Professional Documents
Culture Documents
Dengue Encephalopathy: S.K. Hendarto, M.D. and Sri Rezeki Hadinegoro, M.D
Dengue Encephalopathy: S.K. Hendarto, M.D. and Sri Rezeki Hadinegoro, M.D
Uploaded by
Tonni ZhengOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dengue Encephalopathy: S.K. Hendarto, M.D. and Sri Rezeki Hadinegoro, M.D
Dengue Encephalopathy: S.K. Hendarto, M.D. and Sri Rezeki Hadinegoro, M.D
Uploaded by
Tonni ZhengCopyright:
Available Formats
(Acta Paediatr Jpn 1992; 34: 350 - 357)
Dengue Encephalopathy
S.K. Hendarto, M.D. and Sri Rezeki Hadinegoro, M.D.
Departnient of Child Health, Medical Facult!,, Universitj, c?f’ Indonesia. Jakarta, Indonesia
Dengue encephalopathy or dengue hemorrhagic fever (DHF) with CNS involvement used
to be considered a relatively rare condition; but the number of cases reported in human
studies has been increasing every year. Diagnosis of dengue encephalopathy is based on
clinically diagnosed D H F according to the W.H.O. criteria (1980), with CNS
manifestations consisting of abrupt onset of hyperpyrexia, nontransient alteration of
- -
consciousness, headache, vomiting with or without seizures and normal CSF. Many
factors may be considered to be directly or indirectly associated with CNS signs and
symptoms in DHF, the main pathology being leakage of plasma into serous spaces and
abnormal hemostasis, leading to hypovolemic shock and hemorrhage in many organs of the
body. Acute liver failure is considered to be one of the main factors causing brain
pathology. One hundred fifty-two cases of dengue encephalopathy admitted during 3
periods at the Cipto Mangunkusumo Hospital in Jakarta were studied retrospectively. The
overall incidence was 152 out of 2,441 D H F cases, or 6.2%. The most pronounced
symptoms were hyperpyrexia, alteration of consciousness and convulsions. Laboratory
examination showed an unusually high increase of serum transaminases, hyponatremia,
and hypoxia. Neurologic abnormalities detected were hemiparesis and tetraparesis of the
extremities, and second nerve atrophy; such abnormalities were found in 10 out of the 152
cases, or 6.5%.
Key Words
Dengue hemorrhagic fever, Encephalopathy
Introduction
Dengue fever has been known for more than
two decades as a tropical endemic infection
Receired February 17. 1992 caused by dengue virus, a flavivirus from the
Correspondence address: S.K. Hendarto. M.D., Depart- arbovirus or arthropod-borne virus group.
ment of Child Health. Medical Faculty. University of Formerly called “five days’ fever,” the classical
Indonesia. Jakarta. Indonesia
dengue infection had the well-known symp-
Reproduced lrom the following with permission: Fuku- toms of acute febrile illness, headache, joint
yama Y . . Kamoshita S.. Ohtsuka C., Suzuki Y., eds.
Modern Perspectives of Child Neurology. Proceedings II and muscle pain, as found with any other viral
of the Joint Convention of the 5th International Child infection, and rash.
Neurology Congress and the 3rd Asian & Oceanian The main reservoir of dengue virus is man,
Congress of Child Neurology. Tokyo, November 4-9.
1990. Tokyo: The Japanese Society of Child Neurology. and it is mainly transmitted by Aedes aegypti
1991; 345-51. mosquitoes; in rural areas other species such
Dengue encephalopathy (93) 35 I
as Aedes albopictus may play a role in the severe clinical manifestations which are classi-
spreading of this disease [ 13. fied as grade 111 or 1V according to the
Aedes mosquitoes habitually multiply in W.H.O. grading of D H F [2]. All the 4
relatively clean water shaded from light; serotypes of dengue virus have been identified
female mosquitoes tend t o bite man at or as causes of dengue infection in Indonesia [3].
afternoon. Increased frequency of dengue The W.H.O. [Z] has proposed clinical
infection usually occurs during the rainy criteria for the diagnosis of D H F as follows:
season when the mosquitoes seek shelter from Acute onset of fever, continuous for at least
the rain and invade the homes. 2-7 days
Dengue fever with hemorrhagic manifesta- Hemorrhagic manifestations proven by a
tions is called dengue hemorrhagic fever positive tourniquet test or by petechiae,
(DHF), and is manifested as fever without purpura, ecchymosis, epistaxis, gum bleed-
severe joint or muscle pain; deterioration with ing, hematemesis and/ or melaena
bleeding tendency occurs after the first two Liver enlargement
days of the illness and is after accompanied by Shock, manifested by rapid and weak
shock. If shock develops it is called dengue pulse, narrowing of the pulse pressure to
shock syndrome (DSS). D H F has become a 20 mm or less, hypotension, clammy sweat
major public health problem in tropical areas; and restlessness
the number of cases has been increasing every Laboratory evidence of thrombocytopenia
year, with an explosive outbreak approximately of less than 8O,OOO, with a steady rise of the
every five years. hematocrit to a hemoconcentration of
Serologic studies have identified 4 serotypes more than 20% in the acute phase of the
of dengue virus in man, Den-I, 2, 3 and 4. illness.
