Professional Documents
Culture Documents
BEAM Workshop
BEAM Workshop
Uploaded by
Ed YC KohOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BEAM Workshop
BEAM Workshop
Uploaded by
Ed YC KohCopyright:
Available Formats
READING
MATERIALS FOR BASIC EMERGENCY AIRWAY WORKSHOP
1st October 2020
WORKSHOP 1: Airway & Breathing Assessment
Basic Airway Management
Objectives:
1. Assess airway and breathing adequacy
2. Indications for emergency airway and positive pressure ventilation
3. Perform specific difficult airway assessment
4. Open airway and maintain airway with adjuncts
5. Perform suction safely & correctly
6. Understand different oxygen delivery devices
7. Perform bag valve mask ventilation correctly
8. Perform proper LMA insertion
WORKSHOP 2: Drugs Assisted Intubation
Approach to Difficult Airway
Objectives:
1. Understand & perform 7P’s of RSI
2. Proper technique of laryngeal intubation (direct and video laryngoscopy)
3. Understand the complications of intubation
4. Strategy for difficult airway management
5. Emergency cricothyroidectomy (needle and open technique)
6. Understand how to troubleshoot post-intubation problems
WORKSHOP 1
Objective 1: Assess airway & breathing adequacy
Assesment of airway patency: Look & Listen fo signs of airway obstruction
Look for – agitation, obtundation, deformity of the jaw, dentures, neck and cervical spine
Listen for – stridor, gurgling, hoarseness of voice
Assessment of breathing: Inspect, Palpate, Percuss, Auscultate (IPPA)
Inspect for – agitation, obtundation, tripod position, use of accessory muscles,
tachypnoea or bradypnoea, chest rise, chest symmetry, flail chest
Palpate for – crepitus, tenderness, tracheal deviation, apex beat
Percuss for – dullness, hyper-resonance
Auscultate for – rhonchi, crepitus, reduced or absent breath sounds
+/- objective asessment: SpO2, ABG, CXR, Lungs ultrasound
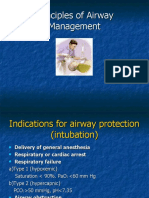
Objective 2: Assess indications for emergency airway and positive pressure ventilation
a) failure to protect airway: e.g. airway obstruction from any cause, reduced
conscious level, intoxication, airway injury, maxilofacial injury
b) failure of oxygenation, despite high concentration oxygen supplement : e.g.
hypoxic lung condition - pneumonia, pulmonary embolism
c) failure of ventilation: e.g. apnea, inadequate respiratory effort, respiratory
muscle paralysis
d) anticipated clinical deterioration: e.g. major burn, inhalational injury,
anaphylaxis
Objective 3: Perform specific difficult airway assessment
Objective 4: Open airway & maintain an open aiway with adjuncts
Non-trauma patients: head tilt chin lift
Trauma patients: Jaw trust or chin lift
Types of airway adjuncts:
Objective 5: Perform suction safely & correctly
Types of suction:
Yankauer suction
Catheter suction : diameter should not exceed
2/3 internal diameter of ETT
Suction pressure:
100-120mmHg – adult
80-100mmHg – children
60-80mmHg – infant
Complications of tracheobronchial suction:
1. Hypoxia from occlusion of ETT and disruption of oxygen flow, usually with
prolonged suctioning
2. Stimulation of vagal nerve causing vasovagal reaction – bradycardia and hypoxia
3. Physical injury to the airway, causing edema and bleeding
4. Introduce infection if not done with aseptic technique
Proper technique of tracheobronchial suction:
Objective 6: Understand different oxygen delivery devices
Oxygen delivery devize, flow rate and oxygen percentage delivered:
1. nasal cannula
Select the appropriate size prong for young adults and children
Maximum flow without humidification: *deliver dry cold air
- 2LPM children < 2 years
- 4LPM children > 2years
Increase in flow by 1LPM increase O2 percentage by 4%
Prolonged exposure to dry cold air may lead to airway inflammation, increase airway
resistance, impair mucociliary function & decrease mucus clearance
*High flow nasal cannula (HFNC) – deliver heated (37 degree C) and humidified air via
special delivery system.
