Professional Documents
Culture Documents
Cecilia, Issaiah Nicolle-Pneumothorax-Ncp
Cecilia, Issaiah Nicolle-Pneumothorax-Ncp
Uploaded by
Issaiah Nicolle Cecilia100%(1)100% found this document useful (1 vote)
266 views7 pagesThe patient has a tension pneumothorax from a gunshot wound to the chest. Signs include cyanosis, subcutaneous emphysema, and tracheal deviation. The nurse must immediately remove the chest wound dressing to release pressure and contact the provider, as a tension pneumothorax is a medical emergency requiring needle decompression and chest tube placement. The nurse will monitor the chest tube drainage and assess for resolution of the pneumothorax.
Original Description:
Original Title
CECILIA, ISSAIAH NICOLLE-PNEUMOTHORAX-NCP
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe patient has a tension pneumothorax from a gunshot wound to the chest. Signs include cyanosis, subcutaneous emphysema, and tracheal deviation. The nurse must immediately remove the chest wound dressing to release pressure and contact the provider, as a tension pneumothorax is a medical emergency requiring needle decompression and chest tube placement. The nurse will monitor the chest tube drainage and assess for resolution of the pneumothorax.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
100%(1)100% found this document useful (1 vote)
266 views7 pagesCecilia, Issaiah Nicolle-Pneumothorax-Ncp
Cecilia, Issaiah Nicolle-Pneumothorax-Ncp
Uploaded by
Issaiah Nicolle CeciliaThe patient has a tension pneumothorax from a gunshot wound to the chest. Signs include cyanosis, subcutaneous emphysema, and tracheal deviation. The nurse must immediately remove the chest wound dressing to release pressure and contact the provider, as a tension pneumothorax is a medical emergency requiring needle decompression and chest tube placement. The nurse will monitor the chest tube drainage and assess for resolution of the pneumothorax.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 7
Issaiah Nicolle L.
Cecilia October 15, 2020
3 NRS A Prof. Lacambra
Let’s begin with small leap.
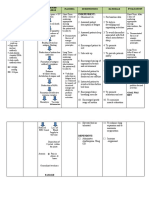
PRIORITY CONCEPT: Gas exchange and Perfusion
RLE ACTIVITY 1
CRITICAL THINKING What Should You Do?
A victim of a gunshot wound to the chest sustained a penetrating injury. The emergency medical
response team applied a nonporous dressing over the victim’s sucking chest wound at the site of
the accident. On arrival at the, the victim is cyanotic, and the nurse notes subcutaneous
emphysema (crepitus) and tracheal deviation away from the affected side. What should the nurse
do?
The patient is experiencing a tension pneumothorax caused by penetrating trauma (gunshot
wound).
Pneumothorax is an accumulation of air in the thoracic cavity between the parietal and visceral
pleurae. It can occur when there is a buildup of intrathoracic pressure in the pleural space and air
cannot escape. The loss of negative intrapleural pressure results in collapse of the lung. The
possible cause of this is the covering of an open chest wound.
Signs and symptoms of a pneumothorax include cyanosis, sudden, sharp pain with breathing
or coughing on the affected side, tachycardia, tachypnea, dyspnea, hypotension, subcutaneous
emphysema as evidenced by crepitus on palpation, neck vein distention, hyperresonance to
percussion, tachycardia, sucking sound with open chest wound, anxiety, and restlessness. The
nurse will hear no sounds of air movement on auscultation on affected side. Meanwhile, tracheal
deviation away from the affected side indicates a tension pneumothorax, which is a medical
emergency. This is a medical emergency requiring possible needle decompression followed by
chest tube insertion with a chest drainage system with continuous negative pressure.to re-expand
the lung and remove air and fluid.
POSSIBLE NURSING DIAGNOSIS
Impaired gas exchange related to decreased oxygen diffusion capacity.
Ineffective breathing pattern related to decreased lung expansion due to air or fluid
accumulation.
Ineffective peripheral tissue perfusion related to severe hypoxemia.
Acute pain related to the positive pressure in the pleural space.
Anxiety related to difficulty in breathing.
