Professional Documents
Culture Documents
Artigo Zé Pedro
Artigo Zé Pedro
Uploaded by
Rodrigo MarceloOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Artigo Zé Pedro
Artigo Zé Pedro
Uploaded by
Rodrigo MarceloCopyright:
Available Formats
6 - ORIGINAL ARTICLE
ISCHEMIA/REPERFUSION
Parecoxib reduces renal injury in an ischemia/reperfusion model in rats1
José Pedro Calistro NetoI, Rômulo da Costa TorresI, Giovanna Maria GonçalvesII, Leopoldo Muniz da SilvaIII, Maria Aparecida
Custódio DominguesIV, Norma Sueli Pinheiro MódoloV, Guilherme Antonio Moreira de BarrosVI
DOI: http://dx.doi.org/10.1590/S0102-865020150040000006
I
Fellow Master degree, Postgraduate Program in Anesthesiology, Botucatu Medical School, Sao Paulo State University (UNESP), Brazil. Conception,
design, intellectual and scientific content of the study.
II
Graduate student, Botucatu Medical School, UNESP, Botucatu-SP, Brazil. Technical procedures.
III
MD, Division of Anesthesiology, Botucatu Medical School, UNESP, Botucatu-SP, Brazil. Acquisition and interpretation of data, statistical analysis.
IV
Assistant Professor. Department of Pathology, Botucatu Medical School, UNESP, Botucatu-SP, Brazil. Acquisition and interpretation of data,
histological examinations.
V
Full Professor, Department of Anesthesiology, Botucatu Medical School, UNESP, Botucatu-SP, Brazil. Critical revision.
VI
Assistant Professor, Department of Anesthesiology, Botucatu Medical School, UNESP, Botucatu-SP, Brazil. Manuscript writing, supervised all
phases of the study.
ABSTRACT
PURPOSE: To evaluate the effect of parecoxib (an NSAID) on renal function by measuring plasma NGAL (serum neutrophil gelatinase-
associated lipocalin) levels in an induced-ischemia rat model.
METHODS: Forty male Wistar rats were randomly assigned to one of four groups: Ischemia (I), Ischemia/parecoxib (IP), No-ischemia
(NI), and No-ischemia/parecoxib (NIP). Body weight, mean arterial pressure, heart rate, body temperature, NGAL levels, and renal
histology were compared across groups.
RESULTS: The Ischemia (I) group, which did not receive parecoxib, showed the highest NGAL levels (p=0.001), while the IP group,
which received the medication, had NGAL levels similar to those of the non-ischemic (NI and NIP) groups.
CONCLUSION: Parecoxib resulted in renal protection in this experimental model.
Key words: Parecoxib. Ischemia. Reperfusion. Kidney. Rats.
270 - Acta Cirúrgica Brasileira - Vol. 30 (4) 2015
Parecoxib reduces renal injury in an ischemia/reperfusion model in rats
Introduction This is a prospective, randomized blind study. Forty
male Wistar rats weighing more than 250 g were used. The sex
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the of the animals, the experimental model, and the sample size were
most commonly-used class of drugs in the world1 and are used determined based on a previous study from our group that used
to treat a number of clinical symptoms, including acute pain2. the same methodology13. The animals were assigned to one of
NSAIDs inhibit the activity of cyclooxigenases (COXs) and are four experimental groups, with ten animals per group: Ischemia
classified as selective (selective COX-2 inhibitors) or non-selective (I), Ischemia/parecoxib (IP), No-ischemia (NI), and No-ischemia/
(COX-1 and COX-2 inhibitors), according to their mechanism of parecoxib (NIP) (Table 1).
action3. Thromboxanes and prostanoids are products of COX-1
and COX-2, respectively, and are involved in the maintenance of
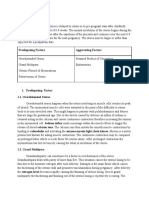
TABLE 1 - Experimental groups: Ischemia (I), Ischemia/
homeostasis of different organs and systems (e.g., gastrointestinal parecoxib (IP), No-ischemia (NI), and No-ischemia/parecoxib (NIP).
tract, kidney, heart, lung, brain, and platelets)4.
Group Inhalational Right Left Parecoxib
COX-1 is also called a constitutive enzyme and is involved (procedure) anesthesia nephrectomy ischemia
in cell function, regeneration and repair, whereas COX-2, which is I + + + -
called an inducible enzyme, depends on an inflammatory process IP + + + +
or the malfunction of the aforementioned organs and systems3,4. NI + + - -
However, the detection of COX-2 in the kidneys under normal NIP + + - +
conditions or under conditions of impaired renal blood flow (RBF)
and glomerular filtration rate (GFR) has attracted the attention of
researchers to the role of these drugs in maintaining renal function4-6. The animals were anesthetized with isoflurane, intubated,
Parecoxib sodium is the only COX-2-selective NSAID and kept under mechanical ventilation. Body temperature was
available in injectable form and approved for clinical use and kept between 36° and 37°C using a heating pad, and mean arterial
has comparable efficacy to that of non-selective NSAIDs7. pressure (MAP), heart rate (HR), and body temperature were
However, administration of parecoxib may affect renal function continuously monitored using a multi-parameter monitor.
in an unknown way, especially in situations of diminished renal Animals were catheterized in the arterial and venous
perfusion such as dehydration, hemorrhage, heart failure, low-salt accesses under local anesthesia of the bilateral cervical region with
diets, and stroke3,8,9. Renal function can be monitored using the 0.3 ml of 0.25% bupivacaine and depending on the experimental
neutrophil gelatinase-associated lipocalin (NGAL) biomarker, group, received either 20 mg/kg parecoxib or 2ml/kg saline
whose expression is induced by renal epithelial injury. In fact, solution, intravenously. The doses of parecoxib were determined
NGAL is one of the earliest markers of renal injury after ischemia according to the calculation recommended by the Food and Drug
or nephrotoxic injury in animal models10. Administration (FDA)14. Volume replacement was performed with
There is no consensus on the effect of parecoxib on renal continuous infusion of 5 ml/h of Ringer’s lactate solution (RLS).
