Professional Documents
Culture Documents
Final Opioid (Fentanyl)
Final Opioid (Fentanyl)
Uploaded by
Gwyn RosalesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Final Opioid (Fentanyl)
Final Opioid (Fentanyl)
Uploaded by
Gwyn RosalesCopyright:
Available Formats
Nursing
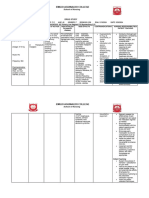
Name of Drug Classification Mechanism of Action Indication Contraindication Side Effects
Responsibilities
Generic Name: Pharmacologic Binds to opioid receptor sites in the CNS, General ● Hypersensitivity to CNS: headache, Before
Fentanyl Class: altering perception of and emotional Indications: drug or transdermal dizziness, vertigo, ● Assess for muscle
Opioid agonist response to pain by inhibiting ascending ➣ Breakthrough adhesive (with floating feeling, rigidity in
pain pathways. Fentanyl may alter pain in fentanyl transdermal) lethargy, confusion, patients receiving
Trade/Brand Name: neurotransmitter release from afferent opioidtolerant ● Opioid-nontolerant light-headedness, high doses; discuss
Actiq, Lazanda, Onsolis, Sublimaze, nerves responsive to painful stimuli, and it patients with patient nervousness, need for
Subsys causes respiratory depression by acting cancer ● Intermittent pain hallucinations, neuromuscular
directly on respiratory centers in the brain ➣ Management (on as-needed basis) delirium, insomnia, blockers with
Patients’ Dose: Therapeutic stem. of chronic pain ● Management of anxiety, prescriber. Patient
Class: in acute or mild pain fear, mood changes, receiving blocker
: Opioid Route Onset Peak Duration patients ● Management of tremor, sedation, will need ventilator.
Route: analgesic, IV 1-2 min 3-5 0.5-1 hr requiring opioid postoperative pain coma, seizures ● Monitor respiratory
IV, IM, Buccal film, Nasal spray, Sublingual anesthesia min analgesics (except for injection CV: palpitations, and cardiovascular
spray, Transdermal, Transmucosal adjunct IM 7-8 min 20- 1-2 hr ➣ Short-term form) hypotension, function and urine
30 analgesia during ● Acute or severe hypertension, output.
Form: min anesthesia and bronchial asthma tachycardia, ● With transdermal
IM or IV injection, Iontophoretic transdermal, Buccal film unknown 1 hr Unknown immediate (Duragesic), bradycardia, system, monitor
transmucosal lozenge (Actiq), Transmucosal Nasal spray unknown 15- unknown preoperative and significant respiratory arrhythmias, patient’s pain level
soluble film (Onsolis), Nasal spray (Lazanda), Controlled 21 postoperative depression, especially circulatory depression, often to determine if
Subingual Spray (Subsys), Transdermal System substance min periods in unmonitored cardiac arrest, shock patch is effective for
(Duragesic) schedule II Sublingual unknown 1.5 Unknown ➣ General settings without EENT: blurred vision, 72 hours or needs
spray hr anesthesia (with resuscitation diplopia, to be replaced after
Maximum dose: Transdermal 6 hr 12- 72 hr oxygen equipment pharyngolaryngeal 48 hours. Know
>Iontophoretic transdermal- Six 40-mcg 24 only) ● Known or suspected pain, laryngospasm that drug level rises
doses/hour and hr ➣ Adjunct to paralytic ileus GI: nausea, vomiting, gradually for first
eighty 40-mcg doses/24 hours for maxi Transmucosa rapid 15- Several regional Precautions constipation, biliary 24 hours after patch
mum of 72 hours Pregnancy l 30 hr anesthesia Use cautiously in: tract spasm, dry is applied;
>Transmucosal soluble film- Maximum: Four Category: min ● diabetes mellitus, mouth, anorexia supplemental
200-mcg film sheets or one C severe or chronic GU: urinary retention analgesics may be
1, 200-mcg film sheet four times daily Patient’s pulmonary or hepatic or hesitancy, needed
>Nasal spray- 800 mcg four times daily. Pharmacokinetics Indication: disease, ureteral or vesical then.
