Professional Documents
Culture Documents
Jain Extrapleural Approach
Jain Extrapleural Approach
Uploaded by
Oj AlimbuyuguenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jain Extrapleural Approach
Jain Extrapleural Approach
Uploaded by
Oj AlimbuyuguenCopyright:
Available Formats
Simultaneous anterior decompression and
posterior instrumentation of the tuberculous
spine using an anterolateral extrapleural
approach
A. K. Jain, Injury to the spinal cord and kyphosis are the two most feared complications of tuberculosis
I. K. Dhammi, of the spine. Since tuberculosis affects principally the vertebral bodies, anterior
B. Prashad, decompression is usually recommended. Concomitant posterior instrumentation is
S. Sinha, indicated to neutralise gross instability from panvertebral disease, to protect the anterior
P. Mishra bone graft, to prevent graft-related complications after anterior decompression in long-
segment disease and to correct a kyphosis. Two-stage surgery is usually performed in these
From the University cases. We present 38 consecutive patients with tuberculosis of the spine for whom anterior
College of Medical decompression, posterior instrumentation, with or without correction of the kyphus, and
Sciences, University anterior and posterior fusion was performed in a single stage through an anterolateral
of Delhi, Delhi, India extrapleural approach. Their mean age was 20.4 years (2.0 to 57.0).
The indications for surgery were panvertebral disease, neurological deficit and severe
kyphosis. The patients were operated on in the left lateral position using a ‘T’-shaped incision
sited at the apex of kyphosis or lesion. Three ribs were removed in 34 patients and two in four
and anterior decompression of the spinal cord was carried out. The posterior vertebral column
was shortened to correct the kyphus, if necessary, and was stabilised by a Hartshill rectangle
and sublaminar wires. Anterior and posterior bone grafting was performed.
The mean number of vertebral bodies affected was 3.24 (2.0 to 9.0). The mean pre-operative
kyphosis in patients operated on for correction of the kyphus was 49.08° (30° to 72°) and there
was a mean correction of 25° (6° to 42°). All except one patient with a neural deficit
recovered complete motor and sensory function. The mean intra-operative blood loss was
1175 ml (800 to 2600), and the mean duration of surgery 3.5 hours (2.7 to 5.0). Wound
healing was uneventful in 33 of 38 patients. The mean follow-up was 33 months (11 to 74).
None of the patients required intensive care.
The extrapleural anterolateral approach provides simultaneous exposure of the anterior
and posterior aspects of the spine, thereby allowing decompression of the spinal cord,
posterior stabilisation and anterior and posterior bone grafting. This approach has much
A. K. Jain, MS, MAMS,
Professor less morbidity than the two-stage approaches which have been previously described.
I. K. Dhammi, MS Ortho,
Senior Specialist
B. Prashad, MS Ortho, Senior
Resident
P. Mishra, MS Ortho,
Injury to the spinal cord and kyphosis are the kyphosis needs to be corrected as early as pos-
Assistant Professor two most feared complications of tuberculosis sible in the active stage of the disease. In a child
University College of Medical
Sciences and GTB Hospital,
of the spine. Damage to the cord may occur in correction should be undertaken if they have
Shahadara, Delhi-95, India. active as well as in healed disease.1 Pressure on ‘spine-at-risk’ signs suggestive of progressive
S. Sinha, MS Ortho, the spinal cord may occur as a result of tuber- kyphosis.4 These are subluxation or disloca-
Specialist cular abscess, granulation tissue, tubercular tion of the facet joint at the apex of the kypho-
Ram Manohas Lohia Hospital,
New Delhi-01, India. debris, caseous tissue, or stretching of the cord sis, the presence of retropulsion, the
Correspondence should be sent
over an internal gibbus, and requires surgical translation of a vertebra in the coronal plane
to Dr A. K. Jain; e-mail: decompression. Panvertebral disease may and the posterior toppling sign. In the last, if a
dranilkjain@gmail.com
cause pathological subluxation or dislocation line drawn along the anterior border of the dis-
©2008 British Editorial Society of the spine and the resultant instability can tal healthy vertebra in an upward direction
of Bone and Joint Surgery
doi:10.1302/0301-620X.90B11.
damage the cord. Anterior decompression and meets the upper half of the proximal healthy
20972 $2.00 instrumented stabilisation may be required. vertebra, the spine is considered to be unstable.