function. For instance, Patel et al.11 used the concentration of After infiltration of the skin and subcutaneous tissue with
creatinine in ischemia/reperfusion models in rats and showed that 0.7 ml of 0.25% bupivacaine, median laparotomy was performed,
parecoxib increases renal dysfunction and injury associated with followed by right nephrectomy. Next, the left renal artery was
this form of renal stress. Conversely, Hauser et al.12 showed that clamped for 30 min.
parecoxib attenuates renal function impairment during porcine Blood samples were collected at the following times: T1
suprarenal aortic cross-clamping. (immediately after arterial access), T2 (5 min after clamping of the
This study aimed to evaluate the effects of parecoxib on left renal artery), T3 (20 min after reperfusion of the left kidney)
renal function by measuring plasma NGAL levels in an induced- and T4 (24 h after the beginning of the procedure). At each time
ischemia model in rats and histologically evaluate possible lesions. point, 1 ml samples of blood were taken and immediately replaced
with the injection of 2 ml RLS.
Methods Blood samples were centrifuged and the supernatant was
stored in a freezer at -80 °C. NGAL levels were measured using
The study was approved by the UNESP Ethics Committee ELISA (enzyme-linked immunosorbent assay) with a Rat NGAL
on Animal Use. ELISA kit (Kit 046, BioPorto Diagnostics, Hellerup, Denmark).
Acta Cirúrgica Brasileira - Vol. 30 (4) 2015 - 271
Calistro Neto JP et al.
This immunoenzyme assay detects the specific plasma antibody also differed significantly between groups: at T1, MAP was higher
by antigen-antibody interaction. in the I group than in the NIP group (p = 0.03), whereas at T2,
Right and left kidneys were stored separately in Duboscq- MAP was lower in the IP than in the NIP group (p = 0.01); at T3,
Brasil solution for 24 h and then transferred to 70% ethyl alcohol. MAP values were highest in the I group (p = 0.001). No significant
The Duboscq-Brasil solution is used to preserve and fixate renal differences in MAP were observed between the I and NI groups
structures and increase the reliability of the histological analysis. at any times, but MAP values were higher in T1 than in T2 and
Histological sections were stained with hematoxylin-eosin and T3 in the IP group (p = 0.007) and in T2 than in T1 and T3 in
evaluated with a light microscope for percentage of tubular the NIP group (p = 0.0002) (Figure 1). In addition, no significant
necrosis by a pathologist who was blind to which experimental differences in heart rate and body temperature were observed
groups the samples belonged to, and classified using the scale between groups.
proposed by Park et al.13 (Table 2). The following microscopic
criteria were used to determine the necrosis of tubular cells:
pyknosis, karyorrhexis or karyolysis, and chromatolysis.
TABLE 2 - Cell damage scores attributed to histological
specimens.
Degree of injury Type of injury % of injury
0 no lesion 0
1 mild < 10
2 moderate 10–25
3 moderately severe 25–50
4 severe 50–75
5 very severe > 75
Adapted from Park et al.13. FIGURE 1 - Mean arterial pressure (MAP) of male Wistar rats in the
Ischemia (I), Ischemia/parecoxib (IP), No-ischemia (NI), and No-
ischemia/parecoxib (NIP) groups at different times. The lines in the box
Data were normally distributed and were expressed
represent the means (middle line) and standard deviations (upper and
as means ± standard deviations. We used analysis of variance lower lines). Comparison between groups: T1: I > NIP (p = 0.03); T2: IP
(ANOVA) followed by the Tukey’s test at p<0.05 to compare < NIP (p = 0.01); T3: I > IP, I > NIP, NI > NIP (p = 0.001). Comparison
between times: I: (p = 0.12); IP: T1 > T2, T1 > T3 (p= 0.007); NI (p =
mean body weight, MAP, HR, body temperature, and NGAL 0.78); NIP: T1 < T2, T2 > T3 (p = 0.0002).
levels between experimental groups and the Friedman’s test to
compare these variables within a group at different times. Renal
histology was scored and renal lesions of right and left kidneys NGAL serum levels differed significantly between
were expressed as medians (25–75% percentiles) and compared groups and times (Table 3). NGAL levels were significantly higher
using the Kruskal-Wallis one-way analysis of variance followed at T4 relative to the other time points in all groups: I (p = 0.006),
by the Dunn’s post-hoc test at p<0.05. The Mann-Whitney test was IP (p < 0.001), NI (p < 0.001), and NIP (p < 0.001). In addition, no
used for intragroup comparison of renal histology scores. We used differences in NGAL levels were observed between groups at T1
the Fisher’s exact test to compare the frequency of renal lesions and T2. Conversely, NGAL levels were significantly higher in the
between the Ischemia (I) and Ischemia/parecoxib (IP) groups. I group than in the IP, NI, and NIP groups at T3 (p = 0.03) and T4
All analyses were performed using the Stata/SE 9.0 software for (p = 0.002) (Table 3).
Windows (Stata Corporation, College Station, Texas, USA). The
significance level was set at p<0.05.
Results
Mean body weight was higher in the I and NI groups than
in the IP and NIP groups (p < 0.05). Mean arterial pressure (MAP)
272 - Acta Cirúrgica Brasileira - Vol. 30 (4) 2015
Parecoxib reduces renal injury in an ischemia/reperfusion model in rats
TABLE 3 - NGAL levels (picograms per milliliter [pg/ The medians of lesion severity and intensity were higher
ml], mean ± sd) of male Wistar rats in the Ischemia (I), Ischemia/ in the I and IP groups than in the NI and NIP groups. Lesion
parecoxib (IP), No-ischemia (NI), and No-ischemia/parecoxib
severity ranged from mild to severe (Table 4).
(NIP) groups at different times.
Group Time
TABLE 4 - Lesion severity in right and left kidneys of
T1 T2 T3 T4
male Wistar rats in the Ischemia (I), Ischemia/parecoxib (IP), No-
I 15.23 ± 6.4 32.43 ± 37.54 ± 1186.63 ± ischemia (NI), and No-ischemia/parecoxib (NIP) groups.
