Professional Documents
Culture Documents
296 1179 1 PB
296 1179 1 PB
Uploaded by
Kriti KumariCopyright:
Available Formats
You might also like
- Fecalysis Examination NotesDocument2 pagesFecalysis Examination NotesNicole Tan90% (10)
- Seemandhra IMA MembersDocument926 pagesSeemandhra IMA MembersKriti Kumari50% (2)
- In 1102 Site ListDocument20 pagesIn 1102 Site ListKriti KumariNo ratings yet
- Gujarat BC Detail Final For Website 25 June 19Document616 pagesGujarat BC Detail Final For Website 25 June 19Kriti KumariNo ratings yet
- DEX DEX DDR Marketing Plan UpdatedDocument68 pagesDEX DEX DDR Marketing Plan UpdatedMuzammel Riaz100% (1)
- Provisional Dispisition List of DoctorsDocument84 pagesProvisional Dispisition List of DoctorsKriti Kumari0% (1)
- TrainingDetail16 17Document64 pagesTrainingDetail16 17Kriti Kumari0% (1)
- Laparoscopic OvariectomíaDocument15 pagesLaparoscopic Ovariectomíasimon alfaro gonzálezNo ratings yet
- The Effect of Different Abdominal Pressures On Liver Function Tests After Laparoscopic CholecystectomyDocument8 pagesThe Effect of Different Abdominal Pressures On Liver Function Tests After Laparoscopic Cholecystectomybashar mohammedNo ratings yet
- Fast Track Pathways in Colorectal Surgery: Rinaldy Teja SetiawanDocument27 pagesFast Track Pathways in Colorectal Surgery: Rinaldy Teja SetiawanRinaldy T SetiawanNo ratings yet
- Roux-en-Y Reconstruction After PancreaticoduodenectomyDocument5 pagesRoux-en-Y Reconstruction After Pancreaticoduodenectomyyacine26No ratings yet
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocument5 pagesA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinNo ratings yet
- Biloma After Laparoscopic Cholecystectomy: Case ReportDocument3 pagesBiloma After Laparoscopic Cholecystectomy: Case ReportAlpriyando Rindy AgustinusNo ratings yet
- Sumber Jurnal ReadingDocument15 pagesSumber Jurnal ReadingagungNo ratings yet
- Articol Colectiiintraabd2013Document8 pagesArticol Colectiiintraabd2013Miha ElaNo ratings yet
- 8-Anatomical V31 1 2016Document6 pages8-Anatomical V31 1 2016DrSaabNo ratings yet
- 1 Salim TahirhvDocument4 pages1 Salim TahirhvTajudin SuryaNo ratings yet
- Case Study Residency2Document21 pagesCase Study Residency2computerwhiz42985No ratings yet
- Case Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseaseDocument4 pagesCase Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseasetafalubisNo ratings yet
- Effect of Intraoperative Fluid Management On Outcome After Intraabdominal SurgeryDocument8 pagesEffect of Intraoperative Fluid Management On Outcome After Intraabdominal Surgeryade_liaNo ratings yet
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDocument3 pagesGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghNo ratings yet
- Predictive Factors For Conversion of Laparoscopic CholecystectomyDocument4 pagesPredictive Factors For Conversion of Laparoscopic CholecystectomyGilang IrwansyahNo ratings yet
- A Prospective Study To Evaluate The Effects of Co2 Pneumoperitoneum On Hepatic Enzymes in Laparoscopic SurgeriesDocument7 pagesA Prospective Study To Evaluate The Effects of Co2 Pneumoperitoneum On Hepatic Enzymes in Laparoscopic SurgeriesIJAR JOURNALNo ratings yet
- Guillot Re Au 2009Document6 pagesGuillot Re Au 2009nimaelhajjiNo ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Intraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus RestrictiveDocument7 pagesIntraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus Restrictiveade_liaNo ratings yet
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyDocument4 pagesLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prevention of Paracentesis Induced Circulatory Dysfunction in Cirrhosis Standard vs. Half Albumin DosesDocument6 pagesPrevention of Paracentesis Induced Circulatory Dysfunction in Cirrhosis Standard vs. Half Albumin DosesEma Emanuela SarcaNo ratings yet
- Annals of Medicine and Surgery: Case ReportDocument4 pagesAnnals of Medicine and Surgery: Case ReportDimas ErlanggaNo ratings yet
- CholeL During BariatricDocument6 pagesCholeL During BariatriclucasakrNo ratings yet
- Anaesthesia For Hepatic Resection SurgeryDocument15 pagesAnaesthesia For Hepatic Resection SurgeryDianita P Ñáñez VaronaNo ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Fast Track Programme in Liver Surgery - BJS 2013Document6 pagesFast Track Programme in Liver Surgery - BJS 2013RobiViNo ratings yet
- 9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsDocument14 pages9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsekoNo ratings yet
- 20 Iunie 2017Document3 pages20 Iunie 2017Radu MiricaNo ratings yet
- Hepatic CancerDocument15 pagesHepatic CancerTrinh TrầnNo ratings yet
- Evaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryDocument7 pagesEvaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryajmrdNo ratings yet
- Amilaze PredictivDocument7 pagesAmilaze PredictivDumitru RadulescuNo ratings yet
- Laparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaDocument4 pagesLaparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaRonald QuezadaNo ratings yet
