Professional Documents
Culture Documents
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Uploaded by
MugiCopyright:
Available Formats
You might also like
- Advanced Smoking Cessation Hypnosis ScriptDocument16 pagesAdvanced Smoking Cessation Hypnosis ScriptShane Fozard94% (17)
- Material: RRC Revision GuideDocument17 pagesMaterial: RRC Revision Guidesheren zamanNo ratings yet
- Healing Through ArchitectureDocument10 pagesHealing Through ArchitectureSakshi DeshmukhNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationGowriNo ratings yet
- Felix2012 4Document6 pagesFelix2012 4rajesh kumarNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerGowriNo ratings yet
- A Patient With Dry Mouth PDFDocument6 pagesA Patient With Dry Mouth PDFWahdatNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionernavyaNo ratings yet
- Dry Mouth-1Document3 pagesDry Mouth-1channadrasmaNo ratings yet
- 53 Article XerosDocument5 pages53 Article XerosNivehthaa VisvamNo ratings yet
- عرض تقديمي من Microsoft PowerPoint جديدDocument10 pagesعرض تقديمي من Microsoft PowerPoint جديدHard TubeNo ratings yet
- Salivary Gland ComplaintsDocument9 pagesSalivary Gland ComplaintsGowriNo ratings yet
- University of Jordan Dentistry 2016: Ibrahim ShawaqfehDocument21 pagesUniversity of Jordan Dentistry 2016: Ibrahim ShawaqfehHanin AbukhiaraNo ratings yet
- Oral Manifestations of Nuritional Diseases in Children1Document5 pagesOral Manifestations of Nuritional Diseases in Children1andrada67No ratings yet
- Clinical Review: Oral Malodour (Halitosis)Document4 pagesClinical Review: Oral Malodour (Halitosis)Maghfira TiechaNo ratings yet
- Salivary Gland DiseaseDocument63 pagesSalivary Gland DiseaseAnchal RainaNo ratings yet
- Vpatho Module 1Document54 pagesVpatho Module 1Lib PalmaresNo ratings yet
- Tongue Diseases NDocument46 pagesTongue Diseases NhazeemmegahedNo ratings yet
- Endocrine DiseaseDocument27 pagesEndocrine Diseasesilentroar1427No ratings yet
- Oral Manifestations of Systemic Disease: Autoimmune DiseasesDocument7 pagesOral Manifestations of Systemic Disease: Autoimmune DiseaseshussainNo ratings yet
- Dry Mouth (Xerostomia)Document18 pagesDry Mouth (Xerostomia)dr_jamal1983No ratings yet
- Saliva DiseaseDocument8 pagesSaliva DiseaseJemuel Bucud LagartoNo ratings yet
- Ilovepdf MergedDocument7 pagesIlovepdf MergedNoval BalanceNo ratings yet
- Xerostomia: Oedijani-Santoso Bagian/SMF Gigi Dan Mulut FK Undip/RSUP DR Kariadi SemarangDocument40 pagesXerostomia: Oedijani-Santoso Bagian/SMF Gigi Dan Mulut FK Undip/RSUP DR Kariadi SemarangRizal Saeful DrajatNo ratings yet
- Xerostomia in Geriatric Patients: A Burgeoning Global ConcernDocument8 pagesXerostomia in Geriatric Patients: A Burgeoning Global ConcernwhiezardNo ratings yet
- 560-Article Text-1066-1-10-20171231 PDFDocument6 pages560-Article Text-1066-1-10-20171231 PDFKrupali JainNo ratings yet
- Oral, Git, Billiary ConditionsDocument107 pagesOral, Git, Billiary ConditionsNathaniel Mbiu TimNo ratings yet
- Article2 CitatDocument7 pagesArticle2 CitatMunteanu DragosNo ratings yet
- Screenshot 2022-09-20 at 8.37.00 AMDocument1 pageScreenshot 2022-09-20 at 8.37.00 AMjvvistopptxNo ratings yet
- Dry Mouth EngDocument25 pagesDry Mouth EngJelena BlagojevicNo ratings yet
- Xerostomia Clinical Aspects and TreatmentDocument14 pagesXerostomia Clinical Aspects and TreatmentThanh Điền LưuNo ratings yet
- Patology of LinguaDocument37 pagesPatology of LinguaVlad ScutelnicNo ratings yet
- Oral Medicine Journal Reading (Complete)Document29 pagesOral Medicine Journal Reading (Complete)Gabriel LowNo ratings yet
- Pediatric Oral Manifestation of Sustemic DiseaseDocument43 pagesPediatric Oral Manifestation of Sustemic DiseaseMike SihombingNo ratings yet
- Gastrointestinal Conditions Related To Tooth Wear: GeneralDocument4 pagesGastrointestinal Conditions Related To Tooth Wear: Generalfdeetny webassNo ratings yet
- DentalDocument8 pagesDentalHan Bich NguyenNo ratings yet
- Name: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentDocument4 pagesName: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentnadiaNo ratings yet
- Dental Erosion and The Role of Saliva: A Systematic ReviewDocument10 pagesDental Erosion and The Role of Saliva: A Systematic Reviewjperico99No ratings yet
- Oral Malodor: by - DR Monisha Kaushik 2Nd Yr MdsDocument55 pagesOral Malodor: by - DR Monisha Kaushik 2Nd Yr Mdsmonishakaus24No ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument63 pagesOral Medicine - Update For The Dental PractitionerPhuong MaiphuongNo ratings yet
- Oral Frictional HyperkeratosisDocument15 pagesOral Frictional HyperkeratosisFajarRahmantiyoNo ratings yet
- Xerostomia (Also Termed Dry Mouth: Xero-StomDocument6 pagesXerostomia (Also Termed Dry Mouth: Xero-Stomnazirrasheed123No ratings yet
- Oral Medicine - Update For The Dental Practitioner Lumps and SwellingsDocument9 pagesOral Medicine - Update For The Dental Practitioner Lumps and SwellingsGowriNo ratings yet
- 55 Diagnosis, Prevention and Management of Dental ErosionDocument29 pages55 Diagnosis, Prevention and Management of Dental Erosionraed ibrahimNo ratings yet
- Diagnosing, Managing, and Preventing Salivary Gland DisordersDocument13 pagesDiagnosing, Managing, and Preventing Salivary Gland DisordersGil JagudaevNo ratings yet
- Xerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganDocument8 pagesXerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganJonathan JojoNo ratings yet
- Oral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsDocument7 pagesOral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsKaty LunaNo ratings yet
- Diseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutDocument17 pagesDiseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutAli H. Sadiek أ.د. علي حسن صديق100% (4)
- Factors Which Complicate Impression Making PDFDocument18 pagesFactors Which Complicate Impression Making PDFMostafa FayadNo ratings yet
- Présentation 3Document13 pagesPrésentation 3Nador AbdennourNo ratings yet
- Awareness of Oral Manifestations Related To Systemic DiseasesDocument5 pagesAwareness of Oral Manifestations Related To Systemic DiseasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Management of Patients With Oral and Esophageal DisordersDocument81 pagesManagement of Patients With Oral and Esophageal DisordersEdmond ChanNo ratings yet
- Oral Submucous FibrosisDocument18 pagesOral Submucous FibrosisDrVaibhav ShrivastavaNo ratings yet
- Oral Submucous Fibrosis - An UpdateDocument90 pagesOral Submucous Fibrosis - An UpdateMugdha FrancisNo ratings yet
- Mohammed 2014Document7 pagesMohammed 2014Larasati RamadianiNo ratings yet
- Feline Oral DiseasesDocument6 pagesFeline Oral DiseasesBogdan PopaNo ratings yet
- A Simple Guide to Bad Breath and Mouth DiseasesFrom EverandA Simple Guide to Bad Breath and Mouth DiseasesRating: 5 out of 5 stars5/5 (3)
- Dryness of Mouth, (Xerostomia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDryness of Mouth, (Xerostomia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Mouth Ulcers of More Serious ConnotationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Mouth Ulcers of More Serious ConnotationMugiNo ratings yet
- Frequently Asked Questionsin Composite Restorative DentistryDocument7 pagesFrequently Asked Questionsin Composite Restorative DentistryMugi100% (1)
- Short Notes AssignmentDocument2 pagesShort Notes AssignmentMugiNo ratings yet
- What The Causative Agent Pneumonia and Microscopic Apperance?Document8 pagesWhat The Causative Agent Pneumonia and Microscopic Apperance?MugiNo ratings yet
- Tutorial 2 Microbe No.13Document1 pageTutorial 2 Microbe No.13MugiNo ratings yet
- Link For VideosDocument1 pageLink For VideosMugiNo ratings yet
- S. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusDocument14 pagesS. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusMugiNo ratings yet
- PRESBIKUSISDocument37 pagesPRESBIKUSISVenny SarumpaetNo ratings yet
- Jurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita MariniDocument7 pagesJurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita Marinihepi nopita sariNo ratings yet
- Teenage PregnancyDocument5 pagesTeenage PregnancyDavid VenturaNo ratings yet
- Walsh The Bermuda Triangle of Autism PDFDocument6 pagesWalsh The Bermuda Triangle of Autism PDFAnupamaNo ratings yet
- Advance Project Final FeasibilityDocument31 pagesAdvance Project Final FeasibilityMohammad Adil ChoudharyNo ratings yet
- Klinefelter SyndromeDocument3 pagesKlinefelter SyndromeKylalerrsssNo ratings yet
- Asia Healthcare Week Main Stage 2024 Overview Skeletal agendaxzQz4oYRaNicu1j6xlahru87z2tk1nrEBwFCR0xBDocument7 pagesAsia Healthcare Week Main Stage 2024 Overview Skeletal agendaxzQz4oYRaNicu1j6xlahru87z2tk1nrEBwFCR0xBjuliettekhooNo ratings yet
- PMDC Past Exam Qbank Step-2 by Dr. Asif KhanDocument80 pagesPMDC Past Exam Qbank Step-2 by Dr. Asif KhanrimshaafshenNo ratings yet
- Medical College Choices 08 NovDocument1 pageMedical College Choices 08 NovamitNo ratings yet
- Disseminated Intravascular CoagulationDocument3 pagesDisseminated Intravascular CoagulationArlan Abragan100% (1)
- Communication Skills in Nursing PDFDocument2 pagesCommunication Skills in Nursing PDFJennifer25% (4)
- A Management Algorithm For Esophageal PerforationDocument4 pagesA Management Algorithm For Esophageal Perforationoscar chirinosNo ratings yet
- AssignmentDocument4 pagesAssignmentMuhammad Moeez WaheedNo ratings yet
- Bag TechniqueDocument5 pagesBag Techniqueamp_raphNo ratings yet
- Yseali Younified 2020 A Guide To Planning A Community Service ActivityDocument17 pagesYseali Younified 2020 A Guide To Planning A Community Service ActivityHamidatun NisaNo ratings yet
- Health ICT Master PlanDocument6 pagesHealth ICT Master Planaboix253No ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet
- Communiqué Émis Par La PSCDocument4 pagesCommuniqué Émis Par La PSCL'express MauriceNo ratings yet
- Urine Screening For Metabolic Disorders PDFDocument5 pagesUrine Screening For Metabolic Disorders PDFJustine Nicole Clavel LachicaNo ratings yet
- Bhs Inggris 9Document19 pagesBhs Inggris 9ieki aiainNo ratings yet
- Critical Appraisal Nurse Staffing and Inpatient Hospital MortalityDocument42 pagesCritical Appraisal Nurse Staffing and Inpatient Hospital Mortalitykristina dewiNo ratings yet
- HX and PX Obstetrics and GynecologyDocument21 pagesHX and PX Obstetrics and GynecologyTadesse MuhammedNo ratings yet
- Ramadan and DiabetesDocument14 pagesRamadan and DiabetesDitoLinggoNo ratings yet
- 19 Disaster SurgeryDocument45 pages19 Disaster SurgeryAhmed noor Ahmed noorNo ratings yet
- Seed HealthTestingDocument9 pagesSeed HealthTestingMd. Sajjad HossenNo ratings yet
- AIDS Foundation of Chicago - Annual Report 2015Document24 pagesAIDS Foundation of Chicago - Annual Report 2015AdamAce VelasquezNo ratings yet
- Asian Pacific ScientistsDocument28 pagesAsian Pacific ScientistsMahmood SanglayNo ratings yet
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Uploaded by
MugiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of Salivation
Uploaded by
MugiCopyright:
Available Formats
7p423-427.