J Bone Joint Surg [Br]
Late-onset paraplegia may be seen when the If two of the four signs are present, the
2008;90-B:1477-81. tuberculous spine heals with a kyphosis of 60° kyphosis is considered to be progressive.3
Received 26 February 2008;
Accepted after revision 10 June
or more, and in children if the kyphosis pro- Instrumented stabilisation is indicated when
2008 gresses with growth.2,3 In the first instance the a patient presents with a panvertebral lesion or
VOL. 90-B, No. 11, NOVEMBER 2008 1477
1478 A. K. JAIN, I. K. DHAMMI, B. PRASHAD, S. SINHA, P. MISHRA
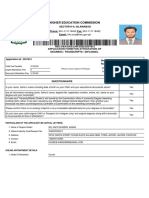
Fig. 1
Mid sagittal T2-weighted MR scan showing a) a hyperintense T6 vertebra
with prevertebral and intraspinal collection compressing the cord and b)
axial T1-weighted and c) T2-weighted scans showing panvertebral
involvement with cord compression.
if a posterior-column shortening has been performed as Fig. 2a Fig. 2b
well as anterior column resection, to correct the kypho-
Anteroposterior (a) and lateral (b) radiographs 16 months after ante-
sis.5,6 In long-segment disease with a neural deficit, anterior rior decompression and posterior stabilisation with a Hartshill rectan-
decompression is required over several levels and a long gle using an extrapleural anterolateral approach showing bony fusion
at the site of disease and a well-maintained dorsal kyphosis.
graft is needed to bridge the defect. This leaves a grossly
unstable spine which needs formal stabilisation.
Tuberculosis of the spine involves the vertebral body in
98% of cases and is usually treated by anterior decompres-
sion, fusion and posterior stabilisation.6-9 In order to a single-stage anterior decompression, posterior Hartshill
achieve this the vertebral body needs to be approached instrumentation and circumferential autogenous bone
from both front and the back. This can be undertaken in grafting through an extrapleural anterolateral approach.
one or two stages. If posterior stabilisation is undertaken There were nine males and 29 females, with a mean age
without previous anterior decompression the kyphosis can- of 20.4 years (2 to 57). Of these, 27 had a neural deficit and
not be corrected. If anterior decompression and fusion are 11 had none. Eight had panvertebral disease (Figs 1 and 2)
performed first without instrumentation, the spine is ren- of whom two had a pathological subluxation and 13 had
dered grossly unstable increasing the risk of further neuro- long-segment disease involving four or more segments
logical injury until second-stage instrumentation is while the rest had three-segment disease.
undertaken.10 To carry out both approaches in one pro- The first indication for surgery was panvertebral disease.
cedure can also cause significant morbidity.11 The ideal There were eight patients in this group of whom two had a
procedure would allow an anterior decompression and neural defect and six did not. The second was neurological
fusion, posterior instrumentation with or without deficit with loss of more than one and a half vertebrae or
posterior-column shortening and fusion to be carried out in involvement of more than three. There were 27 patients in
one stage through a single approach. this group of whom 20 required correction of their kypho-
We present a series of 38 cases of tuberculosis of the sis. In the third group were children with active or partially-
spine treated by single-stage anterior decompression and treated disease and two or more radiological signs of pro-
fusion, posterior instrumentation with or without gressive kyphosis who had undergone surgery for
posterior-column shortening and posterior fusion for spe- correction of the kyphus.
cific indications in a single stage using an extrapleural The indications for correction of the kyphus were as fol-
anterolateral approach. lows: an adult with loss of more than one and a half verte-
bral bodies, loss with an anticipated final kyphosis angle of
Patients and Methods 60° or more4 and in a child more than two radiological
Between 1998 and 2006 we treated 38 consecutive patients signs of progressive kyphosis. In all, 23 patients underwent
with tuberculosis of the spine from T1-L2. Each underwent simultaneous correction of the kyphus.
THE JOURNAL OF BONE AND JOINT SURGERY
SIMULTANEOUS ANTERIOR DECOMPRESSION AND POSTERIOR INSTRUMENTATION OF THE TUBERCULOUS SPINE 1479
Fig. 3a Fig. 3b
a) Peri-operative photograph showing the anterior rib graft (upper arrow), and posterior Hartshill rectangle (lower arrow), and
b) photograph at follow-up showing a well-healed posterior T-shaped incision.
The neural deficit was staged using Tuli’s method as posterior incision 14 cm to 15 cm long was made with the
modified by Jain and Sinha12 as follows: central incision over the spinous process at the apex of the
Stage 1. The patient is not aware of neural deficit but the kyphosis, and the transverse incision about 8 cm from the
clinician detects signs of deficit. midline and perpendicular to it at the apex of kyphosis on
Stage 2. The patient has spasticity with a motor deficit the left side. The subcutaneous tissues and deep fascia were
but is able to lift the upper limbs against gravity or is a incised in the line of incision, creating a full-thickness
walker. The anticipated motor score in tetraparesis is fasciocutaneous flap. The trapezius, latissimus dorsi and
between 60 and 100 and in paraparesis between 80 and periscapular muscles were divided along the same line. The
100. There is sensory impairment of the lateral column at skin and muscle flaps were reflected and held by stay
all the root levels below the involvement of the cord. sutures. The three ribs at the apex of the kyphosis were
Stage 3. A bedridden spastic patient. The anticipated identified and marked and their posterior 6 cm to 8 cm, up
motor score for paraplegia is between 50 and 80 and for to the angle of the ribs, were resected. The diseased verte-
quadriplegia between 0 and 30. bral bodies were sufficiently debrided or resected to decom-
Stage 4. A bedridden patient with severe sensory loss. press the spinal cord which was exposed over the whole
The anticipated motor score in paraplegia is 50 and in length of the diseased segment.