Serotype Den-3 is known to cause D H F with
Table I . Age distribution of group I and I I D H F cases. 7-able 2. Classification of 98 cases of dengue encepha-
compared with cases of group 111 lopathy according to W H O classification
Age group Group I Group II Group I l l D H F grading Number of cases r:;
(years) N-358 N-754 N-98
D H F GR 1 - 0
<I 7 (1.9Q) 10 (1.3%) 10 (10.2%) D H F GR I1 22 22.6
14 148 (41 4%) 173 (22.8%) 37 (37.3%) D H F GR 111 13 13.3
5 9 105 (46.1'%,) 359 (47.6%) 40 (48.8%) D H F GR IV 63 64.3
> 10 38 (10.6%)) 212 (28.1%) I I (11.3%)
Total number 98 100.0
Table 3. Clinical manilestations in 3 groups of dengue encephalopathy
Clinical signs Group I Group I I Group I l l Total
and symptoms N-33 Y-2 I S-98 N-152
Abrupt onset of hyperpyrexia 33 (100.0'h) 21 (IOo.W%,) Y8 (IOo.ock)
Alteration of consciousness 33 (100.0(%) 21 (IOo.W&) 92 (93.8%) 146 (98.0%.)
Headache 10 (30.3%) 2 (9.5%) I3 ( 13.2%) 25 (16.4%)
Vomiting 23 (69.7%) 15 (71.4%) 23 (23.3%) 61 (40.4%)
Convulsions 28 (84.8%) I I (52.4%) 84 (84.9%) I23 (80.9%)
Neurologic abnormalities I0 (6.59;)
Hemiparesis 0 (0.0%) 2 (2.0%)
Tetraparesis 2 (9.57b) 2 (2.00?)
Optic atrophy I (9.5%) 0 (0.00?)
Normal CSF 21 (lOo.W+) 98 (lOo.O%)
Vol. 34 No. 3 June 1992
352 (94) Hendarro and Hadinegoro
The diagnosis of DHF is made if there are Mangunkusumo Hospital, Medical Faculty,
2 or more clinical manifestations with throm- University of Indonesia, Jakarta, at 3 different
bocytopenia and hemoconcentration. Confir- periods were evaluated.
mation of the diagnosis is made by virus The first group consisted of dengue
isolation or serologic hemagglutination inhibi- encephalopathy cases admitted from May Ist,
tory titer evaluation. 1975 to September 31st, 1976. The second
Outbreaks of DHF have occurred in many group were those admitted from January Ist,
tropical and subtropical areas including South- 1985, to December 31st, 1986. These 2 groups
East Asia, where Indonesia ranks second after had been studied previously by another author
Thailand in the number of cases detected; the [lo].
number in Indonesia reached its highest point The third group included cases of dengue
in 1983 with 11,875 cases, of which 491 died encephalopathy admitted from January lst,
~41. 1988, to December 31st, 1989.
Recently more cases have been reported in The method used was a retrospective
the literature of DHF with CNS manifestations evaluation of cases of dengue encephalopathy,
[5-91, which are now recognized as dengue
encephalopathies. In Indonesia, dengue en- Table 4. Other signs and symptoms of 98 cases of dengue
cephalopathy was first reported in 1981 [6]. encephalopathy during the pcriod 1988 1989 (Group 111)
The object of this study is to evaluate the
Signs and symptoms No. of cases %
clinical, laboratory findings and outcome of
D H F with CNS manifestations, or the so- Alteration of consciousness 92 9.3
called dengue encephalopathy, in patients Apathy 19 19.2
admitted to the Cipto Mangunkusumo Hospi- Somnolence 54 55.6
tal, Medical School, University of Indonesia, Stupor 14 14.1
in Jakarta at 3 different periods of time. Coma 5 5. I
Hepatoniegaly 62 62.6
Materials and Methods Hemorrhagic manifestations
Peleehiae 68 69.4
Three groups of cases with the diagnosis of Epistaxis 19 19.4
dengue encephalopathy admitted to the Cipto Hematcmcsis & melarna 54 55. I
I able 5 laboratory examinations in 98 c a m of dengue encephalopathy (Group 111)
Average Minimum Maximum
Hemoglobin (g d l . ) 11.4 4.4 18.2
tieniatocrit (vol 5 ) 36.0 20.0 52.9
I.eucoc)tes (pl) 6.300 3.ooo I5,XW
I’lateleta ( X 1.000) 82.7 4.0 368.0
Serum Sodium (niiiq 1.) 132.5 113.0 151.0
Serum Potassium ( m H q I.) 4.2 2.0 1.7
S.<;.O
‘1.(units) 357.x 25.0 1.x5o.o
S.G.P.1 (units) 299.0 10.0 I .785.0
No. of cases c/i
Primar!, infection 3 4.0
Secondary infection 31 43.0
f’resumptive secondary infeaton 25 34.6
Xot ewmined 39
Acta Paediair Jpn
Dengue encephalopathy (95) 353
based on the presence of CNS manifestations and 5-9 years age groups (87.5%), while a
in clinically proven D H F cases. CNS manifes- high number of cases in group 11 were in the
tations were abrupt onset of high fever, 5-9 years group (47.6%) (Table I). In all the
seizures, headache, vomiting, alteration of 98 cases of dengue encephalopathy we studied,
consciousness and neurological abnormalities. more were found in the 14 and 5-9 years age
Seizures that had been diagnosed previously groups.
