Professional Documents
Culture Documents
100%(1)100% found this document useful (1 vote)
55 viewsSedative and Hypnotics: Morphine
Sedative and Hypnotics: Morphine
Uploaded by
FathimathThis document summarizes information on several medical topics in 3 sentences or less each:
1) It discusses the use of diazepam as a sedative and hypnotic drug, and its pharmacological effects including sedation, hypnosis, anticonvulsant and muscle relaxation properties.
2) It covers the use of L-Dopa in treating Parkinson's disease and hepatic coma by increasing dopamine levels in the brain, and potential drug interactions with carbidopa, selegiline and COMT inhibitors.
3) It provides an overview of morphine as an opioid analgesic, its central effects such as analgesia and respiratory depression, and therapeutic uses for pain, acute pulmonary edema, diarrhea
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Prescribing Controlled SubstancesDocument128 pagesPrescribing Controlled SubstancesrickyandsheenaNo ratings yet
- Mechanism of Action of AriprazoleDocument5 pagesMechanism of Action of AriprazoleSiegfried CristoforNo ratings yet
- Hydrochlorothiazide ThiazideDocument1 pageHydrochlorothiazide ThiazideE100% (1)
- Past Papers II PharmacologyDocument7 pagesPast Papers II PharmacologyNasir KhanNo ratings yet
- NURS 3203 Exam 3 Study Guide and BluePrintDocument31 pagesNURS 3203 Exam 3 Study Guide and BluePrintandreaaaaamor28No ratings yet
- 2152 Trifed 1444226440 PDFDocument1 page2152 Trifed 1444226440 PDFLouis WakumNo ratings yet
- PH Info ExamDocument44 pagesPH Info ExamANa AntonioNo ratings yet
- Algoritma Terapi JNC 8 Hypertension GuidelineDocument3 pagesAlgoritma Terapi JNC 8 Hypertension GuidelineRhenty NarusNo ratings yet
- Herb Drug Interaction Chart From MediherbDocument5 pagesHerb Drug Interaction Chart From Mediherbquinn941No ratings yet
- Barbiturates: Francisco H. Cabrera IIIDocument13 pagesBarbiturates: Francisco H. Cabrera IIIFrancisco CabreraNo ratings yet
- BarbituratesDocument5 pagesBarbituratesGlenn Mark Frejas RinionNo ratings yet
- Antidepressants: HistoryDocument8 pagesAntidepressants: HistoryTejus Murthy A GNo ratings yet
- Chapter 14 BuspironeDocument10 pagesChapter 14 Buspironeleeperlhan2000No ratings yet
- 7 - Chapter - CNS Edited CheckedDocument49 pages7 - Chapter - CNS Edited Checkedleon100% (1)
- Nej MR A 2216691Document15 pagesNej MR A 2216691lakshminivas PingaliNo ratings yet
- Anxiolytic Sedative-Hypnotic DrugsDocument31 pagesAnxiolytic Sedative-Hypnotic DrugsRoman MamunNo ratings yet
- General Anaesthesia OverviewDocument21 pagesGeneral Anaesthesia OverviewKamel HadyNo ratings yet
- Adrenoceptor - Activating Other Sympathomimetic Drugs PDFDocument43 pagesAdrenoceptor - Activating Other Sympathomimetic Drugs PDFRupal RaghuwanshiNo ratings yet
- The Medical Letter: On Drugs and TherapeuticsDocument11 pagesThe Medical Letter: On Drugs and TherapeuticsTom BiusoNo ratings yet
- Part Agents Act NG On The Central Ner Ous System: Liu JuntianDocument89 pagesPart Agents Act NG On The Central Ner Ous System: Liu Juntianapi-19916399No ratings yet
- Toxicology PDFDocument44 pagesToxicology PDFhuong LNo ratings yet
- AdrenalineDocument20 pagesAdrenalinecreatativeNo ratings yet
- URAPIDILDocument41 pagesURAPIDILFrancesco LucianiNo ratings yet
- AAD BF Chemotherapy Specific Cutaneous ReactionsDocument3 pagesAAD BF Chemotherapy Specific Cutaneous Reactionskahkashanahmed065No ratings yet
- AntidepressantsDocument42 pagesAntidepressantsemmwatson7113No ratings yet
- Sketchy OpioidsDocument1 pageSketchy OpioidsSandy MaeNo ratings yet
- Asthma SIM AnswersDocument4 pagesAsthma SIM Answersscorpioaj133No ratings yet
- Anxiolytics and Hypnotics by Sue HendersonDocument8 pagesAnxiolytics and Hypnotics by Sue HendersonJoyabrata SarkarNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharDocument97 pagesNonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharTarek NasrallahNo ratings yet
- BIODocument14 pagesBIOshreyansh shailaan100% (1)
- Analeptic DrugDocument23 pagesAnaleptic DrugKhadim MohiuddinNo ratings yet
- Clonidine For The Treatment of Paroxysmal Autonomic InstabilityDocument1 pageClonidine For The Treatment of Paroxysmal Autonomic Instabilityiri_balNo ratings yet
- Barbiturate PoisoningDocument17 pagesBarbiturate PoisoningRaymond ManjengwaNo ratings yet
- Dr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityDocument41 pagesDr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityredderdatNo ratings yet
- Midazolam FinalDocument2 pagesMidazolam FinalAhmad AbqariNo ratings yet
- Analeptic Anti Depression: (Cns Stimulant) andDocument23 pagesAnaleptic Anti Depression: (Cns Stimulant) andMohammad NorzaimNo ratings yet
- Antianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheDocument10 pagesAntianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheMIR SARTAJNo ratings yet
- Cholinergic DrugsDocument22 pagesCholinergic Drugsmug ashNo ratings yet
- Muscle Relaxants and Neuromuscular Blocking AgentsDocument45 pagesMuscle Relaxants and Neuromuscular Blocking AgentsSomesh SharmaNo ratings yet
- Adrenergic Blocking, Cholinergic, Sedatives and Hypnotic WORDDocument5 pagesAdrenergic Blocking, Cholinergic, Sedatives and Hypnotic WORDKeon RicoNo ratings yet
- A Technician's Guide To Pharmacy Abbreviations: Cibo ("With Food")Document7 pagesA Technician's Guide To Pharmacy Abbreviations: Cibo ("With Food")Joyce RevitaNo ratings yet
- NyeriDocument33 pagesNyeriAndriHernadi100% (1)
- Bad Guidelines Management of Adults With Delusional InfestationDocument18 pagesBad Guidelines Management of Adults With Delusional InfestationRBGBGB RBGNo ratings yet
- Workbook 2016 StomDocument186 pagesWorkbook 2016 StomAysenNo ratings yet
- Mayra Pagan: Pharmacology-NursingDocument50 pagesMayra Pagan: Pharmacology-NursingmayraNo ratings yet
- Efficacy of Pregabalin in Acute Postoperative Pain: A Meta-AnalysisDocument9 pagesEfficacy of Pregabalin in Acute Postoperative Pain: A Meta-Analysisyessy32lNo ratings yet
- Antimicrobial DrugsDocument11 pagesAntimicrobial DrugsAudhrey BNo ratings yet
- MCQDocument17 pagesMCQpradeephdNo ratings yet
- Antipsychotic Final PresentationDocument24 pagesAntipsychotic Final PresentationKhadija ArshadNo ratings yet
- Antidepressants DrugsDocument2 pagesAntidepressants DrugsSony Montaño CañeteNo ratings yet
- The ABC's of Dopamine Receptor Partial Agonists - Aripiprazole, Brexpiprazole and CariprazineDocument10 pagesThe ABC's of Dopamine Receptor Partial Agonists - Aripiprazole, Brexpiprazole and Cariprazineolivukovic100% (1)
- Pharmacological Classification of DrugsDocument68 pagesPharmacological Classification of Drugssanjeev khanalNo ratings yet