quadriplegia 0. There is impairment of both lateral and In the thoracolumbar spine the skin incision was similar
posterior columns. to that in the thoracic spine. The transverse process of the
Stage 5. As in stage 4 with bladder and bowel involve- diseased level, either L1 or L2, was identified and its tip
ment and/or flexor spasm/flaccid paraplegia/quadriplegia. defined by diathermy. Subperiosteal blunt dissection was
The upper thoracic spine (T1-6) was involved in 11 carried out in front of the transverse process. The lumbar
cases, the lower (T7-12) in 22 cases and the thoracolumbar nerve roots were identified and protected with an infant
junction (T10-L2) in five. There was no single vertebral feeding tube. A spatula was placed under the reflected psoas
lesion but two, three, four or more than four vertebral bod- muscle exposing the anterolateral surface of the vertebral
ies were affected in 15, ten, nine and four patients, respec- body which was removed to decompress the spinal cord.
tively. The mean number of vertebrae involved as judged by After this, the anterior wound was packed and the poste-
CT, was 3.24 (2 to 9). In only two patients were more than rior midline paraspinal exposure completed. In patients
six vertebral bodies involved. The mean initial vertebral with short-segment or partially-healed disease, the two
body loss was 1.2 (0.4 to 3.1). Active pulmonary tuber- adjacent healthy vertebrae on either side of the involved
culosis was identified in eight patients, six of whom had a segment were exposed. In those with long-segment disease
neural defect and two did not. at least one healthy segment on each side was exposed. The
Of the 38 patients, 23 had a haemoglobin level of 9 g/dl sublaminar spaces were prepared for the introduction of
or less. None tested positive for HIV. the wires. A Hartshill loop of suitable length was prebent to
Operative approach. The technique has been described pre- allow correction of 30° to 40° in the sagittal plane. A series
viously.13 A parenteral third-generation cephalosporin of 20-gauge sublaminar wires was then passed. Posterior-
(Ceftriaxone; 1 gm BD) was given six hours before surgery column shortening was carried out if correction of the
and was continued for three days after surgery. The patient kyphus was indicated, before tightening of the sublaminar
was placed in a right lateral decubitus position. A T-shaped wires. The sublaminar wires were tightened first on one
VOL. 90-B, No. 11, NOVEMBER 2008
1480 A. K. JAIN, I. K. DHAMMI, B. PRASHAD, S. SINHA, P. MISHRA
side of the diseased segment and then at the opposite end. A related outcome between patients treated with iliac crest or
wake-up test was performed in neurologically intact rib. Two patients stopped taking their anti-tuberculous
patients. Next, the anterior wound was approached again. drugs three months after surgery. They presented at eight
The gap created by the excision of the vertebral bodies was and 12 months, respectively, with reactivation of their dis-
grafted with autogenous bone by creating a slot in the ease and progression of kyphosis. The mean kyphosis in the
healthy proximal and distal vertebra (Fig. 3). Tricortical immediate post-operative period was 22.5° (10° to 50°)
iliac-crest graft was used in eight patients and the ribs in 30. and at final follow-up it was 24° (11° to 54°). Thus the
In children, the distal part of the Hartshill loop was cut to mean final correction achieved was 25° (6° to 42°). No
the open loop so that it did not become a posterior tether junctional kyphosis was seen. One child had a prominent
during growth. Hartshill rectangle under the skin, which necessitated
In the post-operative period each patient was nursed in removal at 18 months.
bed, with postural turning and exercises allowed on the first
post-operative day after surgery. For the first week patients Discussion
preferred to be on their right side. Standard anti-tubercular The aim of treatment in spinal tuberculosis is to eradicate
chemotherapy was continued for 12 months. No patient the disease and to arrest and correct any kyphosis.8 Decom-
required intensive care. If any patient did not show signs of pression of the spinal cord may be required. This is usually
neural recovery in four weeks myelography was performed undertaken from the front since it is the vertebral body
to assess the adequacy of the surgical decompression. Sitting which is affected.14 Stabilisation of the spine is indicated for
and walking in a brace were allowed after six to eight weeks instability resulting from a panvertebral lesion11 or in long-
in patients who were neurologically intact. Sitting and walk- segment disease after cord decompression and correction of
ing in paralysed patients were allowed depending on the the kyphus.
extent of the neurological recovery. Patients were followed The vertebral column is at its weakest immediately after
up every three months for the first year, every six months for debridement and bone grafting. The graft is able to provide
the next two years and then annually. At each visit we sufficient stability and structural support in only 41% of
assessed the extent of neurological recovery, healing of the patients with a short defect.15 However, if the graft is more
vertebral lesion and the degree of kyphosis. than 4 cm to 5 cm long, it needs to be protected to prevent
graft-related complications such as fracture, or displace-
Results ment of the graft with a consequent increase in kyphosis
The mean operating time was 3.5 hours (2.66 to 5.0) and and/or increase in the neural deficit.10,11,15 Stabilisation of
the mean blood loss was 1175 ml (800 to 2600). Each the spine is indicated if there is a panvertebral lesion, if the
patient needed a blood transfusion of at least two units. We post-debridement defect spans more than two discs (5 cm
had to remove three ribs in each of 34 patients and two in or more) or when correction of the kyphus is contemplated.
