Professional Documents
Culture Documents
Respi and Cardio
Respi and Cardio
Uploaded by
Karlo Jose Dao-ayanCopyright:
Available Formats
You might also like
- Essential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsFrom EverandEssential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsRating: 3 out of 5 stars3/5 (5)
- 4 First Aid BFPDocument52 pages4 First Aid BFPJoyce FalladoNo ratings yet
- Framingham Risk ScoreDocument2 pagesFramingham Risk ScoreAsyiqin NasirNo ratings yet
- Scoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedDocument8 pagesScoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedKarlo Jose Dao-ayanNo ratings yet
- Competency Performance Checklist: Tagoloan Community CollegeDocument2 pagesCompetency Performance Checklist: Tagoloan Community CollegeRam AugustNo ratings yet
- PRS Heart Neck VesselsDocument2 pagesPRS Heart Neck VesselsIra Velle ViosNo ratings yet
- Midterm Activities 1Document7 pagesMidterm Activities 1ndxx4xsnfcNo ratings yet
- Checklist - Donning & Removing GlovesDocument1 pageChecklist - Donning & Removing GlovesKyle Ethan De la RiarteNo ratings yet
- Basic Assessment and Basic Care ProceduresDocument31 pagesBasic Assessment and Basic Care Proceduresjanice lopezNo ratings yet
- Module 1 Lesson 1 5 SPEAR 4FitnessAT - PrelimDocument17 pagesModule 1 Lesson 1 5 SPEAR 4FitnessAT - PrelimMichelle PeralesNo ratings yet
- RLENCM103 - Week 5 - Vital Signs (20230306144205) PDFDocument63 pagesRLENCM103 - Week 5 - Vital Signs (20230306144205) PDFMarian Kyla MarianoNo ratings yet
- Ibarondo NCM 101 Rle - Heart and Neck Vessels Assessment PDFDocument2 pagesIbarondo NCM 101 Rle - Heart and Neck Vessels Assessment PDFDenise IbarondoNo ratings yet
- HA Lab OBJECTIVESDocument21 pagesHA Lab OBJECTIVESAries CruzNo ratings yet
- Blood PressureDocument2 pagesBlood PressuremarilexdomagsangNo ratings yet
- 4 Objective Data PDFDocument97 pages4 Objective Data PDFrenz bartolomeNo ratings yet
- Module No. 1 Fitness Exercise Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDocument17 pagesModule No. 1 Fitness Exercise Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDovah KiinNo ratings yet
- Basic First Aid Vital Signs and Bandaging Techniques 11Document42 pagesBasic First Aid Vital Signs and Bandaging Techniques 11Darlene CarmonaNo ratings yet
- Basic First Aid Vital Signs and Bandaging TechniquesDocument42 pagesBasic First Aid Vital Signs and Bandaging TechniquesErisNo ratings yet
- 1Q W1 G12 - Performance Task 1.1 Continuation (HRF Procedure)Document5 pages1Q W1 G12 - Performance Task 1.1 Continuation (HRF Procedure)Jay LinesNo ratings yet
- MATUTE - Module-1-Lesson-1-SPEAR-1-Fitness-Assessment-TestDocument17 pagesMATUTE - Module-1-Lesson-1-SPEAR-1-Fitness-Assessment-TestRodel MatuteNo ratings yet
- Module No. 1 Physical Activities Towards Health and Fitness 2 Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDocument18 pagesModule No. 1 Physical Activities Towards Health and Fitness 2 Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameKurt RaftusNo ratings yet
- BP and HR Monitoring For ChildrenDocument5 pagesBP and HR Monitoring For Childrentao.careyNo ratings yet
- Cardiovascular Assessment - RDDocument2 pagesCardiovascular Assessment - RDANGELICA CLAIRE BARECUATRONo ratings yet
- Cast, PDFDocument26 pagesCast, PDFDrmirfat AlkashifNo ratings yet
- Module 1 Lesson 1 5 SPEAR 2 FitnessAT - PrelimDocument17 pagesModule 1 Lesson 1 5 SPEAR 2 FitnessAT - Prelimkit merandaNo ratings yet
- Lesson 2Document15 pagesLesson 2Arriene Chris Ocho DiongsonNo ratings yet
- Health Assessment of Lungs Breasts HeartDocument6 pagesHealth Assessment of Lungs Breasts HearttyuldeNo ratings yet
