Professional Documents
Culture Documents
The Art of Medicine: Trial and Error
The Art of Medicine: Trial and Error
Uploaded by
MuhCopyright:
Available Formats
You might also like
- DR Breath by Carl Stough PDFDocument128 pagesDR Breath by Carl Stough PDFJuan Vizán86% (7)
- Gray Matter: A Neurosurgeon Discovers the Power of Prayer . . . One Patient at a TimeFrom EverandGray Matter: A Neurosurgeon Discovers the Power of Prayer . . . One Patient at a TimeRating: 4 out of 5 stars4/5 (37)
- Sentimental Medicine PDFDocument8 pagesSentimental Medicine PDF杨飞燕No ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineSuwandi ChangNo ratings yet
- Physical Diagnosis of Pain An Atlas of Signs and Symptoms 3rd Edition CompressDocument369 pagesPhysical Diagnosis of Pain An Atlas of Signs and Symptoms 3rd Edition CompressProsenjit MajiNo ratings yet
- NEJMp2402006Document2 pagesNEJMp2402006crazycrane12321No ratings yet
- Nej MP 2011418Document3 pagesNej MP 2011418The Dark DreamerNo ratings yet
- Full Download Book Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition PDFDocument41 pagesFull Download Book Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition PDFola.sumrall565100% (24)
- Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition Waldman MD JD All ChapterDocument67 pagesPhysical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition Waldman MD JD All Chapterkevin.roberts692100% (11)
- What I Do Not Tell The Medical StudentDocument2 pagesWhat I Do Not Tell The Medical StudentMohan PrasadNo ratings yet
- Hypnosis in The Emergency Department BIERMANDocument5 pagesHypnosis in The Emergency Department BIERMANAyoub LilouNo ratings yet
- Learning To TalkDocument2 pagesLearning To Talkgeochu02No ratings yet
- Lévinas - A Doutrine For DoctorsDocument2 pagesLévinas - A Doutrine For DoctorsTássia MatosNo ratings yet
- Unexpected Closure: PerspectiveDocument3 pagesUnexpected Closure: PerspectivePatrick CommettantNo ratings yet
- VR TherapyDocument5 pagesVR TherapyHec ChavezNo ratings yet
- Atbaseline NejmDocument2 pagesAtbaseline NejmSandeep SasidharanNo ratings yet
- Direct Red: A Surgeon's View of Her Life-or-Death ProfessionFrom EverandDirect Red: A Surgeon's View of Her Life-or-Death ProfessionRating: 3.5 out of 5 stars3.5/5 (31)
- Battlefield Acupuncture: My Story: EditorialDocument2 pagesBattlefield Acupuncture: My Story: Editorialyan92120No ratings yet
- Cap 2023 01 01Document51 pagesCap 2023 01 01Yaser MNo ratings yet
- Piis0140673699903914 2Document1 pagePiis0140673699903914 2Aditi S MathNo ratings yet
- Positional Cervical Cord Compression Fibromyalgia PaperDocument7 pagesPositional Cervical Cord Compression Fibromyalgia PaperValiant LordNo ratings yet
- Sri Magazine 2017Document68 pagesSri Magazine 2017Moosa Babul M37No ratings yet
- Emergency Medicine MotrelyDocument4 pagesEmergency Medicine MotrelyOsman PazNo ratings yet
- The World of Medical Transcription - A Broad Perspective From A Team Approach PDFDocument0 pagesThe World of Medical Transcription - A Broad Perspective From A Team Approach PDFAgung Budiman Agustinus SilalahiNo ratings yet
- Bedell 04 Words That HarmDocument4 pagesBedell 04 Words That HarmR.L. BandaNo ratings yet
- Pendular Diagnosis - From Dowsing To Diagnostic MethodologyDocument7 pagesPendular Diagnosis - From Dowsing To Diagnostic MethodologyVijay MuthekarNo ratings yet
- Boundaries of Evolution: What Would Darwin Think Now About Dna, the Big Bang, and Finite Time?From EverandBoundaries of Evolution: What Would Darwin Think Now About Dna, the Big Bang, and Finite Time?No ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicinedavideNo ratings yet
- Honey, Mud, Maggots and Other Medical Marvels: by R. and M. Root-BernsteinDocument1 pageHoney, Mud, Maggots and Other Medical Marvels: by R. and M. Root-BernsteinAndrei BombardieruNo ratings yet
- ARTÍCULOSDocument308 pagesARTÍCULOSDavid OlveraNo ratings yet
- Patient's Cures His Snoring: The EditorDocument1 pagePatient's Cures His Snoring: The EditorDiegoNo ratings yet
- Jaocr: Emergency RadiologyDocument38 pagesJaocr: Emergency Radiologyasp annishyaNo ratings yet
- Tales From The Temporal Lobes: PerspectiveDocument3 pagesTales From The Temporal Lobes: PerspectiveDini CahyaNo ratings yet
- Quick Physical Exam PDFDocument2 pagesQuick Physical Exam PDFffocussNo ratings yet
- 2004, Vol.6, No.4, Pediatric Surgery PDFDocument95 pages2004, Vol.6, No.4, Pediatric Surgery PDFAnty Dewi Sarty RanyabarNo ratings yet
- The Emperor's New Clothes: A Critical Appraisal of Evidence-Based MedicineDocument9 pagesThe Emperor's New Clothes: A Critical Appraisal of Evidence-Based MedicineCarlos Antonio Párraga GómezNo ratings yet
