Professional Documents
Culture Documents
Tips For Patient Discharge Counseling From The Hospital Setting: Improving Adherence
Tips For Patient Discharge Counseling From The Hospital Setting: Improving Adherence
Uploaded by
Maab Alrsheed0 ratings0% found this document useful (0 votes)
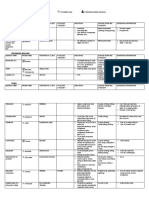
10 views3 pages1) When counseling psychiatric patients before discharge from the hospital, pharmacists should emphasize medication adherence as paramount to positive outcomes. They should describe common and severe side effects and ways to manage them.
2) Pharmacists should remind patients about follow-up appointments with psychiatrists and labs, and the need for long-term monitoring of their condition. They should also discuss any long-acting injection medications.
3) Filling initial prescriptions for patients before discharge can help alleviate non-adherence and encourage patients in their recovery.
Original Description:
Original Title
Rtjjvjbcccf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1) When counseling psychiatric patients before discharge from the hospital, pharmacists should emphasize medication adherence as paramount to positive outcomes. They should describe common and severe side effects and ways to manage them.
2) Pharmacists should remind patients about follow-up appointments with psychiatrists and labs, and the need for long-term monitoring of their condition. They should also discuss any long-acting injection medications.
3) Filling initial prescriptions for patients before discharge can help alleviate non-adherence and encourage patients in their recovery.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
10 views3 pagesTips For Patient Discharge Counseling From The Hospital Setting: Improving Adherence
Tips For Patient Discharge Counseling From The Hospital Setting: Improving Adherence
Uploaded by
Maab Alrsheed1) When counseling psychiatric patients before discharge from the hospital, pharmacists should emphasize medication adherence as paramount to positive outcomes. They should describe common and severe side effects and ways to manage them.
2) Pharmacists should remind patients about follow-up appointments with psychiatrists and labs, and the need for long-term monitoring of their condition. They should also discuss any long-acting injection medications.
3) Filling initial prescriptions for patients before discharge can help alleviate non-adherence and encourage patients in their recovery.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 3
Tips for patient discharge counseling from the hospital setting: Improving
adherence
John R. Tomko (Randy), PharmD, BCPP
Assistant Professor and Clinical Pharmacy Specialist
Duquesne University Mylan School of Pharmacy and UPMC Mercy Hospital, Pittsburgh, PA
KEYWORDS
Discharge counseling, adherence, pharmacist
Psychiatric pharmacists make a constant effort to are both medication as well as non-medication related
Downloaded from http://meridian.allenpress.com/mhc/article-pdf/2/8/240/2094678/mhc_n133122.pdf by Sudan user on 28 August 2021
improve patient’s psychiatric outcomes while minimizing issues that should be articulated and emphasized with
the untoward side effects that can occur as a result of patients to improve overall patient care outcomes in the
taking psychiatric medications. Once patients show an psychiatric populations. Performing these tasks at or prior
adequate response, and ultimately remission, of to discharge can aid in transitioning the patient from a
psychiatric symptoms, many may conclude that patients controlled hospital environment to success in the
will continue improvement for the foreseeable future. outpatient setting.
Those who have experience with psychiatric
4. Describe the incidence and relative severity of specific
pharmacotherapy know otherwise. Medication adherence
adverse effects of medications and suggest methods
is the ultimate long term goal in both the medical and
of management. Some of the drug information
psychiatric populations in order to maintain sustained
provided to patients by their pharmacy as a result of
illness remission; however, it is known that adherence
the Omnibus Budget Reconciliation Act of 1990
rates are far below what is optimal.1 It has been estimated
(OBRA 90) may be overwhelming and confusing. Lists
that approximately 50% of patients become non-
of possible adverse effects, while comprehensive,
adherent with medications within a short period of time.2
may intimidate patients and lead to possible non-
The reasons for this vary. Some of the reasons are
adherence. Provide patients with a brief handout
economic, lack of insight into illness, misunderstanding of
which reviews the most common side effects,
care goals, or even stigma of mental illness.3, 4, 5 Each of
management strategies, and the incidence of their
these can facilitate medication non-adherence, leading
occurrence. These effects can be further divided into
patients to discontinue medications, remain ill, or seek
two categories; one that requires immediate
readmission to the acute hospital unit.