>Subingual Spray- 1600 Absorption: Transmucosal: Rapidly absorbed cardiovascular sphincter spasm,
mcg given twice 30 minutes apart four from buccal and nasal mucosa, the remainder is disease, CNS tumors, decreased libido,
times daily swallowed and slowly absorbed from the GI adrenal insufficiency, erectile dysfunction During
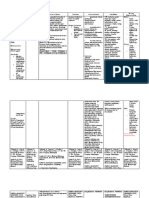
tract. Transdermal: Slow absorption after hypothyroidism, Musculoskeletal: ● If patient develops
Minimum dose: application. Bioavailability: Buccal film: 71%; renal impairment, skeletal and thoracic fever, assess for
>IM or IV injection- 0.05 to 0.1 mg I.M. or slow head injury or muscle rigidity signs and symptoms
I.V. over buccal tab: 65%; lozenge: Approx 50%; increased intracranial Respiratory: epistaxis, of opioid toxicity,
1 to 2 min. sublingual spray: 76%; sublingual tab: 54%. pressure (use cough, nasal as more drug is
>Iontophoretic transdermal- 40 mg on-demand, Time to peak plasma concentration: Buccal film: with extreme caution) discomfort, absorbed at higher
released over 10 0.75-4 hr; sublingual spray: 10-120 min; ● concurrent use of rhinorrhea, nasal body temperatures.
min sublingual tab: 15-240 min; transdermal patch: CNS depressants congestion, postnasal ● If adverse reactions
>Transmucosal lozenge- Initial: 200 mcg placed 20-72 hr. ● alcoholism or drug drip (Lazanda), to transdermal
between Distribution: Highly lipophilic, distributes abuse dyspnea, slow and system occur,
cheek and gum for 15 min followed by rapidly from blood into the lungs and skeletal ● MAO inhibitor use shallow respirations, monitor patient for at
second dose 15 min after first dose ends, if muscles then into deeper fat compartments. It within 14 days suppressed cough least 12 hours after
needed. Dosage increased according to crosses the placenta, enters the breast milk and (not recommended) reflex, apnea, patch removal.
patient’s needs. appears in the CSF. Volume of distribution: 4-6 ● elderly patients bronchospasm ● Carefully monitor
>Transmucosal soluble film- . Initial: 200-mcg L/kg. Plasma protein binding: Approx 80%. ● pregnant patients Skin: local skin hematologic studies
film sheet placed Metabolism: Hepatic via N-dealkylation and ● labor and delivery irritation (with and hepatic enzyme
against inside of cheek per episode. Increased, hydroxylation by CYP3A4 isoenzyme.. ● breastfeeding transdermal system), levels.
as needed, by 200 mcg in each subsequent Excretion: Via urine (75%, primarily as patients (not rash, urticaria,
episode, with doses at least 2 hours apart. metabolites; <7-10% as unchanged drug); faeces recommended) pruritus, diaphoresis,
>Nasal spray- Initial: 100 mcg. Increased, as (approx 9%). Elimination half-life: IV: 2-4 hr; ● children younger flushing, erythema, After
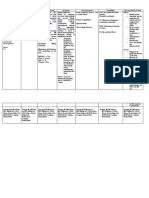
needed, to 200 mcg, then 400 mcg, then transdermal patch: 20-27 hr; transmucosal: 3-14 than age 2 (Duragesic, cold sensitivity ● Instruct patient to
800 mcg with doses spaced at least 2 hours hr (dose-dependent); nasal spray: 15-25 hr Sublimaze), younger Other: oral mucosal place lozenge
apart. than age 16 reactions (at between cheek and
>Subingual Spray- Initial: 100 mcg followed by (Actiq), or younger application site with gum and suck on it
100 than age 18 buccal tablets), for 15 minutes
mcg 30 minutes later, if needed. Increased, (Abstral, Fentora, physical or without chewing or
as needed, to 200 mcg, then 400 mcg, then Lazanda, Onsolis, psychological drug swallowing.