- A New Leadership Curriculum: The Multiplication of IntelligenceDocument4 pagesA New Leadership Curriculum: The Multiplication of IntelligenceGisele PhaloNo ratings yet
- Jamainternal Heger 2023 PP 230001 1681398072.43626Document2 pagesJamainternal Heger 2023 PP 230001 1681398072.43626Paola Cristini Gama SilvaNo ratings yet
- Mutation Research/Reviews in Mutation Research: Narendra P. SinghDocument8 pagesMutation Research/Reviews in Mutation Research: Narendra P. SinghAndrea bedoya vasquezNo ratings yet
- Nursing Care Plan Endometrial CancerDocument2 pagesNursing Care Plan Endometrial Cancerderic88% (16)
- Burnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBADocument3 pagesBurnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBALeon BosnjakNo ratings yet
- Ofri - Medical Humanities - Week1Document2 pagesOfri - Medical Humanities - Week1isabella brantonNo ratings yet
- Osborne 1928Document1 pageOsborne 1928lam lamNo ratings yet
- General IandsDocument4 pagesGeneral IandsScooterKatNo ratings yet
- Cranial Manipulative TherapyDocument6 pagesCranial Manipulative Therapypurple112650% (2)
- College Essay Example #3: This Is A College Essay That Worked ForDocument2 pagesCollege Essay Example #3: This Is A College Essay That Worked ForCristian ArevaloNo ratings yet
- Aim4pg Magazine July December 2019Document27 pagesAim4pg Magazine July December 2019AnirbanMallikNo ratings yet
- #Pendular Diagnosis - From Dowsing To Diagnostic MetholologyDocument7 pages#Pendular Diagnosis - From Dowsing To Diagnostic MetholologyAivlys100% (1)
- The CaseDocument2 pagesThe Casetemp3rarNo ratings yet
- Neurypnology - JamesBraidDocument296 pagesNeurypnology - JamesBraidCarlNo ratings yet
- HOLOMBE What Is Homoeopathy A New Exposition of A Great Truth!Document28 pagesHOLOMBE What Is Homoeopathy A New Exposition of A Great Truth!Bharatibhushan NayakNo ratings yet
- A Manual of Instruction For Giving Swedish Movement and Massage 1889Document1 pageA Manual of Instruction For Giving Swedish Movement and Massage 1889Davide Di GiacomoNo ratings yet
- GNM Schizophrenic Constellations en MarkolinDocument107 pagesGNM Schizophrenic Constellations en MarkolinAngela LovarcoNo ratings yet
- Complete Autopsy PDFDocument6 pagesComplete Autopsy PDFJAVIER ERNESTO CAÑON FRIASNo ratings yet
- ECI-B14Fx: 4 MP Outdoor IR Network Bullet CameraDocument3 pagesECI-B14Fx: 4 MP Outdoor IR Network Bullet CameraMuhNo ratings yet
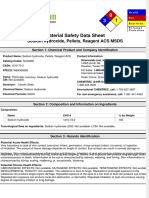
- Material Safety Data Sheet: Sodium Hydroxide, Pellets, Reagent ACS MSDSDocument6 pagesMaterial Safety Data Sheet: Sodium Hydroxide, Pellets, Reagent ACS MSDSMuhNo ratings yet
- Material Safety Data Sheet: Hydrochloric Acid, 37% MSDSDocument8 pagesMaterial Safety Data Sheet: Hydrochloric Acid, 37% MSDSMuhNo ratings yet
- SARS CoV 2 and Influenza Virus Co Infection - 2020 - The LancetDocument1 pageSARS CoV 2 and Influenza Virus Co Infection - 2020 - The LancetMuhNo ratings yet
- Shell Helix Ultra Professional AJ-L 0W-20: Main Applications Specifications, Approvals & RecommendationsDocument2 pagesShell Helix Ultra Professional AJ-L 0W-20: Main Applications Specifications, Approvals & RecommendationsMuhNo ratings yet
- Best Motor Oil For Hyundai Tucson (2021 Professional Review) Hyundai Tucson Engine Oil Recommendations - OilapDocument23 pagesBest Motor Oil For Hyundai Tucson (2021 Professional Review) Hyundai Tucson Engine Oil Recommendations - OilapMuhNo ratings yet
- Bpxe AbjfycDocument2 pagesBpxe AbjfycMuhNo ratings yet
- Product Information: Special Tec AA 10W-30 BenzinDocument1 pageProduct Information: Special Tec AA 10W-30 BenzinMuhNo ratings yet
- Shell Helix Ultra 5W-40: Performance, Features & BenefitsDocument2 pagesShell Helix Ultra 5W-40: Performance, Features & BenefitsMuhNo ratings yet
- EDGE Extended Performance: DescriptionDocument3 pagesEDGE Extended Performance: DescriptionMuhNo ratings yet
- Castrol EDGE 5W-30 A5/B5: DescriptionDocument2 pagesCastrol EDGE 5W-30 A5/B5: DescriptionMuhNo ratings yet
- 1ph Hybrid Solar Inverter (1000va - 5000va) - Farber PowerDocument4 pages1ph Hybrid Solar Inverter (1000va - 5000va) - Farber PowerMuhNo ratings yet
- Bpxe 9P9HK3Document2 pagesBpxe 9P9HK3MuhNo ratings yet
- Bpxe 9pu2leDocument3 pagesBpxe 9pu2leMuhNo ratings yet
- Safety Data Sheet: Ubstance and Ource DentificationDocument6 pagesSafety Data Sheet: Ubstance and Ource DentificationMuhNo ratings yet
- Specification: Model FA-MPCHR-12V-300W FA-MPCHR-12V/24V-600W FA-MPCHR-36V-850W FA-MPCHR-12V/48V-3000W InputDocument1 pageSpecification: Model FA-MPCHR-12V-300W FA-MPCHR-12V/24V-600W FA-MPCHR-36V-850W FA-MPCHR-12V/48V-3000W InputMuhNo ratings yet