- Antihistamines - AMBOSS PDFDocument5 pagesAntihistamines - AMBOSS PDFOpio IsaacNo ratings yet
- Drugs Acting On The Autonomic Nervous SystemDocument21 pagesDrugs Acting On The Autonomic Nervous SystemyewollolijfikreNo ratings yet
- DRUG STUDY - AnticonvulsantsDocument1 pageDRUG STUDY - AnticonvulsantsZam PamateNo ratings yet
- Valium DSDocument2 pagesValium DSSoniaMarieBalanayNo ratings yet
- Unit 2-CNS and ANS (Part 3) Modified 2021Document30 pagesUnit 2-CNS and ANS (Part 3) Modified 2021Donia ShormanNo ratings yet
- Anti Anxiety DrugsDocument15 pagesAnti Anxiety DrugsMr. Psycho Sam100% (1)
- Anxiolytic, Sedative-Hypnotic DrugsDocument39 pagesAnxiolytic, Sedative-Hypnotic DrugsNina100% (1)
- Psychopharmacological AgentsDocument44 pagesPsychopharmacological Agentsbazet49No ratings yet
- PHARMACOLOGY of ANS (Synopsis For Students)Document16 pagesPHARMACOLOGY of ANS (Synopsis For Students)JIEHASMARTNo ratings yet
- Unit 2Document12 pagesUnit 2parmarkeval1610No ratings yet
- Pain and Palliative - Topic DiscussionDocument7 pagesPain and Palliative - Topic Discussionapi-535001113No ratings yet
- Drugs Acting On CNSDocument19 pagesDrugs Acting On CNSAditya sagarNo ratings yet
- Chapter 6 Diseases of The Cardiovascular Sysrem: CompanyDocument31 pagesChapter 6 Diseases of The Cardiovascular Sysrem: CompanyFathimathNo ratings yet
- Pathology Lab Exam (SEM 5) KEY POINT Slide Part: by Dorm 19 Room 422 (Thailand)Document12 pagesPathology Lab Exam (SEM 5) KEY POINT Slide Part: by Dorm 19 Room 422 (Thailand)FathimathNo ratings yet
- Ecgs (Again!) : Mary L. Dohrmann, MD Professor of Clinical Medicine Division of Cardiovascular MedicineDocument18 pagesEcgs (Again!) : Mary L. Dohrmann, MD Professor of Clinical Medicine Division of Cardiovascular MedicineFathimathNo ratings yet
- Fluid & Electrolyte Balance: PresentedDocument30 pagesFluid & Electrolyte Balance: PresentedFathimathNo ratings yet
- Endocrinology and Metabolic Diseases: Qian Xing, MD, PHDDocument49 pagesEndocrinology and Metabolic Diseases: Qian Xing, MD, PHDFathimathNo ratings yet
- Psychiatry Keypoints20150424155630895Document68 pagesPsychiatry Keypoints20150424155630895FathimathNo ratings yet
- Guidance in Studying: Nan Feng (Associate-Professor) Second Affiliated Hospital of DMUDocument25 pagesGuidance in Studying: Nan Feng (Associate-Professor) Second Affiliated Hospital of DMUFathimathNo ratings yet
- Systemic Lupus Erythematosus (SLE)Document31 pagesSystemic Lupus Erythematosus (SLE)FathimathNo ratings yet
- Vomiting of Gastrointestinal OriginDocument4 pagesVomiting of Gastrointestinal OriginFathimathNo ratings yet
- Chapter 6 Diagnostic EnzymologyDocument81 pagesChapter 6 Diagnostic EnzymologyFathimathNo ratings yet
- Clinical Examination - Eric Sarpong-NtiamoahDocument52 pagesClinical Examination - Eric Sarpong-NtiamoahFathimathNo ratings yet
- Chapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraDocument20 pagesChapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraFathimathNo ratings yet
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocument131 pagesApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathNo ratings yet
- Ovarian Tumor: Obstetrics & GynecologyDocument37 pagesOvarian Tumor: Obstetrics & GynecologyFathimathNo ratings yet
- Chapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraDocument20 pagesChapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraFathimathNo ratings yet
- Laboratorial Diagnostics Keypoints RevisionDocument6 pagesLaboratorial Diagnostics Keypoints RevisionFathimathNo ratings yet
- MigraineDocument30 pagesMigraineFathimathNo ratings yet
- Fetal DistressDocument22 pagesFetal DistressFathimath0% (1)
- Notes For USMLE Rx-01312019-Part IDocument410 pagesNotes For USMLE Rx-01312019-Part IjillNo ratings yet
- DIURETICSDocument55 pagesDIURETICSRAVISH100% (1)
- Pharma TablesDocument5 pagesPharma TablesSHRIKANTNo ratings yet
- CVPR Prototype Drugs TableDocument27 pagesCVPR Prototype Drugs TablethommyvaNo ratings yet
- Hypertension Management RecommendationDocument32 pagesHypertension Management RecommendationSomnath Das GuptaNo ratings yet
- AntihypertensionDocument17 pagesAntihypertension백지원 (소네트리)No ratings yet
- 2014 JNC 8 Hypertension - 221105 - 134757Document3 pages2014 JNC 8 Hypertension - 221105 - 134757Ei lessonNo ratings yet
- Hypertension CompiledDocument106 pagesHypertension CompiledRozzie ReyesNo ratings yet
- Thiazide Diuretic - PharmacologyDocument1 pageThiazide Diuretic - PharmacologyChona FontanillaNo ratings yet
- AHA JNC 8 GuidelineDocument12 pagesAHA JNC 8 GuidelineFamidur RsNo ratings yet
- 2013 ABFM ITE Critique - HighlightsDocument81 pages2013 ABFM ITE Critique - Highlightskelvin273219No ratings yet
- Diuretic DrugsDocument2 pagesDiuretic DrugsEngku ElisaNo ratings yet
- Mishba +pharmacology + Tapan ShahDocument232 pagesMishba +pharmacology + Tapan ShahRaushan BlakeNo ratings yet
- Pharmacology Mnemonics Collection For Medical StudentsDocument21 pagesPharmacology Mnemonics Collection For Medical StudentsAamir KhanNo ratings yet
- DiureticsDocument10 pagesDiureticsAyla NacariøNo ratings yet
- Anti Hypertensive Drugs - DiureticsDocument49 pagesAnti Hypertensive Drugs - DiureticsApurba Sarker Apu100% (1)
- HypertensionDocument109 pagesHypertensionmburukalex100% (1)
- p200 Magdy McVeigh IndraratnaDocument5 pagesp200 Magdy McVeigh IndraratnaAmmarersNo ratings yet
- Tutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiDocument34 pagesTutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiGitaaNo ratings yet
- Cardiotonic DrugsDocument67 pagesCardiotonic DrugsLady Mae Ramos100% (1)
- Diuretic Drugs PHMDocument36 pagesDiuretic Drugs PHMshenae3No ratings yet
- Drug Study: SaluronDocument4 pagesDrug Study: Saluronunkown userNo ratings yet
- Pharmacology HandoutDocument84 pagesPharmacology Handoutnanashimii100% (4)
- Hypertension in ElderlyDocument13 pagesHypertension in ElderlybookwormMD100% (2)
- Drugs Acting On Renal SystemDocument98 pagesDrugs Acting On Renal SystemIsmael JaaniNo ratings yet
- Monograph of Medicinal PlantsDocument19 pagesMonograph of Medicinal PlantsKimberly Dawn RoxasNo ratings yet
Sedative and Hypnotics: Morphine
Sedative and Hypnotics: Morphine
Uploaded by
Fathimath100%(1)100% found this document useful (1 vote)
55 views7 pagesThis document summarizes information on several medical topics in 3 sentences or less each:
1) It discusses the use of diazepam as a sedative and hypnotic drug, and its pharmacological effects including sedation, hypnosis, anticonvulsant and muscle relaxation properties.