physician notification, and the other which should be
Pharmacists have provided patients with pharmaceutical discussed at the next visit. Providing perspective and
care for years. Helping patients understand their clarity to the relative risks of side effects may calm
medications’ role in their recovery from illness, while patient apprehension regarding psychiatric
simultaneously educating them on possible side effects medications and improve adherence.
and the management of these effects, are some of the 5. Emphasize the need for long term monitoring,
services that pharmacists frequently participate in.6 In including laboratory tests and psychiatric evaluation.
recent years, the concept of medication therapy Psychiatric symptomatology may wax and wane over
management has been introduced, expanding the time with the introduction of life or physiologic
traditional pharmacist roles with the addition of patient stressors. Accentuating the need for adherence to
follow-up and ongoing care management.7 While follow-up psychiatric and physical assessment on a
medication provision and counseling encompass the scheduled basis is essential. This may seem
primary care roles of the pharmacist, there are many elementary, but patients should be aware of their
facets of care that a psychiatric pharmacist must next appointment with their psychiatrist and have
incorporate into patient interactions in order to afford the that information reiterated by the pharmacist at
best opportunity for long-term treatment success and discharge. In addition to psychiatric assessment, the
positive outcomes. patient should be reminded that some of their
medications require periodic laboratory testing to
When counseling patients prior to discharge, medication
avoid adverse events or insure that serum drug levels
adherence is paramount to positive outcomes. Yet there
Mental Health Clinician, February 2013, Vol. 2, Issue 8 240
are appropriate. Educating the patient on the periodic to discuss the integrative role of these treatments
need for these tests gives an opportunity for with medications may prevent patients from
pharmacists to allay patient apprehensions, achieving optimal outcomes. Thus, adherence to
disarming a potential reason for non-adherence. appointments with psychologists, therapists, or
6. Counsel patients on any prescribed long-acting counselors should be included in patient counseling,
antipsychotic injections prior to discharge. Don’t and these appointment dates should be added to the
forget about these! Patients may have prescriptions patient’s outpatient care plan.
for oral medications upon hospital discharge, but 9. If possible, have an initial supply of medications filled
forgetting about outpatient administration of long- for patients at discharge. Having an ambulatory
acting injections may bring about serious pharmacy in or near the hospital can help to facilitate
consequences for the patient, leading to potential this. Develop a system where faxing of prescriptions
non-adherence and possible rehospitalization. Since to the pharmacy and delivery of initial supplies can be
Downloaded from http://meridian.allenpress.com/mhc/article-pdf/2/8/240/2094678/mhc_n133122.pdf by Sudan user on 28 August 2021
the depot injection may have been administered accomplished. Discharge counseling for patients with
during the acute hospital admission, the importance the presence of their filled prescriptions is well
of attending the next scheduled injection needs to be accepted by patients and provides the patient with a
discussed. Patients may or may not have an actual visual learning experience prior to discharge. Filling
prescription for this type of medication when an initial supply of psychiatric medications for
discharged. Pharmacists should investigate the patients helps to alleviate the opportunity for non-
administration date and location during hospital adherence by failing to fill prescriptions after
admission and proactively counsel the patient prior to discharge. Patients can then be discharged with their
discharge. Discussion on these medications should medications, not just a prescription.
include the date and place of the next administration Findings suggest that the addition of these key points to
as well as management of the potential unique side medication discharge counseling, coupled with providing
effects of these drugs. the patient with filled prescriptions for their psychiatric
7. Obtain necessary medication prior authorizations. medications immediately at discharge can decrease 30
Since insurance plans may require prior day rapid readmission between 35 and 50%.11
authorizations for coverage of certain medications,
Employing these tips can help to prevent rapid
failure to obtain these may lead to delays in obtaining
readmission to the hospital, encourage medication
medications upon discharge. This can be discouraging
adherence in the initial acute phase of treatment
for patients. While waiting for an inadvertently
following hospitalization, and give patients the
missed authorization, patients may leave their
opportunity to be treated in a less intrusive outpatient
pharmacy, causing unnecessary delays in care or
setting. Not only can these improve patient quality of life,
avoidable non-adherence. If these medications are
but they can increase hospital bed availability, leading to
identified during admission, and prior authorizations
better stewardship of precious acute care resources.
obtained, patients can receive their medications in a
timely manner in the community. This avoidable REFERENCES
adherence issue, if not addressed, may cause 1. Hayes, RB. NCPIE Prescription Month, October 1989.
