Professional Documents
Culture Documents
Procoagulant Platelet Potential Is Inversely Correlated With Bleedi - 2018 - Blo
Procoagulant Platelet Potential Is Inversely Correlated With Bleedi - 2018 - Blo
Uploaded by
Michael John AguilarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Procoagulant Platelet Potential Is Inversely Correlated With Bleedi - 2018 - Blo
Procoagulant Platelet Potential Is Inversely Correlated With Bleedi - 2018 - Blo
Uploaded by
Michael John AguilarCopyright:
Available Formats
322.
DISORDERS OF COAGULATION OR FIBRINOLYSIS: POSTER I | NOVEMBER 29, 2018
Procoagulant Platelet Potential Is Inversely Correlated
with Bleeding and Joint Disease in Severe Hemophilia A
1,2 3,4 *,5
Shawn M. Jobe, MD PhD, Amy L. Dunn, MD, Traci Leong, PhD
1
Pediatrics, Medical College of Wisconsin, Milwaukee, WI
2
Blood Research Institute, Blood Center of Wisconsin, Milwaukee, WI
3
Division of Hematology/Oncology/BMT, Nationwide Childrens Hospital, Columbus, OH
4
The Ohio State University, Columbus, OH
5
Department of Biostatistics and Bioinformatics, Emory University, Atlanta, GA
Blood (2018) 132 (Supplement 1) : 1185.
http://doi.org/10.1182/blood-2018-99-117989
Abstract
The variability of clinical phenotype in patients with severe hemophilia A (factor VIII activity < 1%)
has been well established, currently and in the era prior to wide-spread prophylaxis. The introduction
of prophylaxis as a treatment modifier of the natural history of severe hemophilia A has led to the
introduction of composite scores to assist in the assessment of disease severity. Perhaps the most
prominent of these is that proposed by Schulman et al (J Thromb Haem 2008;6(7):1113-21) which utilizes
three domains of phenotypic presentation to characterize a patient's clinical phenotype, acute (annualized
bleeding rate), chronic (joint status), and treatment intensity (normalized factor usage). However, the
biologic mechanisms driving this variability in clinical phenotype continue to remain largely uncertain.
Procoagulant platelet potential is an individual's ability to generate procoagulant platelets in response
to a standard concentration of agonist. This response, which generates platelets capable of intensely
supporting coagulation, tends to remain relatively constant and varies substantially between individuals.
A few small case-control studies have investigated the role of procoagulant platelet potential or platelet-
supported thrombin generation in mediating the phenotypic variability with discordant results.
The relationship of procoagulant platelet potential and platelet-supported thrombin generation to
phenotypic severity was investigated in a single-center cohort of 92 pediatric and adult severe hemophilia
A patients without active inhibitors. Procoagulant platelet potential (defined as the ratio of procoagulant
platelets / all activated platelets following stimulation with thrombin (0.5 units/mL) and convulxin (250 ng/
mL)) and the expression of other platelet activation markers, including P-selectin (granule release) and
PAC-1 (integrin activation) were investigated in washed platelets. Platelet-dependent thrombin generation
was investigated in a limited cohort (45) of these patients. Phenotypic data was collected in regard to
reported bleeding events over the past 5 years, joint health using the hemophilia joint health score,
intensity of factor therapy, and therapeutic intent (prophylaxis or on-demand). Correlations were assessed
as continuous variables using regression analysis with p <0.05 deemed significant.
Procoagulant platelet potential was inversely correlated with both acute (annualized bleeding rate) (r =
-0.47, p = 0.0006) and chronic measures (joint score) (r = -0.38, p = 0.0001) of phenotypic severity. In
contrast, when platelet-dependent thrombin generation or other markers of thrombin or GPVI-dependent
platelet activation potential were assessed i.e. P-selectin expression or PAC-1, no correlation was
identified with either acute or chronic measures of phenotypic severity or with the HSS composite
score. Surprisingly, when the composite score of HSS as defined by Schulman (acute + chronic +
factor utilization) was utilized to assess a potential relationship this correlation was not observed.
Further analysis revealed that this lack of correlation was due to the fact that therapeutic intensity (factor
utilization) was directlycorrelated with procoagulant platelet potential (r = 0.54, p = 0.0006).
