Professional Documents
Culture Documents
Pathogenesis of Infection
Pathogenesis of Infection
Uploaded by
Cardion Rayon Bali UIN MalangCopyright:
Available Formats
You might also like
- Anti Inflammation Cook Book PDFDocument69 pagesAnti Inflammation Cook Book PDFinmatxetxuNo ratings yet
- Chapter 6Document22 pagesChapter 6Marlop CasicasNo ratings yet
- Duck RaisingDocument12 pagesDuck RaisingRosel Gonzalo-Aquino60% (10)
- An Ethnobotanical Perspective On AyahuascaDocument7 pagesAn Ethnobotanical Perspective On AyahuascaLucho DiazNo ratings yet
- 3 - Pathogenesis of Bacterial InfectionDocument46 pages3 - Pathogenesis of Bacterial InfectionNindya Nabilah Utami100% (1)
- Patogenesis Infeksi BakteriDocument47 pagesPatogenesis Infeksi BakteribellabelbonNo ratings yet
- Lesson 4 - Virus InfectionDocument72 pagesLesson 4 - Virus Infectionpc.bhcNo ratings yet
- Microbiology 1 PDFDocument5 pagesMicrobiology 1 PDFRaven CocjinNo ratings yet
- Microbiology Burton's Chapter 16Document74 pagesMicrobiology Burton's Chapter 16Whenzhie Villaverde PampoNo ratings yet
- Table of Communicable Diseases PDFDocument12 pagesTable of Communicable Diseases PDFkayekristine2001No ratings yet
- Entre The Microcosmos of Life - : Introduntion To BiochemistryDocument48 pagesEntre The Microcosmos of Life - : Introduntion To BiochemistryEINSTEIN2DNo ratings yet
- Laboratory-Activity-1 - Microscopy 2Document5 pagesLaboratory-Activity-1 - Microscopy 2Khate CyrelleNo ratings yet
- Characteristics of VirusDocument13 pagesCharacteristics of VirusTimmygreyNo ratings yet
- Cardiovascular Health 2016Document1 pageCardiovascular Health 2016Jeremy KurnNo ratings yet
- Psychoanalytic Reflections On A Changing WorldDocument299 pagesPsychoanalytic Reflections On A Changing WorldMichael LazarusNo ratings yet
- MicrosDocument4 pagesMicrosTalla CaboteNo ratings yet
- Patient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansDocument21 pagesPatient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansMark Vincent JanoyogNo ratings yet
- Medical Microbiology LEC 2 PDFDocument20 pagesMedical Microbiology LEC 2 PDFيوسف عسكرNo ratings yet
- (Surg2) 5.1b Introduction To Anesthesia-Part 2Document16 pages(Surg2) 5.1b Introduction To Anesthesia-Part 2AlloiBialbaNo ratings yet
- Bacterial Cell StructureDocument6 pagesBacterial Cell StructureCasey StuartNo ratings yet
- Lozano Disaster Nursing PDFDocument21 pagesLozano Disaster Nursing PDFDeva Hiyas100% (1)
- Pathogenesis of InfectionDocument52 pagesPathogenesis of InfectionChandra100% (2)
- Stool ExaminationDocument6 pagesStool Examinationwycliffe kiprotichNo ratings yet
- Chapter11Epidemiology and Public Health RevisedDocument45 pagesChapter11Epidemiology and Public Health Revisedbaku narsNo ratings yet
- Antiviral Agents: Viruses Are Obligate Cellular Parasites Composed of Nucleic AcidDocument47 pagesAntiviral Agents: Viruses Are Obligate Cellular Parasites Composed of Nucleic AcidhadeelNo ratings yet
- Antibiotic Prophylaxis: Francis Neil C. CaranayDocument11 pagesAntibiotic Prophylaxis: Francis Neil C. CaranayNdor BariboloNo ratings yet
- SSI PrventionDocument27 pagesSSI PrventionIPC PFKCCNo ratings yet
- Professionalism: Workplace EthicsDocument45 pagesProfessionalism: Workplace Ethicsprecious maningasNo ratings yet
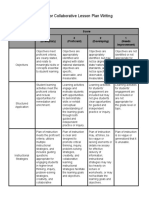
- Rubric For Collaborative Lesson Plan Writing: Score 4 (Exemplary) 3 (Proficient) 2 (Developing) 1 (Needs Improvement)Document3 pagesRubric For Collaborative Lesson Plan Writing: Score 4 (Exemplary) 3 (Proficient) 2 (Developing) 1 (Needs Improvement)Nikki CrystelNo ratings yet
- Pharmacology AntibioticsDocument70 pagesPharmacology Antibioticsmaggie100% (1)
- EBM HarmDocument24 pagesEBM HarmCOVID RSHJNo ratings yet
- Guidelines of Surgical Site InfectionsDocument33 pagesGuidelines of Surgical Site InfectionsAndrie KundrieNo ratings yet
- Ursing Care of Client With CancerDocument51 pagesUrsing Care of Client With CancerJimmelyn PalosNo ratings yet
- Economic Importances of NematodesDocument5 pagesEconomic Importances of Nematodesyayeg raja100% (1)
- Presentation SSIDocument41 pagesPresentation SSIJawad Mustafa100% (1)
- DiphteriaDocument64 pagesDiphteriaOmarNo ratings yet
- PALOMADO Midterm Microbiology 2020Document9 pagesPALOMADO Midterm Microbiology 2020MARLON PALOMADONo ratings yet
- Bot 101 NotesDocument2 pagesBot 101 NotesAbid Hussain100% (1)
- Infection Control in Surgical PracticeDocument41 pagesInfection Control in Surgical PracticeMuhammad Azeem KhanNo ratings yet
- Sterilization and DisinfectionDocument31 pagesSterilization and Disinfectionnana8767100% (2)
- Diagnosis of TrypanosomiasisDocument82 pagesDiagnosis of TrypanosomiasisDrVijayata Choudhary100% (1)
- Intestinal Coccidian ParasitesDocument23 pagesIntestinal Coccidian ParasitesABC100% (1)
- Invasion and Tumour MetastasisDocument33 pagesInvasion and Tumour MetastasisShimmering MoonNo ratings yet
- Genetics of VirusesDocument15 pagesGenetics of VirusesJeneviev Pacres100% (1)
- 9.2-Epidemiology of Infectious DiseasesDocument67 pages9.2-Epidemiology of Infectious DiseasesMarin Jr., Reynaldo J.No ratings yet
- Infection and Modes of TransmissionDocument14 pagesInfection and Modes of TransmissionLucky Radita Alma100% (1)
