Professional Documents
Culture Documents
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
Uploaded by
Danisa AzzahraCopyright:
Available Formats
You might also like
- Cell Organelles WorksheetDocument8 pagesCell Organelles WorksheetJohn OsborneNo ratings yet
- An Asian Perspective On Povidone Iodine in Wound Healing: Review PaperDocument11 pagesAn Asian Perspective On Povidone Iodine in Wound Healing: Review PaperAsmita KurniaNo ratings yet
- Study On Emergence of MDR Pathogen and Its Microbiological StudyDocument9 pagesStudy On Emergence of MDR Pathogen and Its Microbiological StudyIJAR JOURNALNo ratings yet
- Locally Administered Probiotic, RCT-articleDocument7 pagesLocally Administered Probiotic, RCT-articleDebjyoti DebnathNo ratings yet
- Hoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFDocument9 pagesHoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFMini Bekti NingsihNo ratings yet
- J Ajo 2020 03 018Document24 pagesJ Ajo 2020 03 018koas forensikNo ratings yet
- Acne CaseDocument5 pagesAcne CaseVeselina StefanovaNo ratings yet
- Gels 08 00163Document10 pagesGels 08 00163Andreea BarbuNo ratings yet
- (M299) RL3Document11 pages(M299) RL3Jessa Louise TurredaNo ratings yet
- A Study On Resistance Pattern of Bacteria Isolated From Diabetic and Non - Diabetic UlcersDocument7 pagesA Study On Resistance Pattern of Bacteria Isolated From Diabetic and Non - Diabetic UlcersBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Kanagalingam2015 PDFDocument10 pagesKanagalingam2015 PDFwatidinaNo ratings yet
- Comparative Evaluation of Locally Delivered.12Document7 pagesComparative Evaluation of Locally Delivered.12samanvi badriNo ratings yet
- RUSSO, Bud-Poplar-Extract-Embedded Chitosan Films AsDocument21 pagesRUSSO, Bud-Poplar-Extract-Embedded Chitosan Films AsANNE LOUISE FALCAO PASCOALNo ratings yet
- Fmicb 12 723834Document16 pagesFmicb 12 723834shalusinhaNo ratings yet
- 10 1016@j Mycmed 2018 08 002Document5 pages10 1016@j Mycmed 2018 08 002Feni SyawelmiNo ratings yet
- A Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyDocument15 pagesA Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyIJAR JOURNALNo ratings yet
- Prospective, Randomized Clinical Trial ofDocument10 pagesProspective, Randomized Clinical Trial ofFarhan RezaNo ratings yet
- Cuppa Wao Journal ProofsDocument22 pagesCuppa Wao Journal ProofsFajar SetiawanNo ratings yet
- 1 s2.0 S0899900715003871 MainDocument7 pages1 s2.0 S0899900715003871 MainThảo Bùi ThanhNo ratings yet
- DR Vidya SagarDocument7 pagesDR Vidya SagarAnil KumarNo ratings yet
- Promote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportDocument4 pagesPromote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportShira michaelNo ratings yet
- 1 s2.0 S092485792030234X MainDocument11 pages1 s2.0 S092485792030234X MainPedro GouveiaNo ratings yet
- Jurnal EED 3Document10 pagesJurnal EED 3Garsa GarnolNo ratings yet
- International Journal of Antimicrobial AgentsDocument11 pagesInternational Journal of Antimicrobial AgentsRita SukitaNo ratings yet
- Understanding Antimicrobial Susceptibility Profile of Finegoldia Magna An Insight To An Untrodden PathDocument5 pagesUnderstanding Antimicrobial Susceptibility Profile of Finegoldia Magna An Insight To An Untrodden Pathd4rkgr455No ratings yet
- A Study On The Healing Effect of Honey On Infected Open Fracture WoundsDocument3 pagesA Study On The Healing Effect of Honey On Infected Open Fracture WoundsMuhammad AlamzebNo ratings yet
- (M299) RL2Document11 pages(M299) RL2Jessa Louise TurredaNo ratings yet
- Designing A Multi-Epitope Vaccine Against Shigella Dysenteriae Using Immuno-Informatics ApproachDocument14 pagesDesigning A Multi-Epitope Vaccine Against Shigella Dysenteriae Using Immuno-Informatics ApproachDr. Sunil RaiNo ratings yet
- Ditorial The Challenge of Controlling Infectious Keratitis: Tom - Lietman@ Ucsf - EduDocument2 pagesDitorial The Challenge of Controlling Infectious Keratitis: Tom - Lietman@ Ucsf - Eduwawan 88No ratings yet
- 10 1111@iwj 13463Document7 pages10 1111@iwj 13463burhanNo ratings yet
- Nitric Oxide Mediated Staphylococcus Aureus Pathogenesis and Protective Role of Nanoconjugated VancomycinDocument8 pagesNitric Oxide Mediated Staphylococcus Aureus Pathogenesis and Protective Role of Nanoconjugated Vancomycinlolamusic90No ratings yet
