Professional Documents
Culture Documents
Jrs0215garzon 2
Jrs0215garzon 2
Uploaded by
Enrique Ferrando BarbenaCopyright:
Available Formats
You might also like
- FBC Vision Screening Template (FVA LMA)Document6 pagesFBC Vision Screening Template (FVA LMA)Taylor BrownNo ratings yet
- Peripheral Vision Improvement ExercisesDocument4 pagesPeripheral Vision Improvement Exercisesmanchiraju raj kumarNo ratings yet
- Research Article: Clinical Results of Diffractive, Refractive, Hybrid Multifocal, and Monofocal Intraocular LensesDocument13 pagesResearch Article: Clinical Results of Diffractive, Refractive, Hybrid Multifocal, and Monofocal Intraocular LensesFitrianiMpiitNo ratings yet
- At Lisatri ArticleDocument10 pagesAt Lisatri ArticleStefoane MadalinNo ratings yet
- Jurnal KuDocument6 pagesJurnal KuTamsilNo ratings yet
- Evaluation of Refractive Error After Cataract Surgery in Highly Myopic EyesDocument6 pagesEvaluation of Refractive Error After Cataract Surgery in Highly Myopic Eyeshenok birukNo ratings yet
- Journal Reading Mata - Pricilia Dan NadyaDocument14 pagesJournal Reading Mata - Pricilia Dan Nadyastepanus 102018062No ratings yet
- Reverse Optic Capture of The SingleDocument10 pagesReverse Optic Capture of The SingleIfaamaninaNo ratings yet
- Clinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaDocument6 pagesClinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaKevin ArdiansyahNo ratings yet
- Status Anak - Fitriani (Print)Document31 pagesStatus Anak - Fitriani (Print)FitrianiMpiitNo ratings yet
- Wa0000Document7 pagesWa0000Ocha24 TupamahuNo ratings yet
- Ebn RugayDocument6 pagesEbn RugayJeffrey Barcelon TanglaoNo ratings yet
- Ophthalmology: Journal of and Advance ResearchDocument7 pagesOphthalmology: Journal of and Advance ResearchAthenaeum Scientific PublishersNo ratings yet
- Influence of Postoperative Astigmatism On Uncorrected Near Visual Acuity in PseudophakiaDocument7 pagesInfluence of Postoperative Astigmatism On Uncorrected Near Visual Acuity in PseudophakiaIJAR JOURNALNo ratings yet
- Rotational Stability of Toric Intraocular - 2022 - Medical Journal Armed ForcesDocument6 pagesRotational Stability of Toric Intraocular - 2022 - Medical Journal Armed ForcesAnisha RanaNo ratings yet
- Ascrs 2Document7 pagesAscrs 2leokapilNo ratings yet
- Highlights From The 2011 ICL/Toric ICL Experts Symposium: Insert ToDocument8 pagesHighlights From The 2011 ICL/Toric ICL Experts Symposium: Insert ToArif MohammadNo ratings yet
- Iris-Claw Intraocular Lenses To Correct Aphakia in The Absence of Capsule SupportDocument6 pagesIris-Claw Intraocular Lenses To Correct Aphakia in The Absence of Capsule SupportAnonymous k4F8sAs25No ratings yet
- Research ArticleDocument9 pagesResearch ArticleRaissaNo ratings yet
- Kjo Jurnal MataDocument7 pagesKjo Jurnal Matanurul hidayati sNo ratings yet
- Visual and Patient-Reported Outcomes of A Diffractive Trifocal Intraocular Lens Compared With Those of A Monofocal Intraocular LensDocument11 pagesVisual and Patient-Reported Outcomes of A Diffractive Trifocal Intraocular Lens Compared With Those of A Monofocal Intraocular Lensakun kd876No ratings yet
- Therapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismDocument7 pagesTherapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismStephanie PfengNo ratings yet
- Moore 2024Document13 pagesMoore 2024youthcp93No ratings yet
- One-Year Results of Health-Related and Vision-Related Quality of Life After Clear Lens Extraction and Multifocal Intraocular Lens ImplantationDocument5 pagesOne-Year Results of Health-Related and Vision-Related Quality of Life After Clear Lens Extraction and Multifocal Intraocular Lens ImplantationDanty IndriastutyNo ratings yet
- s12886 022 02620 7Document8 pagess12886 022 02620 7MarioNo ratings yet
- IolDocument7 pagesIolAnonymous h0DxuJTNo ratings yet
- Toric ICLDocument8 pagesToric ICLjbahalkehNo ratings yet
- Ju 2023Document9 pagesJu 2023youthcp93No ratings yet
- 3 Piece IOL SCL FixDocument6 pages3 Piece IOL SCL FixTvrtka BenašićNo ratings yet
- Fixation Stability, Fixation Location, and Visual Acuity After Successful Macular Hole SurgeryDocument6 pagesFixation Stability, Fixation Location, and Visual Acuity After Successful Macular Hole SurgeryAlpi AnorNo ratings yet
- 2016 Article 229Document7 pages2016 Article 229nisa_kartikaNo ratings yet
- Mertens - The Staar Toric ICLDocument4 pagesMertens - The Staar Toric ICLAndreea L. MihalceaNo ratings yet
- Visual and Refractive Outcomes of Small-Incision Lenticule Extraction in High Myopia - 5-Year ResultsDocument7 pagesVisual and Refractive Outcomes of Small-Incision Lenticule Extraction in High Myopia - 5-Year Resultspriscilla christina natanNo ratings yet
- Clinical Differences Between Toric Intraocular LenDocument8 pagesClinical Differences Between Toric Intraocular LenonderonderNo ratings yet
- Adminku Journal Manager ErlaniDocument7 pagesAdminku Journal Manager Erlanirm suryaubungNo ratings yet
- ArtIOLs - Biblio 2Document16 pagesArtIOLs - Biblio 2blazquezjoseignacioNo ratings yet
- Acta Ophthalmologica - 2018 - Garc A Montero - Binocular Vision Alterations After Refractive and Cataract Surgery A ReviewDocument11 pagesActa Ophthalmologica - 2018 - Garc A Montero - Binocular Vision Alterations After Refractive and Cataract Surgery A ReviewFrancisco Arturo MánuelNo ratings yet
- Sulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryDocument6 pagesSulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryPrizilia SaimimaNo ratings yet
- Karakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia LatuasanDocument10 pagesKarakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia Latuasanwasobiru isbiruNo ratings yet
- Ecop 09 00286Document11 pagesEcop 09 00286GabrielNo ratings yet
- Evaluation of SuturlessDocument7 pagesEvaluation of SuturlesskenapayaNo ratings yet
- Astigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionDocument6 pagesAstigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- BSN Reading (Scleral Buckling) RosalesDocument8 pagesBSN Reading (Scleral Buckling) RosalesYvonnie RosalesNo ratings yet
- 1112CRSTEuro Cs VinciguerraDocument3 pages1112CRSTEuro Cs VinciguerraR Andres Plaza ZNo ratings yet
- Effectiveness of Accommodating Intra Ocular Lens: Department of Ophthalmology, Faculty of Medicine, Universitas LampungDocument7 pagesEffectiveness of Accommodating Intra Ocular Lens: Department of Ophthalmology, Faculty of Medicine, Universitas LampungayuNo ratings yet
- Intraindividual Comparison of Aspherical and Spherical Intraocular Lenses of Same Material and PlatformDocument6 pagesIntraindividual Comparison of Aspherical and Spherical Intraocular Lenses of Same Material and PlatformAkhilesh KumarNo ratings yet
- 25904-Texto Do Trabalho-118421-1-10-20221008Document10 pages25904-Texto Do Trabalho-118421-1-10-20221008vergarajaviera548No ratings yet
- #12 Baviera RayOne EMV Study White PaperDocument6 pages#12 Baviera RayOne EMV Study White PaperPiet ConradieNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleAnnisak FitriyanaNo ratings yet
- Visualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot StudyDocument15 pagesVisualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot Studymistic0No ratings yet
- s12886 022 02600 XDocument8 pagess12886 022 02600 XHariom ShuklaNo ratings yet
- Visual Outcomes and Accommodat PDFDocument13 pagesVisual Outcomes and Accommodat PDFfatiNo ratings yet
- Corneal Endothelial Morphologic Assessment in Pediatric Cataract Surgery With Intraocular Lens Implantation - A Comparison of Preoperative and Early Postoperative Specular MicrosDocument8 pagesCorneal Endothelial Morphologic Assessment in Pediatric Cataract Surgery With Intraocular Lens Implantation - A Comparison of Preoperative and Early Postoperative Specular MicrosRael Rodrigues Dos SantosNo ratings yet
- Jurding MataDocument7 pagesJurding Matarandy_27995No ratings yet
- Chang 2016Document5 pagesChang 2016steviaNo ratings yet