as febrile convulsions were not included. The WHO (1980) has classified D H F
In all cases routine examinations of blood according to the severity of clinical symptoms
were performed such as hemoglobin content, into 4 grades as follows: grade 1, fever
white blood cells, hematocrit, blood platelets, accompanied by nonspecific constitutional
electrolytes, acid-base balance and serum symptoms, the only hemorrhagic manifestation
transaminases, and in most cases viral isolation being a positive tourniquet test; grade 11,
and hemagglutination inhibition tests. The manifestations of grade I plus spontaneous
results of the first 2 groups were taken from bleeding in skin or elsewhere; grade 111,
the investigation of Indra Roemaja Bahro- symptoms of circulatory failure such as rapid
emsyah, published in 1988 as a comparative and weak pulse, narrowing of pulse pressure
study. to 20 mmHg or less, or hypotension, with cold
any clammy skin or restlessness; and grade
Results IV, profound shock with undetectable blood
pressure and pulse.
There were 358 cases of D H F in the first In the 98 cases we studied, more than half
group, 745 in the second [lo] and 1,329 in the (77.6%) were classified as severe DHF (Table
third, out of which dengue encephalopathy 2).
was diagnosed in 33, 21 and 98 cases, or 9.2%, Evaluation of the clinical symptoms of the
2.5% and 7.3% respectively. 3 groups is shown in Table 3. Besides the
The age distribution of D H F cases in
group I showed a preponderance of the 1 4
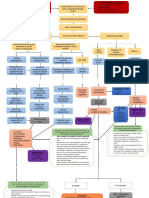
* Clinical & Laboratory Evidence of DHF;DSS
Table 6. Outcomc of 98 cases of dengue encephalopathy
(Group 111) * Abrupt Onset of Hyperpyrexia
* Alteration of Consciousness
No. of
cases
% * Headache, Vomiting
* Neurological Abnormalities
Death 51 52.0
* Normal CSF
Recovery 47 47.9
Neurologically normal 44 Fig. I : Diagnosis of dengue encephalopathy
h'eurologically abnormal 3
Hemiparesis 2 Patho physiology
Tetraparesis I
Total 98 la, All organs
~~ ~
Plasma leakage
Table 7. Most pronounced symptoms in fatal cases Hemorrhage
Symptoms No. of cases
Prolonged shock
Shock/ recurrent shock 26 -. Edema - Metabolic acidosis
Massive gastrointestinal bleeding 18 - Hemorrhage .- Hyponatremia
CNS manifestations 7 - Occlusion
Total 51
Fig. 2: Pathophysiology of dcngue encephalopathy
Vol. 34 No. 3 June 1992
354 (96) Hrndarro and Hudinegoro
classical manifestations of DHF such as The age distribution of DHF cases indicated
hepatomegaly and bleeding tendency, the a shift to the older age group [9, 101, which
most prominent symptoms in dengue encepha- can be explained by the hypothesis of
lopathy are alteration of consciousness and sccondary heterologous infection [ 121, which
convulsions. states that infection with other strains of
Out of the 98 cases of dengue encepha- dengue virus with clinical manifestations may
lopathy, 54 or 55.6(2) were in a state of occur after a latent period of 6 months to 5
somnolence. while 14 or 14.1% were in a state years. The shift to the older age group could
of stupor or coma. Other symptoms and signs also be related to the increase in the number
of D H F are shown in Table 4. Severe liver of seropositive reactions against dengue with
enlargement was found in 62 or 62.6% of increase of age. The finding of 4 serotypes of
cases; other symptoms were petechiae in 68 or dengue virus may also add to the risk of
69.4gf : profuse nose bleeding in 19 or 19.4%: secondary infection.
and profuse gastrointestinal bleeding in 54 or Cases of dengue encephalopathy have been
55.19; of cases. recorded since 1981, confirmed by viral
Laboratory evaluation of the cases of isolation and serological evidence [7- 91. Sero-
group 111 revealed mostly hemoconcentration type Den-3 was usually found with the severe
and thrombocytopenia. The maximum hemat- type of dengue infection, DHF grades 111 and
ocrit value was 52.9 vol% and the lowest IV. Such infections are usually complicated by
platelet count was 4.000 (Table 5). Low shock, profuse gastrointestinal bleeding and
sodium and potassium levels were also noted CNS involvement. and end in death.
in most cases. Serum transaminases were The diagnosis of dengue encephalopathy is
increased in 90 out of 98 cases (91.8%); they based on the clinical signs and symptoms of
were found to be normal in 8 cases only. DHF with cerebral manifestations such as are
Serologic hemaglutination inhibition antibody found in other types of encephalitis/encepha-
tests ( H I ) showed that out of 59 cases studied, lopathy: hyperpyrexia, alteration of conscious-
55 o r 77.6?+ had a secondary or presumptivc ness, headache, vomiting and neurological
secondary infection. In 39 cases, serologic HI abnormalities, with normal C S F (Fig. I).
evaluation was not done due to technical Headache was usually found as a complaint in
d iff cult ies. the older age group.