Flow can be set to maximum 50-60 LPM to achieve FiO2 1.0
May deliver up to 1mmHg of PEEP with every 10LPM flow (with closed mouth nasal
breathing)
2. Simple face mask
Supply 35-60% oxygen with flow rate 6-10L/min
Oxygen concentration delivered also depends on:
-mask size and fit; tight or loose
-patient inspiratory flow rate
3. Venturi mask
Deliver an accurate and constant oxygen concentration for patients on controlled
oxygen therapy e.g. COPD or OSA with chronic hypoxia and CO2 retention (where high
FiO2 need to be avoided)
Use of Bernoulli principle: O2 is passed through a narrow orifice – the small diameter
of the tube create a high velocity flow–cause a drop in pressure which pulls room air
into the mask – the oxygen poor air (room air) mix with pure oxygen and give the
Oxygen percentage that is desired (24-60%)
4. Mask with Oxygen reservoir
Reservoir bag is attached to the gas flow
One way valve between the reservoir bag and patient – prevent expired air from
entering the reservoir bag and keep 600ml – 1L of pure oxygen inside
A sufficient oxygen flow is needed to prevent reservoir bag collapse during inspiration
The presence of unidirectional valves at each sides does not allow for outside air to
enter into the mask during inspiration, hence patient only inspire from the reservoir bag
However, FiO2 is difficult to achieve due to lack of tight fit mask and valve inefficiency
Objective 7: Perform bag-valve-mask ventilation correctly
Bag valve mask device consist of self-inflating bag, reservoir bag and valves - can be
connected to mask or advanced airway (e.g. laryngeal mask airway or endotracheal
tube) via a standard 15mm adapter
Provides positive pressure ventilation and PEEP with high flow oxygen
For spontaneously breathing patient; sufficient negative inspiratory pressure is
required to overcome the non-rebreathing valve – otherwise, there will be no air and
oxygen flow if the valve is not open (patient with poor respiratory effort is at risk)
Instead, coordinate manual bagging with patient’s own spontaneous effort to ensure the
valve is opening with every inhalation.
Bag-valve mask device consist of:
1. self-inflating bag – sizes 240ml, 500ml and 1600ml for infant, children and adult
(Laerdal)
2. oxygen inlet – connect to tubing and oxygen source
3. oxygen reservoir bag (to allow high concentration of oxygen) with 2 one-way valves: -
inlet valve allow room air to enter if the pressure in the bag is too low
- outlet valve allow oxygen to excape if pressure in the bag is excessive
4. expiratory valve/non-rebreathing valve – direct oxygen flow to patient & prevent
exhaled air (incl. vomitus, secretion) from entering the self-inflating bag.
5. Built in or detachable PEEP valve to the exhalation port with titratable PEEP 5-
15cmH2O, not to exceed 20 (this pressure can open lower esophageal sphincter, leading
to regurgitation and aspiration).
6. Pop-off valve: a pressure relieve valve – allow air to flow out when patient exhale as
to prevent barotrauma.
Technique for BVM: remember JAWS
J: jaw trust
A: airway adjunct
W: work together (2 person, ensure good mask seal, oxygen connected with flow of at
least 15LPM, coordinate with patient’s own spontaneous ventilation, observe for
adequate chest rise and other signs of improved oxygenation & ventilation)
S: slow, small squeeze – 6-7mls/kg over 1-2 seconds at 12 per minute
“Thenar eminence grip” – lift the face into the mask – this will also lift the oropharynx
away from the posterior wall
Adjustment that can be made if patient is edentulous (no teeth):
Complications:
1. hyperventilation
2. poor mask seal (esp if 1 hand CE clamp is used)
3. gastric distension, regurgitation, vomiting and aspiration
4. over pressurization and barotrauma
5. equipment failure e.g. incorrect assembly of bag-valve-mask device
Objective 8: Perform proper LMA insertion
Laryngeal mask airway (LMA) –a type of extraglottic airway device
Uses in ED/PHC:
-rescue device when intubation is unsuccessful (can’t intubate can ventilate scenario)
-temporary airway when intubation is not feasible/desirable immediately e.g. at the
scene/inside ambulance, during CPR
-facilitate blind insertion of bougie or ETT (intubating LMA e.g. FastTrack)
ProSeal
LMA consists of:
1. shaft (tube) with bite-block – prevent patient from biting and kinking the tube
2. proximal 15mm connector
3. distal end with broad elliptical inflatable cuff
– upper smooth suface that holds pharyngeal secretion and prevent it from entering the
larynx
- under surface (with airway tube and drain tube orifices) that sit over the larynx and
create a seal
4. pilot balloon
Methods of LMA insertion:
1. position patient in sniffing position
2. preparation: select correct sized LMA, inflate and deflate cuff to check for leak, apply
lubricant over the mask under surface
3. pre-oxygenate the patient with BVM ventilation before insertion
4. insert the deflated LMA with the mask face anteriorly, have an assistant to pull the
mandible downwards
5. follow the steps below
Contraindications:
1. Restricted mouth opening < 2 cm
2. Impassable upper airway obstruction
3. Patients with increased risk of regurgitation e.g.gastric obstruction, post meal,
pregnant > 10 weeks, obesity *relative contraindications in emergency
Complications:
1. Vomiting and aspiration
2. Dental and soft tissue trauma during insertion
WORKSHOP 2
Objective 1: Understand and perform 7Ps of RSI
Rapid sequence induction – sequential administration of induction agent and
neuromuscular blockade to facilitate endotrachea intubation.
