Professional Documents
Culture Documents
2020 Can Pelvic Floor Muscle Training
2020 Can Pelvic Floor Muscle Training
Uploaded by
juan pabloCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2020 Can Pelvic Floor Muscle Training
2020 Can Pelvic Floor Muscle Training
Uploaded by
juan pabloCopyright:
Available Formats
EVIDENCE-BASED PHYSIATRY: COCHRANE CORNER
Can Pelvic Floor Muscle Training Versus No Treatment or Inactive
Control Treatments Reduce or Cure Urinary Incontinence in
Women?
A Cochrane Review Summary With Commentary
Paolo Di Benedetto, MD
Downloaded from http://journals.lww.com/ajpmr by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 07/22/2021
he aim of this commentary is to summarize and discuss of PFM improve in response to an exercise program, that
T from a rehabilitation point of view the published Cochrane
Review “Pelvic floor muscle training versus no treatment,
contemplates low numbers of repetitions with high loads
to improve muscle strength and high numbers of repetitions
or inactive control treatments, for urinary incontinence in or prolonged contractions with low to moderate loads to
women” by Dumoulin et al.1 (https://www.cochranelibrary. improve muscle endurance. In addition, we have to men-
com/cdsr/doi/10.1002/14651858.CD005654.pub4/full? tion coordination training consisting of PFM contraction
cookiesEnabled), in collaboration with Cochrane Incontinence. in response to a specific situation (eg, before cough, “the
This Cochrane Corner is produced in agreement with the knack theory”).5
American Journal of Physical Medicine & Rehabilitation by The biological rationale for PFMT for SUI and MUI is
Cochrane Rehabilitation. twofold: with the PFM contraction (a) increasing the urethral
pressure and (b) providing support for the pelvic floor organs
BACKGROUND (ie, reducing bladder neck displacement). The biological ratio-
Urinary incontinence (UI), defined by the International nale for PFMT for UUI is based on the observation by Godec
Continence Society as the complaint of any involuntary loss et al.6 that a detrusor muscle contraction can be inhibited by
of urine, affects approximately a quarter to a third of women a PFM contraction; thereby, voluntary PFM contractions could
in their lifetime. Three common types of nonneurogenic UI be used to control the urgency to void, allowing the woman to
are observed: stress UI (SUI), urgency UI (UUI), and mixed reach the toilet in time to prevent urine leakage.1
UI (MUI). Stress UI is characterized by an involuntary loss
of urine during increased intra-abdominal pressure (effort or
physical exertion); UUI is present when a woman reports invol- PELVIC FLOOR MUSCLE TRAINING VERSUS NO
untary leakage associated with or immediately preceded by a TREATMENT, OR INACTIVE CONTROL
sudden and strong need to void (urgency); MUI is observed TREATMENTS, FOR UI IN WOMEN
when women have both symptoms and signs of SUI and UUI.2 (Dumoulin et al., 2018)
A wide range of treatments have been used in the manage-
ment of UI, including conservative interventions, medication, What Was the Aim of This Cochrane Review?
and surgery. The aim of this Cochrane Review was to assess the ef-
This review focuses on one of the most used conservative fects of PFMT for women with UI in comparison with no
interventions, specifically pelvic floor muscle training (PFMT) treatment, placebo drug or sham electrical stimulation, or
that is a program of exercises to improve pelvic floor muscle other inactive control treatments (anti-incontinence device,
(PFM) function.3,4 Generally, after achieving PFM awareness incontinence pads, general education class, access to an ed-
and correct motor learning, both strength and fatigue resistance ucational pamphlet).1
From the Friuli Riabilitazione Centre, Roveredo in Piano (Pordenone), Italy. What Was Studied in This Cochrane Review?
All correspondence should be addressed to: Paolo Di Benedetto, MD, Friuli
Riabilitazione Centre, 42 G. Carducci St, 33080 Roveredo in Piano The population addressed in this review was women
(Pordenone), Italy. with UI and diagnosed as having SUI, UUI, or MUI on the
This summary is based on a Cochrane Review previously published in the Cochrane
Database of Systematic Reviews 2018, Issue 10, Art. No.: CD005654, DOI: basis of symptoms, signs, or urodynamic study; trials of
10.1002/14651858.CD005654.pub4 (see http://www.cochranelibrary.com for women whose UI due to factors outside the lower urinary
information). Cochrane Reviews are regularly updated as new evidence emerges tract or to pregnancy or postnatal period were excluded.
and in response to feedback, and Cochrane Database of Systematic Reviews
should be consulted for the most recent version of the review. Other common exclusion criteria were urinary tract infec-
The views expressed in the summary with commentary are those of the Cochrane tion, significant postmicturition residual volume, neurologi-
Corner author(s) and do not represent the Cochrane Library or Wiley.