the other four. The mean number of segments stabilised was Anterior instrumentation16-22 has been described in the
7.83 (5 to 11). The mean pre-operative kyphus was 49.08° past when 51.5% cases had only one vertebra affected and
(30° to 72°). There were no peri-operative deaths. The sur- the rest had two or more vertebrae affected. The mean cor-
gical wounds healed uneventfully in 33 patients, and in five rection of the kyphus achieved was 25.35° to 12.35° by
there was wound dehiscence and healing occurred by anterior surgery. It was primarily carried out to prevent
secondary intention. The mean follow-up was 32.9 months deterioration of the kyphus during treatment and is proba-
(11 to 74). Acid-fast bacilli were observed in five patients bly only appropriate for this indication. Posterior instru-
while the polymerase chain reaction was positive for mentation in spinal tuberculosis has been reported using
Mycobacterium tuberculosis in all. Histological examina- Harrington rods,23 and with sublaminar segmental wiring
tion confirmed the diagnosis of tuberculosis in every case. to prevent graft-related complications and progression of
All except three patients showed some sign of neural kyphosis.7-9,24-26 The advantage of posterior instrumenta-
recovery after a mean of ten days (1 to 48). Of the three tion is that good fixation can be achieved in healthy poste-
who did not, one with a pathological dislocation at T9-10, rior vertebrae even when the anterior vertebral body is
miliary tuberculosis and bed sores died one month after diseased. The instrumentation only needs to extend one
surgery of disseminated tuberculosis. The second showed healthy segment above and one below.6 However, most
no evidence of neural recovery even at the final follow-up at series have used posterior instrumentation in short-segment
one year and the third patient showed no sign of neural disease in which the kyphosis has initially ranged from 30°
recovery for 48 days. A myelogram on the 48th day showed to 35° and has been corrected to 15° to 18°, post-opera-
free flow of dye confirming an adequate surgical decom- tively.5 Hence, posterior instrumentation is of value in the
pression. The next day he started to improve and after a treatment of tuberculosis of the spine.
week had recovered full neurological function. The ideal procedure is a single-stage anterior decompres-
There was radiological evidence of healing with reminer- sion followed by posterior instrumented stabilisation and
alisation of the diseased segment and incorporation of bone anterior grafting. Transpedicular decompression and
graft in 37 patients. There was no difference in the graft- instrumentation through a posterior midline approach have
THE JOURNAL OF BONE AND JOINT SURGERY
SIMULTANEOUS ANTERIOR DECOMPRESSION AND POSTERIOR INSTRUMENTATION OF THE TUBERCULOUS SPINE 1481
been described;27 but the objective was not to correct a 4. Rajasekaran S, Shanmugasundaram TK. Prediction of the angle of gibbus defor-
mity in tuberculosis of the spine. J Bone Joint Surg [Am] 1987;69-A:503-9.
kyphosis but to prevent its progression and hence surgery
5. Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop 2007;460:39-49.
was only carried out over one or two levels. Moon8 and
6. Jain AK, Maheshwari AV, Jena S. Kyphus correction in spinal tuberculosis. Clin
Moon et al9 have described two-stage surgery in which the Orthop 2007;460:117-23.
spine was stabilised by posterior instrumentation first fol- 7. Laheri VJ, Badhe NP, Dewnany GT. Single stage decompression, anterior inter-
lowed by transthoracic anterior decompression and bone body fusion and posterior instrumentation for tuberculous kyphosis of the dorso-lum-
bar spine. Spinal Cord 2001;39:429-36.
grafting two to three weeks later. In later cases they per- 8. Moon M-S. Combined posterior instrumentation and anterior interbody fusion for
formed both procedures in one stage. The surgery again active tuberculous kyphosis of the thoraco-lumbar spine. Curr Orthopaedics
1991;5:177-9.
was primarily undertaken not to correct the kyphosis but to
9. Moon MS, Woo YK, Lee KS, et al. Posterior instrumentation and anterior interbody
prevent its progression. The mean pre-operative kyphosis fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine 1995;20:1910-16.
of 37° was improved to 15° and settled at 18°. Laheri et al7 10. Altman GT, Altman DT, Frankovitch KF. Anterior and posterior fusion for children
performed a single-stage decompression, anterior interbody with tuberculosis of the spine. Clin Orthop 1996;325:225-31.