qxd 26/09/2005 11:05 Page 423
3
IN BRIEF
• Most cases of dry mouth are caused by inadequate fluid intake, or by excess fluid
loss — for example in diabetes.
• Drugs are a common cause of hyposalivation.
• Hyposalivation also follows irradiation but some systemic diseases may present in this way.
Oral Medicine — Update for the dental practitioner.
Dry mouth and disorders of salivation
C. Scully1 and D. H. Felix2
This series provides an overview of current thinking in the more relevant areas of oral medicine for primary care practitioners,
written by the authors while they were holding the Presidencies of the European Association for Oral Medicine and the British
Society for Oral Medicine, respectively. A book containing additional material will be published. The series gives the detail
necessary to assist the primary dental clinical team caring for patients with oral complaints that may be seen in general dental
practice. Space precludes inclusion of illustrations of uncommon or rare disorders, or discussion of disorders affecting the hard
tissues. Approaching the subject mainly by the symptomatic approach — as it largely relates to the presenting complaint — was
considered to be a more helpful approach for GDPs rather than taking a diagnostic category approach. The clinical aspects of the
relevant disorders are discussed, including a brief overview of the aetiology, detail on the clinical features and how the diagnosis
is made. Guidance on management and when to refer is also provided, along with relevant websites which offer further detail.
ORAL MEDICINE Saliva is essential to oral health. The most obvi- • Reduced salivary flow (hyposalivation)
1. Aphthous and other ous and important function of saliva is in eat- and/or
common ulcers ing, for taste and to lubricate food and protect • Changed salivary composition.
2. Mouth ulcers of more the mucosa and teeth. The water, mucins and
serious connotation proline-rich glycoproteins lubricate food and Patients who have chronically decreased sali-
3. Dry mouth and disorders help swallowing, and saliva is essential for nor- vary flow (hyposalivation) suffer from lack of
of salivation mal taste perception. Saliva is protective via the oral lubrication, affecting many functions, and
4. Oral malodour washing action, via various antimicrobial com- they may complain of dryness (xerostomia), and
ponents such as mucin, histatins, lysozyme and can develop dental caries and other infections
5. Oral white patches
lactoferrin, and via specific antibodies to a (candidosis, or acute bacterial sialadenitis) as a
6. Oral red and range of micro-organisms that the host has consequence of the reduced defences.
hyperpigmented patches encountered.
7. Orofacial sensation and Salivary gland secretion from the major Causes
movement (parotid, submandibular and sublingual) and There are physiological causes of hyposaliva-
8. Orofacial swellings and minor glands (multiple mucous glands scattered tion. Thus a dry mouth is common during peri-
lumps throughout the mouth — especially the lips and ods of anxiety, due to sympathetic activity;
9. Oral cancer soft palate) is mainly under neural control, under mouthbreathers may also have a dry mouth
10. Orofacial pain the influence of the autonomic nervous system, and advancing age is associated with dry
although various hormones may also modulate
its composition. In general, parasympathetic Table 1 Causes of dry mouth
1*Professor, Consultant, Dean, Eastman
stimulation increases salivation, while sympa- Iatrogenic
Dental Institute for Oral Health Care
Sciences, 256 Gray’s Inn Road, UCL,
thetic stimulation produces more viscous saliva Drugs
University of London, London WC1X 8LD; and therefore appears to depress salivation.
2Consultant, Senior Lecturer, Glasgow Irradiation
Thus, in acute anxiety, when there is sympa-
Dental Hospital and School, 378 Graft versus host disease
thetic stimulation, the mouth feels dry. The
Sauchiehall Street, Glasgow G2 3JZ /
Associate Dean for Postgraduate Dental mouth is also dry if the parasympathetic system
Education, NHS Education for Scotland, is inhibited by, for example, various drugs. Any- Disease
2nd Floor, Hanover Buildings, 66 Rose thing that damages the glands, or reduces body Dehydration
Street, Edinburgh EH2 2NN Psychogenic
*Correspondence to: Professor Crispian
fluids can also reduce salivation.
Scully CBE Salivary gland disease
Email: c.scully@eastman.ucl.ac.uk DRY MOUTH (XEROSTOMIA) Sjögren’s syndrome
Dry mouth (xerostomia) is a complaint that is the Sarcoidosis
Refereed Paper
© British Dental Journal 2005; 199: most common salivary problem and is the sub- Salivary aplasia
423–427 jective sense of dryness which may be due to:
BRITISH DENTAL JOURNAL VOLUME 199 NO. 7 OCT 8 2005 423
7p423-427.qxd 26/09/2005 11:11 Page 424
PRACTICE
mouth probably because of a reduction of sali- and neck region, such as oral cancer, can
vary acini, with a fall in salivary secretory produce profound xerostomia. Other sources of
reserve. irradiation such as radioactive iodine (131I) used
Very rarely, children are born missing sali- for treating thyroid disease, may also damage
vary glands — so-called salivary gland aplasia or the salivary glands, which take up the
agenesis. Most salivary gland dysfunction how- radioactive iodine.
ever is acquired (Table 1).