Financial disclosure statements have been obtained, and no conflicts of interest have
cal disorders, and cognitive impairments.
been reported by the authors or by any individuals in control of the content of The interventions included PFMT in comparison with no
this article. treatment, or inactive treatments. Pelvic floor muscle training
Copyright © 2019 Wolters Kluwer Health, Inc. All rights reserved.
ISSN: 0894-9115 was a program of repeated voluntary PFM contractions taught
DOI: 10.1097/PHM.0000000000001347 and generally supervised by a healthcare professional.
178 www.ajpmr.com American Journal of Physical Medicine & Rehabilitation • Volume 99, Number 2, February 2020
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Volume 99, Number 2, February 2020 Urinary Incontinence in Women
The outcomes of interest in the review were as follows: The evidence was generally downgraded to moderate
on methodological grounds with the exception of
(a) primarily, symptomatic cure or improvement of UI, “participant-perceived cure” in women with SUI, which
symptom-, and condition-specific quality-of-life (QoL) was rated as high quality.
measures, and
(b) secondarily, longer-term symptomatic cure or improve- What Were the Authors’ Conclusions?
ment of UI, satisfaction and need for further treatment, Pelvic floor muscle training can cure or improve symp-
number of leakage episodes in 24 hrs on bladder diary, toms of SUI reducing the number of leakage episodes, the
amount of leakage from a short or long pad-test, and gen- quantity of leakage on the short pad tests, and symptoms on
eral QoL. UI-specific symptom questionnaires. A similar pattern is seen
in studies that recruit women with all types of UI (SUI, MUI,
Search Methodology and Up-to-Dateness of the and UUI) rather one specific type of UI.
Cochrane Review The long-term effectiveness of PFMT needs to be fur-
The review authors searched for studies published up to ther researched.
February 12, 2018.
What Are the Implications of the Cochrane
What Were the Main Results of This Cochrane Evidence for Practice in Rehabilitation?
Review? The Cochrane review indicates that PFMT should be
The review included 31 trials (10 of which were new for included in first-line conservative management for women
this update) involving 1817 women from 14 countries. The tri- with UI.
als included women with SUI, UUI, MUI, or UI all types. The Rehabilitation professionals should get involved in this
women were allocated randomly to either receive or not receive field because UI is a frequent and bothersome condition and
PFMT, and the effects were compared. the efficacy of this rehabilitation intervention (PFMT) is sup-
ported by high level of evidence.
Symptomatic Cure of UI
Remaining Issues
Women with SUI in the PFMT groups were, on aver-
age, eight times more likely to report being cured, whereas Although the PFMT is useful to reduce or cure UI, there
women with UI all types were, on average, five times to re- are some unresolved issues.
port being cured. The proposed PFMT programs differed in terms of type
and number of voluntary PFM contractions, duration of hold-
Symptomatic Cure or Improvement of UI ing and rest time, body positions, and treatment length. Thus,
optimal program has not yet been identified. However, it could
Women with SUI in PFMT groups were, on average, six
also be argued that this heterogeneity in exercise content adds
times more likely to report that they were cured or improved.
to the robust nature of the evidence; then, the finer detail of
Women with UI all types were roughly twice as likely to report program content may be less important.
that they were cured or improved.
As said before, there is no strong evidence of the long-
term effects of PFMT. Research is needed to identify strat-
Urinary Incontinence–Specific Symptoms and egies, which may allow patients to maintain the positive
Condition-Specific QoL treatment outcomes.
Women with SUI and UI all types in the PFMT groups
were more likely to report significant improvement in UI ACKNOWLEDGMENTS
symptoms and condition-specific QoL. One small trial for We thank the authors of Cochrane Review (Chantale
women with MUI reported better QoL. Dumoulin, Licia Cacciari, and Jean Hay-Smith), the Cochrane
Rehabilitation and Cochrane Incontinence Group for reviewing
Leakage Episodes in 24 hrs the Contents of the Cochrane Corner.
