnosis of epilepsy?
12. Have you ever been diagnosed with chronic kidney disease? □ Yes □ No □ Not sure
13. Have you ever been diagnosed with liver disease? □ Yes □ No □ Not sure
14. Have you been diagnosed with or treated for a mental health illness in the past 2 years? □ Yes □ No □ Not sure
(ex. depression, anxiety, bipolar disorder, schizophrenia)?
Medication History:
15. Do you take a monoamine oxidase inhibitor (MAOI) antidepressant? □ Yes □ No □ Not sure
(ex. selegiline [Emsam®, Zelapar®], Phenelzine [Nardil®], Isocarboxazid [Marplan®],
Tranylcypromine [Parnate®], Rasagiline [Azilect®])
16. Do you take linezolid? □ Yes □ No □ Not sure
17. Do you use alcohol or have you recently stopped taking sedatives? □ Yes □ No □ Not sure
(ex. Benzodiazepines)
The Patient Health Questionnaire 2 (PHQ 2):
Over the last 2 weeks, how often have you been Not At All Several Days More Than Nearly Every Day
bothered by any of the following problems? Half the Days
Little interest or pleasure in doing things 0 1 2 3
Feeling down, depressed or hopeless 0 1 2 3
Suicide Screening:
Over the last 2 weeks, how often have you had 0 1 2 3
thoughts that you would be better off dead, or
have you hurt yourself or had thoughts of hurting
yourself in some way?
Patient Signature Date
Oregon Board of Pharmacy 3 of 6 v. 06/2021
Tobacco Cessation Assessment & Treatment Care Pathway
STEP 1: Health and History Screen Part 1 No = No Contraindicating Refer to PCP and/or
Yes/Not sure = Contraindicating
Review Tobacco Cessation Patient Conditions. Oregon Quit Line 1-
Conditions. Refer
Questionnaire (Questions 1 -2) Continue to step 2 800-QUIT-NOW
STEP 2: Health and History Screen Part 2 Refer to Oregon Quit Line
Smoking Cigarettes. Yes to question 3 Refer
Review Tobacco Cessation Patient 1-800-QUIT-NOW to receive
Continue to step 3
Questionnaire (Question 3) counseling and NRT
STEP 3: Blood Pressure Screen Refer to PCP AND
BP < 160/100.
Take and document patient’s current blood pressure. (Note: RPh BP > 160/100 Refer Oregon Quit Line
Continue to step 4
may choose to take a second reading if initial is high) 1-800-QUIT-NOW
STEP 4: Medical History Refer to PCP AND
No, to question 4 and 5. Yes, to question
Nicotine Replacement Therapy Refer Oregon Quit Line
Continue to step 5 4 and/or 5
Questions (Questions 4-5) 1-800-QUIT-NOW
STEP 5: Medical History
Nicotine Replacement Therapy Questions (Questions 6-8) If patient wants NRT, prescribe If patient wants bupropion or
Question 6 = if Yes, avoid using nicotine gum NRT* varenicline, continue to step 6.
Question 7 = if Yes, avoid using nicotine nasal spray
Question 8 = if Yes, avoid using nicotine inhaler
Prescribing • Combination NRT is preferred Tobacco History (Question 9 on questionnaire)
NRT*(pg.6): (Nicotine patch + Acute NRT) If Yes to smoking </=10 cigs/day, start with nicotine patch 14mg/day
• Acute NRT = Nicotine gum, Nicotine lozenge, If No to smoking > 10 cigs/day start with nicotine patch 21mg/day
Nicotine nasal spray, Nicotine inhaler
Consider NRT* if yes to any question from 10-14
a) If yes to any question avoid bupropion.
Refer Refer to PCP AND
If patient still wants bupropion, refer.
STEP 6: Medical History Oregon Quit Line
b) If yes to any questions from 12-14 avoid varenicline.
Bupropion and varenicline screening Refer 1-800-QUIT-NOW
If patient still wants varenicline, refer.
Questions 10-14
If patient answered no to questions 10 – 14, continue to step 7.
If patient answered no to questions 12-14, but yes to question 10 and/or
11, AND wants varenicline (but not bupropion), skip to step 8
If patient answered If patient answered yes to any question from Refer to PCP if patient
no to questions 15-17, 15-17 Avoid bupropion. Refer wants bupropion;
STEP 7: Medication History
review depression - Refer if patient still wants bupropion. NRT* can be
Questions 15-17 on questionnaire.
screening step 8. - If patient wants varenicline, continue to considered
depression screening step 8.