- Case Study: Bronchopneumoniae With Melioidosis Infection in A Paediatric PatientDocument8 pagesCase Study: Bronchopneumoniae With Melioidosis Infection in A Paediatric PatientlolllllNo ratings yet
- 2020 The Potential of Probiotics For Treating Acne Vulgaris - A Review of Literature On Acne and MicrobiotDocument6 pages2020 The Potential of Probiotics For Treating Acne Vulgaris - A Review of Literature On Acne and MicrobiotJeslyn TengkawanNo ratings yet
- Engineering Probiotics For Therapeutic ApplicationsDocument9 pagesEngineering Probiotics For Therapeutic ApplicationsElinaNo ratings yet
- The Use of Antimicrobial Peptides in Ophthalmology: An Experimental Study in Corneal Preservation and The Management of Bacterial KeratitisDocument30 pagesThe Use of Antimicrobial Peptides in Ophthalmology: An Experimental Study in Corneal Preservation and The Management of Bacterial KeratitisAgam ThebadboysNo ratings yet
- Journal of Periodontology - 2021 - Lu - Effect of Adjunctive Systemic Antibiotics On Microbial Populations Compared WithDocument14 pagesJournal of Periodontology - 2021 - Lu - Effect of Adjunctive Systemic Antibiotics On Microbial Populations Compared WithShakeel AhmedNo ratings yet
- Fmicb 08 00659Document9 pagesFmicb 08 00659Helena VenanteNo ratings yet
- Antibiotic in CDDocument11 pagesAntibiotic in CDYaseerNo ratings yet
- Development of Polyurethane Foam Dressing Containing Silver and Asiaticoside For Healing of Dermal WoundDocument15 pagesDevelopment of Polyurethane Foam Dressing Containing Silver and Asiaticoside For Healing of Dermal WoundritaNo ratings yet
- Adrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077Document5 pagesAdrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077Ous linosNo ratings yet
- Current Anti-Biofilm Strategies and Potential of Antioxidants in Biofilm ControlDocument10 pagesCurrent Anti-Biofilm Strategies and Potential of Antioxidants in Biofilm ControlBeshoy RafatNo ratings yet
- Chenodeoxycholic Acid-Amikacin Combination Enhances ERradication of StaphyDocument17 pagesChenodeoxycholic Acid-Amikacin Combination Enhances ERradication of StaphyAlex HernandezNo ratings yet
- Novel Bacteriophage Specific Against Staphylococcus Epidermidis and With Antibiofilm ActivityDocument11 pagesNovel Bacteriophage Specific Against Staphylococcus Epidermidis and With Antibiofilm ActivityZaenab AzzahraNo ratings yet
- Genetic Signatures From Adaptation of Bacteria To Lytic Phage Identify Potential Agents To Aid Phage-Killing of Multidrug-Resistant Acinetobacter BaumanniiDocument15 pagesGenetic Signatures From Adaptation of Bacteria To Lytic Phage Identify Potential Agents To Aid Phage-Killing of Multidrug-Resistant Acinetobacter BaumanniiGreater K. OYEJOBINo ratings yet
- Journal Homepage: - : IntroductionDocument7 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Potential Properties of Lactobacillus Plantarum F-10 As A Bio-Control Strategy For Wound InfectionsDocument14 pagesPotential Properties of Lactobacillus Plantarum F-10 As A Bio-Control Strategy For Wound InfectionsIgor BaltaNo ratings yet
- Fdocuments - in Biology Investigatory Project 561e79b91f5a0Document18 pagesFdocuments - in Biology Investigatory Project 561e79b91f5a0ASHOKNo ratings yet
- A Five-Day Course of Ivermectin May Reduce The DurationDocument3 pagesA Five-Day Course of Ivermectin May Reduce The DurationPaulinho CtsNo ratings yet
- Manejo y Control de Enfermedades RespiratoriasDocument13 pagesManejo y Control de Enfermedades RespiratoriasNicolás Ortiz RojasNo ratings yet
- EdiblevaccinesDocument11 pagesEdiblevaccinesAbduNo ratings yet
- Povidone Iodine: Useful For More Than Preoperative AntisepsisDocument4 pagesPovidone Iodine: Useful For More Than Preoperative AntisepsisNur AjiNo ratings yet
- Cells 12 02169Document24 pagesCells 12 02169Robert StryjakNo ratings yet
- Antifungal Resistance in Dermatology: Varadraj Pai, Ajantha Ganavalli, Naveen Narayanshetty KikkeriDocument8 pagesAntifungal Resistance in Dermatology: Varadraj Pai, Ajantha Ganavalli, Naveen Narayanshetty KikkerirehanaNo ratings yet
- Biofilm Formation by The Interaction of Fungi With Varoius BacteriaDocument10 pagesBiofilm Formation by The Interaction of Fungi With Varoius BacteriaLaborat MenurNo ratings yet
- Adrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077 PDFDocument5 pagesAdrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077 PDFfebrinaNo ratings yet
- Scope of Various Phytoconstituents in The Treatment of Multidrug Resistant Bacteria - A ReviewDocument6 pagesScope of Various Phytoconstituents in The Treatment of Multidrug Resistant Bacteria - A ReviewIJAR JOURNALNo ratings yet
- Effective Method To Remove Wound Bacteria Using Woundwand Bipolar RFA NusbaumDocument7 pagesEffective Method To Remove Wound Bacteria Using Woundwand Bipolar RFA NusbaumBob RiouxNo ratings yet
- Life 12 01240Document3 pagesLife 12 01240tauchragaNo ratings yet
- Fmicb 13 876058Document13 pagesFmicb 13 87605815041168No ratings yet
- Accepted Manuscript: 10.1016/j.ajo.2016.10.004Document22 pagesAccepted Manuscript: 10.1016/j.ajo.2016.10.004benefits35No ratings yet
- Revision Ch-Ii (Sexual Reproduction in Flowering Plants)Document11 pagesRevision Ch-Ii (Sexual Reproduction in Flowering Plants)Sahil GautamNo ratings yet
- GCLP Guidelines 2020 FinalDocument78 pagesGCLP Guidelines 2020 FinalGyanuNo ratings yet
- Dan BurischDocument103 pagesDan BurischDavid NowakowskiNo ratings yet
- EMBL-EBI Train OnlineDocument19 pagesEMBL-EBI Train OnlineThyagoNo ratings yet
- Bio-FIT Book EN PDFDocument256 pagesBio-FIT Book EN PDFCesar Augusto Colorado RamirezNo ratings yet
- Review: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2Document12 pagesReview: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2GREESTYNo ratings yet
- Types of Leukocytes and The PlateletsDocument25 pagesTypes of Leukocytes and The PlateletscarcuevajailamarieNo ratings yet
- GP Dorsal Pain Case June 2021Document5 pagesGP Dorsal Pain Case June 2021Lisa NurhasanahNo ratings yet
- VPH 83.43 Rev.1Document60 pagesVPH 83.43 Rev.1jubatus.libroNo ratings yet
- Handwriting Saying - OralDocument1 pageHandwriting Saying - OralEsther FernandezNo ratings yet
- EcoCRM A Recombinant CRM197 Carrier ProteinDocument1 pageEcoCRM A Recombinant CRM197 Carrier ProteinRamakrishnaNo ratings yet
- Activity Science 9 First QuarterDocument11 pagesActivity Science 9 First QuarterCristian PortugalNo ratings yet
- Cor 007 Module 17Document12 pagesCor 007 Module 17Camille ManlongatNo ratings yet
- General Biology - Chapter IDocument10 pagesGeneral Biology - Chapter IG.k. Vinnan Rao100% (2)
- Genetic History of Spain and PortugalDocument10 pagesGenetic History of Spain and PortugalaleytonsNo ratings yet
- RojiMolu - Effect of Growing Media On Seed Germination and Seedling Growth of Porang (Amorphophallus Muelleri Blume)Document10 pagesRojiMolu - Effect of Growing Media On Seed Germination and Seedling Growth of Porang (Amorphophallus Muelleri Blume)Hari HartantoNo ratings yet
- National Museum of Natural History: January 2008Document21 pagesNational Museum of Natural History: January 2008Martin Moller NielsenNo ratings yet
- Natural Regeneration: Don Minore Robert J. LaackeDocument26 pagesNatural Regeneration: Don Minore Robert J. LaackeAngela Marie AlducenteNo ratings yet
- Biology Photosynthesis CourseworkDocument7 pagesBiology Photosynthesis Courseworkbdg72wjj100% (2)
- Stan DigestiveDocument3 pagesStan Digestivejoanna carrenNo ratings yet
- Sample Weekly Planner 2Document9 pagesSample Weekly Planner 2api-662941487No ratings yet
- Pewarisan Sifat Warna Dan Tipe Biji Jagungmanado KuningDocument8 pagesPewarisan Sifat Warna Dan Tipe Biji Jagungmanado KuningZallNo ratings yet
- Shilajit A Panacea For CancerDocument9 pagesShilajit A Panacea For CancerRakeshKumarNo ratings yet
- RETINADocument4 pagesRETINAElizabeth Anne Loto100% (1)
- Grafting Eggplant Techniques PDFDocument6 pagesGrafting Eggplant Techniques PDFAjaya Kumar PaniNo ratings yet
- Introduction To The Study of BiochemistryDocument3 pagesIntroduction To The Study of BiochemistryMIA, Joy Beatrice R.No ratings yet
- 12 Fructose MetabolismDocument61 pages12 Fructose MetabolismAnand Veeranan100% (1)
- Pratibha 01 08 2020Document1 pagePratibha 01 08 2020R MedipalliNo ratings yet
- Descriptions of 16 Arthropods Pests On Potato in South Africa 16may2017Document44 pagesDescriptions of 16 Arthropods Pests On Potato in South Africa 16may2017vishal37256No ratings yet
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
Uploaded by
Danisa AzzahraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