600 mcg, then 800 mcg, then 1200 mcg, Subsys) (safety not dependence, drug ● Teach patient
then 1600 mcg with doses spaced at least 4 established). tolerance, pain or proper technique for
hours apart. A second dose of same phlebitis applying and
strength may be taken 30 minutes after the at injection site, disposing of
first dose, as needed and counted as 1 hypersensitivity, transdermal
breakthrough episode. anaphylaxis (with oral patch.
>Transdermal System- Initial: transmucosal ● Tell patient that
One 25-mcg/hr patch, replaced every 72 hr forms) transdermal form is
(or 48 hr, if needed). Dosage increased by absorbed more
12.5 mcg/hr, as needed, after first 72 hr and rapidly if skin is
then every 6 days. For more than 100 mcg/ warm
hr, more than one patch is used. from fever or hot
environment.
Instruct patient to
Availability: avoid electric
Buccal soluble film: 200 mcg, 400 mcg, blankets, heating
600 mcg, 800 mcg, 1,200 mcg pads, heat lamps, hot
Buccal tablets: 100 mcg, 200 mcg, tubs, and heated
400 mcg, 600 mcg, 800 mcg water beds and to
Injection: 0.05 mg/ml promptly report fever
Nasal spray: 100 mcg, 400 mcg in 5-ml or a move to a
bottle hot climate.
Sublingual spray: 100 mcg, 200 mcg, ● Instruct patient not
400 mcg, 600 mcg, 800 mcg to open buccal
Tablets (buccal): 100 mcg, 200 mcg, tablet blister pack
300 mcg, 400 mcg, 600 mcg, 800 mcg until ready to use.
Tablets (sublingual): 100 mcg, 200 mcg, Teach patient to peel
300 mcg, 400 mcg, 600 mcg, 800 mcg back blister backing
Transdermal system: 12 mcg/hour, 25 to expose buccal
mcg/hour, 50 mcg/hour, 75 mcg/hour, tablet and not to
100 mcg/hour push tablet through
Transmucosal lozenges: 200 mcg, 400 blister.
mcg, 600 mcg, 800 mcg, 1,200 mcg, ● Caution patient not
1,600 mcg to break, suck,
chew, or swallow
Content: buccal tablet.
● Instruct patient to
Fentanyl is a synthetic opioid, which means it is place buccal tablet
manmade in laboratories. It does not rely on the between upper check
opium poppy for production like opiates such as and gum near
morphine. It is produced through a number of rear molar until it
chemical reactions that require specialized skills dissolves, and to
and access to restricted chemicals. swallow remnants
with a glass of water
after 30 minutes.
● Instruct patient to
use alternate sides
of mouth when taking
subsequent
doses of buccal
tablets.
● Instruct patient to
open buccal soluble
film or spray
packages
immediately
before use.
Schull, P. D. Schull, P. D. (2013). McGraw-Hill nurses drug Schull, P. D. Schull, P. D. (2013). Schull, P. D. (2013). Schull, P. D. (2013).
(2013). handbook. New York: McGraw-Hill Medical. (2013). McGraw-Hill nurses McGraw-Hill nurses McGraw-Hill nurses
McGraw-Hill McGraw-Hill drug handbook. New drug handbook. New drug handbook. New
Schull, P. D. (2013). McGraw-Hill nurses drug
nurses drug JONES & BARTLETT LEARNING. (2018). nurses drug York: McGraw-Hill York: McGraw-Hill York: McGraw-Hill
handbook. New York: McGraw-Hill Medical.
handbook. New Nurses Drug Handbook. SUDBURY. handbook. New Medical. Medical. Medical.
York: McGraw- York: McGraw-
JONES & BARTLETT LEARNING. (2018).
Hill Medical. Hill Medical. JONES & JONES & JONES &
Nurses Drug Handbook. SUDBURY.
BARTLETT BARTLETT BARTLETT
JONES & JONES & LEARNING. (2018). LEARNING. (2018). LEARNING. (2018).
