Professional Documents
Culture Documents
Analysis of Blood Culture Profile and Factors Related To Microbial Patterns and Antibiotic Resistance in Intensive Care Unit
Analysis of Blood Culture Profile and Factors Related To Microbial Patterns and Antibiotic Resistance in Intensive Care Unit
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Analysis of Blood Culture Profile and Factors Related To Microbial Patterns and Antibiotic Resistance in Intensive Care Unit
Analysis of Blood Culture Profile and Factors Related To Microbial Patterns and Antibiotic Resistance in Intensive Care Unit
Copyright:
Available Formats
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Analysis of Blood Culture Profile and Factors Related
to Microbial Patterns and Antibiotic Resistance in
Intensive Care Unit
Apriandeny Haithami*, Yutu Solihat**, Bastian Lubis**
*Post Graduate Program in Anesthesiology and Intensive Therapy, Faculty of Medicine, University of Sumatera Utara, Medan,
Indonesia
**Department of Anesthesiology and Intensive Therapy, Faculty of Medicine, University of Sumatera Utara, Medan, Indonesia
Introduction:- Bloodstream infection is an infectious I. INTRODUCTION
disease characterized by the presence of live bacterial or
fungal microorganisms in the bloodstream, as evidenced A bloodstream infection (BSI) is an infectious disease
by positive blood cultures. These pathogens have an characterized by the presence of live bacterial or fungal
important role in infection, especially in the intensive microorganisms in the bloodstream, as evidenced by a
care unit (ICU). Although infection is not the most positive blood culture.1 BSI is a frequent and life-
common cause of mortality in ICU care, infection is threatening event in the hospital environment, where it is
confirmed to be associated with increased hospitalization associated with a high mortality of around 40-60%. Severely
and high treatment costs. ill patients are predisposed to getting BSI, which occurs in
about 7% of patients in the first month of treatment in the
Objective: This study aims to determine the profile of intensive care unit (ICU).2
blood culture, the factors that have a bearing on the
results, and the description of antibiotic resistance in Recently, there has been a shift towards resistant
patients at Haji Adam Malik General Hospital. strains in recent years, such as methicillin-resistant
Staphylococcus aureus (MRSA), vancomycin-resistant
Method: This study is a study using secondary data from enterococci (VRE), extended - spectrum beta-lactamases
patients in ICU Haji Adam Malik General Hospital in (ESBLs), carbapenems - resistant Enterobacteriaceae (CRE),
2019 - 2020 conducted by blood culture. colistin resistant acinetobacter, and fluconazole‑resistant
Candida spp. These pathogens have an important role in
Results: This study included data from 52 patients who infection especially in the ICU. Although infection is not the
were recorded between 2019 – 2020 and underwent single most common cause of mortality in ICU patients, it is
blood culture. There are 50% women and men each with confirmed that infection is associated with increased length
an average age of 54,69 years. Based on the acquisition of of stay and high hospital costs. Information and scientific
a positive blood culture in terms of the day of admission, development regarding clinical epidemiology,
found 33 people (61.4%) positive patients after passing microbiological etiology, and pathophysiology of disease
48 hours. The highest morphology was Gram negative can certainly help understand the concept of infection
rods, 52.8% with the most species, Klebsiella pneumoniae control, and ultimately the appropriate use of antibiotics. 3
ESBL positive, and found Carbapenemase-producing
bacteria (5.5%). The most common Gram-positive This study aims to determine the profile of blood
bacterium is Staphylococcus aureus (15%), and half is culture, the factors - factors related to the results, as well as
suspected MRSA. the description of antibiotic resistance in patients with Haji
Adam Malik General Hospital.
Conclusion: Most types of bacteria found in ICU patients
in Haji Adam Malik General Hospital are Gram- II. METHOD
negative rod bacteria, with the time it was found above
48 hours after entering the hospital. The picture of This study is a descriptive analytic study with a cross-
antibiotic resistance is in line with the bacteria found sectional approach. This research was conducted in the ICU
with the property of drug resistance. Preventive of Haji Adam Malik General Hospital Medan. This study
measures are needed to prevent patients from the started from March 2020 with secondary data meeting the
possibility of transmitting these microorganisms. criteria taken from treatment in 2019 - 2020. The research
subjects were secondary data of all patients who were
Keywords:- Culture, Blood, Microorganisms, Resistance, treated in the ICU ward of Haji Adam Malik General
ICU. Hospital Medan and blood cultures were performed in the
ICU of Haji Adam Malik General Hospital Medan.
IJISRT21JUL1032 www.ijisrt.com 1497
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
The number of subjects included in this study were 52 Subject Characteristics N %
people. The inclusion criteria of the patient was an ICU Gender
patient at Haji Adam Malik General Hospital, at least 18 Male 26 50
years old, and a blood culture was performed. There were no Female 26 50
exclusion criteria in that study. Subjects were selected by Age (WHO Classification)
consecutive sampling. Adult (20 – 60 years old) 37 69,8
Elderly (> 60 years old) 15 28,3
In addition to demographic characteristics in the form
of age and sex, some of the variables examined include Elderly Based on positive blood culture obtained from
conditions of bloodstream infections such as bacteremia and the day of admission, 33 (61.4%) patients were positive after
fungemia, bacterial patterns described by Gram and species 48 hours of treatment, while the rest were under 48 hours. It
identification, and patterns of antibiotic resistance. A history is included in the category of bloodstream infection with
of central venous catheter placement and mechanical onset or hospital-acquired, because it is identified after 48
ventilation was also seen in the patient. hours of admission.