The mortality of the 98 cases of dengue Alteration of consciousness as one of the
encephalopathy in group 111 was 51. or 52%; most prominent symptoms of dengue en-
out of the 47 survivors, 3 were found to be cephalopathy was found in 100% of groups I
neurologically abnormal, with permanent and 11, and nearly 100% of group 111. That
hemiparesis or tetraparesis of the extremities alteration of consciousness was due to
(Table 6 ) . encephalopathy and not simply to DHF could
be concluded by the fact that it does not occur
Discussion even in the most severe cases of D H F , except
terminally.
The incidence of dengue encephalopathy in I n our study of 98 cases of group 111 of
thc 3 groups evaluated was 9.2%. 2.4% and confirmed DHF, the most pronounced symp-
7.3%. respectively. toms in the 51 fatal cases were not the CNS
The overall incidcnce in the 3 groups of symptoms per se, but massive gastrointestinal
dengue encephalopathy was 152 out of 2,441 bleeding and shock, although all showed CNS
DHF cases admitted, or 6.2%. symptoms which were less pronounced than
A high frequency of DHF with CNS the general symptoms. CNS symptoms seen
manifestations was found during 1988 1989. were alteration of consciousness, hyperpyrexia
which may be correlated with the five-yearly and convulsions (Table 7).
outbreak of dengue in 1988. The exact cause of death in the fatal cases
Acra Paediatr Jpn
Dengue encephalopathy (97) 355
could only be assumed clinically, since all but one case.
autopsy is nearly impossible to obtain due to In the gastrointestinal tract, focal petechiae
local beliefs and religion in our country. and submucosal bleeding were nearly always
CSF examination in 152 cases in the 3 found on autopsy, sometimes accompanied by
groups examined revealed normal values. profuse hematemesis and melaena.
Recently, more investigators have pointed
Pathophysiology of Dengue Encephalopathy out the important role of liver involvement in
The basic pathophysiology of DHF/ DSS DHF complicated by encephalopathy [9, 131.
is plasma leakage and abnormal hemostasis Symptoms of acute liver failure which may
leading to hypovolemic shock and hemor- induce CNS involvement are an unusually
rhage. Hemorrhage may occur in any organ of high increase of serum transaminases, pro-
the body such as the heart, brain, liver or longed plasma prothrombin time and jaundice.
gastrointestinal tract [9]. The pathophysiologic In 98 cases studied in group 111, more than
changes in the brain due to plasma leakage 90% showed an increase of serum trans-
and hemorrhage are brain edema and intra- aminases as a sign of liver failure.
cranial bleeding. Such bleeding may manifest Marked liver destruction was noted in all
itself as intracerebral, intraventricular, sub- nonfatal cases of dengue in the Nirnmannitya
dural or subarachnoid bleeding. study [9]. Liver failure was detected in cases of
The causes of abnormal plasma leakage Den-2 and Den-3 viral infection who died in
and abnormal hemostasis are cellular damage, the first days of admission [Ill. Other
direct or indirect, through an immunologic investigators suggested that liver failure may
process following secondary heterologous be potentiated by the intake of drugs during
infection or sequential dengue virus infection. the early stages of the illness, such as
The pathophysiology of dengue infection is paracetamol, acetosal or antiemetics; however,
set out in Fig. 2. An associated factor which others found no correlation between serum
may directly or indirectly induce organ acetaminophen/paracetamol serum content
involvement, including the brain, is dissemi- and the development of liver failure [14].
nated intravascular coagulation (DIC) [9]. The possibility of associated Reye’s syn-
DIC causes occlusion of the brain vessels drome as a cause of acute liver failure was
and/or tissue hemorrhage in addition to the also proposed [6, 81, but histopathological
already occurring brain hemorrhage and liver biopsy examination in dengue encepha-
edema which are common findings in autopsy lopathy revealed different changes from those
cases of dengue encephalopathy. seen in Reye’s syndrome [13]. Dengue anti-
Prolonged shock may induce hypoxia and bodies were found in nearly all virologically or
metabolic acidosis with the consequence of serologically confirmed cases of dengue en-
abnormal brain metabolism, leading to further cephalopathy [13]; in one case flavivirus
convulsions and alteration of consciousness. antigen was detected. Dengue antigen was
Decreased serum sodium content, a common detected in hepatocytes, Kupfer cells and
finding in hypovolemic shock, may induce occasionally in acute inflammatory cells.
convulsions, water intoxication and further Dengue virus was not found in liver cell
brain edema, especially if the serum sodium cultures. Extensive necrosis of hepatocytes
falls below 120 meq/l. was seen in massive or submassive distribution.