STEP 8: The Patient Health Score < 3 on PHQ2. Score > 3 on PHQ. Refer Refer to PCP;
Questionnaire 2 (PHQ 2): Depression Review Suicide Screening in Avoid bupropion and varenicline, refer to NRT* can be
Screening step 9. PCP for treatment. NRT* can be offered. considered
Call PCP office to notify them of
Score of 0 on suicide Refer
positive suicide screening and
screening. Score > 1 on suicide screening.
STEP 9: Suicide Screening determine next steps. After
May prescribe bupropion or Immediate referral to PCP.
hours, refer to suicide hotline
varenicline.
1-800-273-8255
Prescribing Bupropion: Prescribing Varenicline:
150mg SR daily for 3 days then 150mg SR twice daily for 8 weeks or 0.5mg daily for 3 days then 0.5mg twice daily for 4 days then 1mg
longer. Quit day after day 7. twice daily for 12 to 24 weeks. Quit day after day 7 or alternatively
quit date up to 35 days after initiation of varenicline.
Consider combining with Nicotine patch or Nicotine lozenge or
Nicotine gum for increased efficacy.* Generally not used in combination with other smoking cessation
medications as first line therapy.
For patients who do not tolerate titration to the full dose, consider
continuing 150mg once daily as the lower dose has shown efficacy.
Oregon Board of Pharmacy 4 of 6 v. 06/2021
Tobacco Cessation Assessment & Treatment Care Pathway
*Nicotine Replacement Dosing:
Dose
Long Acting NRT
Nicotine Patches • Patients smoking >10 cigarettes/day: begin with 21mg/day for 6 weeks, followed by 14mg/day for 2
weeks, finish with 7mg/day for 2 weeks
• Patients smoking < 10 cigarettes/day: begin with 14mg/day for 6 weeks, followed by 7mg/day for 2
weeks
• Note: Adjustment may be required during initial treatment (move to higher dose if experiencing
withdrawal symptoms; lower dose if side effects are experienced).
Acute NRT
Nicotine Gum • Chew 1 piece of gum when urge to smoke occurs. If strong or frequent cravings are present after 1
piece of gum, may use a second piece within the hour (do not continuously use one piece after the
other).
• Patients who smoke their first cigarette within 30 minutes of waking should use the 4 mg strength;
otherwise the 2 mg strength is recommended.
• Use according to the following 12-week dosing schedule:
o Weeks 1 to 6: Chew 1 piece of gum every 1 to 2 hours (maximum: 24 pieces/day); if using nicotine
gum alone without nicotine patches, to increase chances of quitting, chew at least 9 pieces/day
during the first 6 weeks
o Weeks 7 to 9: Chew 1 piece of gum every 2 to 4 hours (maximum: 24 pieces/day)
o Weeks 10 to 12: Chew 1 piece of gum every 4 to 8 hours (maximum: 24 pieces/day)
Nicotine Lozenges • 1 lozenge when urge to smoke occurs; do not use more than 1 lozenge at a time
• Patients who smoke their first cigarette within 30 minutes of waking should use the 4 mg strength;
otherwise the 2 mg strength is recommended.
• Use according to the following 12-week dosing schedule:
o Weeks 1 to 6: 1 lozenge every 1 to 2 hours (maximum: 5 lozenges every 6 hours; 20 lozenges/day);
if using nicotine lozenges alone without nicotine patches, to increase chances of quitting, use at
least 9 lozenges/day during the first 6 weeks
o Weeks 7 to 9: 1 lozenge every 2 to 4 hours (maximum: 5 lozenges every 6 hours; 20 lozenges/day)
o Weeks 10 to 12: 1 lozenge every 4 to 8 hours (maximum: 5 lozenges every 6 hours; 20
lozenges/day)
Nicotine Inhaler • Initial treatment: 6 to 16 cartridges/day for up to 12 weeks; maximum: 16 cartridges/day
• Use beyond 6 months is not recommended (has not been studied). If patient is unable to stop smoking
by the fourth week of therapy, consider discontinuation.
• Discontinuation of therapy: After initial treatment, gradually reduce daily dose over 6 to 12 weeks.
