Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
55 viewsAssessment Gastro Nursing
Assessment Gastro Nursing
Uploaded by
LienyPerasThe document discusses the gastrointestinal system and common gastrointestinal disorders. It covers topics such as abdominal pain, gas, nausea, vomiting, changes in bowel habits, and stool characteristics. The physical examination of the gastrointestinal system includes inspection of the mouth, gums, tongue, lips and abdomen as well as auscultation of bowel sounds.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Nursing PharmacologyDocument13 pagesNursing Pharmacologyjeshema100% (4)
- 6-7 - Medical Nursing - GIS DisordersDocument108 pages6-7 - Medical Nursing - GIS DisordersmichaelNo ratings yet
- Diseases of The OesophagusDocument6 pagesDiseases of The OesophagusMohamed AlsaabNo ratings yet
- hs320 W11 DigestiveSystemDisordersDocument41 pageshs320 W11 DigestiveSystemDisordersjoseyalm2323No ratings yet
- Bowel EliminationDocument123 pagesBowel EliminationSharon LawrenceNo ratings yet
- 22 Manuscript Intestinal ObstructionDocument8 pages22 Manuscript Intestinal Obstructionkint manlangitNo ratings yet
- The GI System Is Composed of Two General Parts Gi TractDocument14 pagesThe GI System Is Composed of Two General Parts Gi TractRexson Alcantara DalanginNo ratings yet
- NSG 306-1Document56 pagesNSG 306-1Anifowose samsonNo ratings yet
- Bowel EliminationDocument59 pagesBowel EliminationRekha DehariyaNo ratings yet
- 1 Gastrointestinal System DisordersDocument14 pages1 Gastrointestinal System DisordersAnna Sofia Reyes100% (1)
- GIT DisordersDocument171 pagesGIT DisordersKatrina PonceNo ratings yet
- What Is Abdominal Pain? TreatmentDocument2 pagesWhat Is Abdominal Pain? TreatmentErick YohanesNo ratings yet
- Chapter 28 Child With A Gastrointestinal ConditionDocument85 pagesChapter 28 Child With A Gastrointestinal Conditionsey_scottNo ratings yet
- NCM 116 Gep MidtermDocument20 pagesNCM 116 Gep MidtermKM PanganibanNo ratings yet
- CancerDocument30 pagesCancerAbhirami BabuNo ratings yet
- Approach To The Child With Nausea and Vomiting: by DR - Ryan Al - GhanemiDocument50 pagesApproach To The Child With Nausea and Vomiting: by DR - Ryan Al - GhanemiyusufharkianNo ratings yet
- Pengkajian Sistem GastrointestinalDocument38 pagesPengkajian Sistem GastrointestinalNabila FatharaniNo ratings yet
- Disorder and Diseases of Digestive SystemDocument8 pagesDisorder and Diseases of Digestive SystemCristina AnganganNo ratings yet
- What Are The Signs of Bleeding in The Digestive Tract?Document6 pagesWhat Are The Signs of Bleeding in The Digestive Tract?draganNo ratings yet
- Ed-Abdominal PainDocument2 pagesEd-Abdominal PainMuhammad Arif RahmanNo ratings yet
- Pemicu 5 GITDocument52 pagesPemicu 5 GITMudita DewiNo ratings yet
- INTESTINEDocument98 pagesINTESTINEDeepika LingamNo ratings yet
- Non-Inflammatory Bowel DisordersDocument33 pagesNon-Inflammatory Bowel Disorderssho bartNo ratings yet
- NCP 1Document3 pagesNCP 1Mary Antonette Adriano EnriquezNo ratings yet
- Assessment of Digestive and Intestinal Tracts Disorders HAMDALLAHDocument141 pagesAssessment of Digestive and Intestinal Tracts Disorders HAMDALLAHMAYHAMDALLAHNo ratings yet
- Peptic Ulcer FinalDocument6 pagesPeptic Ulcer FinalLarra MoslaresNo ratings yet
- Pumpkin Spice and Everything NiceDocument7 pagesPumpkin Spice and Everything Niceotum.shayneNo ratings yet
- Pathology Gis: Aanisah F 14.103Document47 pagesPathology Gis: Aanisah F 14.103rftdlsNo ratings yet
- Bowel Elimination and Urinary Incontinence ProblemsDocument5 pagesBowel Elimination and Urinary Incontinence ProblemsMegan Rose MontillaNo ratings yet
- Concept of Elimination-1Document39 pagesConcept of Elimination-1kalimulallah4No ratings yet
- Nursing Care Plan Nausea & VomitingDocument3 pagesNursing Care Plan Nausea & Vomitingderic87% (47)
- "Gosh, Mrs. Doubtfire You Look Pale": Fire" in Television at The Emergency Departement You Worked ForDocument84 pages"Gosh, Mrs. Doubtfire You Look Pale": Fire" in Television at The Emergency Departement You Worked ForAngela Kristiana IntanNo ratings yet
- Gastro-Oesophageal Reflux Disease (GORD) : Anish DhakalDocument31 pagesGastro-Oesophageal Reflux Disease (GORD) : Anish DhakalnrauliaprtwNo ratings yet
- Management of Client With Gastrointestinal DisordersDocument33 pagesManagement of Client With Gastrointestinal DisordersKelly TayagNo ratings yet
- Intestinal Obstruction 4Document25 pagesIntestinal Obstruction 4Muvenn KannanNo ratings yet
- Assessment of The AbdomenDocument7 pagesAssessment of The AbdomenS StPierreNo ratings yet
- Department of Surgery: Case Presentation Intestinal ObstructionDocument46 pagesDepartment of Surgery: Case Presentation Intestinal Obstructionhadil ayeshNo ratings yet
- Common Causes of PUD: Duodenal Ulcer: A Peptic Ulcer of TheDocument8 pagesCommon Causes of PUD: Duodenal Ulcer: A Peptic Ulcer of Thestudy mailNo ratings yet
- Irritable Bowel SyndromeDocument5 pagesIrritable Bowel Syndromedrnareshkumar32810% (1)
- C. Disorders of The Lowel BowelDocument69 pagesC. Disorders of The Lowel BowelJmarie Brillantes PopiocoNo ratings yet
- Presenting Problems in Gastrointestinal Disease:: DysphagiaDocument9 pagesPresenting Problems in Gastrointestinal Disease:: DysphagiaMohamed AlsaabNo ratings yet
- Nursing Management of Git Problems: Oral and Esophageal DisordersDocument18 pagesNursing Management of Git Problems: Oral and Esophageal Disorderslcpot_se7en7505100% (2)
- Acute Abdomen, Nyeri Akut AbdomenDocument35 pagesAcute Abdomen, Nyeri Akut AbdomenYanuar Yudha SudrajatNo ratings yet
- Chronic Diarrhea-HTKDocument63 pagesChronic Diarrhea-HTKcerenblgstrNo ratings yet
- Acute AbdomenDocument21 pagesAcute AbdomenMillicent AwuzieNo ratings yet
- GastritisDocument18 pagesGastritisleian28No ratings yet
- Anorexia: Basic InformationDocument34 pagesAnorexia: Basic InformationcarlosNo ratings yet
- Ms Prelim NewDocument12 pagesMs Prelim NewJane LaquihonNo ratings yet
- Hiatal Hernia FactsheetDocument6 pagesHiatal Hernia FactsheetHoney Bee S. PlatolonNo ratings yet
- Elimination: Dumip-Ig, Maricel Gregorio, Kristine Milagrosa, Nina JesusaDocument30 pagesElimination: Dumip-Ig, Maricel Gregorio, Kristine Milagrosa, Nina JesusaKristine Las GregorioNo ratings yet