35.52 38.64 1574.77
Group Kidney
IP 11.72 ± 10.68 ± 5.7 12.63 ± 5.48 254.56 ±
5.45 103.69 Right Left
NI 12.44 ± 23.51 ± 15.99 ± 5.21 311.05 ± I 0 (0.00) 1 (0.25–2) [4]
5.51 34.86 163.2 IP 0 (0.00) 0 (0.00) [2]
NIP 11.80 ± 10.02 ± 2.91 12.84 ± 2.55 295.63 ± NI 0 (0.00) 0 (0.00) [0]
3.42 78.37 NIP 0 (0.00) 0 (0.00) [0]
Comparison between times: I: T1 < T4, T2 < T4, T3 < T4 (p = 0.006); IP: T1 < T4, Values expressed as medians (25–75% percentiles) [total range]. Kruskal-Wallis
T2 < T4, T3 < T4 (p < 0.001); NI: T1 < T4; T2 < T4, T3 < T4 (p < 0.001); NIP: T1 one-way ANOVA – Dunn’s post-hoc test: Left kidney: I > IP, I> NIP (p = 0.01);
< T4, T2 < T4, T3 < T4 (p < 0.001). Comparison between groups: T1 (p = 0.56); T2 Right kidney: n.s. Intragroup comparison (Mann-Whitney test): I
(p = 0.17); T3: I > IP, NI, and NIP (p = 0.03); T4: I > IP, NI, and NIP (p = 0.002). (p = 0.004), IP (p = 0.70), NI (p = 1.00), NIP (p = 1.00).
For the histological analysis, right kidneys in all Discussion
experimental groups had a score of zero for acute tubular necrosis.
Animals in the NI and NIP groups, which had not received In this study, we used the ischemia/reperfusion model
renal ischemia-reperfusion but only systemic injection of anti- developed for kidney function and injury studies at the Department
inflammatory drugs, also had a score of zero for acute tubular of Anesthesiology, Botucatu Medical School. This model consists
necrosis. The left kidneys of animals in the I and IP groups, which of right nephrectomy in all animals, followed by randomization of
had been subjected to ischemia-reperfusion and administration the animals into four groups of 10 animals per group: Ischemia,
of parecoxib (IP), had varying scores of acute tubular necrosis. Ischemia + drug, Non-ischemia, and Non-ischemia + drug. Thus,
Lesions were more frequent in rats in the I group, in which seven parecoxib was tested in two groups, in the presence and absence
animals had lesions, with scores ranging from 1–4 (mild to of I/R (IP and NIP groups), and NGAL levels were measured in all
moderate lesions), and less frequent in the IP group, in which only groups at four times to evaluate renal function.
one animal had a renal injury with a score of 2 (mild lesion). Thus, Nephrectomy followed by ischemia/reperfusion may
tubular lesions were more frequent in the I group than in the IP, NI, trigger mechanisms of renal preconditioning, reducing histological
and NIP groups (Figure 2). lesions and preserving or facilitating recovery of renal function
in the ischemic kidney. For instance, animals that had not been
nephrectomized prior to ischemia/reperfusion had oliguric renal
failure, whereas animals that had been nephrectomized prior to
I/R developed polyuric renal failure with better prognosis and
recovery of renal function. The incidence of renal lesions in the
ischemic kidney was also higher in non-nephrectomized animals.
Plasma renin activity and renin content in the post-ischemic kidney
increased significantly in nephrectomized rats. Conversely, the
levels of thromboxane A2 and endothelin, which are responsible for
renal vasoconstriction, were higher in non-nephrectomized rats17.
Renal susceptibility to ischemic injury is directly related
to body temperature. Thus, maintaining body temperature within
FIGURE 2 - Total number of renal histological lesions in the left kidney a constant range and recording it is essential for the validation of
of male Wistar rats in the Ischemia (I) and Ischemia/parecoxib (IP) results, especially in ischemic models. In the absence of ischemic
groups (Fisher’s exact test). The number of histological renal lesions was stress, temperatures above 38°C do not alter renal morphology and
lower in the IP than in the I group (p = 0.01).
Acta Cirúrgica Brasileira - Vol. 30 (4) 2015 - 273
Calistro Neto JP et al.
function. However, hyperthermia has been shown to cause severe Blood pressure patterns were similar in the groups that
lesions in ischemia-reperfusion models. Conversely, temperatures received parecoxib (IP and NIP) and lower than in groups that did
below 35°C provided a protective effect, resulting in mild, not receive parecoxib (I and NI). Also, treated animals had the
reversible lesions and renal recovery 24–48 h after ischemic injury. lowest blood pressure levels at T3, regardless of whether they had
In our study, all animals were normothermic, with temperatures been exposed to I/R injury.
ranging between 36 and 37°C, a temperature range that favors a The reduction in blood pressure was also observed in
rapid recovery from ischemic renal injury. Thus, no significant another study about the effect of parecoxib on renal function. The
differences in body temperature were observed during the study. hypotensive effect in treated animals, combined with the diminished
Similarly, heart rate did not differ significantly between groups15,16. creatinine clearance and worse histology were associated with a
The right nephrectomy and stable temperature resulted negative effect of parecoxib on renal function, which was attributed
in similar ischemic preconditioning and susceptibility to renal to the non-activation of the renin-angiotensin-aldosterone system
injury in all groups, which reinforces our choice of using this secondary to the inhibition of COX-2 by parecoxib. The authors
model to evaluate the influence of parecoxib on renal function in also argued that COX-2 is of great importance for renal dynamics,
experimentally simulated simulations that are frequent in clinical especially in situations of imminent risk or renal injury11.
practice such as hemorrhage, dehydration, heart failure, surgery A study that evaluated the effects of intrarenal
performed under extracorporeal circulation, and shock. administration of parecoxib during suprarenal aortic cross-
Mean body weight was higher for animals in the I and clamping in pigs found that parecoxib attenuated renal impairment
NI groups than in the IP and NIP groups. However, we believe measured by kidney creatinine clearance and improved renal lactate
that this weight difference between groups had no effect on data balance. Additionally, no effects on the cardiovascular system of
collection because we used the human-equivalent parecoxib treated animals were observed, and the authors concluded that
dosage based on FDA guidelines for animal testing. Additionally, intrarenal parecoxib infusion positively affected kidney function12.