Pelvic floor muscle training reduced leakage episodes by
one in 24 hrs in women with SUI and UI all types. Pelvic floor
muscle training seemed to reduce urine loss in women with REFERENCES
UUI alone. 1. Dumoulin C, Cacciari LP, Hay-Smith EJC: Pelvic floor muscle training versus no treatment, or
inactive control treatments, for urinary incontinence in women (Review). Cochrane Database
Leakage on Short (up to 1 hr) Clinic-Based Pad Test Syst Rev 2018;10:CD005654
2. Abrams P, Cardozo L, Wagg A, et al: (eds): Incontinence, 6th ed 2017. Tokyo, 6th International
Women with SUI and UI all types in the PFMT groups Consultation on Incontinence, 2016
lost significantly less urine in short pad tests than controls. 3. Kegel AH: Progressive resistance exercise in the functional restoration of the perineal muscles.
Am J Obstet Gynecol 1948;56:238–48
4. Bø K: Pelvic floor muscle training for stress urinary incontinence. In: Bø K, Berghmans B,
Other Outcomes Mørkved S, Van Kampen M (eds): Evidence-Based Physical Therapy for the Pelvic Floor.
Women in the PFMT groups were also more satisfied with Bridging Science and Clinical practice. Philadelphia, PA, Butterworth Heinemann Elsevier, 2007
5. Dumoulin C, Glazener C, Jenkinson D: Determining the optimal pelvic floor muscle training
treatment and their sexual outcomes were better. Women in
regimen for women with stress urinary incontinence. NeurourolUrodyn 2011;30:746–53
control groups were more likely to seek further treatments. 6. Godec C, Cass AS, Ayala GF: Bladder inhibition with functional electrical stimulation.
Adverse events were very rare and promptly resolved. Urology 1975;6:663–6
© 2019 Wolters Kluwer Health, Inc. All rights reserved. www.ajpmr.com 179
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
You might also like
- Trauma Symptom Checklist For Children TSCCDocument6 pagesTrauma Symptom Checklist For Children TSCCblack smith0% (1)
- Sumita Mehta, Poonam Sachdeva (Eds.) - Colposcopy of Female Genital Tract-Springer Singapore (2017)Document243 pagesSumita Mehta, Poonam Sachdeva (Eds.) - Colposcopy of Female Genital Tract-Springer Singapore (2017)Rosu George100% (2)
- Pharmaceutical CareDocument114 pagesPharmaceutical CareRisdaFitriaNo ratings yet
- The Mechanisms of Muscle Hypertrophy and Their.40Document16 pagesThe Mechanisms of Muscle Hypertrophy and Their.40Raphael Bruno ChagasNo ratings yet
- SCR January 2021 SampleDocument13 pagesSCR January 2021 SampleDima KotNo ratings yet
- 35 Full PDFDocument9 pages35 Full PDFdespNo ratings yet
- 1 s2.0 S2173578618301458 MainDocument10 pages1 s2.0 S2173578618301458 Mainitziar.13.riveraNo ratings yet
- Balance Training With A Dynamometric Platform.3Document6 pagesBalance Training With A Dynamometric Platform.3Victor CorreiaNo ratings yet
- Recovery Matters 1619566999Document14 pagesRecovery Matters 1619566999tonigp369No ratings yet
- Exercise in Chronic Pulmonary Disease Aerobic.5Document9 pagesExercise in Chronic Pulmonary Disease Aerobic.5mvmarentesNo ratings yet
- Advances in Physical Rehab of MSDocument7 pagesAdvances in Physical Rehab of MSsarawu9911No ratings yet
- Exercise For OA KneeDocument5 pagesExercise For OA KneezumantaraNo ratings yet
- The Mechanisms of Muscle Hypertrophy and Their.40Document16 pagesThe Mechanisms of Muscle Hypertrophy and Their.40Sebastián EscuderoNo ratings yet
- Recovery After ExerciseDocument10 pagesRecovery After ExerciseMari PaoNo ratings yet
- Julian 2018Document14 pagesJulian 2018Harsh BohraNo ratings yet
- Management of Pancreatic Fluid Collections An.4Document16 pagesManagement of Pancreatic Fluid Collections An.4ji.cervanteshotmail.comNo ratings yet
- KeagleDocument6 pagesKeaglewispa handayaniNo ratings yet