2. Akhunzada WA, Dogar IA, Rahman R, Maqsood N. Depression and drug
psychiatric decompensation and subsequent non-adherence. Professional Med J. Jun 2010;17(2):340-346.
rehospitalization. 3. Sullivan G, Wells KB, Morgenstern H, Leake B. Identifying modifiable risk
8. Reiterate the importance of non-pharmacologic factors for rehospitalization: a case-control study of seriously mentally ill
persons in Mississippi. Am J Psychiatry. 1995;152(12):1749-56.
means of care following discharge. Mental illnesses 4. Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and
such as major depressive disorder and anxiety risk factors for medication nonadherence in patients with schizophrenia. J.
disorders (including OCD and PTSD) respond well to Clin. Psychiatry. 2002;63(10):892- 909. DOI: 10.4088/JCP.v63n1007.
5. Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J, Weiden PJ.
various forms of talk therapies. Adherence to these Predicting medication noncompliance after hospital discharge among
forms of treatment should be discussed during patients with schizophrenia. Psychiatr Serv. 2000;51(2):216-22. PubMed
PMID: 10655006.
patient counseling sessions. Combination therapy 6. Hepler CD, Strand LM. Opportunities and responsibilities in
with medications and CBT or other psychotherapies pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533-43. PubMed
provide for more rapid resolution of symptoms in PMID: 2316538.
7. American Pharmacists Association. Medication Therapy Management in
depressive disorders and anxiety disorders.8,9,10 Other Pharmacy Practice: Core Elements of and MTM Service Model. Available
therapies such as Interpersonal and Social Rhythm at
Therapy (IPSRT) are helpful in mood disorders. Failure http://www.pharmacist.com/sites/default/files/files/core_elements_of_an
_mtm_practice.pdf. Accessed 19 Oct 2012.
Mental Health Clinician, February 2013, Vol. 2, Issue 8 241
8. Bowers WA. Treatment of depressed in-patients. Cognitive therapy plus
medication, relaxation plus medication, and medication alone. Br J
Psychiatry. 1990;156(1):73- 78. DOI: 10.1192/bjp.156.1.73.
9. Blom MBJ, Jonker K, Dusseldorp E, Spinhoven P, Hoencamp E, Haffmans
J, et al. Combination treatment for acute depression is superior only when
psychotherapy is added to medication. Psychother Psychosom.
2007;76(5):289-97. DOI: 10.1159/000104705. PubMed PMID: 17700049.
10. Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral
therapy, imipramine, or their combination for panic disorder: A
randomized controlled trial. JAMA. 2000;283(19):2529-36. PubMed PMID:
10815116.
11. Tomko JR, Ahmed N, Mukherjee K, Roma RS, DiLucente D, Orchowski K.
Evaluation of a discharge medication program in an acute psychiatric unit.
Hosp Pharm. 2013;48(4):314-20. DOI: 10.1310/hpj4804-314.
How to cite this editor-reviewed article
Downloaded from http://meridian.allenpress.com/mhc/article-pdf/2/8/240/2094678/mhc_n133122.pdf by Sudan user on 28 August 2021
Tomko JR. Tips for patient discharge counseling from the hospital setting;
Improving adherence. Ment Health Clin [Internet]. 2013;2(8):240-2. Available
from: http://dx.doi.org/10.9740/mhc.n133122
Mental Health Clinician, February 2013, Vol. 2, Issue 8 242
You might also like
- Mischs Contemporary Implant Dentistry Randolph R Resnik DMD Mds Full ChapterDocument67 pagesMischs Contemporary Implant Dentistry Randolph R Resnik DMD Mds Full Chapterlinda.landfair766100% (19)
- PPCCMidterm Study Guide 1Document5 pagesPPCCMidterm Study Guide 1Kaitlyn CabreraNo ratings yet
- Writing Multiple-Choice QuestionsDocument7 pagesWriting Multiple-Choice QuestionsStanislav Sevostyanov0% (1)