- Chapter VDocument15 pagesChapter VJellou MacNo ratings yet
- Kohler TIPSPortalveinthrombosis 10102015Document29 pagesKohler TIPSPortalveinthrombosis 10102015sirrfsNo ratings yet
- Ausencia Congenita Del Conducto Cistico. Mini-Revision 2013Document6 pagesAusencia Congenita Del Conducto Cistico. Mini-Revision 2013Bolivar IseaNo ratings yet
- Postoperative Fistula PancreaticDocument7 pagesPostoperative Fistula PancreaticstonmanNo ratings yet
- ANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Document13 pagesANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Ammar magdyNo ratings yet
- Journal ReadingDocument8 pagesJournal ReadingAnonymous Uh2myPxPHNo ratings yet
- Early Ercp and Papillotomy Compared With Conservative Treatment For Acute Biliary PancreatitisDocument6 pagesEarly Ercp and Papillotomy Compared With Conservative Treatment For Acute Biliary PancreatitisRT_BokNo ratings yet
- Anesthesiafor Hepatobiliarysurgery: Chris Snowden,, James PrentisDocument17 pagesAnesthesiafor Hepatobiliarysurgery: Chris Snowden,, James PrentisGiovanni AgugginiNo ratings yet
- Posthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)Document12 pagesPosthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)drsubramanianNo ratings yet
- Pancreatic ®stula After Pancreatic Head ResectionDocument7 pagesPancreatic ®stula After Pancreatic Head ResectionNicolas RuizNo ratings yet
- Annals of Medicine and SurgeryDocument4 pagesAnnals of Medicine and SurgeryRadu MiricaNo ratings yet
- Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy in 2020Document3 pagesAssociating Liver Partition and Portal Vein Ligation for Staged Hepatectomy in 2020Crimson Publishers Novel Approaches in Cancer StudyNo ratings yet
- 1 s2.0 S2210261215002680 MainDocument4 pages1 s2.0 S2210261215002680 Mainnaili nsnNo ratings yet
- ABolton Poster FinalDocument1 pageABolton Poster FinalcardiffmedicsscNo ratings yet
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocument4 pagesConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosNo ratings yet
- Bar Dram 2000Document6 pagesBar Dram 2000Prasetyö AgungNo ratings yet
- TIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent AscitesDocument7 pagesTIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent Ascitesray liNo ratings yet
- Bahasa IndonesiaDocument4 pagesBahasa IndonesiaNadiah Umniati SyarifahNo ratings yet
- Outcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisDocument9 pagesOutcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisAfkar30No ratings yet
- Post Operative PancreatitisDocument7 pagesPost Operative PancreatitisNirajan SubediNo ratings yet
- 492 568 1 SMnjsjsdjsDocument4 pages492 568 1 SMnjsjsdjsZidna MazayatulNo ratings yet
- Br. J. Anaesth.-2002-Holte-622-32Document11 pagesBr. J. Anaesth.-2002-Holte-622-32Syauqi DarussalamNo ratings yet
- Left Hepatectomy For Hepatocellular Carcinoma Left Liver With Underlying Cirrhosis and Portal HypertensionDocument3 pagesLeft Hepatectomy For Hepatocellular Carcinoma Left Liver With Underlying Cirrhosis and Portal HypertensionPeertechz Publications Inc.No ratings yet
- Lafaro 2020Document17 pagesLafaro 2020Noemi Di FucciaNo ratings yet
- Randomized Clinical Trial of Epidural, Spinal or Patient-Controlled Analgesia For Patients Undergoing Laparoscopic Colorectal SurgeryDocument11 pagesRandomized Clinical Trial of Epidural, Spinal or Patient-Controlled Analgesia For Patients Undergoing Laparoscopic Colorectal Surgeryvalerio.messinaNo ratings yet
- Resultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaDocument9 pagesResultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaNicolás Javier Acevedo OjedaNo ratings yet
- Surgtest GI Surgery NEET SS 2022 RecallDocument58 pagesSurgtest GI Surgery NEET SS 2022 RecallRajhan 410No ratings yet
- Pathology (2) 16.9.13Document2 pagesPathology (2) 16.9.13Kriti Kumari100% (1)
- SubDocument38 pagesSubkirthikaNo ratings yet
- Name Class Code Year of AdmissionDocument7 pagesName Class Code Year of AdmissionKriti KumariNo ratings yet
- ANM Detail of Uttar Pradesh Validated ANMsDocument894 pagesANM Detail of Uttar Pradesh Validated ANMsKriti KumariNo ratings yet
- University - Regi Stration - Numbe R (Temprory)Document9 pagesUniversity - Regi Stration - Numbe R (Temprory)Kriti KumariNo ratings yet
- S.No Doctor Name Address Area Speciality EmailDocument24 pagesS.No Doctor Name Address Area Speciality Emailgaurav chauhanNo ratings yet
- A Prospective Study of Clinico-Radiological Assesment and Management of Obstructive Jaundice in Mmimsr, MullanaDocument9 pagesA Prospective Study of Clinico-Radiological Assesment and Management of Obstructive Jaundice in Mmimsr, MullanaKriti KumariNo ratings yet
- Institution Data in Prescribed FormatDocument135 pagesInstitution Data in Prescribed FormatKriti KumariNo ratings yet
- NMCH Regular ListDocument289 pagesNMCH Regular ListKriti KumariNo ratings yet
- List of Psychitrist Doctors Who Are Registred in U.K.M.CDocument327 pagesList of Psychitrist Doctors Who Are Registred in U.K.M.CKriti Kumari0% (1)