An Asian Perspective On Povidone Iodine in Wound Healing: Review Paper
Uploaded by
Danisa AzzahraCopyright:
Available Formats
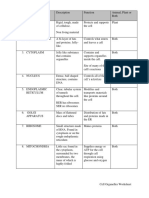
Review Paper
Dermatology 2017;233:223–233 Received: January 6, 2017
Accepted after revision: July 4, 2017
DOI: 10.1159/000479150
Published online: August 29, 2017
An Asian Perspective on Povidone Iodine
in Wound Healing
Paul Bigliardi a, b Stefan Langer c Jose Joven Cruz d Sang Wha Kim e
Harikrishna Nair f Gulapar Srisawasdi g
a
Clinical Research Unit for Skin, Allergy and Regeneration (CRUSAR), Institute of Medical Biology, Agency for
Science, Technology and Research, and b Division of Rheumatology, National University Hospital, National
University of Singapore Yong Loo Lin School of Medicine and University Medicine Cluster, National University
Health System, Singapore; c Department of Plastic, Esthetic and Special Hand Surgery, University Hospital Leipzig,
Leipzig, Germany; d Division of Plastic Surgery, University of the Philippines – College of Medicine and Philippine
General Hospital, Manila, Philippines; e Department of Plastic and Reconstructive Surgery, Seoul National University
Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea; f Wound Care Unit, Department
of Internal Medicine, Kuala Lumpur Hospital, Kuala Lumpur, Malaysia; g Siriraj Interdisciplinary Diabetic Lower
Extremity Care Team, Department of Rehabilitation Medicine, Faculty of Medicine, Siriraj Hospital,
Mahidol University, Bangkok, Thailand
Keywords in the clinical reality in humans. In this paper, we discuss the
Povidone iodine · Wound healing · Antiseptic · efficacy and safety of PVP-I and outline its place in wound
Antimicrobial agents healing in Asia, based on an appraisal of recent literature and
clinical practice across the region. © 2017 S. Karger AG, Basel
Abstract
Antiseptics, with a broader spectrum of antimicrobial effi-
cacy, lower risk of antibiotic resistance development, and Introduction
minimal collateral damage to host tissues, are important al-
ternatives to control the bioburden in wounds. Povidone io- Antiseptics are defined as agents used to inhibit or kill
dine (PVP-I), in use for several decades, has the broadest microorganisms present within a wound or on intact skin
spectrum of activity, a persistent antimicrobial effect, an [1, 2] and have long been used on wounds to prevent or
ability to penetrate biofilms, and a lack of acquired or cross- treat infections. Despite this, and in the absence of stan-
resistance. It demonstrates good skin tolerance and low cy- dardized practice and clinical study guidelines, there con-
totoxicity. However, some reports on PVP-I have raised con- tinues to be a great deal of debate and controversy on the
cerns over allergy, ineffective penetration, and toxic effects appropriate use of antiseptics.
on host cells. The majority of these concerns are based on in Iodine has been used as an antiseptic in the treatment
vitro or rodent wound studies with diverse study designs of wounds for more than a century [3], yet questions are
and outcomes; these results may not be directly applicable raised about the place of iodine-based agents in the man-
© 2017 S. Karger AG, Basel Assoc. Prof. Paul Bigliardi
Clinical Research Unit for Skin, Allergy and Regeneration (CRUSAR)
Institute of Medical Biology, 8A Biomedical Grove, #06-06 Immunos
E-Mail karger@karger.com
Singapore 138648 (Singapore)
www.karger.com/drm
E-Mail paul.bigliardi @ gmail.com
Povidone Iodine eradication of an established 7-day mixed Pseudomonas
Iodine has been extensively used for decades as an an- and Staphylococcus biofilm by using iodine-based dress-
tiseptic. PVP-I, the most well-established iodophor, is a ings. Furthermore, Hoekstra et al. [24] recently demon-
combination of molecular iodine and a polyvinylpyrrol- strated the efficacy of PVP-I in the presence of biofilms
idone surfactant/iodine complex which acts as a reservoir grown in a mixed culture of MRSA and Candida albicans,
of free iodine [17, 18]. The bactericidal component of even when diluted. However, these are studies conducted
PVP-I is the free iodine, the levels of which are dependent in an in vitro environment and do not conclusively prove
on the concentration of the PVP-I solution. the efficacy of PVP-I on biofilms.