Here we have identified a potentially critical role for procoagulant platelets as biologic modifiers of
hemophilia A. Furthermore, we have identified a risk associated with the use of a composite score in
assessing disease severity in hemophilia. Utilization of a composite score as the sole measure would
have missed the significant effects noted in each of the individual domains. Procoagulant platelets both
support thrombin generation and inflammatory cell recruitment. Thus, one potential hypothesis for these
opposing effects on the domains of the composite score is that increased procoagulant platelet formation
supports stable hemostatic plug formation (reduced bleeding rate) or increases inflammatory presentation
resulting in therapy intensification or both. Finally, our results here point towards new tools and pathways
for risk stratification and therapeutic modulation in patients with hemophilia A based on assessment of
procoagulant platelet potential.
Disclosures
Jobe: Shire: Consultancy; Octapharma: Consultancy; CSL: Consultancy.
Author notes
* Asterisk with author names denotes non-ASH members.
© 2018 by the American Society of Hematology
You might also like
- A Dowry of A Single GalleonDocument159 pagesA Dowry of A Single GalleonAdele D'souzaNo ratings yet
- Chap 24Document16 pagesChap 24Phú NguyễnNo ratings yet
- A Is For Allah J Is For JihadDocument6 pagesA Is For Allah J Is For JihadJobhiyar7123No ratings yet
- Platelet Dependent Thrombin Generation Is Correlated With Phenotypi - 2017 - BloDocument2 pagesPlatelet Dependent Thrombin Generation Is Correlated With Phenotypi - 2017 - BloMichael John AguilarNo ratings yet
- Breakthrough Bleeding in Hemophilia A Patients On ProphylaxisDocument4 pagesBreakthrough Bleeding in Hemophilia A Patients On ProphylaxisMichael John AguilarNo ratings yet
- Efficacy of Red Blood Cell Transfusion in The Critically Ill (Original Article)Document8 pagesEfficacy of Red Blood Cell Transfusion in The Critically Ill (Original Article)Rayhan OemarNo ratings yet
- Assessment of Bleeding Phenotype in Hemophilia: Α By a Novel Point-of-Care Global AssayDocument4 pagesAssessment of Bleeding Phenotype in Hemophilia: Α By a Novel Point-of-Care Global AssayMichael John AguilarNo ratings yet
- Immune Tolerance Induction ITI With A Plasma Derived Factor VIII F - 2019 - BLDocument4 pagesImmune Tolerance Induction ITI With A Plasma Derived Factor VIII F - 2019 - BLMichael John AguilarNo ratings yet
- Verma 2009Document15 pagesVerma 2009Zorobabel AzondogaNo ratings yet
- Indications For Platelet Transfusion in Children With Acute LeukemiaDocument10 pagesIndications For Platelet Transfusion in Children With Acute LeukemiaAbidi HichemNo ratings yet
- A Double-Blind, Placebo-Controlled Trial of Ruxolitinib For MyelofibrosisDocument9 pagesA Double-Blind, Placebo-Controlled Trial of Ruxolitinib For MyelofibrosisharlessitompulNo ratings yet
- Epidemiology of Familial Hypercholesterolaemia CoDocument9 pagesEpidemiology of Familial Hypercholesterolaemia CoSusana RocheNo ratings yet
- 2303 FullDocument19 pages2303 Fullnurul annisaNo ratings yet
- An Etiological Reappraisal of Pancytopenia - LargestDocument9 pagesAn Etiological Reappraisal of Pancytopenia - LargestKaye Antonette AntioquiaNo ratings yet
- The Predictive Value of Four Serum Biomarkers ForDocument8 pagesThe Predictive Value of Four Serum Biomarkers Forsebasags19No ratings yet