- SocivoDocument16 pagesSocivoSlobodan MilovanovicNo ratings yet
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocument10 pagesClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNo ratings yet
- Iris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaDocument7 pagesIris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaMuhammad SukriNo ratings yet
- Coscarelli, 2012Document8 pagesCoscarelli, 2012vitor auzierNo ratings yet
- 1 s2.0 S2773157X2400047X MainDocument3 pages1 s2.0 S2773157X2400047X MainomarNo ratings yet
- Early Intervention in Orbital Floor Fractures: Postoperative Ocular Motility and Diplopia OutcomesDocument9 pagesEarly Intervention in Orbital Floor Fractures: Postoperative Ocular Motility and Diplopia OutcomesHải Ngọc Đinh VũNo ratings yet
- Current Advances in Ophthalmic TechnologyFrom EverandCurrent Advances in Ophthalmic TechnologyParul IchhpujaniNo ratings yet
- D D I 6055.04 D D M V T S: O Nstruction O Otor Ehicle and Raffic AfetyDocument38 pagesD D I 6055.04 D D M V T S: O Nstruction O Otor Ehicle and Raffic AfetyEnrique Ferrando BarbenaNo ratings yet
- c145 CorruptionDocument178 pagesc145 CorruptionEnrique Ferrando BarbenaNo ratings yet
- Ordinance # 2001-23: E:/Wpdata/Efm/Dcaol-2/Ol02.0RdDocument26 pagesOrdinance # 2001-23: E:/Wpdata/Efm/Dcaol-2/Ol02.0RdEnrique Ferrando BarbenaNo ratings yet
- Kas16 - Mat&Des - Correlation Between Porosity and Processing Parameters in TiAl6V4 Produced by Selective Laser Melting+corrigendumDocument13 pagesKas16 - Mat&Des - Correlation Between Porosity and Processing Parameters in TiAl6V4 Produced by Selective Laser Melting+corrigendumEnrique Ferrando BarbenaNo ratings yet
- Value Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatDocument5 pagesValue Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatEnrique Ferrando BarbenaNo ratings yet
- A123 Rev PDFDocument35 pagesA123 Rev PDFEnrique Ferrando BarbenaNo ratings yet
- Top 10 Taxpayer Report: 2020 City of CombineDocument55 pagesTop 10 Taxpayer Report: 2020 City of CombineEnrique Ferrando BarbenaNo ratings yet
- CMS Manual System: Pub 100-04 Medicare Claims ProcessingDocument17 pagesCMS Manual System: Pub 100-04 Medicare Claims ProcessingEnrique Ferrando BarbenaNo ratings yet
- 07 Kuha Dandolo Chronica PDFDocument18 pages07 Kuha Dandolo Chronica PDFEnrique Ferrando BarbenaNo ratings yet
- Citrix Netscaler Data SheetDocument12 pagesCitrix Netscaler Data SheetEnrique Ferrando BarbenaNo ratings yet
- Yaesu G-800S G-800SDX G-1000S SDX User PDFDocument21 pagesYaesu G-800S G-800SDX G-1000S SDX User PDFEnrique Ferrando BarbenaNo ratings yet
- SC1 Mod 3-4 Fuzzy-Applications 811 AaDocument15 pagesSC1 Mod 3-4 Fuzzy-Applications 811 AaEnrique Ferrando BarbenaNo ratings yet
- BrmsDocument210 pagesBrmsEnrique Ferrando BarbenaNo ratings yet
- SS34 C8678Document2 pagesSS34 C8678Enrique Ferrando BarbenaNo ratings yet
- UMP SEBB Preferred Drug ListDocument135 pagesUMP SEBB Preferred Drug ListEnrique Ferrando BarbenaNo ratings yet
- Manual en PDFDocument81 pagesManual en PDFEnrique Ferrando BarbenaNo ratings yet
- Quartz Crystal SS3: Pin Type Crystal 11.35 X 4.65 MMDocument2 pagesQuartz Crystal SS3: Pin Type Crystal 11.35 X 4.65 MMEnrique Ferrando BarbenaNo ratings yet
- Commercial Chinook: Mark LambertreportsfromphiladelphiaDocument1 pageCommercial Chinook: Mark LambertreportsfromphiladelphiaEnrique Ferrando BarbenaNo ratings yet
- Man ENDocument94 pagesMan ENEnrique Ferrando BarbenaNo ratings yet
- AMI US Dollar RatesDocument1 pageAMI US Dollar RatesEnrique Ferrando BarbenaNo ratings yet
- Bird Tours GBPDocument9 pagesBird Tours GBPEnrique Ferrando BarbenaNo ratings yet
- KDC-168U: Instruction Manual Mode D'Emploi Manual de InstruccionesDocument64 pagesKDC-168U: Instruction Manual Mode D'Emploi Manual de InstruccionesEnrique Ferrando BarbenaNo ratings yet
- Finitte DiferenceDocument522 pagesFinitte DiferenceEnrique Ferrando Barbena100% (1)
- Colorandquality 1Document59 pagesColorandquality 1oktay yetginNo ratings yet
- Cet 5Document4 pagesCet 5jumi26No ratings yet
- SBI Eye - Surgery 1Document24 pagesSBI Eye - Surgery 1Munam WaqarNo ratings yet
- Method of Extending The Range of The KeratometerDocument3 pagesMethod of Extending The Range of The KeratometerDanielle SangalangNo ratings yet
- Modified Sewing Machine Technique For IridodialysiDocument8 pagesModified Sewing Machine Technique For IridodialysiRonal PerinoNo ratings yet
- Physio Lab PBLDocument4 pagesPhysio Lab PBLtheodore_estradaNo ratings yet
- Anatomy of The Eye, Orbit and Related Structures: Basic Science ExaminationDocument8 pagesAnatomy of The Eye, Orbit and Related Structures: Basic Science ExaminationOana PaladeNo ratings yet
- Lab Manual - Senses Eye - A+p - 2-12-18Document19 pagesLab Manual - Senses Eye - A+p - 2-12-18Ajit Sinha0% (1)
- Intravitreal Injection of Triamcinolone Acetonide: Core MessagesDocument22 pagesIntravitreal Injection of Triamcinolone Acetonide: Core MessagesSiva LoveNo ratings yet
- Igcse AccommodationDocument3 pagesIgcse AccommodationChr1zFX4No ratings yet
- Tatalaksana Katarak Komplikata Yang Disebabkan Oleh Uveitis - Ericka Febriyanti Pratama Putri 1Document14 pagesTatalaksana Katarak Komplikata Yang Disebabkan Oleh Uveitis - Ericka Febriyanti Pratama Putri 1Cynthia Isra MandahutaNo ratings yet
- A Pinhole Camera Has No Lens.Document1 pageA Pinhole Camera Has No Lens.M. Amaan AamirNo ratings yet
- Angle Recession GlaucomaDocument15 pagesAngle Recession GlaucomaDia Asri RusliNo ratings yet
- Glaucoma PPT For Final YearDocument57 pagesGlaucoma PPT For Final YearDarshan SinghNo ratings yet
- IOL PowerDocument273 pagesIOL Powermarlon García100% (3)
- Stargardt DiseaseDocument9 pagesStargardt DiseaseEstefhany SCNo ratings yet
- Anatomy and Physiology of The EyeDocument18 pagesAnatomy and Physiology of The EyeMargaretha AdhiningrumNo ratings yet
- Poze La Partic CliniceDocument3 pagesPoze La Partic CliniceLoredana CiubotaruNo ratings yet
- Notification Admit Card Results Exam AnalysisDocument10 pagesNotification Admit Card Results Exam AnalysisChellamani UmakanthanNo ratings yet
- Inventario Pink Up - Hoja 1Document7 pagesInventario Pink Up - Hoja 1Mich RiveraNo ratings yet
- TopazDocument2 pagesTopazJoevince Neil GacusNo ratings yet
- Maders Understanding Human Anatomy and Physiology 8th Edition Susannah Nelson Longenbaker Test Bank Full Chapter PDFDocument68 pagesMaders Understanding Human Anatomy and Physiology 8th Edition Susannah Nelson Longenbaker Test Bank Full Chapter PDFCindyCurrywpbfd100% (11)
- PDF Neuroanatomy Text and Atlas John D Martin Ebook Full ChapterDocument53 pagesPDF Neuroanatomy Text and Atlas John D Martin Ebook Full Chapteroscar.warner960100% (1)
- Fusion and Binocular SummationDocument3 pagesFusion and Binocular Summationblack00swanNo ratings yet
- OphthalmologyDocument12 pagesOphthalmologyMahesh Shrestha100% (1)
- ReferencesDocument6 pagesReferencesAndrew MakariosNo ratings yet
- Human Eye PDFDocument13 pagesHuman Eye PDFHaidir MuhammadNo ratings yet
Jrs0215garzon 2
Jrs0215garzon 2
Uploaded by
Enrique Ferrando BarbenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jrs0215garzon 2
Jrs0215garzon 2
Uploaded by
Enrique Ferrando BarbenaCopyright:
Available Formats
ORIGINAL ARTICLE
Evaluation of Rotation and Visual Outcomes
After Implantation of Monofocal and
Multifocal Toric Intraocular Lenses
Nuria Garzón, OD, MSc; Francisco Poyales, MD; Begoña Ortíz de Zárate, MD;
Jose Luis Ruiz-García, OD, MSc; Juan Antonio Quiroga, PhD
ABSTRACT
PURPOSE: To evaluate rotational stability and its influ-
ence on postoperative visual acuity of different monofo-
O ne of the main challenges in astigmatism-correcting
IOLs is ensuring precise alignment on the patient’s
axis of corneal astigmatism and rotational stability
after IOL implantation.1,2 The slightest variation in alignment
will mean that the patient will develop a postoperative astig-
cal and multifocal toric intraocular lenses (IOLs).
