Professional Documents
Culture Documents
Risk For Bleeding - Cirrhosis NCP
Risk For Bleeding - Cirrhosis NCP
Uploaded by
Paula AbadOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Risk For Bleeding - Cirrhosis NCP
Risk For Bleeding - Cirrhosis NCP
Uploaded by
Paula AbadCopyright:
Available Formats
Risk for Bleeding
related to portal hypertension and altered clotting factors
Desired Outcomes: The patient is free of bleeding/hemorrhage as evidenced by blood
pressure (BP) at least 90/60 mm Hg; heart rate (HR) 100 bpm or less; warm extremities;
distal pulses greater than 2 on a 0-4 scale; brisk capillary refill (less than 2 sec); and
orientation to person, place, and time. Bruising, melena, and hematemesis are absent.
Assess vital signs (VS) q4h (or more frequently if VS are outside of the
patient’s baseline values).
Upper GI hemorrhage is common in patients with chronic liver
disease and can result from esophageal varices, portal
hypertensive gastropathy, duodenal or gastric ulcers, or Mallory-
Weiss tear (mucosal laceration at the juncture of the distal
esophagus and proximal stomach). Early diagnosis is essential to
enable appropriate intervention. Hypotension and increased HR, as
well as cool extremities, delayed capillary refill, decreased
amplitude of distal pulses, mental status changes, and decreasing
level of consciousness (LOC), are indicators of hypovolemia and
hemorrhage.
Assess for signs of bleeding and notify the health care provider of
significant findings.
Bruising, melena, and hematemesis are signs of bleeding. Altered VS,
irritability, air hunger, pallor, and weakness are signs of
significant bleeding and necessitate prompt intervention.
Inspect stools for the presence of blood; perform stool occult blood test as
indicated.
This is an assessment for bleeding within the GI tract.
Monitor PT and INR for abnormality. INR: Normal range is less than 2.0 sec for
patients not receiving anticoagulant therapy.
PT: Normal range is 10.5-13.5 sec. A PT that is prolonged signals the
patient is at risk for bleeding.
Teach the patient to avoid swallowing foods that are chemically or
mechanically irritating.
Rough or spicy foods, hot foods, hot liquids, and alcohol may be
injurious to the esophagus and result in bleeding.
Teach the importance of avoiding actions such as sneezing, lifting, or
vomiting.
These actions increase intraabdominothoracic pressure, which can
result in bleeding.
Administer stool softeners as prescribed.
Stool softeners help prevent straining with defecation, which puts
patients at risk for bleeding.
As appropriate, encourage intake of foods rich in vitamin K (e.g., spinach,
cabbage, cauliflower, liver).
These foods may help decrease PT.
As often as possible, avoid invasive procedures such as giving injections
and taking rectal temperatures.
If clotting is altered, invasive procedures could result in prolonged
bleeding.
Monitor the patient undergoing band ligation or injection sclerotherapy of
varices for increased HR, decreased BP, pallor, weakness, and air
hunger.
These are signs of esophageal perforation caused by the treatment of
varices, whether by injection, cautery, or the scope itself.
If signs of perforation occur, notify the health care provider immediately,
keep the patient nothing by mouth (NPO), and prepare for gastric
suction. Administer antibiotics as prescribed to prevent infection.
NPO status and gastric suction prevent leakage of fluid, secretions, or
food through the perforation into the mediastinum. This
emergency situation necessities immediate intervention.