This research process has passed the ethical clearance In this study, it was found that 52 blood cultures were
test from the Medical Research Ethics Commission of the collected with positive results of microorganism growth,
University of Sumatra Utara and obtained a research permit where all samples obtained bacterial growth (100%). Fungal
from the institution where the research was conducted, growth was only found in one sample (1.9%). Multiple
namely the Haji Adam Malik General Hospital Medan. infections were found in two samples, namely infection with
two types of bacteria (Escherichia coli ESBL positive and
III. RESULT Klebsiella pneumoniae ESBL positive), and infection with
bacteria and fungi (Enterococcus faecium and Candida
This study includes data from 52 patients who were lucitanae)(Table 2).
recorded between 2019 – 2020 and underwent a blood
culture process. There are 26 people (50%) women and 26 Based on Gram staining, it was found that there were
samples (50%) are men. The majority of the population in almost equal numbers of Gram negative bacteria (52.8%)
this study were adults, namely 37 people (69.8%) with an and Gram positive bacteria (47.1%). The most morphology
average (mean) age of 54.69 years (Table 1). was Gram negative rods, which was 52.8% with the most
species being Klebsiella pneumoniae ESBL positive with 11
Table 1. Frequency distribution of research subjects by samples.
gender
Table 2. Blood Culture Result
Results %
Based on Blood Culture Results
- Bacterimia 52 100
- Fungemia 1 1,9
- Multiple infections 2
Based on Gram Stains (n = 53)
- Gram Positive 25 47,1
- Gram Negative 28 52,8
Based on Bacterial Morphology (n = 53)
- Coccus Gram Positif 23 43,3
- Coccus Gram Negatif 0 0
- Batang Gram Positif 2 3,7
- Batang Gram Negatif 28 52,8
Based on Bacterial Species (n = 53)
- Acinetobacter baumanii 3 5,6
- Acinetobacter baumanii Carbapenemase positif 1 1,8
- Burkholderia cepacia 1 1,8
- Burkholderia pseudomallei 1 1,8
- Enterobacter cloacae 2 3,7
- Escherichia coli 1 1,8
- Escherichia coli ESBL positif 5 9,4
- Klebsiella pneumoniae ESBL positif 11 20,8
- Psedomonas aeruginosa 1 1,8
- Psedomonas aeruginosa Cabapenemase positif 2 3,7
- Actinomyces odontylicus 1 1,8
- Corynebacterium striatum 1 1,8
- Enterococcus faecium 4 7,5
IJISRT21JUL1032 www.ijisrt.com 1498
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
- Staphylococcus aureus 4 7,5
- Staphylococcus aureus cefoxitin positif (Susp MRSA) 4 7,5
- Staphylococcus capitis 1 1,8
- Staphylococcus epidermidis 3 5,6
- Staphylococcus epidermidis Cefoxitin + 1 1,8
- Staphylococcus haemolyticus 2 3,7
- Staphylococcus hominis 2 3,7
- Staphylococcus hominis Cefoxitin positif 2 3,7
Based on Fungal Species
- Candida lusitaniae 1 1,8
Based on the types of Gram-positive bacteria, the most found in the treatment above 48 hours. The results of the
common genus found was Gram-positive cocci with the relationship between the two categorical variables obtained
most species being Staphylococcus aureus, which was about a P value of 0.081 from the Chi Square test. There was no
8 samples (15%). Four of the eight samples of relationship between the time of admission and the
Staphylococcus aureus had positive Cefoxitin screening test incidence of Gram-positive bacteria (Table 5).
results so that they were suspected to be MRSA.
Table 5. Bacterial Patterns Based on Admission
From 44 patients who had CVC installed, it was found Blood Culture
that the number of Gram negative and Gram positive P value
<48hour >48hour
bacteria was almost the same, namely 45.46% and 54.54%, Gram Positive 12 13
respectively. The results of the relationship between two Gram Negative 7 21 0,081
categorical variables obtained a P value of 0.308 from Total 19 34
Fisher's test, there is no relationship between CVC
installation and the incidence of Gram positive bacteria There are variations in the distribution of germ
(Table 3). patterns based on the patient's diagnosis. The most bacteria
were found, namely Gram-positive in diseases of the
From 44 patients who had CVC installed, it was found urogenital system, and the most Gram-negative in diseases
that the number of Gram negative and Gram positive of the nervous system and infections. One fungal infection
bacteria was almost the same, namely 45.46% and 54.54%, was found in one patient with acute peritonitis.
respectively. The results of the relationship between two
categorical variables obtained a P value of 0.308 from There are 33 types of antibiotics recorded that have
Fisher's exact test, which means that there is no relationship been tested. Some of the most common antibiotics tested
between CVC installation and the incidence of Gram were Ciprofloxacin (51 times), Tigecycline (43 times),
positive bacteria (Table 3). Gentamycin (46 times), and Ampicillin Sulbactam (46
times). The minimum tests were antibiotics Azithromycin (1
Table 3. Bacterial Patterns Based on the Use of CVC time), Cefixim (1 time), Chloramphenicol (1 time),
Yes No P value Cotrimoxazole (2 times), and Penicillin (3 times) (Table 7).
Gram Positive 20 5 The antibiotics with the highest sensitivity level were
Gram Negative 24 3 0,308 Cefoperazone and Cefixim, with 100% of a single
Total 44 8 examination. Antibiotics with the highest sensitivity after
being examined in more than half of the samples were
Of the 48 patients who were on a ventilator, it was Amikacin (88.9%), Meropenem (85.7%), Tigecycline
found that the number of Gram negative and Gram positive (91.5%). Antibiotics with the highest resistance level were
bacteria was almost the same, namely 45.8% and 54.2%, Azithromycin, Chloramphenicol, Penicillin with a value of
respectively. The results of the relationship between the two 100%. Antibiotics with the highest resistance after being
categorical variables obtained a P value of 0.278 from examined in more than half of the samples were Ampicillin
Fisher's test, which means that there is no relationship (92.6%) and Cefazolin (89.7%).