- Blood Flow Restriction Training and The Physique AthleteDocument15 pagesBlood Flow Restriction Training and The Physique AthleteDouglas MarinNo ratings yet
- Improving Strength and Power in Trained Athletes With 3 Weeks of Occlusion TrainingDocument7 pagesImproving Strength and Power in Trained Athletes With 3 Weeks of Occlusion Trainingmatheus ramosNo ratings yet
- Lack of Human Muscle Architectural Adaptation After Short Term Strength TrainingDocument9 pagesLack of Human Muscle Architectural Adaptation After Short Term Strength TrainingwaelNo ratings yet
- The Mechanisms of Muscle Hypertrophy and Their.40Document16 pagesThe Mechanisms of Muscle Hypertrophy and Their.40João Pedro Adegas CarvalhoNo ratings yet
- Rodilla 8Document14 pagesRodilla 8AdosotoNo ratings yet
- Rehab-1. PP en IFDocument7 pagesRehab-1. PP en IFJavi Belén Soto MoralesNo ratings yet
- 14 ArticleDocument9 pages14 ArticleGianmarco BenottiNo ratings yet
- Campbell 2012Document11 pagesCampbell 2012NICOLÁS ANDRÉS AYELEF PARRAGUEZNo ratings yet
- Woodley Et Al-2020-Cochrane Database of Systematic ReviewsDocument157 pagesWoodley Et Al-2020-Cochrane Database of Systematic ReviewsLoretoNo ratings yet
- Effects of A Modified German Volume Training.21Document11 pagesEffects of A Modified German Volume Training.21leal thiagoNo ratings yet
- LAGRIMAS, Kathleen Kay V. MODULE 3: Structural/functional and Menstrual DisorderDocument8 pagesLAGRIMAS, Kathleen Kay V. MODULE 3: Structural/functional and Menstrual DisorderVictor ValerianoNo ratings yet
- Effect of Eccentric Strengthening After Anterior Cruciate Ligament Reconstruction On Quadriceps StrengthDocument7 pagesEffect of Eccentric Strengthening After Anterior Cruciate Ligament Reconstruction On Quadriceps StrengthQuiroprácticaParaTodosNo ratings yet
- Cross-Education of Strength Has A Positive Impact On Post-Stroke Rehabilitation: A Systematic Literature ReviewDocument11 pagesCross-Education of Strength Has A Positive Impact On Post-Stroke Rehabilitation: A Systematic Literature ReviewciccioNo ratings yet
- E000256 FullDocument12 pagesE000256 FullFADHLAN ARISNo ratings yet
- Training Practices and Ergogenic Aids Used by Male.20Document9 pagesTraining Practices and Ergogenic Aids Used by Male.20Gabriel BarrosNo ratings yet
- Pelvic Floor Muscle Training Is Effective in Treatment of Female Stress Urinary Incontinence, But How Does It Work?Document10 pagesPelvic Floor Muscle Training Is Effective in Treatment of Female Stress Urinary Incontinence, But How Does It Work?alonsosduranNo ratings yet
- Pelvic Floor and Exercise Science: Motor LearningDocument20 pagesPelvic Floor and Exercise Science: Motor LearningDiego Quidequeo ReffersNo ratings yet
- Is Combining Gait Retraining or An Exercise Programme With EducationDocument9 pagesIs Combining Gait Retraining or An Exercise Programme With EducationAhmet ÖztürkNo ratings yet
- Buteyko Clinic Trial ReviewDocument20 pagesButeyko Clinic Trial Reviewdghiwaudy728No ratings yet
- The Mechanisms of Muscle Hypertrophy and Their.40Document16 pagesThe Mechanisms of Muscle Hypertrophy and Their.40Luis ricardo Véjar felixNo ratings yet
- Articulo 3Document9 pagesArticulo 3Camilo RinconNo ratings yet
- Attentional Focus For Maximizing Muscle (NSCA Paper)Document3 pagesAttentional Focus For Maximizing Muscle (NSCA Paper)Gabriel ArnoldNo ratings yet
- NCP IacDocument1 pageNCP IacCrisza HalosNo ratings yet
- O Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiDocument6 pagesO Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiLeticia ZaniniiNo ratings yet
- BodyBallancer Sport Brochure PDFDocument2 pagesBodyBallancer Sport Brochure PDFRoss GaleNo ratings yet
- Mcgill 2010Document15 pagesMcgill 2010Júnior Alvacir CamargoNo ratings yet