- Jemds Title Page - OraDocument2 pagesJemds Title Page - OraKriti KumariNo ratings yet
- List of Unclaimed Dividend For FY 2012-13Document1,447 pagesList of Unclaimed Dividend For FY 2012-13Kriti KumariNo ratings yet
- FDA PR 2008 Mar 2009Document2,024 pagesFDA PR 2008 Mar 2009Kriti KumariNo ratings yet
- P.G. Admission List 2020Document21 pagesP.G. Admission List 2020Kriti KumariNo ratings yet
- UIC NetworklistDocument563 pagesUIC NetworklistKriti KumariNo ratings yet
- Mysore Medical College Alumni Association. Mysore®.: 12th and 13th Dec 2015Document7 pagesMysore Medical College Alumni Association. Mysore®.: 12th and 13th Dec 2015Kriti KumariNo ratings yet
- 139-Article Text-416-1-10-20180204Document3 pages139-Article Text-416-1-10-20180204Kriti KumariNo ratings yet
- Idfb B3Document1,194 pagesIdfb B3Kriti KumariNo ratings yet
- GSM Ssa Wise Closed Connections Feb 20Document64 pagesGSM Ssa Wise Closed Connections Feb 20Kriti KumariNo ratings yet
- Employee AppndxDocument43 pagesEmployee AppndxKriti KumariNo ratings yet
- Laparoscopic Extirpation of An Intra-Abdominal Compressed Air Firearm Pellet in A Grownup: A Rare Case ReportDocument4 pagesLaparoscopic Extirpation of An Intra-Abdominal Compressed Air Firearm Pellet in A Grownup: A Rare Case ReportKriti KumariNo ratings yet
- Rs. 2,500 / DD No.-Date Rs. 2,000 / DD No.-Date: 5th CONVOCATION - 2016 of WBUHS (Details of Drafts Received)Document66 pagesRs. 2,500 / DD No.-Date Rs. 2,000 / DD No.-Date: 5th CONVOCATION - 2016 of WBUHS (Details of Drafts Received)Kriti KumariNo ratings yet
- Training FP by SifpsaDocument134 pagesTraining FP by SifpsaKriti KumariNo ratings yet
- 2856 - Jemds Title PageDocument2 pages2856 - Jemds Title PageKriti KumariNo ratings yet
- 8 Jemds Title PageDocument3 pages8 Jemds Title PageKriti KumariNo ratings yet
- C - Syiam Amalia Rahmah - Topik 4Document7 pagesC - Syiam Amalia Rahmah - Topik 4Syiam Amalia RahmahNo ratings yet
- Analisis Edukasi Mahasiswa Mengenai Sirosis Sebagai Strategi Pencegahan SirosisDocument5 pagesAnalisis Edukasi Mahasiswa Mengenai Sirosis Sebagai Strategi Pencegahan Sirosiselsa hewuniNo ratings yet
- Laboratory 9 Digestive SystemDocument8 pagesLaboratory 9 Digestive SystemClyde Alec (Clydealec)No ratings yet
- Routine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsDocument3 pagesRoutine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsSheila GarciaNo ratings yet
- Full Download Advanced Nutrition and Human Metabolism 7th Edition Gropper Solutions Manual PDF Full ChapterDocument36 pagesFull Download Advanced Nutrition and Human Metabolism 7th Edition Gropper Solutions Manual PDF Full Chapterdatiscincnidariak6y549100% (15)
- Aquifer InternalMedicine09 - 55Document7 pagesAquifer InternalMedicine09 - 55JulieNo ratings yet
- Physiology of Digestive SystemDocument70 pagesPhysiology of Digestive SystemVincent SerNo ratings yet
- Anorectal DiseaseDocument122 pagesAnorectal DiseasejolagusuNo ratings yet
- ST - Science 4 - Q2Document6 pagesST - Science 4 - Q2Norman LopezNo ratings yet
- Science PT3 PDFDocument5 pagesScience PT3 PDFKomagal KunaisekaranNo ratings yet
- Song: Introducing Me - Nick Jonas Parody Digestive SystemDocument2 pagesSong: Introducing Me - Nick Jonas Parody Digestive SystemCymer Romeo DizonNo ratings yet
- Health Talk On GastritisDocument12 pagesHealth Talk On GastritisSomyee Pachuau100% (1)
- GastritisDocument2 pagesGastritisUyun JohariNo ratings yet
- ERCPDocument4 pagesERCPbilly wilsonNo ratings yet
- 10.1.2 - Antacid Agents (2007-Jan2016)Document14 pages10.1.2 - Antacid Agents (2007-Jan2016)Gabrielle NnomoNo ratings yet
- Frog DissectionDocument4 pagesFrog Dissection2110038No ratings yet
- Jceh S 23 00268 3Document9 pagesJceh S 23 00268 3Faisal RasheedNo ratings yet
- MetoclopramideDocument3 pagesMetoclopramideapi-3797941100% (1)
- ANTI Ulcer DrugsDocument1 pageANTI Ulcer Drugsapi-3739910100% (1)
- Diseases of Small and Large IntestineDocument20 pagesDiseases of Small and Large IntestineOluwagbemisoke Estherr OlatunjiNo ratings yet
- Gastroenterology AscitesDocument2 pagesGastroenterology AscitesNour SamadNo ratings yet
- Enemas ProcedureDocument6 pagesEnemas ProcedureAdinda MaulinaNo ratings yet
- Pyloric StenosisDocument23 pagesPyloric StenosisRama ItachiNo ratings yet
- Gastric Funcn TestDocument18 pagesGastric Funcn TestArshdeep SinghNo ratings yet
- Gender Age : Animal Nutrition What Is A Balanced Diet?Document10 pagesGender Age : Animal Nutrition What Is A Balanced Diet?KekeletsoNo ratings yet
- Expt6 FR BC35lab SmallintestineDocument11 pagesExpt6 FR BC35lab SmallintestineYnuehSolomonNo ratings yet
- Coin in The Esophagus: General ConsiderationsDocument3 pagesCoin in The Esophagus: General ConsiderationsFreddy PanjaitanNo ratings yet
- Fleet EnemaDocument4 pagesFleet EnemaAngelene CalivaNo ratings yet
296 1179 1 PB
296 1179 1 PB
Uploaded by
Kriti KumariOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
296 1179 1 PB
296 1179 1 PB
Uploaded by
Kriti KumariCopyright:
Available Formats
Volume-9 | Issue-9 | September - 2019 | PRINT ISSN No. 2249 - 555X | DOI : 10.