- Evaluation Tool: College of Nursing Document Code Revision No. 1 Effectivity Date January 2020Document7 pagesEvaluation Tool: College of Nursing Document Code Revision No. 1 Effectivity Date January 2020Gemmalene PaclebNo ratings yet
- Checklist BPDocument2 pagesChecklist BPHoneylouAzOpondaNo ratings yet
- Lesson 11 First AidDocument8 pagesLesson 11 First AidJojo ChuaNo ratings yet
- Vital SignsDocument12 pagesVital SignsLabs MendozaNo ratings yet
- Cardiovascular RD ScriptDocument9 pagesCardiovascular RD ScriptMary Joy Anne LucasNo ratings yet
- Peritoneal Dialysis: Performance Points I KnowledgeDocument12 pagesPeritoneal Dialysis: Performance Points I KnowledgeRafael RebongNo ratings yet
- AOP AdultDocument93 pagesAOP AdultKvothe EdemaRuhNo ratings yet
- First Aid and Water SafetyDocument14 pagesFirst Aid and Water SafetyASHLEY JOY ARZADON (SCJE)No ratings yet
- Assignment 3 - Business LiteracyDocument6 pagesAssignment 3 - Business Literacymaleisha kistenNo ratings yet
- Lesson 4 - Pulse RateDocument6 pagesLesson 4 - Pulse RatexXmineskingXxNo ratings yet
- Performance Checklist in Assessing The Cardiovascular SystemDocument3 pagesPerformance Checklist in Assessing The Cardiovascular SystemZaina RodrigoNo ratings yet
- Clinical Lab Skills Assignment 2Document9 pagesClinical Lab Skills Assignment 2Daniel WoodardNo ratings yet
- Checklist Female and Male Breast Heart and NeckDocument4 pagesChecklist Female and Male Breast Heart and NeckShades ofyellowNo ratings yet
- NCM 107 RLE Module 2 Nov 16 18 2020Document34 pagesNCM 107 RLE Module 2 Nov 16 18 2020mirai desuNo ratings yet
- Apex BeatDocument22 pagesApex BeatdanielNo ratings yet
- Evaluative Tool For NRG 105 Assessing The AbdomenDocument18 pagesEvaluative Tool For NRG 105 Assessing The AbdomenKhim BalcitaNo ratings yet
- Checklist 7 Assessment of Cardiovascular System and AbdomenDocument3 pagesChecklist 7 Assessment of Cardiovascular System and AbdomenDaniel Ray QuintanillaNo ratings yet
- Adult CPRDocument19 pagesAdult CPRMinalin FSNo ratings yet
- Hse Training Manual ThreeDocument61 pagesHse Training Manual ThreeEneyo VictorNo ratings yet
- Maternal and Child Health Nursing Ii: Nurse Hooman, RN 2020Document130 pagesMaternal and Child Health Nursing Ii: Nurse Hooman, RN 2020Charlaine Gripal SudlaNo ratings yet
- Vital SignsDocument32 pagesVital SignsJacqueline de AsisNo ratings yet
- Module 1 Lesson 1 SPEAR 1 Fitness Assessment TestDocument15 pagesModule 1 Lesson 1 SPEAR 1 Fitness Assessment TestKlent CabrasNo ratings yet
- Nated Unit2roughdraft&coverletterDocument9 pagesNated Unit2roughdraft&coverletterapi-284277228No ratings yet
- I. EmergencyDocument10 pagesI. EmergencyGloryJaneNo ratings yet
- Health Assessment SAS Session 3Document5 pagesHealth Assessment SAS Session 3Mary Maxiluch TabudlongNo ratings yet
- Nated Unit2finaldraftDocument10 pagesNated Unit2finaldraftapi-284277228No ratings yet
- Maternal and Child Health Nursing Ii: Krishan Soriano, MSNDocument130 pagesMaternal and Child Health Nursing Ii: Krishan Soriano, MSNjay5ar5jamorabon5torNo ratings yet
- 2 Neck AssessmentDocument3 pages2 Neck AssessmentAbsalon, J. A. (2201986)No ratings yet
- PRS Thorax Lungs by WeberDocument3 pagesPRS Thorax Lungs by WeberIra Velle ViosNo ratings yet
- Taking Vital Signs of A PatientDocument28 pagesTaking Vital Signs of A PatientkavithsamuelNo ratings yet
- Physical Fitness Test DepedDocument36 pagesPhysical Fitness Test DepedMark John DomingoNo ratings yet
- Assessing AbdomenDocument2 pagesAssessing AbdomenXoisagesNo ratings yet
- Fitness Evaluation of the HorseFrom EverandFitness Evaluation of the HorseRating: 5 out of 5 stars5/5 (1)
- Coc - Revised Curriculum For BS Nursing Program, Sy 2020-2021Document3 pagesCoc - Revised Curriculum For BS Nursing Program, Sy 2020-2021Karlo Jose Dao-ayanNo ratings yet