The polyvinylpyrrolidone component of PVP-I deliv-
ers the iodine directly to the microorganism cell surface; Resistance
the free iodine penetrates into the cell wall and targets Increasing bacterial resistance to antibiotics is a major
proteins, nucleotides, and fatty acids, resulting in cell clinical and public health problem worldwide [9, 11, 26],
death [3, 18, 19]. The free iodine concentration increases and Asia is no exception [12, 27].
with increasing dilutions of PVP-I: dilution weakens the Bacterial resistance to topical antimicrobial agents,
iodine linkage to the carrier, resulting in an increase in such as vancomycin, mupirocin, fusidic acid, and genta-
free iodine in the solution [19]. It is believed that the con- micin, has been widely reported [11, 28, 29]. Bacterial re-
centration of free iodine contributes to the bactericidal sistance to chlorhexidine, quaternary ammonium salts,
activity of PVP-I; this is thought to explain the paradoxi- triclosan, and silver has also been reported [11, 22, 23].
cal increase in the antibacterial action of PVP-I with in- Furthermore, cross-resistance to other antibiotics and
creasing degree of dilution (0.1–1% solutions were re- antiseptics has been documented with chlorhexidine and
ported to be more rapidly bactericidal than the 10% solu- triclosan [30]. However, despite widespread and exten-
tion) [19]. sive use, no acquired or cross-resistance has ever been
reported for iodine [11, 22, 23, 30].
Efficacy: In vitro Studies
Spectrum of Activity Efficacy: In vivo Studies
PVP-I has demonstrated a broad spectrum of activity In vitro studies with PVP-I have reported contradic-
against Gram-positive (including methicillin-resistant tory results [6, 7, 31, 32]. The role of PVP-I in wound
Staphylococcus aureus [MRSA]) and Gram-negative bac- healing has also been investigated in animal studies, with
teria, fungi, viruses, protozoa, and bacterial spores in sev- varying results [17, 33]. Most of these animal studies were
eral studies [11, 17, 18, 20, 21]. PVP-I has also shown high published at least 2 decades ago, were conducted in bea-
bactericidal activity against test strains comprising caus- gles, rats, rabbits, and guinea pigs, and demonstrated that
ative organisms of nosocomial infections (MRSA, Serratia concentrations of up to 10% of PVP-I did not cause any
marcescens, Pseudomonas aeruginosa, Burkholderia cepa- inhibition in the granulation and epithelialization pro-
cia) after 30 s of exposure [22]. In addition, PVP-I proved cess [33]. Increased microcirculation is an important fea-
to be the only antiseptic without the development of cross- ture of the wound healing process. In experiments per-
resistance. A similar study confirmed the efficacy of PVP- formed on wounds in male SKH1-hr hairless mice, PVP-I
I against two Gram-negative bacteria (Xanthomonas products (PVP-I liposomal hydrogel) showed a positive
maltophilia and S. marcescens), including resistant strains effect on dermal wound healing and wound microcircu-
of both species; both sensitive and resistant strains of both lation [34]. In full thickness wounds in mice, Kjolseth et
species were killed within 20 s of exposure to PVP-I [23]. al. [35] also demonstrated earlier and complete neovas-
cularization with PVP-I versus other antiseptics.
Efficacy against Biofilms Some human studies conducted in varying settings
Wound biofilms – bacterial communities living within have established the efficacy of PVP-I in reducing the
a protective extracellular matrix – are often resistant to bacterial load in both acute and chronic wounds [8, 9, 17,
conventional treatment with antimicrobials and delay the 36–42]. Gravett et al. [36] and Stringer et al. [37] reported
wound healing process [20, 24]. The sustained efficacy of that PVP-I in patients prior to suturing lacerations re-
PVP-I in wound healing in the presence of biofilms has duces the incidence of wound infection. Similarly, post-
been described in several studies [20, 24, 25]. Hill et al. operative irrigation of surgical wounds with PVP-I re-
[25] used an in vitro biofilm model closely mimicking sulted in a decrease in wound infection rates in another
chronic wound biofilms and demonstrated the complete study [38]. Further, in a study of 294 pediatric surgical