- Flowcytometric Assessment of Activated Cytotoxic T Cells in Rapid Diagnosis of Hemophagocytic Lymphohistiocytosis in Pediatric PatientsDocument1 pageFlowcytometric Assessment of Activated Cytotoxic T Cells in Rapid Diagnosis of Hemophagocytic Lymphohistiocytosis in Pediatric Patientsgocelij948No ratings yet
- The Use of Chromogenic Factor VIII Assay Changes Treatment Approach - 2019 - BLDocument3 pagesThe Use of Chromogenic Factor VIII Assay Changes Treatment Approach - 2019 - BLMichael John AguilarNo ratings yet
- Use of Blood Product in SepsisDocument6 pagesUse of Blood Product in SepsisAditya IrawanNo ratings yet
- Angiogenesis: What We Know, What We Do Not Understand Yet, and What We Have To DoDocument2 pagesAngiogenesis: What We Know, What We Do Not Understand Yet, and What We Have To DoAnca Maria CimpeanNo ratings yet
- 2015 Article 244Document8 pages2015 Article 244nasar adenNo ratings yet
- Miyata 2006Document7 pagesMiyata 2006Mestre O ToloNo ratings yet
- BiologicDocument13 pagesBiologicGabriela BichirNo ratings yet
- Children LeukemiaDocument6 pagesChildren LeukemiakemalmiaNo ratings yet
- 8 PDFDocument8 pages8 PDFBaru Chandrasekhar RaoNo ratings yet
- Blood Loss and Clinical SignsDocument10 pagesBlood Loss and Clinical SignsElias Emmanuel JaimeNo ratings yet
- Review of Current Transfusion Therapy and Blood Banking PracticesDocument52 pagesReview of Current Transfusion Therapy and Blood Banking PracticesAmaranto SantosoNo ratings yet
- The Clinical Associations and Outcomes of Patients Admitted With Acq - 2015 - BLDocument3 pagesThe Clinical Associations and Outcomes of Patients Admitted With Acq - 2015 - BLMichael John AguilarNo ratings yet
- Prevalence Patterns and Factors Associated With Bleeding Tendencies in DengueDocument6 pagesPrevalence Patterns and Factors Associated With Bleeding Tendencies in DengueSawettachai JaitaNo ratings yet
- Hemoglobin Targets For The Anemia in Patients With Dialysis Dependent Chronic Kidney Disease A Meta Analysis of Randomized Controlled TrialsDocument10 pagesHemoglobin Targets For The Anemia in Patients With Dialysis Dependent Chronic Kidney Disease A Meta Analysis of Randomized Controlled TrialsDesi MeliaNo ratings yet
- Genetics of Hypertension: The Lack of EvidenceDocument11 pagesGenetics of Hypertension: The Lack of EvidenceInternational Medical PublisherNo ratings yet
- CC 9290Document12 pagesCC 9290elektifppra2022No ratings yet
- Shinchiro Oshima 2018Document6 pagesShinchiro Oshima 2018Bogdan NeamtuNo ratings yet
- Influence of Transfusions, Hemodialysis and Extracorporeal Life Support On Hyperferritinemia in Critically Ill PatientsDocument12 pagesInfluence of Transfusions, Hemodialysis and Extracorporeal Life Support On Hyperferritinemia in Critically Ill PatientsAmalNo ratings yet
- Artículo OriginalDocument9 pagesArtículo OriginalMariana MoraNo ratings yet
- Folic Acid in Stroke Prevention in Countries Without MandatoryDocument16 pagesFolic Acid in Stroke Prevention in Countries Without MandatoryAzka SamalNo ratings yet
- Coagulation Changes in Individuals With Sickle Cell TraitDocument6 pagesCoagulation Changes in Individuals With Sickle Cell TraitMohaNo ratings yet
- TransfusiDocument10 pagesTransfusiDevia PebriyentiNo ratings yet
- Motiei Langroudi2019Document5 pagesMotiei Langroudi2019LailNo ratings yet
- A Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimDocument14 pagesA Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimNo NameNo ratings yet
- Blood in TraumaDocument17 pagesBlood in TraumaEmtha SeeniNo ratings yet
- Hemorragia Obstetrica 2018 EstrategiasDocument3 pagesHemorragia Obstetrica 2018 EstrategiasSandra SayayNo ratings yet