- NcpsDocument10 pagesNcpskotoirNo ratings yet
- 62 DiarrheaChronic MGHG MIMG MFM 20161229Document10 pages62 DiarrheaChronic MGHG MIMG MFM 20161229Wei HangNo ratings yet
- A Simple Guide to Gastritis and Related ConditionsFrom EverandA Simple Guide to Gastritis and Related ConditionsRating: 4.5 out of 5 stars4.5/5 (3)
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Perfect Lpr Diet Cookbook:The Complete Nutrition Guide To Lowering Stomach Acid Naturally And Easing Gastritis With Delectable and Nourishing RecipesFrom EverandThe Perfect Lpr Diet Cookbook:The Complete Nutrition Guide To Lowering Stomach Acid Naturally And Easing Gastritis With Delectable and Nourishing RecipesNo ratings yet
- Constipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationFrom EverandConstipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- Medical Surgical Nursing 2 Denn Hill RiorosoDocument10 pagesMedical Surgical Nursing 2 Denn Hill RiorosoLienyPerasNo ratings yet
- Muskuloskeletal DisordersDocument15 pagesMuskuloskeletal DisordersLienyPerasNo ratings yet
- Drugs For Gastrointestinal SystemDocument6 pagesDrugs For Gastrointestinal SystemLienyPerasNo ratings yet
- Nursing REVIEWER 2Document11 pagesNursing REVIEWER 2LienyPerasNo ratings yet
- Schizophrenia and Other Psychotic Disorders Clinical Practice GuidelineDocument7 pagesSchizophrenia and Other Psychotic Disorders Clinical Practice GuidelineDani NugrohoNo ratings yet
- CrampsDocument14 pagesCrampsJen PassilanNo ratings yet
- EmpiemaDocument19 pagesEmpiemaArrol Iswahyudi100% (1)
- Document PDFDocument18 pagesDocument PDFlilisNo ratings yet
- PDEV Notes For Periodical ExamDocument7 pagesPDEV Notes For Periodical ExamErjie GerasmioNo ratings yet
- Active IngredientDocument2 pagesActive IngredientNeri Jane JablaNo ratings yet
- What Is MDocument2 pagesWhat Is MkasjdkasNo ratings yet
- Cutaneous Manifestation of HivDocument36 pagesCutaneous Manifestation of Hivyunita hapsariNo ratings yet
- Diabetes and RamadanDocument4 pagesDiabetes and Ramadan80082583No ratings yet
- Post Op Alveoloplasty - RRR - 1 PDFDocument1 pagePost Op Alveoloplasty - RRR - 1 PDFAndykaYayanSetiawanNo ratings yet
- Global Health Current Issues Future Trends and ForDocument8 pagesGlobal Health Current Issues Future Trends and ForMsMhey PalattaoNo ratings yet
- Junk FoodDocument17 pagesJunk FoodCorey Page0% (1)
- Shave Your Balls and 100 Other Things Your Mother Should Have Told YouDocument112 pagesShave Your Balls and 100 Other Things Your Mother Should Have Told Youdelski14No ratings yet
- Surgery Short Case - HydroceleDocument1 pageSurgery Short Case - HydroceleHeroNo ratings yet
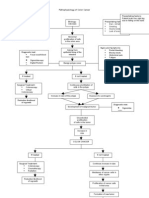
- Pa Tho Physiology of Colon CancerDocument2 pagesPa Tho Physiology of Colon Cancernick_nock0893% (14)
- EMREE Q BANK - Edited and Revised Part 1Document101 pagesEMREE Q BANK - Edited and Revised Part 1Sandra Abboud100% (1)
- Longevity - Wikipedia, The Free EncyclopediaDocument11 pagesLongevity - Wikipedia, The Free EncyclopediaJames DriscollNo ratings yet
- Cholera in NepalDocument57 pagesCholera in NepalBinayaNo ratings yet
- AttentionDocument6 pagesAttentionSneha BhattNo ratings yet
- Myasthenia GravisDocument3 pagesMyasthenia Gravisapi-3822433100% (2)
- Endotracheal Intubation & ER Board Exam QuestionsDocument33 pagesEndotracheal Intubation & ER Board Exam QuestionsJo-Anne Karen Serdeña0% (1)
- Bio 9th 2nd Chapter Biological MethodDocument7 pagesBio 9th 2nd Chapter Biological Methodhamza0% (1)
- Flexi Medical Plan BrochureDocument28 pagesFlexi Medical Plan BrochurewoodksdNo ratings yet
- Diabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaDocument6 pagesDiabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- AgnosiaDocument15 pagesAgnosiaMUHAMMAD BILALNo ratings yet
- Ewing Sarcoma PDFDocument2 pagesEwing Sarcoma PDFShellyNo ratings yet
- Health - I'm SickDocument1 pageHealth - I'm SickKaled LamouriNo ratings yet
- Kode Diagnosis ElinkDocument1 pageKode Diagnosis ElinksandraldiraNo ratings yet
- Pediatric Ist SeminarDocument21 pagesPediatric Ist SeminarAsha jiluNo ratings yet
Assessment Gastro Nursing
Assessment Gastro Nursing
Uploaded by
LienyPeras0 ratings0% found this document useful (0 votes)
55 views14 pagesThe document discusses the gastrointestinal system and common gastrointestinal disorders. It covers topics such as abdominal pain, gas, nausea, vomiting, changes in bowel habits, and stool characteristics. The physical examination of the gastrointestinal system includes inspection of the mouth, gums, tongue, lips and abdomen as well as auscultation of bowel sounds.
Original Description:
Original Title
assessment gastro nursing
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses the gastrointestinal system and common gastrointestinal disorders. It covers topics such as abdominal pain, gas, nausea, vomiting, changes in bowel habits, and stool characteristics. The physical examination of the gastrointestinal system includes inspection of the mouth, gums, tongue, lips and abdomen as well as auscultation of bowel sounds.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
55 views14 pagesAssessment Gastro Nursing
Assessment Gastro Nursing
Uploaded by
LienyPerasThe document discusses the gastrointestinal system and common gastrointestinal disorders. It covers topics such as abdominal pain, gas, nausea, vomiting, changes in bowel habits, and stool characteristics. The physical examination of the gastrointestinal system includes inspection of the mouth, gums, tongue, lips and abdomen as well as auscultation of bowel sounds.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 14
digestion longer than proteins or
Gastrointestinal System carbohydrates.
and Disorders Intestinal Gas
o The accumulation of gas in the GI tract
Health History may result in belching or flatulence
o Patients often complain of bloating,
Information about: distention, or feeling “full of gas” with
• abdominal pain excessive flatulence as a symptom of
• dyspepsia food intolerance or gallbladder disease
• gas Nausea and Vomiting
• nausea and vomiting
• diarrhea o Nausea is a vague, uncomfortable
• constipation sensation of sickness or “queasiness”
• fecal incontinence that may or may not be followed by
• jaundice vomiting.