11. Mehta JS, Bhojraj SY. Tuberculosis of the thoracic spine: a classification based on
fusion and posterior instrumentation through a postero- the selection of surgical strategies. J Bone Joint Surg [Br] 2001;83-B:859-63.
lateral retroperitoneal approach in the prone position. 12. Jain AK, Sinha S. Evaluation of systems of grading of neurological deficit in tuber-
Louw28 performed a two-stage anterior and posterior pro- culosis of spine. Spinal Cord 2005;43:375-80.
cedure in 13 of 19 patients and a single-stage procedure in 13. Jain AK, Aggarwal A, Dhammi IK, Aggarwal PK, Singh S. Extrapleural antero-
lateral decompression in tuberculosis of the dorsal spine. J Bone Joint Surg [Br]
the rest. All patients needed intensive care post-operatively 2004;86-B:1027-31.
until their general condition was stable. We performed both 14. Hodgson AR, Stock FE, Fang HS, Ong GB. Anterior spinal fusion: the operative
the anterior decompression and posterior instrumentation approach and pathological findings in 412 patients with Pott’s disease of the spine. Br
J Surg 1960;48:172-8.
through a single incision which allowed us to decompress 15. Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of
the spinal cord anteriorly under direct vision. The surgical the spine treated by anterior arthrodesis. J Bone Joint Surg [Am] 1989;71-A:1314-23.
approach is that as described by Jain et al.13 16. Ozdemir HM, Us AK, Ogün T. The role of anterior spinal instrumentation and
allograft fibula for the treatment of pott disease. Spine 2003;28:474-9.
The risk of cord injury was minimised by placing the
17. Christodoulou AG, Givissis P, Karataglis D, Symeonidis PD, Pournaras J.
patient in the lateral position thereby avoiding uncon- Treatment of tuberulosis spondylitis with anterior stabilization and titanium cage. Clin
trolled correction of the kyphus which may be encountered Orthop 2006;444:60-5.
18. Korkusuz F, Islam C, Korkusuz Z. Prevention of postoperative late kyphosis in Pott’s
after anterior decompression in the prone position. Once disease by anterior decompression and intervertebral grafting. World J Surg
the spine had been stabilised posteriorly it was still possible 1997;21:524-8.
to inspect the spinal cord anteriorly for any remaining cord 19. Korkusuz Z, Binnet MS, Isiklar ZU. Pott’s disease and extrapleural anterior decompres-
sion: results of 108 consecutive cases. Arch Orthop Trauma Surg 1989;108:349-52.
compression from granulation tissue or residual seques-
20. Dai LY, Jiang LS, Wang W, Cui YM. Single-stage anterior autogenous bone graft-
trum. The tricortical graft could then be inserted in the ing and instrumentation in the surgical management of thoracolumbar spinal tuber-
anterior defect. The resected ribs were used as graft for the culosis. Spine 2005;30:2342-9.
posterior fusion.13 The mean pre-operative kyphus of 49° 21. Yilmaz C, Selek HY, Gürkan I, Erdemli B, Korkusuz Z. Anterior instrumentation
for the treatment of spinal tuberculosis. J Bone Joint Surg [Am] 1999;81-B:1261-7.
was corrected to 24° at the final follow-up. Since the 22. Jin D, Qu D, Chen J, Zhang H. One-stage anterior interbody autografting and instru-
approach to the vertebral body was extrapleural, respira- mentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur
Spine J 2004;13:114-21.
tory function was not compromised. This is of considerable
23. Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M. Modern management of spi-
importance and the approach can be used in patients with nal tuberculosis. J Neurosurgery 1995;36:87-97.
concomitant pulmonary tuberculosis and compromised 24. Güven O, Kumano K, Yalçin S, Karaham M, Tsuji S. A single stage posterior
pulmonary reserve.20 approach and rigid fixation for preventing kyphosis in the treatment of spinal tuber-
culosis. Spine 1994;19:1039-43.
No benefits in any form have been received or will be received from any com- 25. Sundararaj GD, Behera S, Ravi V, et al. Role of posterior stabilisation in the man-
mercial party related directly or indirectly to the subject of this article. agement of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg [Br]
2003;85-B:100-6.
26. Chen WJ, Chen CH, Shih CH. Surgical treatment of tuberculous spondylitis: 50
References patients followed for 2-8 years. Acta Orthop Scand 1995;66:137-42.
1. Luk KD. Tuberculosis of the spine in the new millennium. Eur Spine J 1999;8:338-45. 27. Lee TC, Lu K, Yang LC, Huang HY, Liang CL. Transpedicular instrumentation as an
2. Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early
1995;19:327-31. state bone destruction. J Neurosurg 1999;91(2 Suppl):163-9.
3. Rajasekaran S. The natural history of post-tubercular kyphosis in children: radio- 28. Louw JA. Spinal tuberculosis with neurological deficit: treatment with anterior vas-
logical signs which predict late increase in deformity. J Bone Joint Surg [Br] cularised rib grafts, posterior osteotomies and fusion. J Bone Joint Surg [Br] 1990;72-
2001;83-B:954-62. B:686-93.