Multiple organ involvement including the The degeneration underlying the necrosis was
brain occurred more frequency with prolonged coagulative. Innis et a1 [I31 found dengue
shock and DIC. encephalopathy in about one third of cases of
In the heart, bleeding in various parts of primary dengue infection, mostly of serotypes
the myocardium may lead to ischemia, Den 1 and 3; contrary to the results of our
convulsions and coma. In the Nimmanitya study, where it occurs with secondary or pre-
series [9], myocardial bleeding was found in sumptive secondary infection with serotypes
Vol. 34 No. 3 June 1992
356 (98) Hcndarro and Hadinegoro
Den-2 and 3, of which Den-3 infection caused Conclusion
more severe clinical symptoms and a high
mortality rate. Many factors contribute t o the development
A study reported by Wei-June Chen et a1 of CNS pathology with signs and symptoms
in 1990 on C S F and sera of clinically and of brain involvement, or dengue encepha-
virologically diagnosed cases of dengue en- lopathy, as one of the most serious complica-
cephalopathy stated that dengue IgM was tions of DHF. Liver pathology or acute liver
detected in 14 out of 20 sera; in one of the failure is considered to be one of the main
positive specimens IgM could still be detected factors involved, as well as pathologic abnor-
up to 252 days after the onset of the illness malities in other organs of the body.
[14]. IgM was detected in all cases with CNS Previously recognized as a relatively rare
symptoms (4 cases); the IgM titer in the CSF complication of DHF, recent studies imply
was always lower than in the serum and faded that more cases of dengue encephalopathy will
within 1 month of the illness. be found in the future. More studies should be
All these studies of the possible pathophys- done, especially in the field of prevention and
iology of dengue encephalopathy suggest that management; for the mortality rate is still very
many factors may be associated with its high.
pathogenesis. That CNS manifestations were
due to encephalopathy and not encephalitis References
was evident from autopsy findings, since
I. Julmali, Sunarto, Gubler, D.J., Nalim S. et al.
macroscopic and microscopic examination of Epidemic dengue hemorrhagic fever in rural Indo-
the brain revealed no evidence of encephalitis. nesia 111. Entomological studies. Am. J. Trop. Med.
Hyg. 1979; 28: 717-21.
2. Technical Advisory Committee on Dengue Hemor-
Treatment and Management of Dengue rhagic Fever for the diagnosis, treatment and control
Encephalopathy of Dengue Hemorrhagic Fever. 2nd edn. Geneva.
Until now no satisfying standard treatment 1980; 7-9.
3. Suharyono W. Ten years dengue virus observation
or management has been proposed that will in Indonesia. Presented at the symposium on
ensure full recovery from the illness. Manage- dengue, hemorrhagic fever Jakarta, 1986.
ment is directed to relief of symptoms and is 4. Report from the Dept. of Health, Republic of
Indonesia, Directorate of infectious disease, 1984
similar to the basic standard management of (unpublished).
D H F DSS. 5. Tin U., Myo A,, Than N u Swe et al. Dengue
The main aim of treatment is t o reduce hemorrhagic fever with encephalitic symptoms.
Conference on dengue hemorrhagic fever: Current
plasma leakage by volume replacement and to knowledge. Seameo Trop. Med. Bangkok. 1976; I .
minimir.e the bleeding. 6. Kho L.K., Soemarmo, Wulur H. et al. Dengue
In prolonged shock, plasma is added. hemorrhagic fever accompanied by encephalopathy
in Jakarta. South Asian J. Trop. Med. Publ. Health
Blood or blood components such as packed 1981; 12: 85 7.
red cells are given to cases with profuse 7. Soemarmo, Muslim A. Nathin, Suharyono &
gastrointestinal bleeding. Vinai Suvatte [ 151 in Gubler D.J. Clinical observation on virologically
confirmed dengue hemorrhagic fever cases in
his study used additional exchange blood Jakarta. In Proc. International Conference on
transfusion, which yielded a higher survival Dengue/ Dengue Hemorrhagic Fever, Kuala I.um-
rate than in previous studies; the survival rate pur, 1983.
8. Wulur H., Djoharman S., Rumalean L. et al. Reye's
in his study was 72.2%. The use of corti- syndrome associated with dengue virus infection.
costeroid to reduce brain edema is still Dengue Newsletter. W.H.O. South East Asia
controversial, as brain edema is not the origin Western Pacific Region 1983; 9: 2 4 4 .
9. Nimmannitya ti., Thisyakorn & Hemsrichart N.
of dengue encephalopathy; but in some Dengue Hemorrhagic Fever with unusual manifes-
centres, corticosteroid is used for brain edema tations. Southeast Asian J. Trop. Med. Publ. Health
if there is no sign of acute gastrointestinal 1987; 18: 398 406.