- Acid Fast Bacteria: M. Tuberculosis, M. LepraeDocument22 pagesAcid Fast Bacteria: M. Tuberculosis, M. LepraeelaNo ratings yet
- Microbiology Lecture 1 - Structure, Classification and MorphologyDocument4 pagesMicrobiology Lecture 1 - Structure, Classification and MorphologyAldwin BagtasNo ratings yet
- Neoplasia 2011 ADocument45 pagesNeoplasia 2011 ACassey Koi FarmNo ratings yet
- An Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajDocument25 pagesAn Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajMwanja MosesNo ratings yet
- Actinomycetes - and NocardiaDocument41 pagesActinomycetes - and NocardiaTummalapalli Venkateswara RaoNo ratings yet
- Antiviral Agents: Dr. Roshna Sh. Aziz Department of Pharmacology School of Medicine University of SulaimaniDocument72 pagesAntiviral Agents: Dr. Roshna Sh. Aziz Department of Pharmacology School of Medicine University of Sulaimaniheta aprianaNo ratings yet
- Healthcare Epidemiology: Ma. Concepcion A. Maico, RN, Man, EddDocument25 pagesHealthcare Epidemiology: Ma. Concepcion A. Maico, RN, Man, EddIconMaicoNo ratings yet
- Overview of Infections and AntimicrobialsDocument43 pagesOverview of Infections and Antimicrobialszainab ElsayedNo ratings yet
- Electron MicrosDocument28 pagesElectron MicrosVEENA DEVINo ratings yet
- Disinfection and SterilizationDocument43 pagesDisinfection and Sterilizationfaizal halimNo ratings yet
- Carcinoma Penis: Pravin NarkhedeDocument36 pagesCarcinoma Penis: Pravin Narkhedepravin narkhede100% (1)
- Infection Associated With Prosthetic JointsDocument8 pagesInfection Associated With Prosthetic JointsReno WaisyahNo ratings yet
- 24 05 2021 Floroquinolones DR - Syeda ZainDocument46 pages24 05 2021 Floroquinolones DR - Syeda ZaintehreemNo ratings yet
- Hemodinamic Disorder, Thrombosis, and ShockDocument50 pagesHemodinamic Disorder, Thrombosis, and Shockbagir_dm10No ratings yet
- Chapter 2 The Chemical Basis of LifeDocument7 pagesChapter 2 The Chemical Basis of LifeJenny AnneNo ratings yet
- Ce Sunt InfectiileDocument5 pagesCe Sunt Infectiilegeorgi.annaNo ratings yet
- ASEPSISDocument8 pagesASEPSISKhecia Freanne TorresNo ratings yet
- Kejadian Balita Stunting Di Posyandu Apel Desa Jambearjo Kecamatan Tajinan Kabupaten MalangDocument6 pagesKejadian Balita Stunting Di Posyandu Apel Desa Jambearjo Kecamatan Tajinan Kabupaten MalangCardion Rayon Bali UIN MalangNo ratings yet
- Efektifitas Pengaturan Euthanasia Dalam KUHP Terhadap Pasien Penderita Kanker Dengan KondisiDocument6 pagesEfektifitas Pengaturan Euthanasia Dalam KUHP Terhadap Pasien Penderita Kanker Dengan KondisiCardion Rayon Bali UIN MalangNo ratings yet
- Epigallocatechin 3 GallateDocument18 pagesEpigallocatechin 3 GallateCardion Rayon Bali UIN MalangNo ratings yet
- Ijerph 16 00923Document17 pagesIjerph 16 00923Cardion Rayon Bali UIN MalangNo ratings yet
- Types of Hearing Loss: Md. Maruf Trainee Offr Otolaryngology & Head & Neck SurgeryDocument40 pagesTypes of Hearing Loss: Md. Maruf Trainee Offr Otolaryngology & Head & Neck SurgeryMaruf MahmoodNo ratings yet
- Cervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerDocument5 pagesCervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerIrina100% (1)
- Gastric Questionnaire (To Be Completed by Life Assured-EnG)Document2 pagesGastric Questionnaire (To Be Completed by Life Assured-EnG)Khamini Dilly KannanNo ratings yet
- Maternal Physiology: Metabolic Changes Hematological ChangesDocument33 pagesMaternal Physiology: Metabolic Changes Hematological ChangesironNo ratings yet
- Medical Terminology and Its Particularities: Zdenka Uherová, Anna HorňákováDocument8 pagesMedical Terminology and Its Particularities: Zdenka Uherová, Anna HorňákováVipul DobariyaNo ratings yet
- Glypican-3 As A Useful Diagnostic Marker That Distinguishes Hepatocellular Carcinoma From Benign Hepatocellular Mass LesionsDocument6 pagesGlypican-3 As A Useful Diagnostic Marker That Distinguishes Hepatocellular Carcinoma From Benign Hepatocellular Mass LesionsBlake_jjNo ratings yet
- 10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Document2 pages10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Larisa IliescuNo ratings yet
- GENESISDocument4 pagesGENESISmonirul islam shohanNo ratings yet
- Diagnosis and Management of PreeclampsiaDocument9 pagesDiagnosis and Management of PreeclampsiaEka YogaNo ratings yet
- Seminar 5 - Traumatic Dislocation and Common Soft Tissue Injury - 2Document149 pagesSeminar 5 - Traumatic Dislocation and Common Soft Tissue Injury - 2Star CruiseNo ratings yet
- Albumin: OSR6102 4 X 29 ML R1 OSR6202 4 X 54 ML R1 OSR6602 4 X 173 ML R1Document2 pagesAlbumin: OSR6102 4 X 29 ML R1 OSR6202 4 X 54 ML R1 OSR6602 4 X 173 ML R1irwoons70No ratings yet
- Masterclass ProgrammeDocument8 pagesMasterclass ProgrammewmogtNo ratings yet
- Rosalina Q. de Sagun, M.D. Maria Antonia Aurora Moral - Valencia, M.DDocument52 pagesRosalina Q. de Sagun, M.D. Maria Antonia Aurora Moral - Valencia, M.DDaphne Jo ValmonteNo ratings yet
- ER-Aid 9459 ENG - Report Full Version 231216Document66 pagesER-Aid 9459 ENG - Report Full Version 231216Nejash Abdo IssaNo ratings yet
- Lewis: Medical-Surgical Nursing, 8 Edition: Chapter 48: Nursing Assessment: Endocrine System Answer GuidelinesDocument1 pageLewis: Medical-Surgical Nursing, 8 Edition: Chapter 48: Nursing Assessment: Endocrine System Answer Guidelinessammm996No ratings yet