36106/ijar
Original Research Paper
General Surgery
LAPAROSCOPIC CHOLECYSTECTOMY: ALTERATIONS IN LIVER
FUNCTION TESTS POST-OPERATIVELY
Dr Shweta Kumari Junior Resident, Department of Surgery, PMCH, Patna
Dr.(Prof) Vimal Professor, Department of Surgery, PMCH, Patna
Mukesh
Dr. Md Sarfaraz Assistant Professor, Department of Surgery, PMCH, Patna
Alam
Dr Md. Habibullah Junior Resident, Department of Surgery, PMCH, Patna *Corresponding Author
Ansari*
ABSTRACT Objective: This study was done to assess the alteration in liver function test following laparoscopic cholecystectomy
post-operatively.
Material and Methods: A prospective study conducted on 182 patients reported in surgery OPD Patna Medical College and Hospital, Patna from
July 2017 to June 2018 with cholelithiasis. All the patients underwent laproscopic cholecystectomy. Both pre-operative and post-operative liver
function test was done.
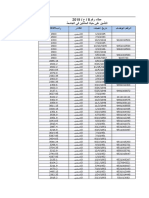
Results: Out of 182 patients, 46 were male and 136 were female patients. The mean age was 32.3 years. The level of serum ALT and AST
increased significantly within the first 24 hours following operation, AST showed mild increase in 36% of the cases while ALT increased in 12%
of the cases. Total bilirubin and direct bilirubin showed a slight increase within the first 24 hours following operation in 2% of the patients.
Alkaline phosphatase increased in 10% of the patients.
Conclusion: Laproscopic Cholecystectomy lead to transient but reversible significant hepatic enzymes alterations. These alterations are self
limited and return to reference values within 7 days of operation. The cause of alteration might be liver tractions, electrocoagulation's and
manipulation of duct.
KEYWORDS : laproscopic cholecystectomy, liver function test, enzymes
INTRODUCTION: normal liver function tests. This study has been undertaken to know the
Laparoscopic cholecystectomy, a minimal-access approach surgery changes in LFTs after Laproscopic Cholecystectomy, the incidences of
for the removal of the gallbladder, was first performed by Mouret in such change, there relation to age, sex, duration of surgery and to know
1987.1 Laparoscopic cholecystectomy offers many advantages that the clinical significances of such disturbances.
include a marked reduction in hospital stay and decreased cost. It has
also been observed, from several studies involving over 4000 patients MATERIALS AND METHODS:
undergoing laparoscopic cholecystectomy, that the complication rate All the patients admitted from surgery OPD in Patna Medical College
is less (about 4%) with the procedure; conversion to open laparotomy and Hospital, Patna diagnosed to have cholelithiasis was included in
occurs in 5% of patients; the death rate is remarkably low (i.e., 0.1%); the study. Any patient with pre-operative abnormality in
bile duct injuries are unusual (i.e., 0.2-0.5%). Because of these distinct liverenzymes, suspected chronic liver diseases, common bile duct
advantages, the procedure has gained worldwide popularity and has pathology, conversion to open cholecystectomy, Hematological
now become one of the most common operations performed in general disorders was excluded.
surgical practice.
Investigations were done to assess the fitness of patients for surgery.
Laparoscopic surgery is performed by the insufflation of gas into the All patients were given pre-operative prophylaxis with Inj.
peritoneal cavity. Carbon dioxide is the standard gas used, largely Ceftriaxone 1gm IV, stat. Regional anesthesia was administered to
because it does not support combustion. After absorption from the patients and Laproscopic cholecystectomy was done.
peritoneum, it is readily excreted via the lungs.2 Carbon dioxide is 20
times more soluble in serum than room air or oxygen and has been Post-operatively, Inj. Diclofenac was given as analgesia for 48 hours.
shown to be absorbed 32 times more quickly than room air when used Post-operatively Inj. Ceftriaxone 1gm IV, BD and Inj. Metronidazole
for double-contrast barium enemas.3 Pneumoperitoneum is likely to be 100cc, TDS was given for 48 hours. The liver function tests were further
smaller in volume and shorter in duration after laparoscopic done 24hour later, and in some patients, the liver function test was
cholecystectomy than after open laparotomy. During the most cases of repeated to monitor liver function. Along with, adverse events were
the surgery, a pneumoperitoneum of 12-14 mm Hg CO2 is noted in all the patients. Finally, the duration of hospital stay was noted.
established.4-6
RESULTS:
Although laparoscopic cholecystectomy offered many advantages We studied 182 patients who underwent laparoscopic chole
over laparotomy, new concerns came-up regarding the effects of cystectomy from July 2017 to June 2018. Out of 182 patients, 46 were
pneumoperitoneum on the cardiovascular and respiratory system. male and 136 were female patients. The mean age was 32.3 years.
These changes are well tolerated even in older and more debilitated
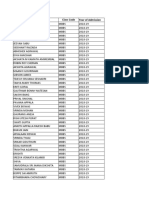
patients and except for a slight increase in the incidence of cardiac SL. PARAMETERS PRE- POST- DIFFERENCE
arrhythmias, no other significant cardiovascular complications occur.7 NO OPERATIVE OPERATIVE
One of the important hemodynamic changes is the transient reduction VALUES VALUES
in hepatic blood flow caused by a pneumoperitoneum. The pressure of 1 TOTAL 0.6 mg/dl 0.9 mg/dl 0.3
the created pneumoperitoneum and its duration was shown to BILIRUBIN
influence the degree of hepatic ischemia. This results in elevations in 2 ALT 16 U/L 34 U/L 18
liver enzymes alanine aminotransferase (ALT), aspartate 3 AST 46 U/L 54 U/L 8
aminotransferase (AST), alkaline phosphatase, gamma-glutamyl
4 GGT 25 U/L 41 U/L 16
transferase (GGT), bilirubin, and international normalized ratio (INR).
Although laparoscopic cholecystectomy is associated with transient 5 PROTIEN 7.1 g/dl 7.2 g/dl 0.1
elevation of liver enzymes, the disturbances after the procedure are 6 ALK. 170 172 2
self-limited and not associated with any morbidity in patients with PHOSPHATASE
INDIAN JOURNAL OF APPLIED RESEARCH 53
Volume-9 | Issue-9 | September - 2019 | PRINT ISSN No. 2249 - 555X | DOI : 10.36106/ijar
Bilirubin (total) pre-operative was 0.6 mg/dl, increased 24 h after using abdominal wall retractors might be feasible in these patient
surgery to 0.90 mg/dl. GGT increased from 25 U/l to 41 U/l. AST and populations.
