Professional Documents
Culture Documents
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Uploaded by
dekatria 2020Copyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- ENACb 1Document166 pagesENACb 1DarrylpnzNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- BBS Book (PT 14) NeglyDocument7 pagesBBS Book (PT 14) Neglyapi-3871208No ratings yet
- Leg Support Calculation PDFDocument2 pagesLeg Support Calculation PDFSanjay MoreNo ratings yet
- Gear Trains: 8.1. Angular Velocity RatioDocument16 pagesGear Trains: 8.1. Angular Velocity RatioaddisudagneNo ratings yet
- He Is A Chocolate Lover: Kamaladevi RengasamyDocument4 pagesHe Is A Chocolate Lover: Kamaladevi RengasamyKamala DeviNo ratings yet
- Air Track Gizmo - ExploreLearningDocument4 pagesAir Track Gizmo - ExploreLearningJeremy Gomez-RojasNo ratings yet
- Allotrope Partners Indonesia Renewable Energy Project AssociateDocument2 pagesAllotrope Partners Indonesia Renewable Energy Project AssociateRizal ZulkarnaenNo ratings yet
- IllithidDocument5 pagesIllithidMattia La RosaNo ratings yet
- South Africa Hard Copy Lit 2Document20 pagesSouth Africa Hard Copy Lit 2Jennifer Española BernalNo ratings yet
- EQUILIBRIUMDocument1 pageEQUILIBRIUMMohammed IliasNo ratings yet
- 3B Reactions of Alcohols and ThiolsDocument27 pages3B Reactions of Alcohols and ThiolsAnloraine GonzalesNo ratings yet
- Jayvee Dime,,,,project in Physics Light and SoundDocument25 pagesJayvee Dime,,,,project in Physics Light and SoundJayvee DimeNo ratings yet
- Structural Identification & Poc-1: Topic Page NoDocument35 pagesStructural Identification & Poc-1: Topic Page Nosiddansh100% (1)
- Arthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832Document318 pagesArthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832cengizozakinciNo ratings yet
- Da0bl7mb6d0 Rev DDocument44 pagesDa0bl7mb6d0 Rev DFerreira da CunhaNo ratings yet
- Snag SummmariesDocument171 pagesSnag Summmarieslaltu adgiriNo ratings yet
- Lecture 7 - Synchronous Generators 7 PDFDocument28 pagesLecture 7 - Synchronous Generators 7 PDFDorwinNeroNo ratings yet
- Relative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationDocument17 pagesRelative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationNguyễn Huy CườngNo ratings yet
- Jack and The Beanstalk Treatment-2Document10 pagesJack and The Beanstalk Treatment-2api-668257195No ratings yet
- Earth Quake DesignDocument13 pagesEarth Quake DesignRanie boy CabanillaNo ratings yet
- Form 67 Delivery Unloading and Loading of Materials and PlantDocument6 pagesForm 67 Delivery Unloading and Loading of Materials and PlantMohamed MedhioubNo ratings yet
- Unit-6 Patterns of Industrialisation PDFDocument12 pagesUnit-6 Patterns of Industrialisation PDFNavdeep SinghNo ratings yet
- Synchronous Generators: Instructional ObjectivesDocument18 pagesSynchronous Generators: Instructional Objectivessanthosh2009No ratings yet
- HP Deskjet D1600 Printer SeriesDocument13 pagesHP Deskjet D1600 Printer SeriesRizki JuliadiNo ratings yet
- Schiavi Enc Met Page015Document1 pageSchiavi Enc Met Page015Adel AdelNo ratings yet
- Transport Phenomena: τ =μ dv dyDocument2 pagesTransport Phenomena: τ =μ dv dySYED ASGHAR ALI SULTANNo ratings yet
- Annual Report 2014 PDFDocument153 pagesAnnual Report 2014 PDFகோகுல் இராNo ratings yet
- Fetomaternal Hemorrhage (FMH), An Update Review of LiteratureDocument35 pagesFetomaternal Hemorrhage (FMH), An Update Review of LiteratureEugenia Jeniffer JNo ratings yet
- Macro Chapter 7Document12 pagesMacro Chapter 7Mary Jane PelaezNo ratings yet
- X PPT CH 12 ElectricityDocument12 pagesX PPT CH 12 ElectricityAakriti100% (1)
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Uploaded by
dekatria 2020Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Non-Alcoholic Fatty Liver Disease (NAFLD) : A Review of Epidemiology, Risk Factors, Diagnosis and Management
Uploaded by
dekatria 2020Copyright:
Available Formats
Non-alcoholic fatty liver disease (NAFLD): a review of
epidemiology, risk factors, diagnosis and management
Authors:
Dr Tony (Dazhong) Huang MD, BMed 1,2
Dr Jason Behary, MBBS, FRACP 1,2
A/Prof Amany Zekry, MBBS, PhD, FRACP 1,2
Accepted Article
Institutional Affiliation:
1. Department of Gastroenterology and Hepatology, St George Hospital, Kogarah, Sydney.
2. St George and Sutherland Clinical School, UNSW Sydney
Correspondence:
Dr Tony (Dazhong) Huang
Address: 1202/5 Rockdale Plaza Drive, Rockdale NSW 2216
Phone: 0450571046
Email: Dazhong.Huang@health.nsw.gov.au
Acknowledgement: nil industrial links, funding or affiliations applicable
Abstract
Due to the rising prevalence of obesity and type II diabetes mellitus, non-alcoholic fatty liver
disease (NAFLD) is becoming the leading cause of chronic liver disease in the Western
world. In some patients, simple steatosis can result in non-alcoholic steatohepatitis (NASH)
which over time can lead to liver cirrhosis and its associated sequalae, including
hepatocellular carcinoma (HCC). Early identification and management of patients at risk with
intensive dietary and lifestyle modification are essential to prevent the development of
advanced liver disease and its complications. In this review, we will discuss the
epidemiology of NAFLD, pathogenesis, diagnosis, management and surveillance strategies
to offset the morbidity and mortality of this disease, as well as liver and non-liver related
complications.
Key words: Non-alcoholic fatty liver disease (NAFLD), Non-alcoholic steatohepatitis (NASH),
liver cirrhosis, hepatocellular carcinoma (HCC).