- Safety Data Sheet Xylene: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingDocument9 pagesSafety Data Sheet Xylene: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingMuhNo ratings yet
- Specification: Model Number FA-OFFINVX-24V-3000VA FA-OFFINVX-48V-5000VADocument1 pageSpecification: Model Number FA-OFFINVX-24V-3000VA FA-OFFINVX-48V-5000VAMuhNo ratings yet
- Safety Data SheetDocument7 pagesSafety Data SheetMuhNo ratings yet
- Safety Data Sheet: Section 1. IdentificationDocument12 pagesSafety Data Sheet: Section 1. IdentificationMuhNo ratings yet
- 19 - 1391926836 - N Butanol CASNO 71 36 3 MSDSDocument7 pages19 - 1391926836 - N Butanol CASNO 71 36 3 MSDSMuhNo ratings yet
- Heart and Circulation Test: NameDocument12 pagesHeart and Circulation Test: NamezipperNo ratings yet
- Silverglide Surgical TechnologiesDocument2 pagesSilverglide Surgical TechnologiesDhruv GandhiNo ratings yet
- Lecture 13 - Extraction of ToothDocument46 pagesLecture 13 - Extraction of Toothvanesa AvramovaNo ratings yet
- 3-Hypothenar Hammer SyndromeDocument22 pages3-Hypothenar Hammer SyndromeProfesseur Christian DumontierNo ratings yet
- Resume 1Document2 pagesResume 1api-400253936No ratings yet
- 50 Topics List 1Document1 page50 Topics List 1akanksha singhNo ratings yet
- Anatomy of The Scalp!Document5 pagesAnatomy of The Scalp!GE EKNo ratings yet
- SurgicalTipsandTricksDuringUrethroplastyforBulbarUrethralStricturesFocusingonAccurateLocalisationoftheStricture ResultsfromaTertiaryCentreDocument8 pagesSurgicalTipsandTricksDuringUrethroplastyforBulbarUrethralStricturesFocusingonAccurateLocalisationoftheStricture ResultsfromaTertiaryCentreTomek RNo ratings yet
- Aortic Valve ReplacementDocument17 pagesAortic Valve Replacementm_alodat6144No ratings yet
- Orthopaedics Assessment: Oncology Division: Dr. Reza Devianto Hambali Dr. Arief Abidin Dr. A.S. Marsahala LumbantobingDocument44 pagesOrthopaedics Assessment: Oncology Division: Dr. Reza Devianto Hambali Dr. Arief Abidin Dr. A.S. Marsahala LumbantobingReza Devianto HambaliNo ratings yet
- Growing Beans Handout - Plant Growth Scientific ExperimentDocument2 pagesGrowing Beans Handout - Plant Growth Scientific ExperimentMariah Alexis EncinaNo ratings yet
- Yang - A New Trick To A Routine Procedure Taking The Fear Out of The Axillary Vein Stick Using The 35' Caudal View - Europace 2015Document4 pagesYang - A New Trick To A Routine Procedure Taking The Fear Out of The Axillary Vein Stick Using The 35' Caudal View - Europace 2015Gabriel JoséNo ratings yet
- Surface Anatomy: David Ebenezer Department of Anatomy Velammal Medical CollegeDocument101 pagesSurface Anatomy: David Ebenezer Department of Anatomy Velammal Medical CollegeKarishma RameshNo ratings yet
- Id QuestionDocument67 pagesId QuestionRahul PradeepNo ratings yet
- Information About Stapedectomy and OtosDocument10 pagesInformation About Stapedectomy and Otosiangould12No ratings yet
- 1 El Alto Origen de La Arteria Radial (Arteria Braquiorradial)Document11 pages1 El Alto Origen de La Arteria Radial (Arteria Braquiorradial)Juan José CabezasNo ratings yet
- Test Bank For Maternity and Womens Health Care 11th Edition by LowdermilkDocument11 pagesTest Bank For Maternity and Womens Health Care 11th Edition by Lowdermilkdonnadaviskjqpxitacn100% (32)
- Georgopoulos Study July 08 PDFDocument9 pagesGeorgopoulos Study July 08 PDFCarlos Julián Ortiz DallosNo ratings yet
- Nerves of Upper LimbDocument13 pagesNerves of Upper LimbHafiz NaveedNo ratings yet
- Anesthesia Side EffectsDocument10 pagesAnesthesia Side EffectsPADAYON MEDISINANo ratings yet
- Miniaturized Reveal LINQ Insertable Cardiac MonitoDocument7 pagesMiniaturized Reveal LINQ Insertable Cardiac MonitoLetícia JanuziNo ratings yet
- Series Coding Certification TipsDocument11 pagesSeries Coding Certification TipsJUNAID RAHMANNo ratings yet
- Hernia QuestionsDocument6 pagesHernia QuestionsNica Lopez Fernandez100% (1)
- Krukenberg Amputation & Its ManagementDocument12 pagesKrukenberg Amputation & Its ManagementSIBASIS PATTANAYAKNo ratings yet
- 1.4 B Tija Centromedulara PFN LungDocument18 pages1.4 B Tija Centromedulara PFN LungGhica CostinNo ratings yet
- 422 Lab 2Document8 pages422 Lab 2kurucz barbaraNo ratings yet
- Imtiaz Notes Main-1-1Document8 pagesImtiaz Notes Main-1-1Dr Afzal HussainNo ratings yet
- Cardiopulmonary Bypass: Learning ObjectivesDocument5 pagesCardiopulmonary Bypass: Learning ObjectivesAnonymous zPwXqwNo ratings yet
- Extraction of Wisdom Teeth Under General Anesthesia-A StudyDocument5 pagesExtraction of Wisdom Teeth Under General Anesthesia-A StudyCiutac ŞtefanNo ratings yet