- 19 Karlo Jose Dao-AyanDocument1 page19 Karlo Jose Dao-AyanKarlo Jose Dao-ayanNo ratings yet
- Assessing ViolenceDocument6 pagesAssessing ViolenceKarlo Jose Dao-ayanNo ratings yet
- Scoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedDocument8 pagesScoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedKarlo Jose Dao-ayanNo ratings yet
- Kelompok 1Document22 pagesKelompok 1teguhNo ratings yet
- Urologi: NO Diagnosis Kode Icd 10Document9 pagesUrologi: NO Diagnosis Kode Icd 10dokter jaga rskb ddsNo ratings yet
- Daftar Pustaka 190719 FixDocument6 pagesDaftar Pustaka 190719 FixyopiNo ratings yet
- Physical Characteristics and VolumeDocument10 pagesPhysical Characteristics and Volumedeepika kushwahNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar. BMJ 2019 PDFDocument15 pagesDiabetic Ketoacidosis and Hyperosmolar. BMJ 2019 PDFJavier Marcano100% (1)
- IntroductionDocument27 pagesIntroductionJan Dominic GUCORNo ratings yet
- Araceli LabDocument268 pagesAraceli LabAldea MangalimanNo ratings yet
- Post Intubation HypotensionDocument37 pagesPost Intubation Hypotensionfifa_0304535100% (1)
- CHNDocument14 pagesCHNAi IrenNo ratings yet
- Blood Suppy of BrainDocument54 pagesBlood Suppy of BrainZoya MoraniNo ratings yet
- Corrected 1041 File Part 1Document160 pagesCorrected 1041 File Part 1walebayo06No ratings yet
- Approach To The Patient With Aphasia - UpToDate PDFDocument13 pagesApproach To The Patient With Aphasia - UpToDate PDFMiguel Garcia100% (1)
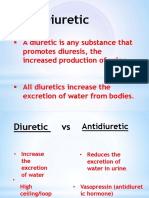
- Diuretic: A Diuretic Is Any Substance ThatDocument17 pagesDiuretic: A Diuretic Is Any Substance ThatAnalizaNo ratings yet
- NEUROPHARMACOLOGYDocument36 pagesNEUROPHARMACOLOGYDebika DasNo ratings yet
- Health9 Q2 Mod3 Drugs Version2Document13 pagesHealth9 Q2 Mod3 Drugs Version2angel winer100% (1)
- Visual Dysfunction in Diabetes PDFDocument395 pagesVisual Dysfunction in Diabetes PDFMarcosNo ratings yet
- UNANSWERED Past Plab 1700 McqsDocument260 pagesUNANSWERED Past Plab 1700 McqsHassaan Imtiaz100% (5)
- Restorative Periodontal Interrelationship: Sreeraj R S, Bindu R NayarDocument8 pagesRestorative Periodontal Interrelationship: Sreeraj R S, Bindu R NayarsujeetNo ratings yet
- Gangguan Haid - PPT YudisDocument34 pagesGangguan Haid - PPT YudisIde Yudis TiyoNo ratings yet
- Psychological Report Writing: Adapted From UP-PGH FormatDocument22 pagesPsychological Report Writing: Adapted From UP-PGH FormatAhmad AliNo ratings yet
- Chapter 44-Activity and ExerciseDocument4 pagesChapter 44-Activity and ExerciseollietonkNo ratings yet
- Heart Attack EssayDocument2 pagesHeart Attack EssayRatih ParamitaNo ratings yet
- Manual - HALODocument42 pagesManual - HALOsanthigiNo ratings yet
- Case For Acute GastroenteritisDocument26 pagesCase For Acute GastroenteritisSheana TmplNo ratings yet
- Status EpilepticusDocument21 pagesStatus EpilepticusbushraNo ratings yet
- Types of Wounds & ManagementDocument19 pagesTypes of Wounds & ManagementHina BatoolNo ratings yet
- Mammography For Breast Cancer ScreeningDocument26 pagesMammography For Breast Cancer Screeningaufar syehan100% (1)
- Vaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDADocument1 pageVaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDAAbdul YounusNo ratings yet
- Teaching Plan PDFDocument92 pagesTeaching Plan PDFRoxanne Jane S. Graycochea100% (1)
Respi and Cardio
Respi and Cardio
Uploaded by
Karlo Jose Dao-ayanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respi and Cardio
Respi and Cardio
Uploaded by
Karlo Jose Dao-ayanCopyright:
Available Formats
NAME: DATE:
CN: C.I.:
Scoring: 1- Excellent 2- Very Good 3- Satisfactory 4- Needs Improvement 5- Failed