10. George R. Ikngue hemorrhagic fever in Malaysia.
bleeding. South East Asia Trop. Med. Publ. Health 1987: 13.
278-83.
Acta Paediatr Jpn
Dengue encephalopathy (99) 357
1 1.lndra Roemaja Bahroemsyah. Clinical picture of Scientific Programme and Abstract Volume, 1990;
dengue hemorrhagic fever on children in Jakarta 64 5.
(1975-1986). Scientific paper to fulfill the require- 14. Wei-June Chen, Kao-Ping Huang & Ay-Huey Fang.
ment for qualification in general pediatrics. Post- Detection of 1gM Antibodies from Cerebrospinal
graduate faculty, University of Indonesia, Jakarta, Fluid and Sera of Dengue Fever Patients. lnterna-
1988. tional Symposium on Dengue and Dengue Haemor-
12. Halstead S.B., Marchette N.J.,& ORouke. Im- rhagic Fever. Scientific Programme and Abstract
munological enhanced dengue infection of mono- Volume, 1990; 77.
nuclear phagocytes. A mechanism which may 15. Vinai Suvatte, Chiresti Vajaradul & Tawee Laoha-
regulate disease severity. Asian J. Infect. Dis. 1978; pana. Liver Failure and Hepatic Encephalopathy in
2: 85-93. Dengue Hemorrhagic FeverlDengue Shock Syn-
13. Bruce L. lnnis, Khin Saw Aye Myint, Ananda drome: A correlation study with acetominophen
Nisalak et al. Liver Failure is one lmportant Cause usage. International Symposium on Dengue and
of Fatal Dengue Infection. lnternational Symposium Dengue Hemorrhagic Fever. Scientific Programme
on Dengue and Dengue Haemorrhagic Fever. and Abstract Volume, 1990; 63.
Vof. 34 No. 3 June 1992
You might also like
- Tropical Med Int Health - 2007 - Gulati - Atypical Manifestations of DengueDocument9 pagesTropical Med Int Health - 2007 - Gulati - Atypical Manifestations of DenguekosalNo ratings yet
- Pathogenesis of Hemorrhagic Due To Dengue Virus: Literature ReviewDocument5 pagesPathogenesis of Hemorrhagic Due To Dengue Virus: Literature Reviewfebyan yohanesNo ratings yet
- 1287-Article Text-3033-1-10-20170221Document15 pages1287-Article Text-3033-1-10-20170221andi ramdhanNo ratings yet
- Journal PNTD 0009666Document16 pagesJournal PNTD 0009666Rida Sophiatul KhofifahNo ratings yet
- Beyond Thrombocytopaenia, Haemorrhage and Shock: The Expanded Dengue SyndromeDocument12 pagesBeyond Thrombocytopaenia, Haemorrhage and Shock: The Expanded Dengue SyndromeLily FitrotunnisaNo ratings yet
- Dengue Case DiscussionDocument16 pagesDengue Case DiscussionCorinne Fatima de AsisNo ratings yet
- Viral MeningitisDocument11 pagesViral Meningitisjmichel2No ratings yet
- Kohil2021 Article ViralMeningitisAnOverviewDocument11 pagesKohil2021 Article ViralMeningitisAnOverviewwinnerfromparisNo ratings yet
- Assessment of Clinical and Hematological Profile IDocument5 pagesAssessment of Clinical and Hematological Profile IRugvedNo ratings yet
- Dengue 1Document14 pagesDengue 1FikaAuliaNo ratings yet
- DengueDocument52 pagesDenguenotchNo ratings yet
- Dengue Virus PathogenesisDocument29 pagesDengue Virus PathogenesisPon_Zi_cuteNo ratings yet
- TBM MedscapeDocument5 pagesTBM MedscapeAsnan Azis FatoniNo ratings yet
- DHF With AppDocument6 pagesDHF With AppputiridhaNo ratings yet
- Decee Marie T. Miranda Saint Mary'S University BSN Group6: Dengue Hemorrhagic FeverDocument5 pagesDecee Marie T. Miranda Saint Mary'S University BSN Group6: Dengue Hemorrhagic FeverJeff Mac Rae RamosNo ratings yet
- DENGUEDocument31 pagesDENGUEVanlal RemruatiNo ratings yet
- Journal Reading: Ade Cahyo Islami Dewinta Putri UtamiDocument17 pagesJournal Reading: Ade Cahyo Islami Dewinta Putri UtamiAde Cahyo IslamiNo ratings yet
- DIREFDocument6 pagesDIREFRahmongNo ratings yet
- DengueDocument2 pagesDengueElsa YuliusNo ratings yet
- Dengue and Chikungunya Infections in ChildrenDocument9 pagesDengue and Chikungunya Infections in ChildrenAl-Harits OctaNo ratings yet
- Dengue MedscapeDocument58 pagesDengue MedscapearuhulaminiNo ratings yet
- Dengue Virus PathogenesisDocument18 pagesDengue Virus Pathogenesisdian eko astariniNo ratings yet
- Dengue Patho 1Document18 pagesDengue Patho 1Rohan Walking TallNo ratings yet