Some patients may not require gradual reduction of dosage and may stop treatment abruptly.
Nicotine Nasal Spray • Initial: 1 to 2 doses/hour (each dose [2 sprays, one in each nostril] contains 1 mg of nicotine)
• Adjust dose as needed based on patient response; do not exceed more than 5 doses (10 sprays) per
hour [maximum: 40 mg/day (80 sprays)] or 3 months of treatment
• If using nicotine nasal spray alone without nicotine patches, for best results, use at least the
recommended minimum of 8 doses per day (less is likely to be effective).
• Use beyond 6 months is not recommended (has not been studied). If patient is unable to stop smoking
by the fourth week of therapy, consider discontinuation.
• Discontinuation of therapy: Discontinue over 4 to 6 weeks. Some patients may not require gradual
reduction of dosage and may stop treatment abruptly.
Oregon licensed pharmacist must adhere to Prescribing Parameters, when issuing any prescription for tobacco cessation.
PRESCRIBING PARAMETERS:
• 1st prescription up to 30 days
• Maximum duration = 12 weeks
• Maximum frequency = 2x in a rolling 12-month period
TREATMENT CARE PLAN:
• Documented follow-up: within 7-21 days, phone consultation permitted
Oregon Board of Pharmacy v. 06/2021
5 of 6
Tobacco Cessation Prescription
Optional-May be used by pharmacy if desired
Patient Name: Date of birth:
Address:
City/State/Zip Code: Phone number:
Verified DOB with valid photo ID
Referred patient to Oregon Quit Line (1-800-QUIT-NOW or www.quitnow.net/oregon)
BP Reading: ____/____ mmHg *must be taken by a RPh
Note: RPh must refer patient if blood pressure > 160/100
Rx
Written Date:
Prescriber Name: Prescriber Signature:
Pharmacy Address: Pharmacy Phone:
-or-
Patient Referred
Notes:__________________________________________________________________
_______________________________________________________________________
_______________________________________________________________________
_______________________________________________________________________
_______________________________________________________________________
Oregon Board of Pharmacy v. 06/2021
6 of 6
You might also like
- Raheel OSCE Notes January 2023Document453 pagesRaheel OSCE Notes January 2023KamleshKumar100% (2)
- Varicocele Secrets: The Underground Solution for Getting Rid of Varicocele for The Rest of Your Life [EN]From EverandVaricocele Secrets: The Underground Solution for Getting Rid of Varicocele for The Rest of Your Life [EN]No ratings yet
- CrackTheNac 8 Case For The NAC OSCEDocument19 pagesCrackTheNac 8 Case For The NAC OSCEEmad Mergan100% (6)
- Station 5 Example ScenariosDocument12 pagesStation 5 Example ScenariosDavidJohnsonNo ratings yet
- Medical Evaluation Form 2022Document2 pagesMedical Evaluation Form 2022jimmy p. lamhi50% (2)
- Step 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionFrom EverandStep 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionNo ratings yet
- 2 CA - Health Profile - 2014-12-19 PDFDocument9 pages2 CA - Health Profile - 2014-12-19 PDFLiamNo ratings yet
- Health Unit Coordinator CoursesDocument13 pagesHealth Unit Coordinator CoursesMan Tue ThaiNo ratings yet
- PFT Medical Evaluation Form 1Document3 pagesPFT Medical Evaluation Form 1Dexter VenguaNo ratings yet
- Template - 2020 PAR-QDocument9 pagesTemplate - 2020 PAR-QJairo OntongNo ratings yet
- Pharmacotherapeutics Soft Copy DIIDocument95 pagesPharmacotherapeutics Soft Copy DIILiyakath AliNo ratings yet
- Detoxification Questionnaire: I. Medical Symptoms Questionnaire (MSQ)Document2 pagesDetoxification Questionnaire: I. Medical Symptoms Questionnaire (MSQ)ddddNo ratings yet