ALT was found to be significantly elevated from 46 U/l to 54 U/l and
from 16 U/l to 34 U/l, respectively. Alkaline phosphatase and protein REFERENCES:
did not show any elevation, the pre-operative values were 170 U/l and 1. Mouret P. How I developed laparoscopic cholecystectomy. Ann Acad Med Singapore
1996;25:744-7.
after 24 h was 172 U/l. and 7.1g/dl to 7.2g/dl respectively. 2. Cuschieri A. Laparoscopic Biliary Surgery. 2nd ed. Oxford: Blackwell Scientific
Publications; 1992. p. 28.
DISCUSSION: 3. Dobranowski J, Stringer DA, Somers S, Stevenson GW. Procedures in Gastrointestinal
Radiology. New York: Sponger - Verlag; 1990. p. 78.
Laparoscopic cholecystectomy, a minimal-access approach surgery, 4. Omari A, Bani-Hani KE. Effect of carbon dioxide pneumoperitoneum on liver function
offers many advantages that include a markedly reduction in hospital following laparoscopic cholecystectomy. J Laparoendoscop Adv Surg Tech
stay and decreased cost. For over 25 years, laparoscopic 2007;17:419-24.
5. Ibraheim OA, Samarkandi AH, Alshehry H, Faden A, Farouk EO. Lactate and acid base
cholecystectomy has replaced Open Cholecystectomy in the changes during laparoscopic cholecystectomy. Middle East J Anaesthesiol
management of benign gallbladder diseases and has become the gold 2006;18:757-68.
standard for symptomatic cholelithiasis. It is also the procedure of 6. Schwenk W, Haase O, Junghans T. Perspectives in sequential pneumatic compression of
the lower extremities (SCD) for laparoscopic surgery. Acta Chir Belg 2002;102:83-91.
choice for most patients referred for elective cholecystectomy. As with 7. Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, et al. Circulatory and
any surgical procedure, it is not 100% safe and free from respiratory complications of carbon dioxide insufflation. Dig Surg 2004;21:95-105.
complications. Retained stones and duct injuries are among the serious 8. Slater K, Strong RW, Wall DR, et al. Iatrogenic bile duct injury: the scourge of
laparoscopic cholecystectomy. Aust N Z J Surg. 2002;72(2):83–88.
complications related to this procedure. Duct injuries are not easy to 9. Halevy A, Gold-Deutch R, Negri M, et al. Are elevated liver enzymes and bilirubin
recognize during surgery and are usually detected postoperatively.8 levels signifi cant aft er laparoscopic cholecystectomy in the absence of bile duct injury?
Ann Surg. 1994;219(4):362–364.
10. Andrei VE, Schein M, Margolis M, et al. Liver enzymes are commonly elevated
Although laparoscopic cholecystectomy offered many advantages following laparoscopic cholecystectomy: is elevated intra-abdominal pressure the
over laparotomy, new concerns arose regarding the effects of a cause? Dig Surg. 1998;15(3):256–259
pneumoperitoneum on the cardiovascular and respiratory system. 11. Morino M, Giraudo G, Festa V. Alterations in hepatic function during laparoscopic
surgery. An experimental clinical study. Surg Endosc 1998;12:968-72.
These changes are well tolerated even in older and more debilitated
patients and except for a slight increase in the incidence of cardiac
arrhythmias, no other significant cardiovascular complications occur.
One of the important hemodynamic changes is the transient reduction
in hepatic blood flow caused by the pneumoperitoneum. The pressure
of a created pneumoperitoneum and its duration was shown to
influence the degree of hepatic ischemia. This results in changes in
liver enzymes ALT, AST, alkaline phosphatase, GGT, Bilirubin, and
protein levels. Apart from the general assessment of liver function,
LFTs are generally used postoperatively as an indicator of duct
obstructions and iatrogenic injuries. The sensitivity of liver function
tests in predicting biliary obstruction has been shown to be high.
An elevation of the liver enzymes is not always suggestive of retained
stones. In earlier studies, a change in liver function tests of up to 70%
has been reported with no adverse clinical outcome.9
Early elevation of LFTs soon after surgery should not cause major
concern as they usually return to normal without intervention. In the
case of laparoscopic cholecystectomy, close monitoring by performing
serial biochemical analyses can be done when there is increased
suspicion of an iatrogenic duct injury or slipped stone as indicated by
elevated levels of alkaline phosphatase and bilirubin.10
In our study, the level of change of AST, ALT, and GGT was high.
There were moderate changes in the postoperative Bilirubin levels,
and the level of ALP and protein remained almost unchanged.
Although laparoscopic cholecystectomy is associated with transient
elevation of liver enzymes, the disturbances after laparoscopic
cholecystectomy are self-limited and not associated with any
morbidity in patients with a normal liver function11. The derangement
of the liver functions had no adverse clinical event. All the values were
found to have returned to normal at the follow-up after 3 weeks.
CONCLUSION:
Liver function tests include AST, ALT, GGT, ALP, Bilirubin and
protein. Raised values of AST, ALT, and GGT represent hepatocellular
dysfunction. Any rise in the values of ALP and Bilirubin suggests
obstructions to the flow of bile and may have clinical manifestations,
warranting more investigations before a surgery. Surgical
manipulations, diathermy, patient position, arterial injury and CO2
pneumoperitoneum are the contributory factors for liver enzymes
changes following Laproscopic cholecystectomy. These changes
return to normal in 3-4 days after procedure and they have no clinical
consequences in patients with normal hepatic function but they may
still cause worry to the surgeon regarding the integrity of biliary tree.