100=1.00 95=1.30 90=1.75 85=2.20 80=2.60 75=3.00 70=3.40 65=3.80 60=4.25 55=4.70
99=1.00 94=1.40 89=1.80 84=2.25 79=2.70 74=3.10 69=3.50 64=3.90 59=4.30 54=4.75
98=1.10 93=1.50 88=1.90 83=2.30 78=2.75 73=3.20 68=3.60 63=4.00 58=4.40 53=4.80
97=1.20 92=1.60 87=2.00 82=2.40 77=2.80 72=3.25 67=3.70 62=4.10 57=4.50 52=4.90
96=1.25 91=1.70 86=2.10 81=2.50 76=2.90 71=3.30 66=3.75 61=4.20 56=4.60 51=5.00
ASSESSING THE RESPIRATORY SYSTEM
CHECKLIST 1 2 3 4 5
1. Gather all equipment.
• Examination gown and drape
• Gloves
• Stethoscope
• Light source
• Mask
• Skin marker
• Metric ruler
2. Perform Hand hygiene and explain procedure to patient
3. Provide privacy and expose only the part to be examined.
INSPECTION
4. Anterior/Posterior/Lateral. Compare side to side. Work apex to
base
5. Assess respiratory rate and rhythm, depth, symmetry for chest
movement
6. Assess AP ratio, costal angle, spinal deformities muscles for
breathing and condition of skin
PALPATION
7. Anterior/Posterior/Lateral. Compare side to side. Work apex to
base
8. Palpate the trachea.
9. Palpate chest for tenderness and sensation.
10. Palpate the chest for crepitus and other abnormalities.
Crepitus- Use your fingers and follow the appropriate
sequence when palpating. Note if there is a crackling sensation
(like bones or hairs rubbing against each other) as you palpate.
11. Assess for tactile fremitus. Use the ball or ulnar edge of one
hand to assess for fremitus. As you move your hand to each
area, ask the client to say “ninety-nine.” Assess all areas for
symmetry and intensity of vibration.
12. Assess for chest expansion. Place your hands on the posterior
chest wall with your thumbs at the level of T9 or T10 and
pressing together a small skin fold. As the client takes a deep
breath, observe the movement of your thumbs
PERCUSSION
13. Percuss Anterior/Posterior/Lateral portion of chest.
14. Note general percussion sound of chest.
15. Percuss for diaphragmatic chest excursion.
• Ask the client to exhale forcefully and hold the
breath. Beginning at the scapular line (T7), percuss
the intercostal spaces of the right posterior chest
wall.
• Percuss downward until the tone changes from
resonance to dullness. Mark this level and allow the
client to breathe.
• Next ask the client to inhale deeply and hold it.
Percuss the intercostal spaces from the mark
downward until resonance changes to dullness.
Revised: January 2020
NAME: DATE:
CN: C.I.:
Scoring: 1- Excellent 2- Very Good 3- Satisfactory 4- Needs Improvement 5- Failed
100=1.00 95=1.30 90=1.75 85=2.20 80=2.60 75=3.00 70=3.40 65=3.80 60=4.25 55=4.70
99=1.00 94=1.40 89=1.80 84=2.25 79=2.70 74=3.10 69=3.50 64=3.90 59=4.30 54=4.75
98=1.10 93=1.50 88=1.90 83=2.30 78=2.75 73=3.20 68=3.60 63=4.00 58=4.40 53=4.80
97=1.20 92=1.60 87=2.00 82=2.40 77=2.80 72=3.25 67=3.70 62=4.10 57=4.50 52=4.90
96=1.25 91=1.70 86=2.10 81=2.50 76=2.90 71=3.30 66=3.75 61=4.20 56=4.60 51=5.00
• Mark the level and allow the client to breathe.
Measure the distance between the two marks.
AUSCULTATION
16. Use diaphragm of stethoscope. Have patient take slow, deep
breaths through mouth.
17. Assess Anterior/Posterior/Lateral. Compare side to side, apex
to base.
18. Assess breath sounds (bronchial, bronchovesicular, vesicular)
• Bronchial- heard over the trachea and thorax.
• Bronchovesicular- heard over the major bronchi—
posterior: between the scapulae; anterior: around the
upper sternum in the first and second intercostal spaces.
• Vesicular- heard over the peripheral lung fields.
19. Assess for voice sounds.
• Bronchophony: Ask the client to repeat the phrase
“ninety-nine” while you auscultate the chest wall.
• Egophony: Ask the client to repeat the letter “E” while
you listen over the chest wall.
• Whispered pectoriloquy: Ask the client to whisper the
phrase “one–two–three” while you auscultate the chest
wall.
20. After the assessment, make the patient comfortable and
perform hand hygiene. Do after care.