• previous GI disease o It can be triggered by odors, activity,
medications, or food intake
o The causes of nausea and vomiting are
many; they may result from:
Common Symptoms • visceral afferent stimulation
Pain • CNS disorders
• irritation of the chemoreceptor
o Pain can be a major symptom of GI trigger zone from radiation
disease therapy, systemic disorders,
o The character, duration, pattern, and endogenous and
frequency, location, distribution of exogenous toxins, which may
referred abdominal pain, and time of include specific classes of drugs
the pain vary greatly depending on the o Distention of the duodenum or upper
underlying cause. intestinal tract is a common cause of
nausea
Dyspepsia
o Vomiting is a physiologic protective
o upper abdominal discomfort associated response that limits the effects of
with eating noxious agents by emptying the
o the most common symptom of patients stomach contents and sections of the
with GI dysfunction small intestine
o symptoms such as:
• pain
• discomfort
Change in Bowel Habits and Stool
• fullness
• bloating Characteristics
• early satiety o Changes in bowel habits may signal
• belching colonic dysfunction or disease
• heartburn o Diarrhea, an abnormal increase in the
• regurgitation frequency and liquidity of the stool or in
o fatty foods cause the most discomfort daily stool weight or volume, commonly
because they remain in the stomach for occurs when the contents move so
rapidly through the intestine and colon Denture Care
that there is inadequate time for the GI
secretions and oral contents to be • Brush dentures twice a day.
absorbed • Clean well under partial dentures,
o Constipation—a decrease in the where food particles tend to get caught.
frequency of stool, or stools that are • Consume nonsticky foods that have
hard, dry, and of smaller volume than been cut into small pieces; chew slowly.
typical—may be associated with anal • Remove dentures at night, and soak
discomfort and rectal bleeding them in water or a denture product.
o Stool is normally light to dark brown • Never put dentures in hot water,
o If blood is shed in sufficient quantities because they may warp.
into the upper GI tract, it produces a • Rinse mouth with warm salt water in
tarry-black color (melena), the morning, after meals, and at
o blood entering the lower portion of the bedtime.
GI tract or passing rapidly through it will • See dentist regularly to assess and
appear bright or dark red adjust fit.
➢ Lower rectal or anal bleeding is
suspected if there is streaking Physical Assessment
of blood on the surface of the o The physical examination includes:
stool or if blood is noted on • assessment of the mouth
toilet tissue
• abdomen and rectum
Other common abnormalities in stool ▪ requires a good source
characteristics described by the patient may of light
include: • full exposure of the abdomen
▪ warm hands with short
• Bulky, greasy, foamy stools that are foul ▪ fingernails, and a
in odor and may or may not float comfortable and
• Light-gray or clay-colored stool, caused relaxed patient with an
by a decrease or absence of conjugated empty bladder
bilirubin
• Stool with mucus threads or pus that Oral Cavity Inspection and Palpation
may be visible on gross inspection of • Dentures should be removed to allow
the stool good visualization of the entire oral
• Small, dry, rock-hard masses cavity
occasionally streaked with blood
• Loose, watery stool that may or may Lips
not be streaked with blood
• The examination begins with inspection
of the lips for:
• Moisture
• Hydration
• Color
• texture,
• symmetry
• the presence of ulcerations or
fissures.
Gums • striae
o Lesions are of particular importance,
o The gums are inspected for:
because GI diseases often produce skin
• inflammation changes
• bleeding o The contour and symmetry of the
• retraction abdomen are noted, and any localized
• discoloration. bulging, distention, or peristaltic waves
o The odor of the breath is also noted. are identified
o The hard palate is examined for color o Expected contours of the anterior
and shape abdominal wall can be described as:
Tongue • Flat
• Rounded
o The patient is instructed to protrude • Scaphoid
the tongue and move it laterally. This
provides the examiner with an Auscultation
opportunity to estimate the tongue’s o always precedes percussion and
size as well as its symmetry and palpation, always precedes percussion
strength and palpation
o Any lesions of the mucosa or any o Auscultation is used to determine the:
abnormalities involving the frenulum or
• Character
superficial veins on the undersurface of
• Location
the tongue are assessed for location,
• frequency of bowel sounds
size, color, and pain.
• to identify vascular sounds
➢ This is a common area for oral
o Bowel sounds are assessed using the
cancer, which presents as a
diaphragm of the stethoscope for soft
white or red plaque, lesions,
clicks and gurgling sounds
ulcers, or nodules
o The frequency and character of the
sounds are usually heard as clicks and
gurgles that occur irregularly and range
Abdominal Inspection, Auscultation, from 5 to 30 per minute
Percussion, and Palpation ➢ The terms normal (sounds
heard about every 5 to 20
o The patient lies supine with knees seconds)
flexed slightly for inspection, ➢ hypoactive (one or two sounds
auscultation, percussion, and palpation in 2 minutes)
of the abdomen ➢ hyperactive (5 to 6 sounds
o The four-quadrant method involves the heard in less than 30 seconds)
use of an imaginary line drawn ➢ absent (no sounds in 3 to 5
Inspection minutes)
o Using the bell of the stethoscope, any
• noting skin changes bruits in the aortic, renal, iliac, and
• nodules femoral arteries are noted
• lesions o Friction rubs are high pitched and can
• scarring be heard over the liver and spleen
• discolorations during respiration.
• inflammation o Borborygmi (“stomach growling”) is
• bruising heard as a loud prolonged gurgle.