There has been no proof to state that these enzyme changes are
reflecting a true hepatic or other organ ischemia in otherwise healthy
patients since all patients recovered without any sequlae within 5 days.
However, surgeons should be cautious before planning to perform
laparoscopic cholecystectomy in patients with known hepatic
insufficiency. Laparoscopic cholecystectomy performed under a low-
pressure pneumoperitoneum or gasless laparoscopic cholecystectomy
54 INDIAN JOURNAL OF APPLIED RESEARCH
You might also like
- Fecalysis Examination NotesDocument2 pagesFecalysis Examination NotesNicole Tan90% (10)
- Seemandhra IMA MembersDocument926 pagesSeemandhra IMA MembersKriti Kumari50% (2)
- In 1102 Site ListDocument20 pagesIn 1102 Site ListKriti KumariNo ratings yet
- Gujarat BC Detail Final For Website 25 June 19Document616 pagesGujarat BC Detail Final For Website 25 June 19Kriti KumariNo ratings yet
- DEX DEX DDR Marketing Plan UpdatedDocument68 pagesDEX DEX DDR Marketing Plan UpdatedMuzammel Riaz100% (1)
- Provisional Dispisition List of DoctorsDocument84 pagesProvisional Dispisition List of DoctorsKriti Kumari0% (1)
- TrainingDetail16 17Document64 pagesTrainingDetail16 17Kriti Kumari0% (1)
- Laparoscopic OvariectomíaDocument15 pagesLaparoscopic Ovariectomíasimon alfaro gonzálezNo ratings yet
- The Effect of Different Abdominal Pressures On Liver Function Tests After Laparoscopic CholecystectomyDocument8 pagesThe Effect of Different Abdominal Pressures On Liver Function Tests After Laparoscopic Cholecystectomybashar mohammedNo ratings yet
- Fast Track Pathways in Colorectal Surgery: Rinaldy Teja SetiawanDocument27 pagesFast Track Pathways in Colorectal Surgery: Rinaldy Teja SetiawanRinaldy T SetiawanNo ratings yet
- Roux-en-Y Reconstruction After PancreaticoduodenectomyDocument5 pagesRoux-en-Y Reconstruction After Pancreaticoduodenectomyyacine26No ratings yet
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocument5 pagesA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinNo ratings yet
- Biloma After Laparoscopic Cholecystectomy: Case ReportDocument3 pagesBiloma After Laparoscopic Cholecystectomy: Case ReportAlpriyando Rindy AgustinusNo ratings yet
- Sumber Jurnal ReadingDocument15 pagesSumber Jurnal ReadingagungNo ratings yet
- Articol Colectiiintraabd2013Document8 pagesArticol Colectiiintraabd2013Miha ElaNo ratings yet
- 8-Anatomical V31 1 2016Document6 pages8-Anatomical V31 1 2016DrSaabNo ratings yet
- 1 Salim TahirhvDocument4 pages1 Salim TahirhvTajudin SuryaNo ratings yet
- Case Study Residency2Document21 pagesCase Study Residency2computerwhiz42985No ratings yet
- Case Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseaseDocument4 pagesCase Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseasetafalubisNo ratings yet
- Effect of Intraoperative Fluid Management On Outcome After Intraabdominal SurgeryDocument8 pagesEffect of Intraoperative Fluid Management On Outcome After Intraabdominal Surgeryade_liaNo ratings yet
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDocument3 pagesGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghNo ratings yet
- Predictive Factors For Conversion of Laparoscopic CholecystectomyDocument4 pagesPredictive Factors For Conversion of Laparoscopic CholecystectomyGilang IrwansyahNo ratings yet
- A Prospective Study To Evaluate The Effects of Co2 Pneumoperitoneum On Hepatic Enzymes in Laparoscopic SurgeriesDocument7 pagesA Prospective Study To Evaluate The Effects of Co2 Pneumoperitoneum On Hepatic Enzymes in Laparoscopic SurgeriesIJAR JOURNALNo ratings yet
- Guillot Re Au 2009Document6 pagesGuillot Re Au 2009nimaelhajjiNo ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Intraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus RestrictiveDocument7 pagesIntraoperative Fluid Management in Open Gastro-Intestinal Surgery: Goal-Directed Versus Restrictiveade_liaNo ratings yet
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyDocument4 pagesLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prevention of Paracentesis Induced Circulatory Dysfunction in Cirrhosis Standard vs. Half Albumin DosesDocument6 pagesPrevention of Paracentesis Induced Circulatory Dysfunction in Cirrhosis Standard vs. Half Albumin DosesEma Emanuela SarcaNo ratings yet
- Annals of Medicine and Surgery: Case ReportDocument4 pagesAnnals of Medicine and Surgery: Case ReportDimas ErlanggaNo ratings yet
- CholeL During BariatricDocument6 pagesCholeL During BariatriclucasakrNo ratings yet
- Anaesthesia For Hepatic Resection SurgeryDocument15 pagesAnaesthesia For Hepatic Resection SurgeryDianita P Ñáñez VaronaNo ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Fast Track Programme in Liver Surgery - BJS 2013Document6 pagesFast Track Programme in Liver Surgery - BJS 2013RobiViNo ratings yet
- 9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsDocument14 pages9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsekoNo ratings yet
- 20 Iunie 2017Document3 pages20 Iunie 2017Radu MiricaNo ratings yet
- Hepatic CancerDocument15 pagesHepatic CancerTrinh TrầnNo ratings yet
- Evaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryDocument7 pagesEvaluation of Factors Affecting Liver Function Test in Patients Underwent Coronary Artery Bypass Graft SurgeryajmrdNo ratings yet
- Amilaze PredictivDocument7 pagesAmilaze PredictivDumitru RadulescuNo ratings yet
- Laparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaDocument4 pagesLaparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaRonald QuezadaNo ratings yet
- Chapter VDocument15 pagesChapter VJellou MacNo ratings yet
- Kohler TIPSPortalveinthrombosis 10102015Document29 pagesKohler TIPSPortalveinthrombosis 10102015sirrfsNo ratings yet
- Ausencia Congenita Del Conducto Cistico. Mini-Revision 2013Document6 pagesAusencia Congenita Del Conducto Cistico. Mini-Revision 2013Bolivar IseaNo ratings yet
- Postoperative Fistula PancreaticDocument7 pagesPostoperative Fistula PancreaticstonmanNo ratings yet
- ANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Document13 pagesANZ J. Surg. 2008 78 (Suppl. 1) A68-A80Ammar magdyNo ratings yet
- Journal ReadingDocument8 pagesJournal ReadingAnonymous Uh2myPxPHNo ratings yet
- Early Ercp and Papillotomy Compared With Conservative Treatment For Acute Biliary PancreatitisDocument6 pagesEarly Ercp and Papillotomy Compared With Conservative Treatment For Acute Biliary PancreatitisRT_BokNo ratings yet
- Anesthesiafor Hepatobiliarysurgery: Chris Snowden,, James PrentisDocument17 pagesAnesthesiafor Hepatobiliarysurgery: Chris Snowden,, James PrentisGiovanni AgugginiNo ratings yet
- Posthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)Document12 pagesPosthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)drsubramanianNo ratings yet
- Pancreatic ®stula After Pancreatic Head ResectionDocument7 pagesPancreatic ®stula After Pancreatic Head ResectionNicolas RuizNo ratings yet
- Annals of Medicine and SurgeryDocument4 pagesAnnals of Medicine and SurgeryRadu MiricaNo ratings yet
- Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy in 2020Document3 pagesAssociating Liver Partition and Portal Vein Ligation for Staged Hepatectomy in 2020Crimson Publishers Novel Approaches in Cancer StudyNo ratings yet
- 1 s2.0 S2210261215002680 MainDocument4 pages1 s2.0 S2210261215002680 Mainnaili nsnNo ratings yet
- ABolton Poster FinalDocument1 pageABolton Poster FinalcardiffmedicsscNo ratings yet
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocument4 pagesConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosNo ratings yet
- Bar Dram 2000Document6 pagesBar Dram 2000Prasetyö AgungNo ratings yet
- TIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent AscitesDocument7 pagesTIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent Ascitesray liNo ratings yet
- Bahasa IndonesiaDocument4 pagesBahasa IndonesiaNadiah Umniati SyarifahNo ratings yet
- Outcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisDocument9 pagesOutcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisAfkar30No ratings yet
- Post Operative PancreatitisDocument7 pagesPost Operative PancreatitisNirajan SubediNo ratings yet
- 492 568 1 SMnjsjsdjsDocument4 pages492 568 1 SMnjsjsdjsZidna MazayatulNo ratings yet
- Br. J. Anaesth.-2002-Holte-622-32Document11 pagesBr. J. Anaesth.-2002-Holte-622-32Syauqi DarussalamNo ratings yet
- Left Hepatectomy For Hepatocellular Carcinoma Left Liver With Underlying Cirrhosis and Portal HypertensionDocument3 pagesLeft Hepatectomy For Hepatocellular Carcinoma Left Liver With Underlying Cirrhosis and Portal HypertensionPeertechz Publications Inc.No ratings yet
- Lafaro 2020Document17 pagesLafaro 2020Noemi Di FucciaNo ratings yet
- Randomized Clinical Trial of Epidural, Spinal or Patient-Controlled Analgesia For Patients Undergoing Laparoscopic Colorectal SurgeryDocument11 pagesRandomized Clinical Trial of Epidural, Spinal or Patient-Controlled Analgesia For Patients Undergoing Laparoscopic Colorectal Surgeryvalerio.messinaNo ratings yet
- Resultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaDocument9 pagesResultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaNicolás Javier Acevedo OjedaNo ratings yet
- Surgtest GI Surgery NEET SS 2022 RecallDocument58 pagesSurgtest GI Surgery NEET SS 2022 RecallRajhan 410No ratings yet
- Pathology (2) 16.9.13Document2 pagesPathology (2) 16.9.13Kriti Kumari100% (1)
- SubDocument38 pagesSubkirthikaNo ratings yet
- Name Class Code Year of AdmissionDocument7 pagesName Class Code Year of AdmissionKriti KumariNo ratings yet
- ANM Detail of Uttar Pradesh Validated ANMsDocument894 pagesANM Detail of Uttar Pradesh Validated ANMsKriti KumariNo ratings yet
- University - Regi Stration - Numbe R (Temprory)Document9 pagesUniversity - Regi Stration - Numbe R (Temprory)Kriti KumariNo ratings yet
- S.No Doctor Name Address Area Speciality EmailDocument24 pagesS.No Doctor Name Address Area Speciality Emailgaurav chauhanNo ratings yet
- A Prospective Study of Clinico-Radiological Assesment and Management of Obstructive Jaundice in Mmimsr, MullanaDocument9 pagesA Prospective Study of Clinico-Radiological Assesment and Management of Obstructive Jaundice in Mmimsr, MullanaKriti KumariNo ratings yet
- Institution Data in Prescribed FormatDocument135 pagesInstitution Data in Prescribed FormatKriti KumariNo ratings yet