- Quite Possibly The Most Ignored Thing Around Kinase Inhibitors.20140816.070713Document2 pagesQuite Possibly The Most Ignored Thing Around Kinase Inhibitors.20140816.070713bailstick37No ratings yet
- Singer-Alloimmunization and Erythrocyte Autoimmunization in Transfusion-DependentDocument5 pagesSinger-Alloimmunization and Erythrocyte Autoimmunization in Transfusion-DependentFatimatuzzahra ShahabNo ratings yet
- Citom NeoplasiasHemat Rev2008Document28 pagesCitom NeoplasiasHemat Rev2008liliana_solari_1No ratings yet
- Sanchez-Aguilera Blood2006 HLexpressionProfilingDocument8 pagesSanchez-Aguilera Blood2006 HLexpressionProfilingAbelSanchezANo ratings yet
- Modul Praktikum PK UrogenitalDocument8 pagesModul Praktikum PK UrogenitalfxkryxieNo ratings yet
- Jama Neal 2023 Ed 230070 1696973944.14124Document2 pagesJama Neal 2023 Ed 230070 1696973944.14124Luz Elena ValderramaNo ratings yet
- Association Between Serum Lipids and Survival in Hemodialysis Patients and Impact of RaceDocument11 pagesAssociation Between Serum Lipids and Survival in Hemodialysis Patients and Impact of RaceJuanCarlosGonzalezNo ratings yet
- Hyperuricemia and Risk of Stroke: A Systematic Review and Meta-AnalysisDocument8 pagesHyperuricemia and Risk of Stroke: A Systematic Review and Meta-AnalysisAnwar Shah SyedNo ratings yet
- Advances in The Treatment of Sickle CellDocument15 pagesAdvances in The Treatment of Sickle CellMayuri P KNo ratings yet
- Editorial: Jai RadhakrishnanDocument2 pagesEditorial: Jai RadhakrishnanLis Borda MuñozNo ratings yet
- NIH Public Access: Author ManuscriptDocument20 pagesNIH Public Access: Author ManuscriptSantiago PilataxiNo ratings yet
- Haploidentical Bone Marrow Transplantation in Patients WithDocument22 pagesHaploidentical Bone Marrow Transplantation in Patients Withcarol.bau2713No ratings yet
- Journal of Pediatric Surgery: Contents Lists Available atDocument6 pagesJournal of Pediatric Surgery: Contents Lists Available atNur Ainatun NadrahNo ratings yet
- Myocardial Infarction & AnemiaDocument2 pagesMyocardial Infarction & AnemiaFinka TangelNo ratings yet
- 100015IJBTIWI2015 WoldieDocument5 pages100015IJBTIWI2015 WoldieSigrid MiNo ratings yet
- Pediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietyDocument64 pagesPediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietySeham GoharNo ratings yet
- Diabetes MellitusDocument11 pagesDiabetes Mellitusika safitriNo ratings yet
- KWF 113Document11 pagesKWF 113Residentes RadiologiaHCENo ratings yet
- Blood 2009 Makris 750 1Document3 pagesBlood 2009 Makris 750 1keneo89No ratings yet
- Comparable Efficacy and Safety of Generic Imatinib and Branded Imatinib in Patients With Newly Diagnosed Chronic Myeloid LeukaemiaDocument39 pagesComparable Efficacy and Safety of Generic Imatinib and Branded Imatinib in Patients With Newly Diagnosed Chronic Myeloid Leukaemiarisna sariNo ratings yet
- Prognostic Value of Hypoalbuminemia at Diagnosis in de Novo Non-M3 Acute Myeloid LeukemiaDocument10 pagesPrognostic Value of Hypoalbuminemia at Diagnosis in de Novo Non-M3 Acute Myeloid LeukemiaekanovicaNo ratings yet
- MIDTERM EXAMINATION CLINICAL CHEMISTRY LECTURE 2324Document15 pagesMIDTERM EXAMINATION CLINICAL CHEMISTRY LECTURE 2324Michael John AguilarNo ratings yet
- Authorization Letter Coe AnjeloDocument1 pageAuthorization Letter Coe AnjeloMichael John AguilarNo ratings yet
- Auf Diagnostic Exam Set cDocument14 pagesAuf Diagnostic Exam Set cMichael John AguilarNo ratings yet
- 19-04 Genes and Medicine - Applications of Molecular GeneticsDocument33 pages19-04 Genes and Medicine - Applications of Molecular GeneticsMichael John AguilarNo ratings yet