- Assessment 2 - Nursing Case Study - 2019Document2 pagesAssessment 2 - Nursing Case Study - 2019Chinney ArceNo ratings yet
- Statements Pharmaceutical CareDocument3 pagesStatements Pharmaceutical CareDiegoAndrésYiZapataNo ratings yet
- NBHS1404 Pharmacology For NursesDocument7 pagesNBHS1404 Pharmacology For Nursessentamilarsi arumugamNo ratings yet
- Medical AdherenceDocument12 pagesMedical AdherenceCristine Loh100% (2)
- Lecture 3. General Guidelines For Clinical Pharmacy PracticeDocument22 pagesLecture 3. General Guidelines For Clinical Pharmacy Practicedaniya nadeem100% (1)
- Best Practice1 Covert Admin MedicinesDocument2 pagesBest Practice1 Covert Admin MedicinesNur NazurahNo ratings yet
- Communication Skills in Pharmacy PracticeDocument7 pagesCommunication Skills in Pharmacy PracticemasorNo ratings yet
- Pharmacology Unit 2Document19 pagesPharmacology Unit 2Bea Bianca CruzNo ratings yet
- Guidelines On Counseling: Approved by PEIPBDocument7 pagesGuidelines On Counseling: Approved by PEIPBEric Chye TeckNo ratings yet
- Psychiatric Pharmacyst Integration in To The Medical HomeDocument5 pagesPsychiatric Pharmacyst Integration in To The Medical HomeAdeyemi OlusolaNo ratings yet
- Lack of Patient CounselingDocument15 pagesLack of Patient CounselingAzan AhmadNo ratings yet
- Adherence To Potent Antiretroviral TherapyDocument5 pagesAdherence To Potent Antiretroviral TherapyGabrieela SiguiNo ratings yet
- Clinical Pharmacists' Role in Paediatric Patients' Medical CareDocument5 pagesClinical Pharmacists' Role in Paediatric Patients' Medical CareHaseeba KhanNo ratings yet
- Review of Pharmaceutical Care Services Provided by The PharmacistsDocument3 pagesReview of Pharmaceutical Care Services Provided by The PharmacistsellianaeyNo ratings yet
- Drug Use EvaluationDocument27 pagesDrug Use Evaluationshanthi dasariNo ratings yet
- Org STP Harm CareDocument3 pagesOrg STP Harm CarelatemmaNo ratings yet
- Effect of Pharmacy Intervention To Patient With Polypharmacy - JournalDocument7 pagesEffect of Pharmacy Intervention To Patient With Polypharmacy - Journalanon_529380518No ratings yet
- Principles of Drug Addiction TreatmentDocument3 pagesPrinciples of Drug Addiction TreatmentMarc Kevin Garcia AretaNo ratings yet
- Basic - Concepts - in - Pharmaceutical - Care CLINICAL PHARMACYDocument17 pagesBasic - Concepts - in - Pharmaceutical - Care CLINICAL PHARMACYPrincess RonsableNo ratings yet
- Maintenan Bipolar With FarmakoEvid Based Mental Health-2014-Malhi-eb-2014-101948Document7 pagesMaintenan Bipolar With FarmakoEvid Based Mental Health-2014-Malhi-eb-2014-101948amro7190No ratings yet
- Pharm Care 4 Chapter 1Document25 pagesPharm Care 4 Chapter 1MaraNagaSambarani100% (1)
- Anesthesia Books 2019 Bonica's-2001-3000Document845 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- 1-29-20 Diabetes Protocol Draft With Pandya and Alvarez EditsDocument12 pages1-29-20 Diabetes Protocol Draft With Pandya and Alvarez Editsapi-552486649No ratings yet
- Administration of Psychotropic DrugsDocument22 pagesAdministration of Psychotropic DrugsdhivyaramNo ratings yet
- Deprescribing Techniques To Minimize Safety Issues Associated With Inappropriate Polypharmacy 2021 THE OREGONDocument4 pagesDeprescribing Techniques To Minimize Safety Issues Associated With Inappropriate Polypharmacy 2021 THE OREGONGERIATRIA 72No ratings yet
- Conceptos Básicos Farmacoterapeutica Melmon y Morelli - OcrDocument5 pagesConceptos Básicos Farmacoterapeutica Melmon y Morelli - Ocrdaniela rodriguezNo ratings yet
- 93 M Deatials PDFDocument5 pages93 M Deatials PDFRatna RoesardhyatiNo ratings yet
- Translator Apr2010 Vo4 Iss1Document4 pagesTranslator Apr2010 Vo4 Iss1Vina Angga RiniNo ratings yet