For patients with intact gag reflex and full stomach requiring immediate airway control
Contraindications:
1. Anticipated difficult airway with total loss of facial and oropharyngeal landmarks or
total upper airway obstruction (require cricothyroidectomy)
2. Cardiac arrest (require crash intubation)
Component Description
Preparation 1. Equipments - MALES
M: Non rebreathing mask and BVM attached to 15LPM oxygen, nasal
cannula for apneic oxygenation
A: Airway (oropharyngeal, nasopharyngeal, LMA)
L: Laryngoscope with different size blades
E: ETT of different sizes
S: Suction, Syringe, Stethoscope
2. Personnel - intubator and assistants in appropriate PPE
3. Patient – assess for difficult airway
4. Environment – monitored area
Pre- 3 minutes or 6 vitals capacity breath with non-rebreathing mask 100%
oxygenation oxygen provide safe apnea time of 8 minutes in healthy adult
But in very ill patients – less than 1 minute
Options: NRB mask, BVM ventilation, NIV
Pre- Medications given to blunt the sympathetic effects of laryngoscopy and
treatment tracheal manipulation
Scant evidence of benefit
Consider for PREMED patients – pediatrics, resistance (asthma), elevated
ICP, MI, elevated BP, dissection
1. atropine 0.2 mg/kg – prevent bradycardia in children
2. fentanyl 2mcg/kg TBW – sympatholytic, neuroprotection in head
injury and vascular emergencies (AMI, aortic dissection)
3. lignocaine 1.5mg/kg – sympatholytic, neuroprotection in head injury,
decrease airway reactivity in asthma
Pre- Induction agents:
medication 1. midazolam 0.1-0.2mg/kg
Use; use in combination with fentanyl for patients who are already
obtunded
Drawback: slow onset, paradoxical agitation, resp depression,
hypotension
2. ethomidate 0.3 mg/kg
Use: suitable for haemodynamic instability & head injury,fast onset, avoid
in sepsis
Drawback: adrenal suppression, myoclonus
3. ketamine 1-2mg/kg
Use: haemodynamic instability, bronchospasm
Drawback: increased secretion, caution in heart disease – tachycardia,
hypertension
4. propofol 1-2 mg/kg IBW
Use: status epilepticus, hemodyamically stable, bronchospasm
Drawback: hypotension, myocardial depression
Paralytic agents:
1. suxamethonium 1-2mg/kg
Onset 45-60 seconds, duration 6-10 minutes
Drawback: hyperkalamia, malignant hyperthermia, bradycardia
2. rocuronium 1.2mg/kg IBW
Onset 45-60 seconds, duration 35-45 minutes
Drawback: avoid in anticipated difficult airway due to long paralysis time
Position Manual in-line immobilization in trauma
Ramp up with folded blankets in obese /pregnant patient
Placement Confirmation of placement by:
of ETT with 1. Direct visualization of ETT passing through the vocal cords
proof 2. 5 points auscultation, symmetrical chest expansion
3. End tidal capnography
Post- Secure the ETT with tape or tie
intubation Maintaining sedation with infusion
care Regular ETT suction
Ryles tube for stomach decompression, CBD
CXR
Appropriate ventilator setting, maintain haemodynamics
Objective 2: Proper technique of laryngeal intubation
Direct laryngoscopy
1. Position the patient
- involve distortion the normal anatomic planes of the upper airway to produce a line of
direct visualization from the operator’s eyes to the larynx
- this requires a new (non-anatomic) visual axis: by maximal alignment of the oral and
pharyngeal cavities and displacement of the tongue
- align the oral, pharyngeal and tracheal axis by careful flexion of the neck and extension
of the atlanto-occipital joint “sniffing position”
- this can be achieved with using folded blankets, towels or pillows
- patient should be placed on the most conducive position from the 1st attempt
normal anatomic plane
new non-anatomic visual plane
2. Patient’s mouth is opened with the thumb and index finger of the right hand using a
“scissor” technique. Laryngoscope blade is placed in the right side of the mouth, the
tongue is swept to the left and up into the floor of the pharynx by the blade’s flange.