VOL. 90-B, No. 11, NOVEMBER 2008
You might also like
- Community and Communication in Modern Art PDFDocument4 pagesCommunity and Communication in Modern Art PDFAlumno Xochimilco GUADALUPE CECILIA MERCADO VALADEZNo ratings yet
- Cerebral Palsy Special Tests and Corrective ProceduresDocument11 pagesCerebral Palsy Special Tests and Corrective ProceduresOj AlimbuyuguenNo ratings yet
- Spine Ant CompDocument6 pagesSpine Ant CompSadashivayya SoppimathNo ratings yet
- Unstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentDocument8 pagesUnstable Burst Fractures of The Thoraco-Lumbar Junction TreatmentRafael Jardim de MouraNo ratings yet
- Pedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineDocument21 pagesPedicle Screw Fixation in Fracture of Thoraco-Lumbar SpineNiyati SharmaNo ratings yet
- Neurofibromatosis Pada Tulang BelakangDocument8 pagesNeurofibromatosis Pada Tulang Belakangdadakan16No ratings yet
- Brachial Plexus Injury in Adult: Comparative Effectiveness of Anterior and Posterior Approach For Shoulder FunctionDocument4 pagesBrachial Plexus Injury in Adult: Comparative Effectiveness of Anterior and Posterior Approach For Shoulder FunctionMedical JournalNo ratings yet
- Bahan Jurnal Neglected Fractures of FemurDocument5 pagesBahan Jurnal Neglected Fractures of Femurgulamg21No ratings yet
- Fuchs 2005Document5 pagesFuchs 2005BudhiNo ratings yet
- 5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case ReportDocument9 pages5-Level Spondylectomy For en Bloc Resection of Thoracic Chordoma: Case Reportholt linNo ratings yet
- Core Decompression With Bone Grafting For Osteonecrosis of The Femoral HeadDocument8 pagesCore Decompression With Bone Grafting For Osteonecrosis of The Femoral Headmuhammad0umar-4No ratings yet
- Fractura de CaderaDocument5 pagesFractura de CaderaalejandraNo ratings yet
- Case Report Surgical Management of Lumbal Compression FractureDocument8 pagesCase Report Surgical Management of Lumbal Compression FractureYustinusrobbyNo ratings yet
- C2 RetropharyngealDocument11 pagesC2 RetropharyngealPeter Paul PascualNo ratings yet
- Artrosis Glenohumeral Despues de Artroscopia Bankart Repair A Long-Term Follow-Up of 13 YearsDocument6 pagesArtrosis Glenohumeral Despues de Artroscopia Bankart Repair A Long-Term Follow-Up of 13 Yearsmarcelogascon.oNo ratings yet
- Svoa Ne 02 020Document10 pagesSvoa Ne 02 020Trina ViskhawatNo ratings yet
- A Case of Eccrine Tumour Metastasis To Spine Managed With Posterior Spinal Stabilization With Recovering ParaparesisDocument3 pagesA Case of Eccrine Tumour Metastasis To Spine Managed With Posterior Spinal Stabilization With Recovering ParaparesisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Surgical Treatment of Tuberculous SpondylodiscitisDocument7 pagesSurgical Treatment of Tuberculous SpondylodiscitisindraNo ratings yet
- Elbow Study 1Document8 pagesElbow Study 1Prashant SurtiNo ratings yet
- (Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic ReviewDocument10 pages(Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic Reviewkarine cim assençoNo ratings yet
- Short Versus Long Outcome RadiologisDocument7 pagesShort Versus Long Outcome Radiologisandy ardiansyahNo ratings yet
- DL TPSFDocument5 pagesDL TPSFPramod N KNo ratings yet
- Anterior Deltopectoral ApproachDocument5 pagesAnterior Deltopectoral ApproachNetravathi EllurNo ratings yet
- Burst Fracture FinDocument11 pagesBurst Fracture Finbosnia agusNo ratings yet
- Surgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewDocument26 pagesSurgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewprototyposNo ratings yet
- Surgical Technique: Vertebral Column Resection (VCR) For Severe Pediatric and Adult Spinal DeformityDocument23 pagesSurgical Technique: Vertebral Column Resection (VCR) For Severe Pediatric and Adult Spinal DeformityPeter Paul PascualNo ratings yet
- C1-C3 Lateral Mass Screw-Rod Fixation and Fusion For C2 Pathologies and Hangman's FracturesDocument12 pagesC1-C3 Lateral Mass Screw-Rod Fixation and Fusion For C2 Pathologies and Hangman's FracturesPeko PekoNo ratings yet
- Abordaje CombinadoDocument5 pagesAbordaje CombinadoJulia LemboNo ratings yet
- Aaos 2019Document283 pagesAaos 2019alealer2708No ratings yet
- Etm 20 05 09218Document7 pagesEtm 20 05 09218José A. RodríguezNo ratings yet
- malham2015Cage沉降分级 非通用Document9 pagesmalham2015Cage沉降分级 非通用kai liuNo ratings yet