- Physical Exam FindingsDocument77 pagesPhysical Exam FindingsMohamed Kamel MehrziNo ratings yet
- ARDSDocument26 pagesARDSDuratul FahliaNo ratings yet
- Ficha Técnica Del Aceite Escencial de LimónDocument2 pagesFicha Técnica Del Aceite Escencial de LimónSheyla GarcésNo ratings yet
- Nephrology Final Spring 2020Document8 pagesNephrology Final Spring 2020Srinivas PingaliNo ratings yet
- The Homoeopathic Concise Repertory PDFDocument28 pagesThe Homoeopathic Concise Repertory PDFShrutika MatteNo ratings yet
- Austin Reid Deborah Reese English 1101 4 December 2013Document11 pagesAustin Reid Deborah Reese English 1101 4 December 2013areid1525No ratings yet
- Statistics PWDs PHDocument5 pagesStatistics PWDs PHStephen TrinidadNo ratings yet
- Breastfeeding and YouDocument203 pagesBreastfeeding and YouEmman Acosta DomingcilNo ratings yet
- Cerebral Aerobics: Alveolar Process of The MaxillaDocument2 pagesCerebral Aerobics: Alveolar Process of The MaxillaJo Hn VengzNo ratings yet
- DES With AnswerDocument123 pagesDES With AnswersoksothyspsNo ratings yet
- UWB Microwave Imaging For Non-Invasive Anomaly Detection in Human Lung and Possible Application in COVID-19 Diagnosis: A ReviewDocument5 pagesUWB Microwave Imaging For Non-Invasive Anomaly Detection in Human Lung and Possible Application in COVID-19 Diagnosis: A ReviewJulia GuintoNo ratings yet
- EU Fundamentals 7thed Sample ChapterDocument12 pagesEU Fundamentals 7thed Sample ChapterAndrada ArmasuNo ratings yet
Pathogenesis of Infection
Pathogenesis of Infection
Uploaded by
Cardion Rayon Bali UIN MalangOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathogenesis of Infection
Pathogenesis of Infection
Uploaded by
Cardion Rayon Bali UIN MalangCopyright:
Available Formats
Chapter
Pathogenesis of infection
2
2.1 Stages of infectious disease 21 Encounter with microorganisms
2.2 Pathogenicity 23
The initial contact with a given microbial species is
Self-assessment: questions 26
critically important. The indigenous microbial flora
Self-assessment: answers 27 is already present on the body surface. Infections
acquired from this pool of organisms are said to be
‘endogenous’, e.g. urinary tract infection. Organisms
Overview acquired as a result of transmission from an external
Given the ubiquitous nature of microorganisms and the source are said to be exogenous. The major routes of
many occasions on which they come into contact with transmission are:
humans, it is surprising how infrequently infectious
diseases occur. The reason why some organisms can • direct contact (including intimate sexual
peacefully coexist with humans while others go on to contact), e.g. soft tissue infections, gonorrhoea,
produce disease lies in the nature of the interaction genital herpes
between microbe and host. Much has been learnt in • inhalation/droplet infection, e.g. common cold,
recent years about mechanisms of microbial disease, pneumonia
especially at the molecular and cellular levels. There is • ingestion/faecal–oral route, e.g. gastroenteritis
a growing awareness of the active contribution of the • inoculation or trauma, e.g. tetanus, malaria
environmental context of infection. Knowledge of these
processes is necessary to understand how to diag-
• transplacentally, e.g. congenital toxoplasmosis.
nose, treat and prevent infection effectively.
Colonisation
The initial encounter with a new microbial species
2.1 Stages of infectious disease may result in nothing more than short-lived
contact with an external body surface. The micro-
organism needs to survive and multiply under
Learning objectives local conditions (e.g. of temperature and pH) to
establish itself in its new habitat. It must success-
You should:
• know the mechanisms that microorganisms use to fully compete against an established indigenous
cause infection microbial flora and resist local defence mechanisms.
• understand infection as a staged biological Some species are capable of producing mucolytic
process enzymes to help them penetrate the layer of
mucus coating internal body surfaces. Other species
have specific adhesins that enable binding with
The process through which microorganisms cause receptor sites on human cells (e.g. gonococcal
disease involves several or all of the following pili attachment to urethral epithelium and influenza
stages: virus adherence to glycoprotein receptors on
upper respiratory mucosal cells). Locally active IgA
1. encounter produced by some mucosal surfaces can be inacti-
2. colonisation vated by bacteria such as Haemophilus influenzae,
3. penetration Streptococcus pneumoniae and Neisseria meningitidis,
4. spread which produce IgA protease. Once established
5. damage on a body surface, an organism is said to have
6. resolution. colonised that site. However, not all organisms
21
Ch002-F10289.indd 21 12/6/2006 10:23:21 AM
Two: Pathogenesis of infection
that colonise will go on to invade and damage tissues, along tissue planes or via the veins and
underlying host tissues. lymphatic vessels. The vascular route of spread is a
particularly effective means of delivering organisms
Penetration of anatomical barriers from an initial focus to distant sites around the body.