2) It covers the use of L-Dopa in treating Parkinson's disease and hepatic coma by increasing dopamine levels in the brain, and potential drug interactions with carbidopa, selegiline and COMT inhibitors.
3) It provides an overview of morphine as an opioid analgesic, its central effects such as analgesia and respiratory depression, and therapeutic uses for pain, acute pulmonary edema, diarrhea
Original Description:
Original Title
kp pharmaco
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes information on several medical topics in 3 sentences or less each:
1) It discusses the use of diazepam as a sedative and hypnotic drug, and its pharmacological effects including sedation, hypnosis, anticonvulsant and muscle relaxation properties.
2) It covers the use of L-Dopa in treating Parkinson's disease and hepatic coma by increasing dopamine levels in the brain, and potential drug interactions with carbidopa, selegiline and COMT inhibitors.
3) It provides an overview of morphine as an opioid analgesic, its central effects such as analgesia and respiratory depression, and therapeutic uses for pain, acute pulmonary edema, diarrhea
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
100%(1)100% found this document useful (1 vote)
55 views7 pagesSedative and Hypnotics: Morphine
Sedative and Hypnotics: Morphine
Uploaded by
FathimathThis document summarizes information on several medical topics in 3 sentences or less each:
1) It discusses the use of diazepam as a sedative and hypnotic drug, and its pharmacological effects including sedation, hypnosis, anticonvulsant and muscle relaxation properties.
2) It covers the use of L-Dopa in treating Parkinson's disease and hepatic coma by increasing dopamine levels in the brain, and potential drug interactions with carbidopa, selegiline and COMT inhibitors.
3) It provides an overview of morphine as an opioid analgesic, its central effects such as analgesia and respiratory depression, and therapeutic uses for pain, acute pulmonary edema, diarrhea
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 7
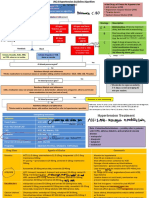
18. sedative and hypnotics 2.L-dopa can also be used in the treatment of hepatic coma.
Diazepam Drug interaction between L-dopa and (choice) :
1.carbidopa ↑therapeutic effect of L-dopa
-Pharmacological effects
Bcuz inhibit the action of decarboxylase in PNS so L-dopa
1. sedation, relief of anxiety
entering CNS will be ↑
2. hypnosis : induce sleep rapidly 2.selegiline↑therapeutic effect of L-dopa
Diazepam can prolong the time of sleep, reduce the awake Bcuz inhibit of MAO-B, so dopamine in CNS will↑, halflife of
frequency and increase the awake threshold. Has insignificant DA will ↑
influence on REM. 3.COMT ↑therapeutic effect of L-dopa
3. anticonvulsant effects So COMT inhibitor es. Nite capone
4.Pyridoxamine (vit B6)↓therapeutic effect of L-dopa bcuz
4. antiepileptic action
of ↑the activity of dopa dehydroxylase in PNS so ↓DA in CNS,
Effective in treating grand mal seizure. Diazepam is the first
↓pass through BBB
choice used in treating status epileptics via iv. (can’t be used incombination with L-dopa)
5. muscle relaxation
-Therapeutic uses 22. Opioid analgesics
1.it is effective in treating various kinds of anxiety. Morphine
2.used before anesthesia to enforce the action of anesthetic -Pharmocological effects
drugs and to relieve the anxiety of patients. Mainly acts on opioid-receptors(µ) and is a strong agonist.
3.it is most widely used hypnotic drugs clinically, effective in (A.)central effects
treating insomnia. 1.analgesia, sedation
4.it is appropriate in treating spasticity in tetanus, rabies, 2.respiratory depression
3.antitussive action
infantile fever of high fever, puerperal convulsion.
4.miosis
5.effective in treating grand mal seizure. Diazepam is the
5.emetic action
first choice used in treating status epileptics via iv. (B.)Effects on cardiovascular system
6.diazepam is used to treat central myotonia 1.morphine causes orthostatic hypotension in some patients
their superiorities comparing with barbiturates; 2.pressure of cerebrospinal fluid↑
1.higher in therapeutic index, it is (diazepam) = 8, slighter in (C.)effects on smooth muscle
-gastrointestinal tract: causes constipation
respiratory inhibition, no anesthetic action used in larger
-biliary tract:constricts biliary smooth muscle, this may result
dose. in biliary colic
2.more insignificance in inducing drug metabolizing enzyme -therapeutic uses.
3.less unwanted action (tolerance, dependence, rebounce of (a).Pain
REM, dizziness, dysfunction of movement) The cause of morphine used to treat myocardial infarction.
1.analgesia
2.sedation, antianxietyO2 comsumption↓
19. drugs effective in Epilepsias 3.dilates blood vesselsworkload of heart↓
choose drug for different type of seizure (matching) (B.)acute pulmonary edema(Cardiac asthma)
Phenytonin sodium dilation 1st grandma seizure (C.)Diarrhea
(D.)Anesthesia
Ethosuximide 1st of absence seizure
Untoward effects(side effects)
Diazepam 1st of status epilepsia via iv
(A.)Tolerance
Clonazepam absence seizure and myoclonic seizure (B.)Dependence
Phenobarbital grand mal seizure and status epilepsia (C.) nausea, constipation and biliary colic.
Sodium valproatetreat every kind of epilepsia (D.) It is abandoned to use in women during labor and milking.
Carbamazepine partial seizure, neuralgia, diabetes Reasons:
Magnesium sulfate1st of treat puerperal convulsion ①delay labor
②depress respiration of neonates and infants
(E) It is contraindicated in patients with asthma, brain injury.
21. Antiparkinsonian drugs
L-Dopa
-Pharmacological effects
In CNS, L-dopa was converted to dopamine by decarboxylase,
and elevated the level of dopamine in the brain, therefore
restoring deficient dopamine in the striatum.
-Clinical uses
1.L-dopa can be used to correct manifestation of parkinsonism
syndrome except caused by antipsychotics
-Supplement of K+ and treatment of arrhythmias.
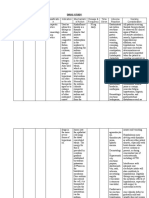
23.Analgesic-Antipyretic and Anti-inflammatory drug 26.Antihypensive drugs
comparing between NSAIDs & Opioid Analgesics classification of antihypensive
NSAIDs Opioid Analgesics 1. Diuretics
1.active site PNS CNS 2. Drugs that alter sympathetic nervous system functions
2.mechanisms -inhibit the activity -stimulate the opioid ● Sympathoplegic drugs.
of cox,↓production receptor in CNS
● Adrenergic neuron blocking agents.
of PG in PNS
● Adrenoceptor antagonists.