- Endobutton™ CL Ultra: Fixation DeviceDocument6 pagesEndobutton™ CL Ultra: Fixation Deviceapi-19808945No ratings yet
The Art of Medicine: Trial and Error
The Art of Medicine: Trial and Error
Uploaded by
MuhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Art of Medicine: Trial and Error
The Art of Medicine: Trial and Error
Uploaded by
MuhCopyright:
Available Formats
Perspectives
The art of medicine
Trial and error
Two decades ago, the estimation that a jumbo jet’s were pressuring. Blood pressures skyrocketed. Urine
worth of Americans were tumbling out of the skies every outputs ground to a halt.
single day due to our medical errors grabbed headlines As I observed these sessions, I thought back to my own
and jumpstarted the modern patient safety movement. training, and how desperately I had yearned for some sort
To Err is Human—the seminal report on medical error of safe zone for my first tentative medical steps. I longed
from the Institute of Medicine, now the US National for a trial run to test out my doctoring, but alas, there was
Academy of Medicine—detonated like a bomb. Ever only the vérité of the hospital ward and the living, breathing
since then, the medical world has been scrambling patients who populated it.
to find ways to decrease medical error and improve One evening on call, well before a medical diploma had
patient safety. Hospital systems have been redesigned. made contact with my eager palm, one of our patients
Electronic medical record systems have been installed needed a central line. He had run out of usable peripheral
nearly universally. Checklists are ubiquitous. And every veins, but still required several more days of intravenous
committee, document, and process now has the word antibiotics, so a central line was in order. My supervising
“quality” mandatorily embedded somewhere within. resident decided that there was no time like the present for
One of the most far-reaching developments has a newbie to learn.
been the use of simulation training. While we’ve In the sprawling Veterans Affairs (VA) Hospital where I
always used some modicum of simulation training was doing my rotation, the patients were largely tolerant
in medicine (remember those Resusci Anne dolls for of trainee doctors, although this was probably because
learning cardiopulmonary resuscitation and mouth-to- trainees were pretty much the only medical personnel they
mouth resuscitation?), the breadth and sophistication ever saw.
of simulation have exploded in the 20 years since the And so that’s how I found myself aiming a dismayingly
publication of To Err is Human. It is now integral to nearly mammoth needle at the jugular vein of a Vietnam veteran
every aspect of medical education. who was respiring patiently under a cornflower-blue
As part of my research for the book When We Do Harm: surgical drape. Palpating my way up the patient’s neck to
A Doctor Confronts Medical Error, I spent time observing the point of entry, I glanced up at my resident with one last,
simulation sessions. They were remarkable in their fraught, “Are you sure?” look. He reassured me with what
intricacy and relevance, offering simulations for obtaining seemed to be the universal answer to any medical student
consent, for giving bad news, for doing procedures, and concern: “This is a teaching hospital.”
for middle-of-the-night clinical decompensation. The I’ll never know what the patient thought about all
simulated patients were short of breath. Their significant this, or if he truly understood just how verdant my
others were anxious and demanding. Team members greenhorn status was. (The Krebs cycle was still in my
working memory, if that gives you any hint.) But forward
I ploughed, literally.
Sweating bullets, I aimed the tip of the needle lateral to
the carotid pulse, whispered a prayer to whichever deity was
on call that night, and sank the needle deep into the terra
incognita of my patient’s neck.
The tidepools of perspiration on my scrubs were
mushrooming, but my resident was as cool as a cucumber,
calmly walking me through the steps. “Don’t cause an
air embolus”, he said casually, as I began to thread in the
guidewire, something that seemed far too metallic to be
slithering into my patient. “And don’t let go of your end of
Amelie-Benoist/BSIP/Science Photo Library
the wire”, he added, almost offhandedly.
Witnessing a foreign object—one dispatched from my
own, medically uncallused hands—sink ever deeper into the
impossible depths of a real live human being was becoming
more than I could bear. I just wanted this to be over.