In order to invade living human tissues, a micro- Organisms may play an active part in spread by
organism must breach surface barriers. In the case of destroying cells, or even by self-propulsion. As the
the skin, bacteria probably do not penetrate intact organisms spread, evasion of host defences becomes
surfaces. Infection thus requires a break in the epi- increasingly important.
thelial cover due to trauma, surgical wounds, chronic
skin disease or insect bites. Some parasites (e.g. Mechanisms of damage
schistosomes, the cause of bilharzia) can penetrate Microorganisms damage tissues by a variety of
intact skin. The respiratory tract is continuously mechanisms:
exposed to air-borne organisms. However, the upper
respiratory tract functions as an inertial filtration • bulk effect
system and protects the more delicate lungs from • toxin mediated
exposure to inhaled particles. The cough reflex and • altered function of host systems
the mucociliary escalator provide back-up, expelling • host response to infection.
any particles inhaled into the airways. Infective par-
ticles (e.g. droplet nuclei, less than 5 μm in diameter) Bulk effect
may reach the alveoli and establish infection. In the The sheer bulk of organisms may obstruct a
gastrointestinal tract, some disease-causing organ- hollow organ, e.g. some helminth infections of the
isms damage the mucosal surface by releasing intestine. Swelling of infected tissues can cause
cytotoxins (e.g. those causing dysentery), while pressure on adjacent hollow organs or neurovascu-
others (Salmonella typhi) are taken up by the M cells lar bundles.
overlying gut-associated lymphoid tissue in Peyer’s
patches. The fetus is not normally exposed to micro- Toxins
organisms in utero. Only a small group of organisms Toxin-mediated disease may also be caused by pro-
cause infection in the mother during pregnancy and duction of microbial substances that damage cells.
can also traverse the placenta to cause intrauterine Most bacterial toxins (Table 1) are proteins released
infections such as toxoplasmosis, rubella, syphilis by the organism or a lipopolysaccharide complex
and cytomegalovirus infection. If an organism is located in the cell wall and liberated during cell
capable of intracellular infection (e.g. tuberculosis, growth or lysis. A number of specific toxins have
chlamydial disease or viral infection), it must also be been shown to play an essential role in correspond-
capable of cell penetration and survival in an intra- ing diseases. They include:
cellular habitat. At this stage, evasion or subversion
of host defences becomes important to microbial • tetanospasmin: tetanus
survival. • botulinum toxin: botulism
• cholera toxin: cholera
Spread • diphtheria toxin: diphtheria.
An invading microorganism may spread by one or In these infections, the toxin causes the main features
more routes: direct extension through surrounding of the disease. However, toxins do not have to
Table 1 Some examples of bacterial toxins
Species Toxin Type Gene location
Clostridium botulinum Botulinum toxin Neurotoxin Bacteriophage
Clostridium tetani Tetanospasmin Neurotoxin Plasmid
Corynebacterium diphtheriae Diphtheria toxin A-B ADP ribosylating Bacteriophage
Escherichia coli Heat-labile toxin A-B ADP ribosylating Plasmid
Vibrio cholerae Cholera toxin A-B ADP ribosylating Chromosome
22
Ch002-F10289.indd 22 12/6/2006 10:23:22 AM
Pathogenicity
destroy cells to cause damage. They can cause sub- Some organisms change their surface antigenic
lethal damage or alter cellular function, adding to makeup intermittently to evade the host immune
the disease process in more subtle ways. Many exo- system (e.g. borrelias and trypanosomes).
toxins have two principal subunits: A (active) and B The genetic determinants of microbial pathoge-
(binding). The B subunit determines tissue specific- nicity are complex. In bacteria, the genes coding for
ity, while the A subunit causes cellular damage after toxin production may be on the chromosome, on the
binding by the B subunit and subsequent penetra- plasmids (extrachromosomal DNA) or even in a bac-
tion of the cell membrane. teriophage. Expression of ‘virulence factors’ in most
cases is a response to an environmental trigger.
Altered function of organs, Work with laboratory animals resulted in the devel-
tissues or cells opment of a promoter gene trap for the study of
Microbial invasion can change the function of organs, bacterial pathogenesis. The system, known as in
tissues or cells. These changes can be the result of vitro expression technology (IVET), led to the
physiological mechanisms acting to remove the identification of the structural and controller genes
Two
infective agent, e.g. increased bowel motility leading responsible for promoting disease. The products
to diarrhoea, or coughing and sneezing. of the disease-promoting genes have been placed in
six categories: adhesins, invasins and toxins, and
The host response to infection cloaking, shielding and scavenging factors. The
The host response usually begins with an inflamma- genetic switching on and off in response to environ-
tory reaction, and is followed by a humoral or cell- mental triggers allows the bacterium to survive
mediated immune response. This may cause damage mechanical, non-specific and immune defences.
due to swelling, increased fragility of tissues, forma- Post-transcriptional regulation via sigma factors
tion of pus, scarring or necrosis. Chronic intracellu- provides a molecular link between the microbial
lar infection may cause formation of fibrous nodules genome and the organism’s physiological response
and a state of latency from which acute infection can to its immediate environment. Whole groups of pro-
be re-established at a much later stage. teins can be up- or downregulated as the microbe
adapts to its environment. Proteins under the control
of a single, unified mechanism constitute a regulon.
2.2 Pathogenicity
Many aspects of bacterial physiology are specific to
a particular phase of growth. If also dependent on
microbial density, they are said to be subject to
Learning objectives quorum sensing, a process in which a group of low-
You should: molecular-weight compounds known as acyl homo-
• know the principal contributors to infection-related serine lactones (AHLs) are expressed in a simple
tissue damage and the factors that might limit this system of intercellular communication.
damage
• understand the balance between the Pathogenesis of viral infection
microorganism, the human recipient and the
intervening environment in determining the As obligate intracellular parasites, viruses require
outcome of an infection. effective mechanisms of transmission, adherence
and cellular penetration to establish infection. Many
viruses have specific preferences for certain host
Individual species or strains vary in their ability to tissues (e.g. rhinoviruses for the upper respiratory
cause disease. A prerequisite of microorganism- epithelium and human immunodeficiency virus
induced damage is microbial growth. Microorgan- (HIV) for CD4 T lymphocytes). Viruses can spread
isms have a great variety of strategies to enable by lysis of the primary infected cell and secondary
continued growth in a hostile environment. They viraemia, or by formation of bridges (syncytia)
compete for substrates such as iron (an important between cells. Human cells need not be destroyed.