- 18-08 Molecular Biology - Tools For Molecular BiologyDocument61 pages18-08 Molecular Biology - Tools For Molecular BiologyMichael John AguilarNo ratings yet
- AUF DIAGNOSTIC EXAM SET ADocument13 pagesAUF DIAGNOSTIC EXAM SET AMichael John AguilarNo ratings yet
- Draft Immunohematology TaxonomyDocument11 pagesDraft Immunohematology TaxonomyMichael John AguilarNo ratings yet
- Auf Diagnostic Exam Set bDocument17 pagesAuf Diagnostic Exam Set bMichael John AguilarNo ratings yet
- Introduction to Analytic DesignsDocument39 pagesIntroduction to Analytic DesignsMichael John AguilarNo ratings yet
- 19-04 CytogeneticsDocument39 pages19-04 CytogeneticsMichael John AguilarNo ratings yet
- 19-03 Tools For Molecular Biology and Medical Genetics - UnlockedDocument50 pages19-03 Tools For Molecular Biology and Medical Genetics - UnlockedMichael John AguilarNo ratings yet
- SARS CoV 2 and Dengue Virus Coinfection in An Adult With Beta Thala 2021 HelDocument7 pagesSARS CoV 2 and Dengue Virus Coinfection in An Adult With Beta Thala 2021 HelMichael John AguilarNo ratings yet
- 19-09 Genetic Diagnosis, Clinical Genetics and Genetic Counselling - UnlockedDocument17 pages19-09 Genetic Diagnosis, Clinical Genetics and Genetic Counselling - UnlockedMichael John AguilarNo ratings yet
- 19-06 Population GeneticsDocument7 pages19-06 Population GeneticsMichael John AguilarNo ratings yet
- 19-03 Genes and Medicine - Genetic Diagnosis Clinical Genetics and Genetic CounsellingDocument17 pages19-03 Genes and Medicine - Genetic Diagnosis Clinical Genetics and Genetic CounsellingMichael John AguilarNo ratings yet
- 19-08 Recombination FrequencyDocument15 pages19-08 Recombination FrequencyMichael John AguilarNo ratings yet
- Role of Red Blood Cells Annexin V and Platelets - 2019 - Hematology Oncology ADocument4 pagesRole of Red Blood Cells Annexin V and Platelets - 2019 - Hematology Oncology AMichael John AguilarNo ratings yet
- Advances in Redox Research: - ThalassemiaDocument10 pagesAdvances in Redox Research: - ThalassemiaMichael John AguilarNo ratings yet
- Interference in Coagulation Testing: Focus On Spurious Hemolysis, Icterus, and LipemiaDocument10 pagesInterference in Coagulation Testing: Focus On Spurious Hemolysis, Icterus, and LipemiaMichael John AguilarNo ratings yet
- Biology of Blood and Marrow Transplantation: PediatricDocument8 pagesBiology of Blood and Marrow Transplantation: PediatricMichael John AguilarNo ratings yet
- Vascular Endothelial Growth Factor and Pulmonary Hypertensi - 2019 - Jornal de PDocument7 pagesVascular Endothelial Growth Factor and Pulmonary Hypertensi - 2019 - Jornal de PMichael John AguilarNo ratings yet
- Pediatric Hematology Oncology Journal: Amrith Mathew, Praveen C. SobtiDocument3 pagesPediatric Hematology Oncology Journal: Amrith Mathew, Praveen C. SobtiMichael John AguilarNo ratings yet
- Spectral Domain Optical Coherence Tomography Findings in - 2019 - Journal of CurDocument6 pagesSpectral Domain Optical Coherence Tomography Findings in - 2019 - Journal of CurMichael John AguilarNo ratings yet
- Soluble Endothelial Protein C Receptor Levels in Egypt - 2018 - Pediatric HematoDocument4 pagesSoluble Endothelial Protein C Receptor Levels in Egypt - 2018 - Pediatric HematoMichael John AguilarNo ratings yet
- Biochemistry and Biophysics ReportsDocument7 pagesBiochemistry and Biophysics ReportsMichael John AguilarNo ratings yet