matism on a different axis to that of the preoperative astig-
METHODS: A prospective interventional study was de- matism.3 To determine the optimal position for accurate IOL
signed. Ninety-one patients with a mean age of 71.65 alignment, several methods have been proposed in which ink
± 11.82 years were implanted with toric IOLs after marks are placed on the corneal limbus.4-9 In some of these
phacoemulsification. Three monofocal toric IOLs (the systems, corneal marks are placed under monocular vision
Lentis LT [Oculentis, Berlin, Germany], enVista [Bausch (occluding one eye) to avoid the convergence produced when
& Lomb, Rochester, NY], and AcrySof IQ [Alcon Labo-
ratories, Inc., Fort Worth, TX]) and one multifocal toric the patient fixates on a near target, or most often under the slit
IOL (AcrySof IQ ReSTOR; Alcon Laboratories, Inc.) were lamp with no fixed viewing position. However, none of these
implanted. Preoperative and postoperative images were methods consider the possibility of cyclotorsion in monocu-
taken to calculate the misalignment due to the marking lar viewing conditions as described in previous studies.9,10
method. To evaluate rotation in the different follow-up On the other hand, if the marks are made binocularly, the
visits, another photograph was taken 1 hour and 1, 7
and 30 days postoperatively. Refraction, uncorrected convergence produced when the patient views a near object
distance visual acuity (UDVA), and corrected distance is not corrected.
visual acuity were measured 30 days postoperatively. Regarding rotational stability, there are several stud-
ies on monofocal toric IOLs with follow-up between 1 and
RESULTS: Postoperative UDVA was 0.1 logMAR or bet- 6 months, where the lens position remained stable from 1
ter in 64.6% of eyes implanted with monofocal IOLs month onward.1,2,11-13 Both misalignment (differences be-
and 46.4% of eyes implanted with multifocal IOLs. The
enVista toric IOL showed the best UDVA compared to tween preoperatively calculated IOL position and real IOL
the other monofocal IOLs, with 81% of eyes with 0.1 position just after surgery) and rotation (differences between
logMAR or better. The mean misalignment in the total real IOL position just after surgery and IOL position at post-
group studied was 0.07° ± 0.60°; 69.6% of monofocal operative follow-up visits) are critical to a successful surgery
IOLs and 67.9% of multifocal IOLs showed less than 5° in terms of visual quality. If the IOL rotates 15° off axis after
of rotation. A correlation was found between postopera-
tive UDVA and rotation in the monofocal and multifocal surgery, there will only be half correction of the power and
IOLs implanted (r = 0.439 [P < .011] and = 0.787 [P the resultant cylinder will be shifted to a new axis.3 If a multi-
= .001], respectively). focal toric IOL was implanted, the rotation, misalignment, or
both will probably worsen uncorrected distance visual acuity
CONCLUSIONS: At 1 month postoperatively, UDVA was (UDVA) compared to a monofocal toric IOL; however, there
slightly more affected by IOL rotation in multifocal than
monofocal toric IOLs. The marking method was also ef- From Instituto de Oftalmología Avanzada, Madrid, Spain (NG, FP, BOD); and
fective. Universidad Complutense de Madrid, Madrid, Spain (JLR-G, JAQ).
Submitted: November 3, 2014; Accepted: December 16, 2014; Posted online:
[J Refract Surg. 2015;31(2):XX-XX.] March 12, 2015
The authors have no financial or proprietary interest in the materials pre-
sented herein.
Correspondence: Nuria Garzón, OD, MSc, Instituto de Oftalmología Avanzada, c/
Galileo 104, Madrid, 28003 Spain. E-mail: ngarzon@oftalmologia-avanzada.com
Journal of Refractive Surgery • Vol. 31, No. 2, 2015 1
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
are few studies on multifocal toric IOLs and their rota- Prior to surgery, topography with the OPD II Scan
tional effects.14-16 (Nidek, Hiroishi, Japan), Pentacam (Oculus Optik-
To the best of our knowledge, no previous studies geräte GmbH, Wetzlar, Germany), laser interference
have been conducted to compare rotational stability biometry IOLMaster (Carl Zeiss Meditec, Jena, Ger-
and its effect on postoperative residual astigmatism many), optical coherence tomography with the Cirrus
between multifocal and monofocal toric IOLs. There- platform (Carl Zeiss Medictec), slit-lamp examination,
fore, the main objective of this study was to evaluate refraction, and CDVA were performed. Postoperative
if there are differences in rotational stability between visits were scheduled at 1 day, 1 week, and 1 month af-
different monofocal and multifocal toric IOL plat- ter surgery. Topography, slit-lamp examination, refrac-
forms and its influence on uncorrected postoperative tion, and UDVA and CDVA were performed 1 month
visual acuity. The second objective was to evaluate postoperatively.
the effectiveness of a new marking method for reduc- We used the Alpins method for calculating astigma-
ing misalignment. tism. The Alpins method uses three fundamental vec-
tors: target-induced astigmatism, surgically induced
PATIENTS AND METHODS astigmatism, and the difference vector. The target-
A prospective interventional study was conducted induced astigmatism is the astigmatic change (by mag-
including 91 patients (91 eyes) with a mean age of nitude and axis) that the surgery is intended to induce
71.65 ± 11.82 years (range: 27 to 95 years). Patients and the surgically induced astigmatism is the amount
were implanted with toric IOLs in one or both eyes and axis of astigmatic change the surgery actually in-
at the Instituto de Oftalmología Avanzada of Madrid duces. The difference vector is the induced astigmatic
during 2013. If a patient had a cataract in both eyes change (by magnitude and axis) that would enable the
and if each lens calculation indicated the need for a initial surgery to achieve the intended target.
toric lens, then only one eye from that patient was in-
cluded in the study. Each eye was randomly selected. IOLs
If a patient had a cataract in both eyes but only one Three monofocal toric IOLs (the Lentis LT [LU-313T;
eye needed a toric lens, that eye was included in the Oculentis, Berlin, Germany], enVista [Bausch & Lomb,
study. If a patient required a toric lens in only one eye Rochester, NY], and AcrySof IQ toric IOL [SN6A T3-
because the other had no cataract or was pseudopha- T9; Alcon Laboratories, Inc., Fort Worth, TX]) and one
kic, that eye was included in the study. In all cases, the multifocal toric IOL (the AcrySof IQ ReSTOR [SND1
patients recruited met all inclusion requirements. T1-T5; Alcon Laboratories, Inc.) were implanted. More
All patients participated voluntarily in the study technical details are shown in Table A (available in the
and were free to withdraw at any time. Informed con- online version of this article).
sent was signed by all patients after the nature of the
study and risks of participation were explained. The Marking Method
study was conducted in accordance with the tenets During the preoperative preparation of the patient,
of the Declaration of Helsinki17 and was approved by two marks were placed at the limbus using a fine-tipped
the Ethics Committee of the Instituto de Oftalmología gentian violet marker (Devon Skin Marker, Fine Tip
Avanzada of Madrid. Detailed demographic character- 151; Covidien, Dublin, Ireland) on the horizontal axis
istics of the study population are shown in Table 1. (0° to 180°) at the 9- and 3-o’clock positions under slit-
The inclusion criteria to participate were: an ex- lamp observation (Figure 1A). A photograph was taken
pected postoperative corrected distance visual acu- of the patient standing 2.5 m or more from the camera,
ity (CDVA) of 0.3 logMAR or better, anterior corneal with the head in normal position without the use of a
astigmatism of 1.00 D or greater, and total astigmatism chinrest or other support. Both eyes were open, thus
(anterior and posterior corneal astigmatism) of 0.50 D avoiding the cyclotorsion that can occur if one is closed.
or less, with respect to the anterior astigmatism. The Images were taken at a distance that avoided cyclotor-
patients were required to have no corneal irregularities sion when looking at a close object. The position of the
when examined under slit lamp or when examined to- marks made by the surgeon were measured on the image
pographically, and to show no observable macular al- acquired. Thus, once a patient was supine, the exact po-
terations following optical coherence tomography. No sition of the mark (made with violet blue) was known,
patient was included who showed corneal or macular independent of any cyclotorsion that might take place.