growth-limiting factor) and other trace elements. Viral penetration of the host cell cytoplasmic mem-
Many species have defences against phagocytic cells brane without cell rupture is a complex process in
(e.g. the polysaccharide capsule of S. pneumonia, and which the virus may use cell surface molecules to
antiphagocytic toxins such as staphylococcal leuko- subvert normal membrane and cytoskeletal func-
cidin) and some have a capacity to survive inside tions. Viruses can be continually formed at the cell
macrophages (such as Mycobacterium tuberculosis). surface or the genome can even be integrated into
23
Ch002-F10289.indd 23 12/6/2006 10:23:22 AM
Two: Pathogenesis of infection
the host cell’s own genome. The long-term survival immune systems are depressed by drugs or infec-
of viruses within human cells as obligate intracellu- tion, particularly by HIV.
lar parasites places them beyond the reach of immune
defences. Some viruses integrate into the host cell
genome to produce a latent state. Viral damage
Infection and the environment
is caused by the cytotoxic effects of the virus or by The model mechanism of infection that we inherited
host immune attack. Mechanisms of late-stage viral from Robert Koch places its emphasis on an identifi-
damage include autoimmune, immune-complex or able microbial pathogen; the presumed external
neoplastic disease. agent of disease. This emphasis may have been
useful in the early days of the germ theory of disease.
Pathogenesis of fungal infection However, a preoccupation with the microorganism
Fungal disease, particularly its life-threatening to the exclusion of all other factors misses the wider
extreme, is relatively rare despite the many species context of the discoveries made by the early pioneers
of fungi present in the environment and on the of microbial disease research. Koch provided a rule
human body surface. Most fungal infections appear of thumb to establish the role of a given microorgan-
to require a breach in host defences in order to ism as the causal agent of a given disease. Unfortu-
become established. Yeasts often cause mucosal nately, Koch’s postulates, as they are known, are
inflammation following alteration of either vaginal only rarely fulfilled, despite attempts to bring them
or gastrointestinal flora. Dermatophytic fungi cause up to date with a molecular biological slant.
a variety of skin conditions but rarely cause more The early immunologists recognised the funda-
invasive disease in immunocompetent patients mental importance of the infected person’s response
because they are restricted to the skin. There is no in the development of infectious disease. Accepting
good evidence for the involvement of toxins in the contribution of humoral and cellular immunity,
fungal disease. Most damage is probably caused by tissue reaction and immune compromise to the
the host response. course of an infection leads to a more sophisticated
model of infection as an interactive process between
Pathogenesis of parasitic infections human and microbe with destructive consequences.
Protozoal and helminth infections have a complex Until very recently, the environment in which the
pathogenesis, which is best understood by referring initial interaction between microbe and host occurs
to the parasite’s life cycle. Some protozoal and hel- was seen as little more than a passive backdrop to
minth infections require transmission by a disease infection, with the possible exception of some vector-
vector. The vector is often an arthropod. The devel- borne parasitic infections. The critical role of the
opment of disease depends on a three-way relation- environment in mediating the encounter with a
ship between microorganism, vector and human potentially infective microorganism, and thereby
victim in these infections. The ecology of the vector influencing the outcome, is a more recent idea.
(sometimes known as the ‘intermediate host’) is The emerging picture of infectious disease patho-
critical to the long-term survival of the parasite genesis is one in which the outcome is determined
within a human population. In developed countries, by a three-way tussle between microorganism,
parasitic infections are most common in interna- human recipient and the intervening environment.
tional travellers, the sexually active, immunocom- The complex cellular and molecular events that
promised patients and poor people. The application determine the final outcome of each encounter are
of novel molecular parasitology techniques has pro- likely to throw more light on the origins of disease.
vided new insights into the mechanisms of parasite This multilayered picture of infection as a process
disease. encompassing molecular events, cellular events,
tissue, whole organism, habitat and geography is
Opportunist infections known as ‘biocomplexity’.
If an organism is capable of causing disease in an
apparently healthy individual, it is clearly aggres- Dynamic biological processes
sively pathogenic. If it is normally incapable of
causing disease but can do so only when the human The dynamics of the interaction between micro-
body is compromised in some way, it is said to be organism and human cells are beginning to open up
opportunist. Opportunist infections are of particular to mechanistic analysis. The application of mathe-
importance in hospital patients and in people whose matical modelling to theoretical biology now allows
24
Ch002-F10289.indd 24 12/6/2006 10:23:22 AM
Pathogenicity
us to predict the consequences of introducing a new encounter between two populations attempting to
disease-causing microbe to a human population. The restore biological order—a noisy negotiation for a
perturbations from the initial steady-state popula- peaceful settlement. This newer way of looking at
tions of microorganisms and humans resemble a pathogenesis (the origins of disease) complements
discordant state that demands resolution before mainstream germ theory, and has taken our
harmony can be restored. Infection can be thought understanding of infectious disease processes into
of as the unsought consequence of an accidental unfamiliar multidisciplinary territory.
Two
25
Ch002-F10289.indd 25 12/6/2006 10:23:22 AM
Questions
Master
Medicine Self-assessment: questions
Extended matching questions Any one answer can be used once, more than once
or not at all.
The following is a list of questions:
A. Cholera
1. What is an example of a vertical B. Gonorrhoea
infection?
C. Pneumonia
2. What is the best example of an infection that
D. Staphylococcal skin infection
requires initial colonisation of a body
surface? E. Fetal (intrauterine) rubella
3. Which infection listed is most likely to result F. Viral gastroenteritis
from inhalation?
4. Which one of these infections is most often Short notes questions
transmitted in air?
5. Which infection needs an initial breach in the Write short notes on the following:
body surface?
1. How microorganisms cause damage in human
6. In which infection does a leukocidin play a disease
role?
2. A comparison of pathogenesis of bacterial and
7. Which infection is caused by an obligate viral infections
intracellular organism?
3. The main routes for transmission of infectious
8. Which infection is entirely due to the action of diseases and how microorganisms penetrate
a toxin? the respective anatomical barriers
9. In which infection is droplet size a critical
factor?
10. Which infection does not require microbial
Viva questions
penetration of the body surface? 1. What is the difference between colonisation
and infection?