This article has been accepted for publication and undergone full peer review but has not been
through the copyediting, typesetting, pagination and proofreading process which may lead to
differences between this version and the Version of Record. Please cite this article as doi:
10.1111/imj.14709
This article is protected by copyright. All rights reserved.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a clinicopathological spectrum of liver disease
ranging from isolated steatosis, non-alcoholic steatohepatitis (NASH) and fibrosis through to
cirrhosis. NAFLD is defined as the development of steatosis in >5% of hepatocytes identified
either histologically or radiologically, in the absence of secondary causes such as viral
hepatitis, alcohol or hereditary liver diseases1. Due to rapidly escalating rates of obesity and
type II diabetes mellitus, NAFLD is now the most common form of chronic liver disease in
developed countries, placing significant burden on healthcare systems worldwide2.
Epidemiology
Accepted Article
NAFLD is estimated to be by far the most common cause of chronic liver disease in
Australia, as highlighted in Table 1. Data on the prevalence of NAFLD in Australia is limited
due to lack of population-based studies but is likely in keeping with global estimates ranging
between 25% and up to 40% in high-risk groups2.
Table 1: Estimated prevalence of chronic liver disease in Australia. Adapted from GESA
3
(Gastroenterology Society of Australia) Full article obtained at www.gesa.org.au
2012 2030
Males
Females Total Males Females Total
Hepatitis A 148 135 284 180 164 344
Hepatitis B 105,555 105,535 211,089 131,782 131,061 262842
Hepatitis C 185,468 121,572 307,040 251,391 162,887 414,278
NAFLD 2,713,372 2,825,305 5,538,677 3,566,969 3,693,619 7,260,588
Primary Liver 1,064 387 1,451 1,652 601 2,253
Cancer
Alcoholic Liver 4,605 1,598 6,203 5,816 2,008 7,824
Disease
Primary Biliary 32 389 433 63 553 616
Cholangitis
Primary Sclerosing 554 318 872 748 425 1,174
Cholangitis
Hereditary 56,343 56,894 113,237 70,000 71,421 142,421
Haemachromatosis
Total 3,067,152 3,112,133 6,179,285 4,029,600 4,062,739 8,092,339
The rising incidence of NAFLD worldwide is in part driven by surging rates of obesity and
type II diabetes mellitus. Alarmingly, the Australian National Health Survey conducted in
2017-2018 reported that 66.9% of Australians over 18 years of age were overweight or
obese, increasing from 56.2% in 1995. The prevalence of type II diabetes mellitus in
Australia similarly increased from 3.3% in 2001 to 4.9% in 2017-184. The Organisation for
Economic Cooperation and Development (OECD) reported similar rates of obesity in other
Western countries such as the United States (38.2%), New Zealand (30.7%) and United
Kingdom (27%)5.
NAFLD is more common in men, and disease prevalence rises with advancing age.
However, there is also emerging evidence of NAFLD developing in obese children and
adolescents which carry higher rates of progression to cirrhosis, development of
hepatocellular carcinoma (HCC), need for transplantation and mortality compared to
adults6,7.
This article is protected by copyright. All rights reserved.
Pathophysiology and the Metabolic Syndrome
NAFLD is a complex spectrum of disease arising from interrelated environmental and
genetic risk factors. It is closely associated with the metabolic syndrome; a cluster of risk
factors for end-organ vascular disease and type II diabetes mellitus8. Table 2 summarises
the characteristics of the metabolic syndrome as proposed by the American Heart
Association.
Accepted Article
Table 2: Components of the Metabolic Syndrome and their measurement threshold as defined by
8
the American Heart Association. Adapted from Beilby et al
Risk Factors Measurement Threshold
(need at least three)
Central obesity Waist circumference >102cm in men, >88cm in women
Hypertriglyceridemia >1.7mmol/L or on drug treatment
Reduced HDL-C <1.0mmol/L in men, <1.3mmol/L in women
Hypertension >130 systolic or >85 diastolic BP or on drug treatment
Impaired fasting glucose >5.5mmol/L fasting glucose or on drug treatment
NAFLD most likely occurs in the context of abnormal metabolic processes in genetically
susceptible individuals9 (Figure 1). The number of metabolic risk factors present directly
correlate with increased risk and severity of NAFLD10. This was shown in a cross-sectional
study by Yang et al., which identified the presence of at least three metabolic risk factors in
3.2%, 20% and 51.4% of patients with normal, mild to moderate and severe NAFLD
respectively, graded using a sonographic scoring system called the US-Fatty Liver Indicator
(US-FLI)10.
This article is protected by copyright. All rights reserved.
Accepted Article
Figure 1: Diagram of processes contributing to pathogenesis of NAFLD and progression to cirrhosis.
11
Adapted from Fiorucci et al .
The pathophysiology of NAFLD is complex, likely involving multiple concurrent mechanisms.
One of the liver’s many functions is to produce both fasting plasma glucose through
gluconeogenesis and very low density lipoprotein (VLDL), which contains most of the
measurable serum triglyceride12. In healthy individuals, insulin suppresses free fatty acid
(FFA) production from peripheral adipose tissue and de novo hepatic VLDL production. As
illustrated in Figure 2., obese individuals have increased visceral adipose tissue leading to,
among numerous other deleterious effects, insulin resistance and subsequent
hyperinsulinemia, which increases circulating FFAs, hepatic VLDL production and
gluconeogenesis1. Visceral adiposity also increases portal blood FFAs that drains into the
liver. The combination of these mechanisms result in excessive hepatic steatosis12.
Progressive steatosis may result in hepatocellular lipotoxicity via cellular and organelle
oxidative stress; endoplasmic reticulum stress and mitochondrial dysfunction drives reactive
oxygen species production, leading to hepatic ballooning, inflammation and cell death
through apoptosis13. This gives rise to non-alcoholic steatohepatitis (NASH), where pro-
inflammatory cytokine production causes infiltration of macrophages into the liver and
activation of Kupffer and hepatic stellate cells (HSCs). Kupffer cells are specialised hepatic
macrophages that further recruit peripheral macrophages, T cells and neutrophils to
upregulate the hepatoxicity seen in NASH13. HSCs are myofibroblasts in the liver which
proliferate in response to TNF-alpha, IL-1beta and other proinflammatory cytokines to
secrete extracellular matrix proteins leading to progressive fibrosis and ultimately cirrhosis13.
This article is protected by copyright. All rights reserved.
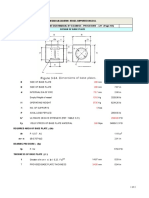
Insulin resistance
Increased
VLDL secretion
insulin / glucose level
Adipose tissue
Increased
De novo Lipogenesis
Increased Plasma FFA
Accepted Article
Increased FFA Increased TG synthesis
Excess Dietary fat
Increased β-oxidation TG accumulation
Steatosis
HEPATOCYTE
Figure 2: Diagram illustrating processes leading to triglyceride accumulation in hepatocytes
57
leading to steatosis. Adapted from Paschos et al .