Percussion o External examination includes
inspection for:
o used to assess the size and density of
• Lumps
the abdominal organs and to detect the
• Rashes
presence of air-filled, fluid-filled, or
• Inflammation
solid masses
• Excoriation
o Percussion is used either independently
or concurrently with palpation because • Tears
it can validate palpation findings • Scars
o All quadrants are percussed for overall: • pilonidal dimpling
• tympani sound that results • tufts of hair at the pilonidal
from the presence of air in the area.
stomach and small intestines o Internal examination is performed with
• Dullness is heard over organs a gloved lubricated index finger inserted
and solid masses into the anal canal while the patient
o The use of light palpation is appropriate bears down
for identifying areas of tenderness or
muscular resistance
o deep palpation is used to identify Diagnostic Evaluation
masses
o Testing for rebound tenderness is not General nursing interventions for the patient
performed by many examiners because who is undergoing a GI diagnostic evaluation
it can cause severe pain include:
Percussion • Establishing the nursing diagnosis
• Providing needed information about the
o light percussion is used instead to test and the activities required of the
produce a mild localized response when patient
peritoneal irritation is present
• Providing instructions about
postprocedure care and activity
restrictions
Rectal Inspection and Palpation • Providing health information and
o The final part of the examination is procedural education to patients and
evaluation of the terminal portions of significant others
the GI tract, the: • Helping the patient cope with
• Rectum discomfort and alleviating anxiety
• perianal region Informing the primary provider of
• anus known medical conditions or abnormal
o Gloves, water-soluble lubrication, a laboratory values that may affect the
penlight, and drapes are necessary tools procedure
for the evaluation • Assessing for adequate hydration
o For women, the rectal examination may before, during, and immediately after
be part of the gynecologic examination the procedure, and providing education
o Positions for the rectal examination about maintenance of hydration
include knee-chest, left lateral with hips
and knees flexed, or standing with hips
flexed and upper body supported by the
examination table
Serum Laboratory Studies • nitrogen
• Clostridium difficile
o Initial diagnostic tests begin with serum
• fecal leukocytes
laboratory studies, including but not
• calculation of stool osmolar gas
limited to:
parasites
• CBC
• pathogens
• complete metabolic panel
• food residues
• prothrombin time/partial
• other substance
thromboplastin time
• require laboratory evaluation
• triglycerides
o the quantitative 24- to 72-hour
• liver function tests
collections must be kept refrigerated
• amylase
until transported to the laboratory.
• lipase
o Fecal occult blood testing (FOBT) is one
o possibly, more specific studies may be
of the most commonly performed stool
indicated, such as:
tests.
• carcinoembryonic antigen (CEA) ➢ FOBT can be performed at the
• cancer antigen (CA) 19–9, bedside, in the laboratory, or at
• alpha-fetoprotein home
▪ which are sensitive and ➢ However, it should not be
specific for colorectal performed when there is
and hepatocellular hemorrhoidal bleeding.
carcinomas, ➢ A small amount of the specimen
respectively is applied to the guaiac-
o CEA is a protein that is normally not impregnated paper slide.
detected in the blood of a healthy o Fecal immunologic tests (FIT) use
person; therefore, when detected it monoclonal or polyclonal antibodies to
indicates that cancer is present, detect the globin protein in human
although not what type of cancer is hemoglobin
present. ➢ Dietary restrictions are not
o CA 19-9 levels are elevated in most required prior to submission of
patients with advanced pancreatic the stool specimen
cancer, but they may also be elevated in ➢ Hematoporphyrin assays detect
other conditions such as colorectal, the broadest range of blood
stomach, and bile duct cancers; derivatives, but a strict dietary
elevated levels may also be found in protocol is essential.
noncancer conditions o Stool DNA testing is a relatively new
means to detect certain DNA related to
colon cancer
Stool Tests ➢ The stool DNA test does not
require any dietary or
o Basic examination of the stool includes:
medication restrictions
• inspecting the specimen for
➢ can detect neoplasia anywhere
consistency
in the colon
• color
• occult (not visible) blood Breath Tests
o Additional studies, including:
o The hydrogen breath test was
• fecal urobilinogen
developed to evaluate carbohydrate
• fecal fat
absorption, in addition to aiding in the • almost immediate results
diagnosis of bacterial overgrowth in the o Endoscopic ultrasonography (EUS) is a
intestine and short bowel syndrome specialized enteroscopic procedure that
➢ determines the amount of aids in the diagnosis of GI disorders by
hydrogen expelled in the breath providing direct imaging of a target
after it has been produced in area.
the colon and absorbed into the ➢ used to evaluate submucosal
blood lesions, specifically their
o Urea breath tests detect the presence location and depth of
of Helicobacter pylori, the bacteria that penetration
can live in the mucosal lining of the ➢ may aid in the evaluation of:
stomach and cause peptic ulcer disease. ▪ Barrett esophagus
➢ After the patient ingests a ▪ portal hypertension
capsule of carbon-labeled urea, ▪ chronic pancreatitis
a breath sample is obtained 10 ▪ suspected pancreatic
to 20 minutes later neoplasm
➢ Prior to urea breath testing, the ▪ biliary tract disease
patient is instructed to avoid: ▪ changes in the bowel
▪ antibiotics or bismuth wall due to ulcerative
subsalicylate (Pepto- colitis.
Bismol) for 1 month
before the test; Nursing Interventions
▪ sucralfate (Carafate) o The patient is instructed to fast for 8 to
and omeprazole 12 hours before ultrasound testing to
(Prilosec) for 1 week decrease the amount of gas in the
before the test bowel.
▪ cimetidine (Tagamet), o If gallbladder studies are being If
famotidine (Pepcid), gallbladder studies are being
and ranitidine (Zantac) o If barium studies are to be performed,
for 24 hours before the they should be scheduled after
test ultrasonography
Abdominal Ultrasonography o Patients who receive moderate
sedation are observed for about 1 hour
o Ultrasonography is a noninvasive to assess for level of consciousness,
diagnostic technique in which orientation, and ability to ambulate.
highfrequency sound waves are passed
into internal body structures
o It is particularly useful in the detection Genetic Testing
of an enlarged gallbladder or pancreas,
the presence of gallstones, an enlarged o People who are identified as being at
ovary, an ectopic pregnancy, or risk for certain GI disorders may choose
appendicitis to have genetic counseling to learn
o Advantages of abdominal about the disease and options for
ultrasonography include: preventing and treating the disease,
• an absence of ionizing radiation and to receive support in coping with
• no noticeable side effects the situation.
• relatively low cost
Imaging Studies o This process (even with normal motility)
can take up to 6 hours and can be quite
1. Upper Gastrointestinal Tract Study
uncomfortable for the patient.
o An upper GI fluoroscopy delineates the o The procedure aids in the diagnosis of
entire GI tract after the introduction of partial small bowel obstructions or
a contrast agent diverticula
o radiopaque liquid (e.g., barium sulfate)
is commonly used Nursing intervention
➢ radiopaque liquid (e.g., barium
sulfate) is commonly used o Instruction regarding dietary changes
prior to the study should include a clear
o enables the examiner to detect or
exclude anatomic or functional liquid diet, with nothing by mouth
disorders of the upper GI organs or (NPO) from midnight the night before
sphincters the study
o It also aids in the diagnosis of ulcers, o Polyethylene glycol (PEG)-based
varices, tumors, regional enteritis, and solutions are considered the most
malabsorption syndromes effective bowel cleansing preparatory
o Multiple x-ray images are obtained agent
during the procedure, and additional o oral medications are withheld on the
morning of the study and resumed that
images may be taken at intervals for up
to 24 hours to evaluate the rate of evening, but each patient’s medication
gastric emptying regimen should be evaluated on an
individual basis
Variations of the upper GI study include: o When a patient with insulin-dependent
diabetes is NPO, their insulin
• double-contrast studies requirements will need to be adjusted
• enteroclysis accordingly
double-contrast method o Follow-up care is provided after the
upper GI procedure to ensure that the
o involves administration of a thick patient has eliminated most of the
barium suspension to outline the ingested barium
stomach and esophageal wall, after
which tablets that release carbon
dioxide in the presence of water are Lower Gastrointestinal Tract Study
given
o This technique has the advantage of o The barium enema can be used to
showing the esophagus and stomach in detect the presence of polyps, tumors,
finer detail, permitting signs of early or other lesions of the large intestine
superficial neoplasms to be noted and demonstrate any anatomic
abnormalities or malfunctioning of the
Enteroclysis bowel.