Select the single answer from the list below that best 2. Can microorganisms be divided into pathogens
matches each one of the questions in the list above. and non-pathogens?
26
Ch002-F10289.indd 26 12/6/2006 10:23:22 AM
Answers
Master
Medicine Self-assessment: answers
Extended matching answers 7. F:
All viruses are obligate intracellular parasites. A few
1. F: bacteria are obligate intracellular organisms, e.g.
Fetal rubella is transmitted from the mother to the chlamydias, and a larger number are facultative
fetus in utero and is therefore an example of a intracellular organisms (e.g. Legionella, Listeria and
vertical infection. All others listed are exogenous Salmonella). The vibrio that causes cholera is extra-
infections due to external agents, with the possible cellular and staphylococci can be both intra- and
exception of some staphylococcal skin infections, extracellular.
which can be caused by inoculation of bacteria from
the endogenous skin flora. 8. A:
The profuse diarrhoea seen in patients with cholera
2. B: is almost entirely due to the extracellular action of
Gonorrhoea requires initial colonisation of the ure- cholera toxin.
thral mucosa and adhesion to the epithelial surface
via pili. Cholera and viral gastroenteritis require 9. C:
ingestion, pneumonia requires inhalation and sta- Inhaled droplet size is of critical importance in the
phylococcal skin infection can result from direct pathogenesis of pneumonia, where droplets must
inoculation. be of the right diameter to reach the smaller air
spaces where the bacteria or viruses that they
3. C: contain can establish infection. Particle size is of
Pneumonia is usually caused by bacteria or lesser or no importance in all the other infections
viruses that have been inhaled into the smaller listed.
airways.
10. A:
4. C: Cholera is due to the effect of a toxin that acts
on the intestinal mucosal surface and therefore
Pneumonia is transmitted by inhalation of
does not require penetration of intestinal epithelial
infective droplet nuclei. Gonorrhoea requires inti-
cells. Intrauterine rubella requires entry of the
mate body contact. Cholera requires a major break-
virus, first into the mother’s circulation, and then
down in sewage disposal and other hygiene failures.
into the fetal bloodstream. The other listed infec-
Viral gastroenteritis is transmitted by the faecal–oral
tions all depend on penetration of an epithelial
route, involves unwashed hands and may some-
surface.
times be spread via the air to those in close
proximity.
5. D:
Short notes answers
Staphylococcal skin infection usually requires at 1. The main topic areas of bulk effect,
least a microscopic breach in the skin surface. Pneu- altered function, toxin-mediated effects and
monia results from inhalation. Gastroenteritis and host response should be covered, with
cholera result from ingestion, and intrauterine infec- examples.
tion results from transplacental spread. 2. Could be tackled as a table. Follow
the sequence of acquisition, colonisation,
6. D: penetration, spread and damage.
Leukocidin plays a part in the invasion stage of Give examples of bacteria and
some of the more severe staphylococcal skin viruses.
infections. It is not a feature of pneumonia, 3. Follow principal routes of transmission and
cholera, viral gastroenteritis or intrauterine means of penetration; probably best done
infection. using a system-based approach.
27
Ch002-F10289.indd 27 12/6/2006 10:23:22 AM
Answers
Viva answers patient. Refer to the balance between
patient and microbe and its modification
1. Briefly define the two terms, then give specific by host defences, antibiotics and
examples and discuss how confusion of the two environmental factors. Give specific examples
terms can cause problems in clinical practice. of how concepts of pathogenesis have
2. Some microbes have not yet been shown to changed recently through developments in
cause human infection. Mention the spectrum molecular and cell biology and now challenge
of virulence from opportunist to those that a simplistic pathogen–non-pathogen
can be highly lethal in the previously healthy dichotomy.
28
Ch002-F10289.indd 28 12/6/2006 10:23:22 AM
You might also like
- Anti Inflammation Cook Book PDFDocument69 pagesAnti Inflammation Cook Book PDFinmatxetxuNo ratings yet
- Chapter 6Document22 pagesChapter 6Marlop CasicasNo ratings yet
- Duck RaisingDocument12 pagesDuck RaisingRosel Gonzalo-Aquino60% (10)
- An Ethnobotanical Perspective On AyahuascaDocument7 pagesAn Ethnobotanical Perspective On AyahuascaLucho DiazNo ratings yet
- 3 - Pathogenesis of Bacterial InfectionDocument46 pages3 - Pathogenesis of Bacterial InfectionNindya Nabilah Utami100% (1)
- Patogenesis Infeksi BakteriDocument47 pagesPatogenesis Infeksi BakteribellabelbonNo ratings yet
- Lesson 4 - Virus InfectionDocument72 pagesLesson 4 - Virus Infectionpc.bhcNo ratings yet
- Microbiology 1 PDFDocument5 pagesMicrobiology 1 PDFRaven CocjinNo ratings yet
- Microbiology Burton's Chapter 16Document74 pagesMicrobiology Burton's Chapter 16Whenzhie Villaverde PampoNo ratings yet
- Table of Communicable Diseases PDFDocument12 pagesTable of Communicable Diseases PDFkayekristine2001No ratings yet
- Entre The Microcosmos of Life - : Introduntion To BiochemistryDocument48 pagesEntre The Microcosmos of Life - : Introduntion To BiochemistryEINSTEIN2DNo ratings yet