between ventilator installation and the incidence of Gram-
negative bacteria (Table 4). IV. DISCUSSION
Table 4. Bacterial Patterns Based on the Use of The global prevalence of bloodstream infections is
Ventilators very difficult to assess because of the different patient
Yes No P value populations and the different types of hospitals. In this
Gram Positive 22 3 study, it took a large time range to meet the needs of the
Gram Negative 26 1 0,276 number of samples that met the positive criteria. In Europe
Total 48 4 alone the prevalence ranges from 2.3 to 10.8 percent, which
means that from 100 people cultured the probability of
Of the 53 types of bacteria obtained on blood cultures, getting a patient with positive bloodstream infection is 2 to
it was found that the treatment was below 48 hours and 10 people.1
above 48 hours, the most Gram-negative bacteria were
IJISRT21JUL1032 www.ijisrt.com 1499
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Table 7. Antibiotic Sensitivity Test Results
Sensitivity Test Results
Antibiotic Type n (%)
S I R SDD
Amikacin (n = 27) 24 (88,9) 3 (11,1)
Amoxicillin (n = 22) 3(13,6) 19(86,4)
Ampicillin (n = 27) 2(7,4) 25(92,6)
Ampicillin Sulbactam (n = 46) 10(21,7) 2(4,3) 34(73,9)
Azithromycin (n = 1) 1(100)
Cefalexin (n = 15) 1(6,7) 14(93,3)
Cefazolin (n = 29) 3(10,3) 26(89,7)
Cefixim (n = 1) 1(100)
Cefotaxim (n = 6) 5(83,3) 1(16,7)
Ceftazidime (n = 31) 11(35,5) 1(3,2) 19(61,3)
Ceftrizxone (n = 28) 5(17,9) 1(3,6) 22(78,6)
Cefuroxime (n = 20) 4(20) 16(80)
Ertapenem (n = 20) 18(90) 1(5) 1(5)
Cefepime (n = 32) 15(46,9) 1(3,1) 13(40,6) 3(9,4)
Cefoperazone Sulbactam (n = 3) 2(66,7) 1(33,3)
Chloramphenicol (n = 1) 1(100)
Ciprofloxacin (n = 51) 8(15,1) 2(3,8) 41(80,4)
Clindamycin (n = 20) 7(35) 1(5) 12(60)
Cotrimoxazole (n = 2) 1(50) 1(50)
Erythromycin (n = 25) 7 (28) 18(72)
Gentamycin (n = 46) 19(41,3) 27(50,9)
Levofloxacin (n = 22) 4(18,2) 18(81,8)
Meropenem (n = 28) 24(85,7) 1(3,6) 3(10,7)
Netilmicin (n = 35) 14(40) 4(11,4) 17(48,6)
Penicillin (n = 3) 3(100)
Tigecycline (n = 47) 43(91,5) 4(8,5)
Tetracycline (n = 45) 15(33,3) 30(66,7)
Vancomycin (n = 25) 23(92) 2(8)
Cefoperazone (n = 4) 4(100)
Trimethoprim Sulfamethoxazole (n=42) 21(50) 21(50)
Aztreonam (n = 22) 1(4,5) 21(95,5)
Fosfomycin (n = 25) 15(60) 1(4) 9(36)
Moxifloxacin (n = 18) 4(22,2) 1(5,6) 13(72,2)
Note: S (sensitive); I (intermediate); R (resistant); SDD (Sensitive Dose Dependent)
It was found in this study that the sexes were balanced Based on the time of admission, in this study, 61.4% of
in number between men and women, namely 26 people patients were positive for blood culture after 48 hours. The
(50%) each. In a study by Christaki & Giamarellos-boubulis group of bloodstream infections can be divided into
in 2014, more of this disease was found in men with old age hospital-acquired infections (<48 hours), and out-of-hospital
or very young age. In terms of age, the largest age group in onset (<48 hours). This indicates the possibility that the
this study was 20-60 years (69.8%) with a large range of infection originated in the hospital.5
variation, and the average age was 54.69 years. In some
countries, including the classification by the Ministry of The use of CVC is routine in the ICU, due to the
Health in 2009, the average age group has been classified as patient's clinical condition and the need to include various
old age.4 types of therapy. In this study, approximately 84.6% of
patients had CVC installed and were positive for bacteremia.
Based on the time of admission, in this study, 61.4% of While the remaining 13.4% did not have a CVC installed
patients were positive for blood culture after 48 hours. The due to access to catheterization elsewhere, for example in
group of bloodstream infections can be divided into this case, patients with chronic kidney disease. Invasive
hospital-acquired infections (<48 hours), and out-of-hospital measures are one of the risk factors for bloodstream
onset (<48 hours). This indicates the possibility that the infections because they provide a port d'entree for
infection originated in the hospital. microorganisms. Rapid catheter change can reduce
bloodstream infections.1
IJISRT21JUL1032 www.ijisrt.com 1500
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
It was found that 48 people (92.30%) in this study production of plasmid-mediated beta lactamase which can
were using ventilators with various microorganisms. inactivate broad-spectrum cephalosporins, penicillins, and
According to Basetti in his study of bloodstream infections aztreonam.8 In this study alone, 3 samples (5.5%) of
in the ICU, the biggest risk factors for bloodstream patients with carbapenemase-producing Gram-negative rods
infections are length of stay, use of mechanical ventilation, were found, and 16 (30.2%) Gram negative ESBL-
surgical therapy, renal replacement therapy, and use of producing bacteria. It is known that the use of a ventilator
intravascular catheters. This statement is in line with the has a risk of contracting a person with positive ESBL
phenomenon found in this study where positive blood enterobacteriaceae, namely a group of Gram-negative rods
culture results were found in the study patients with an of about 5-20%. The most common microorganisms isolated
average length of stay of 8 days, the use of mechanical were Pseudomonas aeruginosa and Staphylococcus aureus,
ventilation around 92.30%, the use of CVC 84.6%, some but enterobacteriaceae such as Eschericia coli and Klebsiella
undergoing surgical therapy and hemodialysis.2 also reached almost 20%, in line with this study where
Klebsiela infection reached 20.8%, and when accumulated
The results of blood culture on all positive samples with other enterobacteriaceae it reached 41.2%. The high
showed that all of them were infected with 92.30 bacteria, of number of ESBL-producing Gram-negative rods in the ICU
which 52.8% of the samples were Gram-negative rods. In where there is an average resistance to third-generation
this study, the most common types of bacteria found were cephalosporins causes the Carbapenem group to be
Gram negative bacteria, this is in line with the pattern of suggested as the drug of choice for infection, but the
changes in bloodstream infections which used to be the presence of Carbapenemase-producing Gram-negative
majority of Gram positive.1 According to Basetti, of the bacteria makes this a concern.9
most isolated Gram negative bacteria, Escherichia coli,
Klebsiella pneumoniae, Acinetobacter baumanii , and The number of ESBL-producing bacteria in this study
Pseudomonas are often isolated in patients. This is in line was 30.2 percent. In a study conducted in France, ESBL
with this study where the previously mentioned colonization increased with the length of stay in the ICU,
microorganisms were among the samples obtained. i.e., an average period of more than five days, although not
Followed by the genus Staphylococcus with the most all patients who had ESBL colonization developed an
species in this study, namely Staphylococcus aureus. And infection. Klebsiella pneumonia itself is a bacterium that is a
the presence of Candida spp infection in one of the samples. flora commonly found in humans. Some isolates that were
This is in line with Basetti's statement regarding rarely found in this study were Burkholderia cepacia,
microorganisms in ICU patients, and shows a similar trend Burkholderia pseudomallei, Actinomyces odolynticus,
in various locations. Corynebacterium striatum, and Staphylococcus capitis
where these bacteria were found each of the 52 samples
One patient had multiple bacterial and fungal examined.