3.intensity and -can relieve pain of -can release all kind of
characteristic in mild to moderate pain, effective in 3. Director vasodilators
relieving the pain intensity reduce both dull and 4. Ca2+ channel blocker
-reduce dull pain of sharp pain 5. Agents that block production or action of angiotensin
various causes eg. -Angiotensin converting enzyme inhibitors (ACEI).
Muscular, dental, -The angiotensin II receptor blockers
joints, neuralgiform
and menstrual pain
-ineffective relieving 27.Antianginal drugs
sharp pain cause by Nitroglycerine
trauma and visceral
-pharmacological effect
smooth muscle colic
4.side effects -no tolerance and -tolerance and ●Effects on vascular smooth muscle
addiction can be seen addiction can develop Veins usually ( low concentrations )
after a long time use after long time use Arterioles (slightly higher dose).
-no respiratory -respiratory inhibition Large coronary artery diameters↑
inhibition Venous capacitance↑
why aspirin should be used in smaller dosage when Ventricular preload and afterload ↓
used with prophylaxis of IHD and stroke? Blood flow of ischemia area↑
-due to the mechanism: The blood supply of the endocardial layer↑
1) Low doses inhibit thromboxane synthetase→ ●Effects on hemodynamics
synthesis of thromboxane A2 ↓ -Systolic and diastolic blood pressure ↓
2)high doses →PGI2 synthesis in walls of blood vessels -Cardiac output decrease ↓
↓ → accelerate thrombosis formation ●Effects on other smooth muscle
*So in treating thrombosis, aspirin should be used with -Almost all smooth muscles↓
small dose. ●Other effects
-Platelet aggregation↓
25.Congestive heart failure -therapeutic application
Treat angina pectoris (effort angina, variant angina and
cardiac glycoside unstable angina) by relieving symptoms of angina.
-pharmacological effects -adverse reaction
(a)Positive inotropic effects -Throbbing headache
↑Cardiac contractility ↓end-systolic and end-diastolic size -Tolerance to organic nitrates could rapidly develop following
+ ↑Cardiac output and renal perfusion. prolonged administration (consumed too much thiol reason).
(b)Negative chronotropic effects
This effect is secondary to the positive inotropic action.
Combination therapy of angina pectori
↑Output↑ parasympathetic activity↓heart rate.
1.Organic nitrates and β-adrenergic receptor antagonists
This effect corrects the over excitement of sympathetic
●When used in combination, organic nitrates can offset
system in CHF patients, conducive to the relief of CHF
increased myocardial oxygen consumption related to
symptoms.
augmented ventricular end-diastolic volume induced by β-
(C) Electrophysiological effects
adrenergic receptor antagonists, and β-adrenergic receptor
-Therapeutic applications
antagonists can reduce the reflected increase of heart rate
● Various types of CHF.
induced by organic nitrates.
● Dosing regimens must be carefully performed.
2.Calcium channel blockers and β-adrenergic receptor
● Effectively decrease the refractory period of the
antagonists.
atrioventricular node and hence ventricular rate.
●β-adrenergic receptor antagonists can abate the reflex-
● Atrial flutter and fibrillation.
induced increase in heart rate induced by calcium channel
-Mechanisms of action blockers.
The increased contractility is caused by an increase in 3.Calcium channel blockers and Organic nitrates
intracellular free calcium concentration. ●Calcium channel blockers and organic nitrates have a
-Adverse reactions and toxicity treatment synergistic effect on reduction of myocardial oxygen. Calcium
●Adverse reactions channel blockers reduce afterload while organic nitrates
-Visual changes, gastrointestinal disturbances decrease preload.
- Cardiac arrhythmia.
●Toxicity treatment
B. antidiuretic effect
32.Diuretic -used in patients with diabetes insipidus. They can reduce
Furosemide urine volume and eliminate thirst.
-Mechanism and pharmacological effects C. Antihypertensive effects
(a)have a prompt and strong diuretic effect. -results from their diuretic effect
-inhibit the Na+- K+-2Cl- cotransporting carrier protein in -Therapeutic uses
ascending limb of Henle’ loop resulting in a profound increase (1) Edema associated with congestive heart failure, hepatic
of Na+, K + and Cl- in urinary excretion . cirrhosis and chronic renal failure.
-Consequently, the dilution and concentration functions of (2) Hypertension
the kidney are affected, and the kidney excretes a large (3) Diabetes insipidus.
amount of nearly isotonic urine. -Adverse Effects
(b) An increase in the excretion of Na + enhances the A. Electrolytes disturbances
exchange of K+ -Na + in distal tubule and collecting duct, -low concentration of K+, Na +, Cl- and Mg2 +.
resulting in a loss of K+. B. Metabolic changes
(c) Loop diuretics increase the renin secretion due to the -result in hyperglycemia and hyperlipidemia . Hyperuricemia
reduction of blood volume, which enhances the aldosterone so should be use incaution in patient with gout.
release and consequently loss of K+.
-therapeutic uses 35.Asthma and cough
(a) severe edema: cardiac, hepatic and renal edema.
which drug is first line?
(b) acute pulmonary edema and brain edema.
-Beclomethazone (inhale) ,cromolyn
-reduces blood volume and venous return →decrease
pulmonary vascular pressure →relieve pulmonary edema which drug treat acute asthma?
-increases the excretion of water→ concentration of blood↑ -β2 agonist given subcutaneous eg.adrenaline
→osmotic pressure of plasma↑→ ameliorate the edema of which drug use in prophylaxis?
brain -cromolyn, nedocromil,beclomethasone
(c) Acute renal failure
The main problem in the early stage of acute renal failure is
short of urine.
36.Oxytocics
-Furosemide increases the urine flow rate in acute renal clinical uses of oxytocin
failure and wash out the obstructed tubules to prevent the 1.induction of term labor
necrosis of tubules. 2.controlling postpartum hemorrhage
-Lowers the resistance of renal blood vessels and increases 3.preventing postpartum uterine atony
glomerular filtration
clinical uses of Ergonovine
(d) Treatment of hypercalcemia and promote the excretion of
1.controlling postpartum bleeding and facilitate uterine
poisons
involution
-adverse effects
A.Disturbance of water and electrolytes 2.Ergotamine can be used to treat migraine, Ergonovine
Excessive diuresis can result in low blood volume, low should not be used for induction of term labor.
concentration of K+, Cl- , Na+ ,Ca2+ and Mg2 +.
B. Ototoxicity 38. Adrenocorticosteroids
It can’t be used with aminoglycosides. why should give in the morning?
C. Hyperuricemia -According to the day-night rhythm of glucosteriods,
-The time of the highest tide of the hormone secretion, the
Thiazides suppression of adrenal cortex by exogenous dosage is
-Mechanism and pharmacological effects relatively slight.
A. Diuretic effects -The advantage may increase compliance, and lower incidence
(1) The thiazide derivatives, act mainly on the distal tubule of adverse effects (HPA suppression).
to decrease the reabsorption of Na+ by inhibition of Na+-Cl- Glucocorticoid
cotransporter on the luminal membrane, resulting in increased -physiological effect
excretion of Cl- and Na+ in the tubular fluid (10% of the 1.carbohydrate metabolism
filtered load) and produce a gentle and lasting diuretic effect. ●gluconegenesis ↑liver/muscle glycogen↑
(2) Loss of K+: Thiazides increase the Na+ in the filtrate ●glucose utilization↓blood glucose↑
arriving at the distal tubule, facilitating K+-Na+ exchange, thus 2.protein metabolism
resulting in the increase of urinary excretion of K+. Also ●protein synthesis↓,protein metabolism↑negative
thiazides inhibit carbonic anhydrase →secretion of H+↓→ k+ nitrogen balance
Na+ exchange↑ excretion of k+↑. 3.lipid metabolism
(3)Thiazides facilitate Ca2+ reabsorption in the distal tubule, ●lipolysis↑,lipid synthesis↓,redistribution of body
thus decrease the concentration of Ca2+ in the urine. fat(long-term)
-It has activity against Giardia lamblia as well as Trichomonas
4.water and electrolyte mentalism vaginalis.