- Effects of A Modified German Volume Training.21Document11 pagesEffects of A Modified German Volume Training.21Luis ricardo Véjar felixNo ratings yet
- 1809 2950 FP 21 04 00320Document7 pages1809 2950 FP 21 04 00320Susana SantanaNo ratings yet
- Cochrane: LibraryDocument17 pagesCochrane: LibraryGita TikihaiNo ratings yet
- Hollowing Vs Bracing PDFDocument9 pagesHollowing Vs Bracing PDFByron Vergara PereiraNo ratings yet
- Assessment Diagnosis Outcome Nursing Interventions Rationale EvaluationDocument1 pageAssessment Diagnosis Outcome Nursing Interventions Rationale EvaluationLight EstelleNo ratings yet
- The Mechanisms of Muscle Hypertrophy and Their.40Document16 pagesThe Mechanisms of Muscle Hypertrophy and Their.40Raquel MoreiraNo ratings yet
- Bishop 2008Document10 pagesBishop 2008Made Hendra, drg.No ratings yet
- Actividad Fisica de Alta IntensidadDocument10 pagesActividad Fisica de Alta IntensidadyatibaduizaNo ratings yet
- Evidence Base Practice: Submitted To: Maam Fizza, 3868Document6 pagesEvidence Base Practice: Submitted To: Maam Fizza, 3868Ambreen TariqNo ratings yet
- Continuous vs. Interrupted Chest Compressions For Cardiac ArrestDocument1 pageContinuous vs. Interrupted Chest Compressions For Cardiac Arrestrizki heriyadiNo ratings yet
- Are All Hip Extension Exercises Created Equal .4Document6 pagesAre All Hip Extension Exercises Created Equal .4leal thiagoNo ratings yet
- Scapular-Stabilization Exercises - Early-Intervention PrescriptionDocument6 pagesScapular-Stabilization Exercises - Early-Intervention PrescriptionJohnnySnow100% (1)
- Physical Performance and Electromyographic.12Document9 pagesPhysical Performance and Electromyographic.12az3ar.sameh449No ratings yet
- How To Incorporate Eccentric Training Into A Resistance Training ProgramDocument13 pagesHow To Incorporate Eccentric Training Into A Resistance Training ProgramAlexandre FerreiraNo ratings yet
- Comparison of Dynamic Push Up Training And.2Document6 pagesComparison of Dynamic Push Up Training And.2LYDIANo ratings yet
- Maioregen Rehabilitation ProgramDocument2 pagesMaioregen Rehabilitation ProgramMihai TintaNo ratings yet
- M R B R P P S S P: Etabolic Esponses To A Attling OPE Rotocol Erformed in The Eated or Tance OsitionsDocument7 pagesM R B R P P S S P: Etabolic Esponses To A Attling OPE Rotocol Erformed in The Eated or Tance OsitionsKaribeños San JavierNo ratings yet
- DeloadDocument27 pagesDeloadtatiNo ratings yet
- Med Surg Week 6Document11 pagesMed Surg Week 6Eunice Cortés100% (1)
- 2015 Effects of Oropharyngeal Exercises On SnoringDocument9 pages2015 Effects of Oropharyngeal Exercises On Snoringjuan pabloNo ratings yet
- 2019 Espondilolistesis Lumbar ItsmicaDocument8 pages2019 Espondilolistesis Lumbar Itsmicajuan pabloNo ratings yet
- 2019 Estado de La Unión. Revisión de Las Indicaciones y Técnicas de Fusión Lumbar para La Enfermedad Degenerativa de La ColumnaDocument14 pages2019 Estado de La Unión. Revisión de Las Indicaciones y Técnicas de Fusión Lumbar para La Enfermedad Degenerativa de La Columnajuan pabloNo ratings yet
- 2019 Fusión Intersomática Lumbar Transforaminal Endoscópica. RevisiónDocument9 pages2019 Fusión Intersomática Lumbar Transforaminal Endoscópica. Revisiónjuan pabloNo ratings yet
- 2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. RevisiónDocument12 pages2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. Revisiónjuan pabloNo ratings yet
- 2009 Rehabilitación Después de La Cirugía de Disco Lumbar. Actualización de Revisión CochraneDocument10 pages2009 Rehabilitación Después de La Cirugía de Disco Lumbar. Actualización de Revisión Cochranejuan pabloNo ratings yet