infections (Enterococcus faecium and Candida lucitanae).
The fungemia that occurred in the sample was a study that Burkholderia pseudomallei in the study sample was
suffered from acute peritonitis. According to Enoch, several found in a 59 year old man with diabetes mellitus who
factors causing invasive fungal infections are the use of suffered from pneumonia. This bacterium is a saprophytic
antineoplastic and immunosuppressants, broad - spectrum microorganism that is widely found in tropical soils and
antibiotics, prosthetic devices and grafts, as well as stagnant water. The risk factors for this disease are diabetes,
aggressive surgery. However, according to Wawrysiuk in a chronic alcoholism, and chronic kidney failure, and age over
2018 case report, Candida lusitaniae infection is a rare 50 years. An article by Abidin in 2017 about a case report of
infection. This fungus itself is often resistant to a patient with acute pneumonia due to Burkholderia
Amphotericin B. In the case report, it was reported that the pseudomallei found this infection in post-traumatic ICU
infection in the patient occurred intraperitoneally after patients where trauma was suspected as a port d'entree
laparoscopic surgery. In another study conducted by mechanism. In the case of culture research, it was carried
Rodolico, he found 66 cases of intra-abdominal infection by out on the sixth day of treatment, so that the criteria for this
Candida spp during a 5 year study.6 is a matter of debate.10
Based on the number of microorganisms isolated, the In the calculation to determine the relationship
most microorganisms found in this study were Klebsiella between hospital admissions, CVC installation, ventilator
pneumonia (20.8%), Staphylococcus aureus (15%), and installation, with a cumulative pattern, it was found that
Escherichia coli (11.2%). This is almost similar to the study there was no significant relationship. This is thought to be
by Edwardson although in a different order, where the most due to the heterogeneity of the sample so that there are many
bacteria isolated from blood was Staphylococcus aureus, possible biases. However, from the search for the types of
followed by Enterococcus spp, Serratia spp, and Klebsiella germs, it can be seen that the trend is in line with the various
spp.7 studies as described.
The incidence of Carbapenemase-producing Gram There are 33 types of antibiotics recorded that have
negative bacteria and Extended Spectrum Beta Lactamase been tested. Some of the most common antibiotics tested
(ESBL) is a threat in the ICU. Most Klebsiella pneumonia were Ciprofloxacin (51 times) with a sensitivity of 15.1%,
and Escherichia coli are resistant to ampicillin due to the Tigecycline (43 times) with a sensitivity of 91.5%,
IJISRT21JUL1032 www.ijisrt.com 1501
Volume 6, Issue 7, July – 2021 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Gentamycin (46 times) with a sensitivity of 41.3%, and [4]. Christaki E, Giamarellos-bourboulis EJ. The complex
Ampicillin Sulbactam (46 times) with sensitivity of 21.7%. pathogenesis of bacteremia From antimicrobial
From Thakuria's statement in his research regarding clearance mechanisms to the genetic background of the
antibiotic resistance in ventilator users, it was found that host. Landes Biosci. 2014;5(1):57–65.
there was a high sensitivity to the Tigecyline and Polymyxin [5]. Laupland KB. Incidence of bloodstream infection : a
B groups against Gram-negative isolates, and Vancomycin review of population-based studies. Clin Microbiol
against Gram-positive isolates. In that study it was also Infect [Internet]. 2013;19(6):492–500. Available from:
observed that the use of cephalosporins as first-line therapy http://dx.doi.org/10.1111/1469-0691. 12144
is very common despite the fact that their performance is
poor. In this study, the level of resistance to the [6]. Wawrysiuk S, Rechberger T, Futyma K, Miotła P.
cephalosporins themselves were Cefalexin (93.3%), Candida lusitaniae – A case report of an intraperitoneal
Cefazolin (89.7%), Ceftazidime (61.3%), Ceftriaxone infection. Prz Menopauzalny. 2018;17(2):94–6.
(78.6%), Cefuroxime (80%), while none were found. [7]. Edwardson S. Nosocomial infections in the ICU.
resistance to Cefotaxime and Cefixim. Cefixim alone was Anaesth Intensive Care Med [Internet].
only examined once in patients with positive Burkholderia 2018;20(1):14–8. Available from:
pseudomallei cultures.11 https://doi.org/10.1016/j.mpaic. 2018.11.004
[8]. Mahon CR, Lehman DC, Manuselis G. textbook of
In Gram positive isolates, the problem of MRSA is Diagnostic Microbiology. 5th ed. Missouri: elsevier;
also a matter of concern. The use of Vancomycin has also 2015.
increased because of this. In this study, the sensitivity of [9]. Pilmis B, Zahar J-R. Ventilator-associated pneumonia
vancomycin was 92%. According to Basetti from related to ESBL-producing gram negative bacilli. Ann
Tumbarello's writings, there was an increase in mortality Transl Med. 2018;6(20):424–424.