The role of the gut microbiome is increasingly recognised in metabolic disease9. Disruption of
the balance of gut microbes, referred to as dysbiosis, is thought to be a contributory factor in
NAFLD14. It is hypothesised that dysbiosis in NAFLD results in changes in the peripheral and
intrahepatic immune response that may contribute to development of NASH. Other
mechanisms by which the microbiota may contribute to NAFLD include disruption of gut
epithelial permeability, leading to translocation of bacterial antigens such as
lipopolysaccharides into portal circulation where they bind to toll-like receptor 4 (TLR-4) and
other co-receptors in the liver, triggering a downstream hepatic inflammatory cascade15.
Dysbiosis may also alter intestinal short chain fatty acid (SCFA) and bile acid profiles which
may contribute to steatosis and NASH14. A consistent microbiota signature to characterise
NAFLD is yet to be determined and is the subject of ongoing research.
Genetic and epigenetic factors also play an important role in the pathogenesis of NAFLD,
with heritability being estimated to be 20-70%16. Several genome-wide studies (GWAS) have
found presence of numerous single-nucleotide polymorphisms (SNPs) of genes such as the
patatin-like phospholipase domain containing protein-3 (PNPLA3) to independently correlate
with NAFLD disease severity, progression and risk of HCC16. Variants in the Apolipoprotein
C3 gene also increases risk of NAFLD through loss of normal lipoprotein lipase activity in
VLDL17.
Diagnosis
Diagnosis of NAFLD relies on identifying hepatic steatosis, which in most cases can be
achieved noninvasively. While not all cases of hepatic steatosis will progress, early detection
of NASH and advanced liver fibrosis is nonetheless important as these patients are at risk of
developing liver cirrhosis and its associated complications such as HCC18. However, early
detection can be difficult as patients are often asymptomatic at time of diagnosis. Serum
markers of liver function such as aminotransferases (ALT and AST) and ferritin can be
elevated in NASH but are not sensitive nor specific for progression of fibrosis or
development of advanced liver disease19.
This article is protected by copyright. All rights reserved.
In clinical practice, most diagnoses of NAFLD are made radiologically. The most common
imaging method for diagnosis is abdominal ultrasound which can sonographically
demonstrate fatty infiltration of the liver20. The sensitivity and specificity of ultrasound is
approximately 85% and 90% respectively, but reliability is operator-dependent and limited in
patients with central obesity20. Vibration controlled transient elastography such as Fibroscan
or ARFI (Acoustic Radiation Force Impulse) can be used to sonographically quantify the
degree of fibrosis to aid in early detection of cirrhosis but are less reliable in those with
intermediate fibrosis severity (F2, F3). An alternative diagnostic method is magnetic
resonance spectroscopy (MRS), which is a magnetic resonance imaging (MRI) modality that
allows quantification of hepatic steatosis and is highly sensitive for small amounts of isolated
21
steatosis but this modality is not readily available or cost effective .
Accepted Article
The gold standard for diagnosis and quantification of hepatic fibrosis in patients with NAFLD
is liver biopsy. Percutaneous or transjugular liver biopsy are invasive procedures with low,
but not negligible complication rates. Bravo et al reported a hospitalisation rate of up to 1-3%
following percutaneous liver biopsy with complications such as pain, vasovagal hypotension,
and less commonly bleeding, sepsis and injury to surrounding organs22. For this reason,
non-invasive methods are preferred as first line investigations. Liver biopsy is ultimately
reserved for patients in whom further clarification of the aetiology of chronic liver disease is
required or when the degree of liver fibrosis or a diagnosis of cirrhosis cannot be clearly
ascertained with non-invasive measures23. NASH is characterised by histological detection
of steatosis, hepatocyte ballooning and lobular inflammation with or without fibrosis23. The
severity of fibrosis can be histologically graded from F1 (mild) to F4 (cirrhosis).
Several non-invasive scoring assessments have been developed to quantify the degree of
hepatic fibrosis as part of risk stratification for cirrhosis and/or HCC. These include the
NAFLD fibrosis score, which incorporates non-invasive clinical and laboratory data such as
age, BMI, glucose levels, AST/ALT ratio, platelet count and albumin. A validation study by
Angulo et al showed a low cut-off score (-1.455) had a high negative predictive value of 93%
in excluding advanced fibrosis, while high cut-off score (0.676) had high positive predictive
value for advanced fibrosis (90%), thereby often negating the need for liver biopsy24. Other
scoring systems include the Fib-4 score (age, AST, ALT, platelets), AST/ALT ratio, APRI
(AST/platelet ratio) and the BARD score (BMI, AST, ALT, diabetes)25.
This article is protected by copyright. All rights reserved.
Management of NAFLD
Diet and lifestyle modification
General principles for management of NAFLD involve early identification of those at risk,
modification of metabolic risk factors, monitoring for progression to advanced liver disease
and preventing concurrent liver injury by other factors such as alcohol. In most cases, weight
loss through dietary modification and exercise is the cornerstone of management26. In
particular, intensive 12-month dietitian-lead lifestyle modification has been shown to be more
effective than standard care for weight loss and achieving remission of NAFLD (64% vs
20%) 27. Musso et al. demonstrated in their meta-analysis that weight loss of >7% body
weight resulted in histological improvement on serial liver biopsies28.
Accepted Article
Table 3: Components of the Mediterranean Diet and recommended serving sizes, adapted from
29
Anania et al .
Components Consumption Rich In
Fresh fruits Daily, 3 servings Vitamin C, polyphenols,
carotenoids, fibres
Vegetables Daily, 6 servings Vitamin C, polyphenols, ꞷ-
3-PUFA, carotenoids, fibres
Olive Oil Daily MUFA, polyphenols
Unrefined cereals Daily, 8 servings Polyphenols, fibres
Nuts Weekly Polyphenols, ꞷ-3-PUFA,
fibres
Legumes Weekly, ≥3 servings Polyphenols, fibres
Fish Weekly, 5-6 servings ꞷ-3-PUFA
Red wine Weekly, ≥7 glasses Polyphenols
The Mediterranean diet, with its components demonstrated in Table 3, has been
demonstrated to be efficacious in reducing risk of metabolic syndrome through exerting anti-
inflammatory, antioxidant effects and lipid-lowering effects, as well as improving microbiota
dysbiosis29. In a controlled intervention study performed by Kontogianni et al., adherence to
Mediterranean diet in NAFLD was found to be associated with lower aminotransferase
levels, insulin resistance, severity of hepatic steatosis on biopsy and overall risk of
developing NASH30.