- Recovery With Posterior Decompression and Dural Suturing 2024 InternationalDocument5 pagesRecovery With Posterior Decompression and Dural Suturing 2024 InternationalRonald QuezadaNo ratings yet
- Case Report Traumatic Fracture: Dislocation of Cervicothoracic Junction - Grand Round Presentation of C7-T1 Instabilities and Different Instrumentation TechniquesDocument6 pagesCase Report Traumatic Fracture: Dislocation of Cervicothoracic Junction - Grand Round Presentation of C7-T1 Instabilities and Different Instrumentation TechniquesMohammad Al-SofyaniNo ratings yet
- Bridging Plate Osteosynthesis of Humeral Shaft Fractures: Bruno Livani, William Dias BelangeroDocument9 pagesBridging Plate Osteosynthesis of Humeral Shaft Fractures: Bruno Livani, William Dias BelangeroMiguel Angel Lamas RamirezNo ratings yet
- (10920684 - Neurosurgical Focus) Surgery For Clival Lesions - Open Resection Versus The Expanded Endoscopic Endonasal ApproachDocument8 pages(10920684 - Neurosurgical Focus) Surgery For Clival Lesions - Open Resection Versus The Expanded Endoscopic Endonasal ApproachAleksandar DimovskiNo ratings yet
- Ijos ArticleDocument5 pagesIjos ArticleReena RaiNo ratings yet
- Percutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsDocument7 pagesPercutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsAmina GoharyNo ratings yet
- Physeal Sparing Reconstruction of The Anterior Cruciate Ligament in Skeletally Immature Prepubescent Children and AdolescentsDocument10 pagesPhyseal Sparing Reconstruction of The Anterior Cruciate Ligament in Skeletally Immature Prepubescent Children and AdolescentsPrabhjeet singhNo ratings yet
- Hangmans Fracture and Its ManagementDocument1 pageHangmans Fracture and Its ManagementPeko PekoNo ratings yet
- Idiopathic Stroke After Syndromic and Neuromuscular Scoliosis Surgery: A Case Report and Literature ReviewDocument7 pagesIdiopathic Stroke After Syndromic and Neuromuscular Scoliosis Surgery: A Case Report and Literature ReviewflashjetNo ratings yet
- Journal Neurosurgery SpineDocument3 pagesJournal Neurosurgery SpineWidi Nugraha HadianNo ratings yet
- 19 Haasper Hinged FixatorDocument4 pages19 Haasper Hinged FixatorudaysravsNo ratings yet
- Raval PDFDocument5 pagesRaval PDFdebby claudiNo ratings yet
- 1413 7852 Aob 24 03 00159Document5 pages1413 7852 Aob 24 03 00159Rakesh KumarNo ratings yet
- Songcharoen 1995Document5 pagesSongcharoen 1995Le Manh ThuongNo ratings yet
- Surgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year SurvivalDocument5 pagesSurgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year Survivallucasnegromonte0001No ratings yet
- Arthroscopic Fixation of Intercondylar Eminence Fractures Using A 4-Portal TechniqueDocument11 pagesArthroscopic Fixation of Intercondylar Eminence Fractures Using A 4-Portal Techniquesyairozi_hidayatNo ratings yet
- Percutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac JointDocument7 pagesPercutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac Jointgevowo3277No ratings yet
- Correcting Genu Varum and Genu Valgum in Children by Guided GrowthDocument4 pagesCorrecting Genu Varum and Genu Valgum in Children by Guided Growthİdrak MammadovNo ratings yet
- Intramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichDocument4 pagesIntramedullary K-Wire Fixation of Metacarpal Fractures: Georg Kelsch Christoph UlrichVolcNo ratings yet
- 264 2014 Article 2282Document4 pages264 2014 Article 2282fm123165464No ratings yet
- Nasional 3 NIC:KOE Penetrating Cervial Spine Injury ENDocument6 pagesNasional 3 NIC:KOE Penetrating Cervial Spine Injury ENHeru Sutanto KNo ratings yet
- New Symptomatic Compression Fracture After Percutaneous Vertebroplasty at The Thoracolumbar JunctionDocument4 pagesNew Symptomatic Compression Fracture After Percutaneous Vertebroplasty at The Thoracolumbar JunctionRamy ElmasryNo ratings yet
- Analysis of Surgical Management of Proximal Humeral FracturesDocument5 pagesAnalysis of Surgical Management of Proximal Humeral FracturesRhizka djitmauNo ratings yet
- Anehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesDocument7 pagesAnehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesHenry Adhy SantosoNo ratings yet
- 10 Aligizakis HadjipavlouDocument9 pages10 Aligizakis HadjipavlouI Made Dhita PriantharaNo ratings yet