3. With curved Macintosh blade: place the tip in the valecula – tense the glassoepiglottic
ligament – displace epiglottis out of the line of sight
With Miller straight blade: place the tip underneath the epiglottis – lift and compress
the epiglottis against the base of the tongue to visualize the vocal cord
With both blades – the handle are lifted up and away from the patient in the direction
perpendicular to patient’s mandible
Never use the upper teeth as the lever! (blade is lifted upward NOT backward)
4. BURP maneuvre (backward, upward, rightward) may applied at the larynx of the neck
by the intubator using his/her right hand – to improve visualization
5. The ETT cuff should be placed beyond the larynx, use the marking on the ETT as a
guide.
6. Inflate the cuff of the ETT to prevent air leak and aspiration. Pressure of the cuff
should not exceed 30mmHg – may impinge capillary blood flow and damage the tracheal
mucosa.
Video laryngoscopy
~4 steps procedure: mouth – screen – mouth – screen
1. mouth - look at the mouth as you insert the blade (as to avoid oral trauma)
2. screen - look at the screen to visualize the glottis then epiglottis
3. mouth - look at the mouth as you insert the ETT
4. screen - pass the tube through the vocal cords under video visualization
~3 key technical skills:
1. Blade is inserted in the midline, use a gentle rocking motion following the curvature of
the airway (instead of lifting motion used in direct laryngoscopy) until glottis is
visualized
2. Insert and advance the ETT following the curvature of the airway until the tip is
visualized on the screen
3. Use “stop, pop and drop” method: stop advancing the stylet once the tip pass through
the vocal cords – pop the stylet up and out of the tube for few centimeters – drop the
now partially non-styletted tube into the trachea
Objective 3: Complications of intubation & mechanical ventilation
Airway –
Dental trauma
Damage to airway: vocal cords injury, false passage creation
Esophageal intubation
Subglottic stenosis from high cuff pressure
Respiratory –
Endobronchial intubation
Aspiration
Bronchospasm (adverse drugs reaction)
Hypoxia from de-recruitment of lungs (atelectasis) during apnea
Sputum retention and pneumonia
Barotrauma
Cardiovascular –
Hypotension from RSI medications, adverse drugs reaction, obtundation of sympathetic
tone
Hypertension and tachycardia – from laryngoscopy and tracheal stimulation
Neurological –
Raised ICP secondary to laryngoscopy
Conversion to unstable spinal cord injury with cervical manipulation in trauma patients
Objective 4: Approach to difficult airway
Difficult airway definition:
One that requires multiple attempts, multiple operators, multiple devices, excessive
lifting force, external laryngeal manipulation or is performed with an inadequate glottic
view (uptoDate)
Suggested equipments for difficult airway preparation:
1. Laryngoscope blades of different designs (straight or curved) and sizes
2. Videolaryngoscope
3. ETT of different sizes
4. ETT guides: stylets, bougie, hyperangulated stylet, light wands, McGill forcep
5. Supraglottic airways: LMA, intubating LMA
6. Equipments for cricothyroidectomy
7. Flexible fibreoptic intubating equipments
Strategy for difficult airway management:
Plan A:
Maintain good positioning of the patient e.g. ramping up with blankets
Preoxygenation – HFM Oxygen / BVM / NIV
Apneic oxygenation in high risk patients
The importance of achieving full paralysis with neuromuscular block
The role of video laryngoscopy in anticipated difficult intubation
A maximum of 3 attempts at laryngoscopy (maintenance of oxygenation is priority)
Remove cricoid presusure when visualization is difficult
Plan B:
Declare failed intubation: call for help – personnel, difficult airway equipments
Priority is maintaining oxygenation with supraglottic airway device e.g. LMA
A maximum of 3 attempts at SAD insertion
May attempt intubation with SAD (intubating LMA)
Plan C:
Declare failed SAD ventilation
Attempt to oxygenate by face mask (BVM)
If face mask ventilation is possible, maintain ventilation and wake the patient up
*depending on underlying pathology
If face ventilation is unsuccessful, declare CICO and start Plan D
Continue attempts at oxygenation via BVM / SAD and nasal cannula
Plan D:
CICO (Can’t intubate Can’t oxygenate scenario) – proceed with front of neck access
Needle or open cricothyroidectomy technique
Continue attempts at oxygenation via BVM / SAD and nasal cannula
Objective 5: Emergency cricothyroidectomy (needle and surgical)
Indication: CICO scenario – airway rescue procedure
Contraindications:
Local infection
Unidentifiable anatomy – hematoma, swelling, distortion due to radiotherapy / trauma /
burn, morbid obesity
Children below 8-10 years where the CTM is not fully developed (for surgical approach)
Needle cricothyridectomy:
Insertion of a needle through the cricothyroid membrane (CTM) into the trachea
Use a large calibre cannula (12-14 gauge I adult, 16-18 gauge in children)
Ideally the cannula has to be attached to high pressure oxygen source – can be achieved
with jet ventilation
Attaching the cannula to BVM connected to standard wall or tank oxygen outlet does not
provide sufficient ventilation and will cause hypercarbia – only a temporizing measure
until surgical cricothyroidectomy can be performed / further attempts at laryngoscopy
and intubation.
Equipment for jet ventilation
Method of insertion:
1. extend the patient’s neck to ease identification of anatomy and procedure
2. Identify CTM and stabilize it with the non-dominant hand. Use the thumb and index
finger to stabilize the trachea with the thumb and middle fingers
3. Hold a 5 ml syringe (with 1-2ml of water) connected to 14G cannula
4. Insert the needle at 45 degree angle in a caudal direction.
5. Aspirate continuously as the needle is advanced and stop once air is aspirated and
immobilize the cannula (the endpoint is free aspiration of air and lack of plunger recoil)
6. Advance the cannula over the needle with your dominant hand and remove the
needle. Do not remove the needle before advancing the cannula fully, otherwise it will
kink.
7. Using a syringe with 1-2ml of water, connect it to the cannula and repeat air
aspiration from the cannula to reconfirm placement.
8. secure the cannula and connect to oxygen source
Surgical cricothyroidectomy:
A: Position the patient by extending the neck, palpate for the CTM and stabilize the
trache using non-dominant hand
B. Perform a single horizntal incision through the skin and CTM. If there is significant
adipose tissue and anatomy is unclear, perform a vertical incision first through the skin,
identify the CTM then perform a horizontal cut through the CTM.
C: rotate the scalpel 90 degrees.
D: Insert the bougie and railroad a well lubricated 6.0 ETT. Inflate the cuff and remove
the bougie. Confirm ETT placement and secure the ETT
Objective 6: How to troubleshoot post intubation problems
Causes of desaturation - DOPES
D: Disloged ETT
Recheck ETT depth, check for cuff leak
O: Obstruction – from secretion, kinking of tube, patient biting the tube
Pass suction cathether and perform suction, ensure patient is not biting the tube, apply
oropharyngeal airway to prevent biting
P: Pneumothorax
Recheck chest expansion, auscultation and percussion, perform lung ultrasound.
E: Equipment failure e.g. oxygen supply failure
Connect to BVM, recheck circuit, oxygen supply and ventilator setting.