o a very detailed, double-contrast study o The procedure usually takes about 15 to
of the entire small intestine that 30 minutes, during which time x-ray
involves the continuous infusion images are obtained
(through a duodenal tube) of 500 to o Other means for visualizing the colon
1000 mL of a thin barium sulfate include:
suspension • double-contrast studies or air-
o after this, methylcellulose is infused contrast barium enema involves
through the tube. the instillation of a thicker
barium solution, followed by ➢ Active GI bleeding may prohibit
the instillation of air. the use of laxatives and
▪ provides a contrast enemas.
between the air-filled o Postprocedural patient education
lumen and the barium- includes information about increasing
coated mucosa, fluid intake, evaluating bowel
allowing easier movements for evacuation of barium,
detection of smaller and noting increased number of bowel
lesions movements
• a water-soluble contrast study
▪ If active inflammatory
disease, fistulas, or Computed Tomography
perforation of the colon
is suspected o provides cross-sectional images of
▪ patient must first be abdominal organs and structures
assessed for allergy to o A CT scan may be performed with or
iodine or contrast agent without oral or intravenous (IV)
▪ Some diarrhea may contrast, but the enhancement of the
occur in some patients study is greater with the use of a
until the contrast agent contrast agent
has been totally o a valuable tool for detecting and
eliminated localizing many inflammatory
conditions in the colon, as well as
Nursing Interventions evaluating the abdomen for diseases of
the liver, spleen, kidney, pancreas, and
o Preparation of the patient includes
pelvic organs, and structural
emptying and cleansing the lower
abnormalities of the abdominal wall
bowel.
o This often necessitates a low-residue Nursing Interventions
diet 1 to 2 days before the test, a clear
liquid diet and a laxative the evening o Common risks from IV contrast agents
before include allergic reactions and acute
o NPO after midnight, and cleansing kidney injury
enemas until returns are clear the o Patients allergic to the contrast agent
following morning may be premedicated with a
o The nurse makes sure that barium corticosteroid and antihistamine
enemas are scheduled before any upper o kidney protective measures include the
GI studies. administration of IV sodium
➢ If the patient has active bicarbonate 1 hour before and 6 hours
inflammatory disease of the after IV contrast and oral N-
colon, enemas are acetylcysteine (Mucomyst) before or
contraindicated. after the study
➢ Barium enemas also are
contraindicated in patients with
signs of perforation or Magnetic Resonance Imaging
obstruction; instead, a water-
o used in gastroenterology to supplement
soluble contrast study may be
ultrasonography and CT. This
performed
noninvasive technique uses magnetic
fields and radio waves to produce ➢ This is useful in diagnosing
images of the area being studied. disorders of gastric motility,
o It is useful in evaluating abdominal soft diabetic gastroparesis, and
tissues as well as blood vessels, dumping syndrome.
abscesses, fistulas, neoplasms, and o Colonic transit studies are used to
other sources of bleeding. evaluate colonic motility and
obstructive defecation syndromes
Nursing Interventions ➢ The patient is given a capsule
o Before the study patient education containing 20 radionuclide
includes NPO status 6 to 8 hours before markers and instructed to
the study and removal of all jewelry and follow a regular diet and usual
other metals. daily activities.
o during this time, the technician will ➢ Abdominal x-rays are taken
instruct the patient to take deep every 24 hours until all markers
breaths at specific intervals are passed.
o Patients may choose to wear a headset ➢ This process usually takes 4 to 5
and listen to music or wear a blindfold days; in the presence of severe
during the procedure constipation it may take as long
as 10 days
Positron Emission Tomography
o produce images of the body by
Endoscopic Procedures
detecting the radiation emitted from Upper Gastrointestinal
radioactive substances Fibroscopy/Esophagogastroduodenoscopy
Scintigraphy o Fibroscopy of the upper GI tract allows
o relies on the use of radioactive isotopes direct visualization of the esophageal,
to reveal displaced anatomic structures, gastric, and duodenal mucosa through a
changes in organ size, and the presence lighted endoscope
of neoplasms or other focal lesions such ➢ This procedure also can be used
as cysts or abscesses. to evaluate esophageal and
o also used to measure the uptake of gastric motility and to collect
tagged red blood cells and leukocytes secretions and tissue specimens
o Abnormal concentrations of blood cells for further analysis
are then detected at 24- and 48-hour o PillCam ESO, or capsule endoscopy
intervals requires that the patient swallows a
capsule that travels by peristalsis
Gastrointestinal Motility Studies through the small intestines.
➢ Transit time from the time the
o Radionuclide testing also is used to
capsule is swallowed until it is
assess gastric emptying and colonic
passed is approximately 24
transit time
hours
➢ During gastric emptying studies,
➢ provides superior visualization
the liquid and solid components
of the small intestines, and is
of a meal (typically scrambled
particularly useful to detect
eggs) are tagged with
occult areas of bleeding,
radionuclide markers
inflammatory bowel disease, broken if the scope is bent at an
and celiac disease acute angle.
o Endoscopic retrograde ➢ The patient wears a mouth
cholangiopancreatography uses the guard to keep from biting the
endoscope in combination with x-rays scope.
to view the bile ducts, pancreatic ducts,
and gallbladder Nursing Intervention
➢ helpful in evaluating jaundice, o The patient should be NPO for 8 hours
pancreatitis, pancreatic tumors, prior to the examination
common bile duct stones, and o Midazolam (Versed), a sedative that
biliary tract disease. provides moderate sedation with loss of
o Upper GI fibroscopy also can be a the gag reflex and relieves anxiety
therapeutic procedure when combined during the procedure, is given.
with other procedures. o Atropine may be given to reduce
➢ Therapeutic endoscopy can be secretions, and glucagon may be given
used to remove common bile to relax smooth muscle
duct stones, dilate strictures, o The patient is positioned in the left
and treat gastric bleeding and lateral position to facilitate clearance of
esophageal varices pulmonary secretions and provide
➢ Sclerosing solutions can be smooth entry of the scope
injected through the scope in o after the patient’s gag reflex has
an attempt to control upper GI returned, lozenges, saline gargle, and
bleeding oral after the patient’s gag reflex has
➢ After the patient is sedated, the returned, lozenges, saline gargle, and
endoscope is lubricated with a oral.
water-soluble lubricant and
passed smoothly and slowly
along the back of the mouth Fiberoptic Colonoscopy
and down into the esophagus.