Pharmacotherapy
In many instances, maintenance of weight loss through lifestyle interventions alone is not
sustainable. Pharmacological therapy can be considered in those who fail to achieve
meaningful weight loss with lifestyle measures alone. Studies, however, have conflicting
results for the efficacy and safety of pharmacotherapy in NASH. In addition, management
guidelines vary in their recommendations for these therapies. Therefore, pharmacotherapy
should be considered on an individual basis. EASL (European Association for Study of the
Liver) guidelines state indications for consideration of pharmacological therapy include those
with progressive NASH with bridging fibrosis and cirrhosis (>F2), early stage NASH at high
risk for disease progression (age >50, multiple metabolic risk factors, elevated ALT), and
those with active NASH with high necro-inflammatory markers31.
For those with diabetes mellitus, pioglitazone and liraglutide have been shown to improve
insulin sensitivity, aminotransferase levels and degree of steatohepatitis26, 28. For those with
biopsy-proven NASH and fibrosis stage >2 who do not have diabetes, vitamin E can be used
This article is protected by copyright. All rights reserved.
to improve steatosis, inflammation and resolution of NASH through its antioxidant effects,
but long-term safety is unclear with some studies showing high dose vitamin E to increase
all-cause mortality27. Lassailly et al. also reports association of vitamin E and pioglitazone
with increased risk of prostate and bladder cancer respectively32. Metformin and statins,
while important in management of diabetes and hypercholesterolemia, have not been shown
to independently improve outcomes in NAFLD26. Current trials are underway for novel
therapeutic approaches to inhibit hepatotoxicity and fibrosis at several of the steps in the
pathogenesis of NASH. These are outlined in Table 4 below.
Table 4: Summary of new NASH treatments currently undergoing clinical trials. Adapted from
Accepted Article
11
Fiorucci et al .
Class Agents Mechanism of action in Stage of research/results
treating NAFLD/NASH
Anti-diabetic GLP1 analogues Induce insulin Undergoing clinical trials in NASH
agents e.g. semaglutide, biosynthesis and
exenatide release from
DPP4 inhibitors pancreatic B cells,
e.g. sitagliptin improves insulin
sensitivity
PPARα/δ Modulate lipid beta- Phase 2b RCT showed
agonists e.g. oxidation, insulin improvement in NASH vs placebo
elafibranor secretion and in those with high NAFLD disease
sensitivity in liver activity score
SGLT1 and 2 Reduce intestinal and LIK066 currently evaluated in
inhibitors e.g. renal glucose Phase 2 trial
LIK066 (dual reabsorption Ipraglifozin shown efficacy in
action), small clinical trials, currently
ipraglifozin approaching Phase 2
(selective SGLT2)
Bile-acid Selective FXR Regulates major steps Phase 2 trial in biopsy proven
derivatives agonists e.g. in lipid and glucose non-cirrhotic NASH show
obeticholic acid metabolism, and histological improvement, Phase
(OCA) inflammation and 3 trial ongoing. Limited by
fibrosis in significant side effects and risk of
enterohepatic tissues liver decompensation
Fibroblast FGF19 and 21 FGF19 reduces bile Phase 2 trial of FGF19 analogue
Growth acid synthesis and showed reduced hepatic steatosis
Factors (FGF) gluconeogenesis and in liver biopsy confirmed NASH
activation of glycogen
storage. Preclinical studies of FGF21
pegylated analogues showed
FGF21 stimulates reduced body weigh an improved
glucose uptake by glucose tolerance in rodent
adipocytes and models, lacking safety data
ameliorates insulin
sensitivity
Anti-lipid Stearoyl-CoA Inhibits catalysis of Multicentre Phase 2b trial
agents desaturase (SCD) rate limiting step in ongoing; initial phase 3-month
-1 inhibitors e.g. synthesis of study showed reduction in hepatic
aramchol monounsaturated fatty steatosis on MRI
acids – decreased liver
injury in response to
high fat diet and
decreased insulin
This article is protected by copyright. All rights reserved.
resistance
Anti- CCR2/CCR5 Attenuates liver and Phase 2b trial in NASH did not
inflammatory/ antagonist e.g. kidney fibrosis meet primary endpoint vs placebo
fibrotic Cenicriviroc but secondary endpoints of
agents amelioration of combined stages
2 and 3 liver fibrosis and
hepatocyte ballooning in
comparison to baseline histology
Galectin-3 Inhibition of Galectin – Phase 2b trial in NASH with
inhibitor e.g. GR- vital protein in liver fibrosis/cirrhosis – interim analysis
MD-02 fibrinogenesis suggests treating cirrhotic patients
significantly improves portal
Accepted Article
pressure and reduces risk of
oesophageal varices
Hormone β-selective Diminishes hepatic Phase trial in biopsy-proven
modulating Thyroid Hormone lipid accumulation NASH, MGL-3196 met all primary
agents Receptor agonists through thyroid endpoints or reducing hepatic
e.g. MGL-3196 hormone receptor steatosis and fibrosis
action in liver
Microbiome- Probiotic/faecal Improvement of Beneficial effects in rodent
modulating microbial intestinal dysbiosis models of NASH, several ongoing
treatment transplantation trials
Macrolide Solithromycin currently in Phase 2
antibiotics e.g. trial
solithromycin
Bariatric surgery
Bariatric surgery is emerging as an effective option in those with severe obesity (BMI ≥40 or
≥35 with co-morbidities) unresponsive to lifestyle and pharmacological measures32.
Indications and contraindications for bariatric surgery are listed in Table 5. Lassailly et al.
reported bariatric surgery to be effective in long term maintenance of weight loss with an
average 14-25% weight loss observed 10 years after surgery, along with improvement in
hyperlipidaemia, insulin resistance and risk of cardiovascular events32. Bariatric surgery has
also been demonstrated to reduce steatosis, inflammation and fibrosis in NAFLD; a
prospective cohort study by Lassailly et al found resolution of NASH in 85.4% of cases one
year following surgery, with significant improvement in all histological features such as
hepatocellular ballooning, lobular inflammation and fibrosis32. Similarly, a meta-analysis by
Lee et al. demonstrated complete resolution of histological features of NASH in 66% of
patients undergoing bariatric surgery, with 40% demonstrating resolution of fibrosis33.