- Family Medicine - General Practice MEQ 2006Document6 pagesFamily Medicine - General Practice MEQ 2006jermie22100% (1)
- 11mastering Medical Long CaseDocument42 pages11mastering Medical Long CaseAthirahRaraNo ratings yet
- January2020PARQPlusFillable 1Document6 pagesJanuary2020PARQPlusFillable 1ssamyang92No ratings yet
- Pharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordDocument20 pagesPharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordNurwahidah Moh WahiNo ratings yet
- All CasesDocument32 pagesAll CasesMona NasrNo ratings yet
- ParQ Plus Jan 2023Document6 pagesParQ Plus Jan 2023troy montarilNo ratings yet
- Par QPlus 2022Document7 pagesPar QPlus 2022MARIKA BALONDONo ratings yet
- Opening The Consultation: Ideas, Concerns and Expectations (ICE)Document8 pagesOpening The Consultation: Ideas, Concerns and Expectations (ICE)Toria053No ratings yet
- ParQ Plus Jan 2022 FillableDocument5 pagesParQ Plus Jan 2022 FillableRaechelle DizonNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneJacquelynne Amba100% (1)
- Drug Study MedicineDocument24 pagesDrug Study MedicineLutzie PagulaNo ratings yet
- SkinDocument6 pagesSkinKrishna Faith P. DelaraNo ratings yet
- Physical Health CheckDocument9 pagesPhysical Health CheckDivya ThanlaeNo ratings yet
- LMCC II GuideDocument79 pagesLMCC II GuideSoleil DaddouNo ratings yet
- Parqplus 2020Document6 pagesParqplus 2020klinikcitrautamapalembangNo ratings yet
- At the Precipice: My Three-Year Journey from Stroke to Good Health with Type 2 DiabetesFrom EverandAt the Precipice: My Three-Year Journey from Stroke to Good Health with Type 2 DiabetesNo ratings yet
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Document49 pagesLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNo ratings yet
- Reading Test - 3 Clinical Depression Text ADocument17 pagesReading Test - 3 Clinical Depression Text AJisha JanardhanNo ratings yet
- The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesThe Physical Activity Readiness Questionnaire For EveryoneFrances RedNo ratings yet
- P Drugs - Personal Drugs For PatientsDocument30 pagesP Drugs - Personal Drugs For Patientsjco jac100% (1)
- Personal Health AssessmentDocument8 pagesPersonal Health AssessmenthelloNo ratings yet
- Coumadin Dosing GuideDocument3 pagesCoumadin Dosing Guidemorale28No ratings yet
- Multitable New Patient FormDocument8 pagesMultitable New Patient Forme-MedTools100% (9)
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- PatientDocument9 pagesPatientkcquitorianoNo ratings yet
- Soap FormsDocument6 pagesSoap FormsJunJieNo ratings yet
- Pharmaceutical Care Plan IIIDocument20 pagesPharmaceutical Care Plan IIIAdemilola AdekoyaNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument6 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneArnel Bagalawis100% (1)
- PAR-Q+: Oo Oo Oo OoDocument6 pagesPAR-Q+: Oo Oo Oo OoRoxyNo ratings yet
- Pre Employment Medical - Declaration - HMCL DOCTORSDocument2 pagesPre Employment Medical - Declaration - HMCL DOCTORSabhishek vermaNo ratings yet
- Self Report MedicationDocument3 pagesSelf Report MedicationMarjhun Flores GuingayanNo ratings yet
- Advance Care or Health Directive. July 2013: With YOUTUBE VIDEODocument2 pagesAdvance Care or Health Directive. July 2013: With YOUTUBE VIDEODr Jerome MellorNo ratings yet
- PFT Form 2023Document2 pagesPFT Form 2023Custodial Facility Pasig CPSNo ratings yet
- Pharmacy CounsellingDocument8 pagesPharmacy CounsellingChrissieNo ratings yet
- General Health Questions: The Physical Activity Readiness Questionnaire For EveryoneDocument4 pagesGeneral Health Questions: The Physical Activity Readiness Questionnaire For EveryoneLenard PagsisihanNo ratings yet