➢ Biopsy forceps to obtain tissue o Virtual colonoscopy provides a
specimens or cytology brushes computer-simulated view of the air-
to obtain cells for microscopic filled distended colon using
study can be passed through conventional CT scanning.
the scope. o It is most frequently used for cancer
➢ The procedure usually takes screening and for surveillance in
about 30 minutes patients with previous colon cancer or
➢ The patient may experience polyps.
nausea, gagging, or choking o Other uses of colonoscopy include the:
➢ The use of topical anesthetic • evaluation of patients with
agents and moderate sedation diarrhea of unknown cause
makes it important to monitor • occult bleeding or anemia
and maintain the patient’s oral • further study of abnormalities
airway during and after the detected on barium enema
procedure • and diagnosis, clarification, and
➢ Precautions must be taken to determination of the extent of
protect the scope, because the inflammatory or other bowel
fiberoptic bundles can be disease
o The procedure can be used to remove ▪ use of 2-L PEG split-
all visible polyps with a special snare dose regimen in low or
and cautery through the colonoscope. no risk patients,
o The use of bipolar and unipolar ▪ 4-L split-dose with
coagulators and heater probes, as well sodium picosulfate plus
as injections of sclerosing agents or bisacodyl in patients
vasoconstrictors, is possible during this with comorbidities such
procedure as diabetes, chronic
o Colonoscopy is performed while the constipation, or current
patient is lying on the left side with the history of opioid use, or
legs drawn up toward the chest with a history of
o Complications during and after the problematic
procedure can include: colonoscopies
• cardiac dysrhythmias and o Then the patient ingests the lavage
respiratory depression resulting solution orally at intervals over 3 to 4
from the medications given hours
• vasovagal reactions o The use of lavage solutions is
• circulatory overload or contraindicated in patients with
hypotension resulting from intestinal obstruction or inflammatory
overhydration or bowel disease
underhydration during bowel o sodium phosphate tablet (OsmoPrep,
preparation Visicol) can be used for colon cleansing
o The patient’s cardiac and respiratory prior to colonoscopy
function and oxygen saturation are ➢ 20 tablets (4 tablets every 15
monitored continuously, with minutes) with 8 oz of any clear
supplemental oxygen used as necessary liquid on the evening prior to
the examination, and 12 tablets
Capsule colonoscopy on the morning of the
o another option for patients who cannot examination
tolerate colonoscopy. o Side effects of the electrolyte solutions
o the patient must ingest a lot of fluids to include:
ensure that the capsule transits through • Nausea
the colon • Bloating
• cramps or abdominal fullness
Nursing Interventions • fluid and electrolyte imbalance
o Adequate colon cleansing provides • hypothermia
optimal visualization and decreases the o Colonoscopy cannot be performed if
time needed for the procedure. there is a suspected or documented:
• The primary provider may • colon perforation
prescribe a laxative for two • acute severe diverticulitis
nights before the examination • fulminant colitis
• a Fleet or saline enema until the o Patients with prosthetic heart valves or
return is clear the morning of a history of endocarditis require
the test prophylactic antibiotics before the
• PEG electrolyte lavage solutions procedure
o During the procedure, the patient is
monitored for changes in:
• oxygen saturation o During the procedure, the nurse
• vital signs monitors:
• color and temperature of the • vital signs
skin • skin color and temperature
• level of consciousness • pain tolerance
• abdominal distention • vagal response
• vagal response o After the procedure, the nurse monitors
• pain intensity the patient for rectal bleeding and signs
o After the procedure, patients are of intestinal perforation
maintained on bed rest until fully alert
o Immediately after the test, the patient
is monitored for signs and symptoms of Small Bowel Studies
bowel perforation
➢ Because of the amnesic effects o Several methods are available for
of midazolam, the patient may visualization of the small intestine,
be unable to recall verbal including:
information and should receive • capsule endoscopy
written instructions • double-balloon enteroscopy
Capsule endoscopy
Anoscopy, Proctoscopy, and Sigmoidoscopy o allows the noninvasive visualization of
the mucosa throughout the entire small
o Endoscopic examination of the anus, intestine
rectum, and sigmoid and descending o It is particularly useful in the evaluation
colon is used to evaluate: of obscure GI bleeding
• chronic diarrhea o the capsule passes from the rectum in 1
• fecal incontinence or 2 days
• ischemic colitis
Double-balloon enteroscopy
• lower GI hemorrhage
• to observe for ulceration, o has made it possible to visualize the
fissures, abscesses, tumors, mucosa of the entire small bowel as
polyps, or other pathologic well as carry out diagnostic and
processes therapeutic interventions
o the patient assumes a comfortable o The procedure takes between 1 and 3
position on the left side with the right hours and requires moderate sedation
leg bent and placed anteriorly
o Biopsies and polypectomies can be Endoscopy Through an Ostomy
performed during this procedure o Endoscopy through an ostomy stoma is
Nursing Interventions useful for visualizing a segment of the
small or large intestine
o These examinations require only limited o may be indicated to evaluate the
bowel preparation, including a warm anastomosis for recurrent disease, or to
tap water or Fleet enema until returns visualize and treat bleeding in a
are clear segment of the bowel
o Dietary restrictions usually are not
necessary, and sedation usually is not
required
Manometry and Electrophysiologic o The results are especially helpful in the
evaluation of patients with chronic
Studies constipation, diarrhea, or incontinence
Esophageal manometry
Electrogastrography
o is used to detect motility disorders of
o an electrophysiologic study, also may be
the esophagus and the upper and lower
performed to assess gastric motility
esophageal sphincter
disturbances and can be useful in
o The patient must refrain from eating or
detecting motor or nerve dysfunction in
drinking for 8 to 12 hours before the
the stomach
test. Medications that could have a
o recorded for up to 24 hours
direct effect on motility are withheld for
24 to 48 hours.
Gastroduodenal, small intestine, and colonic Gastric Analysis, Gastric Acid
manometry
Stimulation Test, and pH Monitoring
o procedures are used to evaluate
delayed gastric emptying and gastric o Analysis of the gastric juice yields
and intestinal motility disorders such as information about the secretory activity
irritable bowel syndrome or atonic of the gastric mucosa and the presence
colon or degree of gastric retention in
o This is often an ambulatory outpatient patients thought to have pyloric or
duodenal obstruction.
procedure lasting 24 to 72 hours
o The patient is NPO for 8 to 12 hours
Anorectal manometry measures before the procedure
o Any medications that affect gastric
o the resting tone of the internal anal secretions are withheld for 24 to 48
sphincter and the contractibility of the hours before the test.
external anal sphincter o Smoking is not allowed on the morning
o It is helpful in evaluating patients with of the test because it increases gastric
chronic constipation or fecal secretions
incontinence and is useful in o This ability is altered in various disease
biofeedback for the treatment of fecal states, including:
incontinence ➢ Pernicious anemia: Patients
o Dibasic sodium (Phospho-soda) or a with this disease secrete no
saline cleansing enema is given 1 hour acid under basal conditions or
before the test, and positioning for the after stimulation.