I began threading the snake-like catheter over the
guidewire into the seemingly endless internal jugular
1538 www.thelancet.com Vol 395 May 16, 2020
Perspectives
vein. “Oh, and just make sure you don’t hit the right It’s certainly possible that our patients back then—as
atrium”, my resident added, stifling a yawn. His they hopefully also do now—benefited from the heavier
preternatural calm was unnerving. My own blood dose of energy, enthusiasm, and academic verve that a
pressure was dipping low enough to require dobutamine, teaching hospital can generate compared with a non-
but I don’t think his pulse nudged north of 60. teaching hospital. But when it came to being guinea pigs
We were finally coming close to the end, and my on the steeper portion of our learning curves, there’s no
resident began cleaning up our supplies. He seemed doubt that our patients endured additional—and frankly
reasonably satisfied with my performance, and so I unnecessary—misery. (Surely no patients suffered
cautiously exhaled a few millilitres of pent-up breath. more in the history of medicine than the first three
“Just push in the saline flushes and we’ll be done”, he upon whose radial arteries I strove to draw an arterial
said, with a quick glance at his watch. And then my fear blood gas).
officially polymerised into true panic. Flushes? What was Perhaps during the COVID-19 pandemic, health
he talking about? professionals can be forgiven for improvising. The
That was the only time I saw a crease prick up on his public is generally understanding that in a crisis like this
otherwise unlined forehead: his idiot medical student we need to graduate our medical students early, pull
hadn’t prepared saline flushes to prevent this newly placed our vaccine nurses over to inpatient duty, recruit our
central line from clotting off. But he recovered in an instant dermatologists to assist with peritoneal dialysis, turn
and strode off to the nurses’ station. I wasn’t exactly sure our orthopaedic surgeons into medical interns, task our
how much I’d screwed things up, so I didn’t say a word to urologists with delicate family conversations, convert
the patient lying motionless under the drape. Nor did he our endoscopy suites into intensive care units. There
say a word to me. will be missteps with this jerry-rigging, no doubt, but
In a flash, my resident was back, gripping three saline- in times of critical need the benefits usually outweigh
filled syringes that he promptly dispatched into the the harms.
three ports of the central line. The day was saved, as was Under regular circumstances, however, the practice
my skin. of medicine needn’t entail actual practising on our
What I remember from that day was that after the patients. Trial and error isn’t an appropriate diagnostic or
procedure I collapsed in a heap in the call room, my therapeutic strategy.
autonomic nerves jangling, riling up every physiological So bravo to simulation technology. It is a critical step
system in my body. What I don’t remember from that day for ensuring that those jumbo jets stay safely tucked in
is how the patient responded to the ordeal, whether it was the sky where they should be. Jab away, medical students,
as traumatic for him as it was for me, or whether it was just at plasticine jugular veins. Go to town with the faux
another day at the VA. joints for arthrocentesis. Suture to your hearts’ content
And so went all of my medical training. All of my firsts— on synthetic abdomens. Ramble all you want with actors
first paracentesis, first arterial line, first lumbar puncture, in simulated renal failure. Experiment lavishly during
first bone-marrow biopsy, first nasogastric tube, first pelvic cardiac resuscitations on interactive apps.
exam, first end-of-life discussion, and first diagnosis of But when you do get to the real thing, however,
cancer—all were done on real people. All under the omnibus remember to peek under the drape. Those are real people
rationale of dwelling in a teaching hospital. under there. Their concerns are not simulated. Their fears
When I look back at this now, I’m frankly horrified at are not fabricated. The worries they are experiencing are
what was considered a routine approach to training— not mocked up for an actor’s prepared clinical encounter.
placing sharp objects and critical conversations in the While they might, in fact, be debuting in their role as
hands of medical fetuses and letting them loose on living, patients, they do not have the luxury of a warm-up or
breathing patients. rehearsal. Yes, they might be improvising, but it’s not
From the modern-day lens of patient safety, this remotely role-play for them. They will be looking directly
trial-and-error method of teaching contains a little too at you and will not desire a simulation of any sort.
much, well, error. As a physician and educator—and They’ll need the real thing.
occasional patient—I’m deeply heartened by the increasing
sophistication of simulation technology. Our trainees Danielle Ofri
should do all their initial bumbling on inanimate objects Bellevue Hospital, NYU School of Medicine, New York,
and computer-simulated scenarios. They should practise NY 10016, USA
the high-stakes conversations with trained actors in risk- danielle.ofri@nyumc.org
free settings. Maybe it’s not quite as good as the real thing, @danielleofri
but it’s close enough. And I’m sure that most patients Danielle Ofri is the author of When We Do Harm: A Doctor Confronts Medical
would be in hearty agreement. Error (Beacon Press, 2020).