- 1992-1997 and 2004 Questions and AnswersDocument56 pages1992-1997 and 2004 Questions and AnswersEmad MerganNo ratings yet
- Dominic Pathfit 1&2Document6 pagesDominic Pathfit 1&2Milbert Patun-ogNo ratings yet
- Botulism Toolkit: Emergency Recognition, Response and Anti Terrorism Training Associates (ERRATA, LLC.)Document18 pagesBotulism Toolkit: Emergency Recognition, Response and Anti Terrorism Training Associates (ERRATA, LLC.)Joko YantoNo ratings yet
- Groups ABCD - Family Medicine End Block QuestionsDocument10 pagesGroups ABCD - Family Medicine End Block QuestionsHisham ChomanyNo ratings yet
- FMcase 2Document27 pagesFMcase 2Ryan Townsend100% (3)
- CPS2 MED20 Scenario 1Document7 pagesCPS2 MED20 Scenario 1mNo ratings yet
- Clinical Document 1Document7 pagesClinical Document 1api-253709303No ratings yet
- Patient Education PlanDocument4 pagesPatient Education Planapi-248022066No ratings yet
- 2021 Revalida - Adult IMDocument11 pages2021 Revalida - Adult IMJv MataNo ratings yet
- Use of Antibiotics For Respiratory Tract Infections in Adults and ChildrenDocument7 pagesUse of Antibiotics For Respiratory Tract Infections in Adults and Childrendokter Hewan AdhonaNo ratings yet
- Measure Blood Pressure Accurately. Healthy Living Solutions Book 3 (for Professionals)From EverandMeasure Blood Pressure Accurately. Healthy Living Solutions Book 3 (for Professionals)Rating: 4 out of 5 stars4/5 (1)
- Staying Alive: The Signs That You Have to See a Doctor Right Now (and the Ways to Avoid Having to See One Again)From EverandStaying Alive: The Signs That You Have to See a Doctor Right Now (and the Ways to Avoid Having to See One Again)No ratings yet
- 2022 Oregon EITC NoticeDocument1 page2022 Oregon EITC NoticeMan Tue ThaiNo ratings yet
- PTO PolicyDocument5 pagesPTO PolicyMan Tue Thai100% (1)
- Mat Act Fact Sheet 117thDocument1 pageMat Act Fact Sheet 117thMan Tue ThaiNo ratings yet
- PA Prescription Requirements 12 18Document8 pagesPA Prescription Requirements 12 18Man Tue ThaiNo ratings yet
- Downtown STREETCAR MapDocument1 pageDowntown STREETCAR MapMan Tue ThaiNo ratings yet
- DumplingWeek 2023 PassportDocument1 pageDumplingWeek 2023 PassportMan Tue ThaiNo ratings yet
- K-ETA FAQ - (Eng)Document9 pagesK-ETA FAQ - (Eng)Man Tue ThaiNo ratings yet
- 2005 National Future Stars Developmental TeamDocument3 pages2005 National Future Stars Developmental TeamMan Tue ThaiNo ratings yet
- Wellness DiscountDocument1 pageWellness DiscountMan Tue ThaiNo ratings yet
- Micronutrients Assignment-14th EdDocument3 pagesMicronutrients Assignment-14th EdMan Tue ThaiNo ratings yet
- Spring 2016: Mon Tues Wed Thu FriDocument2 pagesSpring 2016: Mon Tues Wed Thu FriMan Tue ThaiNo ratings yet
- Associate Cover LetterDocument2 pagesAssociate Cover LetterMan Tue ThaiNo ratings yet
- The Crucial Acquisition of KnowledgeDocument5 pagesThe Crucial Acquisition of KnowledgeMan Tue ThaiNo ratings yet
- Fundamentals of Visualization With TableauDocument1 pageFundamentals of Visualization With TableauMan Tue ThaiNo ratings yet
- MT ThesisDocument19 pagesMT ThesisMan Tue ThaiNo ratings yet
- GraduationChecklist 003Document1 pageGraduationChecklist 003Man Tue ThaiNo ratings yet
- Eng/Npd Girish Comprehen Sive Charan Marketing: Internal Quality Audit Schedule No:Qms Ia-1Document1 pageEng/Npd Girish Comprehen Sive Charan Marketing: Internal Quality Audit Schedule No:Qms Ia-1DhinakaranNo ratings yet
- Migrating and Installing Avaya Appliance Virtualization PlatformDocument68 pagesMigrating and Installing Avaya Appliance Virtualization PlatformSathish RajanNo ratings yet