PLANNING EVALUATION
NURSING GOAL / NURSING RATIONALE
ASSESSMENT DIAGNOSIS EXPECTED INTERVENTIONS
OUTCOME
Objective Ineffective SHORT TERM Immediately release the chest Tension pneumothorax SHORT TERM
Cyanotic breathing GOAL wound dressing and contact occur due to covering of GOAL
Dyspnea pattern related After 8 hours of the health care provider. an open chest wound. After 8 hours of
Tacypnea to decreased nursing Thus, this chest wound nursing
lung expansion interventions, the dressing should be interventions, the
Subcutaneous
due to air or patient will be removed immediately. patient
emphysema
fluid able to establish established an
(Crepitus) on
accumulation an improvement Evaluate respiratory function, Respiratory distress and improvement in
palpation in respiratory rate, noting rapid or shallow changes in vital signs respiratory rate,
Neck vein depth, and pattern. respirations, dyspnea, reports occur because ofdepth, and
distention of “air hunger,” development physiological stress and pattern.
Tracheal deviation LONG TERM of cyanosis, and changes in pain or may indicate
Diminished or GOAL vital signs. development of shock LONG TERM
absent breath After a series of due to hypoxia or GOAL
sounds over the nursing hemorrhage. After a series of
affected area intervention, the nursing
patient will be Auscultate breath sounds. Breath sounds may be intervention, the
VS taken as follows: able to establish a diminished or absent in patient
T – 37.0 C normal and a lobe, lung segment, or established a
P – 105 bpm effective entire lung field normal and
RR – 32 cpm breathing pattern (unilateral). Atelectatic effective
BP – 90/50 mmhg within normal area will have no breath breathing pattern
O2 – 90% range. sounds, and partially within normal
collapsed areas range.
have decreased sounds.
Assess hemodynamics and Tension pneumothorax
vital signs. can cause a significant
decrease in cardiac
output and is a medical
emergency. Early
intervention is the key
to good outcomes.
Note chest excursion and Chest excursion is
position of trachea. unequal until lung re-
expands. Trachea
deviates from affected
side with tension
pneumothorax.
Administer oxygen as It can help to reduce the
prescribed. size of the
pneumothorax by
decreasing the alveolar
nitrogen partial
pressure. Aids in
reducing work of
breathing; promotes
relief of respiratory
distress and cyanosis
associated with
hypoxemia.
Place the client in a Fowler’s
position. Promotes maximal
inspiration; enhances
lung expansion and
ventilation in unaffected
side.
Prepare for chest tube
placement, which will remain Tension pneumothorax
in place until the lung has requires immediate
expanded fully. Provide needle depression,
appropriate post-procedure followed by chest tube
care. placement. Chest tube
placement is the
treatment of choice for
traumatic
hemopneumothoraxes.
Monitor the chest tube
drainage system, assess for A chest drainage system
air leaks in the system and needs to be a
keep it secure. continuously closed
system to maintain the
negative pressure
necessary for normal
respiratory function.
Any air leak interrupts
this closed system.
Note character and amount of
chest tube drainage, whether Useful in evaluating
tube is warm and full of resolution of
blood and whether bloody pneumothorax or
fluid. development of
level in water-seal bottle is hemorrhage requiring
rising. prompt intervention.