Restrictive procedures such as gastric banding and sleeve gastrectomy directly affect weight
loss by promoting satiety and caloric restriction, as well as reducing secretion of ghrelin, an
orexigenic hormone34. Gastric bypass procedures such as Roux-En-Y, in addition to caloric
restriction, have the additional effects of greater glycaemic control with increased post-
prandial secretion of glucagon-like peptide-1 (GLP-1) and improved hepatic insulin
sensitivity35. The benefits of bariatric surgery must, however, be balanced against high-
anaesthetic risk as seen patients with NAFLD who often have cardiovascular disease. Peri-
operative and post-operative complication rates of bariatric surgery range from 13% in
gastric banding and sleeve gastrectomy to 21% in Roux-En-Y36. Additionally, risk of weight
gain relapse can occur postoperatively with poor diet and sedentary lifestyle. Studies thus far
have also not demonstrated an improvement in liver-related mortality after bariatric surgery.
This article is protected by copyright. All rights reserved.
Table 5: Indications and contraindications for bariatric surgery. Adapted from Lassailly et al.32
Indications Contraindications
BMI >40 without comorbid disease Cardiovascular risk factor control in absence
of obesity (BMI >30)
BMI 35 – 40 with at least one serious co- Other medical or psychiatric conditions
morbidity including precluding surgery
Diabetes mellitus Untreated major
Obstructive Sleep Apnoea depression/psychosis
Accepted Article
Hypertension Uncontrolled eating disorders
Hyperlipidaemia Current drug/alcohol abuse
Obesity hypoventilation syndrome Severe cardiac disease with high
NAFLD/NASH anaesthetic surgical risk
Gastroesophageal reflux disease Severe coagulopathy
Asthma Inability to comply with nutritional
Pseudotumour cerebri requirements
Severe arthritis
Impaired quality of life
Disqualification from other surgeries
due to obesity
BMI 30 – 35 with one or more of the
following:
Uncontrollable diabetes mellitus
Metabolic syndrome
Just as with other causes of chronic liver disease, liver transplantation is the most definitive
treatment option in carefully selected patients with NAFLD-related end stage liver disease
and/or HCC. In general, patients with cirrhosis are considered candidates for transplantation
once the MELD (Model for End-stage Liver Disease) is ≥15, though referral to a transplant
team is often made for pre-transplantation evaluation at ≥10. Patients with HCC are also
carefully selected for transplantation based on either the Milan Criteria or the University of
California, San Francisco (UCSF) scoring system taking into account tumour size, number
and presence of vascular invasion or metastases37. As mentioned above, NAFLD-related
cirrhosis and HCC is rapidly becoming the most common indication for liver transplant due to
the rise in prevalence of NAFLD/NASH and the stabilisation of HCV-related cirrhosis due to
highly effective direct-acting antiviral treatment38. Pais et al. reports an increase of 170% in
the incidence of NAFLD patients referred for transplant from 2006 to 2016, compared to
increases of 15% and 45% in HCV and alcoholic cirrhosis respectively39.
Liver transplantation
Patients with NAFLD often present a challenge for transplantation due to their elevated BMI
and metabolic risk40. Intraoperatively, obesity and diabetes is associated with prolonged
operative time, hospital stay, and risk of early post-operative infection and cardiovascular
events41. Fortunately, long-term graft survival has not been shown to differ in NAFLD
compared to other causes of liver disease42. Another important consideration is that
transplantation does not reverse the underlying metabolic processing driving the
development of hepatic steatosis. A cohort study by Malik et al. of those transplanted for
NASH cirrhosis reported recurrence of NAFLD in 70% at 65 weeks post-transplant with 24%
This article is protected by copyright. All rights reserved.
having features of NASH43. Anti-rejection drugs such as tacrolimus, corticosteroids and
mTOR inhibitors can also worsen or result in de novo metabolic syndrome 39.
Complications of NAFLD
Liver cirrhosis
As mentioned previously, the phenotypes of NAFLD range from simple steatosis, NASH to
advanced liver disease. The prevalence of NASH in NAFLD varies significantly in the
,
literature from 10-20% up to 59% based on studies that performed liver biopsies 44 . With
progressive fibrosis, an estimated 25% of those with NASH progress to cirrhosis, and a
smaller proportion to end stage liver disease and HCC. Liver-related complications are the
Accepted Article
third highest cause of death in NAFLD (10%) behind cardiovascular disease (48%) and
extrahepatic malignancy (22%)45.
NAFLD is rapidly emerging as a major cause of cirrhosis; the burden of NAFLD-related
cirrhosis in the US is estimated to be double that of Hepatitis C (HCV) related cirrhosis, and
is projected to overtake HCV as the leading indication for liver transplantation within 5
years18. The prevalence of NAFLD-related cirrhosis has historically been underestimated;
recent studies have identified that 30-75% of patients previously diagnosed with cryptogenic
cirrhosis instead have “burnt out” NAFLD-related cirrhosis, where a gradual loss of steatosis
during the progression towards cirrhosis results in the lack of the distinctive histological
features of NASH46.
Poor awareness, clinical suspicion of those at risk, and misrepresentation of NAFLD as a
benign disease without potential for progression have often contributed to a delay in
diagnosis or institution of appropriate management to prevent advanced liver disease.
Indeed, Pais et al. reported that 38-45% of patients with NAFLD-related cirrhosis are
diagnosed only after presenting with decompensated liver failure39. The authors also
demonstrated a greater potential for disease progression than previously appreciated; their
prospective longitudinal study of follow-up biopsies, in those with isolated steatosis,
performed less than 5 years apart found 32% progressed to NASH and 24% developed
bridging fibrosis47. Similarly, Nasr et al. found that in a prospective cohort study of NAFLD
patients followed over 30 years, 61% of those with simple steatosis progressed in fibrosis of
at least one stage, 34% developed advanced fibrosis and 29% of NAFLD patients developed
clinically significant disease45.The most important predictor of progression and overall
mortality was the presence and degree of hepatic fibrosis at time of diagnosis 45.
Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most feared liver-related complication of NAFLD.
HCC is the fifth most common cancer worldwide and the second leading cause of cancer-
related mortality48. NAFLD is rapidly overtaking HCV as the most common cause of HCC;
Wong et al. reported a 9% annual increase in the incidence of NAFLD related HCC between
2004 and 200949, while Dyson et al. noted a nearly 4-fold increase in NASH-related HCC
from 2002 to 201250. Indeed some studies have already shown NAFLD to be the most
common risk factor for HCC (24%) compared to HCV (23%) and Hepatitis B (19.3%) in the
US51. NAFLD also increases the risk of HCC in other liver disease; concurrent NAFLD and
HCV increases HCC risk by 2-3 fold18. NAFLD-HCC tend to have worse liver-related
morbidity and survival outcomes than other causes of HCC due to diagnosis at older age
with greater co-morbidities rendering them poor transplant candidates. They are also often
diagnosed later with larger tumours that have higher rates of recurrence after resection.
This article is protected by copyright. All rights reserved.