- MBA Course StructureDocument2 pagesMBA Course StructureAnupama JampaniNo ratings yet
- Math 8 Q3 Module 5 With Answer KeyDocument13 pagesMath 8 Q3 Module 5 With Answer KeyJimcris villamorNo ratings yet
- Electrical Engineering Software PDFDocument12 pagesElectrical Engineering Software PDFAkd Deshmukh50% (2)
- Plants and Animals Live Together Lesson PlanDocument3 pagesPlants and Animals Live Together Lesson Planapi-374921894No ratings yet
- Fundamentals of Thermal Sensors: Thu HuynhDocument39 pagesFundamentals of Thermal Sensors: Thu HuynhsamcaridoNo ratings yet
- Experiment 7: Investigating The Change of Volume in The Change of Temperature (Document2 pagesExperiment 7: Investigating The Change of Volume in The Change of Temperature (EDWIN SIMBARASHE MASUNUNGURENo ratings yet
- Ongc V Saw PipesDocument9 pagesOngc V Saw PipesManisha SinghNo ratings yet
- HT Motors Data SheetDocument3 pagesHT Motors Data SheetSE ESTNo ratings yet
- Normalized Impedance and Admittance Coordinates: Name Title Dwg. NoDocument1 pageNormalized Impedance and Admittance Coordinates: Name Title Dwg. NoJayeng WidiatmokoNo ratings yet
- Final Report: Simulation Using Star CCM+ Theory and Practice in Marine CFD BenaoeDocument10 pagesFinal Report: Simulation Using Star CCM+ Theory and Practice in Marine CFD BenaoeRaviindra singhNo ratings yet
- 2012 GR 7 Maths PDFDocument8 pages2012 GR 7 Maths PDFmarshy bindaNo ratings yet
- Değişim Sınavı 2020Document29 pagesDeğişim Sınavı 2020Mustafa CinNo ratings yet
- MRD Carotid StentDocument5 pagesMRD Carotid StentKhushboo WarhadeNo ratings yet
- 11thsamplebooklet PDFDocument200 pages11thsamplebooklet PDFSoumyodeep ChowdhuryNo ratings yet
- S17.s1 - Final Project - Inglés 3 - MANUEL LAURA MAMANIDocument3 pagesS17.s1 - Final Project - Inglés 3 - MANUEL LAURA MAMANIManuel Sebastian Laura MamaniNo ratings yet
- R1600H Sistema ImplementosDocument31 pagesR1600H Sistema ImplementosLuis Angel Pablo Juan de Dios100% (1)
- Digital NativesDocument10 pagesDigital NativesJonathan Blanco Sa RiyadhNo ratings yet
- Solucionario Ingenieria en Control Moderna OGATADocument240 pagesSolucionario Ingenieria en Control Moderna OGATAanandpj444471% (7)
- FMCG Organisation Chart: Board of DirectorsDocument1 pageFMCG Organisation Chart: Board of DirectorsKumar Panchal0% (1)
- Jadual BerkalaDocument2 pagesJadual BerkalaRohani Yusof75% (4)
- CMP 1 1 CDPDocument11 pagesCMP 1 1 CDPSachin NakadeNo ratings yet
- Philippine Notices To MarinersDocument42 pagesPhilippine Notices To MarinersTaneo Prince CalebNo ratings yet
- Name of Customer - Name of Project - TE-112045 - WFC - Print - OutDocument1 pageName of Customer - Name of Project - TE-112045 - WFC - Print - OutJavier EspinosaNo ratings yet
- Heat Exchanger Design CHE 311 Final Project MSUDocument15 pagesHeat Exchanger Design CHE 311 Final Project MSUnefoussiNo ratings yet
- 2018 Trial 1 Biology Questions and Marking SchemeDocument11 pages2018 Trial 1 Biology Questions and Marking SchemeKodhekNo ratings yet
- Beyond Locative Media - Mark Tuters and Kazys VarnelisDocument6 pagesBeyond Locative Media - Mark Tuters and Kazys VarnelisEduardoNo ratings yet
- Physics Notes Class 11 CHAPTER 13 KINETIC THEORY With SOLUTIONSDocument6 pagesPhysics Notes Class 11 CHAPTER 13 KINETIC THEORY With SOLUTIONSSk ShivamNo ratings yet
- Cyber CrimeDocument366 pagesCyber CrimeRufino Gerard MorenoNo ratings yet

![Varicocele Secrets: The Underground Solution for Getting Rid of Varicocele for The Rest of Your Life [EN]](https://imgv2-2-f.scribdassets.com/img/word_document/544312715/149x198/dc87e19c66/1645158464?v=1)