Educate patient on chest Rapid, shallow
expansion exercises. breathing, plus a
collapsed lung, means a
high risk for atelectasis
and pneumonia. Deep
breathing exercises like
Incentive Spirometry
and Turn, Cough, Deep
Breathe, can help
reinflate the lungs
You might also like
- Preoperative and Post Liver Transplant Nursing Care PlanDocument5 pagesPreoperative and Post Liver Transplant Nursing Care PlanOctoober67% (6)
- TAHBSO InstrumentsDocument14 pagesTAHBSO InstrumentsJoseph Joshua OtazaNo ratings yet
- OCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesOCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale Evaluationchurva_freak433533% (9)
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Punnett Square Practice Worksheet: Bobtails in Cats Are Recessive. Normal Tails Are DominantDocument2 pagesPunnett Square Practice Worksheet: Bobtails in Cats Are Recessive. Normal Tails Are DominantZaxbiyNo ratings yet
- CaseanalysisDocument2 pagesCaseanalysisChrislyn Dian Pene100% (1)
- Posi CaineDocument2 pagesPosi CaineArss Muhammad Budi PNo ratings yet
- NCP Ineffective Airway ClearanceDocument5 pagesNCP Ineffective Airway ClearanceEmm Estipona HaoNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluationria_soriano_2No ratings yet
- Maternity Nursing: Final CoachingDocument116 pagesMaternity Nursing: Final Coachingmale nurse0% (1)
- Comprehensive Nclex Exam Answer KeyDocument12 pagesComprehensive Nclex Exam Answer KeyAmy93% (15)
- Word Ncp.......... TetanusDocument3 pagesWord Ncp.......... TetanusYvounne Ananias Bautista RNNo ratings yet
- Nursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Document1 pageNursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Caroline ChaNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Chest Tube Reflective EssayDocument2 pagesChest Tube Reflective EssayAnjae GariandoNo ratings yet
- Acute Pain OsteosarcomaDocument8 pagesAcute Pain OsteosarcomaMaryjoy Gabriellee De La Cruz100% (1)
- Nursing Care Plan: Cystic FibrosisDocument4 pagesNursing Care Plan: Cystic FibrosisYael EzraNo ratings yet
- Gout N C P BY BHERU LALDocument1 pageGout N C P BY BHERU LALBheru LalNo ratings yet
- LESSON PLAN in Herbal MakingDocument5 pagesLESSON PLAN in Herbal MakingCheenee Serenuela-Monto100% (1)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocument2 pagesNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocument2 pagesNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Biopsy: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument5 pagesBiopsy: Assessment Diagnosis Planning Intervention Rationale EvaluationDan HizonNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- NCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingDocument3 pagesNCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingCedie BarcaNo ratings yet
- 2 NCPDocument2 pages2 NCPJohn CenasNo ratings yet
- Fdar UTIDocument2 pagesFdar UTINickaela CalalangNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTimothy Joseph F. RosalesNo ratings yet
- Multiple MyelomaDocument2 pagesMultiple MyelomaKolin JandocNo ratings yet
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway Clearancejae_007No ratings yet
- Answer: 59.5 KG: Rationale: Although All of These Clients Might Experience Fluid Volume Deficit, TheDocument14 pagesAnswer: 59.5 KG: Rationale: Although All of These Clients Might Experience Fluid Volume Deficit, TheMikeeNo ratings yet
- NCP - Patient With Endotracheal TubeDocument1 pageNCP - Patient With Endotracheal TubeSelwynVillamorPatenteNo ratings yet
- General Objective and Specific Objective (Goso)Document1 pageGeneral Objective and Specific Objective (Goso)BSN CMUNo ratings yet
- Assessment Explanatio Nofthe Problem Objectives Nursing Intervention Rationale EvaluationDocument3 pagesAssessment Explanatio Nofthe Problem Objectives Nursing Intervention Rationale EvaluationAziil LiizaNo ratings yet