abnormalities, who required a follow-up different to The camera used was a Coolpix P90 (Nikon, Tokyo,
that outlined in the protocol used at the center (either Japan), with a 26.0- to 624.0-mm lens (at 35 mm), a
before or after surgery), or who required a suture. charge-coupled device of 12.10 effective megapixels,
2 Copyright © SLACK Incorporated
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
TABLE 1
Preoperative Patient Demographics
Mean ± SD (Range)
AcrySof IQ AcrySof IQ
Parameter Total Toric IOL enVista Toric IOL Lentis LT IOL ReSTOR Toric IOL
No. of patients (eyes) 91 (91) 28 (28) 21 (21) 14 (14) 28 (28)
Mean age (y) 71.65 ± 11.82 77.21 ± 8.60 71.19 ± 9.34 72.07 ± 11.41 64.25 ± 14.72
(27 to 95) (58 to 95) (57 to 89) (57 to 93) (27 to 91)
Gender (female/male) 52/39 16/12 10/11 10/4 16/12
Spherical equivalent (D) 0.59 ± 3.75 -0.92 ± 3.45 -0.17 ± 3.64 0.25 ± 4.69 -0.10 ± 4.35
(-10.75 to 9.00) (-9.00 to 7.38) (-10.75 to 6.13) (-7.50 to 9.00) (-6.63 to 6.50)
Mean corneal astigmatism (D) 1.87 ± 0.67 1.72 ± 0.85 1.89 ± 0.57 1.93 ± 0.66 1.91 ± 0.61
(1.00 to 4.55) (1.00 to 4.55) (1.01 to 3.31) (1.07 to 3.27) (1.00 to 3.08)
Mean keratometry (D)
Flat 43.10 ± 1.61 43.34 ± 1.61 43.63 ± 1.33 43.13 ± 2.23 42.63 ± 1.54
Steep 44.97 ± 1.63 45.07 ± 1.77 45.51 ± 1.38 45.06 ± 2.36 44.54 ± 1.41
Mean refractive sphere (D) 0.76 ± 3.66 -0.16 ± 2.99 0.88 ± 3.58 1.11 ± 4.98 0.79 ± 4.32
(-9.00 to -10.50) (-7.50 to 4.00) (-9.00 to 7.25) (-7.00 to 10.50) (-6.00 to 7.50)
Mean refractive cylinder (D) 2.03 ± 0.86 2.26 ± 0.95 2.09 ± 0.58 1.71 ± 0.87 1.85 ± 0.99
(0.50 to 4.25) (0.75 to 4.25) (1.25 to 3.50) (0.50 to 3.50) (0.50 to 3.75)
Preoperative CDVA (logMAR) 0.19 ± 0.17 0.30 ± 0.21 0.15 ± 0.17 0.22 ± 0.13 0.10 ± 0.12
(0.01 to 0.82) (0.05 to 0.52) (0 to 0.70) (0 to 0.82) (0 to 0.52)
IOL power (sphere) (D) 20.79 ± 5.64 19.98 ± 5.98 20.47 ± 4.33 20.67 ± 3.78 19.72 ± 6.82
IOL power (cylinder) (D) 1.91 ± 1.22 2.43 ± 0.97 2.32 ± 0.55 2.84 ± 0.52 2.38 ± 0.72
SD = standard deviation; IOL = intraocular lens; D = diopters; CDVA = corrected distance visual acuity
The AcrySof IQ and AcrySof IQ ReSTOR are manufactured by Alcon Laboratories, Inc., Fort Worth, TX. The enVista is manufactured by Bausch & Lomb, Rochester,
NY. The Lentis LT is manufactured by Oculentis, Berlin, Germany.
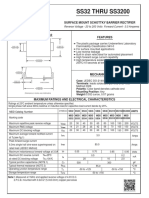
Figure 1. (A) Two marks placed at the
limbus on the horizontal axis (0° to 180º)
at the 9- and 3-o’clock positions performed
under slit-lamp observation. (B and C) The
exact position of the marks and their angu-
lar difference with respect to the “real” 0°
to 180° line.
and a 324 (optical)/34 (digital) zoom. The camera was the patient lying down, using the Méndez ring and tak-
placed on a tripod and connected to a bubble level to ing reference of the previous marks, the axis was to be
ensure the photograph was perfectly aligned. The cam- aligned with the IOL’s index marks, considering the
era lens was positioned at eye level and at 2.5 m or angle difference observed in the photographic mea-
more. The optical zooming option allowed us to simul- surements was marked. The preoperative image and
taneously photograph both eyes. The photograph was last photograph obtained during surgery showing the
then exported to a computer equipped with software final axis position of the IOL were compared to cal-
that enables precise angle measurements by means of culate the misalignment due to the marking method.
the Scale 2.0 package (AQ1Software R. Sgrillo, Brazil). To assess the rotation in the different follow-up visits,
On the photograph, the angle the corneal marks another photograph was taken 1 hour and 1, 7, and 30
form with the horizontal line that transects the corneal days after surgery.
reflex was measured (Figures 1B-1C). This gives the A triangulation method was used for measuring the
exact position of the marks and their angular differ- rotation. This required the determination of the lim-
ence with respect to the “real” 0° to 180° line. With bal edge, the determination of the IOL edge (optical
Journal of Refractive Surgery • Vol. 31, No. 2, 2015 3
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
zone), one reproducible marker (eg, a vessel crossover, sults regarding visual acuity, refraction, and rotation
a pupil mark) on the eye, and the marks on the IOL. are shown in Table 2.
The IOL diameter is the same whatever the distance Postoperative UDVA was 0.1 logMAR
of the slit lamp to the eye, allowing the distance mea- (20/25 Snellen) or better in 64.6% of eyes im-
sured to be harmonized between one photograph and planted with monofocal toric IOLs and 46.4%
another. The triangle is formed by the IOL center, IOL of eyes implanted with multifocal toric IOLs
mark, and biometric marker (eg, a vessel crossover). (Figure A, available in the online version of this article).
The change in triangle rotation determines the IOL ro- The enVista toric IOL showed the best UDVA compared
tation. Clockwise rotation was counted as positive ro- to the other monofocal toric IOLs, with 81% of eyes
tation and anti-clockwise rotation as negative rotation. with 0.1 logMAR (20/25 Snellen) or better (Figure 2).
Mean CDVA showed a statistically significant in-
Cataract Surgery Procedure crease after IOL implantation in all lenses studied. The
All surgeries were performed by the same experi- mean preoperative CDVA was 0.19 ± 0.17 (range: 0.01
enced surgeon. The cylinder power and axis were cal- to 0.82) and mean postoperative CDVA was 0.02 ± 0.05
culated using the software provided by the manufactur- (range: 0.00 to 0.30) (P < .05; Student’s t test).
ers and taking into account the keratometric readings The mean spherical equivalent for all patients de-
measured with a topographer. Phacoemulsification creased after surgery to -0.10 ± 0.51 D (range: -1.25 to
was performed through a 2.2-mm clear corneal inci- 2.38 D) and was statistically significant compared to
sion. The astigmatism induced by the surgeon (FP) was mean preoperative spherical equivalent (P < .05; Stu-
previously known. The lenses were introduced via a dent’s t test), but no differences were found with the
2.2-mm incision and the surgeon induced an astigma- mean targeted spherical equivalent, which was - 0.03
tism of 0.1 D in the right eye (temporal incision). In the ± 0.40 D (range: -1.95 to 0.75 D). The mean difference
left eye, the superior incision produced an astigmatism between targeted spherical equivalent and mean post-
of 0.2 D. This was taken into account when the power operative spherical equivalent was -0.07 ± 0.46 D,
of the lenses to be implanted was calculated. and no significant differences were seen between the
In any case, it was necessary to open the incision for postoperative spherical equivalent and the targeted
inserting the foldable IOL with the injector. To shield value programmed after performing the lens calcula-
the corneal endothelial cells, a dispersive viscoelastic tion. No statistical differences were found between the
(Viscoat; Alcon Laboratories, Inc.) was first injected IOLs implanted, the enVista being the lens with the
into the anterior chamber followed by another cohe- highest mean spherical equivalent and the AcrySof
sive viscoelastic (Amvisc Plus; Bausch & Lomb) inject- IQ ReSTOR toric IOL with the lowest mean spherical
ed below the first one. The incision was not sutured equivalent after surgery.
and the eyes were not patched. Mean cylinder decreased in all patients from 2.03
± 0.86 D to 0.61 ± 0.57 D after surgery. Statistical dif-
Statistical Analysis ferences were found for all lenses studied (P < .05;
Data were analyzed by SPSS version 17.0 (SPSS, Student’s t test). Postoperative cylinder between plano
Inc., Chicago, IL) for Windows. The values presented and 0.50 D was found in 73.3% and 43.9% of eyes with
are the mean ± standard deviation of the values ob- monofocal and multifocal IOLs, respectively (Figure
tained. Normality of distribution was assessed using B). The enVista IOL showed more eyes with postopera-
the Kolmogorov–Smirnov test. One-way repeated mea- tive cylinder between plano and 0.50 D than the other
sure analysis of variance was used to assess the trend of monofocal toric IOLs studied, with more than 80% of
IOL rotation during postoperative follow-up visits. Stu- eyes within this range (Figure 3).
dent’s t test for related samples was used to compare A new marking method was also evaluated in this
preoperatively calculated IOL position with IOL posi- study. The misalignment was the difference between
tion just after surgery (misalignment). To correlate rota- preoperatively and postoperatively calculated IOL
tion (absolute values) at 30 days and misalignment val- positions. The mean misalignment in the total group
ues with UDVA and astigmatism postoperative power, studied was 0.07° ± 0.60° (range: -2.00° to 3.00°).
Pearson bivariate regression was used. A P value of less Table 2 shows misalignment values for the different
than .05 was considered statistically significant. IOLs. No statistical difference was found between
preoperatively and postoperatively calculated IOL po-
RESULTS sitions for any IOL studied (P < .05; Student’s t test).