21. Document the data.
TOTAL SCORE = ______ = ______ %
21
Revised: January 2020
NAME: DATE:
CN: C.I.:
Scoring: 1- Excellent 2- Very Good 3- Satisfactory 4- Needs Improvement 5- Failed
100=1.00 95=1.30 90=1.75 85=2.20 80=2.60 75=3.00 70=3.40 65=3.80 60=4.25 55=4.70
99=1.00 94=1.40 89=1.80 84=2.25 79=2.70 74=3.10 69=3.50 64=3.90 59=4.30 54=4.75
98=1.10 93=1.50 88=1.90 83=2.30 78=2.75 73=3.20 68=3.60 63=4.00 58=4.40 53=4.80
97=1.20 92=1.60 87=2.00 82=2.40 77=2.80 72=3.25 67=3.70 62=4.10 57=4.50 52=4.90
96=1.25 91=1.70 86=2.10 81=2.50 76=2.90 71=3.30 66=3.75 61=4.20 56=4.60 51=5.00
ASSESSING THE CARDIOVASCULAR SYSTEM
CHECKLIST 1 2 3 4 5
1. Assemble equipment
2. Remove jewelry, if possible, and secure in a safe place. A plain wedding band may
remain in place.
3. Introduce yourself, and verify the client’s identity. Explain to the procedure to the
client and how the client can cooperate.
4. Perform hand hygiene, and observe other appropriate infection control procedures.
Provide for client privacy.
5. Inquire if the client has any history of the following:
- Family history of incidence and age of heart disease, high cholesterol levels, high
blood pressure, stroke, obesity, congenital heart disease, hypertension, and
rheumatic fever
- Client’s past history of rheumatic fever, heart murmur, heart attack, varicosities,
or heart failure
- Present symptoms indicative of heart disease
- Presence of diseases that affect the heart
- Lifestyle habits that are risk factors for cardiac disease
NECK VESSELS
INSPECTION
6. Inspect the jugular veins for distention. The client is placed in a semi-Fowler’s
position, with the head supported on a small pillow.
7. If jugular vein distention is present, assess the jugular venous pressure (JVP)
- Locate the highest visible point of distention of the internal jugular vein.
- Measure the vertical height of this point in centimeters from the sternal angle,
the point at which the clavicles meet.
- Repeat the steps above on the other side.
AUSCULTATION
8. Auscultate the carotid arteries.
- Always auscultate the carotid artery first before palpating because palpation
may increase or slow the heart rate, changing the strength of the carotid impulse
heard
- Place the bell of the stethoscope over the carotid artery and ask the client to
hold his or her breath for a moment so that breath sounds do not conceal any
vascular sounds.
- Auscultate for bruit.
PALPATION
9. If occlusion is detected during auscultation, palpate very lightly to avoid blocking
circulation or triggering vagal stimulation and bradycardia, hypotension, or even
cardiac arrest.
10. Palpate the carotid arteries.
- Palpate each carotid artery alternately.
- Bilateral palpation could result in reduced cerebral blood low.
- Place the pads of the index and middle fingers medial to the
sternocleidomastoid muscle on the neck.
- Note amplitude and contour of the pulse, elasticity of the artery, and any thrills.
Revised: January 2020
NAME: DATE:
CN: C.I.:
Scoring: 1- Excellent 2- Very Good 3- Satisfactory 4- Needs Improvement 5- Failed
100=1.00 95=1.30 90=1.75 85=2.20 80=2.60 75=3.00 70=3.40 65=3.80 60=4.25 55=4.70
99=1.00 94=1.40 89=1.80 84=2.25 79=2.70 74=3.10 69=3.50 64=3.90 59=4.30 54=4.75
98=1.10 93=1.50 88=1.90 83=2.30 78=2.75 73=3.20 68=3.60 63=4.00 58=4.40 53=4.80
97=1.20 92=1.60 87=2.00 82=2.40 77=2.80 72=3.25 67=3.70 62=4.10 57=4.50 52=4.90
96=1.25 91=1.70 86=2.10 81=2.50 76=2.90 71=3.30 66=3.75 61=4.20 56=4.60 51=5.00
HEART (PRECORDIUM)
INSPECTION
11. Inspect the aortic and pulmonic areas, observing them at an angle and to the side, to
note the presence or absence of pulsations
12. Inspect for Apical Impulse.
- This represents the brief early pulsation of the left ventricle as it moves
anteriorly during contraction and through the chest wall located at 4 th or 5th
intercostal Space (ICS).
- If displaced laterally, record distance between the apex and the MCL in
centimeters
13. Inspect epigastric area at the base of the sternum for abdominal aortic pulsations
PALPATION
14. Palpate the aortic and pulmonic areas, observing them at an angle and to the side, to
note the presence or absence of pulsations
15. Palpate Apical Impulse. You may ask the client to roll to the left side to better feel the
impulse using palmar surfaces of the hand.
16. Palpate epigastric area at the base of the sternum for abdominal aortic pulsations.
PERCUSSION
17. Percussion estimates cardiac border.
- Determine size and location of heart, note displacement or enlargement.
- There should be dullness at 3rd, 4th and 5th ICS to the left sternum at left mid-
clavicular line.
- Begin at the anterior axillary line and percuss to the sternum at the 5 th ICS.
- There should be a change of sound from resonance to dullness as you reach the
left sternal border of the heart.