- Ncp-For-Sle-Fatigue-And-Pain EDITEDDocument4 pagesNcp-For-Sle-Fatigue-And-Pain EDITEDJordz PlaciNo ratings yet
- Cad NCPDocument1 pageCad NCPKrizzia Mae F. MayoresNo ratings yet
- Activity Intolerance NCPDocument3 pagesActivity Intolerance NCPGen RodriguezNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway Clearanceapi-252726911No ratings yet
- Framework For Prevention in Community NursingDocument8 pagesFramework For Prevention in Community NursingjeremydbutlerNo ratings yet
- FAELDONEA, PJ - Nursing Care PlanDocument6 pagesFAELDONEA, PJ - Nursing Care PlanPatricia Jean Faeldonea100% (1)
- Moral Principles ExerciseDocument1 pageMoral Principles ExerciseGerome Isaiah RabangNo ratings yet
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDocument2 pages"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- Ineffective Breathing PatternDocument7 pagesIneffective Breathing PatternJanmae JivNo ratings yet
- Nursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Document1 pageNursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Caroline ChaNo ratings yet
- Ineffective Airway Clearance - PTBDocument2 pagesIneffective Airway Clearance - PTBIrish Eunice FelixNo ratings yet
- NCP (Acute Pain)Document2 pagesNCP (Acute Pain)jennilois100% (1)
- NCP sLEEP DEPRIVATIONDocument4 pagesNCP sLEEP DEPRIVATIONArianna MabungaNo ratings yet
- Nursing Care Plan Assessment Cues Nursing Diagnosis Background of Knowledge Nursing Objectives/Goal Nursing Interventions Rationale EvaluationDocument2 pagesNursing Care Plan Assessment Cues Nursing Diagnosis Background of Knowledge Nursing Objectives/Goal Nursing Interventions Rationale EvaluationIvy Lapore100% (1)
- Word Ncp.......... TetanusDocument6 pagesWord Ncp.......... TetanusaianrNo ratings yet
- NCP CR Impaired Spontaneous VentilationDocument8 pagesNCP CR Impaired Spontaneous VentilationJosett Romano75% (4)
- Dysfunctional Uterine Bleeding (DUB)Document1 pageDysfunctional Uterine Bleeding (DUB)Bheru LalNo ratings yet
- Prenatal Care Common Discomforts During PregnancyDocument5 pagesPrenatal Care Common Discomforts During PregnancyKarina MadriagaNo ratings yet
- Ineffective Airway Clearance-Nursing Care Plan For COPDDocument2 pagesIneffective Airway Clearance-Nursing Care Plan For COPDRnspeakcom100% (1)
- Nursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationDocument2 pagesNursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationGrace MellaineNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanSophia Loraine Dorone Jesura100% (1)
- NCPDocument4 pagesNCPJames_A_Hamoy_2514100% (1)
- Risk For Aspiration Related To Insufficient Parental Knowledge Regarding Breastfeeding TechniquesDocument2 pagesRisk For Aspiration Related To Insufficient Parental Knowledge Regarding Breastfeeding TechniquesNicolai MabituinNo ratings yet
- Ncp-Imbalance NutritionDocument2 pagesNcp-Imbalance NutritionMariko BarbaNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainDyanne B100% (1)
- FATIGUE NCP Que Fransis A.Document4 pagesFATIGUE NCP Que Fransis A.Irene Grace BalcuevaNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- Subjective: Ventilation AssistanceDocument3 pagesSubjective: Ventilation AssistanceJobelle Acena100% (2)
- A.) Signs and Symptoms/Assessment: B.) Diagnostic ProceduresDocument13 pagesA.) Signs and Symptoms/Assessment: B.) Diagnostic ProceduresJake Yvan DizonNo ratings yet
- Nursing Care Plans: Blood Pleural EffusionDocument9 pagesNursing Care Plans: Blood Pleural Effusionjamil aldasriNo ratings yet
- CECILIA, ISSAIAH NICOLLE-EvaluationDocument1 pageCECILIA, ISSAIAH NICOLLE-EvaluationIssaiah Nicolle CeciliaNo ratings yet
- NCM: 112 Care of The Client With Problem in Oxygenation Venipuncture Using Needle or CatheterDocument7 pagesNCM: 112 Care of The Client With Problem in Oxygenation Venipuncture Using Needle or CatheterIssaiah Nicolle CeciliaNo ratings yet