Drugs, in most older people complaining of Dehydration, as in diabetes mellitus, chronic
xerostomia, are the cause. Indeed, the main renal failure, hyperparathyroidism, any fever
causes of dry mouth are iatrogenic. There is or diabetes insipidus can cause xerostomia.
usually a fairly close temporal relationship
between starting the drug treatment or Diseases of salivary glands can also cause
increasing the dose, and experiencing the dry salivary dysfunction. These are mainly Sjögren’s
mouth. However, the reason for which the syndrome (a multisystem auto-immune
drug is being taken may also be important. For condition discussed below); sarcoidosis; HIV
example, patients with anxiety or depressive disease; hepatitis C virus infection; liver
conditions may complain of dry mouth even diseases; and cystic fibrosis (mucoviscidosis)
in the absence of drug therapy (or evidence of (Fig. 1).
reduced salivary flow). Finally, it is important to also recognise that
Drugs recognised as causes of reduced sali- some patients complaining of a dry mouth have
vation include mainly those with anticholiner- no evidence of a reduced salivary flow or a sali-
gic, or sympathomimetic, or diuretic activity. vary disorder (ie they have xerostomia but not
These include those shown in Table 2. hyposalivation), and in these there may be a
Irradiation for malignant tumours in the head psychogenic reason for the complaint.
Table 2 Drugs associated with dry mouth Clinical features
The patient with hyposalivation may have
Drugs which directly damage the salivary glands difficulty in:
Cytotoxic drugs • Swallowing — especially dry foods such as
Drugs with anticholinergic activity biscuits (the cracker sign)
Anticholinergic agents such as atropine, atropinics and • Controlling dentures
hyoscine • Speaking, as the tongue tends to stick to the
Antireflux agents eg proton-pump inhibitors (such as palate — leading to ‘clicking’ speech.
omeprazole)
Psychoactive agents with anticholinergic activities such as: Patients may also complain of unpleasant
Antidepressants, including tricyclic (eg amitriptyline, taste or loss of sense of taste, or halitosis.
nortriptyline, clomipramine and dothiepin [dosulepin]),
selective serotonin re-uptake inhibitors (eg fluoxetine),
The patient with hyposalivation may com-
lithium and others. plain of a dry mouth or these sequelae alone, or
Phenothiazines also complain of dryness of the eyes and other
Benzodiazepines
mucosae (nasal, laryngeal, genital). Those with
eye complaints have blurring, light intolerance,
Opioids
burning, itching or grittiness, and sometimes an
Antihistamines
inability to cry.
Bupropion
Systemic features (such as joint pains) may be
Drugs acting on sympathetic system suggestive of Sjögren’s syndrome.
Drugs with sympathomimetic activity eg ephedrine Examination may reveal that the lips adhere
Antihypertensives; alpha 1 antagonists (e.g. terazosin and one to another and an examining dental mirror
prazosin) and alpha 2 agonists (e.g. clonidine) may reduce may stick to the mucosa because of the reduced
salivary flow. Beta blockers (e.g. atenolol, propranolol) also
change salivary protein levels. lubrication. Lipstick or food debris may be seen
Drugs which deplete fluid
sticking to the teeth or soft tissues, and the usual
pooling of saliva in the floor of the mouth may
Diuretics
be absent. Thin lines of frothy saliva may form
along lines of contact of the oral soft tissues, on
the tongue, or in the vestibule. Saliva may not be
expressible from the parotid ducts. The tongue is
dry (Fig. 2) and may become characteristically
lobulated and usually red, with partial or com-
plete depapillation (Fig. 3).
Complications of hyposalivation can include:
• Dental caries — which tends to involve
smooth surfaces and areas otherwise not
very prone to caries — such as the lower
incisor region and roots. Hyposalivation may
explain patients with uncontrollable
Fig. 1 Saliva production recurrent caries, who are apparently comply-
and factors inhibiting it ing with dietary advice.
424 BRITISH DENTAL JOURNAL VOLUME 199 NO. 7 OCT 8 2005
7p423-427.qxd 26/09/2005 11:13 Page 425
PRACTICE
Diagnosis
Hyposalivation is a clinical diagnosis which can Keypoints for dentists:
be made by the practitioner predominantly on dry mouth
the basis of the history and examination. Diagnosis is clinical but investigations
may be indicated, including:
It can be helpful to document salivary func-
tion by salivary function studies such as salivary • Blood tests (ESR and SS-A and SS-
flow rates (sialometry). Collection of whole saliva B antibodies; see below)
(oral fluid) is currently the routine technique for • Eye tests (Schirmer; see below)
sialometry used by many clinicians, despite the • Urinalysis
fact that it is rather inaccurate and non-specific. • Salivary flow rate tests (sialometry)
It is usually carried out by allowing the patient • Salivary gland biopsy (labial gland
to sit quietly and dribble into a measuring con- biopsy)
tainer over 15 minutes; in a normal person, such
• Imaging
an unstimulated whole saliva flow rate exceeds
• Chest radiograph
1.5 ml/15 min (0.1 ml/min).
• Sialography
The specialist may be needed to: • Scintiscanning
• Study and document the degree of salivary • Ultrasound
dysfunction
• Determine the cause
• Arrange future dental care although much of
Key points for patients:
this can be undertaken in the primary care dry mouth
environment. • Saliva helps swallowing, talking,
and taste, and protects the mouth
Investigations may be indicated to exclude • Where saliva is reduced there is a
systemic disease, particularly to exclude: risk of dental decay (caries),
Fig. 2 Dry mouth • Sjögren’s syndrome and connective tissue halitosis, altered taste, mouth
disorders soreness and infections
• Diabetes • Saliva may be reduced by
radiotherapy or chemotherapy,
• Sarcoidosis
various drugs, after bone marrow
• Viral infections (hepatitis C; HIV). transplant, in diabetes, in some
viral infections, in
Commonly used investigations may thus include: anxiety/stress/depression, or in
• Blood tests (mainly to exclude diabetes, salivary gland disorders.