due to MRSA due to inadequate empiric antibiotics given.2 [10]. Zainal Abidin H, Muhd Besari A, Nadarajan C, Wan
Due to the high mortality and frequent finding of pathogen Shukeri WF, Mazlan MZ, Chong SE, et al. Acute
isolates which are considered difficult to treat according to bacteremic pneumonia due to melioidosis developing
various studies, as well as the large number of patients with in the intensive care setting. IDCases. 2017;8:63–5.
various dangerous comorbidities in the ICU, preventive [11]. Thakuria B, Singh P, Agrawal S, Asthana V. Profile of
measures must be taken to prevent this from happening. infective microorganisms causing ventilator-associated
Reducing transmission is one way to control outbreaks of pneumonia: A clinical study from resource limited
pathogenic MDR bacteria. There have been many protocols intensive care unit. J Anaesthesiol Clin Pharmacol.
regarding many safe ways such as standard catheter 2013;29(3):361–6.
insertion and management of care in patients in the ICU that
can reduce the incidence of bloodstream infections in the
ICU.
V. CONCLUSION
The most common types of bacteria found were Gram-
negative rods, followed by Gram-positive cocci, with the
highest number of bloodstream infections found after 48
hours of treatment. It is necessary to take preventive
measures and strengthen protocols in all actions to prevent
the transmission of dangerous pathogens, and periodic
evaluation and monitoring are necessary to protect patients
and health workers in the ICU.
REFERENCES
[1]. Viscoli C. Bloodstream infections : The peak of the
iceberg. Virulence [Internet]. 2016;7(3):248–51.
Available from:
http://dx.doi.org/10.1080/21505594.2016.1152440
[2]. Bassetti M, Righi E, Carnelutti A. Bloodstream
infections in the Intensive Care Unit. Virulence
[Internet]. 2016;7(3):267–79. Available from:
http://dx.doi.org/10.1080/21505594.2015.1134072
[3]. Mukhopadhyay C. Infection Control in Intensive Care
Units. Indian J Respir Care. 2018;7:14–21.
IJISRT21JUL1032 www.ijisrt.com 1502
You might also like
- 2019 CCS - Self ReviewDocument5 pages2019 CCS - Self ReviewKash Jamasali91% (22)
- Change Theory Project: University of Texas at Arlington Leadership and Management N4455 By: Jordan GossageDocument16 pagesChange Theory Project: University of Texas at Arlington Leadership and Management N4455 By: Jordan GossageInna NaraievskaNo ratings yet
- Private Health Institutions LawDocument22 pagesPrivate Health Institutions LawShankar Sanyal100% (1)
- CPG On CsomDocument8 pagesCPG On CsomRobert Ross DulayNo ratings yet
- Nstemi PathoDocument2 pagesNstemi PathoSheana TmplNo ratings yet
- Jurnal Interna 123456Document9 pagesJurnal Interna 123456vonnyandira28No ratings yet
- Molecular Diversity Analysis Using SSR MarkersDocument12 pagesMolecular Diversity Analysis Using SSR Markersrushi tahakikNo ratings yet
- Evolving Trends in Infective Endocarditis in A Developing Country: A Consequence of Medical Progress?Document9 pagesEvolving Trends in Infective Endocarditis in A Developing Country: A Consequence of Medical Progress?Hassan Abdi JamaNo ratings yet
- Accepted ManuscriptDocument23 pagesAccepted ManuscriptMrcom HvqyNo ratings yet
- PMID 36974854 OpportunisticDocument8 pagesPMID 36974854 Opportunisticajaya basnetNo ratings yet
- Bacteriological Profile and Antibiogram of Blood Culture Isolates From Paediatric Patients With Special Referenc..Document6 pagesBacteriological Profile and Antibiogram of Blood Culture Isolates From Paediatric Patients With Special Referenc..HArdik NegiNo ratings yet
- Utility of Previous Culture Results For Guiding Empirical Treatment of Sepsis in The Emergency DepartmentDocument6 pagesUtility of Previous Culture Results For Guiding Empirical Treatment of Sepsis in The Emergency Departmenteditorial.boardNo ratings yet
- Teori Eosinopenia DewasaDocument7 pagesTeori Eosinopenia DewasaNurlyanti RustamNo ratings yet
- Jurnal PilihanDocument7 pagesJurnal PilihanNovia khasanahNo ratings yet
- Bloodstream Infections in Hospitalized Children: Epidemiology and Antimicrobial SusceptibilitiesDocument4 pagesBloodstream Infections in Hospitalized Children: Epidemiology and Antimicrobial SusceptibilitiesrasioputraNo ratings yet
- 55-Article Text-103-1-10-20200408Document7 pages55-Article Text-103-1-10-20200408Kshitiz112No ratings yet
- Ceftri Vs StaphyDocument12 pagesCeftri Vs StaphyFarhan Athallah RafifNo ratings yet
- 2018 Article 2099Document10 pages2018 Article 2099igariok06No ratings yet
- Re 9Document6 pagesRe 9HArdik NegiNo ratings yet
- Jurnal Antibiotik Resistensi Pada Kasus OMSKDocument10 pagesJurnal Antibiotik Resistensi Pada Kasus OMSKAnonymous a2nxIq5No ratings yet
- JC On StenoDocument5 pagesJC On StenotanviaggrawalNo ratings yet
- MaybeDocument4 pagesMaybepertama bestNo ratings yet
- Brevundimonas Vesicularis Bacteremia Resistant To Trimethoprim-Sulfamethoxazole and Ceftazidime in A Tertiary Hospital in Southern TaiwanDocument5 pagesBrevundimonas Vesicularis Bacteremia Resistant To Trimethoprim-Sulfamethoxazole and Ceftazidime in A Tertiary Hospital in Southern TaiwanSihome ThodireNo ratings yet
- 2018 Article 3216Document7 pages2018 Article 3216Betty YayaNo ratings yet
- Ciz 1049Document9 pagesCiz 1049Justin WilliemNo ratings yet
- BJBMS 19 86Document8 pagesBJBMS 19 86overmegaNo ratings yet
- Diagnose of BSIDocument12 pagesDiagnose of BSIWong Chun ShengNo ratings yet
- Candidiasis in PICUDocument6 pagesCandidiasis in PICUMeirinda HidayantiNo ratings yet