Asian Perspective on PVP-I in Wound Dermatology 2017;233:223–233 225
Healing DOI: 10.1159/000479150
You might also like
- Cell Organelles WorksheetDocument8 pagesCell Organelles WorksheetJohn OsborneNo ratings yet
- An Asian Perspective On Povidone Iodine in Wound Healing: Review PaperDocument11 pagesAn Asian Perspective On Povidone Iodine in Wound Healing: Review PaperAsmita KurniaNo ratings yet
- Study On Emergence of MDR Pathogen and Its Microbiological StudyDocument9 pagesStudy On Emergence of MDR Pathogen and Its Microbiological StudyIJAR JOURNALNo ratings yet
- Locally Administered Probiotic, RCT-articleDocument7 pagesLocally Administered Probiotic, RCT-articleDebjyoti DebnathNo ratings yet
- Hoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFDocument9 pagesHoekstra Et al-2016Povidone-iodineointmentdemonstratesinvitroefcacyagainstbiofilmformationIWJ PDFMini Bekti NingsihNo ratings yet
- J Ajo 2020 03 018Document24 pagesJ Ajo 2020 03 018koas forensikNo ratings yet
- Acne CaseDocument5 pagesAcne CaseVeselina StefanovaNo ratings yet
- Gels 08 00163Document10 pagesGels 08 00163Andreea BarbuNo ratings yet
- (M299) RL3Document11 pages(M299) RL3Jessa Louise TurredaNo ratings yet
- A Study On Resistance Pattern of Bacteria Isolated From Diabetic and Non - Diabetic UlcersDocument7 pagesA Study On Resistance Pattern of Bacteria Isolated From Diabetic and Non - Diabetic UlcersBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Kanagalingam2015 PDFDocument10 pagesKanagalingam2015 PDFwatidinaNo ratings yet
- Comparative Evaluation of Locally Delivered.12Document7 pagesComparative Evaluation of Locally Delivered.12samanvi badriNo ratings yet
- RUSSO, Bud-Poplar-Extract-Embedded Chitosan Films AsDocument21 pagesRUSSO, Bud-Poplar-Extract-Embedded Chitosan Films AsANNE LOUISE FALCAO PASCOALNo ratings yet
- Fmicb 12 723834Document16 pagesFmicb 12 723834shalusinhaNo ratings yet
- 10 1016@j Mycmed 2018 08 002Document5 pages10 1016@j Mycmed 2018 08 002Feni SyawelmiNo ratings yet
- A Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyDocument15 pagesA Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyIJAR JOURNALNo ratings yet
- Prospective, Randomized Clinical Trial ofDocument10 pagesProspective, Randomized Clinical Trial ofFarhan RezaNo ratings yet
- Cuppa Wao Journal ProofsDocument22 pagesCuppa Wao Journal ProofsFajar SetiawanNo ratings yet
- 1 s2.0 S0899900715003871 MainDocument7 pages1 s2.0 S0899900715003871 MainThảo Bùi ThanhNo ratings yet
- DR Vidya SagarDocument7 pagesDR Vidya SagarAnil KumarNo ratings yet
- Promote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportDocument4 pagesPromote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportShira michaelNo ratings yet
- 1 s2.0 S092485792030234X MainDocument11 pages1 s2.0 S092485792030234X MainPedro GouveiaNo ratings yet
- Jurnal EED 3Document10 pagesJurnal EED 3Garsa GarnolNo ratings yet
- International Journal of Antimicrobial AgentsDocument11 pagesInternational Journal of Antimicrobial AgentsRita SukitaNo ratings yet
- Understanding Antimicrobial Susceptibility Profile of Finegoldia Magna An Insight To An Untrodden PathDocument5 pagesUnderstanding Antimicrobial Susceptibility Profile of Finegoldia Magna An Insight To An Untrodden Pathd4rkgr455No ratings yet
- A Study On The Healing Effect of Honey On Infected Open Fracture WoundsDocument3 pagesA Study On The Healing Effect of Honey On Infected Open Fracture WoundsMuhammad AlamzebNo ratings yet
- (M299) RL2Document11 pages(M299) RL2Jessa Louise TurredaNo ratings yet
- Designing A Multi-Epitope Vaccine Against Shigella Dysenteriae Using Immuno-Informatics ApproachDocument14 pagesDesigning A Multi-Epitope Vaccine Against Shigella Dysenteriae Using Immuno-Informatics ApproachDr. Sunil RaiNo ratings yet
- Ditorial The Challenge of Controlling Infectious Keratitis: Tom - Lietman@ Ucsf - EduDocument2 pagesDitorial The Challenge of Controlling Infectious Keratitis: Tom - Lietman@ Ucsf - Eduwawan 88No ratings yet
- 10 1111@iwj 13463Document7 pages10 1111@iwj 13463burhanNo ratings yet
- Nitric Oxide Mediated Staphylococcus Aureus Pathogenesis and Protective Role of Nanoconjugated VancomycinDocument8 pagesNitric Oxide Mediated Staphylococcus Aureus Pathogenesis and Protective Role of Nanoconjugated Vancomycinlolamusic90No ratings yet