Sjögren’s syndrome, sarcoidosis, hepatitis and • Diagnosis is clinical but
investigations may be indicated,
other infections) including
• Eye tests (eg Schirmer test mainly to exclude
• Blood tests
Sjögren’s syndrome)
• Eye tests
• Salivary gland biopsy (if there is suspicion of
organic disease such as Sjögren’s syndrome ) • Urinalysis
• Imaging (mainly to exclude Sjögren’s • Salivary flow rate
Fig. 3 Dry mouth and lobulated tongue • Salivary gland biopsy
syndrome, sarcoidosis or neoplasia).
• X-rays or scans
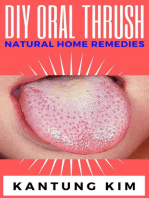
• Candidosis (Fig. 4) — which may cause a It is important to remember, as stated above,
burning sensation or mucosal erythema, that in some patients complaining of a dry
lingual filiform papillae atrophy, and angular mouth no evidence of a reduced salivary flow or
stomatitis (angular cheilitis) a salivary disorder can be found. There may then
• Halitosis (Article 4) be a psychogenic reason for the complaint.
• Ascending (suppurative) sialadenitis — which
presents with pain and swelling of a major Management (see below)
salivary gland, and sometimes purulent
discharge from the duct. SJÖGREN’S SYNDROME
Sjögren’s syndrome (SS) is an uncommon condi-
tion, the association of dry mouth and dry eyes.
The other key features of SS are evidence of an
autoimmune reaction shown usually by serum
autoantibodies and sometimes confirmed by
demonstrating mononuclear cell infiltrates in a
labial salivary gland biopsy. Sjögren’s syndrome
can affect any age but the onset is most common
in middle age or older. The majority of patients
are women.
Aetiopathogenesis
SS is an autoimmune disease affecting mainly
Fig. 4 Dry mouth complicated by candidosis exocrine glands like the salivary glands, lacrimal
BRITISH DENTAL JOURNAL VOLUME 199 NO. 7 OCT 8 2005 425
7p423-427.qxd 26/09/2005 11:13 Page 426
PRACTICE
glands and pancreas. There may be a viral aeti- Oral complaints (often the presenting feature)
ology and a genetic predisposition. including:
The most common type of SS is secondary • Xerostomia
Sjögren’s syndrome (SS-2) which comprises dry • Swollen salivary glands; causes include
eyes and dry mouth and a connective tissue or chronic sialadenitis as part of the fundamen-
autoimmune disease usually rheumatoid arthri- tal autoimmune disease process, ascending
tis (RA) (Table 3). However, SS can appear by bacterial sialadenitis which can arise if bacte-
itself, and in the absence of a connective tissue ria ascend the ducts because salivation is
disease is often termed sicca syndrome, usually impaired, benign lymphoepithelial lesions/
referred to as primary Sjögren’s syndrome (SS- myoepithelial sialadenitis (pseudolymphoma)
1). Nevertheless, both forms are chronic and can and lymphoma (Fig. 6).
affect not only the salivary glands (Fig. 5), but
also extraglandular tissues. Chronic B lympho-
cyte stimulation can occasionally lead to B cell
neoplasms such as lymphoma.
Table 3 Sjögren’s syndrome
SS-1 SS-2
Dry mouth Yes Yes
Dry eyes Yes Yes
Connective tissue No Yes
disease
Extraglandular More common Less common
problems Fig. 6 Complications of Sjögren’s syndrome
However, SS is a more generalised disorder
which involves not only the exocrine salivary
and lacrimal glands, but can have a range of
other complications, summarised in Figure 6.
Diagnosis
Diagnosis is made from the history and clinical
features, and may be confirmed by autoantibody
studies and sometimes by other investigations
such as sialometry and labial salivary gland
biopsy. In specialist units various international
criteria are used to confirm the diagnosis. There
is no specific treatment yet for SS, but the
hyposalivation can be managed, and dental pre-
ventive care is essential. The dental team have
an important role to play in this.
Management of hyposalivation
Any underlying cause of xerostomia should if
possible be rectified; for example, xerostomia-
producing drugs may be changed for an alterna-
tive, and causes such as diabetes should be treated.
Patients should be educated into efforts to
Fig. 5 Parotid gland swelling avoid factors that may increase dryness , and to
keep the mouth moist (Table 4).
SS is often characterised by a raised erythrocyte
sedimentation rate (ESR) and several autoanti- Salivary substitutes may help symptomatically.
bodies — particularly antinuclear factor (ANF) A variety are available including:
and rheumatoid factor (RF), and more specific • Water or ice chips; frequent sips of water are
antinuclear antibodies known as SS-A (Ro) and generally effective
SS-B (La). • Synthetic salivary substitutes (Table 5).
Clinical features As patients with objective xerostomia are at
SS presents mainly with eye complaints which increased risk of developing caries it is impor-
include sensations of grittiness, soreness, itch- tant that they take a non-cariogenic diet and
ing, dryness, blurred vision or light intolerance. maintain a high standard of oral hygiene. The
The eyes may be red with inflammation of the regular use of topical fluoride agents forms an
conjunctivae and soft crusts at the angles (ker- important component of their long-term care.
atoconjunctivitis sicca). The lacrimal glands Salivation may be stimulated by using
may swell. diabetic sweets or chewing gums (containing
426 BRITISH DENTAL JOURNAL VOLUME 199 NO. 7 OCT 8 2005
7p423-427.qxd 26/09/2005 11:13 Page 427
PRACTICE
Table 4 Ten tips for managing a dry mouth Table 5 Some salivary replacements
Drink enough water, and sip on water and other non-sugary UK trade names Offered as Contains Main Comments
fluids throughout the day. Rinse with water after meals. fluoride constituents
Keep water at your bedside.