test is either the prone or the lateral ➢ Severe chronic atrophic gastritis
position or gastric cancer: Patients with
Rectal sensory function studies these diseases secrete little or
no acid.
o are used to evaluate rectal sensory ➢ Gastric ulcer: Patients with this
function and neuropathy disease secrete some acid.
o Then the tone and pressure of the ➢ Duodenal ulcers: Patients with
rectum and anal sphincter are this disease usually secrete an
measured excess amount of acid
The gastric acid stimulation test • chronic abdominal pain
• abdominal masses
o usually is performed in conjunction with
• gallbladder and liver disease
gastric analysis
o Laparoscopy usually requires general
o Histamine or pentagastrin is given
anesthesia and sometimes requires that
subcutaneously to stimulate gastric
the stomach and bowel be
secretions.
decompressed.
o It is important to inform the patient
that this injection may produce a
flushed feeling
o The nurse monitors the patient’s blood
pressure and pulse frequently to detect
hypotension
o Gastric specimens are collected after
the injection every 15 minutes for 1
hour and are labeled to indicate the
time of specimen collection after
histamine injection.
➢ Papanicolaou technique may be
used to determine the presence
or absence of malignant cells
Esophageal reflux of gastric acid
o may be diagnosed by ambulatory pH
monitoring
o The patient is NPO for 6 hours before
the test
o all medications affecting gastric
secretions are withheld for 24 to 36
hours before the test
Bravo pH monitoring system
o offers the advantage of pH monitoring
of the esophagus without the transnasal
catheter
o Data are collected for up to 48 hours
o The patient is evaluated for both acid
reflux and nonacid reflux
Laparoscopy (Peritoneoscopy)
o After a pneumoperitoneum
o is created, a small incision is made
lateral to the umbilicus, allowing for the
insertion of the fiberoptic laparoscope
o This procedure can be used to evaluate:
• peritoneal disease
You might also like
- Nursing PharmacologyDocument13 pagesNursing Pharmacologyjeshema100% (4)
- 6-7 - Medical Nursing - GIS DisordersDocument108 pages6-7 - Medical Nursing - GIS DisordersmichaelNo ratings yet
- Diseases of The OesophagusDocument6 pagesDiseases of The OesophagusMohamed AlsaabNo ratings yet
- hs320 W11 DigestiveSystemDisordersDocument41 pageshs320 W11 DigestiveSystemDisordersjoseyalm2323No ratings yet
- Bowel EliminationDocument123 pagesBowel EliminationSharon LawrenceNo ratings yet
- 22 Manuscript Intestinal ObstructionDocument8 pages22 Manuscript Intestinal Obstructionkint manlangitNo ratings yet
- The GI System Is Composed of Two General Parts Gi TractDocument14 pagesThe GI System Is Composed of Two General Parts Gi TractRexson Alcantara DalanginNo ratings yet
- NSG 306-1Document56 pagesNSG 306-1Anifowose samsonNo ratings yet
- Bowel EliminationDocument59 pagesBowel EliminationRekha DehariyaNo ratings yet
- 1 Gastrointestinal System DisordersDocument14 pages1 Gastrointestinal System DisordersAnna Sofia Reyes100% (1)
- GIT DisordersDocument171 pagesGIT DisordersKatrina PonceNo ratings yet
- What Is Abdominal Pain? TreatmentDocument2 pagesWhat Is Abdominal Pain? TreatmentErick YohanesNo ratings yet
- Chapter 28 Child With A Gastrointestinal ConditionDocument85 pagesChapter 28 Child With A Gastrointestinal Conditionsey_scottNo ratings yet
- NCM 116 Gep MidtermDocument20 pagesNCM 116 Gep MidtermKM PanganibanNo ratings yet
- CancerDocument30 pagesCancerAbhirami BabuNo ratings yet
- Approach To The Child With Nausea and Vomiting: by DR - Ryan Al - GhanemiDocument50 pagesApproach To The Child With Nausea and Vomiting: by DR - Ryan Al - GhanemiyusufharkianNo ratings yet
- Pengkajian Sistem GastrointestinalDocument38 pagesPengkajian Sistem GastrointestinalNabila FatharaniNo ratings yet
- Disorder and Diseases of Digestive SystemDocument8 pagesDisorder and Diseases of Digestive SystemCristina AnganganNo ratings yet
- What Are The Signs of Bleeding in The Digestive Tract?Document6 pagesWhat Are The Signs of Bleeding in The Digestive Tract?draganNo ratings yet
- Ed-Abdominal PainDocument2 pagesEd-Abdominal PainMuhammad Arif RahmanNo ratings yet
- Pemicu 5 GITDocument52 pagesPemicu 5 GITMudita DewiNo ratings yet
- INTESTINEDocument98 pagesINTESTINEDeepika LingamNo ratings yet
- Non-Inflammatory Bowel DisordersDocument33 pagesNon-Inflammatory Bowel Disorderssho bartNo ratings yet
- NCP 1Document3 pagesNCP 1Mary Antonette Adriano EnriquezNo ratings yet
- Assessment of Digestive and Intestinal Tracts Disorders HAMDALLAHDocument141 pagesAssessment of Digestive and Intestinal Tracts Disorders HAMDALLAHMAYHAMDALLAHNo ratings yet
- Peptic Ulcer FinalDocument6 pagesPeptic Ulcer FinalLarra MoslaresNo ratings yet
- Pumpkin Spice and Everything NiceDocument7 pagesPumpkin Spice and Everything Niceotum.shayneNo ratings yet
- Pathology Gis: Aanisah F 14.103Document47 pagesPathology Gis: Aanisah F 14.103rftdlsNo ratings yet
- Bowel Elimination and Urinary Incontinence ProblemsDocument5 pagesBowel Elimination and Urinary Incontinence ProblemsMegan Rose MontillaNo ratings yet
- Concept of Elimination-1Document39 pagesConcept of Elimination-1kalimulallah4No ratings yet
- Nursing Care Plan Nausea & VomitingDocument3 pagesNursing Care Plan Nausea & Vomitingderic87% (47)
- "Gosh, Mrs. Doubtfire You Look Pale": Fire" in Television at The Emergency Departement You Worked ForDocument84 pages"Gosh, Mrs. Doubtfire You Look Pale": Fire" in Television at The Emergency Departement You Worked ForAngela Kristiana IntanNo ratings yet
- Gastro-Oesophageal Reflux Disease (GORD) : Anish DhakalDocument31 pagesGastro-Oesophageal Reflux Disease (GORD) : Anish DhakalnrauliaprtwNo ratings yet
- Management of Client With Gastrointestinal DisordersDocument33 pagesManagement of Client With Gastrointestinal DisordersKelly TayagNo ratings yet