all animals weighed more than 250 g, which was the minimum The reduction in blood pressure in the groups that
weight for inclusion in the study. Moreover, volume replacement received parecoxib was not pronounced and the blood pressure
was based on the individual weight of each animal14. levels recorded were able to maintain RBF and GFR and not
The effects of NSAIDs on blood pressure have been significantly increase NGAL serum levels.
investigated in several experimental trials and in heterogeneous NGAL serum levels were lowest at T1 and highest at T4
populations18,19. COX-2-derived prostanoids such as PGE-2 and PGI- in all groups. In addition, NGAL levels were significantly higher
2, which act on renal tubules and ducts and on the macula densa, in the Ischemia group (I), which was not treated with parecoxib,
respectively, modulate the resorption of sodium and water and stimulate than in the IP, NI, and NIP groups. Conversely, at T4, NGAL levels
the production and release of renin, which acts as a potent systemic and in the IP group were similar to those in the NI and NIP groups,
renal vasoconstrictor3,20. This action increases the resorption of sodium/ which had not been subjected to I/R injury, and lower than in the
water and the secretion of potassium and maintains the glomerular I group.
filtration rate (GFR) and renal homeostasis, especially in situations of NGAL levels in the I group were higher at T3 and T4,
hemodynamic impairment and consequent renal injury21. Additionally, confirming the precocity of this biomarker in serum measures only
COX-1 prostanoids such as thromboxane also act as vasoconstrictors 50 min after injury (30 min of renal ischemia and 20 min of renal
and increase the resorption of sodium and water3. reperfusion). The use of parecoxib prior to I/R injury in the IP
NSAIDs are well-tolerated by individuals without group was solely responsible for the lower NGAL levels in this
impaired renal function and who do not depend on the COX system group. Moreover, the use of parecoxib in the NIP group did not
to maintain renal hemodynamics. However, NSAIDs should be result in increased NGAL levels.
used with caution in older individuals and in those with congestive A similar study about the effects of indomethacin, a
heart failure, liver cirrhosis, low-salt diets, or in situations of non-selective NSAID, and rofecoxib, a selective NSAID, showed
hypovolemia, because these individuals are dependent on the that both NSAIDs were associated with improved renal function,
mechanisms described above to maintain adequate GFR3,20. The use as measured by blood urea levels. The authors also observed
of parecoxib after coronary-artery bypass grafting was associated a reduction in proinflammatory cytokine levels and fewer
with an increased incidence of cardiovascular events and should histological lesions, especially in animals treated with rofecoxib.
be avoided in patients undergoing this type of procedure9. Part of the renal injury secondary to ischemia/reperfusion is a
274 - Acta Cirúrgica Brasileira - Vol. 30 (4) 2015
Parecoxib reduces renal injury in an ischemia/reperfusion model in rats
consequence of the inflammatory response with involvement Med. 2005 Mar;352(11):1081-91. PMID: 15713945.
10. Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C,
of COX-2 and prostaglandins, in addition to the production
Ruff SM, Zahedi K, Shao M, Bean J, Mori K, Barasch J, Devarajan
and secretion of chemokines, cytokines (IL-1, IL-6, IL-19, and P. Neutrophil gelatinase-associated lipocalin (NGAL) as a
TNF-α), and reactive oxygen species, gene activation, and cell biomarker for acute renal injury after cardiac surgery. Lancet. 2005
Apr;365(9466):1231-8. PMID: 15811456.
infiltration. The use of NSAIDs inhibited part of this response, 11. Patel NS, Cuzzocrea S, Collino M, Chaterjee PK, Mazzon E, Britti
resulting in renal protection22. D, Yaqoob MM, Thiemermann C. The role of cycloxygenase-2 in
No signs of histological lesions were observed in the rodent kidney following ischaemia/reperfusion injury in vivo.
Eur J Pharmacol. 2007 May;562(1-2):148-54. PMID: 17343844.
previously nephrectomized right kidneys and left kidneys that had 12. Hauser B, Froba G, Bracht H, Strater J, Chkhouta AB, Vassilev D,
not been subjected to ischemia (NI and NIP groups). Histological Schoaff MJ, Huber-Lang M. Effects of intrarenal administration of
the cox-2 inhibitor parecoxib during porcine suprarenal aortic cross-
lesions were observed only in the Ischemia (I) and Ischemia/ clamping. Shock. 2005 Nov;24(5):476-81. PMID: 16247335.
parecoxib (IP) groups, and were more frequent in animals in the I 13. Park Y, Hirose R, Dang K, Xu F, Behrends M, Tan V, Roberts JP,
group. The use of parecoxib was solely responsible for the lower Niemann CU. Increased severity of renal ischemia-reperfusion
injury with venous clamping compared to arterial clamping in
frequency of lesions in the IP than in the I group. The medians a rat model. Surgery. 2008 Feb;143(2):243-51. doi: 10.1016/j.
of cell damage scores did not differ between the I and IP groups surg.2007.07.041.
14. Food and Drug Administration. Guidance for industry: estimating the
and were significantly higher in these groups than in the NI and
maximum safe starting dose in intial clinical trial for therapeuthics
NIP groups. Thus, parecoxib administration does not appear to in adult health volunteers. Silver Spring: FDA; 2005.
determine lesion intensity in our experimental model. 15. Zager RA, Altschuld R. Body temperature: an important determinant
of severity of ischemic renal injury. Am J Physiol. 1986 Jul;251(1 Pt
2):F87-93. PMID: 3728686.
Conclusion 16. Delbridge MS, Shrestha BM, Raftery AT, El Nahas AM, Haylor JL.
The effect of body temperature in a rat model of renal ischemia-
reperfusion injury. Transplant Proc. 2007 Dec;39(10):2983-5.