The majority of HCC in NAFLD occurs in the setting of NAFLD-related cirrhosis; the annual
cumulative incidence of HCC is approximately 2.6% in NAFLD-related cirrhosis, which
exceeds the 1.5% incidence rate threshold to justify HCC surveillance 49. However, there is
also a subset of patients with NAFLD that develop HCC in the absence of cirrhosis. While
the annual incidence rate is much lower at 0.04%, due to the high prevalence of NAFLD in
the general population, the absolute number of newly diagnosed HCC cases in those without
cirrhosis approaches those with cirrhosis18. Histopathological studies of new HCC diagnoses
have shown only 50% of NAFLD-related HCC occur with cirrhosis present compared to
100% of HCV-related HCC52. This suggests that steatosis and steatohepatitis, in addition to
fibrosis, contribute to hepatocarcinogenesis through hormonal and inflammatory
mechanisms. This is highlighted by Mohamad et al. who compared the histology of cirrhotic
Accepted Article
and non-cirrhotic HCC, finding 89.1% of the non-cirrhotic HCC group had stage 1 steatosis
and 63% lobular inflammation but only 44.1% had any evidence of fibrosis53.
The increasing incidence of HCC and greater awareness of its occurrence in the absence of
cirrhosis therefore postulates the role of surveillance in all NAFLD cases for earlier diagnosis
and therefore better treatment outcomes. Current guidelines recommend screening for those
with cirrhosis with 6 monthly liver ultrasound examination.
While the same guidelines if applied to those without liver cirrhosis may aid in early HCC
detection, the overall incidence is too low to be deemed cost effective54. Even in cirrhosis,
compliance with surveillance is often poor and currently non-invasive surveillance methods
do not yield a reliable method for risk stratification54. Sensitivity of ultrasound for small
nodules is also impaired by suboptimal image quality due to central adiposity and increased
echogenicity in the steatosis liver. Strategies for reducing the incidence and burden of
disease should therefore be targeted towards early risk factor modification in NAFLD to
minimise the progression to advanced liver disease and HCC.
Cardiovascular Disease
Cardiovascular disease is the leading cause of mortality in NAFLD. The underlying
pathophysiological processes linking NAFLD with atherosclerotic disease is thought to mirror
those causing steatosis and/or steatohepatitis in the liver such as increased release of free
fatty acids and pro-inflammatory mediators resulting in atherosclerosis, impaired flow-
mediated vasodilation and increased vascular intimal-medial thickness, stiffness and
calcification55.
Hepatic steatosis is a well-established independent risk factor for cardiovascular events, with
one study reporting a hazard ratio of 1.55-1.85 for cardiovascular mortality in NAFLD56.
Similarly, Targher et al., in their meta-analysis, found that the presence of NAFLD was
associated with a 64% increased risk of fatal and non-fatal cardiovascular events such as
myocardial infarction, angina, stroke and more significant coronary artery disease during
angiography. The severity of NASH derived from imaging, biopsy or NAFLD fibrosis score is
also positively correlated with the degree of carotid artery intimal/medial thickness,
independent of metabolic risk factors55. In addition to vascular disease, NAFLD has also
been shown to affect cardiac contractility. Targher et al. found young people with NAFLD to
have signs of early left ventricular dysfunction and impaired energy metabolism on cardiac
MRI55. For these reasons, it is important to closely monitor and manage cardiovascular risk
factors in patients with NAFLD.
This article is protected by copyright. All rights reserved.
Conclusion
NAFLD is a leading cause of chronic liver disease. Rates of NAFLD are rising in parallel to
rates of obesity and type II diabetes, presenting as an ever-increasing burden to the health
care system. This report highlights the critical role of the metabolic syndrome in the
development of NAFLD, and the challenges faced in the diagnosis and management of this
complex condition. Left untreated, simple steatosis may progress to NASH and ultimately
liver cirrhosis. Greater awareness of this condition by medical practitioners in primary care is
crucial to offset the burden of this disease in Australia, through the screening and
management of metabolic risk factors.
Accepted Article
References
1. Yki-Järvinen, H. Non-alcoholic fatty liver disease as a cause and a consequence of
metabolic syndrome. Lancet Diabetes Endocrinol. 2, 901–910 (2014).
2. Mahady, S. E. & Adams, L. A. Burden of non-alcoholic fatty liver disease in Australia.
J. Gastroenterol. Hepatol. 33, 1–11 (2018).
3. Economics, D. A. The economic cost and health burden of liver diseases in Australia
The Gastroenterological Society of Australia. Gastroenterol. Soc. Aust. (2013).
4. National Health Survey: First Results, 2017-18. Australian Bureau of Statistics
Available at: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by
Subject/4364.0.55.001~2017-18~Main Features~Overweight and obesity~90.
5. Organización para la Cooperación y el Desarrollo Económicos. Obesity Update 2017.
OECD Updat. Rep. 13, 331–341 (2017).
6. Ayonrinde, O. T. et al. Gender-specific differences in adipose distribution and
adipocytokines influence adolescent nonalcoholic fatty liver disease. Hepatology 53,
800–809 (2011).
7. Berentzen, T. ., Gamborg, M., Holst, C. & Sorensen, T. I. . Body mass index in
childhood and adult risk of primary liver cancer. J. Hepatol. 60, 325–330 (2014).
8. Beilby, J. Definition of Metabolic Syndrome: Report of the National Heart, Lung, and
Blood Institute/American Heart Association. Clin Biochem Rev 25, 195–198 (2004).
This article is protected by copyright. All rights reserved.
9. Diehl, A. M. & Day, C. Cause, Pathogenesis, and Treatment of Nonalcoholic
Steatohepatitis. N. Engl. J. Med. 377, 2063–2072 (2017).
10. Yang, K. C. et al. Association of Non-alcoholic Fatty Liver Disease with Metabolic
Syndrome Independently of Central Obesity and Insulin Resistance. Sci. Rep. 6, 1–10
(2016).
11. Fiorucci, S., Biagioli, M. & Distrutti, E. Future trends in the treatment of non-alcoholic
steatohepatitis. Pharmacol. Res. 134, 289–298 (2018).
12. Birkenfeld, A. L. & Shulman, G. I. Nonalcoholic fatty liver disease, hepatic insulin
resistance, and type 2 Diabetes. Hepatology 59, 713–723 (2014).
Accepted Article
13. Marra, F. & Lotersztajn, S. Pathophysiology of NASH: Perspectives for a Targeted
Treatment. Curr. Pharm. Des. 19, 5250–5269 (2013).