- NMCH Regular ListDocument289 pagesNMCH Regular ListKriti KumariNo ratings yet
- List of Psychitrist Doctors Who Are Registred in U.K.M.CDocument327 pagesList of Psychitrist Doctors Who Are Registred in U.K.M.CKriti Kumari0% (1)
- Jemds Title Page - OraDocument2 pagesJemds Title Page - OraKriti KumariNo ratings yet
- List of Unclaimed Dividend For FY 2012-13Document1,447 pagesList of Unclaimed Dividend For FY 2012-13Kriti KumariNo ratings yet
- FDA PR 2008 Mar 2009Document2,024 pagesFDA PR 2008 Mar 2009Kriti KumariNo ratings yet
- P.G. Admission List 2020Document21 pagesP.G. Admission List 2020Kriti KumariNo ratings yet
- UIC NetworklistDocument563 pagesUIC NetworklistKriti KumariNo ratings yet
- Mysore Medical College Alumni Association. Mysore®.: 12th and 13th Dec 2015Document7 pagesMysore Medical College Alumni Association. Mysore®.: 12th and 13th Dec 2015Kriti KumariNo ratings yet
- 139-Article Text-416-1-10-20180204Document3 pages139-Article Text-416-1-10-20180204Kriti KumariNo ratings yet
- Idfb B3Document1,194 pagesIdfb B3Kriti KumariNo ratings yet
- GSM Ssa Wise Closed Connections Feb 20Document64 pagesGSM Ssa Wise Closed Connections Feb 20Kriti KumariNo ratings yet
- Employee AppndxDocument43 pagesEmployee AppndxKriti KumariNo ratings yet
- Laparoscopic Extirpation of An Intra-Abdominal Compressed Air Firearm Pellet in A Grownup: A Rare Case ReportDocument4 pagesLaparoscopic Extirpation of An Intra-Abdominal Compressed Air Firearm Pellet in A Grownup: A Rare Case ReportKriti KumariNo ratings yet
- Rs. 2,500 / DD No.-Date Rs. 2,000 / DD No.-Date: 5th CONVOCATION - 2016 of WBUHS (Details of Drafts Received)Document66 pagesRs. 2,500 / DD No.-Date Rs. 2,000 / DD No.-Date: 5th CONVOCATION - 2016 of WBUHS (Details of Drafts Received)Kriti KumariNo ratings yet
- Training FP by SifpsaDocument134 pagesTraining FP by SifpsaKriti KumariNo ratings yet
- 2856 - Jemds Title PageDocument2 pages2856 - Jemds Title PageKriti KumariNo ratings yet
- 8 Jemds Title PageDocument3 pages8 Jemds Title PageKriti KumariNo ratings yet
- C - Syiam Amalia Rahmah - Topik 4Document7 pagesC - Syiam Amalia Rahmah - Topik 4Syiam Amalia RahmahNo ratings yet
- Analisis Edukasi Mahasiswa Mengenai Sirosis Sebagai Strategi Pencegahan SirosisDocument5 pagesAnalisis Edukasi Mahasiswa Mengenai Sirosis Sebagai Strategi Pencegahan Sirosiselsa hewuniNo ratings yet
- Laboratory 9 Digestive SystemDocument8 pagesLaboratory 9 Digestive SystemClyde Alec (Clydealec)No ratings yet
- Routine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsDocument3 pagesRoutine Fecalysis Stool Analysis: Is A Series of Tests Done On A Stool Sample To Help Diagnose Certain ConditionsSheila GarciaNo ratings yet
- Full Download Advanced Nutrition and Human Metabolism 7th Edition Gropper Solutions Manual PDF Full ChapterDocument36 pagesFull Download Advanced Nutrition and Human Metabolism 7th Edition Gropper Solutions Manual PDF Full Chapterdatiscincnidariak6y549100% (15)
- Aquifer InternalMedicine09 - 55Document7 pagesAquifer InternalMedicine09 - 55JulieNo ratings yet
- Physiology of Digestive SystemDocument70 pagesPhysiology of Digestive SystemVincent SerNo ratings yet
- Anorectal DiseaseDocument122 pagesAnorectal DiseasejolagusuNo ratings yet
- ST - Science 4 - Q2Document6 pagesST - Science 4 - Q2Norman LopezNo ratings yet
- Science PT3 PDFDocument5 pagesScience PT3 PDFKomagal KunaisekaranNo ratings yet
- Song: Introducing Me - Nick Jonas Parody Digestive SystemDocument2 pagesSong: Introducing Me - Nick Jonas Parody Digestive SystemCymer Romeo DizonNo ratings yet
- Health Talk On GastritisDocument12 pagesHealth Talk On GastritisSomyee Pachuau100% (1)
- GastritisDocument2 pagesGastritisUyun JohariNo ratings yet
- ERCPDocument4 pagesERCPbilly wilsonNo ratings yet
- 10.1.2 - Antacid Agents (2007-Jan2016)Document14 pages10.1.2 - Antacid Agents (2007-Jan2016)Gabrielle NnomoNo ratings yet
- Frog DissectionDocument4 pagesFrog Dissection2110038No ratings yet
- Jceh S 23 00268 3Document9 pagesJceh S 23 00268 3Faisal RasheedNo ratings yet
- MetoclopramideDocument3 pagesMetoclopramideapi-3797941100% (1)
- ANTI Ulcer DrugsDocument1 pageANTI Ulcer Drugsapi-3739910100% (1)
- Diseases of Small and Large IntestineDocument20 pagesDiseases of Small and Large IntestineOluwagbemisoke Estherr OlatunjiNo ratings yet
- Gastroenterology AscitesDocument2 pagesGastroenterology AscitesNour SamadNo ratings yet
- Enemas ProcedureDocument6 pagesEnemas ProcedureAdinda MaulinaNo ratings yet
- Pyloric StenosisDocument23 pagesPyloric StenosisRama ItachiNo ratings yet
- Gastric Funcn TestDocument18 pagesGastric Funcn TestArshdeep SinghNo ratings yet
- Gender Age : Animal Nutrition What Is A Balanced Diet?Document10 pagesGender Age : Animal Nutrition What Is A Balanced Diet?KekeletsoNo ratings yet
- Expt6 FR BC35lab SmallintestineDocument11 pagesExpt6 FR BC35lab SmallintestineYnuehSolomonNo ratings yet
- Coin in The Esophagus: General ConsiderationsDocument3 pagesCoin in The Esophagus: General ConsiderationsFreddy PanjaitanNo ratings yet
- Fleet EnemaDocument4 pagesFleet EnemaAngelene CalivaNo ratings yet