Detailed demographic characteristics of the study Rotation of the lenses was measured 1 hour and 1, 7,
population are shown in Table 1. All postoperative re- and 30 days after surgery. Figure C (available in the on-
4 Copyright © SLACK Incorporated
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
TABLE 2
Postoperative Results of Visual Acuity to Refraction to Misalignment and
Rotation With the Different IOLs Implanted
Mean ± SD (Range)
AcrySof IQ
Parameter AcrySof IQ Toric IOL enVista Toric IOL Lentis LT IOL ReSTOR Toric IOL
Postoperative UDVA (logMAR) 0.14 ± 0.16 0.09 ± 0.14 0.09 ± 11.82 0.12 ± 0.11
(0 to 0.52) (0 to 0.52) (0 to 0.30) (0 to 0.40)
Postoperative sphere (D) -0.01 ± 0.53 -0.06 ± 0.31 0.52 ± 0.60 0.32 ± 0.44
Postoperative cylinder (D) 0.45 ± 0.48 0.41 ± 0.51 0.63 ± 0.56 0.64 ± 0.53
Equivalent sphere (D) -0.24 ± 0.56 -0.27 ± 0.38 0.21 ± 0.48 0.00 ± 0.33
(-2.38 to 0.75) (-1.25 to 0.25) (-0.75 to 1.00) (-0.75 to 0.75)
Postoperative CDVA (logMAR) 0.04 ± 0.08 0.01 ± 0.02 0.00 ± 0.01 0.01 ± 0.03
(0 to 0.30) (0 to 0.1) (0 to 0.05) (0 to 0.15)
Misalignment (degrees) 0.00 ± 0.67 -0.10 ± 0.70 0.35 ± 0.63 0.17 ± 0.54
(-1.00 to 3.00) (-2.00 to 1.00) (0 to 2.00) (-1.00 to 1.00)
Rotation 1 hour (degrees) 0.96 ± 4.51 -0.67 ± 6.09 3.78 ± 6.20 2.82 ± 5.11
(-5.00 to 13.00) (-22.00 to 10.00) (-8.00 to 18.00) (-8.00 to 18.00)
Rotation 1 day (degrees) 0.57 ± 4.79 -0.90 ± 6.22 3.78 ± 5.87 2.82 ± 5.40
(-8.00 to 13.00) (-22.00 to 10.00) (-7.00 to 17.00) (-8.00 to 18.00)
Rotation 7 days (degrees) 0.50 ± 4.99 -0.71 ± 6.07 3.78 ± 5.87 2.82 ± 5.40
(-9.00 to 13.00) (-22.00 to 10.00) (-7.00 to 17.00) (-8.00 to 18.00)
Rotation 30 days (degrees) 0.32 ± 5.85 -0.42 ± 5.87 3.71 ± 5.94 2.78 ± 5.83
(-10.00 to 12.00) (-22.00 to 10.00) (-7.00 to 17.00) (-12.00 to 18.00)
IOL = intraocular lens; SD = standard deviation; UDVA = uncorrected distance visual acuity; D = diopters; CDVA = corrected distance visual acuity
The AcrySof IQ and AcrySof IQ ReSTOR are manufactured by Alcon Laboratories, Inc., Fort Worth, TX. The enVista is manufactured by Bausch & Lomb, Rochester,
NY. The Lentis LT is manufactured by Oculentis, Berlin, Germany.
Figure 2. Comparison of postoperative uncorrected distance visual acuity Figure 3. Comparison of postoperative refractive astigmatism frequency
frequency at 30 days between different monofocal toric intraocular lenses at 30 days between different monofocal toric intraocular lenses (the
(the AcrySof IQ [Alcon Laboratories, Inc., Fort Worth, TX], enVista [Bausch AcrySof IQ [Alcon Laboratories, Inc., Fort Worth, TX], enVista [Bausch
& Lomb, Rochester, NY] and Lentis LT [Oculentis, Berlin, Germany]) for & Lomb, Rochester, NY] and Lentis LT [Oculentis, Berlin, Germany]) for
different visual acuity values. different powers.
line version of this article) shows rotation values of the LT). The enVista lens was the most stable and the only
monofocal and multifocal IOL implanted at the differ- one to show anti-clockwise rotation; all of the others
ent follow-up visits. No statistical differences between showed clockwise rotation (Figure 4).
visits were found between monofocal and multifocal At 30 days postoperatively, 69.6% of monofocal
IOLs (P > .05; one-way repeated measure analysis of IOLs and 67.9% of multifocal IOLs showed less than
variance). 5° of rotation. Fifteen (18.9%) eyes implanted with
One hour after surgery, the lens that showed the monofocal IOLs and 5 (17.8%) eyes implanted with
most rotation was that with the plate design (Lentis multifocal IOLs showed more than 10° of rotation.
Journal of Refractive Surgery • Vol. 31, No. 2, 2015 5
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
violet, thus providing accurate and precise marks of
the real axis instead of relative position marks.
Seventy-five percent of patients did not present mis-
alignment and only 3 of 91 patients had 2° or more
of misalignment. In the comparison of the theoretical
position of the toric lens (obtained by calculation) with
that observed in the last image obtained during cata-
ract surgery, no significant difference was seen. These
results demonstrated the usefulness of this marking
method because it clearly reduced the misalignment
Figure 4. Rotation observed for each design. Negative values indicate after surgery.
an anti-clockwise rotation and positive values indicate a clockwise rota- There are several studies on toric IOL rotation,1,2,11-13
tion. The AcrySof IQ and AcrySof IQ ReSTOR are manufactured by Alcon
Laboratories, Inc., Fort Worth, TX. The enVista is manufactured by Bausch
but to the best of our knowledge this is the first study
& Lomb, Rochester, NY. The Lentis LT is manufactured by Oculentis, to compare rotational stability between monofocal and
Berlin, Germany. multifocal toric IOLs and between different designs.
Moreover, in this study, monofocal toric IOLs were
At 30 days postoperatively, 90.5% of eyes im- compared with the surgery protocol performed by the
planted with the enVista toric IOL showed less than same surgeon. Toric IOL rotation after implantation
5° of rotation, whereas the figures for the AcrySof IQ was due to various mechanisms. Factors that may in-
toric IOL and Lentis LT IOL were 64.3% and 64.6%, duce toric IOL rotation include postoperative intraoc-
respectively. More than 10° of rotation was observed ular pressure fluctuations,18 reduced friction between
in 21.4% of eyes with the AcrySof toric IOL, 9.5% with the haptics and the capsular bags produced by an in-
the enVista toric IOL, and 14.28% with the Lentis LT complete ophthalmic viscoelastic device removal,19 or
IOL. capsule size,20 IOL design and materials,12 and com-
There was a correlation between postoperative pression of the IOL from capsule shrinkage.21
UDVA and postoperative cylinder power in the mono- The current results indicated that rotation occurs
focal and multifocal IOLs implanted (r = 0.807, P < in all of the lenses during the first hour after surgery
.001 and r = 0.631, P < .001, respectively), between and remains stable during the first month. These re-
postoperative UDVA and rotation 30 days after the sults were in agreement with others demonstrating
surgery in multifocal IOLs (r = 0.787, P = .001), and be- that rotation occurred 1 hour after surgery.12 The fact
tween postoperative UDVA and rotation 30 days after that the rotation takes place so quickly suggests that it
surgery in eyes implanted with monofocal IOLs (r = might be a consequence of poor friction between the
0.439, P = .011). haptic and the capsular bag due to an incomplete oph-
thalmic viscoelastic device clearance, as previously
DISCUSSION suggested. Alternatively, it could be due to the size
In this study, a new toric IOL marking method was difference between the capsular bag and IOL diam-
proposed that minimizes patient movement errors by eter. A large diameter of the lens with respect to the
having the patient sitting or standing while adopting a capsule would produce more friction and therefore
normal head position. The marks were made at a dis- a minimal risk of rotation, but could provoke distor-
tance at which there should be no convergence in bilat- tion of the capsular bag and zonules. Nevertheless, it
eral viewing conditions, avoiding possible monocular is important to note that the preoperative calculation
cyclotorsion. The main error of all available methods of the capsule size is complicated and there is not
published to date was regarding the marking because a clear relation between parameters such as corneal
the general idea was that those marks performed in the diameter and capsule size.22
0° to 180° axis corresponded just to that meridian. It When the mean rotation among the different toric
is almost impossible to avoid the typical patient reflex monofocal IOLs was compared, the AcrySof IQ and
of small eye movements, eyes closing, or head turning enVista toric lenses showed less rotation than the
when seeing the marker approaching. These changes Lentis LT lens, although none of the lenses showed a
can generate errors of up to 15° and therefore will af- mean rotation of more than 5°. Both the AcrySof IQ
fect the final refraction after surgery. toric and enVista lenses are open-loop haptic lenses,
The main advantage of the marking method de- whereas the Lentis LT is a plate-haptic lens. These
scribed in the current study compared to existing ones characteristics may be the reasons for these variations
was the checking of the real axis marked with gentian in the rotation among the different lenses. Neverthe-
6 Copyright © SLACK Incorporated
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
less, it is important to indicate that these results were achieved by patients with multifocal toric IOLs was
in disagreement with those described by Patel et al.23 comparable to that obtained by patients with monofo-
because they described plate-haptic lenses as more sta- cal toric IOLs.
ble in terms of rotation than open-loop haptic lenses. The new marking method for the alignment of toric
Interestingly, Prinz et al.12 found a similar rotational IOLs is effective and it is not influenced by conver-
behavior between both lens designs. Surprisingly, the gence, monocular cyclotorsion, or both. On the other
multifocal design of the AcrySof IQ toric IOL showed hand, all toric IOLs studied (both monocular and mul-
2° more rotation than the monofocal design. It remains tifocal) showed rotation 1 hour after surgery. This rota-
unclear whether the haptic design plays an important tion was stable during the first month and had slightly
role in lens rotation and hence the controversy about more influence on UDVA after multifocal than mono-
which haptic design is better for rotational stability. focal toric IOL implantation.
More studies are needed to clarify this point.