What Is Fentanyl Made Of? Ingredients &
BARTLETT BARTLETT Nurses Drug Nurses Drug Nurses Drug
Cutting Agents. (n.d.). Retrieved from
LEARNING. LEARNING. Handbook. Handbook. Handbook.
https://deserthopetreatment.com/opioids/fentanyl
(2018). Nurses (2018). Nurses SUDBURY. SUDBURY. SUDBURY.
-addiction/how-its-made/
Drug Drug Handbook.
Handbook. SUDBURY.
SUDBURY.
You might also like
- My Study Plan Guide For AmcDocument7 pagesMy Study Plan Guide For Amc0d&H 8No ratings yet
- Recombinant Human Erythropoietin Stimulates Erythropoiesis Via Division and Differentiation of Progenitor Cells in Bone MarrowDocument2 pagesRecombinant Human Erythropoietin Stimulates Erythropoiesis Via Division and Differentiation of Progenitor Cells in Bone MarrowGwyn RosalesNo ratings yet
- Drug Study - NitroglycerinDocument2 pagesDrug Study - NitroglycerinKian Herrera100% (1)
- Modern Compressible FlowDocument9 pagesModern Compressible FlowSara Shoghi80% (5)
- The Secrets of Numerology Meanings Made EasyDocument8 pagesThe Secrets of Numerology Meanings Made Easydiana tolopia100% (3)
- Dosage: 50 MG Order: PRN q6h Route: IV (Case Scenario Based)Document3 pagesDosage: 50 MG Order: PRN q6h Route: IV (Case Scenario Based)Edward Luis EsguerraNo ratings yet
- PromethazineDocument3 pagesPromethazineGwyn RosalesNo ratings yet
- Brand Name: Chemical Effect: CNS: DizzinessDocument2 pagesBrand Name: Chemical Effect: CNS: DizzinessGwww BabababaNo ratings yet
- Bonilla Drug Study 2 20Document9 pagesBonilla Drug Study 2 20YLA KATRINA BONILLANo ratings yet
- Tramadol NestDocument9 pagesTramadol NestAbegail PolicarpioNo ratings yet
- Drug Study AntipsychoticDocument9 pagesDrug Study AntipsychoticAMAL ALI HASSANNo ratings yet
- DRUG STUDY Exams Ms - LavarraDocument15 pagesDRUG STUDY Exams Ms - LavarraCharm Abyss la MorenaNo ratings yet
- TRAMADOLDocument4 pagesTRAMADOLRudie Lee PascualNo ratings yet
- Narcotic Analgesics PDFDocument13 pagesNarcotic Analgesics PDFZehra AmirNo ratings yet
- PCEP-PC Module 4 Slides and Key PointsDocument5 pagesPCEP-PC Module 4 Slides and Key PointsMan MedNo ratings yet
- MeperidineDocument3 pagesMeperidineGwyn RosalesNo ratings yet
- Name of Drug Classification Mechanism of Action Indication Contraindicatio N Side Effects Nursing ResponsibilitiesDocument2 pagesName of Drug Classification Mechanism of Action Indication Contraindicatio N Side Effects Nursing ResponsibilitiesGwyn RosalesNo ratings yet
- DiazepamDocument3 pagesDiazepamGwyn RosalesNo ratings yet
- Aaaaa AaaaaaaaaaaaaaaDocument48 pagesAaaaa AaaaaaaaaaaaaaaYaneth Angeles Benavente mamaniNo ratings yet
- Drug Study: ContraindicationsDocument1 pageDrug Study: ContraindicationsMenly SusadaNo ratings yet
- DRUG STUDY - Delos SantosDocument1 pageDRUG STUDY - Delos SantosJulia Rae Delos SantosNo ratings yet
- Drug Classification Action Indication Contraindication Nursing ResposibilitiesDocument10 pagesDrug Classification Action Indication Contraindication Nursing ResposibilitiesAngelicaNo ratings yet
- Vicodin Drug Study Que Fransis A.Document3 pagesVicodin Drug Study Que Fransis A.Irene Grace BalcuevaNo ratings yet