S: Stacked breath – from auto PEEP/air trapping in patients with asthma/COPD
Disconnect from ventilator, allow exhalation for few seconds, recheck ventilator
settings, administer bronchodilators
How to fix? DOTTS
D: Disconnect ventilator and put on light pressure on patient’s breaths
O: Oxygen 15L/min with BVM – check for chest rise, air entry, resonance. Check for cuff
leak
T: Tube position and patency – Pass suction cathether all the way to remove obstruction,
make sure ETT is not kinked
T: Tweak the ventilator e.g. in breath stacking, need to increase expiratory time and
decrease RR
S: Sonography (ultrasound) to check for lungs sliding and CXR
“invest some of your time,
for your patients, it could mean a lifetime”
You might also like
- Teamwork Skill Communicating Effectively in GroupDocument21 pagesTeamwork Skill Communicating Effectively in Groupsiyalohia8No ratings yet
- Hospital Bill FormatDocument2 pagesHospital Bill Formatsandee1910100% (2)
- Basic Airway ManagementDocument98 pagesBasic Airway ManagementRani Salsabilah100% (1)
- (Oxy) Med-Surg Checklist With RationaleDocument13 pages(Oxy) Med-Surg Checklist With RationaleUri Perez MontedeRamos100% (1)
- Eradicate Hunger MoroccoDocument2 pagesEradicate Hunger Moroccoapi-257471763No ratings yet
- Stages of Artistic Development by Viktor LowenfeldDocument17 pagesStages of Artistic Development by Viktor LowenfeldMarie Joy GarmingNo ratings yet
- Critical Care SuctioningDocument5 pagesCritical Care SuctioningChinta Nabila 조롱 수없는No ratings yet
- Endotracheal TubeDocument19 pagesEndotracheal TubeSarvess Muniandy100% (1)
- Laboratory Unit 3 1Document6 pagesLaboratory Unit 3 1Mushy_ayaNo ratings yet
- Extubation TestDocument5 pagesExtubation TestMel GriffinNo ratings yet
- HANDOUTSDocument6 pagesHANDOUTSquennieNo ratings yet
- Respi Modalities 2Document6 pagesRespi Modalities 2Karlo ReyesNo ratings yet
- Bedside ClinicDocument6 pagesBedside Clinicyer tagalajNo ratings yet
- Oxygen DeliveryDocument8 pagesOxygen DeliveryCnette S. LumboNo ratings yet
- SuctioningDocument13 pagesSuctioningAmanda ScarletNo ratings yet
- Nursing Management of Clients With COPD: - Initiate Infusion of Intravenous Antibiotic As PrescribedDocument3 pagesNursing Management of Clients With COPD: - Initiate Infusion of Intravenous Antibiotic As PrescribedNiña AngNo ratings yet
- MMC OxyDocument13 pagesMMC OxyAira KieNo ratings yet
- Oxygen AdministrationDocument38 pagesOxygen AdministrationKate Angelique RodriguezNo ratings yet
- Methods of Oxygen AdministrationDocument3 pagesMethods of Oxygen AdministrationMenard Tobias VelascoNo ratings yet
- 12 OxygenationDocument46 pages12 Oxygenationjoshua florNo ratings yet
- Advanced Airway Care: Intensive Care Unit PerspectiveDocument42 pagesAdvanced Airway Care: Intensive Care Unit PerspectiveJeffery Samuel100% (1)
- Oxygen Delivery Systems: Under Guidance of Dr. Shraddha Patel by - Dr. Dhwani PatelDocument68 pagesOxygen Delivery Systems: Under Guidance of Dr. Shraddha Patel by - Dr. Dhwani PatelDeep ShahNo ratings yet
- Oxygen Delivery SystemsDocument9 pagesOxygen Delivery Systemsanon_784834955No ratings yet
- Assisting in Endotracheal SuctioningDocument38 pagesAssisting in Endotracheal SuctioningMargarita Limon BalunesNo ratings yet
- Rapid Sequence Intubation ReportDocument55 pagesRapid Sequence Intubation Reportlorkan19100% (1)
- UntitledDocument2 pagesUntitledAriana Oliveros CubelaNo ratings yet