14. Kolodziejczyk, A. A., Zheng, D., Shibolet, O. & Elinav, E. The role of the microbiome
in NAFLD and NASH . EMBO Mol. Med. 11, 1–13 (2019).
15. Safari, Z. & Gérard, P. The links between the gut microbiome and non-alcoholic fatty
liver disease (NAFLD). Cell. Mol. Life Sci. 76, 1541–1558 (2019).
16. Sookoian, S. & Pirola, C. J. Genetic predisposition in nonalcoholic fatty liver disease.
Clin. Mol. Hepatol. 23, 1–12 (2017).
17. Duseja, A. & Chalasani, N. Epidemiology and risk factors of nonalcoholic fatty liver
disease (NAFLD). Hepatol. Int. 7, S755–S764 (2013).
18. Michelotti, G. A., Machado, M. V. & Diehl, A. M. NAFLD, NASH and liver cancer. Nat.
Rev. Gastroenterol. Hepatol. 10, 656–665 (2013).
19. Adams, L. A., Knuiman, M. W., Divitini, M. L. & Olynyk, J. K. Body mass index is a
stronger predictor of alanine aminotransaminase levels than alcohol consumption. J.
Gastroenterol. Hepatol. 23, 1089–1093 (2008).
20. Ruben Hernaez, Mariana Lazo, Susanne Bonekamp, Ihab Kamel, Frederick Brancati,
Eliseo Guallar, J. C. Diagnostic Accuracy and Reliability of Ultrasonography for the
Detection of Fatty Liver: A Meta-Analysis. 54, 1082–1090 (2014).
21. Cowin, G. J. et al. Magnetic resonance imaging and spectroscopy for monitoring liver
steatosis. J. Magn. Reson. Imaging 28, 937–945 (2008).
22. Bravo, A.A., Sheth, S.G., Chopra, S. Liver Biopsy. N. Engl. J. Med. 344, 495–500
(2001).
23. Boyd, A., Cain, O., Chauhan, A. & Webb, G. J. Medical liver biopsy: Background,
indications, procedure and histopathology. Frontline Gastroenterol. 1–8 (2019).
doi:10.1136/flgastro-2018-101139
24. Angulo, P. et al. ORIGINAL ARTICLES The NAFLD Fibrosis Score: A Noninvasive
System That Identifies Liver Fibrosis in Patients with NAFLD. doi:10.1002/hep.21496
25. McPherson, S., Stewart, S. F., Henderson, E., Burt, A. D. & Day, C. P. Simple non-
invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients
with non-alcoholic fatty liver disease. Gut 59, 1265–1269 (2010).
26. Leoni, S. et al. Current guidelines for the management of non-alcoholic fatty liver
disease: A systematic review with comparative analysis. World J. Gastroenterol. 24,
3361–3373 (2018).
27. Dyson, J. K., Anstee, Q. M. & McPherson, S. Non-alcoholic fatty liver disease: A
This article is protected by copyright. All rights reserved.
practical approach to treatment. Frontline Gastroenterol. 5, 277–286 (2014).
28. Musso, G., Cassader, M., Rosina, F. & Gambino, R. Impact of current treatments on
liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver
disease (NAFLD): A systematic review and meta-analysis of randomised trials.
Diabetologia 55, 885–904 (2012).
29. Anania, C., Massimo Perla, F., Olivero, F., Pacifico, L. & Chiesa, C. Mediterranean
diet and nonalcoholic fatty liver disease. World J. Gastroenterol. 24, 2083–2094
(2018).
30. Kontogianni, M. D. et al. Adherence to the Mediterranean diet is associated with the
severity of non-alcoholic fatty liver disease. Clin. Nutr. 33, 678–683 (2014).
Accepted Article
31. Marchesini, G., Roden, M. & Vettor, R. Response to: Comment to “EASL-EASD-
EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver
disease”. J. Hepatol. 66, 466–467 (2017).
32. Lassailly, G. et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in
morbidly obese patients. Gastroenterology 149, 379–388 (2015).
33. Lee, Y. et al. Complete Resolution of Nonalcoholic Fatty Liver Disease After Bariatric
Surgery: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 17,
1040-1060.e11 (2019).
34. Laursen, T. L. et al. Bariatric surgery in patients with non-alcoholic fatty liver disease -
From pathophysiology to clinical effects. World J. Hepatol. 11, 138–249 (2019).
35. Jørgensen, N. B. et al. Acute and long-term effects of Roux-en-Y gastric bypass on
glucose metabolism in subjects with Type 2 diabetes and normal glucose tolerance.
Am. J. Physiol. - Endocrinol. Metab. 303, 122–131 (2012).
36. Ma, I. T. & Madura, J. A. Gastrointestinal complications after bariatric surgery.
Gastroenterol. Hepatol. 11, 526–535 (2015).
37. Martin, P., DiMartini, A. Feng, S., Brown Jr, R. Fallon, M. Evaluation for Liver
Transplantation in Adults: 2013 Practice Guideline by the American Association for
the Study of Liver Diseases and the American Society of Transplantation. Hepatology
59, 1144–1165 (2014).
38. Patel, Y. A., Berg, C. L. & Moylan, C. A. Nonalcoholic Fatty Liver Disease: Key
Considerations Before and After Liver Transplantation. Dig. Dis. Sci. 61, 1406–1416
(2016).
39. Pais, R. et al. NAFLD and liver transplantation: Current burden and expected
challenges. J. Hepatol. 65, 1245–1257 (2016).
40. Stine, J. G. et al. Increased risk of portal vein thrombosis in patients with cirrhosis due
to nonalcoholic steatohepatitis. Liver Transplant. 21, 1016–1021 (2015).
41. Dare, A. J. et al. Additive effect of pretransplant obesity, diabetes, and cardiovascular
risk factors on outcomes after liver transplantation. Liver Transplant. 20, 281–290
(2014).
42. Vanwagner, L. B. et al. Patients transplanted for nonalcoholic steatohepatitis are at
increased risk for postoperative cardiovascular events. Hepatology 56, 1741–1750
(2012).
43. Malik, S. M. et al. Recurrent disease following liver transplantation for nonalcoholic
steatohepatitis cirrhosis. Liver Transplant. 15, 1843–1851 (2009).
This article is protected by copyright. All rights reserved.
44. Lindenmeyer, C. C. & McCollough, A. . The Natural History of Nonalcoholic Fatty
Liver Disease - An Evolving View. Clin. Liver Dis. 22, 11–21 (2018).
45. Nasr, P., Ignatova, S., Kechagias, S. & Ekstedt, M. Natural history of nonalcoholic
fatty liver disease: A prospective follow‐up study with serial biopsies. Hepatol.
Commun. 2, 199–210 (2017).