- Laboratory-Activity-1 - Microscopy 2Document5 pagesLaboratory-Activity-1 - Microscopy 2Khate CyrelleNo ratings yet
- Characteristics of VirusDocument13 pagesCharacteristics of VirusTimmygreyNo ratings yet
- Cardiovascular Health 2016Document1 pageCardiovascular Health 2016Jeremy KurnNo ratings yet
- Psychoanalytic Reflections On A Changing WorldDocument299 pagesPsychoanalytic Reflections On A Changing WorldMichael LazarusNo ratings yet
- MicrosDocument4 pagesMicrosTalla CaboteNo ratings yet
- Patient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansDocument21 pagesPatient Care Pathogen Reservoir Mode of Transmission: Viral Infections of HumansMark Vincent JanoyogNo ratings yet
- Medical Microbiology LEC 2 PDFDocument20 pagesMedical Microbiology LEC 2 PDFيوسف عسكرNo ratings yet
- (Surg2) 5.1b Introduction To Anesthesia-Part 2Document16 pages(Surg2) 5.1b Introduction To Anesthesia-Part 2AlloiBialbaNo ratings yet
- Bacterial Cell StructureDocument6 pagesBacterial Cell StructureCasey StuartNo ratings yet
- Lozano Disaster Nursing PDFDocument21 pagesLozano Disaster Nursing PDFDeva Hiyas100% (1)
- Pathogenesis of InfectionDocument52 pagesPathogenesis of InfectionChandra100% (2)
- Stool ExaminationDocument6 pagesStool Examinationwycliffe kiprotichNo ratings yet
- Chapter11Epidemiology and Public Health RevisedDocument45 pagesChapter11Epidemiology and Public Health Revisedbaku narsNo ratings yet
- Antiviral Agents: Viruses Are Obligate Cellular Parasites Composed of Nucleic AcidDocument47 pagesAntiviral Agents: Viruses Are Obligate Cellular Parasites Composed of Nucleic AcidhadeelNo ratings yet
- Antibiotic Prophylaxis: Francis Neil C. CaranayDocument11 pagesAntibiotic Prophylaxis: Francis Neil C. CaranayNdor BariboloNo ratings yet
- SSI PrventionDocument27 pagesSSI PrventionIPC PFKCCNo ratings yet
- Professionalism: Workplace EthicsDocument45 pagesProfessionalism: Workplace Ethicsprecious maningasNo ratings yet
- Rubric For Collaborative Lesson Plan Writing: Score 4 (Exemplary) 3 (Proficient) 2 (Developing) 1 (Needs Improvement)Document3 pagesRubric For Collaborative Lesson Plan Writing: Score 4 (Exemplary) 3 (Proficient) 2 (Developing) 1 (Needs Improvement)Nikki CrystelNo ratings yet
- Pharmacology AntibioticsDocument70 pagesPharmacology Antibioticsmaggie100% (1)
- EBM HarmDocument24 pagesEBM HarmCOVID RSHJNo ratings yet
- Guidelines of Surgical Site InfectionsDocument33 pagesGuidelines of Surgical Site InfectionsAndrie KundrieNo ratings yet
- Ursing Care of Client With CancerDocument51 pagesUrsing Care of Client With CancerJimmelyn PalosNo ratings yet
- Economic Importances of NematodesDocument5 pagesEconomic Importances of Nematodesyayeg raja100% (1)
- Presentation SSIDocument41 pagesPresentation SSIJawad Mustafa100% (1)
- DiphteriaDocument64 pagesDiphteriaOmarNo ratings yet
- PALOMADO Midterm Microbiology 2020Document9 pagesPALOMADO Midterm Microbiology 2020MARLON PALOMADONo ratings yet
- Bot 101 NotesDocument2 pagesBot 101 NotesAbid Hussain100% (1)
- Infection Control in Surgical PracticeDocument41 pagesInfection Control in Surgical PracticeMuhammad Azeem KhanNo ratings yet
- Sterilization and DisinfectionDocument31 pagesSterilization and Disinfectionnana8767100% (2)
- Diagnosis of TrypanosomiasisDocument82 pagesDiagnosis of TrypanosomiasisDrVijayata Choudhary100% (1)
- Intestinal Coccidian ParasitesDocument23 pagesIntestinal Coccidian ParasitesABC100% (1)
- Invasion and Tumour MetastasisDocument33 pagesInvasion and Tumour MetastasisShimmering MoonNo ratings yet
- Genetics of VirusesDocument15 pagesGenetics of VirusesJeneviev Pacres100% (1)
- 9.2-Epidemiology of Infectious DiseasesDocument67 pages9.2-Epidemiology of Infectious DiseasesMarin Jr., Reynaldo J.No ratings yet
- Infection and Modes of TransmissionDocument14 pagesInfection and Modes of TransmissionLucky Radita Alma100% (1)
- Acid Fast Bacteria: M. Tuberculosis, M. LepraeDocument22 pagesAcid Fast Bacteria: M. Tuberculosis, M. LepraeelaNo ratings yet
- Microbiology Lecture 1 - Structure, Classification and MorphologyDocument4 pagesMicrobiology Lecture 1 - Structure, Classification and MorphologyAldwin BagtasNo ratings yet
- Neoplasia 2011 ADocument45 pagesNeoplasia 2011 ACassey Koi FarmNo ratings yet
- An Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajDocument25 pagesAn Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajMwanja MosesNo ratings yet
- Actinomycetes - and NocardiaDocument41 pagesActinomycetes - and NocardiaTummalapalli Venkateswara RaoNo ratings yet
- Antiviral Agents: Dr. Roshna Sh. Aziz Department of Pharmacology School of Medicine University of SulaimaniDocument72 pagesAntiviral Agents: Dr. Roshna Sh. Aziz Department of Pharmacology School of Medicine University of Sulaimaniheta aprianaNo ratings yet
- Healthcare Epidemiology: Ma. Concepcion A. Maico, RN, Man, EddDocument25 pagesHealthcare Epidemiology: Ma. Concepcion A. Maico, RN, Man, EddIconMaicoNo ratings yet
- Overview of Infections and AntimicrobialsDocument43 pagesOverview of Infections and Antimicrobialszainab ElsayedNo ratings yet
- Electron MicrosDocument28 pagesElectron MicrosVEENA DEVINo ratings yet
- Disinfection and SterilizationDocument43 pagesDisinfection and Sterilizationfaizal halimNo ratings yet
- Carcinoma Penis: Pravin NarkhedeDocument36 pagesCarcinoma Penis: Pravin Narkhedepravin narkhede100% (1)