- 1 s2.0 S2212628719301665 MainDocument4 pages1 s2.0 S2212628719301665 MainRafael Jardim de MouraNo ratings yet
- Damage Control Surgery For Spine TraumaDocument10 pagesDamage Control Surgery For Spine TraumaSacha SalasNo ratings yet
- 2005 Jpo Distraction For Bayne Type 4Document5 pages2005 Jpo Distraction For Bayne Type 4MeetJainNo ratings yet
- Surgery of the Cranio-Vertebral JunctionFrom EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitoreNo ratings yet
- Spinal Tumor Surgery: A Case-Based ApproachFrom EverandSpinal Tumor Surgery: A Case-Based ApproachDaniel M. SciubbaNo ratings yet
- 2023 SUNAN MEDICAL Catalog - CompressedDocument17 pages2023 SUNAN MEDICAL Catalog - CompressedOj AlimbuyuguenNo ratings yet
- SLICS Classification DetailedDocument7 pagesSLICS Classification DetailedOj AlimbuyuguenNo ratings yet
- Luk 2011Document3 pagesLuk 2011Oj AlimbuyuguenNo ratings yet
- BacteriologyDocument20 pagesBacteriologyOj Alimbuyuguen100% (2)
- Assignment - Research Methods For ManagementDocument19 pagesAssignment - Research Methods For Managementnatashashaikh93No ratings yet
- It8078 Web Design and ManagementDocument27 pagesIt8078 Web Design and ManagementsanjayNo ratings yet
- Miciano Vs BrimoDocument2 pagesMiciano Vs BrimoElla Marie Sanico-AbustanNo ratings yet
- DAS AppFormDocument3 pagesDAS AppFormZia HashmiNo ratings yet
- Sample Diary Curriculum Map SUBJECT: Mathematics QUARTER: Second Grade Level: 10 TOPIC: CircleDocument3 pagesSample Diary Curriculum Map SUBJECT: Mathematics QUARTER: Second Grade Level: 10 TOPIC: CircleRichimon LicerioNo ratings yet
- The Last Leaf-TestDocument1 pageThe Last Leaf-TestAleqsandra MartiashviliNo ratings yet
- Route 201/202/302 Combined: Doncaster/Box HillDocument6 pagesRoute 201/202/302 Combined: Doncaster/Box Hillmushroom620No ratings yet
- HealthcareStudentWorkbook XIIDocument130 pagesHealthcareStudentWorkbook XIIRobin McLarenNo ratings yet
- Tekken Corporation: Company GuideDocument9 pagesTekken Corporation: Company Guidehout rothanaNo ratings yet
- Startup Law OverviewDocument11 pagesStartup Law OverviewAgibise AkanliseNo ratings yet
- Subcontract Agreement (Jenesis) V.1.1Document4 pagesSubcontract Agreement (Jenesis) V.1.1sigit l.prabowoNo ratings yet
- Ajax Asynchronous Javascript + XML: "A Fundamental Shift in What'S Possible On The Web"Document60 pagesAjax Asynchronous Javascript + XML: "A Fundamental Shift in What'S Possible On The Web"lucasNo ratings yet
- Microsoft Power Point - Organsiational Culture MSC Revised 1010Document6 pagesMicrosoft Power Point - Organsiational Culture MSC Revised 1010mattstewartis9589No ratings yet
- Hasil SKD Publish (Ok) 3Document60 pagesHasil SKD Publish (Ok) 3SolahudinNo ratings yet
- Review of Related Literature On Environmental SanitationDocument8 pagesReview of Related Literature On Environmental SanitationkmffzlvkgNo ratings yet
- SurvivalPhrases Arabic S1L03Document2 pagesSurvivalPhrases Arabic S1L03JohannCoxNo ratings yet
- Surgical Technique: Available in Titanium and Stainless SteelDocument53 pagesSurgical Technique: Available in Titanium and Stainless SteelJorge Trinidad de la CruzNo ratings yet
- Angela's Infantwear and Accessories: InvoiceDocument1 pageAngela's Infantwear and Accessories: InvoiceAngelas InfantwearNo ratings yet
- Parliament Denies Amidu's AllegationsDocument3 pagesParliament Denies Amidu's Allegationsmyjoyonline.comNo ratings yet
- 7 VideoDocument17 pages7 VideoKARTIKNo ratings yet
- Alvaro - Now Creatives Freelancer AgreementDocument10 pagesAlvaro - Now Creatives Freelancer AgreementEdward Rey EbaoNo ratings yet
- Diagnosis of Stroke-Associated PneumoniaDocument16 pagesDiagnosis of Stroke-Associated PneumoniaCecilia Casandra UneputtyNo ratings yet
- Law - Lesson 9-10Document8 pagesLaw - Lesson 9-10Stephanie AndalNo ratings yet
- Royal College Grade 11 Tamil Literature Second Term Paper 2022Document9 pagesRoyal College Grade 11 Tamil Literature Second Term Paper 2022naveen naveenan50% (2)
- Final ExamDocument3 pagesFinal ExamFaidah PangandamanNo ratings yet
- Vampires Werewolves and Witches Oh MyDocument51 pagesVampires Werewolves and Witches Oh Myangelg29850% (1)
- Nep Schools - VZM Dist - 26072021Document27 pagesNep Schools - VZM Dist - 26072021WHO IS ITNo ratings yet
- Mini TestDocument2 pagesMini TestDinh LongNo ratings yet
- RubricsDocument2 pagesRubricsJohannes B. MirafuentesNo ratings yet