46. Caldwell, S. H. et al. Cryptogenic cirrhosis: Clinical characterization and risk factors
for underlying disease. Hepatology 29, 664–669 (1999).
47. Pais, R. et al. A systematic review of follow-up biopsies reveals disease progression
in patients with non-alcoholic fatty liver. J. Hepatol. 59, 550–556 (2013).
Accepted Article
48. Loomba, R. & Sanyal, A. J. The global NAFLD epidemic. Nat. Rev. Gastroenterol.
Hepatol. 10, 686–690 (2013).
49. Wong, S.-W., Ting, Y.-W. & Chan, W.-K. Epidemiology of non-alcoholic fatty liver
disease-related hepatocellular carcinoma and its implications. JGH Open 2, 235–241
(2018).
50. Dyson, J., Jaques, B., Chattopadyhay, D. & Lochan, R. Hepatocellular Cancer: The
Impact of Obesity, Type 2 Diabetes and a Multidisciplinary Team. J. Hepatol. 60, 110–
117 (2014).
51. Wong, R. J., Cheung, R. & Ahmed, A. Nonalcoholic steatohepatitis is the most rapidly
growing indication for liver transplantation in patients with hepatocellular carcinoma in
the U.S. Hepatology 59, 2188–2195 (2014).
52. Piscaglia, F. et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty
liver disease: A multicenter prospective study. Hepatology 63, 827–838 (2016).
53. Mohamad, B. et al. Characterization of hepatocellular carcinoma (HCC) in non-
alcoholic fatty liver disease (NAFLD) patients without cirrhosis. Hepatol. Int. 10, 632–
639 (2016).
54. Younes, R. & Bugianesi, E. Should we undertake surveillance for HCC in patients with
NAFLD? J. Hepatol. 68, 326–334 (2018).
55. Targher, G., Day, C. . & Bonora, E. Risk of Cardiovascular Disease in Patients with
Nonalcoholic Fatty Liver Disease. N. Engl. J. Med. 363, 1341–1350 (2010).
56. Ekstedt, M., Nasr, P. & Kechagias, S. Natural History of NAFLD/NASH. Curr. Hepatol.
Reports 16, 391–397 (2017).
57. Paschos, P . Paleta, K. Non alcoholic fatty liver disease and metabolic syndrome.
Hippokratia 13, 9–19 (2009).
This article is protected by copyright. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5835)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- ENACb 1Document166 pagesENACb 1DarrylpnzNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- BBS Book (PT 14) NeglyDocument7 pagesBBS Book (PT 14) Neglyapi-3871208No ratings yet
- Leg Support Calculation PDFDocument2 pagesLeg Support Calculation PDFSanjay MoreNo ratings yet
- Gear Trains: 8.1. Angular Velocity RatioDocument16 pagesGear Trains: 8.1. Angular Velocity RatioaddisudagneNo ratings yet
- He Is A Chocolate Lover: Kamaladevi RengasamyDocument4 pagesHe Is A Chocolate Lover: Kamaladevi RengasamyKamala DeviNo ratings yet
- Air Track Gizmo - ExploreLearningDocument4 pagesAir Track Gizmo - ExploreLearningJeremy Gomez-RojasNo ratings yet
- Allotrope Partners Indonesia Renewable Energy Project AssociateDocument2 pagesAllotrope Partners Indonesia Renewable Energy Project AssociateRizal ZulkarnaenNo ratings yet
- IllithidDocument5 pagesIllithidMattia La RosaNo ratings yet
- South Africa Hard Copy Lit 2Document20 pagesSouth Africa Hard Copy Lit 2Jennifer Española BernalNo ratings yet
- EQUILIBRIUMDocument1 pageEQUILIBRIUMMohammed IliasNo ratings yet
- 3B Reactions of Alcohols and ThiolsDocument27 pages3B Reactions of Alcohols and ThiolsAnloraine GonzalesNo ratings yet
- Jayvee Dime,,,,project in Physics Light and SoundDocument25 pagesJayvee Dime,,,,project in Physics Light and SoundJayvee DimeNo ratings yet
- Structural Identification & Poc-1: Topic Page NoDocument35 pagesStructural Identification & Poc-1: Topic Page Nosiddansh100% (1)
- Arthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832Document318 pagesArthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832cengizozakinciNo ratings yet
- Da0bl7mb6d0 Rev DDocument44 pagesDa0bl7mb6d0 Rev DFerreira da CunhaNo ratings yet
- Snag SummmariesDocument171 pagesSnag Summmarieslaltu adgiriNo ratings yet
- Lecture 7 - Synchronous Generators 7 PDFDocument28 pagesLecture 7 - Synchronous Generators 7 PDFDorwinNeroNo ratings yet
- Relative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationDocument17 pagesRelative Color Pickup of Three Different Knits and Predictive Dyeing Recipe FormulationNguyễn Huy CườngNo ratings yet
- Jack and The Beanstalk Treatment-2Document10 pagesJack and The Beanstalk Treatment-2api-668257195No ratings yet
- Earth Quake DesignDocument13 pagesEarth Quake DesignRanie boy CabanillaNo ratings yet
- Form 67 Delivery Unloading and Loading of Materials and PlantDocument6 pagesForm 67 Delivery Unloading and Loading of Materials and PlantMohamed MedhioubNo ratings yet
- Unit-6 Patterns of Industrialisation PDFDocument12 pagesUnit-6 Patterns of Industrialisation PDFNavdeep SinghNo ratings yet
- Synchronous Generators: Instructional ObjectivesDocument18 pagesSynchronous Generators: Instructional Objectivessanthosh2009No ratings yet
- HP Deskjet D1600 Printer SeriesDocument13 pagesHP Deskjet D1600 Printer SeriesRizki JuliadiNo ratings yet
- Schiavi Enc Met Page015Document1 pageSchiavi Enc Met Page015Adel AdelNo ratings yet
- Transport Phenomena: τ =μ dv dyDocument2 pagesTransport Phenomena: τ =μ dv dySYED ASGHAR ALI SULTANNo ratings yet
- Annual Report 2014 PDFDocument153 pagesAnnual Report 2014 PDFகோகுல் இராNo ratings yet
- Fetomaternal Hemorrhage (FMH), An Update Review of LiteratureDocument35 pagesFetomaternal Hemorrhage (FMH), An Update Review of LiteratureEugenia Jeniffer JNo ratings yet
- Macro Chapter 7Document12 pagesMacro Chapter 7Mary Jane PelaezNo ratings yet
- X PPT CH 12 ElectricityDocument12 pagesX PPT CH 12 ElectricityAakriti100% (1)