Parecoxib provided renal protection to animals subjected PMID: 18089305.
to ischemia-reperfusion and its administration in non-ischemic 17. Islam CF, Mathie RT, Dinneen MD, Kiely EA, Peters AM, Grace
PA. Ischaemia-reperfusion injury in the rat kidney: the effect of
animals was not responsible for renal injury based on NGAL
preconditioning. Br J Urol. 1997 Jun;79(6):842-7. PMID: 9202547.
levels and histological analysis. 18. Johnson AG. NSAIDs and increased blood pressure. What is the
clinical significance? Drug Saf. 1997 Nov;17(5):277-89. Review.
PMID: 9391772.
References 19. Wang JL, Cheng HF, Harris RC. Cyclooxygenase-2 inhibition
decreases renin content and lowers blood pressure in a model of
1. Singh G, Triadafilopoulos G. Epidemiology of NSAID induced renovascular hypertension. Hypertension. 1999 Jul;34(1):96-101.
gastrointestinal complications. J Rheumatol Suppl. 1999 Apr;56:18- PMID: 104068.
24. Review. PMID: 10225536. 20. Brater DC, Harris C, Redfern JS, Gertz BJ. Renal effects of COX-
2. Kummer CL, Coelho TCRB. Anti-inflamatórios não esteroidais 2-selective inhibitors. Am J Nephrol. 2001 Jan-Feb;21(1):1-15.
inibidores da ciclooxigenase-2 (COX-2): aspectos atuais. Rev Bras PMID: 11275626.
Anestesiol. 2002 Jul;52(4):498-512. PMID: 19479115. 21. Noroian G, Clive D. Cyclo-oxygenase-2 inhibitors and the kidney: a
3. Harris RC. COX-2 and the kidney. J Cardiovasc Pharmacol. 2006;47 case for caution. Drug Saf. 2002;25(3):165-72. PMID: 11945113.
Suppl 1:S37-42. Review. PMID: 16785827. 22. Feitoza CQ, Goncalves GM, Semedo P, Cenedeze MA, Pinheiro HS,
4. Dirig DM, Isakson PC, Yaksh TL. Effect of COX-1 and COX- Beraldo FC, dos Santos OF, Teixeira Vde P, dos Reis MA, Mazzali
2 inhibition on induction and maintenance of carrageenan- M, Pacheco-Silva A, Câmara NO. Inhibition of COX 1 and 2 prior
evoked thermal hyperalgesia in rats. J Pharmacol Exp Ther. 1998 to renal ischemia/reperfusion injury decreases the development
Jun;285(3):1031-8. PMID: 9618405. of fibrosis. Mol Med. 2008 Nov-Dec;14(11-12):724-30. doi:
5. Brater DC, Harris C, Redfern JS, Gertz BJ. Renal effects of COX- 10.2119/2008-00064.
2-selective inhibitors. Am J Nephrol. 2001 Jan-Feb;21(1):1-15.
Review. PMID: 11275626.
6. Whelton A. Renal and related cardiovascular effects of conventional
and COX-2-specific NSAIDs and non-NSAID analgesics. Am J Correspondence:
Ther. 2000 Mar;7(2):63-74. Review. PMID: 11319575. Guilherme Antonio Moreira de Barros
7. Cheer SM, Goa KL. Parecoxib (parecoxib sodium). Drugs. Departamento de Anestesiologia
2001;61(8):1133-41. PMID: 11465874. Faculdade de Medicina de Botucatu-UNESP
8. Zhang J, Ding EL, Song Y. Adverse effects of cyclooxygenase Distrito de Rubião Junior
2 inhibitors on renal and arrhythmia events: meta-analysis of Caixa Postal 530
randomized trials. JAMA. 2006;Oct;296(13):1619-32. PMID: 18618-970 Botucatu - SP Brasil
16968832. Tel.: (55 14)3880-1411
9. Nussmeier NA, Whelton AA, Brown MT, Langford RM, Hoeft A, barros@fmb.unesp.br
Parlow JL, Boyce SW, Verburg KM. Complications of the COX-2
inhibitors parecoxib and valdecoxib after cardiac surgery. N Engl J
Acta Cirúrgica Brasileira - Vol. 30 (4) 2015 - 275
Calistro Neto JP et al.
Received: Dec 16, 2014
Review: Feb 19, 2015
Accepted: Mar 18, 2015
Conflict of interest: none
Financial source: none
1
Research performed at Experimental Laboratory of Anesthesiology,
Botucatu Medical School, Sao Paulo State University (UNESP), Brazil.
Part of Master degree thesis, Postgraduate Program in Anesthesiology,
UNESP. Tutor: Guilherme Antonio Moreira de Barros.