- The Use of Chromogenic Factor VIII Assay Changes Treatment Approach - 2019 - BLDocument3 pagesThe Use of Chromogenic Factor VIII Assay Changes Treatment Approach - 2019 - BLMichael John AguilarNo ratings yet
- Socio Unit3Document12 pagesSocio Unit3priya sharmaNo ratings yet
- Simon The Sportsman: Activity TypeDocument3 pagesSimon The Sportsman: Activity TypeEkaterina DatsenkoNo ratings yet
- Richik Dadhich 1742 Ugiv Crime and Punishment CA3Document3 pagesRichik Dadhich 1742 Ugiv Crime and Punishment CA3Richik DadhichNo ratings yet
- National Lotteries AuthorityDocument14 pagesNational Lotteries AuthorityJohn AbebreseNo ratings yet
- Setiawan D S, Tjahyono K, Afifah D N. 2016Document7 pagesSetiawan D S, Tjahyono K, Afifah D N. 2016Ismi WahyuniNo ratings yet
- Vernacular ArchitectureDocument6 pagesVernacular ArchitectureJia RodriguezNo ratings yet
- w3 - Presentation - Robbins - uhwo.Isa330.Lecture - Week03.28september2013Document164 pagesw3 - Presentation - Robbins - uhwo.Isa330.Lecture - Week03.28september2013Khoi DangNo ratings yet
- Class ProphecyDocument3 pagesClass ProphecyClaudine Fay BaylonNo ratings yet
- Bullying: by Cathlyn de Dios and Mary Yochabel FrancoDocument31 pagesBullying: by Cathlyn de Dios and Mary Yochabel FrancoKDNo ratings yet
- Module 3 SAMURAI DAUGHTERSDocument9 pagesModule 3 SAMURAI DAUGHTERSMicaela Cea MortilNo ratings yet
- QIDS SR16 DepressionDocument3 pagesQIDS SR16 DepressionSergioMSaraivaNo ratings yet
- Math 23 Lecture 3.7 Line Integral of Scalar FieldsDocument22 pagesMath 23 Lecture 3.7 Line Integral of Scalar FieldsyeahNo ratings yet
- Impact Test On Steel SampleDocument4 pagesImpact Test On Steel SampleAdil Javed Chaudhary100% (2)
- Mapeh 10 Exam 4th QuarterDocument2 pagesMapeh 10 Exam 4th QuarterMaybelyn de los ReyesNo ratings yet
- FM302 Financial Management in The Pacific Region: Week 4: Lecture 7 - Major Assignment Some Discussions and DirectionsDocument15 pagesFM302 Financial Management in The Pacific Region: Week 4: Lecture 7 - Major Assignment Some Discussions and DirectionsHitesh MaharajNo ratings yet
- RZA V Imposters ComplaintDocument14 pagesRZA V Imposters ComplaintMatias SmithNo ratings yet
- PUBLIC LEADERSHIP (1) NewDocument13 pagesPUBLIC LEADERSHIP (1) NewHanief GuswantoroNo ratings yet
- Khanqah of Sarwari Qadri OrderDocument74 pagesKhanqah of Sarwari Qadri OrderSultan ul Faqr PublicationsNo ratings yet
- SC TRDocument15 pagesSC TRNishat SinghNo ratings yet
- NIS Daily Lesson Plan: Subject Unit/UOI TeacherDocument3 pagesNIS Daily Lesson Plan: Subject Unit/UOI TeacheraalshehabNo ratings yet
- 2007 Justicia, Rebeca ECUADOR'S CHOCO ANDEAN CORRIDOR: A LANDSCAPE APPROACH FOR CONSERVATION AND SUSTAINABLE DEVELOPMENTDocument248 pages2007 Justicia, Rebeca ECUADOR'S CHOCO ANDEAN CORRIDOR: A LANDSCAPE APPROACH FOR CONSERVATION AND SUSTAINABLE DEVELOPMENTRebeca JusticiaNo ratings yet
- A South India Study Tour Report: Vaishali Nair Academic Year: 2022 - 2023 MAY 2023Document20 pagesA South India Study Tour Report: Vaishali Nair Academic Year: 2022 - 2023 MAY 2023Anandhi PandiyanNo ratings yet
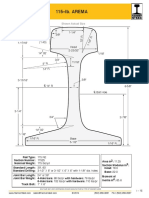
- Arema 115REDocument1 pageArema 115REAntonioNo ratings yet
- Every Transfer of ImmovableDocument3 pagesEvery Transfer of ImmovableAdan HoodaNo ratings yet
- De Thi Giua Ki 1 Tieng Anh Lop 5 Co Dap An 2021Document28 pagesDe Thi Giua Ki 1 Tieng Anh Lop 5 Co Dap An 2021Đỗ Thanh XuânNo ratings yet
- Chapter 15 Conflict and Negotiation PDFDocument2 pagesChapter 15 Conflict and Negotiation PDFDiane Cris DuqueNo ratings yet
- Cricket SepepDocument7 pagesCricket Sepepapi-308918232No ratings yet