AUSCULTATION
18. Auscultate for S1, S2, S3, S4 and murmurs.
19. Auscultate from apex to base; mitral, tricuspid, Erb’s point, pulmonic and aortic areas,
noting for murmurs, rate, rhythm, pitch and intensity, duration, timing, quality and
location.
LOCATION:
• Aortic area: Second ICS at the right sternal border—the base of the heart
• Pulmonic area: Second or third ICS at the left sternal border—the base of the
heart
• Erb point: Third ICS at the left sternal border
• Mitral (apical): Fifth ICS near the left MCL—the apex of the heart
• Tricuspid area: Fourth or fifth ICS at the left lower sternal border
20. After the assessment, make the patient comfortable. Perform hand hygiene and do
after care.
21. Document findings in the client record.
TOTAL SCORE = ______ = ______ %
21
Revised: January 2020
You might also like
- Essential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsFrom EverandEssential Examination, third edition: Step-by-step guides to clinical examination scenarios with practical tips and key facts for OSCEsRating: 3 out of 5 stars3/5 (5)
- 4 First Aid BFPDocument52 pages4 First Aid BFPJoyce FalladoNo ratings yet
- Framingham Risk ScoreDocument2 pagesFramingham Risk ScoreAsyiqin NasirNo ratings yet
- Scoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedDocument8 pagesScoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedKarlo Jose Dao-ayanNo ratings yet
- Competency Performance Checklist: Tagoloan Community CollegeDocument2 pagesCompetency Performance Checklist: Tagoloan Community CollegeRam AugustNo ratings yet
- PRS Heart Neck VesselsDocument2 pagesPRS Heart Neck VesselsIra Velle ViosNo ratings yet
- Midterm Activities 1Document7 pagesMidterm Activities 1ndxx4xsnfcNo ratings yet
- Checklist - Donning & Removing GlovesDocument1 pageChecklist - Donning & Removing GlovesKyle Ethan De la RiarteNo ratings yet
- Basic Assessment and Basic Care ProceduresDocument31 pagesBasic Assessment and Basic Care Proceduresjanice lopezNo ratings yet
- Module 1 Lesson 1 5 SPEAR 4FitnessAT - PrelimDocument17 pagesModule 1 Lesson 1 5 SPEAR 4FitnessAT - PrelimMichelle PeralesNo ratings yet
- RLENCM103 - Week 5 - Vital Signs (20230306144205) PDFDocument63 pagesRLENCM103 - Week 5 - Vital Signs (20230306144205) PDFMarian Kyla MarianoNo ratings yet
- Ibarondo NCM 101 Rle - Heart and Neck Vessels Assessment PDFDocument2 pagesIbarondo NCM 101 Rle - Heart and Neck Vessels Assessment PDFDenise IbarondoNo ratings yet
- HA Lab OBJECTIVESDocument21 pagesHA Lab OBJECTIVESAries CruzNo ratings yet
- Blood PressureDocument2 pagesBlood PressuremarilexdomagsangNo ratings yet
- 4 Objective Data PDFDocument97 pages4 Objective Data PDFrenz bartolomeNo ratings yet
- Module No. 1 Fitness Exercise Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDocument17 pagesModule No. 1 Fitness Exercise Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDovah KiinNo ratings yet
- Basic First Aid Vital Signs and Bandaging Techniques 11Document42 pagesBasic First Aid Vital Signs and Bandaging Techniques 11Darlene CarmonaNo ratings yet
- Basic First Aid Vital Signs and Bandaging TechniquesDocument42 pagesBasic First Aid Vital Signs and Bandaging TechniquesErisNo ratings yet
- 1Q W1 G12 - Performance Task 1.1 Continuation (HRF Procedure)Document5 pages1Q W1 G12 - Performance Task 1.1 Continuation (HRF Procedure)Jay LinesNo ratings yet
- MATUTE - Module-1-Lesson-1-SPEAR-1-Fitness-Assessment-TestDocument17 pagesMATUTE - Module-1-Lesson-1-SPEAR-1-Fitness-Assessment-TestRodel MatuteNo ratings yet
- Module No. 1 Physical Activities Towards Health and Fitness 2 Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameDocument18 pagesModule No. 1 Physical Activities Towards Health and Fitness 2 Lesson No. 1-5 Fitness Assessment Test Learning Outcomes Time FrameKurt RaftusNo ratings yet
- BP and HR Monitoring For ChildrenDocument5 pagesBP and HR Monitoring For Childrentao.careyNo ratings yet