276 - Acta Cirúrgica Brasileira - Vol. 30 (4) 2015
You might also like
- Evidence Based Physical Diagnosis 5E Sep 1 2021 - 032375483X - Elsevier 5Th Edition Mcgee MD Full ChapterDocument51 pagesEvidence Based Physical Diagnosis 5E Sep 1 2021 - 032375483X - Elsevier 5Th Edition Mcgee MD Full Chapteranthony.pilkinton238100% (11)
- SNB QuestionsDocument7 pagesSNB Questionshardie himerNo ratings yet
- Oxygenation Response in Experimental Diabetic Retinopathy: - Lipoic Acid Corrects Late-Phase Supernormal RetinalDocument6 pagesOxygenation Response in Experimental Diabetic Retinopathy: - Lipoic Acid Corrects Late-Phase Supernormal RetinalmagreaNo ratings yet
- An Experimental Study of Ascorbic Acid Effects in Acute RenalDocument9 pagesAn Experimental Study of Ascorbic Acid Effects in Acute RenalfgonzalezNo ratings yet
- Captopril Alleviates Hypertension-Induced Renal Damage, in Ammation, and NF-KB ActivationDocument9 pagesCaptopril Alleviates Hypertension-Induced Renal Damage, in Ammation, and NF-KB ActivationpipikafiyaNo ratings yet
- Ardm 3 124Document4 pagesArdm 3 124Peertechz Publications Inc.No ratings yet
- Pluripotent Anti-Inflammatory Immunomodulatory Effects of Papaverine Against Cerebral Ischemic-Reperfusion InjuryDocument23 pagesPluripotent Anti-Inflammatory Immunomodulatory Effects of Papaverine Against Cerebral Ischemic-Reperfusion InjuryDragomir MirunaNo ratings yet
- 2012 The Effects of Medical Ozone Therapy On Renal Ischemia:Reperfusion InjuryDocument6 pages2012 The Effects of Medical Ozone Therapy On Renal Ischemia:Reperfusion InjuryAcupuntura de EquinosNo ratings yet
- Decreased Accumulation of Ultrasound Contrast in The Liver of Nonalcoholic Steatohepatitis Rat ModelDocument8 pagesDecreased Accumulation of Ultrasound Contrast in The Liver of Nonalcoholic Steatohepatitis Rat ModeldavdavdavdavdavdavdaNo ratings yet
- Effectiveness of Interleukin-1 Receptor Antagonist (Anakinra) On Cerulein-Induced Experimental Acute Pancreatitis in RatsDocument8 pagesEffectiveness of Interleukin-1 Receptor Antagonist (Anakinra) On Cerulein-Induced Experimental Acute Pancreatitis in RatsmattpauziNo ratings yet
- Histopathology Changes:: Acetaminophen-InducedDocument9 pagesHistopathology Changes:: Acetaminophen-InducedTanveer AhamadNo ratings yet
- In Uence of Cancer Cachexia On Drug Liver Metabolism and Renal Elimination in RatsDocument8 pagesIn Uence of Cancer Cachexia On Drug Liver Metabolism and Renal Elimination in RatsGregorius HocevarNo ratings yet
- Penelitian GlyserizinDocument9 pagesPenelitian GlyserizinNovita ApramadhaNo ratings yet
- Protective Effect of 3-N-Butylphthalide Against Hypertensive Nephropathy in Spontaneously Hypertensive RatsDocument19 pagesProtective Effect of 3-N-Butylphthalide Against Hypertensive Nephropathy in Spontaneously Hypertensive Ratsberliana syifaNo ratings yet
- Burnstock 1988Document7 pagesBurnstock 1988afifahridhahumairahhNo ratings yet
- J Nucl Med-1992-Lee-739-43Document6 pagesJ Nucl Med-1992-Lee-739-43felixwinataNo ratings yet
- British J Pharmacology - 2009 - Angulo - Differential Effects of Serotonin Reuptake Inhibitors On Erectile ResponsesDocument5 pagesBritish J Pharmacology - 2009 - Angulo - Differential Effects of Serotonin Reuptake Inhibitors On Erectile ResponsesSimone BelfioriNo ratings yet
- Citicoline Improved Cardiovascular Function in Animal Model of DysautonomiaDocument12 pagesCiticoline Improved Cardiovascular Function in Animal Model of DysautonomiaShaimaa NasrNo ratings yet
- P-Glycoprotein in Rats: Apocynum Venetum Extract Does Not Induce CYP3A andDocument4 pagesP-Glycoprotein in Rats: Apocynum Venetum Extract Does Not Induce CYP3A andZulfikar0526No ratings yet
- 2007-Effects and Mechanisms of Electroacupuncture at PC6 On Frequency of Transient Lower Esophageal Sphincter Relaxation in Cats PDFDocument8 pages2007-Effects and Mechanisms of Electroacupuncture at PC6 On Frequency of Transient Lower Esophageal Sphincter Relaxation in Cats PDFvictoregvNo ratings yet
- Plasma Leptin Levels in Rats With PancreatitisDocument6 pagesPlasma Leptin Levels in Rats With PancreatitisAndykaYayanSetiawanNo ratings yet
- A C A D e M I C S C I e N C e SDocument3 pagesA C A D e M I C S C I e N C e SM Rasya SanimanNo ratings yet
- Early Detection of Ketoprofen-Induced Acute Kidney Injury in Sheep As Determined by Evaluation of Urinary Enzyme ActivitiesDocument7 pagesEarly Detection of Ketoprofen-Induced Acute Kidney Injury in Sheep As Determined by Evaluation of Urinary Enzyme ActivitiesCamilaGalvisNo ratings yet
- AdiponectinDocument8 pagesAdiponectinfransiskaNo ratings yet
- Changes in Nucleotide Hydrolysis in RatDocument6 pagesChanges in Nucleotide Hydrolysis in RatconstanceNo ratings yet
- A Form of Distributive Shock Without Inhibition of Oxygen ConsumptionDocument10 pagesA Form of Distributive Shock Without Inhibition of Oxygen ConsumptionTerim ErdemlierNo ratings yet
- (Doi 10.1089/neu.2014.3497) A. D. Sauerbeck J. L. Laws V. v. Bandaru P. G. Popovich N. J - Spinal Cord Injury Causes Chronic Liver Pathology in RatsDocument11 pages(Doi 10.1089/neu.2014.3497) A. D. Sauerbeck J. L. Laws V. v. Bandaru P. G. Popovich N. J - Spinal Cord Injury Causes Chronic Liver Pathology in RatsDitaIsnainiNo ratings yet