- Patient Medication Adherence PDFDocument5 pagesPatient Medication Adherence PDFAlexandrahautaNo ratings yet
- 1268 PDFDocument5 pages1268 PDFCMargs ConceptsNo ratings yet
- Ward Round Participation & Drug Therapy MonitoringDocument20 pagesWard Round Participation & Drug Therapy MonitoringAman UpadhyayNo ratings yet
- Done By: Assis - Lec. Lubab Tarek NafeaDocument29 pagesDone By: Assis - Lec. Lubab Tarek Nafeadugasanuguse1No ratings yet
- Compliance and AdheranceDocument56 pagesCompliance and Adherancetf.almutairi88100% (1)
- Anesthesia Books 2019 Bonica's-2001-3000Document1,000 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- Kevin L. Villarante BSN-II Nur104 Pharmacology Ii 1. Outline The Steps Involved in Developing and Approving A New DrugDocument8 pagesKevin L. Villarante BSN-II Nur104 Pharmacology Ii 1. Outline The Steps Involved in Developing and Approving A New DrugKevin VillaranteNo ratings yet
- Unit 1. Clinical PharmacyDocument5 pagesUnit 1. Clinical PharmacyAashish BhattaraiNo ratings yet
- Drug Therapy Monitoring and Pharmaceutical CareDocument48 pagesDrug Therapy Monitoring and Pharmaceutical CareHarsh Bhardwaj100% (1)
- Preventing Misuse of Medicines DR - Marwa Salih Al-NaimiDocument12 pagesPreventing Misuse of Medicines DR - Marwa Salih Al-NaimiMustafa MuayedNo ratings yet
- Outpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020Document37 pagesOutpatient Pharmacy: Course Name: Hospital Training Course Code: PHD311 Date: 22 October 2020honeylemon.coNo ratings yet
- Pharmaceutical CareDocument7 pagesPharmaceutical Caresomayya waliNo ratings yet
- Medication Nonadherence and Psychiatry: ReviewDocument7 pagesMedication Nonadherence and Psychiatry: ReviewVidho RiveraNo ratings yet
- Adherence MedicationDocument12 pagesAdherence Medicationb.modNo ratings yet
- Role of Pharmacist Finale FatimaDocument5 pagesRole of Pharmacist Finale FatimafaramaNo ratings yet
- Medication Errors Their Causative and Preventive Factors2.Doc 1Document11 pagesMedication Errors Their Causative and Preventive Factors2.Doc 1Mary MannNo ratings yet
- Medicine Use Evaluation: A Guide To ImplementationDocument26 pagesMedicine Use Evaluation: A Guide To ImplementationmrboredguyNo ratings yet
- 10 TH Conf Poly PharmacyDocument5 pages10 TH Conf Poly Pharmacytr14niNo ratings yet
- Session 4 GeronDocument18 pagesSession 4 Geronjuancarlosfetalvero17No ratings yet
- Medication ErrorDocument7 pagesMedication ErrorLenny SucalditoNo ratings yet
- Medication AdherenceDocument36 pagesMedication AdherenceDr-Jagadeesh MangamooriNo ratings yet
- 4Document5 pages4Creepy PotatoesNo ratings yet
- Phm423: Clinical Pharmacy Week 1: Introduction: Hadassah M. Reyes-Cendana, RPH January 2022Document36 pagesPhm423: Clinical Pharmacy Week 1: Introduction: Hadassah M. Reyes-Cendana, RPH January 2022Hadassah ReyesNo ratings yet
- Daily Activity of Clinical PharmacistDocument18 pagesDaily Activity of Clinical PharmacistŖÖŸÄĻ ŚÏVÄッNo ratings yet
- Drug Therapy MonitoringDocument38 pagesDrug Therapy MonitoringSumanth100% (1)
- Course: Patient Safety Solutions Topic:: Some DefinitionsDocument5 pagesCourse: Patient Safety Solutions Topic:: Some DefinitionsKian GonzagaNo ratings yet
- Correspondence: Prof. Saeed Farooq, MCPS, FCPS, Professor Department ofDocument2 pagesCorrespondence: Prof. Saeed Farooq, MCPS, FCPS, Professor Department ofKaram Ali ShahNo ratings yet
- Pharmacoepidemiology: Drug-Related Problems: Their Structure and FunctionDocument5 pagesPharmacoepidemiology: Drug-Related Problems: Their Structure and FunctionhukamaNo ratings yet
- Becker 1980Document23 pagesBecker 1980Lorena PăduraruNo ratings yet