- Drug Study: Morphine SulfateDocument8 pagesDrug Study: Morphine SulfateShara Lailanie A. Azis100% (1)
- Drug Study (Haloperidol)Document3 pagesDrug Study (Haloperidol)Mae Ann Bueno CastillonNo ratings yet
- Drug StudyDocument4 pagesDrug Studyshiela marie cortezNo ratings yet
- Case Presentation Station 3B Drug Study ClinidineDocument6 pagesCase Presentation Station 3B Drug Study ClinidinehahahahaaaaaaaNo ratings yet
- Nicolas, Krizha-Drug StudyDocument3 pagesNicolas, Krizha-Drug StudyKrizha Angela NicolasNo ratings yet
- Procedural SedationDocument9 pagesProcedural SedationZayar SweNo ratings yet
- Drug Study SPRDocument9 pagesDrug Study SPRKate WeyganNo ratings yet
- FlupentixolDocument3 pagesFlupentixolshiplusNo ratings yet
- Week 5 - Course TaskDocument7 pagesWeek 5 - Course TaskCher Allain BellosilloNo ratings yet
- LevetiracetamDocument4 pagesLevetiracetamGwyn RosalesNo ratings yet
- MeclizineDocument2 pagesMeclizineGwyn Rosales100% (1)
- Drugs For Angina Pectoris and Myocardial Infarction: OpioidDocument6 pagesDrugs For Angina Pectoris and Myocardial Infarction: OpioidApple MaeNo ratings yet
- DrugDocument10 pagesDrugMelodia Turqueza GandezaNo ratings yet
- Drug-Drug: DecreasedDocument10 pagesDrug-Drug: DecreasedMelodia Turqueza GandezaNo ratings yet
- Stroke Drug Study (GROUP)Document8 pagesStroke Drug Study (GROUP)Fran LanNo ratings yet
- Drugstudy ForcasestudyDocument22 pagesDrugstudy ForcasestudyRovic Selga TrisinioNo ratings yet
- Anes - Premedication and PositioningDocument7 pagesAnes - Premedication and PositioningChristine MendozaNo ratings yet
- Er DrugsDocument4 pagesEr Drugsanne_18No ratings yet
- Drugs Mechanism of Action Indication Contraindica Tion Side Effects Adverse Effect Nursing ResponsibilityDocument2 pagesDrugs Mechanism of Action Indication Contraindica Tion Side Effects Adverse Effect Nursing ResponsibilityNica RodriguezNo ratings yet
- Name of Drug Dosage, Route and Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilityDocument2 pagesName of Drug Dosage, Route and Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilityLizli LoredoNo ratings yet
- Activity 2 Narcotics & NMJDocument7 pagesActivity 2 Narcotics & NMJKristineNo ratings yet
- TRAMADOL HCL (Ultram)Document2 pagesTRAMADOL HCL (Ultram)karenmichellelecarozNo ratings yet
- DroperidolDocument1 pageDroperidolIvanne HisolerNo ratings yet
- PDF Drug Study Morphine SulfateDocument3 pagesPDF Drug Study Morphine SulfateCrishelNo ratings yet
- Loxapine Drug StudyDocument5 pagesLoxapine Drug Studyshadow gonzalezNo ratings yet
- Drug Classification Indication Action and Pharmacokinetics Contraindication Adverse Effect Monitoring ParameterDocument5 pagesDrug Classification Indication Action and Pharmacokinetics Contraindication Adverse Effect Monitoring ParameteryssatNo ratings yet
- Drug StudyDocument2 pagesDrug Studyunkown userNo ratings yet
- PhenobarbitalDocument1 pagePhenobarbitalSherwin LauronNo ratings yet
- Drug StudyDocument4 pagesDrug StudyGerome ManantanNo ratings yet
- Tramadol Drug-StudyDocument3 pagesTramadol Drug-StudyPang ProjectNo ratings yet
- Focused ReviewDocument11 pagesFocused ReviewJeffrey LiddellNo ratings yet