- Reactive Oxygen and Nitrogen Species in Sepsis-Induced Hepatic Microvascular DysfunctionDocument10 pagesReactive Oxygen and Nitrogen Species in Sepsis-Induced Hepatic Microvascular DysfunctionGiosué Reyes HernandezNo ratings yet
- Original ArticleDocument7 pagesOriginal ArticleIntan AnanthaNo ratings yet
- Is There A Therapeutic Window For Pentoxifylline After The Onset of Acute PancreatitisDocument7 pagesIs There A Therapeutic Window For Pentoxifylline After The Onset of Acute PancreatitisalexandreunifenasNo ratings yet
- Left Ventricular Hypertrophy Is Associated With Inflammation in Sodium Loaded Subtotal Nephrectomized RatsDocument8 pagesLeft Ventricular Hypertrophy Is Associated With Inflammation in Sodium Loaded Subtotal Nephrectomized RatsLuis Marcas VilaNo ratings yet
- AnandDocument12 pagesAnandre septian IlhamsyahNo ratings yet
- MMR 2 5 857 PDFDocument8 pagesMMR 2 5 857 PDFguugle gogleNo ratings yet
- Evaluation of Urinary Variables As Diagnostic Indicators of Acute Kidney Injury in Egyptian Draft Horses Treated With Phenylbutazone TherapyDocument6 pagesEvaluation of Urinary Variables As Diagnostic Indicators of Acute Kidney Injury in Egyptian Draft Horses Treated With Phenylbutazone TherapyMarilú ValdepeñaNo ratings yet
- Pone 0085481Document8 pagesPone 0085481nadiaNo ratings yet
- Ebselen, A Seleno-Organic Antioxidant, Is Neuroprotective After Embolic Strokes in RabbitsDocument7 pagesEbselen, A Seleno-Organic Antioxidant, Is Neuroprotective After Embolic Strokes in RabbitsZahra NisaNo ratings yet
- Ebselen, A Seleno-Organic Antioxidant, Is Neuroprotective After Embolic Strokes in RabbitsDocument7 pagesEbselen, A Seleno-Organic Antioxidant, Is Neuroprotective After Embolic Strokes in RabbitsZahra NisaNo ratings yet
- Influence of Antidepressant Drugs On EctDocument7 pagesInfluence of Antidepressant Drugs On EctconstanceNo ratings yet
- Intermittent Hypoxia and Isoniazid Plus Rifampicin.35Document5 pagesIntermittent Hypoxia and Isoniazid Plus Rifampicin.35k52g248y2xNo ratings yet
- Jurnal LisinoprilDocument7 pagesJurnal LisinoprildidiisafitriNo ratings yet
- tmp1006 TMPDocument10 pagestmp1006 TMPFrontiersNo ratings yet
- BloodDocument5 pagesBloodIstván PortörőNo ratings yet
- 2022 Article 8889Document10 pages2022 Article 8889wiwiNo ratings yet
- Artificially Cultivated Ophiocordyceps Sinensis AlleviatesDocument17 pagesArtificially Cultivated Ophiocordyceps Sinensis AlleviatesHoang IceNo ratings yet
- Hesperidin Improves Warm Ischemia/reperfusion-Induced Oxidative Renal Injury in RatsDocument11 pagesHesperidin Improves Warm Ischemia/reperfusion-Induced Oxidative Renal Injury in RatsN Nur AriniNo ratings yet
- Aji Tridika WardanaDocument6 pagesAji Tridika WardanaRaymonNo ratings yet
- Inhibition of Prostaglandin Synthesis During Polystyrenemicrosphere-Induced Pulmonary Embolism in The RatDocument10 pagesInhibition of Prostaglandin Synthesis During Polystyrenemicrosphere-Induced Pulmonary Embolism in The RatshintaNo ratings yet
- Extract of Induced FlavonoidDocument11 pagesExtract of Induced FlavonoidMohammad SutamiNo ratings yet
- Research Article: Effects of Proton Pump Inhibitors and H Receptor Antagonists On The Ileum MotilityDocument8 pagesResearch Article: Effects of Proton Pump Inhibitors and H Receptor Antagonists On The Ileum MotilityAjengNo ratings yet
- 17tohj (Ervandi)Document4 pages17tohj (Ervandi)Ervandi AbudiNo ratings yet
- Hyperamylasemia With Normal Pancreas in Leptospirosis: Vasu Pillai Letchumanan Manisekar K. Subramaniam FrcsDocument4 pagesHyperamylasemia With Normal Pancreas in Leptospirosis: Vasu Pillai Letchumanan Manisekar K. Subramaniam FrcsherrerachaimNo ratings yet
- Where Hypertension Happens: CommentariesDocument4 pagesWhere Hypertension Happens: CommentariesIlvita MayasariNo ratings yet
- Vol-1, Issue 7 Paper (5) Page 26-31Document7 pagesVol-1, Issue 7 Paper (5) Page 26-31IJMSHCNo ratings yet
- Lung Lobe Torsion in Seven Juvenile DogsDocument7 pagesLung Lobe Torsion in Seven Juvenile DogsKelvinSueyzyNo ratings yet
- Lack of Nephrotoxicity by 6% Hydroxyethyl Starch 130/0.4 During Hip ArthroplastyDocument11 pagesLack of Nephrotoxicity by 6% Hydroxyethyl Starch 130/0.4 During Hip ArthroplastyKarina Mega WNo ratings yet
- 2011 Ozone Postconditioning in Renal Ischaemia Reperfusion ModelDocument7 pages2011 Ozone Postconditioning in Renal Ischaemia Reperfusion ModelSidnei GomesNo ratings yet
- MainDocument11 pagesMainDhonz R AdiwaramanNo ratings yet
- 17TOHJDocument4 pages17TOHJAriffa DiazNo ratings yet
- Protective Effect of Casperome An Orally Bioavailable Frankincense Extract On Lipopolysaccharide Induced Systemic Inflammation in MiceDocument18 pagesProtective Effect of Casperome An Orally Bioavailable Frankincense Extract On Lipopolysaccharide Induced Systemic Inflammation in Miceana mariaNo ratings yet
- 2021 - ACC - MarcelloDocument6 pages2021 - ACC - MarcelloMarcello HenriqueNo ratings yet
- Ni Hms 406767Document19 pagesNi Hms 406767Alex BuruianaNo ratings yet
- Taleofheike0000unse 0007Document10 pagesTaleofheike0000unse 0007Rodrigo MarceloNo ratings yet