www.thelancet.com Vol 395 May 16, 2020 1539
You might also like
- DR Breath by Carl Stough PDFDocument128 pagesDR Breath by Carl Stough PDFJuan Vizán86% (7)
- Gray Matter: A Neurosurgeon Discovers the Power of Prayer . . . One Patient at a TimeFrom EverandGray Matter: A Neurosurgeon Discovers the Power of Prayer . . . One Patient at a TimeRating: 4 out of 5 stars4/5 (37)
- Sentimental Medicine PDFDocument8 pagesSentimental Medicine PDF杨飞燕No ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineSuwandi ChangNo ratings yet
- Physical Diagnosis of Pain An Atlas of Signs and Symptoms 3rd Edition CompressDocument369 pagesPhysical Diagnosis of Pain An Atlas of Signs and Symptoms 3rd Edition CompressProsenjit MajiNo ratings yet
- NEJMp2402006Document2 pagesNEJMp2402006crazycrane12321No ratings yet
- Nej MP 2011418Document3 pagesNej MP 2011418The Dark DreamerNo ratings yet
- Full Download Book Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition PDFDocument41 pagesFull Download Book Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition PDFola.sumrall565100% (24)
- Physical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition Waldman MD JD All ChapterDocument67 pagesPhysical Diagnosis of Pain An Atlas of Signs and Symptoms 4Th Edition Waldman MD JD All Chapterkevin.roberts692100% (11)
- What I Do Not Tell The Medical StudentDocument2 pagesWhat I Do Not Tell The Medical StudentMohan PrasadNo ratings yet
- Hypnosis in The Emergency Department BIERMANDocument5 pagesHypnosis in The Emergency Department BIERMANAyoub LilouNo ratings yet
- Learning To TalkDocument2 pagesLearning To Talkgeochu02No ratings yet
- Lévinas - A Doutrine For DoctorsDocument2 pagesLévinas - A Doutrine For DoctorsTássia MatosNo ratings yet
- Unexpected Closure: PerspectiveDocument3 pagesUnexpected Closure: PerspectivePatrick CommettantNo ratings yet
- VR TherapyDocument5 pagesVR TherapyHec ChavezNo ratings yet
- Atbaseline NejmDocument2 pagesAtbaseline NejmSandeep SasidharanNo ratings yet
- Direct Red: A Surgeon's View of Her Life-or-Death ProfessionFrom EverandDirect Red: A Surgeon's View of Her Life-or-Death ProfessionRating: 3.5 out of 5 stars3.5/5 (31)
- Battlefield Acupuncture: My Story: EditorialDocument2 pagesBattlefield Acupuncture: My Story: Editorialyan92120No ratings yet
- Cap 2023 01 01Document51 pagesCap 2023 01 01Yaser MNo ratings yet
- Piis0140673699903914 2Document1 pagePiis0140673699903914 2Aditi S MathNo ratings yet
- Positional Cervical Cord Compression Fibromyalgia PaperDocument7 pagesPositional Cervical Cord Compression Fibromyalgia PaperValiant LordNo ratings yet
- Sri Magazine 2017Document68 pagesSri Magazine 2017Moosa Babul M37No ratings yet
- Emergency Medicine MotrelyDocument4 pagesEmergency Medicine MotrelyOsman PazNo ratings yet
- The World of Medical Transcription - A Broad Perspective From A Team Approach PDFDocument0 pagesThe World of Medical Transcription - A Broad Perspective From A Team Approach PDFAgung Budiman Agustinus SilalahiNo ratings yet
- Bedell 04 Words That HarmDocument4 pagesBedell 04 Words That HarmR.L. BandaNo ratings yet
- Pendular Diagnosis - From Dowsing To Diagnostic MethodologyDocument7 pagesPendular Diagnosis - From Dowsing To Diagnostic MethodologyVijay MuthekarNo ratings yet
- Boundaries of Evolution: What Would Darwin Think Now About Dna, the Big Bang, and Finite Time?From EverandBoundaries of Evolution: What Would Darwin Think Now About Dna, the Big Bang, and Finite Time?No ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicinedavideNo ratings yet
- Honey, Mud, Maggots and Other Medical Marvels: by R. and M. Root-BernsteinDocument1 pageHoney, Mud, Maggots and Other Medical Marvels: by R. and M. Root-BernsteinAndrei BombardieruNo ratings yet
- ARTÍCULOSDocument308 pagesARTÍCULOSDavid OlveraNo ratings yet
- Patient's Cures His Snoring: The EditorDocument1 pagePatient's Cures His Snoring: The EditorDiegoNo ratings yet
- Jaocr: Emergency RadiologyDocument38 pagesJaocr: Emergency Radiologyasp annishyaNo ratings yet
- Tales From The Temporal Lobes: PerspectiveDocument3 pagesTales From The Temporal Lobes: PerspectiveDini CahyaNo ratings yet
- Quick Physical Exam PDFDocument2 pagesQuick Physical Exam PDFffocussNo ratings yet
- 2004, Vol.6, No.4, Pediatric Surgery PDFDocument95 pages2004, Vol.6, No.4, Pediatric Surgery PDFAnty Dewi Sarty RanyabarNo ratings yet
- The Emperor's New Clothes: A Critical Appraisal of Evidence-Based MedicineDocument9 pagesThe Emperor's New Clothes: A Critical Appraisal of Evidence-Based MedicineCarlos Antonio Párraga GómezNo ratings yet