- Oxygen Therapy AdministrationDocument15 pagesOxygen Therapy AdministrationMike Faustino Solangon100% (1)
- Oxygen TherapyDocument8 pagesOxygen TherapysumNo ratings yet
- Oxygen TherapyDocument4 pagesOxygen TherapyĐan TâmNo ratings yet
- Specimen Collection Sputum Skill COVID 19 Toolkit - 010320 PDFDocument7 pagesSpecimen Collection Sputum Skill COVID 19 Toolkit - 010320 PDFMary AlabiNo ratings yet
- SuctioningDocument5 pagesSuctioningNina Buenaventura100% (1)
- Administering Oxygen Therapy Powerpoint 3Document58 pagesAdministering Oxygen Therapy Powerpoint 3reema_rt75% (8)
- Mechanical VentilationDocument3 pagesMechanical VentilationDivine Mercy De JulianNo ratings yet
- Techniques of Oxygen DeliveryDocument55 pagesTechniques of Oxygen DeliveryRabi DhakalNo ratings yet
- KTP 1 RespiratoryDocument5 pagesKTP 1 RespiratoryMarisa TullochNo ratings yet
- DrowningDocument9 pagesDrowningAkshata HingeNo ratings yet
- Oxygen TherapyDocument74 pagesOxygen TherapyMark Reynie Renz Silva100% (6)
- Airway ManagementDocument18 pagesAirway ManagementReza ManefoNo ratings yet
- Airway Management: Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong KongDocument9 pagesAirway Management: Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong KongErwinRamadhaniNo ratings yet
- Assisting For Endotracheal IntubationDocument16 pagesAssisting For Endotracheal IntubationSREEDEVI T SURESH100% (1)
- First Two Steps Are Discussed in This SectionDocument26 pagesFirst Two Steps Are Discussed in This SectionArchanaShenoyNo ratings yet
- EMERGENCY MEDICINE - Basic - Airway - Management - PrintableDocument8 pagesEMERGENCY MEDICINE - Basic - Airway - Management - PrintableMedic DestinationNo ratings yet
- Suctioning: Endotracheal/ Tracheal Suctioning ProcedureDocument3 pagesSuctioning: Endotracheal/ Tracheal Suctioning ProcedureChristine_P_Es_229No ratings yet
- Ambu Beatmungsbeutel Silicone Gebrauchsanweisung Ab Seite12 in DeutschDocument108 pagesAmbu Beatmungsbeutel Silicone Gebrauchsanweisung Ab Seite12 in DeutschBo ScoobmanNo ratings yet
- Assissting IntubationDocument17 pagesAssissting IntubationTriciaNo ratings yet
- Medical ManagementDocument6 pagesMedical ManagementYORO MIKE ANGELO O.No ratings yet
- IV-C Safety Guidelines For Emergency Drugs, Endotracheal Set-Up and Defibrillator UseDocument21 pagesIV-C Safety Guidelines For Emergency Drugs, Endotracheal Set-Up and Defibrillator UseRio DanteNo ratings yet
- Ventilatory MNGTDocument31 pagesVentilatory MNGTlianrose448No ratings yet
- Oxygen Therapy: Yani Dewi Suryani Pediatric DepartementDocument22 pagesOxygen Therapy: Yani Dewi Suryani Pediatric DepartementFaishalNo ratings yet
- NCM 118 (Skills)Document45 pagesNCM 118 (Skills)akiNo ratings yet
- Care of Patients Requiring Oxygen Therapy or TracheostomyDocument5 pagesCare of Patients Requiring Oxygen Therapy or TracheostomyAnnie Rose Dorothy MamingNo ratings yet
- Oxygen TherapyDocument46 pagesOxygen Therapyoxidalaj100% (4)
- P 10 Ion StandardDocument5 pagesP 10 Ion StandardBeatrix RunkelNo ratings yet
- AiwaryManagement 1Document72 pagesAiwaryManagement 1Giselle EstoquiaNo ratings yet
- Ventilater CareDocument6 pagesVentilater CarehelenfreedaeqdNo ratings yet
- SECTION 2 CHAPTER 4 Tracheal IntubationDocument46 pagesSECTION 2 CHAPTER 4 Tracheal IntubationRhea Andrea UyNo ratings yet
- Ventilated Patient Care.Document25 pagesVentilated Patient Care.Rashmi BoraNo ratings yet
- Oxygen Therapy PDFDocument28 pagesOxygen Therapy PDFS01164503No ratings yet