- 2020 Manual Therapy and Excercice in Temporomandibular Joint Disc Displacement Without Reduction. A Systematic ReviewDocument12 pages2020 Manual Therapy and Excercice in Temporomandibular Joint Disc Displacement Without Reduction. A Systematic Reviewjuan pabloNo ratings yet
- Narrative EssayDocument9 pagesNarrative Essaytk324No ratings yet
- Prebiotic and ProbioticDocument5 pagesPrebiotic and ProbioticIshan GhaiNo ratings yet
- 20 Spiritual Herbs For Activating Higher Consciousness, Awakening Intuition and Deep HealingDocument20 pages20 Spiritual Herbs For Activating Higher Consciousness, Awakening Intuition and Deep HealingLinda Pride100% (2)
- Lithium Carbonate (Lithicarb, Quilonum SR) : Information For PatientsDocument2 pagesLithium Carbonate (Lithicarb, Quilonum SR) : Information For PatientsgavinbuzzNo ratings yet
- 2011 Nosocomial Infections - Knowledge and Source of Information Among Clinical Health Care Students in GhanaDocument4 pages2011 Nosocomial Infections - Knowledge and Source of Information Among Clinical Health Care Students in GhanaMostafa AbdelrahmanNo ratings yet
- Infections of Dengue Viruses in Belgaum, Karnataka and India, Dengue in BelgaumDocument120 pagesInfections of Dengue Viruses in Belgaum, Karnataka and India, Dengue in BelgaumJ NuchinNo ratings yet
- Libro The Molecular Basis of Human Cancer William B. Coleman PHD, Gregory J. Tsongalis PHDDocument580 pagesLibro The Molecular Basis of Human Cancer William B. Coleman PHD, Gregory J. Tsongalis PHDBerenice LoredoNo ratings yet
- Rubric A3-HSNS362Document3 pagesRubric A3-HSNS362mandyNo ratings yet
- Herbal Medicine BSC Honours 2018 19 PDFDocument11 pagesHerbal Medicine BSC Honours 2018 19 PDFioanamarinelaNo ratings yet
- JLR-8600 Instruct Manual 1-3-2019Document180 pagesJLR-8600 Instruct Manual 1-3-2019Alan TanNo ratings yet
- DentalDocument4 pagesDentalBreeNo ratings yet
- PancreatitisDocument23 pagesPancreatitissalmanhabeebekNo ratings yet
- RtiDocument2 pagesRtiMexico EnglishNo ratings yet
- Epidemiology and The Web of Causation: Has Anyone Seen The Spider?Document17 pagesEpidemiology and The Web of Causation: Has Anyone Seen The Spider?prim1842No ratings yet
- Lasa Antasida: Ambroxol Tablet 30 MG Tablet Amoxicillin Tablet 500 MG Tablet 100 MGDocument6 pagesLasa Antasida: Ambroxol Tablet 30 MG Tablet Amoxicillin Tablet 500 MG Tablet 100 MGCilly ArliniNo ratings yet
- Bandung ISPN Course 2019 Final ReportDocument19 pagesBandung ISPN Course 2019 Final ReportMuhammad Azhary LazuardyNo ratings yet
- RPGNDocument13 pagesRPGNArun GeorgeNo ratings yet
- A. Checklist On Range of Motion Exercise (Rome)Document3 pagesA. Checklist On Range of Motion Exercise (Rome)Sheená EspañolNo ratings yet
- Loog Book Kardiologi Khusus-1Document8 pagesLoog Book Kardiologi Khusus-1marjuwarNo ratings yet
- Tracy EnfingerDocument4 pagesTracy Enfingerapi-364917278No ratings yet
- 6) RESPIRATORY MUSCLES by DR Hasnain NorthDocument28 pages6) RESPIRATORY MUSCLES by DR Hasnain NorthHasin's QueenNo ratings yet
- Atypical Serological Profile in Hepatitis B Virus InfectionDocument18 pagesAtypical Serological Profile in Hepatitis B Virus InfectionMai TuyếtNo ratings yet
- Group 4 - STKA BDocument4 pagesGroup 4 - STKA BNadia Izzatul AzkaNo ratings yet
- Tarip7komponen 2019newDocument632 pagesTarip7komponen 2019newB177Razy RizkiNo ratings yet
- Naturalmedicalmission PDFDocument509 pagesNaturalmedicalmission PDFkuralenthiNo ratings yet
- AST Standards of Practice For Surgical DrapesDocument7 pagesAST Standards of Practice For Surgical DrapesAyu PutriNo ratings yet
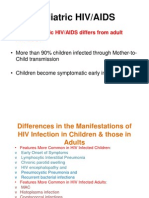
- Paediatric HIV Infection by DR A.K.Gupta, Additional Project Director, Delhi State AIDS Control SocietyDocument88 pagesPaediatric HIV Infection by DR A.K.Gupta, Additional Project Director, Delhi State AIDS Control Societydr.a.k.gupta6924No ratings yet