AS Saliva Orthana Spray + /- Mucin Spray contains fluoride
Replace missing saliva with salivary substitutes, eg Artificial or lozenge Xylitol but is unsuitable if there
Saliva, (Glandosane, Luborant, Biotene Oralbalance, AS are religious objections
Saliva Orthana, Salivace, Saliveze). Alcohol-free to porcine mucin
mouthrinses (BioXtra and Biotène), or moisturising gels Biotene Oralbalance Gel - Glycerate polymer
(Oralbalance, BioXtra) may help. base, lactoperoxidase,
Stimulate saliva with: glucose oxidase, xylitol
• sugar-free chewing gums ( eg EnDeKay, Orbit, Biotène BioXtra Gel - Colostrum,
dry mouth gum or BioXtra chewing gum) or lactoperoxidase,
glucose oxidase, xylitol
• diabetic sweets or
Luborant Spray + Carboxymethylcellulose May contain fluoride
• Salivix or SST if advised or
• drugs that stimulate salivation (eg pilocarpine [Salagen]) Glandosane Spray - Carboxymethylcellulose
if advised by a specialist.
Salivace
Always take water or non-alcoholic drinks with meals and
Saliveze
avoid dry or hard crunchy foods such as biscuits, or dunk in
liquids. Take small bites and eat slowly. Eat soft creamy
foods (casseroles, soups), or cool foods with a high liquid
content — melon, grapes, or ice cream. Moisten foods with • http://www.nidcr.nih.gov/HealthInforma-
gravies, sauces, extra oil, margarine, salad dressings, sour tion/DiseasesAndConditions/SjogrenSjö-
cream, mayonnaise or yogurt. Pineapple has an enzyme that grensSyndrome.htm
helps clean the mouth. Avoid spices. • http://www.sjsworld.org/
Avoid anything that may worsen dryness, such as: • http://www.nidcr.nih.gov/HealthInforma-
• drugs, unless they are essential (eg antidepressants) tion/DiseasesAndConditions/DryMouthXe-
• alcohol (including in mouthwashes) rostomia/drymouth.htm
• smoking • http://www.oralcancerfoundation.org/den-
• caffeine (coffee, some soft drinks such as colas) tal/xerostomia.htm
• mouthbreathing.
SIALORRHOEA (HYPERSALIVATION; PTYALISM)
Protect against dental caries by avoiding sugary
Infants frequently drool but this is normal. The
foods/drinks and by:
complaint of sialorrhoea (excess salivation) is
• reducing sugar intake (avoid snacking and eating last
thing at night)
uncommon and may be true salivary hyper-
secretion — usually caused by physiological fac-
• avoiding sticky foods such as toffee
tors such as menstruation or early pregnancy,
• keeping your mouth very clean (twice daily local factors such as teething or oral inflamma-
toothbrushing and flossing)
tory lesions, food or medications (those with
• using a fluoride toothpaste cholinergic activity such as pilocarpine, tetra-
• using fluoride gels or mouthwashes (0.05% fluoride) benazine, clozapine), or by nasogastric intuba-
daily before going to bed
tion. In some cases, apparent hypersalivation is
• having regular dental checks. caused not by excess saliva production but by an
Protect against thrush, gum problems and halitosis by: inability to swallow a normal amount of saliva
• keeping your mouth very clean (false sialorrhoea) caused by neuromuscular
• keeping your mouth as moist as possible dysfunction (eg in Parkinson’s disease, cerebral
• rinsing twice daily with chlorhexidine (eg Chlorohex, palsy, or learning disability) or by pharyngeal or
Corsodyl, Eludril) or triclosan (eg Plax) oesophageal obstruction, such as by a neoplasm.
• brushing or scraping your tongue Treatment is of the underlying cause if possi-
• keeping dentures out at night ble and then the use of behavioural approaches
or antisialogogues. Occasionally, surgery to
• disinfecting dentures in hypochlorite (eg Milton, Dentural)
redirect the salivary gland ducts into the
• using antifungals if recommended by specialist.
oropharynx may be helpful.
Protect the lips with a lip salve or petroleum jelly (eg
Vaseline).
Avoid hot dry environments — consider a humidifier for the
bedroom.
sorbitol or xylitol, not sucrose). Cholinergic
drugs that stimulate salivation (sialogogues),
such as pilocarpine, or cevimeline should be
used only by a specialist. Oral complications
should be prevented and treated.