- Bacteriological Profile of Blood Stream Infections at A Rural Tertiary Care Teaching Hospital of Western Uttar PradeshDocument9 pagesBacteriological Profile of Blood Stream Infections at A Rural Tertiary Care Teaching Hospital of Western Uttar PradeshHArdik NegiNo ratings yet
- A Study On Central Line Associated Bloodstream Infections (CLABSI) in Hemodialysis Patients at A Tertiary Care HospitalDocument6 pagesA Study On Central Line Associated Bloodstream Infections (CLABSI) in Hemodialysis Patients at A Tertiary Care HospitalOpenaccess Research paperNo ratings yet
- 2023 - Epidemiology and Outcomes of Hospital Acquired Bloodstream Infections in Intensive Care Unit Patients The EUROBACT 2Document13 pages2023 - Epidemiology and Outcomes of Hospital Acquired Bloodstream Infections in Intensive Care Unit Patients The EUROBACT 2giseladlrNo ratings yet
- The Surveillance of Antibiotics Resistance in Indonesia: A Current ReportsDocument6 pagesThe Surveillance of Antibiotics Resistance in Indonesia: A Current ReportsRahmanu ReztaputraNo ratings yet
- Bacterial and Fungal Coinfections in Covid 19 Patients Hospitalized During The New York City Pandemic SurgeDocument5 pagesBacterial and Fungal Coinfections in Covid 19 Patients Hospitalized During The New York City Pandemic SurgeReynaldo CarvajalNo ratings yet
- TBC y Shock SepticoDocument9 pagesTBC y Shock Septicogiseladelarosa2006No ratings yet
- CREMJHIDDocument9 pagesCREMJHIDAnggy de RinconNo ratings yet
- Venous Thromboembolism in Covid-19 ICU Patients: A Narrative ReviewDocument9 pagesVenous Thromboembolism in Covid-19 ICU Patients: A Narrative ReviewMarj MendezNo ratings yet
- Nac Etiologia Implicacion para La Seleccion de La Poblacion Diseño de Estudios Cid 2008Document4 pagesNac Etiologia Implicacion para La Seleccion de La Poblacion Diseño de Estudios Cid 2008Gustavo GomezNo ratings yet
- Antimicrobial Resistance of Pathogens Causing Nosocomial Bloodstream Infection in Hubei Province, China, From 2014 To 2016 A Multicenter Retrospective StudyDocument8 pagesAntimicrobial Resistance of Pathogens Causing Nosocomial Bloodstream Infection in Hubei Province, China, From 2014 To 2016 A Multicenter Retrospective StudyMrcom HvqyNo ratings yet
- JurnalDocument6 pagesJurnalAchmad YunusNo ratings yet
- Evaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalDocument6 pagesEvaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalEditor IJTSRDNo ratings yet
- Current Trends in The Epidemiologyof Nosocomial Bloodstream Infectionsin Patients With Hematological Malignanciesand Solid Neoplasms in Hospitalsin The United StatesDocument8 pagesCurrent Trends in The Epidemiologyof Nosocomial Bloodstream Infectionsin Patients With Hematological Malignanciesand Solid Neoplasms in Hospitalsin The United StatespaulaveronicaNo ratings yet
- العجز الكلوي والفطرياتDocument7 pagesالعجز الكلوي والفطرياتDhurghammNo ratings yet
- The Frequency of Influenza and Bacterial Co-Infection - A SystematDocument12 pagesThe Frequency of Influenza and Bacterial Co-Infection - A Systematrahma_husna_1No ratings yet
- Providencia StuartiiDocument7 pagesProvidencia StuartiiNoviaCandraDwipaNo ratings yet
- Bsi 29 JulDocument12 pagesBsi 29 JulDr Sumit KarNo ratings yet
- J. Clin. Microbiol.-2003-Weinstein-2275-8 - Blood Culture Contamination Persisting Problems and Partial Progress PDFDocument4 pagesJ. Clin. Microbiol.-2003-Weinstein-2275-8 - Blood Culture Contamination Persisting Problems and Partial Progress PDFmela renNo ratings yet
- Candidemia A Hospital Based Study in Haematological Patients in Adult Population of Northern IndiaDocument10 pagesCandidemia A Hospital Based Study in Haematological Patients in Adult Population of Northern IndiaAthenaeum Scientific PublishersNo ratings yet
- 10 1016@j Jaad 2019 05 096Document8 pages10 1016@j Jaad 2019 05 096JohnNo ratings yet
- Adjunctive Dexamethasone Therapy in Unconfirmed Bacterial Meningitis in Resource Limited Settings: Is It A Risk Worth Taking?Document8 pagesAdjunctive Dexamethasone Therapy in Unconfirmed Bacterial Meningitis in Resource Limited Settings: Is It A Risk Worth Taking?Tofik HusseinNo ratings yet
- Antibiotics 11 01326 v2Document10 pagesAntibiotics 11 01326 v2hawamasfufahNo ratings yet
- (03241750 - Acta Medica Bulgarica) Fungal Peritonitis Due To Gastroduodenal Perforation - Diagnostic and Treatment ChallengesDocument8 pages(03241750 - Acta Medica Bulgarica) Fungal Peritonitis Due To Gastroduodenal Perforation - Diagnostic and Treatment ChallengesTeodorNo ratings yet
- Advani 2024 Oi 240106 1709228327.56877Document12 pagesAdvani 2024 Oi 240106 1709228327.56877Dora Maria Guadamuz MoralesNo ratings yet
- Antibiotico CovidDocument12 pagesAntibiotico CovidPaul ArtigasNo ratings yet
- Cryptococcal Infection in Plhiv: Series of 12 Cases at The Laboratory of Mohammed Vi University Hospital of MarrakechDocument6 pagesCryptococcal Infection in Plhiv: Series of 12 Cases at The Laboratory of Mohammed Vi University Hospital of MarrakechIJAR JOURNALNo ratings yet
- Journal 1Document4 pagesJournal 1Alberto TaolinNo ratings yet
- Wiley Cbin.11440Document10 pagesWiley Cbin.11440RK VermaNo ratings yet
- Cell-Based Therapy To Reduce Mortality From COVID-19Document16 pagesCell-Based Therapy To Reduce Mortality From COVID-19Chelsea Shannen Marie CarreonNo ratings yet
- Usefulness of Presepsin As A Diagnostic and Prognostic Marker of Sepsis in Daily Clinical PracticeDocument7 pagesUsefulness of Presepsin As A Diagnostic and Prognostic Marker of Sepsis in Daily Clinical Practicefaraz.mirza1No ratings yet
- Sepsis 1Document17 pagesSepsis 1lizzie clavijoNo ratings yet