- A New Leadership Curriculum: The Multiplication of IntelligenceDocument4 pagesA New Leadership Curriculum: The Multiplication of IntelligenceGisele PhaloNo ratings yet
- Jamainternal Heger 2023 PP 230001 1681398072.43626Document2 pagesJamainternal Heger 2023 PP 230001 1681398072.43626Paola Cristini Gama SilvaNo ratings yet
- Mutation Research/Reviews in Mutation Research: Narendra P. SinghDocument8 pagesMutation Research/Reviews in Mutation Research: Narendra P. SinghAndrea bedoya vasquezNo ratings yet
- Nursing Care Plan Endometrial CancerDocument2 pagesNursing Care Plan Endometrial Cancerderic88% (16)
- Burnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBADocument3 pagesBurnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBALeon BosnjakNo ratings yet
- Ofri - Medical Humanities - Week1Document2 pagesOfri - Medical Humanities - Week1isabella brantonNo ratings yet
- Osborne 1928Document1 pageOsborne 1928lam lamNo ratings yet
- General IandsDocument4 pagesGeneral IandsScooterKatNo ratings yet
- Cranial Manipulative TherapyDocument6 pagesCranial Manipulative Therapypurple112650% (2)
- College Essay Example #3: This Is A College Essay That Worked ForDocument2 pagesCollege Essay Example #3: This Is A College Essay That Worked ForCristian ArevaloNo ratings yet
- Aim4pg Magazine July December 2019Document27 pagesAim4pg Magazine July December 2019AnirbanMallikNo ratings yet
- #Pendular Diagnosis - From Dowsing To Diagnostic MetholologyDocument7 pages#Pendular Diagnosis - From Dowsing To Diagnostic MetholologyAivlys100% (1)
- The CaseDocument2 pagesThe Casetemp3rarNo ratings yet
- Neurypnology - JamesBraidDocument296 pagesNeurypnology - JamesBraidCarlNo ratings yet
- HOLOMBE What Is Homoeopathy A New Exposition of A Great Truth!Document28 pagesHOLOMBE What Is Homoeopathy A New Exposition of A Great Truth!Bharatibhushan NayakNo ratings yet
- A Manual of Instruction For Giving Swedish Movement and Massage 1889Document1 pageA Manual of Instruction For Giving Swedish Movement and Massage 1889Davide Di GiacomoNo ratings yet
- GNM Schizophrenic Constellations en MarkolinDocument107 pagesGNM Schizophrenic Constellations en MarkolinAngela LovarcoNo ratings yet
- Complete Autopsy PDFDocument6 pagesComplete Autopsy PDFJAVIER ERNESTO CAÑON FRIASNo ratings yet
- ECI-B14Fx: 4 MP Outdoor IR Network Bullet CameraDocument3 pagesECI-B14Fx: 4 MP Outdoor IR Network Bullet CameraMuhNo ratings yet
- Material Safety Data Sheet: Sodium Hydroxide, Pellets, Reagent ACS MSDSDocument6 pagesMaterial Safety Data Sheet: Sodium Hydroxide, Pellets, Reagent ACS MSDSMuhNo ratings yet
- Material Safety Data Sheet: Hydrochloric Acid, 37% MSDSDocument8 pagesMaterial Safety Data Sheet: Hydrochloric Acid, 37% MSDSMuhNo ratings yet
- SARS CoV 2 and Influenza Virus Co Infection - 2020 - The LancetDocument1 pageSARS CoV 2 and Influenza Virus Co Infection - 2020 - The LancetMuhNo ratings yet
- Shell Helix Ultra Professional AJ-L 0W-20: Main Applications Specifications, Approvals & RecommendationsDocument2 pagesShell Helix Ultra Professional AJ-L 0W-20: Main Applications Specifications, Approvals & RecommendationsMuhNo ratings yet
- Best Motor Oil For Hyundai Tucson (2021 Professional Review) Hyundai Tucson Engine Oil Recommendations - OilapDocument23 pagesBest Motor Oil For Hyundai Tucson (2021 Professional Review) Hyundai Tucson Engine Oil Recommendations - OilapMuhNo ratings yet
- Bpxe AbjfycDocument2 pagesBpxe AbjfycMuhNo ratings yet
- Product Information: Special Tec AA 10W-30 BenzinDocument1 pageProduct Information: Special Tec AA 10W-30 BenzinMuhNo ratings yet
- Shell Helix Ultra 5W-40: Performance, Features & BenefitsDocument2 pagesShell Helix Ultra 5W-40: Performance, Features & BenefitsMuhNo ratings yet
- EDGE Extended Performance: DescriptionDocument3 pagesEDGE Extended Performance: DescriptionMuhNo ratings yet
- Castrol EDGE 5W-30 A5/B5: DescriptionDocument2 pagesCastrol EDGE 5W-30 A5/B5: DescriptionMuhNo ratings yet
- 1ph Hybrid Solar Inverter (1000va - 5000va) - Farber PowerDocument4 pages1ph Hybrid Solar Inverter (1000va - 5000va) - Farber PowerMuhNo ratings yet
- Bpxe 9P9HK3Document2 pagesBpxe 9P9HK3MuhNo ratings yet
- Bpxe 9pu2leDocument3 pagesBpxe 9pu2leMuhNo ratings yet
- Safety Data Sheet: Ubstance and Ource DentificationDocument6 pagesSafety Data Sheet: Ubstance and Ource DentificationMuhNo ratings yet
- Specification: Model FA-MPCHR-12V-300W FA-MPCHR-12V/24V-600W FA-MPCHR-36V-850W FA-MPCHR-12V/48V-3000W InputDocument1 pageSpecification: Model FA-MPCHR-12V-300W FA-MPCHR-12V/24V-600W FA-MPCHR-36V-850W FA-MPCHR-12V/48V-3000W InputMuhNo ratings yet