- Cholinergic Pharmacology - Drug TableDocument2 pagesCholinergic Pharmacology - Drug TableFNo ratings yet
- Ketorolac Tromethamine Toradol: Drug OrderDocument1 pageKetorolac Tromethamine Toradol: Drug OrderAbigail BascoNo ratings yet
- Drugs For The Control of Pain: OpioidDocument8 pagesDrugs For The Control of Pain: OpioidApple MaeNo ratings yet
- Drug Study: Medication Indication Contraindicati0N Side Effects Use Caution inDocument17 pagesDrug Study: Medication Indication Contraindicati0N Side Effects Use Caution inAngely Dianne Santiago II100% (2)
- 4th Rot Drug StudyDocument3 pages4th Rot Drug StudyAaron GarciaNo ratings yet
- Drug Study: Atropine: RecommendedDocument6 pagesDrug Study: Atropine: RecommendedShara Lailanie A. AzisNo ratings yet
- DRUG STUDY - AnticonvulsantsDocument1 pageDRUG STUDY - AnticonvulsantsZam PamateNo ratings yet
- Perioperative Pain ManagementFrom EverandPerioperative Pain ManagementFelicia CoxNo ratings yet
- Sulfamethaxazole, Salbu + IpraDocument5 pagesSulfamethaxazole, Salbu + IpraGwyn RosalesNo ratings yet
- PhenobarbitalDocument6 pagesPhenobarbitalGwyn RosalesNo ratings yet
- NimodipineDocument5 pagesNimodipineGwyn Rosales100% (1)
- Ipratropium SalbutamolDocument2 pagesIpratropium SalbutamolGwyn RosalesNo ratings yet
- GliclazideDocument5 pagesGliclazideGwyn RosalesNo ratings yet
- LevetiracetamDocument4 pagesLevetiracetamGwyn RosalesNo ratings yet
- EnalaprilDocument4 pagesEnalaprilGwyn RosalesNo ratings yet
- AcetazolamideDocument3 pagesAcetazolamideGwyn RosalesNo ratings yet
- ESOMEPRAZOLEDocument6 pagesESOMEPRAZOLEGwyn RosalesNo ratings yet
- ColistinDocument2 pagesColistinGwyn RosalesNo ratings yet
- Tetanus ToxoidDocument3 pagesTetanus ToxoidGwyn Rosales100% (1)
- FenofibrateDocument4 pagesFenofibrateGwyn RosalesNo ratings yet
- DiphenhydramineDocument3 pagesDiphenhydramineGwyn RosalesNo ratings yet
- (Per System Preferably) : AntihypertensiveDocument4 pages(Per System Preferably) : AntihypertensiveGwyn RosalesNo ratings yet
- DexamethasoneDocument3 pagesDexamethasoneGwyn RosalesNo ratings yet
- CeftriaDocument5 pagesCeftriaGwyn RosalesNo ratings yet
- DiazepamDocument3 pagesDiazepamGwyn RosalesNo ratings yet
- Per System PreferablyDocument3 pagesPer System PreferablyGwyn RosalesNo ratings yet
- CaptoprilDocument3 pagesCaptoprilGwyn RosalesNo ratings yet
- AmikacinDocument2 pagesAmikacinGwyn Rosales100% (2)
- CEFUROXIMEDocument3 pagesCEFUROXIMEGwyn RosalesNo ratings yet
- Cefuroxime 1Document3 pagesCefuroxime 1Gwyn RosalesNo ratings yet
- Final Magnesium SulfateDocument3 pagesFinal Magnesium SulfateGwyn RosalesNo ratings yet
- Final AcetylcysteineDocument2 pagesFinal AcetylcysteineGwyn RosalesNo ratings yet
- 6 MAGNESIUM SULFATE Drug StudyDocument2 pages6 MAGNESIUM SULFATE Drug StudyGwyn Rosales100% (2)
- Final ColistinDocument3 pagesFinal ColistinGwyn RosalesNo ratings yet
- Aerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaDocument4 pagesAerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaGwyn RosalesNo ratings yet
- AcetylcysteineDocument2 pagesAcetylcysteineGwyn Rosales100% (1)