- Infection Associated With Prosthetic JointsDocument8 pagesInfection Associated With Prosthetic JointsReno WaisyahNo ratings yet
- 24 05 2021 Floroquinolones DR - Syeda ZainDocument46 pages24 05 2021 Floroquinolones DR - Syeda ZaintehreemNo ratings yet
- Hemodinamic Disorder, Thrombosis, and ShockDocument50 pagesHemodinamic Disorder, Thrombosis, and Shockbagir_dm10No ratings yet
- Chapter 2 The Chemical Basis of LifeDocument7 pagesChapter 2 The Chemical Basis of LifeJenny AnneNo ratings yet
- Ce Sunt InfectiileDocument5 pagesCe Sunt Infectiilegeorgi.annaNo ratings yet
- ASEPSISDocument8 pagesASEPSISKhecia Freanne TorresNo ratings yet
- Kejadian Balita Stunting Di Posyandu Apel Desa Jambearjo Kecamatan Tajinan Kabupaten MalangDocument6 pagesKejadian Balita Stunting Di Posyandu Apel Desa Jambearjo Kecamatan Tajinan Kabupaten MalangCardion Rayon Bali UIN MalangNo ratings yet
- Efektifitas Pengaturan Euthanasia Dalam KUHP Terhadap Pasien Penderita Kanker Dengan KondisiDocument6 pagesEfektifitas Pengaturan Euthanasia Dalam KUHP Terhadap Pasien Penderita Kanker Dengan KondisiCardion Rayon Bali UIN MalangNo ratings yet
- Epigallocatechin 3 GallateDocument18 pagesEpigallocatechin 3 GallateCardion Rayon Bali UIN MalangNo ratings yet
- Ijerph 16 00923Document17 pagesIjerph 16 00923Cardion Rayon Bali UIN MalangNo ratings yet
- Types of Hearing Loss: Md. Maruf Trainee Offr Otolaryngology & Head & Neck SurgeryDocument40 pagesTypes of Hearing Loss: Md. Maruf Trainee Offr Otolaryngology & Head & Neck SurgeryMaruf MahmoodNo ratings yet
- Cervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerDocument5 pagesCervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerIrina100% (1)
- Gastric Questionnaire (To Be Completed by Life Assured-EnG)Document2 pagesGastric Questionnaire (To Be Completed by Life Assured-EnG)Khamini Dilly KannanNo ratings yet
- Maternal Physiology: Metabolic Changes Hematological ChangesDocument33 pagesMaternal Physiology: Metabolic Changes Hematological ChangesironNo ratings yet
- Medical Terminology and Its Particularities: Zdenka Uherová, Anna HorňákováDocument8 pagesMedical Terminology and Its Particularities: Zdenka Uherová, Anna HorňákováVipul DobariyaNo ratings yet
- Glypican-3 As A Useful Diagnostic Marker That Distinguishes Hepatocellular Carcinoma From Benign Hepatocellular Mass LesionsDocument6 pagesGlypican-3 As A Useful Diagnostic Marker That Distinguishes Hepatocellular Carcinoma From Benign Hepatocellular Mass LesionsBlake_jjNo ratings yet
- 10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Document2 pages10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Larisa IliescuNo ratings yet
- GENESISDocument4 pagesGENESISmonirul islam shohanNo ratings yet
- Diagnosis and Management of PreeclampsiaDocument9 pagesDiagnosis and Management of PreeclampsiaEka YogaNo ratings yet
- Seminar 5 - Traumatic Dislocation and Common Soft Tissue Injury - 2Document149 pagesSeminar 5 - Traumatic Dislocation and Common Soft Tissue Injury - 2Star CruiseNo ratings yet
- Albumin: OSR6102 4 X 29 ML R1 OSR6202 4 X 54 ML R1 OSR6602 4 X 173 ML R1Document2 pagesAlbumin: OSR6102 4 X 29 ML R1 OSR6202 4 X 54 ML R1 OSR6602 4 X 173 ML R1irwoons70No ratings yet
- Masterclass ProgrammeDocument8 pagesMasterclass ProgrammewmogtNo ratings yet
- Rosalina Q. de Sagun, M.D. Maria Antonia Aurora Moral - Valencia, M.DDocument52 pagesRosalina Q. de Sagun, M.D. Maria Antonia Aurora Moral - Valencia, M.DDaphne Jo ValmonteNo ratings yet
- ER-Aid 9459 ENG - Report Full Version 231216Document66 pagesER-Aid 9459 ENG - Report Full Version 231216Nejash Abdo IssaNo ratings yet
- Lewis: Medical-Surgical Nursing, 8 Edition: Chapter 48: Nursing Assessment: Endocrine System Answer GuidelinesDocument1 pageLewis: Medical-Surgical Nursing, 8 Edition: Chapter 48: Nursing Assessment: Endocrine System Answer Guidelinessammm996No ratings yet
- Physical Exam FindingsDocument77 pagesPhysical Exam FindingsMohamed Kamel MehrziNo ratings yet
- ARDSDocument26 pagesARDSDuratul FahliaNo ratings yet
- Ficha Técnica Del Aceite Escencial de LimónDocument2 pagesFicha Técnica Del Aceite Escencial de LimónSheyla GarcésNo ratings yet
- Nephrology Final Spring 2020Document8 pagesNephrology Final Spring 2020Srinivas PingaliNo ratings yet
- The Homoeopathic Concise Repertory PDFDocument28 pagesThe Homoeopathic Concise Repertory PDFShrutika MatteNo ratings yet
- Austin Reid Deborah Reese English 1101 4 December 2013Document11 pagesAustin Reid Deborah Reese English 1101 4 December 2013areid1525No ratings yet
- Statistics PWDs PHDocument5 pagesStatistics PWDs PHStephen TrinidadNo ratings yet
- Breastfeeding and YouDocument203 pagesBreastfeeding and YouEmman Acosta DomingcilNo ratings yet
- Cerebral Aerobics: Alveolar Process of The MaxillaDocument2 pagesCerebral Aerobics: Alveolar Process of The MaxillaJo Hn VengzNo ratings yet
- DES With AnswerDocument123 pagesDES With AnswersoksothyspsNo ratings yet
- UWB Microwave Imaging For Non-Invasive Anomaly Detection in Human Lung and Possible Application in COVID-19 Diagnosis: A ReviewDocument5 pagesUWB Microwave Imaging For Non-Invasive Anomaly Detection in Human Lung and Possible Application in COVID-19 Diagnosis: A ReviewJulia GuintoNo ratings yet
- EU Fundamentals 7thed Sample ChapterDocument12 pagesEU Fundamentals 7thed Sample ChapterAndrada ArmasuNo ratings yet