You might also like
- Darkness Visible: A Memoir of Madness IDocument4 pagesDarkness Visible: A Memoir of Madness ILucas ValdezNo ratings yet
- Colon Rectal CancerDocument6 pagesColon Rectal Cancerbryantmaroney811No ratings yet
- RLEFand ECSDocument3 pagesRLEFand ECSPaul JacksonNo ratings yet
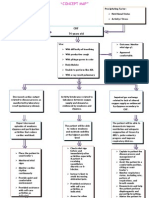
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Nursing Care Plan Priorities: Risk For InjuryDocument6 pagesNursing Care Plan Priorities: Risk For InjuryPauling FrezNo ratings yet
- Alzheimers Nursing Care PlanDocument6 pagesAlzheimers Nursing Care Planmp1757100% (1)
- I.intrODUCTION Hypertension (High Blood Pressure) Is ADocument19 pagesI.intrODUCTION Hypertension (High Blood Pressure) Is Aoril04No ratings yet
- Actual NCPDocument3 pagesActual NCPMabz BoholNo ratings yet
- Case Presentation AnaphylaxisDocument14 pagesCase Presentation AnaphylaxisKevin GarciaNo ratings yet
- RevisionDocument17 pagesRevisionMatt RenaudNo ratings yet
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiNo ratings yet
- Levemir Product Insert PDFDocument11 pagesLevemir Product Insert PDFDegee O. GonzalesNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planusama_salaymehNo ratings yet
- Decreased Cardiac OutputDocument1 pageDecreased Cardiac OutputPrecious Heart Sotero TababaNo ratings yet
- GitDocument302 pagesGitjgcriste100% (7)
- Nursing Care PlanDocument13 pagesNursing Care Planyumiko0% (1)
- Case Study ReportDocument23 pagesCase Study Reportapi-290866384No ratings yet
- Pathophysiology of Shock Sepsis and Organ Failure PDFDocument1,179 pagesPathophysiology of Shock Sepsis and Organ Failure PDFNotInterested100% (1)
- Post Cesarean Section DeliveryDocument5 pagesPost Cesarean Section Deliveryᒙᕧᖇᕦᙏᖻ ᗴᔛᓦᗩᖆᗩNo ratings yet
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalanteNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- Propranolol 1 PresentationDocument17 pagesPropranolol 1 Presentationapi-284092317100% (1)
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationMara Jon Ocden CasibenNo ratings yet
- Guillain Barre Case StudyDocument18 pagesGuillain Barre Case Studymydnyt02No ratings yet
- HCVDDocument5 pagesHCVDkhrizaleehNo ratings yet
- Decreased Cardiac Output FinalDocument2 pagesDecreased Cardiac Output FinalSandraDeeNo ratings yet
- Nursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy MalaiseDocument1 pageNursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy Malaise06eltianNo ratings yet
- 01 NGT Procedure With RationaleDocument4 pages01 NGT Procedure With RationaleAryaj SulitNo ratings yet
- PT EducationDocument4 pagesPT Educationapi-248017509No ratings yet
- NCP FVDDocument1 pageNCP FVDsisjing88510No ratings yet
- Betahistine Drug InfoDocument3 pagesBetahistine Drug InfoAshish KarnNo ratings yet
- Introduction - MIDocument10 pagesIntroduction - MIkhimiiiNo ratings yet
- TAHBSO ReportDocument4 pagesTAHBSO ReportsachiiMeNo ratings yet
- HypopituitarismDocument2 pagesHypopituitarismAnne de VeraNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- PathophysiologyDocument1 pagePathophysiologyHazel PalomaresNo ratings yet
- Meniere's Disease - Case StudyDocument3 pagesMeniere's Disease - Case StudyZORANASNNo ratings yet
- Myocardial Infarction Concept MapDocument7 pagesMyocardial Infarction Concept Mapkarelclarke629280% (5)
- Surgical Managment of DMDocument42 pagesSurgical Managment of DMHaroon Malik100% (1)
- Decreased Cardiac Output RM 7Document9 pagesDecreased Cardiac Output RM 7api-283470660No ratings yet
- AcknowledgementDocument9 pagesAcknowledgementjhzenNo ratings yet
- Cues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationMiggy SikatNo ratings yet
- 4th Yr. Med Cardio Module Question - Copy-1Document11 pages4th Yr. Med Cardio Module Question - Copy-1Sheda BondNo ratings yet
- NCP 2 CabalunaDocument7 pagesNCP 2 CabalunaIrene Grace BalcuevaNo ratings yet
- NCP PleuralDocument5 pagesNCP Pleuraljanine_valdezNo ratings yet
- NCP Micu Hascvd Cad - RioDocument5 pagesNCP Micu Hascvd Cad - RioRio BonifacioNo ratings yet
- Topic 5 - Fluid & ElectrolytesDocument3 pagesTopic 5 - Fluid & Electrolyteschristy INo ratings yet
- Case CHFDocument10 pagesCase CHFAgnes Erlita Distriani Patade50% (2)
- Nursing Care PlanDocument8 pagesNursing Care PlanKing RamosNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationAriaNo ratings yet