-less effect on electrolytes and water balance -Metronidazole has antibacterial activity against all anaerobic
-long term use: the mineralocorticoid-like properties will bacilli.
appear 4 generations of Quinolones
-excessive glucocorticoids: lower the blood Ca2+ and the (1) First generation (nalidixic acid)
bone will be decalcified -They inhibit part of gram negative bacterium, because of narrow
5.permissive effect antibacterial spectrum, microbial resistance, poor absorption after
-many normal functions become deficient in the absence of oral administration, they are only used for urinary tract infections.
glucocorticoids. (2) Second generation (pipemidic acid)
-They have better activity against gram negative and part of gram
-pharmacological effect positive bacteria. They are effective after oral administration, low
1.anti-inflammatory properties microbial resistance and few side effects. They are used for urinary
2.immunosuppressive effects and intestinal tract infections.
3.antitoxic effects: glucocorticoids increase the endurance (3) Third generation (Fluoroquinolones)
of body tobacterial endotoxin. -They possess much higher activity against gram negative (E. coli,
4.antishock effects: large dosage is needed for treatment Salmonella, Shigella) and gram positive bacterium (staphylococci,
of all kinds of severe shock methicillin-resistant strains)
-Fluoroquinolones represents an important therapeutic advance,
5.effects on blood and hematopoietic system
since they have broad antimicrobial activity and are effective after
6.other effects of glucocorticoids oral administration for the treatment of a wide variety of infective
-GI tract: ↑gastric acid and pepsin production diseases.
-CNS: ↑excitability, eg.insomnia, irritability (4) Fourth generation (trovafloxacin, moxifloxacin)
-clinical application -They have an extensive activity against Gram-positive bacteria,
1.replacement therapy including resistant strains and anaerobic bacteria.
2.severe infection and prevention of inflammatory sequel Sulfonamide
3.autoimmune and allergic diseases
-Antimicrobial Activities
4.anti-shock therapy
Sulfonamides inhibit a wide range of microorganisms
5.hematologic disease
6.local administration including Streptococcus pyogenes, Streptococcus pneumoniae,
-adverse reactions Haemophilus influenzae, Nocardia, Chlamydia trachomatis,
1.ADR by long-term and large dosage therapy and some protozoa. Some enteric bacteria, such as E coli,
-hyperadrenalism-like syndrome(Cushings syndrome): the salmonella, and shigella are inhibited.
symptoms include moon faces, buffalo hump, central obesity, skin -mechanism reaction
atrophy, acne, adema, hypokalemia, hypertension, diabetes mellitus ●Susceptible microorganisms require extracellular para-
etc. aminobenzoic acid (PABA) in order to form dihydrofolic acid,
2.induction or aggravation of infections an essential step in the production of purines and the
-glucocorticosteriod should be comboined with effective
synthesis of nucleic acids.
antibiotics.
●The structures of sulfonamides are similar to PABA
3.Gastrointestinal reactions
-induce or aggravate the ulcers, even induce hemorrhage or ●Sulfonamides competitively inhibit dihydropteroate
perforation of the gastrointestinal tract. synthase and prevent normal bacterial utilization of PABA.
4.cardiovascular complications ●Sulfonamides are bacteriostatic. Sulfonamides do not
5.osteoporosis, amyotrophy, delayed wound healing affect mammalian cells since they require preformed folic
6.central nervous system effects acid.
42. -Clinical usage
Quinolones 1. Systemic infection
-mechanism -Sulfisoxazole (SIZ) and sulfamethoxazole (SMZ) are often
●Quinolones exert their bactericidal effect by inhibiting type II used to treat urinary tract infections.
topoisomerase (DNA gyrase, DNA) and topoisomerase IV. -SMZ given together with TMP, is used widely for respiratory
●DNA gyrase is a heterotetramer composed of two A subunits and tract infections, such as sinusitis and bronchitis, and enteric
two B subunits. The enzyme introduces negative superhelical twists infection.
into bacterial DNA and this is essential for replication and -Sulfadiazine (SD) achieves therapeutic concentrations in
transcription cerebrospinal fluid and is a first-line therapy for treatment
●Topoisomerase IV is composed of two C subunits and two E
of epidemic cerebrospinal meningitis.
subunits .
-Inhibition of topoisomerase Ⅳprobably interferes with separation
2. Local infection
of replicated chromosomal DNA into the respective daughter cells -Sodium sulfacetamide (SA-Na) is employed effectively in the
during cell division. therapy of ophthalmic infections
advantage of combine SMZ+TMP -Mafenide sulfamylon (SML) and silver sulfadiazine (SD-Ag)
1.Antibacterial spectrum are used topically to prevent bacterial colonization and
2. Antibacterial activity double blocking of folic acid synthesis; infection of burn wounds.
similar t1/2 3. Intestinal tract infection
3. Resistance -Salazosulfapyridine (SASP) is poorly absorbed so it is used
4. Adverse reaction for intestinal tract infections.
pharmacologic effect of metronidazole
-kills trophozoites but not cysts of Entamoeba histolytica.
-spectrum: G+, G- bacilli, E.coli, H.imfluenzae, Salmonella,
Proteus speciesG-
-acid: acid stable
43. β-lactam Antibiotics -β-lactamase: Penicillinase-resistance
Penicillin G Carbenicillin :
-Spectrum of activity -spectrum: same as Amipicillin, but is also used in sever G -
The penicillin-susceptible organisms include infection caused by proteus, pseudomonas, aeroginosa strains
●Gram-positive cocci, e.g., Streptococcus pyogenes -acid: acid stable
(A,B,C,G,F), non-β-lactamase producing staphylococcus -β-lactamase: not penicillinase-resistance
aureus, sensitive streptococcus pneumoniae; 4.Anti G- bacillus Penicillin (mecillinam, temocillin)
●Gram-positive bacilli, e.g., corynebacterium diphtheriae; -spectrum: some G- organism
Anthrax bacillus; tetanus bacillus -β-lactamse: β-lactamse-resistance(G - bacillus)
● gram-negative cocci. e.g., nesseria meningitides -treatment of urinary tract infection caused by G- bacillus
●spirochetes.
-Mechanism of action 44.Chloramphenicol and Tetracyclines
1) Penicillins inhibit the formation of cell wall and are Chloramphenicol
bactericidal in action. -Untoward effects
●Penicillin exerts its effect by binding to cellular receptors ●Bone marrow disturbances
(penicillin-binding protein) now identified as transpeptidase -Reversible anemia is apparently dose-related
which catalyzed the cross-linking reaction of cell wall. and occurs concomitantly with period of treatment.