- Articulos 2Document8 pagesArticulos 2Alejandro Andrés Salazar GuzmánNo ratings yet
- Espondilodiscitis Infecciosa Por Patógenos Poco ComunesDocument5 pagesEspondilodiscitis Infecciosa Por Patógenos Poco ComunesOthoniel RamirezNo ratings yet
- Journal of Clinical Microbiology-2011-Wolk-S62.fullDocument6 pagesJournal of Clinical Microbiology-2011-Wolk-S62.fullAli AhmedNo ratings yet
- Ejifcc 27 147Document9 pagesEjifcc 27 147Riski Nur RamadhaniNo ratings yet
- 80 Iajps80122017 PDFDocument4 pages80 Iajps80122017 PDFBaru Chandrasekhar RaoNo ratings yet
- A Proposed Model for Fainting People Detection Using Media Pipe TechnologyDocument4 pagesA Proposed Model for Fainting People Detection Using Media Pipe TechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Automatic Essay Scoring with Context-based Analysis with Cohesion and CoherenceDocument8 pagesAutomatic Essay Scoring with Context-based Analysis with Cohesion and CoherenceInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Design Information Security in Electronic-Based Government Systems Using NIST CSF 2.0, ISO/IEC 27001: 2022 and CIS ControlDocument8 pagesDesign Information Security in Electronic-Based Government Systems Using NIST CSF 2.0, ISO/IEC 27001: 2022 and CIS ControlInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Making and Assessing an Antibacterial Cream with Dalbergia Sissoo Leaf ExtractDocument9 pagesMaking and Assessing an Antibacterial Cream with Dalbergia Sissoo Leaf ExtractInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Teaching in “The “Land of Smile”: Anecdote of Filipino Substitute Teachers in ThailandDocument5 pagesTeaching in “The “Land of Smile”: Anecdote of Filipino Substitute Teachers in ThailandInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Role of Haematological Indices, Interleukin-10, Tumour Necrosis Factor and Vascular Endothelial Growth Factor on Gastric Ulcer Healing in Obese Wistar Rats: Effect of Garlic OilDocument13 pagesRole of Haematological Indices, Interleukin-10, Tumour Necrosis Factor and Vascular Endothelial Growth Factor on Gastric Ulcer Healing in Obese Wistar Rats: Effect of Garlic OilInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Evaluating the Performance of Vapor Compression Cycle by Adding NanoparticleDocument12 pagesEvaluating the Performance of Vapor Compression Cycle by Adding NanoparticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Temperature Call Alert to Prevent Child Death from Heatstroke in Smart Car using IoTDocument12 pagesTemperature Call Alert to Prevent Child Death from Heatstroke in Smart Car using IoTInternational Journal of Innovative Science and Research Technology100% (2)
- Exploring Well-being in College Students: The Influence of Resilience and Social SupportDocument11 pagesExploring Well-being in College Students: The Influence of Resilience and Social SupportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Human-Computer Interaction in Cloud SystemsDocument6 pagesHuman-Computer Interaction in Cloud SystemsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparative Cognitive Performance of 60-Year-Old Asian and Western Pilots on the CogScreen Test: A Cross-Sectional StudyDocument6 pagesComparative Cognitive Performance of 60-Year-Old Asian and Western Pilots on the CogScreen Test: A Cross-Sectional StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical Approach to Advanced Mantle Cell Lymphoma: A Detailed Case AnalysisDocument5 pagesClinical Approach to Advanced Mantle Cell Lymphoma: A Detailed Case AnalysisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- ALBULARYO: Advanced Learning for Botanical Understanding, Leveraging Artificial Recognition using Convolutional Neural NetworksDocument5 pagesALBULARYO: Advanced Learning for Botanical Understanding, Leveraging Artificial Recognition using Convolutional Neural NetworksInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Thickness CipherDocument3 pagesThickness CipherInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Optimizing Textual Regulation Interpretation for Maximum ImpactDocument5 pagesOptimizing Textual Regulation Interpretation for Maximum ImpactInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Teacher Humor Style and Attention Span of Grade 7 StudentsDocument5 pagesTeacher Humor Style and Attention Span of Grade 7 StudentsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Promotion and Brand Awareness Analysis of Purchase Intention Sharp Brand Smart TVs in Surabaya TimurDocument7 pagesPromotion and Brand Awareness Analysis of Purchase Intention Sharp Brand Smart TVs in Surabaya TimurInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Store Atmosphere and Customer Experience on Consumer Purchasing Decisions of KFC Wahidin GresikDocument5 pagesThe Impact of Store Atmosphere and Customer Experience on Consumer Purchasing Decisions of KFC Wahidin GresikInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Digital Literacy and Critical Thinking Skills Among Grade 5 LearnersDocument4 pagesDigital Literacy and Critical Thinking Skills Among Grade 5 LearnersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Rise of Advanced VTS/VTMS SystemsDocument14 pagesThe Rise of Advanced VTS/VTMS SystemsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- An Appraisal of Employable Content of the National Diploma in Architectural Technology Program in North East NigeriaDocument5 pagesAn Appraisal of Employable Content of the National Diploma in Architectural Technology Program in North East NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Conceptualized Fusion Reactor based on Gas Turbine with High Temperature CO2Document7 pagesConceptualized Fusion Reactor based on Gas Turbine with High Temperature CO2International Journal of Innovative Science and Research TechnologyNo ratings yet