- Case Study: Bronchopneumoniae With Melioidosis Infection in A Paediatric PatientDocument8 pagesCase Study: Bronchopneumoniae With Melioidosis Infection in A Paediatric PatientlolllllNo ratings yet
- 2020 The Potential of Probiotics For Treating Acne Vulgaris - A Review of Literature On Acne and MicrobiotDocument6 pages2020 The Potential of Probiotics For Treating Acne Vulgaris - A Review of Literature On Acne and MicrobiotJeslyn TengkawanNo ratings yet
- Engineering Probiotics For Therapeutic ApplicationsDocument9 pagesEngineering Probiotics For Therapeutic ApplicationsElinaNo ratings yet
- The Use of Antimicrobial Peptides in Ophthalmology: An Experimental Study in Corneal Preservation and The Management of Bacterial KeratitisDocument30 pagesThe Use of Antimicrobial Peptides in Ophthalmology: An Experimental Study in Corneal Preservation and The Management of Bacterial KeratitisAgam ThebadboysNo ratings yet
- Journal of Periodontology - 2021 - Lu - Effect of Adjunctive Systemic Antibiotics On Microbial Populations Compared WithDocument14 pagesJournal of Periodontology - 2021 - Lu - Effect of Adjunctive Systemic Antibiotics On Microbial Populations Compared WithShakeel AhmedNo ratings yet
- Fmicb 08 00659Document9 pagesFmicb 08 00659Helena VenanteNo ratings yet
- Antibiotic in CDDocument11 pagesAntibiotic in CDYaseerNo ratings yet
- Development of Polyurethane Foam Dressing Containing Silver and Asiaticoside For Healing of Dermal WoundDocument15 pagesDevelopment of Polyurethane Foam Dressing Containing Silver and Asiaticoside For Healing of Dermal WoundritaNo ratings yet
- Adrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077Document5 pagesAdrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077Ous linosNo ratings yet
- Current Anti-Biofilm Strategies and Potential of Antioxidants in Biofilm ControlDocument10 pagesCurrent Anti-Biofilm Strategies and Potential of Antioxidants in Biofilm ControlBeshoy RafatNo ratings yet
- Chenodeoxycholic Acid-Amikacin Combination Enhances ERradication of StaphyDocument17 pagesChenodeoxycholic Acid-Amikacin Combination Enhances ERradication of StaphyAlex HernandezNo ratings yet
- Novel Bacteriophage Specific Against Staphylococcus Epidermidis and With Antibiofilm ActivityDocument11 pagesNovel Bacteriophage Specific Against Staphylococcus Epidermidis and With Antibiofilm ActivityZaenab AzzahraNo ratings yet
- Genetic Signatures From Adaptation of Bacteria To Lytic Phage Identify Potential Agents To Aid Phage-Killing of Multidrug-Resistant Acinetobacter BaumanniiDocument15 pagesGenetic Signatures From Adaptation of Bacteria To Lytic Phage Identify Potential Agents To Aid Phage-Killing of Multidrug-Resistant Acinetobacter BaumanniiGreater K. OYEJOBINo ratings yet
- Journal Homepage: - : IntroductionDocument7 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Potential Properties of Lactobacillus Plantarum F-10 As A Bio-Control Strategy For Wound InfectionsDocument14 pagesPotential Properties of Lactobacillus Plantarum F-10 As A Bio-Control Strategy For Wound InfectionsIgor BaltaNo ratings yet
- Fdocuments - in Biology Investigatory Project 561e79b91f5a0Document18 pagesFdocuments - in Biology Investigatory Project 561e79b91f5a0ASHOKNo ratings yet
- A Five-Day Course of Ivermectin May Reduce The DurationDocument3 pagesA Five-Day Course of Ivermectin May Reduce The DurationPaulinho CtsNo ratings yet
- Manejo y Control de Enfermedades RespiratoriasDocument13 pagesManejo y Control de Enfermedades RespiratoriasNicolás Ortiz RojasNo ratings yet
- EdiblevaccinesDocument11 pagesEdiblevaccinesAbduNo ratings yet
- Povidone Iodine: Useful For More Than Preoperative AntisepsisDocument4 pagesPovidone Iodine: Useful For More Than Preoperative AntisepsisNur AjiNo ratings yet
- Cells 12 02169Document24 pagesCells 12 02169Robert StryjakNo ratings yet
- Antifungal Resistance in Dermatology: Varadraj Pai, Ajantha Ganavalli, Naveen Narayanshetty KikkeriDocument8 pagesAntifungal Resistance in Dermatology: Varadraj Pai, Ajantha Ganavalli, Naveen Narayanshetty KikkerirehanaNo ratings yet
- Biofilm Formation by The Interaction of Fungi With Varoius BacteriaDocument10 pagesBiofilm Formation by The Interaction of Fungi With Varoius BacteriaLaborat MenurNo ratings yet
- Adrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077 PDFDocument5 pagesAdrizain 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012077 PDFfebrinaNo ratings yet
- Scope of Various Phytoconstituents in The Treatment of Multidrug Resistant Bacteria - A ReviewDocument6 pagesScope of Various Phytoconstituents in The Treatment of Multidrug Resistant Bacteria - A ReviewIJAR JOURNALNo ratings yet
- Effective Method To Remove Wound Bacteria Using Woundwand Bipolar RFA NusbaumDocument7 pagesEffective Method To Remove Wound Bacteria Using Woundwand Bipolar RFA NusbaumBob RiouxNo ratings yet
- Life 12 01240Document3 pagesLife 12 01240tauchragaNo ratings yet
- Fmicb 13 876058Document13 pagesFmicb 13 87605815041168No ratings yet
- Accepted Manuscript: 10.1016/j.ajo.2016.10.004Document22 pagesAccepted Manuscript: 10.1016/j.ajo.2016.10.004benefits35No ratings yet
- Revision Ch-Ii (Sexual Reproduction in Flowering Plants)Document11 pagesRevision Ch-Ii (Sexual Reproduction in Flowering Plants)Sahil GautamNo ratings yet
- GCLP Guidelines 2020 FinalDocument78 pagesGCLP Guidelines 2020 FinalGyanuNo ratings yet
- Dan BurischDocument103 pagesDan BurischDavid NowakowskiNo ratings yet
- EMBL-EBI Train OnlineDocument19 pagesEMBL-EBI Train OnlineThyagoNo ratings yet
- Bio-FIT Book EN PDFDocument256 pagesBio-FIT Book EN PDFCesar Augusto Colorado RamirezNo ratings yet
- Review: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2Document12 pagesReview: Zebrafish (Danio Rerio) Sebagai Model Obesitas Dan Diabetes Melitus Tipe 2GREESTYNo ratings yet
- Types of Leukocytes and The PlateletsDocument25 pagesTypes of Leukocytes and The PlateletscarcuevajailamarieNo ratings yet
- GP Dorsal Pain Case June 2021Document5 pagesGP Dorsal Pain Case June 2021Lisa NurhasanahNo ratings yet
- VPH 83.43 Rev.1Document60 pagesVPH 83.43 Rev.1jubatus.libroNo ratings yet
- Handwriting Saying - OralDocument1 pageHandwriting Saying - OralEsther FernandezNo ratings yet
- EcoCRM A Recombinant CRM197 Carrier ProteinDocument1 pageEcoCRM A Recombinant CRM197 Carrier ProteinRamakrishnaNo ratings yet
- Activity Science 9 First QuarterDocument11 pagesActivity Science 9 First QuarterCristian PortugalNo ratings yet
- Cor 007 Module 17Document12 pagesCor 007 Module 17Camille ManlongatNo ratings yet
- General Biology - Chapter IDocument10 pagesGeneral Biology - Chapter IG.k. Vinnan Rao100% (2)
- Genetic History of Spain and PortugalDocument10 pagesGenetic History of Spain and PortugalaleytonsNo ratings yet
- RojiMolu - Effect of Growing Media On Seed Germination and Seedling Growth of Porang (Amorphophallus Muelleri Blume)Document10 pagesRojiMolu - Effect of Growing Media On Seed Germination and Seedling Growth of Porang (Amorphophallus Muelleri Blume)Hari HartantoNo ratings yet
- National Museum of Natural History: January 2008Document21 pagesNational Museum of Natural History: January 2008Martin Moller NielsenNo ratings yet
- Natural Regeneration: Don Minore Robert J. LaackeDocument26 pagesNatural Regeneration: Don Minore Robert J. LaackeAngela Marie AlducenteNo ratings yet
- Biology Photosynthesis CourseworkDocument7 pagesBiology Photosynthesis Courseworkbdg72wjj100% (2)
- Stan DigestiveDocument3 pagesStan Digestivejoanna carrenNo ratings yet
- Sample Weekly Planner 2Document9 pagesSample Weekly Planner 2api-662941487No ratings yet
- Pewarisan Sifat Warna Dan Tipe Biji Jagungmanado KuningDocument8 pagesPewarisan Sifat Warna Dan Tipe Biji Jagungmanado KuningZallNo ratings yet
- Shilajit A Panacea For CancerDocument9 pagesShilajit A Panacea For CancerRakeshKumarNo ratings yet
- RETINADocument4 pagesRETINAElizabeth Anne Loto100% (1)
- Grafting Eggplant Techniques PDFDocument6 pagesGrafting Eggplant Techniques PDFAjaya Kumar PaniNo ratings yet
- Introduction To The Study of BiochemistryDocument3 pagesIntroduction To The Study of BiochemistryMIA, Joy Beatrice R.No ratings yet
- 12 Fructose MetabolismDocument61 pages12 Fructose MetabolismAnand Veeranan100% (1)
- Pratibha 01 08 2020Document1 pagePratibha 01 08 2020R MedipalliNo ratings yet
- Descriptions of 16 Arthropods Pests On Potato in South Africa 16may2017Document44 pagesDescriptions of 16 Arthropods Pests On Potato in South Africa 16may2017vishal37256No ratings yet