Useful websites: Patients to refer
• http://www.arc.org.uk/about_arth/book- Suspected Sjögren’s syndrome
lets/6041/6041.htm
BRITISH DENTAL JOURNAL VOLUME 199 NO. 7 OCT 8 2005 427
You might also like
- Advanced Smoking Cessation Hypnosis ScriptDocument16 pagesAdvanced Smoking Cessation Hypnosis ScriptShane Fozard94% (17)
- Material: RRC Revision GuideDocument17 pagesMaterial: RRC Revision Guidesheren zamanNo ratings yet
- Healing Through ArchitectureDocument10 pagesHealing Through ArchitectureSakshi DeshmukhNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationGowriNo ratings yet
- Felix2012 4Document6 pagesFelix2012 4rajesh kumarNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerGowriNo ratings yet
- A Patient With Dry Mouth PDFDocument6 pagesA Patient With Dry Mouth PDFWahdatNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionernavyaNo ratings yet
- Dry Mouth-1Document3 pagesDry Mouth-1channadrasmaNo ratings yet
- 53 Article XerosDocument5 pages53 Article XerosNivehthaa VisvamNo ratings yet
- عرض تقديمي من Microsoft PowerPoint جديدDocument10 pagesعرض تقديمي من Microsoft PowerPoint جديدHard TubeNo ratings yet
- Salivary Gland ComplaintsDocument9 pagesSalivary Gland ComplaintsGowriNo ratings yet
- University of Jordan Dentistry 2016: Ibrahim ShawaqfehDocument21 pagesUniversity of Jordan Dentistry 2016: Ibrahim ShawaqfehHanin AbukhiaraNo ratings yet
- Oral Manifestations of Nuritional Diseases in Children1Document5 pagesOral Manifestations of Nuritional Diseases in Children1andrada67No ratings yet
- Clinical Review: Oral Malodour (Halitosis)Document4 pagesClinical Review: Oral Malodour (Halitosis)Maghfira TiechaNo ratings yet
- Salivary Gland DiseaseDocument63 pagesSalivary Gland DiseaseAnchal RainaNo ratings yet
- Vpatho Module 1Document54 pagesVpatho Module 1Lib PalmaresNo ratings yet
- Tongue Diseases NDocument46 pagesTongue Diseases NhazeemmegahedNo ratings yet
- Endocrine DiseaseDocument27 pagesEndocrine Diseasesilentroar1427No ratings yet
- Oral Manifestations of Systemic Disease: Autoimmune DiseasesDocument7 pagesOral Manifestations of Systemic Disease: Autoimmune DiseaseshussainNo ratings yet
- Dry Mouth (Xerostomia)Document18 pagesDry Mouth (Xerostomia)dr_jamal1983No ratings yet
- Saliva DiseaseDocument8 pagesSaliva DiseaseJemuel Bucud LagartoNo ratings yet
- Ilovepdf MergedDocument7 pagesIlovepdf MergedNoval BalanceNo ratings yet
- Xerostomia: Oedijani-Santoso Bagian/SMF Gigi Dan Mulut FK Undip/RSUP DR Kariadi SemarangDocument40 pagesXerostomia: Oedijani-Santoso Bagian/SMF Gigi Dan Mulut FK Undip/RSUP DR Kariadi SemarangRizal Saeful DrajatNo ratings yet
- Xerostomia in Geriatric Patients: A Burgeoning Global ConcernDocument8 pagesXerostomia in Geriatric Patients: A Burgeoning Global ConcernwhiezardNo ratings yet
- 560-Article Text-1066-1-10-20171231 PDFDocument6 pages560-Article Text-1066-1-10-20171231 PDFKrupali JainNo ratings yet
- Oral, Git, Billiary ConditionsDocument107 pagesOral, Git, Billiary ConditionsNathaniel Mbiu TimNo ratings yet
- Article2 CitatDocument7 pagesArticle2 CitatMunteanu DragosNo ratings yet
- Screenshot 2022-09-20 at 8.37.00 AMDocument1 pageScreenshot 2022-09-20 at 8.37.00 AMjvvistopptxNo ratings yet
- Dry Mouth EngDocument25 pagesDry Mouth EngJelena BlagojevicNo ratings yet
- Xerostomia Clinical Aspects and TreatmentDocument14 pagesXerostomia Clinical Aspects and TreatmentThanh Điền LưuNo ratings yet
- Patology of LinguaDocument37 pagesPatology of LinguaVlad ScutelnicNo ratings yet
- Oral Medicine Journal Reading (Complete)Document29 pagesOral Medicine Journal Reading (Complete)Gabriel LowNo ratings yet
- Pediatric Oral Manifestation of Sustemic DiseaseDocument43 pagesPediatric Oral Manifestation of Sustemic DiseaseMike SihombingNo ratings yet
- Gastrointestinal Conditions Related To Tooth Wear: GeneralDocument4 pagesGastrointestinal Conditions Related To Tooth Wear: Generalfdeetny webassNo ratings yet
- DentalDocument8 pagesDentalHan Bich NguyenNo ratings yet
- Name: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentDocument4 pagesName: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentnadiaNo ratings yet
- Dental Erosion and The Role of Saliva: A Systematic ReviewDocument10 pagesDental Erosion and The Role of Saliva: A Systematic Reviewjperico99No ratings yet
- Oral Malodor: by - DR Monisha Kaushik 2Nd Yr MdsDocument55 pagesOral Malodor: by - DR Monisha Kaushik 2Nd Yr Mdsmonishakaus24No ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument63 pagesOral Medicine - Update For The Dental PractitionerPhuong MaiphuongNo ratings yet
- Oral Frictional HyperkeratosisDocument15 pagesOral Frictional HyperkeratosisFajarRahmantiyoNo ratings yet
- Xerostomia (Also Termed Dry Mouth: Xero-StomDocument6 pagesXerostomia (Also Termed Dry Mouth: Xero-Stomnazirrasheed123No ratings yet
- Oral Medicine - Update For The Dental Practitioner Lumps and SwellingsDocument9 pagesOral Medicine - Update For The Dental Practitioner Lumps and SwellingsGowriNo ratings yet
- 55 Diagnosis, Prevention and Management of Dental ErosionDocument29 pages55 Diagnosis, Prevention and Management of Dental Erosionraed ibrahimNo ratings yet
- Diagnosing, Managing, and Preventing Salivary Gland DisordersDocument13 pagesDiagnosing, Managing, and Preventing Salivary Gland DisordersGil JagudaevNo ratings yet
- Xerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganDocument8 pagesXerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganJonathan JojoNo ratings yet