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafeNo ratings yet
- Angiotensin Converting Enzyme (ACE) InhibitorsDocument4 pagesAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanNo ratings yet
- Imbalanced NutritionDocument3 pagesImbalanced NutritionIlisa ParilNo ratings yet
- Ineffective Tissue Perfusion Secondary To Cellulitis DM Type 2Document3 pagesIneffective Tissue Perfusion Secondary To Cellulitis DM Type 2MichaelaKatrinaTrinidadNo ratings yet
- Dr. Sunatrio - Management Hypovolemic ShockDocument59 pagesDr. Sunatrio - Management Hypovolemic ShockArga Putra SaboeNo ratings yet
- NCM 114 Gerontology - WeeK 1Document38 pagesNCM 114 Gerontology - WeeK 1Jmarie Brillantes Popioco0% (1)
- Discharge PlanDocument1 pageDischarge PlanBernalene SyNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetDocument5 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: STO: Within 4 Hour of DX: DX: Sto: Goal MetRussel SantosNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- HemodialysisDocument4 pagesHemodialysisJon Adam Bermudez SamatraNo ratings yet
- Zinc Toxicity in Humans: Jerome Nriagu, School of Public Health, University of MichiganDocument7 pagesZinc Toxicity in Humans: Jerome Nriagu, School of Public Health, University of MichiganAfshee umarNo ratings yet
- Vijaya DiagnosticDocument5 pagesVijaya Diagnosticuma reddyNo ratings yet
- Asperheim/Favaro: Introduction To Pharmacology, 12th EditionDocument2 pagesAsperheim/Favaro: Introduction To Pharmacology, 12th Editionvinhson65-1No ratings yet
- GRP 3 - Galatians - Borgia Et1Document3 pagesGRP 3 - Galatians - Borgia Et1Kyle BARRIOSNo ratings yet
- Diabetic RetinopathyDocument5 pagesDiabetic RetinopathyAndreiNo ratings yet
- Nursing Audit in Obstetric Care (1) - Mrs. Sarla TakooDocument45 pagesNursing Audit in Obstetric Care (1) - Mrs. Sarla TakooSaritaNo ratings yet
- Module 2 Handout CO2 Adverse Health Effects Fact SheetDocument1 pageModule 2 Handout CO2 Adverse Health Effects Fact Sheetdennis ovichNo ratings yet
- Chapter 21 Male ReproDocument34 pagesChapter 21 Male ReproIsfahan MasulotNo ratings yet
- DermatologyDocument27 pagesDermatologydranilshindeNo ratings yet
- InggrisDocument4 pagesInggrisRatuNo ratings yet
- SC003 1 Order of Draw WebsiteDocument3 pagesSC003 1 Order of Draw WebsitemariamNo ratings yet
- Chronic Renal Failure enDocument2 pagesChronic Renal Failure enSinggih Pratiknyo SundawaNo ratings yet
- Application For LicenseDocument11 pagesApplication For LicenseSadaf RizwanhumayoonNo ratings yet
- Cardiovascular Diseases: Risk FactorsDocument18 pagesCardiovascular Diseases: Risk FactorsShin QuinnNo ratings yet
- Soal Praktek-EBM-THTKL-Daniel BramantyoDocument20 pagesSoal Praktek-EBM-THTKL-Daniel BramantyoDaniel BramantyoNo ratings yet
- D G Model Making Sense of Clinical Examination of The Adult Patient Hands-On GuideDocument313 pagesD G Model Making Sense of Clinical Examination of The Adult Patient Hands-On GuidevaidyamNo ratings yet
- Scientific PaperDocument7 pagesScientific PaperLaura AlfaroNo ratings yet
- FNCPDocument2 pagesFNCPKimberlyjoycsolomonNo ratings yet
- Schwann Cells PowerpointDocument16 pagesSchwann Cells PowerpointabibtdottyNo ratings yet
- 13 HemostasisDocument38 pages13 HemostasissiratelNo ratings yet
- Sickle Cell DiseaseDocument22 pagesSickle Cell DiseaseDias SetiawanNo ratings yet
- Perbedaan Kadar Kolesterol Sebelum Dan Sesudah Dilakukan Brisk Walking Pada SiswaDocument8 pagesPerbedaan Kadar Kolesterol Sebelum Dan Sesudah Dilakukan Brisk Walking Pada SiswaEva RahmadaniNo ratings yet
- FlexiQuin Leaflet InsertDocument1 pageFlexiQuin Leaflet InsertHaseeb QadriNo ratings yet
- Moore Kiana - Family Planning BrochureDocument2 pagesMoore Kiana - Family Planning Brochureapi-518091160No ratings yet
- Seminar On Organization of Camps and Clinics in Community SettingsDocument18 pagesSeminar On Organization of Camps and Clinics in Community SettingsRethina Bai C100% (2)
- Drowning PhysDocument1 pageDrowning Physmentor67No ratings yet
- Chemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireDocument6 pagesChemistry Analyzer: Chemistry Analyzers Can Be Benchtop Devices or Placed On A Cart Other Systems RequireCalvin KleinNo ratings yet
- School Health Examination Card: Republic of The Philippines Department of EducationDocument4 pagesSchool Health Examination Card: Republic of The Philippines Department of EducationDanny LineNo ratings yet