- Cardiovascular Assessment - RDDocument2 pagesCardiovascular Assessment - RDANGELICA CLAIRE BARECUATRONo ratings yet
- Cast, PDFDocument26 pagesCast, PDFDrmirfat AlkashifNo ratings yet
- Module 1 Lesson 1 5 SPEAR 2 FitnessAT - PrelimDocument17 pagesModule 1 Lesson 1 5 SPEAR 2 FitnessAT - Prelimkit merandaNo ratings yet
- Lesson 2Document15 pagesLesson 2Arriene Chris Ocho DiongsonNo ratings yet
- Health Assessment of Lungs Breasts HeartDocument6 pagesHealth Assessment of Lungs Breasts HearttyuldeNo ratings yet
- Evaluation Tool: College of Nursing Document Code Revision No. 1 Effectivity Date January 2020Document7 pagesEvaluation Tool: College of Nursing Document Code Revision No. 1 Effectivity Date January 2020Gemmalene PaclebNo ratings yet
- Checklist BPDocument2 pagesChecklist BPHoneylouAzOpondaNo ratings yet
- Lesson 11 First AidDocument8 pagesLesson 11 First AidJojo ChuaNo ratings yet
- Vital SignsDocument12 pagesVital SignsLabs MendozaNo ratings yet
- Cardiovascular RD ScriptDocument9 pagesCardiovascular RD ScriptMary Joy Anne LucasNo ratings yet
- Peritoneal Dialysis: Performance Points I KnowledgeDocument12 pagesPeritoneal Dialysis: Performance Points I KnowledgeRafael RebongNo ratings yet
- AOP AdultDocument93 pagesAOP AdultKvothe EdemaRuhNo ratings yet
- First Aid and Water SafetyDocument14 pagesFirst Aid and Water SafetyASHLEY JOY ARZADON (SCJE)No ratings yet
- Assignment 3 - Business LiteracyDocument6 pagesAssignment 3 - Business Literacymaleisha kistenNo ratings yet
- Lesson 4 - Pulse RateDocument6 pagesLesson 4 - Pulse RatexXmineskingXxNo ratings yet
- Performance Checklist in Assessing The Cardiovascular SystemDocument3 pagesPerformance Checklist in Assessing The Cardiovascular SystemZaina RodrigoNo ratings yet
- Clinical Lab Skills Assignment 2Document9 pagesClinical Lab Skills Assignment 2Daniel WoodardNo ratings yet
- Checklist Female and Male Breast Heart and NeckDocument4 pagesChecklist Female and Male Breast Heart and NeckShades ofyellowNo ratings yet
- NCM 107 RLE Module 2 Nov 16 18 2020Document34 pagesNCM 107 RLE Module 2 Nov 16 18 2020mirai desuNo ratings yet
- Apex BeatDocument22 pagesApex BeatdanielNo ratings yet
- Evaluative Tool For NRG 105 Assessing The AbdomenDocument18 pagesEvaluative Tool For NRG 105 Assessing The AbdomenKhim BalcitaNo ratings yet
- Checklist 7 Assessment of Cardiovascular System and AbdomenDocument3 pagesChecklist 7 Assessment of Cardiovascular System and AbdomenDaniel Ray QuintanillaNo ratings yet
- Adult CPRDocument19 pagesAdult CPRMinalin FSNo ratings yet
- Hse Training Manual ThreeDocument61 pagesHse Training Manual ThreeEneyo VictorNo ratings yet
- Maternal and Child Health Nursing Ii: Nurse Hooman, RN 2020Document130 pagesMaternal and Child Health Nursing Ii: Nurse Hooman, RN 2020Charlaine Gripal SudlaNo ratings yet
- Vital SignsDocument32 pagesVital SignsJacqueline de AsisNo ratings yet
- Module 1 Lesson 1 SPEAR 1 Fitness Assessment TestDocument15 pagesModule 1 Lesson 1 SPEAR 1 Fitness Assessment TestKlent CabrasNo ratings yet
- Nated Unit2roughdraft&coverletterDocument9 pagesNated Unit2roughdraft&coverletterapi-284277228No ratings yet
- I. EmergencyDocument10 pagesI. EmergencyGloryJaneNo ratings yet
- Health Assessment SAS Session 3Document5 pagesHealth Assessment SAS Session 3Mary Maxiluch TabudlongNo ratings yet
- Nated Unit2finaldraftDocument10 pagesNated Unit2finaldraftapi-284277228No ratings yet
- Maternal and Child Health Nursing Ii: Krishan Soriano, MSNDocument130 pagesMaternal and Child Health Nursing Ii: Krishan Soriano, MSNjay5ar5jamorabon5torNo ratings yet
- 2 Neck AssessmentDocument3 pages2 Neck AssessmentAbsalon, J. A. (2201986)No ratings yet
- PRS Thorax Lungs by WeberDocument3 pagesPRS Thorax Lungs by WeberIra Velle ViosNo ratings yet