●By binding to and inhibiting transpeptidation reactions, (reversible suppression of red cell production)
it interrupts the synthesis of cell wall peptidoglycan. -Aplastic anemia is idiosyncratic and usually fatal, which is
●A defective cell wall allows water to enter and swell the not related to dose and therapy.
cell, causing membrane lysis and cell death. ●Gray-baby syndrome (short)
2) increase the activity of cell-wall autolytic enzyme. 1.This condition is seen in neonates, especially premature
When the cell wall synthesis is inhibited, the bacteria infants who have been given relatively large doses of
become larger and then the autolytic enzyme is triggered to chloramphenicol;
lyse the cell. 2.Vomiting, hypothermia, gray color, respiratory
-Therapeutic uses irregularities and shock are often observed.
A wide variety of infectious diseases induced by most 3.The condition develops because of the immature hepatic
cocci, gram-positive bacilli, and spirochetes, and certain conjugating mechanism and the inadequate mechanism for
gram-negative bacilli. renal excretion in neonates.
• the first choice when the following def of Superinfection
infections are indicated. is caused by overgrowing of resistant organism and yeasts in
• Streptococcal infections, respiratory and gastrointestinal tract. Superinfection is a
infective endocarditis caused by streptococci significant problem which can result in staphylococcal
• Staphylococcal infections. enterocolitis, intestinal candidosis, and pseudomembranous
• Pneumococcal infections. colitis. These superinfections should be treated with
• Meningococcal infections, meningitis caused by vancomycin and other drugs. (intestinal flora)
meningococi.
• gonococcal infections.
• syphilis infections.
46. Aminoglycoside
• Diphtheria, anthrax. common characteristic
-Untoward effects -Spectrum of activity
●Aminoglycosides are highly active againstaerobic G– bacteria, such
Allergic reactions
as Escherichia coli, Pseudomonas aeruginosa, Klebsiella, Salmonella.
• Most severe anaphylactic shock
●Anaerobic bacteria are resistant because aminoglycosides’
Herxheimer reaction transport into cells is oxygen-dependent.
compare characteristic of 4 semisynthesized penicillin ●Aminoglycosides used in combination with β-lactams to extend
1.acid stable Penicillins (β-lac tamase unstable) coverage to G+ microbes.
Penicillin V : -Mechanism of action
-spectrun: same as penicillin G but lower activity The mechanism of Aminoglycosides is to inhibit protein synthesis by
-acid: acid stable, can be taken orally binding to 30S subunit of the ribosome in susceptible
microorganisms .
-β-lactamase:unstable
●by interfering with the initiation complex of peptide
2.Penicillinase-resistant Penicillin (oxacillin, methiallin,
formation.
cloxacillin) ●inducing misreading of the code on the mRNA template, which
-spectrum: same as Penicillin G causes incorporation of inappropriate amino acid into peptide.
-acid: acid stable, can be taken orally, i.v., i.m. ●by rupturing the polysomes into monosome, which become
-β-lactamase: Penicillinase-resistance nonfunctional.
MRSAcaused by↓affinity of Penicillin bind to PBPs -Adverse reaction
3.Broad-spectrum Penicillins Ototoxicity-should not be use with flurosemide
Ampicillin : Nephrotoxicity
Neuromuscular blockade
Allergic reactions Vinblastine (VLB) and Vincristine (VCR) are CCS agents (M
phase cells specific). The two agents are spindle poisons,
which block the formation of mitotic spindle by preventing the
assembly of tubulin dimmers into microtubules.
47. Antifungal Drugs& Antiviral drug
classification antimetabolites
A. Drugs for systemic mycotic infections Antimetabolites are similar to necessary substances such as
(a) amphotericin B, (b) flucytosine, (c) azoles including folic acid , purine and pyridine in chemical structure. These
ketoconazole, fluconazole, et al. agents compete the action site on an essential enzyme and
B. Drugs for superficial mycotic infections inhibit nucleic acid synthesis. Agents of this group mainly
(a) griseofulvin, (b) nystatin, (c) topical azoles affect S phase cells. All antimetabolites undergo intracellular
(clotrimazole, ketoconazole, et al. ). activation.
Azole mechanism
inhibit of fungal cytochrome P450 enzymes, thereby impairing 52. Immunosuppression drug
the biosynthesis of ergosterol for the cytoplasmic Cyclosporin and tacrolimus
membrane. -The action of cyclosporin and tacrolimus is to inhibit T-cell
48. AntiTB & Anti leprosy Drug activation . They preferentially Inhibits antigen-triggered
First-line agents signal transduction in T lymphocytes, blunting expression of
isoniazid, rifampin, ethambutol, streptomycin and many lymphokines, including IL-2, as well as expression of
pyrazinamide antiapoptotic proteins.
Isoniazid -Mechanisms: inhibiting calcineurin-catalyzed
-pharmacological dephosphorylation of nuclear factor of activated T-cells
Isoniazid is bacteriostatic for resting M. tuberculosis but (NFAT)
bactericidal for reproducing bacilli. -The clinical application : organ transplantation, and
-mechanism rheumatoid arthritis.
●inhibiting the synthesis of DNA in tubercle bacillus; -Adverse reactions: Nephrotoxicity toxicity, induce cancer
●inhibiting the synthesis of mycolic acids, important
constituents of the mycobacterial cell wall. 41.Antimicrobial drug general consideration
-clinical usage antibiotic : A drug used to treat infections caused by bacteria and
●the primary drug for the treatment of all types of other microorganisms. Originally, an antibiotic is a substance
tuberculosis produced by one microorganism that selectively inhibits the growth of
●be used alone for prophylaxis or the early pulmonary another.
antibacterial drug : any drug that destroys bacteria or inhibits
tuberculosis with slight symptom.
their growth
-adverse of reaction Antimicrobial spectrum :means the species of microorganisms that
●Reactions on nervous system-toxicity to CNS due to the drug can inhibit or kill.
deficiency of vitamin B6 because Isoniazid can increase the -Divided in to: Narrow spectrum, Extended spectrum,
excretion of vitamin B6. Broad spectrum
●Hepatotoxicity Chemotherapy index (CI) :To evaluate the safety of
Ethambutol chemotherapeutic drugs, the value is LD50/ED50 or LD5/ED95.
-adverse effect is optic neuritis Minimal inhibitory concentration (MIC): MIC is the lowest