- Streptococcus Suis Infection: Overview of Case Reports: in ThailandDocument6 pagesStreptococcus Suis Infection: Overview of Case Reports: in ThailandAram Dumnoen-ngamNo ratings yet
- 1471 2334 12 240 PDFDocument4 pages1471 2334 12 240 PDFBreno PontesNo ratings yet
- Dengue_activity_in_Puerto_Rico_during_an_interepidDocument10 pagesDengue_activity_in_Puerto_Rico_during_an_interepidCrónicos Jurisdicción J5No ratings yet
- Ijss Jan Oa12Document4 pagesIjss Jan Oa12Subhan Hasbi YudaNo ratings yet
- 1 PDFDocument22 pages1 PDFnursidiq10No ratings yet
- A Patient Dengue Hemorrhagic Fever With Spasms: Literature ReviewDocument6 pagesA Patient Dengue Hemorrhagic Fever With Spasms: Literature ReviewMarisajoineNo ratings yet
- Dengue Hemorrhagic FeverDocument74 pagesDengue Hemorrhagic FeverGERSON RYANTONo ratings yet
- Draft He DBDDocument32 pagesDraft He DBDTri Utami WahyuningsihNo ratings yet
- Incubation Period: 3 - 6 Days Some Cases May Reach 15Document3 pagesIncubation Period: 3 - 6 Days Some Cases May Reach 15Neil AlviarNo ratings yet
- Martina 2009Document18 pagesMartina 2009Valeria MedinaNo ratings yet
- Dengue FeverDocument38 pagesDengue FeverroshnajayesNo ratings yet
- 278 977 1 SMDocument2 pages278 977 1 SMMohamed MukhrizNo ratings yet
- Dengue MedscapeDocument36 pagesDengue Medscapejeanne_mbNo ratings yet
- To Study About DengueDocument46 pagesTo Study About Denguekanha kumarNo ratings yet
- Dengue Hemorrhagic FeverDocument3 pagesDengue Hemorrhagic FeverhelimpNo ratings yet
- Clinical Significance of Skin Rash in Dengue FeverDocument6 pagesClinical Significance of Skin Rash in Dengue FevernorabumantariNo ratings yet
- Yang LengkapDocument9 pagesYang LengkapauliyasaumaNo ratings yet
- Acetaminophen Is An Analgesic Used To Temporarily Relieve Minor Aches and PainsDocument7 pagesAcetaminophen Is An Analgesic Used To Temporarily Relieve Minor Aches and Painsmysterious galNo ratings yet
- Acetaminophen Is An Analgesic Used To Temporarily Relieve Minor Aches and PainsDocument7 pagesAcetaminophen Is An Analgesic Used To Temporarily Relieve Minor Aches and Painsmysterious galNo ratings yet
- Prune BellyDocument4 pagesPrune BellyErwin Chiquete, MD, PhDNo ratings yet
- Journal Medicine: The New EnglandDocument7 pagesJournal Medicine: The New EnglandThania Intan Sari WibawaNo ratings yet
- Clinical Experience of Dengue Fever in A Regional Teaching Hospital in Southern TaiwanDocument7 pagesClinical Experience of Dengue Fever in A Regional Teaching Hospital in Southern TaiwanYan Sheng HoNo ratings yet
- 14 1662 PDFDocument4 pages14 1662 PDFlukman fatkhulNo ratings yet
- Final SCRUB TYPHUS AS DIFFERENTIAL DIAGNOSIS OF COVIDDocument6 pagesFinal SCRUB TYPHUS AS DIFFERENTIAL DIAGNOSIS OF COVIDDr Gaurav SinghNo ratings yet
- Dengue Fever: "Dengue Fever" Redirects Here. For The Band of The Same Name, SeeDocument13 pagesDengue Fever: "Dengue Fever" Redirects Here. For The Band of The Same Name, SeeJaeni PringgowibowoNo ratings yet
- Case Report Angelin Putri GozaliDocument30 pagesCase Report Angelin Putri GozaliAngelinNo ratings yet
- Dengue Hemorrhagic Fever With Special Emphasis On ImmunopathogenesisDocument12 pagesDengue Hemorrhagic Fever With Special Emphasis On ImmunopathogenesisHadley AuliaNo ratings yet
- Zika - GBS ResumenDocument3 pagesZika - GBS Resumenjarvis rivasNo ratings yet
- Dengue: Cadawas, Daphne Gail S. BSN2-D5Document6 pagesDengue: Cadawas, Daphne Gail S. BSN2-D5Daphne Gail CadawasNo ratings yet
- Dengue Fever Out Break in Lahore, Pakistan. A Clinical Management ExperienceDocument4 pagesDengue Fever Out Break in Lahore, Pakistan. A Clinical Management ExperienceĂwăııs ÍshtıăqNo ratings yet
- A Systematic Review of Brain Imaging Findings in Neur - 2022 - International JouDocument9 pagesA Systematic Review of Brain Imaging Findings in Neur - 2022 - International JouJoanna LynNo ratings yet
- Assignment Dengue Fever (DF) in PakistanDocument7 pagesAssignment Dengue Fever (DF) in PakistanTauseef AhmadNo ratings yet