- Cecilia-IV ComplicationsDocument7 pagesCecilia-IV ComplicationsIssaiah Nicolle CeciliaNo ratings yet
- Issaiah Nicolle L. Cecilia 3 BSN - A: Peaks in 30 To 60 Minutes Peaks in 5 To 6 HoursDocument2 pagesIssaiah Nicolle L. Cecilia 3 BSN - A: Peaks in 30 To 60 Minutes Peaks in 5 To 6 HoursIssaiah Nicolle CeciliaNo ratings yet
- Issaiah Nicolle L. Cecilia 3 BSN - ADocument14 pagesIssaiah Nicolle L. Cecilia 3 BSN - AIssaiah Nicolle CeciliaNo ratings yet
- Issaiah Nicolle L. Cecilia 3 BSN - ADocument6 pagesIssaiah Nicolle L. Cecilia 3 BSN - AIssaiah Nicolle CeciliaNo ratings yet
- Issaiah Nicolle L. Cecilia 3 BSN - ADocument2 pagesIssaiah Nicolle L. Cecilia 3 BSN - AIssaiah Nicolle CeciliaNo ratings yet
- Issaiah Nicolle L. Cecilia 3 BSN - ADocument2 pagesIssaiah Nicolle L. Cecilia 3 BSN - AIssaiah Nicolle CeciliaNo ratings yet
- Operational FrameworkDocument2 pagesOperational FrameworkIssaiah Nicolle CeciliaNo ratings yet
- Group 3 Group 3: 3 BSN - A 3 BSN - ADocument71 pagesGroup 3 Group 3: 3 BSN - A 3 BSN - AIssaiah Nicolle CeciliaNo ratings yet
- What Is HydrocephalusDocument5 pagesWhat Is HydrocephalusGregory JoeyNo ratings yet
- 16 Daftar PustakaDocument4 pages16 Daftar PustakaClarisa AnindyaNo ratings yet
- Kindle Hamad 28 MarcDocument1,646 pagesKindle Hamad 28 MarczozNo ratings yet
- Drugs Study For Surgery WardDocument4 pagesDrugs Study For Surgery WardMariquita BuenafeNo ratings yet
- NCM 109-Cerebral PalsyDocument36 pagesNCM 109-Cerebral PalsyLeigh Ann Prosyne LozadaNo ratings yet
- Perth Sunday Times - Week 1 - 18/4/2010Document1 pagePerth Sunday Times - Week 1 - 18/4/2010John_Bishop_3317No ratings yet
- RHU Situanional ReportDocument8 pagesRHU Situanional ReportErnest AtonNo ratings yet
- Natural Coloring AgentsDocument100 pagesNatural Coloring AgentsvrimanekNo ratings yet
- Matary Vascular Surgery 2013Document92 pagesMatary Vascular Surgery 2013Raouf Ra'fat Soliman100% (4)
- Brain Rules ReferencesDocument69 pagesBrain Rules ReferencesPear PressNo ratings yet
- GES Classroom Daily Health Monitoring ToolDocument4 pagesGES Classroom Daily Health Monitoring ToolBeverlyRose Bueno Delos SantosNo ratings yet
- 2010 - Szumilas Explaining Odds RatioDocument3 pages2010 - Szumilas Explaining Odds RatioM Arif Naufal IlhamNo ratings yet
- Exam 2021Document37 pagesExam 2021Yasser ezzatNo ratings yet
- Chapter 1Document52 pagesChapter 1marialourdes2489100% (15)
- Pharmaceutical Care Untuk Penyakit Infeksi Saluran PernapasanDocument7 pagesPharmaceutical Care Untuk Penyakit Infeksi Saluran PernapasanSynyster GatesNo ratings yet
- MCN 1Document9 pagesMCN 1Margarita RemolloNo ratings yet
- HTN and Arrh AfzalDocument8 pagesHTN and Arrh AfzalAFA.BLSNo ratings yet
- I Notes Ophthalmology PDFDocument690 pagesI Notes Ophthalmology PDFpriya arrachman0% (1)
- Preventive Dentistry 1Document19 pagesPreventive Dentistry 1blue nNo ratings yet
- AmputationsDocument66 pagesAmputationsM Lateef GanaieNo ratings yet
- Ope-101-Human Anatomy-ModuleDocument37 pagesOpe-101-Human Anatomy-ModuleAlbert MartinezNo ratings yet
- Inhaler Technique Metered Dose Inhalers With Volumatic SpacerDocument4 pagesInhaler Technique Metered Dose Inhalers With Volumatic Spacerdiana iurașcuNo ratings yet
- In-Silico Analysis and Docking of Human Serum Protein With Quercetin in T2DMDocument4 pagesIn-Silico Analysis and Docking of Human Serum Protein With Quercetin in T2DMAnonymous kw8Yrp0R5rNo ratings yet
- "Five-Plus-Five" Rights of Medication Administration: Right PatientDocument9 pages"Five-Plus-Five" Rights of Medication Administration: Right PatientAlex BasadaNo ratings yet
- CHAP 5 Quest For HealthDocument42 pagesCHAP 5 Quest For HealthRajkishor YadavNo ratings yet
- Heme Metabolism PDFDocument19 pagesHeme Metabolism PDFAnonymous jW7BU44ACNo ratings yet