concentration of antimicrobial agents that prevents visible bacterial
51. Antineoplastic growth in 18-24 hours incubation.
classification classification according to mechanism of action of antimicrobial
1.according to cell cycle divided into CCS and CCNS agents
2.according to mechanism action 1)inhibitors of cell wall synthesis :penicillin, cephalosporins
●agents affecting synthesis of nucleic acids 2) inhibitors of synthesis or damage to cytoplasmic
●agents directly affecting structure and function of DNA membrane:
●agents interrupting transcription and RNA synthesis polymyxins
●agents affecting protein synthesis 3) modification in synthesis or metabolism of nucleic acids:
●agents affecting hormone balances. Quinolones, rifampin
3.according to structure and sources 4) inhibitors of protein synthesis:tetracyclines,
(a) alkylating agents; (b) antimetabolites; (c) antibiotics; chloramphenicol, erythromycin
(d) alkaloids; (e) hormones; (g) miscellanous agents :Platinum 5) modification in energy metabolism (folic acid metabolism)
Alkylating Agents : Sulfonamides, trimethoprim trimethoprim
Mechanism of action Antimicrobial agents’ resistance
Alkylation of DNA results in DNA interactions, which damage ●Enzymic inactivation: to destroy the antimicrobial such as
the structure and function of DNA, leading to β-lactamase destroy many penicillins and cephalosporins
cell death. ●Modification (alteration) of target sites
Vinblastine and Vincristine ●Decreased accumulation: an efflux system that pumps out
Mechanism of action the drug
●Genetic mutations: such as quinolones (DNA gyrase gene
mutation)
THAI KEYPOINT
By V & HY ♪
You might also like
- Prescribing Controlled SubstancesDocument128 pagesPrescribing Controlled SubstancesrickyandsheenaNo ratings yet
- Mechanism of Action of AriprazoleDocument5 pagesMechanism of Action of AriprazoleSiegfried CristoforNo ratings yet
- Hydrochlorothiazide ThiazideDocument1 pageHydrochlorothiazide ThiazideE100% (1)
- Past Papers II PharmacologyDocument7 pagesPast Papers II PharmacologyNasir KhanNo ratings yet
- NURS 3203 Exam 3 Study Guide and BluePrintDocument31 pagesNURS 3203 Exam 3 Study Guide and BluePrintandreaaaaamor28No ratings yet
- 2152 Trifed 1444226440 PDFDocument1 page2152 Trifed 1444226440 PDFLouis WakumNo ratings yet
- PH Info ExamDocument44 pagesPH Info ExamANa AntonioNo ratings yet
- Algoritma Terapi JNC 8 Hypertension GuidelineDocument3 pagesAlgoritma Terapi JNC 8 Hypertension GuidelineRhenty NarusNo ratings yet
- Herb Drug Interaction Chart From MediherbDocument5 pagesHerb Drug Interaction Chart From Mediherbquinn941No ratings yet
- Barbiturates: Francisco H. Cabrera IIIDocument13 pagesBarbiturates: Francisco H. Cabrera IIIFrancisco CabreraNo ratings yet
- BarbituratesDocument5 pagesBarbituratesGlenn Mark Frejas RinionNo ratings yet
- Antidepressants: HistoryDocument8 pagesAntidepressants: HistoryTejus Murthy A GNo ratings yet
- Chapter 14 BuspironeDocument10 pagesChapter 14 Buspironeleeperlhan2000No ratings yet
- 7 - Chapter - CNS Edited CheckedDocument49 pages7 - Chapter - CNS Edited Checkedleon100% (1)
- Nej MR A 2216691Document15 pagesNej MR A 2216691lakshminivas PingaliNo ratings yet
- Anxiolytic Sedative-Hypnotic DrugsDocument31 pagesAnxiolytic Sedative-Hypnotic DrugsRoman MamunNo ratings yet
- General Anaesthesia OverviewDocument21 pagesGeneral Anaesthesia OverviewKamel HadyNo ratings yet
- Adrenoceptor - Activating Other Sympathomimetic Drugs PDFDocument43 pagesAdrenoceptor - Activating Other Sympathomimetic Drugs PDFRupal RaghuwanshiNo ratings yet
- The Medical Letter: On Drugs and TherapeuticsDocument11 pagesThe Medical Letter: On Drugs and TherapeuticsTom BiusoNo ratings yet
- Part Agents Act NG On The Central Ner Ous System: Liu JuntianDocument89 pagesPart Agents Act NG On The Central Ner Ous System: Liu Juntianapi-19916399No ratings yet
- Toxicology PDFDocument44 pagesToxicology PDFhuong LNo ratings yet
- AdrenalineDocument20 pagesAdrenalinecreatativeNo ratings yet
- URAPIDILDocument41 pagesURAPIDILFrancesco LucianiNo ratings yet
- AAD BF Chemotherapy Specific Cutaneous ReactionsDocument3 pagesAAD BF Chemotherapy Specific Cutaneous Reactionskahkashanahmed065No ratings yet
- AntidepressantsDocument42 pagesAntidepressantsemmwatson7113No ratings yet
- Sketchy OpioidsDocument1 pageSketchy OpioidsSandy MaeNo ratings yet
- Asthma SIM AnswersDocument4 pagesAsthma SIM Answersscorpioaj133No ratings yet
- Anxiolytics and Hypnotics by Sue HendersonDocument8 pagesAnxiolytics and Hypnotics by Sue HendersonJoyabrata SarkarNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharDocument97 pagesNonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharTarek NasrallahNo ratings yet
- BIODocument14 pagesBIOshreyansh shailaan100% (1)
- Analeptic DrugDocument23 pagesAnaleptic DrugKhadim MohiuddinNo ratings yet
- Clonidine For The Treatment of Paroxysmal Autonomic InstabilityDocument1 pageClonidine For The Treatment of Paroxysmal Autonomic Instabilityiri_balNo ratings yet
- Barbiturate PoisoningDocument17 pagesBarbiturate PoisoningRaymond ManjengwaNo ratings yet
- Dr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityDocument41 pagesDr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityredderdatNo ratings yet
- Midazolam FinalDocument2 pagesMidazolam FinalAhmad AbqariNo ratings yet
- Analeptic Anti Depression: (Cns Stimulant) andDocument23 pagesAnaleptic Anti Depression: (Cns Stimulant) andMohammad NorzaimNo ratings yet
- Antianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheDocument10 pagesAntianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheMIR SARTAJNo ratings yet
- Cholinergic DrugsDocument22 pagesCholinergic Drugsmug ashNo ratings yet
- Muscle Relaxants and Neuromuscular Blocking AgentsDocument45 pagesMuscle Relaxants and Neuromuscular Blocking AgentsSomesh SharmaNo ratings yet
- Adrenergic Blocking, Cholinergic, Sedatives and Hypnotic WORDDocument5 pagesAdrenergic Blocking, Cholinergic, Sedatives and Hypnotic WORDKeon RicoNo ratings yet
- A Technician's Guide To Pharmacy Abbreviations: Cibo ("With Food")Document7 pagesA Technician's Guide To Pharmacy Abbreviations: Cibo ("With Food")Joyce RevitaNo ratings yet
- NyeriDocument33 pagesNyeriAndriHernadi100% (1)
- Bad Guidelines Management of Adults With Delusional InfestationDocument18 pagesBad Guidelines Management of Adults With Delusional InfestationRBGBGB RBGNo ratings yet
- Workbook 2016 StomDocument186 pagesWorkbook 2016 StomAysenNo ratings yet
- Mayra Pagan: Pharmacology-NursingDocument50 pagesMayra Pagan: Pharmacology-NursingmayraNo ratings yet
- Efficacy of Pregabalin in Acute Postoperative Pain: A Meta-AnalysisDocument9 pagesEfficacy of Pregabalin in Acute Postoperative Pain: A Meta-Analysisyessy32lNo ratings yet
- Antimicrobial DrugsDocument11 pagesAntimicrobial DrugsAudhrey BNo ratings yet