- Safety Data Sheet Xylene: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingDocument9 pagesSafety Data Sheet Xylene: SECTION 1: Identification of The Substance/mixture and of The Company/undertakingMuhNo ratings yet
- Specification: Model Number FA-OFFINVX-24V-3000VA FA-OFFINVX-48V-5000VADocument1 pageSpecification: Model Number FA-OFFINVX-24V-3000VA FA-OFFINVX-48V-5000VAMuhNo ratings yet
- Safety Data SheetDocument7 pagesSafety Data SheetMuhNo ratings yet
- Safety Data Sheet: Section 1. IdentificationDocument12 pagesSafety Data Sheet: Section 1. IdentificationMuhNo ratings yet
- 19 - 1391926836 - N Butanol CASNO 71 36 3 MSDSDocument7 pages19 - 1391926836 - N Butanol CASNO 71 36 3 MSDSMuhNo ratings yet
- Heart and Circulation Test: NameDocument12 pagesHeart and Circulation Test: NamezipperNo ratings yet
- Silverglide Surgical TechnologiesDocument2 pagesSilverglide Surgical TechnologiesDhruv GandhiNo ratings yet
- Lecture 13 - Extraction of ToothDocument46 pagesLecture 13 - Extraction of Toothvanesa AvramovaNo ratings yet
- 3-Hypothenar Hammer SyndromeDocument22 pages3-Hypothenar Hammer SyndromeProfesseur Christian DumontierNo ratings yet
- Resume 1Document2 pagesResume 1api-400253936No ratings yet
- 50 Topics List 1Document1 page50 Topics List 1akanksha singhNo ratings yet
- Anatomy of The Scalp!Document5 pagesAnatomy of The Scalp!GE EKNo ratings yet
- SurgicalTipsandTricksDuringUrethroplastyforBulbarUrethralStricturesFocusingonAccurateLocalisationoftheStricture ResultsfromaTertiaryCentreDocument8 pagesSurgicalTipsandTricksDuringUrethroplastyforBulbarUrethralStricturesFocusingonAccurateLocalisationoftheStricture ResultsfromaTertiaryCentreTomek RNo ratings yet
- Aortic Valve ReplacementDocument17 pagesAortic Valve Replacementm_alodat6144No ratings yet
- Orthopaedics Assessment: Oncology Division: Dr. Reza Devianto Hambali Dr. Arief Abidin Dr. A.S. Marsahala LumbantobingDocument44 pagesOrthopaedics Assessment: Oncology Division: Dr. Reza Devianto Hambali Dr. Arief Abidin Dr. A.S. Marsahala LumbantobingReza Devianto HambaliNo ratings yet
- Growing Beans Handout - Plant Growth Scientific ExperimentDocument2 pagesGrowing Beans Handout - Plant Growth Scientific ExperimentMariah Alexis EncinaNo ratings yet
- Yang - A New Trick To A Routine Procedure Taking The Fear Out of The Axillary Vein Stick Using The 35' Caudal View - Europace 2015Document4 pagesYang - A New Trick To A Routine Procedure Taking The Fear Out of The Axillary Vein Stick Using The 35' Caudal View - Europace 2015Gabriel JoséNo ratings yet
- Surface Anatomy: David Ebenezer Department of Anatomy Velammal Medical CollegeDocument101 pagesSurface Anatomy: David Ebenezer Department of Anatomy Velammal Medical CollegeKarishma RameshNo ratings yet
- Id QuestionDocument67 pagesId QuestionRahul PradeepNo ratings yet
- Information About Stapedectomy and OtosDocument10 pagesInformation About Stapedectomy and Otosiangould12No ratings yet
- 1 El Alto Origen de La Arteria Radial (Arteria Braquiorradial)Document11 pages1 El Alto Origen de La Arteria Radial (Arteria Braquiorradial)Juan José CabezasNo ratings yet
- Test Bank For Maternity and Womens Health Care 11th Edition by LowdermilkDocument11 pagesTest Bank For Maternity and Womens Health Care 11th Edition by Lowdermilkdonnadaviskjqpxitacn100% (32)
- Georgopoulos Study July 08 PDFDocument9 pagesGeorgopoulos Study July 08 PDFCarlos Julián Ortiz DallosNo ratings yet
- Nerves of Upper LimbDocument13 pagesNerves of Upper LimbHafiz NaveedNo ratings yet
- Anesthesia Side EffectsDocument10 pagesAnesthesia Side EffectsPADAYON MEDISINANo ratings yet
- Miniaturized Reveal LINQ Insertable Cardiac MonitoDocument7 pagesMiniaturized Reveal LINQ Insertable Cardiac MonitoLetícia JanuziNo ratings yet
- Series Coding Certification TipsDocument11 pagesSeries Coding Certification TipsJUNAID RAHMANNo ratings yet
- Hernia QuestionsDocument6 pagesHernia QuestionsNica Lopez Fernandez100% (1)
- Krukenberg Amputation & Its ManagementDocument12 pagesKrukenberg Amputation & Its ManagementSIBASIS PATTANAYAKNo ratings yet
- 1.4 B Tija Centromedulara PFN LungDocument18 pages1.4 B Tija Centromedulara PFN LungGhica CostinNo ratings yet
- 422 Lab 2Document8 pages422 Lab 2kurucz barbaraNo ratings yet
- Imtiaz Notes Main-1-1Document8 pagesImtiaz Notes Main-1-1Dr Afzal HussainNo ratings yet
- Cardiopulmonary Bypass: Learning ObjectivesDocument5 pagesCardiopulmonary Bypass: Learning ObjectivesAnonymous zPwXqwNo ratings yet
- Extraction of Wisdom Teeth Under General Anesthesia-A StudyDocument5 pagesExtraction of Wisdom Teeth Under General Anesthesia-A StudyCiutac ŞtefanNo ratings yet
- Endobutton™ CL Ultra: Fixation DeviceDocument6 pagesEndobutton™ CL Ultra: Fixation Deviceapi-19808945No ratings yet