- LIVRO - Introdução A Estudos de Fonologia Do Português Brasileiro - Leda BisolDocument250 pagesLIVRO - Introdução A Estudos de Fonologia Do Português Brasileiro - Leda BisolRodrigo MarceloNo ratings yet
- BURKERT, Walter. Pleading For Hell. Postulates, Fantasies, and The Senselessness of PunishmentDocument21 pagesBURKERT, Walter. Pleading For Hell. Postulates, Fantasies, and The Senselessness of PunishmentRodrigo MarceloNo ratings yet
- HIRASAWA, Caroline. The Inflatable, Collapsible Kingdom of Retribution. A Primer On Japanese Hell Imagery and ImaginationDocument59 pagesHIRASAWA, Caroline. The Inflatable, Collapsible Kingdom of Retribution. A Primer On Japanese Hell Imagery and ImaginationRodrigo Marcelo100% (1)
- POOLTHUPYA, Srisurang. The Influence of The Ramayana On Thai Culture. Kingship, Literature, Fine Arts and Performing Arts.Document10 pagesPOOLTHUPYA, Srisurang. The Influence of The Ramayana On Thai Culture. Kingship, Literature, Fine Arts and Performing Arts.Rodrigo MarceloNo ratings yet
- PIAYURA, Orathai. Metrosexual Men in Thai Classical Literature.Document4 pagesPIAYURA, Orathai. Metrosexual Men in Thai Classical Literature.Rodrigo MarceloNo ratings yet
- 022 PTSD & StrokeDocument2 pages022 PTSD & Strokejim912No ratings yet
- Diabetes MellitusDocument8 pagesDiabetes MellitusRegiever SalvanteNo ratings yet
- Drugs Uses For Heart FailureDocument45 pagesDrugs Uses For Heart FailureJoshua ObrienNo ratings yet
- ICSE Skin WorksheetDocument1 pageICSE Skin WorksheetpreetaNo ratings yet
- Suggested Answers To Exercise, Reading To Learn and Cross-Topic ExerciseDocument19 pagesSuggested Answers To Exercise, Reading To Learn and Cross-Topic ExerciseBernardNo ratings yet
- The Cardiovascular System: The Heart: Human Anatomy & PhysiologyDocument36 pagesThe Cardiovascular System: The Heart: Human Anatomy & PhysiologymalisalukmanNo ratings yet
- 1st Periodical TestDocument9 pages1st Periodical TestJezzaMay TambauanNo ratings yet
- PericardiocentesisDocument3 pagesPericardiocentesisThe Multilingual MedicNo ratings yet
- What Is Subinvolution?Document5 pagesWhat Is Subinvolution?Xierl BarreraNo ratings yet
- Chapter 24 (Digestive System) Chapter 24 (Digestive System)Document30 pagesChapter 24 (Digestive System) Chapter 24 (Digestive System)Pranali BasuNo ratings yet
- 3.2 Organisms and Substance Exchange - Gas Exchange 2 - QuestionsDocument22 pages3.2 Organisms and Substance Exchange - Gas Exchange 2 - QuestionsMaymunah HussainNo ratings yet
- Exercise Based Cardiac Rehabilitation For Adults After Heart Valve SurgeryDocument39 pagesExercise Based Cardiac Rehabilitation For Adults After Heart Valve Surgeryrima rizky nourliaNo ratings yet
- Mahmud RAHMAN - Edexcel - Biology - Health, Disease and The Development of Medicines - KnowIT - GCSE 2Document49 pagesMahmud RAHMAN - Edexcel - Biology - Health, Disease and The Development of Medicines - KnowIT - GCSE 2Mahmud RahmanNo ratings yet
- Hemodynamic Disturbance: Dr. Usha.MDocument77 pagesHemodynamic Disturbance: Dr. Usha.MOlumide Omotola AjayiNo ratings yet
- Steal SyndromeDocument5 pagesSteal SyndromeIrma SihotangNo ratings yet
- Raksha Yadav B.SC Nursing 2 Year Aiims, JodhpurDocument22 pagesRaksha Yadav B.SC Nursing 2 Year Aiims, JodhpurrohitNo ratings yet
- Heat Illness: Melissa Platt and Salvator VicarioDocument11 pagesHeat Illness: Melissa Platt and Salvator VicarioSNo ratings yet
- 2019 ESC Guidelines For The Diagnosis and Management of Chronic Coronary SyndromeDocument71 pages2019 ESC Guidelines For The Diagnosis and Management of Chronic Coronary SyndromeOber SánchezNo ratings yet
- Acr-Nasci-Sir-Spr Practice Parameter For The Performance and Interpretation of Body Computed Tomography Angiography (Cta)Document15 pagesAcr-Nasci-Sir-Spr Practice Parameter For The Performance and Interpretation of Body Computed Tomography Angiography (Cta)kirim mammoNo ratings yet
- Sunday Academic Meet - 240204 - 081157Document7 pagesSunday Academic Meet - 240204 - 081157Srinivas PingaliNo ratings yet
- Study-Guide-2-Management-of-Patients-with-Cardiovacular-Copy For StudentsDocument17 pagesStudy-Guide-2-Management-of-Patients-with-Cardiovacular-Copy For StudentsDan Dan ManaoisNo ratings yet
- Checked - Unit 1 Molecules, Diet, Transport and Health - Exam - MSDocument16 pagesChecked - Unit 1 Molecules, Diet, Transport and Health - Exam - MSEllane leeNo ratings yet
- Stroke Drug Study (GROUP)Document8 pagesStroke Drug Study (GROUP)Fran LanNo ratings yet
- Neonatal Hyperbilirubemia: (Jaundice in Neonates)Document13 pagesNeonatal Hyperbilirubemia: (Jaundice in Neonates)Hendrix Antonni AmanteNo ratings yet
- 1820 Retroperitoneum 64072e4e94d52Document37 pages1820 Retroperitoneum 64072e4e94d52Leticia JiménezNo ratings yet
- Anatomy and Physiology ASCVDDocument9 pagesAnatomy and Physiology ASCVDAlvheen JoaquinNo ratings yet
- Essence of Anesthesia Practice e Book 4th Edition Ebook PDFDocument61 pagesEssence of Anesthesia Practice e Book 4th Edition Ebook PDFalla.adams464100% (56)
- The Anatomy and Physiology of The Small Bowel: David GourevitchDocument2 pagesThe Anatomy and Physiology of The Small Bowel: David GourevitchNur Ainaa Almardhiyah TubungNo ratings yet