- Role of Environmental Accounting in Promoting Sustainable Business Practices A Case Study of Turkana County, KenyaDocument7 pagesRole of Environmental Accounting in Promoting Sustainable Business Practices A Case Study of Turkana County, KenyaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Multinational Telecommunication Companies as a Moderator to Achieve Sustainable Development Considering Standard of Living and Digital Education in Sri LankaDocument11 pagesThe Multinational Telecommunication Companies as a Moderator to Achieve Sustainable Development Considering Standard of Living and Digital Education in Sri LankaInternational Journal of Innovative Science and Research Technology100% (1)
- The Expanding Attack Surface: Securing AI and Machine Learning Systems in Security OperationsDocument8 pagesThe Expanding Attack Surface: Securing AI and Machine Learning Systems in Security OperationsInternational Journal of Innovative Science and Research Technology100% (1)
- Human Resource Functions: Examining Insights from ABC Research OrganizationDocument9 pagesHuman Resource Functions: Examining Insights from ABC Research OrganizationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of the Commercial Agriculture Credit Scheme (CACS) on the Agricultural Economy of Nigeria and its Total Output (2015-2019)Document8 pagesThe Impact of the Commercial Agriculture Credit Scheme (CACS) on the Agricultural Economy of Nigeria and its Total Output (2015-2019)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Assessing Fine-Tuning Efficacy in LLMs: A Case Study with Learning Guidance ChatbotsDocument11 pagesAssessing Fine-Tuning Efficacy in LLMs: A Case Study with Learning Guidance ChatbotsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Teacher-Induced Academic Stress: Predicting Eating Behavior Problems in College StudentsDocument8 pagesTeacher-Induced Academic Stress: Predicting Eating Behavior Problems in College StudentsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Barriers to Natural Disaster Risks Management Within Coastal Communities: The Case of Limbe and Ideneau in CameroonDocument11 pagesBarriers to Natural Disaster Risks Management Within Coastal Communities: The Case of Limbe and Ideneau in CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- About Blood CellsDocument5 pagesAbout Blood CellsJoshua RaviNo ratings yet
- Endometriosis-An Enigma (Seema Chopra (Editor) )Document199 pagesEndometriosis-An Enigma (Seema Chopra (Editor) )Anna PodsiadłoNo ratings yet
- Treating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionDocument12 pagesTreating Vulvovaginal Atrophy Genitourinary Syndrome of Menopause How Important Is Vaginal Lubricant and Moisturizer CompositionPELVIC ANGELNo ratings yet
- Case Log TotalsDocument6 pagesCase Log Totalsnatalie nodayNo ratings yet
- ScoliosisDocument122 pagesScoliosisCatalina Elena González CarvajalNo ratings yet
- Pneumonia PathophysiologyDocument1 pagePneumonia PathophysiologyDee Sarajan100% (3)
- CLR 12021Document63 pagesCLR 12021Eliza DNNo ratings yet
- Ventilator-Associated Pneumonia: Intensive Care Tutorial382Document6 pagesVentilator-Associated Pneumonia: Intensive Care Tutorial382mariskaNo ratings yet
- Pelvic Physical Therapy For Chronic Pain and Dysfunction FollowinDocument13 pagesPelvic Physical Therapy For Chronic Pain and Dysfunction Followincode PVSNo ratings yet
- Factors Influencing Folic Acid and Iron Supplement Use Among Pregnant Women at Hoima Regional Referral Hospital in UgandaDocument10 pagesFactors Influencing Folic Acid and Iron Supplement Use Among Pregnant Women at Hoima Regional Referral Hospital in UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
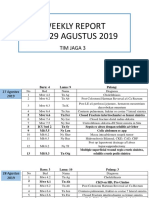
- WR Tim Jaga 3Document285 pagesWR Tim Jaga 3VincentiusNo ratings yet
- LEC#34 Anti Helimintic DrugsDocument17 pagesLEC#34 Anti Helimintic Drugsalihyderabro166No ratings yet
- نموذج الامتيازات السريريةDocument67 pagesنموذج الامتيازات السريريةSAFA ALYNo ratings yet
- Digestive 7Document1 pageDigestive 7MA. LOURDES S. PALERNo ratings yet
- IPCR July Dec 2020 FINAL Na KaauDocument7 pagesIPCR July Dec 2020 FINAL Na KaauCristina MelloriaNo ratings yet
- Handbook of OrthodonticsDocument1 pageHandbook of OrthodonticsCarlos Alberto CastañedaNo ratings yet
- Journal Reading - Allergic Rhinitis - Safira AmaliaDocument34 pagesJournal Reading - Allergic Rhinitis - Safira AmaliasafiraNo ratings yet
- Pediatric Cardiology Thesis TopicsDocument4 pagesPediatric Cardiology Thesis Topicspzblktgld100% (2)
- Studi Kasus LAINNYA PDFDocument3 pagesStudi Kasus LAINNYA PDFElgaNo ratings yet
- Lower Extremity AmputationsDocument42 pagesLower Extremity Amputationsalinutza_childNo ratings yet
- Probiotics, Prebiotics and Synbiotics - A ReviewDocument12 pagesProbiotics, Prebiotics and Synbiotics - A ReviewluthfikhairulNo ratings yet
- Mental Health: Unit - 1Document17 pagesMental Health: Unit - 1Ramandeep KaurNo ratings yet
- Микра Англ 1 ЧастьDocument33 pagesМикра Англ 1 ЧастьAuthentic IdiotNo ratings yet
- Occupational Safety and HealthDocument9 pagesOccupational Safety and HealthWan SaitamaNo ratings yet
- Naturopathy 02 Hydrotherapy (I)Document48 pagesNaturopathy 02 Hydrotherapy (I)Ashisha Kaushal100% (1)