- Case Report: Fatal Staphylococcal Infection Following Classic Dengue FeverDocument4 pagesCase Report: Fatal Staphylococcal Infection Following Classic Dengue FeverRia Septi HarmiaNo ratings yet
- Ajayan 2013Document3 pagesAjayan 2013Dung TranNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Fast Facts: Multiple Sclerosis: A new era of disease modification and treatmentFrom EverandFast Facts: Multiple Sclerosis: A new era of disease modification and treatmentNo ratings yet
- Dental Assistant Resume TemplateDocument1 pageDental Assistant Resume TemplateShyam MurugesanNo ratings yet
- P.E Answer KeyDocument3 pagesP.E Answer KeyAustinly Bermejo67% (6)
- Cerebral Concussion - PathophyDocument4 pagesCerebral Concussion - PathophyFretzgine Lou ManuelNo ratings yet
- Megan Frano Current ResumeDocument1 pageMegan Frano Current Resumeapi-544878035No ratings yet
- Detailed Hospital Operational PlanDocument26 pagesDetailed Hospital Operational PlanKarol ZarorNo ratings yet
- Essay On ManDocument5 pagesEssay On ManZiaUlhaqNo ratings yet
- Tes Potensi Skolastik: Try Out Simulasi Program Persiapan LangsungDocument4 pagesTes Potensi Skolastik: Try Out Simulasi Program Persiapan LangsungRikhwanul LukmanNo ratings yet
- Descarga VaginalDocument8 pagesDescarga VaginalMELVYN HAROLD CHAVEZ MAURICIONo ratings yet
- 10 Ways STDs Impact Women Differently From MenDocument1 page10 Ways STDs Impact Women Differently From MenJuan Francisco Pintado MejiaNo ratings yet
- Infectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedDocument1 pageInfectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedJoshua MendozaNo ratings yet
- The Safe & Effective Care EnvironmentDocument140 pagesThe Safe & Effective Care EnvironmentMoreiyamNo ratings yet
- Abortion: Violation of Human Rights in The PhilippinesDocument14 pagesAbortion: Violation of Human Rights in The PhilippinesAngelica AlejandroNo ratings yet
- Chapter 7: Health and Biotechnology: Microorganisms: Disease and FoodDocument31 pagesChapter 7: Health and Biotechnology: Microorganisms: Disease and FoodTendy WatoNo ratings yet
- CoronaDocument2 pagesCoronaArgie Joy Marie AmpolNo ratings yet
- 1.) Generic Name: Gabapentin Brand Name Classification Dosage Route and Frequency Mechanism of ActionDocument15 pages1.) Generic Name: Gabapentin Brand Name Classification Dosage Route and Frequency Mechanism of ActionTyron ChuaNo ratings yet
- Mammography Sas 10Document11 pagesMammography Sas 10faith mari madrilejosNo ratings yet
- MSDS - Valve LubricantDocument6 pagesMSDS - Valve LubricantFirstyan Dhika AldaniNo ratings yet
- GM FoodsDocument7 pagesGM Foodsapi-276860380No ratings yet
- Separation Anxiety PDFDocument27 pagesSeparation Anxiety PDFDiego M LisNo ratings yet
- LFA Houston DoctorsDocument2 pagesLFA Houston Doctorsjanel882No ratings yet
- Flowchart Covid 19 ResponseDocument2 pagesFlowchart Covid 19 ResponseAlberto SarmientoNo ratings yet
- Updated 1212Document58 pagesUpdated 1212point clickNo ratings yet
- People Risk Infographics MercerDocument1 pagePeople Risk Infographics MercerChanakya NitiNo ratings yet
- Community Assessment On Antibiotic Medication Compliance in Barangay GuizoDocument67 pagesCommunity Assessment On Antibiotic Medication Compliance in Barangay GuizoJeanny Mae NgujoNo ratings yet
- Acute Mesenteric IschemiaDocument46 pagesAcute Mesenteric Ischemiashita febrianaNo ratings yet
- 11 Health Benefits of Grape Seed Extract - Health BenefitsDocument3 pages11 Health Benefits of Grape Seed Extract - Health BenefitsCheryl WestNo ratings yet
- Characteristics of Community HealthDocument2 pagesCharacteristics of Community HealthRichard Balili100% (1)
- 2015 - Swanson - How To Practice Evidence-Based MedicineDocument14 pages2015 - Swanson - How To Practice Evidence-Based MedicineAudrey VivierNo ratings yet
- Chorioamnionitis by DR Simon ByonanuweDocument31 pagesChorioamnionitis by DR Simon ByonanuweDr Simon ByonanuweNo ratings yet
- Antimicrobial Susceptibility Testing PDFDocument19 pagesAntimicrobial Susceptibility Testing PDFdatitoxNo ratings yet