Stephenson24 reported 9% of patients implanted AUTHOR CONTRIBUTIONS
with the enVista toric lens showed a rotation of greater Study concept and design (NG, FP); data collection (NG, BOD,
than 5°. This result is similar to that achieved with JLR-G); analysis and interpretation of data (NG, FP, JAQ); drafting
this lens in the current study. Our results were slightly of the manuscript (BOD, JLR-G); critical revision of the manuscript
worse than those reported by Chua et al.11 for the Ac- (NG, FP, JAQ); statistical expertise (NG, JAQ); supervision (NG, FP)
rySof monofocal lens. The literature contained no in-
formation on the Lentis LT lenses for any comparison REFERENCES
to be made. With respect to the AcrySof toric multifo- 1. Bachernegg A, Ruckl T, Riha W, Grabner G, Dexl AK. Rotational
stability and visual outcome after implantation of a new toric
cal lens, our results contrast with those of other stud- intraocular lens for the correction of corneal astigmatism during
ies14 that report a lens rotation of no more than 10°; in cataract surgery. J Cataract Refract Surg. 2013;39:1390-1398.
the current study, 17.68% of patients showed a rota- 2. Wolffsohn JS, Buckhurst PJ. Objective analysis of toric intra-
tion of at least this amount. ocular lens rotation and centration. J Cataract Refract Surg.
2010;36:778-782.
Postoperative UDVA was similar for all monofo-
3. Felipe A, Artigas JM, Diez-Ajenjo A, Garcia-Domene C, Alcocer
cal toric IOLs and also when we compared monofocal P. Residual astigmatism produced by toric intraocular lens rota-
with multifocal lenses. The results presented here con- tion. J Cataract Refract Surg. 2011;37:1895-1901.
firm the results described by other studies indicating 4. Jain AK, Gupta R, Chakma P. A simple technique for corneal
that the use of toric IOLs permits patients to achieve marking before toric intraocular lens implantation. J Cataract
good UDVA after surgery.15,25 With respect to UDVA, Refract Surg. 2013;39:966-967.
0.1 logMAR or better was achieved with 66.4% of the 5. Roumeliotis GA, Hutnik CM. A simple, reproducible, and cost
effective axis marking system for toric lens implantation. J Re-
monofocal toric lenses and with 46.4% of the multifo- fract Surg. 2012;28:12-13.
cal toric lenses. Other studies with monofocal lenses 6. Visser N, Berendschot TT, Bauer NJ, Jurich J, Kersting O, Nuijts
have reported similar results with the AcrySof toric RM. Accuracy of toric intraocular lens implantation in cataract
IOL26-28 and enVista toric IOL.24 The literature contains and refractive surgery. J Cataract Refract Surg. 2011;37:1394-1402.
no reports on the Lentis LT lenses that would allow 7. Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking
a comparison. Other studies14 on the same multifocal method for a toric intraocular lens: mapping method. J Refract
Surg. 2011;27:375-379.
lens report similar results to those of the current study.
8. Graether JM. Simplified system of marking the cornea for a toric
One of the goals of the current study was to see how intraocular lens. J Cataract Refract Surg. 2009;35:1498-1500.
IOL rotation affects UDVA when different designs 9. Viestenz A, Seitz B, Langenbucher A. Evaluating the eye’s ro-
are used and to compare monofocal and multifocal tational stability during standard photography: effect on deter-
lenses. A correlation was found between UDVA and mining the axial orientation of toric intraocular lenses. J Cata-
ract Refract Surg. 2005;31:557-561.
rotation with monofocal and multifocal lenses, which
was stronger in the case of toric multifocal IOLs. The 10. Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4
corneal astigmatic marking methods. J Cataract Refract Surg.
correlation was positive in both cases, indicating that 2012;38:2094-2099.
the higher the lens rotation, the higher the logMAR 11. Chua WH, Yuen LH, Chua J, Teh G, Hill WE. Matched com-
UDVA value obtained, and therefore worse visual acu- parison of rotational stability of 1-piece acrylic and plate-haptic
ity. It was expected that patients’ visual acuity would silicone toric intraocular lenses in Asian eyes. J Cataract Re-
fract Surg. 2012;38:620-624.
be more affected by a greater rotation of the multifo-
12. Prinz A, Neumayer T, Buehl W, et al. Rotational stability
cal lenses. In this regard, the distorted image caused and posterior capsule opacification of a plate-haptic and an
by residual astigmatism due to rotation was added to open-loop-haptic intraocular lens. J Cataract Refract Surg.
the loss of image quality due to the apodized diffrac- 2011;37:251-257.
tive design of multifocal toric IOLs. Still, the UDVA 13. Buckhurst PJ, Wolffsohn JS, Naroo SA, Davies LN. Rotational and
Journal of Refractive Surgery • Vol. 31, No. 2, 2015 7
Implantation of Monofocal and Multifocal Toric IOLs/Garzón et al
centration stability of an aspheric intraocular lens with a simulated asymmetric capsule shrinkage in rabbits. J Cataract Refract
toric design. J Cataract Refract Surg. 2010;36:1523-1528. Surg. 1999;25:1147-1150.
14. Ferreira TB, Marques EF, Rodrigues A, Montes-Mico R. Visual 22. Khng C, Osher RH. Evaluation of the relationship between
and optical outcomes of a diffractive multifocal toric intraocu- corneal diameter and lens diameter. J Cataract Refract Surg.
lar lens. J Cataract Refract Surg. 2013;39:1029-1035. 2008;34:475-479.
15. Alfonso JF, Knorz M, Fernandez-Vega L, et al. Clinical out- 23. Patel CK, Ormonde S, Rosen PH, Bron AJ. Postoperative in-
comes after bilateral implantation of an apodized +3.0 D toric traocular lens rotation: a randomized comparison of plate and
diffractive multifocal intraocular lens. J Cataract Refract Surg. loop haptic implants. Ophthalmology. 1999;106:2190-2195.
2014;40:51-59. 24. Stephenson M. Early users share the enVista experience.
16. Bellucci R, Bauer NJ, Daya SM, et al. Visual acuity and refrac- Review of Ophthalmology. 2013;January(available: http://
tion with a diffractive multifocal toric intraocular lens. J Cata- www.reviewofophthalmology.com/content/t/intraocular_
ract Refract Surg. 2013;39:1507-1518. lenses/c/38573/)
17. Williams JR. The Declaration of Helsinki and public health. 25. Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: his-
Bull World Health Organ. 2008;86:650-652. torical overview, patient selection, IOL calculation, surgical
techniques, clinical outcomes, and complications. J Cataract
18. Pereira FA, Milverton EJ, Coroneo MT. Miyake-Apple study of
Refract Surg. 2013;39:624-637.
the rotational stability of the AcrySof Toric intraocular lens af-
ter experimental eye trauma. Eye (Lond). 2010;24:376-378. 26. Mendicute J, Irigoyen C, Aramberri J, Ondarra A, Montés-Micó
R. Foldable toric intraocular lens for astigmatism correction in
19. Chang DF. Early rotational stability of the longer Staar toric in-
cataract patients. J Cataract Refract Surg. 2008;34:601-607.
traocular lens: fifty consecutive cases. J Cataract Refract Surg.
2003;29:935-940. 27. Dardzhikova A, Shah CR, Gimbel HV. Early experience with
the AcrySof toric IOL for the correction of astigmatism in cata-
20. Ohmi S. Decentration associated with asymmetric capsular
ract surgery. Can J Ophthalmol. 2009;44:269-273.
shrinkage and intraocular lens size. J Cataract Refract Surg.
1993;19:640-643. 28. Tsinopoulos IT, Tsaousis KT, Tsakpinis D, Ziakas NG, Dimi-
trakos SA. Acrylic toric intraocular lens implantation: a single
21. Ohmi S, Tanaka S, Saika S, Ohnishi Y. Silicone and
center experience concerning clinical outcomes and postopera-
poly(methyl methacrylate) lens decentration associated with
tive rotation. Clin Ophthalmol. 2010;4:137-142.
AUTHOR QUERIES
AQ1 Please provide the full manufacturer and location (inluding manufacturer name, city, and country).
8 Copyright © SLACK Incorporated
TABLE A
Characteristic Details of Implanted IOLs
Parameter AcrySof IQ Toric IOL enVista Toric IOL Lentis LT IOL AcrySof IQ ReSTOR Toric IOL
Type Toric Toric Toric Multifocal toric
Design Open-loop haptic Open-loop haptic Plate-haptic Open-loop haptic
Optic size 6.0 mm 6.0 mm 6.0 mm 6.0 mm
Overall length 13.0 mm 12.50 mm 11.0 mm 13.0 mm
Optic design Biconvex toric Aspheric Biconvex aspheric Biconvex apodized
aspheric monotoric diffractive aspheric toric
IOL powers (D) +6 to +30 +10 to +30 +10 to +30 +6 to +30
IOL cylinders (D) 1.50 to 6.00 (T3-T9) 1.25 to 5.75 1.50 to 5.25 (T1-T6) 1.00 to 3.00 (T2-T5)
Haptic angulation 0° 0° 0° 0°
Refractive index 1.55 1.54 1.46 1.55
IOL = intraocular lens; D = diopters
The AcrySof IQ and AcrySof IQ ReSTOR are manufactured by Alcon Laboratories, Inc., Fort Worth, TX. The enVista is manufactured by Bausch & Lomb, Rochester,
NY. The Lentis LT is manufactured by Oculentis, Berlin, Germany.