- Oxygen InhalationDocument32 pagesOxygen Inhalationvarshasharma05100% (3)
- Airway ObstructionDocument10 pagesAirway ObstructionyoantamaraNo ratings yet
- Management of AirwaysDocument12 pagesManagement of AirwaysdyahNo ratings yet
- Principles of Airway Management.Document68 pagesPrinciples of Airway Management.Shimmering MoonNo ratings yet
- Clinical Profile of Patients of Central Serous Chorioretinopathy Presented To The Tertiary Health Care CentreDocument4 pagesClinical Profile of Patients of Central Serous Chorioretinopathy Presented To The Tertiary Health Care CentreIJAR JOURNALNo ratings yet
- Yoga Meditation Class Reservation Healthy Lifestyle Instagram StoryDocument16 pagesYoga Meditation Class Reservation Healthy Lifestyle Instagram StoryRanjell Allain Bayona TorresNo ratings yet
- Factsheet: E-Health in EstoniaDocument2 pagesFactsheet: E-Health in EstoniaNasrullah roslanNo ratings yet
- Collaborate Test Vocabulary Unit 4 PDFDocument5 pagesCollaborate Test Vocabulary Unit 4 PDFDesirée Serra AbellánNo ratings yet
- Report AL182C77837807491833 2023 07 07 R LDocument14 pagesReport AL182C77837807491833 2023 07 07 R LRishwan GuptaNo ratings yet
- School of Nursing Science and Research Sharda UniversityDocument5 pagesSchool of Nursing Science and Research Sharda UniversityBhawna JoshiNo ratings yet
- Pedia Patient ChartDocument16 pagesPedia Patient ChartClemerick PulancoNo ratings yet
- Exercises of Pronouns.Document3 pagesExercises of Pronouns.Alifzidan 86No ratings yet
- TAC L2P Learner Driver HandbookDocument5 pagesTAC L2P Learner Driver HandbookConnor GreenNo ratings yet
- dm2022 0394Document21 pagesdm2022 0394Arlo Winston De GuzmanNo ratings yet
- Message To All Applicants 2021Document3 pagesMessage To All Applicants 2021PGold Goodboy Golden RupNo ratings yet
- Introduction To HRMDocument12 pagesIntroduction To HRMmbusa josephNo ratings yet
- A Review of Mushrooms in Human Nutrition and HealthDocument14 pagesA Review of Mushrooms in Human Nutrition and HealthBegoña MartinezNo ratings yet
- Reymark L Bald Pe Interview Narrative ReportDocument3 pagesReymark L Bald Pe Interview Narrative ReportReymark BaldoNo ratings yet
- 2MADS StudyDocument7 pages2MADS StudyANA MARIA ELISA DIAZ DE LA GARZANo ratings yet
- Vacancy For: M&E OfficerDocument3 pagesVacancy For: M&E OfficerZawhtet HtetNo ratings yet
- Unit III. Theories of Human Development: Freud'S Psychoanalytic TheoryDocument4 pagesUnit III. Theories of Human Development: Freud'S Psychoanalytic TheoryHannah Gwyneth Riego MontefalcoNo ratings yet
- Clinical Psychology For Trainees 3rd Ed.Document363 pagesClinical Psychology For Trainees 3rd Ed.saeedz2100% (5)
- WoahDocument23 pagesWoahapi-665352428No ratings yet
- Class 13 - TreatmentDocument18 pagesClass 13 - TreatmentDaniela Pérez MartínezNo ratings yet
- Felicity Baker Music Therapy SongwritingDocument15 pagesFelicity Baker Music Therapy SongwritingSam CrowNo ratings yet
- HeavymetalinKelantanRiver PDFDocument20 pagesHeavymetalinKelantanRiver PDFwan marlinNo ratings yet
- Role of Physio in Neurological Disorders.Document17 pagesRole of Physio in Neurological Disorders.Maheen AnwaarNo ratings yet
- CH 08Document4 pagesCH 08Jessica Meagan Fullerton-SolanoNo ratings yet
- Assignment 1 CompleteDocument8 pagesAssignment 1 CompleteAsyraaf SaidNo ratings yet
- Basketball Is A Team Sport in WhichDocument4 pagesBasketball Is A Team Sport in Whichmohdrehan12No ratings yet