- Prescribing&mdash The: of AllDocument5 pagesPrescribing&mdash The: of AllKaraengGalesongNo ratings yet
- Drug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingFrom EverandDrug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingNo ratings yet
- NR 222 Health and Wellness Final Exam Study GuideDocument6 pagesNR 222 Health and Wellness Final Exam Study GuideNelson MandelaNo ratings yet
- Definition/Description: Types of SyringomyeliaDocument8 pagesDefinition/Description: Types of SyringomyeliaNurfadiyah YasinNo ratings yet
- Injection 101: Overview, Types, Common Uses & Risks: What Is An Injection?Document1 pageInjection 101: Overview, Types, Common Uses & Risks: What Is An Injection?Barbara Akua AntwiNo ratings yet
- Self Declaration Form Details For International Arriving PassengersDocument2 pagesSelf Declaration Form Details For International Arriving PassengersSharafat AliNo ratings yet
- Project Propasal FormatDocument12 pagesProject Propasal FormatPeter Osundwa KitekiNo ratings yet
- MR (Medical Representative) - 28Document2 pagesMR (Medical Representative) - 28rakesharain123No ratings yet
- OT Practice December 17 IssueDocument24 pagesOT Practice December 17 IssueThe American Occupational Therapy Association100% (1)
- Sdo PM QF Sgod SHN 001 Students Health Card ElementaryDocument3 pagesSdo PM QF Sgod SHN 001 Students Health Card ElementaryShiela E. EladNo ratings yet
- Ranula Management: Suggested Modifications in The Micro-Marsupialization TechniqueDocument3 pagesRanula Management: Suggested Modifications in The Micro-Marsupialization Techniquemehak malhotraNo ratings yet
- Pediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsDocument2 pagesPediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsBobet Reña100% (2)
- Ahuja Book Company PVT LTD.,: 4348/4C, Ansari Road, Darya Ganj, New Delhi - 110 002Document27 pagesAhuja Book Company PVT LTD.,: 4348/4C, Ansari Road, Darya Ganj, New Delhi - 110 002Roshan KumarNo ratings yet
- A Guide To What Works For DepressionDocument96 pagesA Guide To What Works For DepressionLynda HernandezNo ratings yet
- Renal Pathology Blok 13Document71 pagesRenal Pathology Blok 13Arsy Mira PertiwiNo ratings yet
- First Aid Kit ListDocument2 pagesFirst Aid Kit ListLoyd Christian MoradaNo ratings yet
- Apatan, John Carlo SenaderoDocument1 pageApatan, John Carlo SenaderoJOHN CARLO APATANNo ratings yet
- ND RDDocument10 pagesND RDOdyNo ratings yet
- Pregnancy Hypertension: An International Journal of Women's Cardiovascular HealthDocument8 pagesPregnancy Hypertension: An International Journal of Women's Cardiovascular HealthIsmael RoseroNo ratings yet
- Temar Diagnostics (Head Office) : Clinical PathologyDocument1 pageTemar Diagnostics (Head Office) : Clinical PathologyJaadi 786No ratings yet
- PCD Commercially Available Devices and Systems 2014 AprilDocument3 pagesPCD Commercially Available Devices and Systems 2014 AprilPedro de LaraNo ratings yet
- The Story of DentistryDocument4 pagesThe Story of DentistryImelda Fabiola Cortez RomeroNo ratings yet
- Daftar Pustaka YyyahahajshDocument7 pagesDaftar Pustaka YyyahahajshDiki NugrahaNo ratings yet
- Harga ObatDocument5 pagesHarga Obathilman fauzanNo ratings yet
- Pharmacovigilance Programme ofDocument4 pagesPharmacovigilance Programme ofpavani valluriNo ratings yet
- 2 Nursing Care PlanDocument3 pages2 Nursing Care PlanJay Ar YasolNo ratings yet
- Ast-Ys08 Vitex 2Document12 pagesAst-Ys08 Vitex 2ambarNo ratings yet
- Curs 15v-2018hDocument96 pagesCurs 15v-2018hMirceaDraghiciNo ratings yet
- Ramachari Anaesthesiologist-Brief BiodataDocument1 pageRamachari Anaesthesiologist-Brief Biodatadr_saketram6146No ratings yet