- Intestinal Obstruction 4Document25 pagesIntestinal Obstruction 4Muvenn KannanNo ratings yet
- Assessment of The AbdomenDocument7 pagesAssessment of The AbdomenS StPierreNo ratings yet
- Department of Surgery: Case Presentation Intestinal ObstructionDocument46 pagesDepartment of Surgery: Case Presentation Intestinal Obstructionhadil ayeshNo ratings yet
- Common Causes of PUD: Duodenal Ulcer: A Peptic Ulcer of TheDocument8 pagesCommon Causes of PUD: Duodenal Ulcer: A Peptic Ulcer of Thestudy mailNo ratings yet
- Irritable Bowel SyndromeDocument5 pagesIrritable Bowel Syndromedrnareshkumar32810% (1)
- C. Disorders of The Lowel BowelDocument69 pagesC. Disorders of The Lowel BowelJmarie Brillantes PopiocoNo ratings yet
- Presenting Problems in Gastrointestinal Disease:: DysphagiaDocument9 pagesPresenting Problems in Gastrointestinal Disease:: DysphagiaMohamed AlsaabNo ratings yet
- Nursing Management of Git Problems: Oral and Esophageal DisordersDocument18 pagesNursing Management of Git Problems: Oral and Esophageal Disorderslcpot_se7en7505100% (2)
- Acute Abdomen, Nyeri Akut AbdomenDocument35 pagesAcute Abdomen, Nyeri Akut AbdomenYanuar Yudha SudrajatNo ratings yet
- Chronic Diarrhea-HTKDocument63 pagesChronic Diarrhea-HTKcerenblgstrNo ratings yet
- Acute AbdomenDocument21 pagesAcute AbdomenMillicent AwuzieNo ratings yet
- GastritisDocument18 pagesGastritisleian28No ratings yet
- Anorexia: Basic InformationDocument34 pagesAnorexia: Basic InformationcarlosNo ratings yet
- Ms Prelim NewDocument12 pagesMs Prelim NewJane LaquihonNo ratings yet
- Hiatal Hernia FactsheetDocument6 pagesHiatal Hernia FactsheetHoney Bee S. PlatolonNo ratings yet
- Elimination: Dumip-Ig, Maricel Gregorio, Kristine Milagrosa, Nina JesusaDocument30 pagesElimination: Dumip-Ig, Maricel Gregorio, Kristine Milagrosa, Nina JesusaKristine Las GregorioNo ratings yet
- NcpsDocument10 pagesNcpskotoirNo ratings yet
- 62 DiarrheaChronic MGHG MIMG MFM 20161229Document10 pages62 DiarrheaChronic MGHG MIMG MFM 20161229Wei HangNo ratings yet
- A Simple Guide to Gastritis and Related ConditionsFrom EverandA Simple Guide to Gastritis and Related ConditionsRating: 4.5 out of 5 stars4.5/5 (3)
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Perfect Lpr Diet Cookbook:The Complete Nutrition Guide To Lowering Stomach Acid Naturally And Easing Gastritis With Delectable and Nourishing RecipesFrom EverandThe Perfect Lpr Diet Cookbook:The Complete Nutrition Guide To Lowering Stomach Acid Naturally And Easing Gastritis With Delectable and Nourishing RecipesNo ratings yet
- Constipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationFrom EverandConstipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- Medical Surgical Nursing 2 Denn Hill RiorosoDocument10 pagesMedical Surgical Nursing 2 Denn Hill RiorosoLienyPerasNo ratings yet
- Muskuloskeletal DisordersDocument15 pagesMuskuloskeletal DisordersLienyPerasNo ratings yet
- Drugs For Gastrointestinal SystemDocument6 pagesDrugs For Gastrointestinal SystemLienyPerasNo ratings yet
- Nursing REVIEWER 2Document11 pagesNursing REVIEWER 2LienyPerasNo ratings yet
- Schizophrenia and Other Psychotic Disorders Clinical Practice GuidelineDocument7 pagesSchizophrenia and Other Psychotic Disorders Clinical Practice GuidelineDani NugrohoNo ratings yet
- CrampsDocument14 pagesCrampsJen PassilanNo ratings yet
- EmpiemaDocument19 pagesEmpiemaArrol Iswahyudi100% (1)
- Document PDFDocument18 pagesDocument PDFlilisNo ratings yet
- PDEV Notes For Periodical ExamDocument7 pagesPDEV Notes For Periodical ExamErjie GerasmioNo ratings yet
- Active IngredientDocument2 pagesActive IngredientNeri Jane JablaNo ratings yet
- What Is MDocument2 pagesWhat Is MkasjdkasNo ratings yet
- Cutaneous Manifestation of HivDocument36 pagesCutaneous Manifestation of Hivyunita hapsariNo ratings yet
- Diabetes and RamadanDocument4 pagesDiabetes and Ramadan80082583No ratings yet
- Post Op Alveoloplasty - RRR - 1 PDFDocument1 pagePost Op Alveoloplasty - RRR - 1 PDFAndykaYayanSetiawanNo ratings yet
- Global Health Current Issues Future Trends and ForDocument8 pagesGlobal Health Current Issues Future Trends and ForMsMhey PalattaoNo ratings yet
- Junk FoodDocument17 pagesJunk FoodCorey Page0% (1)
- Shave Your Balls and 100 Other Things Your Mother Should Have Told YouDocument112 pagesShave Your Balls and 100 Other Things Your Mother Should Have Told Youdelski14No ratings yet
- Surgery Short Case - HydroceleDocument1 pageSurgery Short Case - HydroceleHeroNo ratings yet
- Pa Tho Physiology of Colon CancerDocument2 pagesPa Tho Physiology of Colon Cancernick_nock0893% (14)
- EMREE Q BANK - Edited and Revised Part 1Document101 pagesEMREE Q BANK - Edited and Revised Part 1Sandra Abboud100% (1)
- Longevity - Wikipedia, The Free EncyclopediaDocument11 pagesLongevity - Wikipedia, The Free EncyclopediaJames DriscollNo ratings yet
- Cholera in NepalDocument57 pagesCholera in NepalBinayaNo ratings yet
- AttentionDocument6 pagesAttentionSneha BhattNo ratings yet
- Myasthenia GravisDocument3 pagesMyasthenia Gravisapi-3822433100% (2)
- Endotracheal Intubation & ER Board Exam QuestionsDocument33 pagesEndotracheal Intubation & ER Board Exam QuestionsJo-Anne Karen Serdeña0% (1)
- Bio 9th 2nd Chapter Biological MethodDocument7 pagesBio 9th 2nd Chapter Biological Methodhamza0% (1)
- Flexi Medical Plan BrochureDocument28 pagesFlexi Medical Plan BrochurewoodksdNo ratings yet
- Diabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaDocument6 pagesDiabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- AgnosiaDocument15 pagesAgnosiaMUHAMMAD BILALNo ratings yet
- Ewing Sarcoma PDFDocument2 pagesEwing Sarcoma PDFShellyNo ratings yet
- Health - I'm SickDocument1 pageHealth - I'm SickKaled LamouriNo ratings yet
- Kode Diagnosis ElinkDocument1 pageKode Diagnosis ElinksandraldiraNo ratings yet
- Pediatric Ist SeminarDocument21 pagesPediatric Ist SeminarAsha jiluNo ratings yet