- Taking Vital Signs of A PatientDocument28 pagesTaking Vital Signs of A PatientkavithsamuelNo ratings yet
- Physical Fitness Test DepedDocument36 pagesPhysical Fitness Test DepedMark John DomingoNo ratings yet
- Assessing AbdomenDocument2 pagesAssessing AbdomenXoisagesNo ratings yet
- Fitness Evaluation of the HorseFrom EverandFitness Evaluation of the HorseRating: 5 out of 5 stars5/5 (1)
- Coc - Revised Curriculum For BS Nursing Program, Sy 2020-2021Document3 pagesCoc - Revised Curriculum For BS Nursing Program, Sy 2020-2021Karlo Jose Dao-ayanNo ratings yet
- 19 Karlo Jose Dao-AyanDocument1 page19 Karlo Jose Dao-AyanKarlo Jose Dao-ayanNo ratings yet
- Assessing ViolenceDocument6 pagesAssessing ViolenceKarlo Jose Dao-ayanNo ratings yet
- Scoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedDocument8 pagesScoring: 1-Excellent 2 - Very Good 3 - Satisfactory 4 - Needs Improvement 5 - FailedKarlo Jose Dao-ayanNo ratings yet
- Kelompok 1Document22 pagesKelompok 1teguhNo ratings yet
- Urologi: NO Diagnosis Kode Icd 10Document9 pagesUrologi: NO Diagnosis Kode Icd 10dokter jaga rskb ddsNo ratings yet
- Daftar Pustaka 190719 FixDocument6 pagesDaftar Pustaka 190719 FixyopiNo ratings yet
- Physical Characteristics and VolumeDocument10 pagesPhysical Characteristics and Volumedeepika kushwahNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar. BMJ 2019 PDFDocument15 pagesDiabetic Ketoacidosis and Hyperosmolar. BMJ 2019 PDFJavier Marcano100% (1)
- IntroductionDocument27 pagesIntroductionJan Dominic GUCORNo ratings yet
- Araceli LabDocument268 pagesAraceli LabAldea MangalimanNo ratings yet
- Post Intubation HypotensionDocument37 pagesPost Intubation Hypotensionfifa_0304535100% (1)
- CHNDocument14 pagesCHNAi IrenNo ratings yet
- Blood Suppy of BrainDocument54 pagesBlood Suppy of BrainZoya MoraniNo ratings yet
- Corrected 1041 File Part 1Document160 pagesCorrected 1041 File Part 1walebayo06No ratings yet
- Approach To The Patient With Aphasia - UpToDate PDFDocument13 pagesApproach To The Patient With Aphasia - UpToDate PDFMiguel Garcia100% (1)
- Diuretic: A Diuretic Is Any Substance ThatDocument17 pagesDiuretic: A Diuretic Is Any Substance ThatAnalizaNo ratings yet
- NEUROPHARMACOLOGYDocument36 pagesNEUROPHARMACOLOGYDebika DasNo ratings yet
- Health9 Q2 Mod3 Drugs Version2Document13 pagesHealth9 Q2 Mod3 Drugs Version2angel winer100% (1)
- Visual Dysfunction in Diabetes PDFDocument395 pagesVisual Dysfunction in Diabetes PDFMarcosNo ratings yet
- UNANSWERED Past Plab 1700 McqsDocument260 pagesUNANSWERED Past Plab 1700 McqsHassaan Imtiaz100% (5)
- Restorative Periodontal Interrelationship: Sreeraj R S, Bindu R NayarDocument8 pagesRestorative Periodontal Interrelationship: Sreeraj R S, Bindu R NayarsujeetNo ratings yet
- Gangguan Haid - PPT YudisDocument34 pagesGangguan Haid - PPT YudisIde Yudis TiyoNo ratings yet
- Psychological Report Writing: Adapted From UP-PGH FormatDocument22 pagesPsychological Report Writing: Adapted From UP-PGH FormatAhmad AliNo ratings yet
- Chapter 44-Activity and ExerciseDocument4 pagesChapter 44-Activity and ExerciseollietonkNo ratings yet
- Heart Attack EssayDocument2 pagesHeart Attack EssayRatih ParamitaNo ratings yet
- Manual - HALODocument42 pagesManual - HALOsanthigiNo ratings yet
- Case For Acute GastroenteritisDocument26 pagesCase For Acute GastroenteritisSheana TmplNo ratings yet
- Status EpilepticusDocument21 pagesStatus EpilepticusbushraNo ratings yet
- Types of Wounds & ManagementDocument19 pagesTypes of Wounds & ManagementHina BatoolNo ratings yet
- Mammography For Breast Cancer ScreeningDocument26 pagesMammography For Breast Cancer Screeningaufar syehan100% (1)
- Vaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDADocument1 pageVaccination Certificate SyedPeerzadaAbdulYounus YZ6Ry6FmMhbMysvAaSDAAbdul YounusNo ratings yet
- Teaching Plan PDFDocument92 pagesTeaching Plan PDFRoxanne Jane S. Graycochea100% (1)