- MCQDocument17 pagesMCQpradeephdNo ratings yet
- Antipsychotic Final PresentationDocument24 pagesAntipsychotic Final PresentationKhadija ArshadNo ratings yet
- Antidepressants DrugsDocument2 pagesAntidepressants DrugsSony Montaño CañeteNo ratings yet
- The ABC's of Dopamine Receptor Partial Agonists - Aripiprazole, Brexpiprazole and CariprazineDocument10 pagesThe ABC's of Dopamine Receptor Partial Agonists - Aripiprazole, Brexpiprazole and Cariprazineolivukovic100% (1)
- Pharmacological Classification of DrugsDocument68 pagesPharmacological Classification of Drugssanjeev khanalNo ratings yet
- Antihistamines - AMBOSS PDFDocument5 pagesAntihistamines - AMBOSS PDFOpio IsaacNo ratings yet
- Drugs Acting On The Autonomic Nervous SystemDocument21 pagesDrugs Acting On The Autonomic Nervous SystemyewollolijfikreNo ratings yet
- DRUG STUDY - AnticonvulsantsDocument1 pageDRUG STUDY - AnticonvulsantsZam PamateNo ratings yet
- Valium DSDocument2 pagesValium DSSoniaMarieBalanayNo ratings yet
- Unit 2-CNS and ANS (Part 3) Modified 2021Document30 pagesUnit 2-CNS and ANS (Part 3) Modified 2021Donia ShormanNo ratings yet
- Anti Anxiety DrugsDocument15 pagesAnti Anxiety DrugsMr. Psycho Sam100% (1)
- Anxiolytic, Sedative-Hypnotic DrugsDocument39 pagesAnxiolytic, Sedative-Hypnotic DrugsNina100% (1)
- Psychopharmacological AgentsDocument44 pagesPsychopharmacological Agentsbazet49No ratings yet
- PHARMACOLOGY of ANS (Synopsis For Students)Document16 pagesPHARMACOLOGY of ANS (Synopsis For Students)JIEHASMARTNo ratings yet
- Unit 2Document12 pagesUnit 2parmarkeval1610No ratings yet
- Pain and Palliative - Topic DiscussionDocument7 pagesPain and Palliative - Topic Discussionapi-535001113No ratings yet
- Drugs Acting On CNSDocument19 pagesDrugs Acting On CNSAditya sagarNo ratings yet
- Chapter 6 Diseases of The Cardiovascular Sysrem: CompanyDocument31 pagesChapter 6 Diseases of The Cardiovascular Sysrem: CompanyFathimathNo ratings yet
- Pathology Lab Exam (SEM 5) KEY POINT Slide Part: by Dorm 19 Room 422 (Thailand)Document12 pagesPathology Lab Exam (SEM 5) KEY POINT Slide Part: by Dorm 19 Room 422 (Thailand)FathimathNo ratings yet
- Ecgs (Again!) : Mary L. Dohrmann, MD Professor of Clinical Medicine Division of Cardiovascular MedicineDocument18 pagesEcgs (Again!) : Mary L. Dohrmann, MD Professor of Clinical Medicine Division of Cardiovascular MedicineFathimathNo ratings yet
- Fluid & Electrolyte Balance: PresentedDocument30 pagesFluid & Electrolyte Balance: PresentedFathimathNo ratings yet
- Endocrinology and Metabolic Diseases: Qian Xing, MD, PHDDocument49 pagesEndocrinology and Metabolic Diseases: Qian Xing, MD, PHDFathimathNo ratings yet
- Psychiatry Keypoints20150424155630895Document68 pagesPsychiatry Keypoints20150424155630895FathimathNo ratings yet
- Guidance in Studying: Nan Feng (Associate-Professor) Second Affiliated Hospital of DMUDocument25 pagesGuidance in Studying: Nan Feng (Associate-Professor) Second Affiliated Hospital of DMUFathimathNo ratings yet
- Systemic Lupus Erythematosus (SLE)Document31 pagesSystemic Lupus Erythematosus (SLE)FathimathNo ratings yet
- Vomiting of Gastrointestinal OriginDocument4 pagesVomiting of Gastrointestinal OriginFathimathNo ratings yet
- Chapter 6 Diagnostic EnzymologyDocument81 pagesChapter 6 Diagnostic EnzymologyFathimathNo ratings yet
- Clinical Examination - Eric Sarpong-NtiamoahDocument52 pagesClinical Examination - Eric Sarpong-NtiamoahFathimathNo ratings yet
- Chapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraDocument20 pagesChapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraFathimathNo ratings yet
- Apyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiDocument131 pagesApyogenous Arthritis: Department of Orthopaedics The First Affiliated Hospital Dalian Medical University Tang KaiFathimathNo ratings yet
- Ovarian Tumor: Obstetrics & GynecologyDocument37 pagesOvarian Tumor: Obstetrics & GynecologyFathimathNo ratings yet
- Chapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraDocument20 pagesChapter 15+17 Hemorrhagic Disease & Thrombocytopenic PurpuraFathimathNo ratings yet
- Laboratorial Diagnostics Keypoints RevisionDocument6 pagesLaboratorial Diagnostics Keypoints RevisionFathimathNo ratings yet
- MigraineDocument30 pagesMigraineFathimathNo ratings yet
- Fetal DistressDocument22 pagesFetal DistressFathimath0% (1)
- Notes For USMLE Rx-01312019-Part IDocument410 pagesNotes For USMLE Rx-01312019-Part IjillNo ratings yet
- DIURETICSDocument55 pagesDIURETICSRAVISH100% (1)
- Pharma TablesDocument5 pagesPharma TablesSHRIKANTNo ratings yet
- CVPR Prototype Drugs TableDocument27 pagesCVPR Prototype Drugs TablethommyvaNo ratings yet
- Hypertension Management RecommendationDocument32 pagesHypertension Management RecommendationSomnath Das GuptaNo ratings yet
- AntihypertensionDocument17 pagesAntihypertension백지원 (소네트리)No ratings yet
- 2014 JNC 8 Hypertension - 221105 - 134757Document3 pages2014 JNC 8 Hypertension - 221105 - 134757Ei lessonNo ratings yet
- Hypertension CompiledDocument106 pagesHypertension CompiledRozzie ReyesNo ratings yet
- Thiazide Diuretic - PharmacologyDocument1 pageThiazide Diuretic - PharmacologyChona FontanillaNo ratings yet
- AHA JNC 8 GuidelineDocument12 pagesAHA JNC 8 GuidelineFamidur RsNo ratings yet
- 2013 ABFM ITE Critique - HighlightsDocument81 pages2013 ABFM ITE Critique - Highlightskelvin273219No ratings yet
- Diuretic DrugsDocument2 pagesDiuretic DrugsEngku ElisaNo ratings yet
- Mishba +pharmacology + Tapan ShahDocument232 pagesMishba +pharmacology + Tapan ShahRaushan BlakeNo ratings yet
- Pharmacology Mnemonics Collection For Medical StudentsDocument21 pagesPharmacology Mnemonics Collection For Medical StudentsAamir KhanNo ratings yet
- DiureticsDocument10 pagesDiureticsAyla NacariøNo ratings yet
- Anti Hypertensive Drugs - DiureticsDocument49 pagesAnti Hypertensive Drugs - DiureticsApurba Sarker Apu100% (1)
- HypertensionDocument109 pagesHypertensionmburukalex100% (1)
- p200 Magdy McVeigh IndraratnaDocument5 pagesp200 Magdy McVeigh IndraratnaAmmarersNo ratings yet
- Tutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiDocument34 pagesTutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiGitaaNo ratings yet
- Cardiotonic DrugsDocument67 pagesCardiotonic DrugsLady Mae Ramos100% (1)
- Diuretic Drugs PHMDocument36 pagesDiuretic Drugs PHMshenae3No ratings yet
- Drug Study: SaluronDocument4 pagesDrug Study: Saluronunkown userNo ratings yet
- Pharmacology HandoutDocument84 pagesPharmacology Handoutnanashimii100% (4)
- Hypertension in ElderlyDocument13 pagesHypertension in ElderlybookwormMD100% (2)
- Drugs Acting On Renal SystemDocument98 pagesDrugs Acting On Renal SystemIsmael JaaniNo ratings yet
- Monograph of Medicinal PlantsDocument19 pagesMonograph of Medicinal PlantsKimberly Dawn RoxasNo ratings yet