Figure A. Comparison of postoperative uncorrected distance visual acuity
Figure B. Comparison of postoperative refractive astigmatism frequency
frequency at 30 days between monofocal toric intraocular lenses (IOLs) (n
at 30 days between monofocal toric intraocular lenses (IOLs) (n = 63)
= 63) and multifocal toric IOLs (n = 28) for different visual acuity values.
and multifocal toric IOLs (n = 28) for different powers.
Figure C. Box and whiskers plot of rotation of monofocal toric intraocular
lenses (IOLs) (n = 63) and multifocal toric IOLs (n = 28) at each follow-
up visit. Values are represented as median and quartiles.
You might also like
- FBC Vision Screening Template (FVA LMA)Document6 pagesFBC Vision Screening Template (FVA LMA)Taylor BrownNo ratings yet
- Peripheral Vision Improvement ExercisesDocument4 pagesPeripheral Vision Improvement Exercisesmanchiraju raj kumarNo ratings yet
- Research Article: Clinical Results of Diffractive, Refractive, Hybrid Multifocal, and Monofocal Intraocular LensesDocument13 pagesResearch Article: Clinical Results of Diffractive, Refractive, Hybrid Multifocal, and Monofocal Intraocular LensesFitrianiMpiitNo ratings yet
- At Lisatri ArticleDocument10 pagesAt Lisatri ArticleStefoane MadalinNo ratings yet
- Jurnal KuDocument6 pagesJurnal KuTamsilNo ratings yet
- Evaluation of Refractive Error After Cataract Surgery in Highly Myopic EyesDocument6 pagesEvaluation of Refractive Error After Cataract Surgery in Highly Myopic Eyeshenok birukNo ratings yet
- Journal Reading Mata - Pricilia Dan NadyaDocument14 pagesJournal Reading Mata - Pricilia Dan Nadyastepanus 102018062No ratings yet
- Reverse Optic Capture of The SingleDocument10 pagesReverse Optic Capture of The SingleIfaamaninaNo ratings yet
- Clinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaDocument6 pagesClinical Study: Aspheric Intraocular Lenses Implantation For Cataract Patients With Extreme MyopiaKevin ArdiansyahNo ratings yet
- Status Anak - Fitriani (Print)Document31 pagesStatus Anak - Fitriani (Print)FitrianiMpiitNo ratings yet
- Wa0000Document7 pagesWa0000Ocha24 TupamahuNo ratings yet
- Ebn RugayDocument6 pagesEbn RugayJeffrey Barcelon TanglaoNo ratings yet
- Ophthalmology: Journal of and Advance ResearchDocument7 pagesOphthalmology: Journal of and Advance ResearchAthenaeum Scientific PublishersNo ratings yet
- Influence of Postoperative Astigmatism On Uncorrected Near Visual Acuity in PseudophakiaDocument7 pagesInfluence of Postoperative Astigmatism On Uncorrected Near Visual Acuity in PseudophakiaIJAR JOURNALNo ratings yet
- Rotational Stability of Toric Intraocular - 2022 - Medical Journal Armed ForcesDocument6 pagesRotational Stability of Toric Intraocular - 2022 - Medical Journal Armed ForcesAnisha RanaNo ratings yet
- Ascrs 2Document7 pagesAscrs 2leokapilNo ratings yet
- Highlights From The 2011 ICL/Toric ICL Experts Symposium: Insert ToDocument8 pagesHighlights From The 2011 ICL/Toric ICL Experts Symposium: Insert ToArif MohammadNo ratings yet
- Iris-Claw Intraocular Lenses To Correct Aphakia in The Absence of Capsule SupportDocument6 pagesIris-Claw Intraocular Lenses To Correct Aphakia in The Absence of Capsule SupportAnonymous k4F8sAs25No ratings yet
- Research ArticleDocument9 pagesResearch ArticleRaissaNo ratings yet
- Kjo Jurnal MataDocument7 pagesKjo Jurnal Matanurul hidayati sNo ratings yet
- Visual and Patient-Reported Outcomes of A Diffractive Trifocal Intraocular Lens Compared With Those of A Monofocal Intraocular LensDocument11 pagesVisual and Patient-Reported Outcomes of A Diffractive Trifocal Intraocular Lens Compared With Those of A Monofocal Intraocular Lensakun kd876No ratings yet
- Therapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismDocument7 pagesTherapeutic Effectiveness of Toric Implantable Collamer Lens in Treating Ultrahigh Myopic AstigmatismStephanie PfengNo ratings yet
- Moore 2024Document13 pagesMoore 2024youthcp93No ratings yet
- One-Year Results of Health-Related and Vision-Related Quality of Life After Clear Lens Extraction and Multifocal Intraocular Lens ImplantationDocument5 pagesOne-Year Results of Health-Related and Vision-Related Quality of Life After Clear Lens Extraction and Multifocal Intraocular Lens ImplantationDanty IndriastutyNo ratings yet
- s12886 022 02620 7Document8 pagess12886 022 02620 7MarioNo ratings yet
- IolDocument7 pagesIolAnonymous h0DxuJTNo ratings yet
- Toric ICLDocument8 pagesToric ICLjbahalkehNo ratings yet
- Ju 2023Document9 pagesJu 2023youthcp93No ratings yet
- 3 Piece IOL SCL FixDocument6 pages3 Piece IOL SCL FixTvrtka BenašićNo ratings yet
- Fixation Stability, Fixation Location, and Visual Acuity After Successful Macular Hole SurgeryDocument6 pagesFixation Stability, Fixation Location, and Visual Acuity After Successful Macular Hole SurgeryAlpi AnorNo ratings yet
- 2016 Article 229Document7 pages2016 Article 229nisa_kartikaNo ratings yet
- Mertens - The Staar Toric ICLDocument4 pagesMertens - The Staar Toric ICLAndreea L. MihalceaNo ratings yet
- Visual and Refractive Outcomes of Small-Incision Lenticule Extraction in High Myopia - 5-Year ResultsDocument7 pagesVisual and Refractive Outcomes of Small-Incision Lenticule Extraction in High Myopia - 5-Year Resultspriscilla christina natanNo ratings yet
- Clinical Differences Between Toric Intraocular LenDocument8 pagesClinical Differences Between Toric Intraocular LenonderonderNo ratings yet
- Adminku Journal Manager ErlaniDocument7 pagesAdminku Journal Manager Erlanirm suryaubungNo ratings yet
- ArtIOLs - Biblio 2Document16 pagesArtIOLs - Biblio 2blazquezjoseignacioNo ratings yet
- Acta Ophthalmologica - 2018 - Garc A Montero - Binocular Vision Alterations After Refractive and Cataract Surgery A ReviewDocument11 pagesActa Ophthalmologica - 2018 - Garc A Montero - Binocular Vision Alterations After Refractive and Cataract Surgery A ReviewFrancisco Arturo MánuelNo ratings yet
- Sulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryDocument6 pagesSulcus Implantation of A Single-Piece Foldable Acrylic Intraocular Lens After Posterior Capsular Rupture in Cataract SurgeryPrizilia SaimimaNo ratings yet
- Karakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia LatuasanDocument10 pagesKarakteristik Klinis Dan Hasil Implantasi Lensa Intra Okular Iris Claw Pada Kasus Afakia Di Rumah Sakit Mata Cicendo - Azalia Latuasanwasobiru isbiruNo ratings yet
- Ecop 09 00286Document11 pagesEcop 09 00286GabrielNo ratings yet
- Evaluation of SuturlessDocument7 pagesEvaluation of SuturlesskenapayaNo ratings yet
- Astigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionDocument6 pagesAstigmatic Change in Manual Small Incision Cataract Surgery (MSICS) With Chevron Type of IncisionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- BSN Reading (Scleral Buckling) RosalesDocument8 pagesBSN Reading (Scleral Buckling) RosalesYvonnie RosalesNo ratings yet
- 1112CRSTEuro Cs VinciguerraDocument3 pages1112CRSTEuro Cs VinciguerraR Andres Plaza ZNo ratings yet
- Effectiveness of Accommodating Intra Ocular Lens: Department of Ophthalmology, Faculty of Medicine, Universitas LampungDocument7 pagesEffectiveness of Accommodating Intra Ocular Lens: Department of Ophthalmology, Faculty of Medicine, Universitas LampungayuNo ratings yet
- Intraindividual Comparison of Aspherical and Spherical Intraocular Lenses of Same Material and PlatformDocument6 pagesIntraindividual Comparison of Aspherical and Spherical Intraocular Lenses of Same Material and PlatformAkhilesh KumarNo ratings yet
- 25904-Texto Do Trabalho-118421-1-10-20221008Document10 pages25904-Texto Do Trabalho-118421-1-10-20221008vergarajaviera548No ratings yet
- #12 Baviera RayOne EMV Study White PaperDocument6 pages#12 Baviera RayOne EMV Study White PaperPiet ConradieNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleAnnisak FitriyanaNo ratings yet
- Visualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot StudyDocument15 pagesVisualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot Studymistic0No ratings yet
- s12886 022 02600 XDocument8 pagess12886 022 02600 XHariom ShuklaNo ratings yet
- Visual Outcomes and Accommodat PDFDocument13 pagesVisual Outcomes and Accommodat PDFfatiNo ratings yet
- Corneal Endothelial Morphologic Assessment in Pediatric Cataract Surgery With Intraocular Lens Implantation - A Comparison of Preoperative and Early Postoperative Specular MicrosDocument8 pagesCorneal Endothelial Morphologic Assessment in Pediatric Cataract Surgery With Intraocular Lens Implantation - A Comparison of Preoperative and Early Postoperative Specular MicrosRael Rodrigues Dos SantosNo ratings yet
- Jurding MataDocument7 pagesJurding Matarandy_27995No ratings yet
- Chang 2016Document5 pagesChang 2016steviaNo ratings yet
- SocivoDocument16 pagesSocivoSlobodan MilovanovicNo ratings yet
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocument10 pagesClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNo ratings yet
- Iris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaDocument7 pagesIris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implanations in Correcting AphakiaMuhammad SukriNo ratings yet
- Coscarelli, 2012Document8 pagesCoscarelli, 2012vitor auzierNo ratings yet
- 1 s2.0 S2773157X2400047X MainDocument3 pages1 s2.0 S2773157X2400047X MainomarNo ratings yet
- Early Intervention in Orbital Floor Fractures: Postoperative Ocular Motility and Diplopia OutcomesDocument9 pagesEarly Intervention in Orbital Floor Fractures: Postoperative Ocular Motility and Diplopia OutcomesHải Ngọc Đinh VũNo ratings yet
- Current Advances in Ophthalmic TechnologyFrom EverandCurrent Advances in Ophthalmic TechnologyParul IchhpujaniNo ratings yet
- D D I 6055.04 D D M V T S: O Nstruction O Otor Ehicle and Raffic AfetyDocument38 pagesD D I 6055.04 D D M V T S: O Nstruction O Otor Ehicle and Raffic AfetyEnrique Ferrando BarbenaNo ratings yet
- c145 CorruptionDocument178 pagesc145 CorruptionEnrique Ferrando BarbenaNo ratings yet
- Ordinance # 2001-23: E:/Wpdata/Efm/Dcaol-2/Ol02.0RdDocument26 pagesOrdinance # 2001-23: E:/Wpdata/Efm/Dcaol-2/Ol02.0RdEnrique Ferrando BarbenaNo ratings yet
- Kas16 - Mat&Des - Correlation Between Porosity and Processing Parameters in TiAl6V4 Produced by Selective Laser Melting+corrigendumDocument13 pagesKas16 - Mat&Des - Correlation Between Porosity and Processing Parameters in TiAl6V4 Produced by Selective Laser Melting+corrigendumEnrique Ferrando BarbenaNo ratings yet
- Value Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatDocument5 pagesValue Focus: Tecnis Synergy Iols - A Breakthrough Innovation ThatEnrique Ferrando BarbenaNo ratings yet
- A123 Rev PDFDocument35 pagesA123 Rev PDFEnrique Ferrando BarbenaNo ratings yet
- Top 10 Taxpayer Report: 2020 City of CombineDocument55 pagesTop 10 Taxpayer Report: 2020 City of CombineEnrique Ferrando BarbenaNo ratings yet
- CMS Manual System: Pub 100-04 Medicare Claims ProcessingDocument17 pagesCMS Manual System: Pub 100-04 Medicare Claims ProcessingEnrique Ferrando BarbenaNo ratings yet
- 07 Kuha Dandolo Chronica PDFDocument18 pages07 Kuha Dandolo Chronica PDFEnrique Ferrando BarbenaNo ratings yet
- Citrix Netscaler Data SheetDocument12 pagesCitrix Netscaler Data SheetEnrique Ferrando BarbenaNo ratings yet
- Yaesu G-800S G-800SDX G-1000S SDX User PDFDocument21 pagesYaesu G-800S G-800SDX G-1000S SDX User PDFEnrique Ferrando BarbenaNo ratings yet
- SC1 Mod 3-4 Fuzzy-Applications 811 AaDocument15 pagesSC1 Mod 3-4 Fuzzy-Applications 811 AaEnrique Ferrando BarbenaNo ratings yet
- BrmsDocument210 pagesBrmsEnrique Ferrando BarbenaNo ratings yet
- SS34 C8678Document2 pagesSS34 C8678Enrique Ferrando BarbenaNo ratings yet
- UMP SEBB Preferred Drug ListDocument135 pagesUMP SEBB Preferred Drug ListEnrique Ferrando BarbenaNo ratings yet
- Manual en PDFDocument81 pagesManual en PDFEnrique Ferrando BarbenaNo ratings yet
- Quartz Crystal SS3: Pin Type Crystal 11.35 X 4.65 MMDocument2 pagesQuartz Crystal SS3: Pin Type Crystal 11.35 X 4.65 MMEnrique Ferrando BarbenaNo ratings yet
- Commercial Chinook: Mark LambertreportsfromphiladelphiaDocument1 pageCommercial Chinook: Mark LambertreportsfromphiladelphiaEnrique Ferrando BarbenaNo ratings yet
- Man ENDocument94 pagesMan ENEnrique Ferrando BarbenaNo ratings yet
- AMI US Dollar RatesDocument1 pageAMI US Dollar RatesEnrique Ferrando BarbenaNo ratings yet
- Bird Tours GBPDocument9 pagesBird Tours GBPEnrique Ferrando BarbenaNo ratings yet
- KDC-168U: Instruction Manual Mode D'Emploi Manual de InstruccionesDocument64 pagesKDC-168U: Instruction Manual Mode D'Emploi Manual de InstruccionesEnrique Ferrando BarbenaNo ratings yet
- Finitte DiferenceDocument522 pagesFinitte DiferenceEnrique Ferrando Barbena100% (1)
- Colorandquality 1Document59 pagesColorandquality 1oktay yetginNo ratings yet
- Cet 5Document4 pagesCet 5jumi26No ratings yet
- SBI Eye - Surgery 1Document24 pagesSBI Eye - Surgery 1Munam WaqarNo ratings yet
- Method of Extending The Range of The KeratometerDocument3 pagesMethod of Extending The Range of The KeratometerDanielle SangalangNo ratings yet
- Modified Sewing Machine Technique For IridodialysiDocument8 pagesModified Sewing Machine Technique For IridodialysiRonal PerinoNo ratings yet
- Physio Lab PBLDocument4 pagesPhysio Lab PBLtheodore_estradaNo ratings yet
- Anatomy of The Eye, Orbit and Related Structures: Basic Science ExaminationDocument8 pagesAnatomy of The Eye, Orbit and Related Structures: Basic Science ExaminationOana PaladeNo ratings yet
- Lab Manual - Senses Eye - A+p - 2-12-18Document19 pagesLab Manual - Senses Eye - A+p - 2-12-18Ajit Sinha0% (1)
- Intravitreal Injection of Triamcinolone Acetonide: Core MessagesDocument22 pagesIntravitreal Injection of Triamcinolone Acetonide: Core MessagesSiva LoveNo ratings yet
- Igcse AccommodationDocument3 pagesIgcse AccommodationChr1zFX4No ratings yet
- Tatalaksana Katarak Komplikata Yang Disebabkan Oleh Uveitis - Ericka Febriyanti Pratama Putri 1Document14 pagesTatalaksana Katarak Komplikata Yang Disebabkan Oleh Uveitis - Ericka Febriyanti Pratama Putri 1Cynthia Isra MandahutaNo ratings yet
- A Pinhole Camera Has No Lens.Document1 pageA Pinhole Camera Has No Lens.M. Amaan AamirNo ratings yet
- Angle Recession GlaucomaDocument15 pagesAngle Recession GlaucomaDia Asri RusliNo ratings yet
- Glaucoma PPT For Final YearDocument57 pagesGlaucoma PPT For Final YearDarshan SinghNo ratings yet
- IOL PowerDocument273 pagesIOL Powermarlon García100% (3)
- Stargardt DiseaseDocument9 pagesStargardt DiseaseEstefhany SCNo ratings yet
- Anatomy and Physiology of The EyeDocument18 pagesAnatomy and Physiology of The EyeMargaretha AdhiningrumNo ratings yet
- Poze La Partic CliniceDocument3 pagesPoze La Partic CliniceLoredana CiubotaruNo ratings yet
- Notification Admit Card Results Exam AnalysisDocument10 pagesNotification Admit Card Results Exam AnalysisChellamani UmakanthanNo ratings yet
- Inventario Pink Up - Hoja 1Document7 pagesInventario Pink Up - Hoja 1Mich RiveraNo ratings yet
- TopazDocument2 pagesTopazJoevince Neil GacusNo ratings yet
- Maders Understanding Human Anatomy and Physiology 8th Edition Susannah Nelson Longenbaker Test Bank Full Chapter PDFDocument68 pagesMaders Understanding Human Anatomy and Physiology 8th Edition Susannah Nelson Longenbaker Test Bank Full Chapter PDFCindyCurrywpbfd100% (11)
- PDF Neuroanatomy Text and Atlas John D Martin Ebook Full ChapterDocument53 pagesPDF Neuroanatomy Text and Atlas John D Martin Ebook Full Chapteroscar.warner960100% (1)
- Fusion and Binocular SummationDocument3 pagesFusion and Binocular Summationblack00swanNo ratings yet
- OphthalmologyDocument12 pagesOphthalmologyMahesh Shrestha100% (1)
- ReferencesDocument6 pagesReferencesAndrew MakariosNo ratings yet
- Human Eye PDFDocument13 pagesHuman Eye PDFHaidir MuhammadNo ratings yet