- Oral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsDocument7 pagesOral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsKaty LunaNo ratings yet
- Diseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutDocument17 pagesDiseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutAli H. Sadiek أ.د. علي حسن صديق100% (4)
- Factors Which Complicate Impression Making PDFDocument18 pagesFactors Which Complicate Impression Making PDFMostafa FayadNo ratings yet
- Présentation 3Document13 pagesPrésentation 3Nador AbdennourNo ratings yet
- Awareness of Oral Manifestations Related To Systemic DiseasesDocument5 pagesAwareness of Oral Manifestations Related To Systemic DiseasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Management of Patients With Oral and Esophageal DisordersDocument81 pagesManagement of Patients With Oral and Esophageal DisordersEdmond ChanNo ratings yet
- Oral Submucous FibrosisDocument18 pagesOral Submucous FibrosisDrVaibhav ShrivastavaNo ratings yet
- Oral Submucous Fibrosis - An UpdateDocument90 pagesOral Submucous Fibrosis - An UpdateMugdha FrancisNo ratings yet
- Mohammed 2014Document7 pagesMohammed 2014Larasati RamadianiNo ratings yet
- Feline Oral DiseasesDocument6 pagesFeline Oral DiseasesBogdan PopaNo ratings yet
- A Simple Guide to Bad Breath and Mouth DiseasesFrom EverandA Simple Guide to Bad Breath and Mouth DiseasesRating: 5 out of 5 stars5/5 (3)
- Dryness of Mouth, (Xerostomia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDryness of Mouth, (Xerostomia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Mouth Ulcers of More Serious ConnotationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Mouth Ulcers of More Serious ConnotationMugiNo ratings yet
- Frequently Asked Questionsin Composite Restorative DentistryDocument7 pagesFrequently Asked Questionsin Composite Restorative DentistryMugi100% (1)
- Short Notes AssignmentDocument2 pagesShort Notes AssignmentMugiNo ratings yet
- What The Causative Agent Pneumonia and Microscopic Apperance?Document8 pagesWhat The Causative Agent Pneumonia and Microscopic Apperance?MugiNo ratings yet
- Tutorial 2 Microbe No.13Document1 pageTutorial 2 Microbe No.13MugiNo ratings yet
- Link For VideosDocument1 pageLink For VideosMugiNo ratings yet
- S. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusDocument14 pagesS. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusMugiNo ratings yet
- PRESBIKUSISDocument37 pagesPRESBIKUSISVenny SarumpaetNo ratings yet
- Jurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita MariniDocument7 pagesJurnal Keperawatan Muhammadiyah: Pipit Festi Wiliyanarti, Lusinta Dwi Kurniawati, Gita Marinihepi nopita sariNo ratings yet
- Teenage PregnancyDocument5 pagesTeenage PregnancyDavid VenturaNo ratings yet
- Walsh The Bermuda Triangle of Autism PDFDocument6 pagesWalsh The Bermuda Triangle of Autism PDFAnupamaNo ratings yet
- Advance Project Final FeasibilityDocument31 pagesAdvance Project Final FeasibilityMohammad Adil ChoudharyNo ratings yet
- Klinefelter SyndromeDocument3 pagesKlinefelter SyndromeKylalerrsssNo ratings yet
- Asia Healthcare Week Main Stage 2024 Overview Skeletal agendaxzQz4oYRaNicu1j6xlahru87z2tk1nrEBwFCR0xBDocument7 pagesAsia Healthcare Week Main Stage 2024 Overview Skeletal agendaxzQz4oYRaNicu1j6xlahru87z2tk1nrEBwFCR0xBjuliettekhooNo ratings yet
- PMDC Past Exam Qbank Step-2 by Dr. Asif KhanDocument80 pagesPMDC Past Exam Qbank Step-2 by Dr. Asif KhanrimshaafshenNo ratings yet
- Medical College Choices 08 NovDocument1 pageMedical College Choices 08 NovamitNo ratings yet
- Disseminated Intravascular CoagulationDocument3 pagesDisseminated Intravascular CoagulationArlan Abragan100% (1)
- Communication Skills in Nursing PDFDocument2 pagesCommunication Skills in Nursing PDFJennifer25% (4)
- A Management Algorithm For Esophageal PerforationDocument4 pagesA Management Algorithm For Esophageal Perforationoscar chirinosNo ratings yet
- AssignmentDocument4 pagesAssignmentMuhammad Moeez WaheedNo ratings yet
- Bag TechniqueDocument5 pagesBag Techniqueamp_raphNo ratings yet
- Yseali Younified 2020 A Guide To Planning A Community Service ActivityDocument17 pagesYseali Younified 2020 A Guide To Planning A Community Service ActivityHamidatun NisaNo ratings yet
- Health ICT Master PlanDocument6 pagesHealth ICT Master Planaboix253No ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet
- Communiqué Émis Par La PSCDocument4 pagesCommuniqué Émis Par La PSCL'express MauriceNo ratings yet
- Urine Screening For Metabolic Disorders PDFDocument5 pagesUrine Screening For Metabolic Disorders PDFJustine Nicole Clavel LachicaNo ratings yet
- Bhs Inggris 9Document19 pagesBhs Inggris 9ieki aiainNo ratings yet
- Critical Appraisal Nurse Staffing and Inpatient Hospital MortalityDocument42 pagesCritical Appraisal Nurse Staffing and Inpatient Hospital Mortalitykristina dewiNo ratings yet
- HX and PX Obstetrics and GynecologyDocument21 pagesHX and PX Obstetrics and GynecologyTadesse MuhammedNo ratings yet
- Ramadan and DiabetesDocument14 pagesRamadan and DiabetesDitoLinggoNo ratings yet
- 19 Disaster SurgeryDocument45 pages19 Disaster SurgeryAhmed noor Ahmed noorNo ratings yet
- Seed HealthTestingDocument9 pagesSeed HealthTestingMd. Sajjad HossenNo ratings yet
- AIDS Foundation of Chicago - Annual Report 2015Document24 pagesAIDS Foundation of Chicago - Annual Report 2015AdamAce VelasquezNo ratings yet
- Asian Pacific ScientistsDocument28 pagesAsian Pacific ScientistsMahmood SanglayNo ratings yet