- Final Salbu-IpraDocument3 pagesFinal Salbu-IpraGwyn RosalesNo ratings yet
- MATLAB-Simulink Based Analysis ofDocument4 pagesMATLAB-Simulink Based Analysis ofAmare KassawNo ratings yet
- Electrode Consumption PDFDocument1 pageElectrode Consumption PDFharold_bhieNo ratings yet
- Biologic Width - The No Encroachment Zone: I J D ADocument8 pagesBiologic Width - The No Encroachment Zone: I J D AJinny ShawNo ratings yet
- Exponents, Radicals and LogarithmsDocument32 pagesExponents, Radicals and LogarithmsandrikaNo ratings yet
- HGTD Data Analysis For June2018Document12 pagesHGTD Data Analysis For June2018Shahzad AliNo ratings yet
- Brgy. Songsong ConcretingDocument29 pagesBrgy. Songsong ConcretingRvin Jay Cabontocan Mariano100% (1)
- MCC Dardenelle Trail LetterDocument3 pagesMCC Dardenelle Trail LetterSabrina BrennanNo ratings yet
- The Physiology of The Lymphatic System: Melody A. SwartzDocument18 pagesThe Physiology of The Lymphatic System: Melody A. SwartzFeña Peña GonzalezNo ratings yet
- Water Level Controller Using 8051 Circuit PrincipleDocument4 pagesWater Level Controller Using 8051 Circuit PrincipleLappi SchematicsNo ratings yet
- Honorato C. Perez, Sr. Memorial Science High SchoolDocument8 pagesHonorato C. Perez, Sr. Memorial Science High SchoolJOMARI DL. GAVINONo ratings yet
- Aqua Puss Instruction Manual 701: Dunlop Manufacturing, Inc. P.O. Box 846 Benicia, Ca 94510 U.S.ADocument2 pagesAqua Puss Instruction Manual 701: Dunlop Manufacturing, Inc. P.O. Box 846 Benicia, Ca 94510 U.S.AJohn JonesNo ratings yet
- Cyscan: Positioning SystemDocument52 pagesCyscan: Positioning SystemRavichanderNo ratings yet
- A Case Study of Holiday Homes Biclatan Subdivision in General Trias, Cavite: Subdivision Planning and LandscapingDocument11 pagesA Case Study of Holiday Homes Biclatan Subdivision in General Trias, Cavite: Subdivision Planning and LandscapingKatrina ManriqueNo ratings yet
- Unit 4 Flow of Water in SoilDocument31 pagesUnit 4 Flow of Water in SoilKhalil FanousNo ratings yet
- Practical Phonetics Exercises: For BachilleratoDocument20 pagesPractical Phonetics Exercises: For BachilleratoJorge RomaNo ratings yet
- Witn (SBG) - Maimun SalehDocument4 pagesWitn (SBG) - Maimun SalehRafly AndrianzaNo ratings yet
- V2 Manual v2.66Document300 pagesV2 Manual v2.66Sazzad Hossan RaselNo ratings yet
- Jen-Dre's Catering Services Originated From The Names of The Owner'sDocument12 pagesJen-Dre's Catering Services Originated From The Names of The Owner'sBianca AsisNo ratings yet
- 3 Ways To Unlock The Power of Your Subconscious Mind PDFDocument2 pages3 Ways To Unlock The Power of Your Subconscious Mind PDFRajeswari RamakrishnanNo ratings yet
- EEE105 Chapter 7 PDFDocument44 pagesEEE105 Chapter 7 PDFAnonymous xuEZu5Ky100% (1)
- Leak Detector and Auto Cut OffDocument8 pagesLeak Detector and Auto Cut OffARUN CHRISTEL ANo ratings yet
- MaglevDocument10 pagesMaglevCaramihai DenisNo ratings yet
- PT-4 Week 2 ExercisesDocument3 pagesPT-4 Week 2 ExercisesElijah Judson AlanzalonNo ratings yet
- Arunpreet Kaur (800941004) Final ThesisDocument62 pagesArunpreet Kaur (800941004) Final ThesisrajeshwariNo ratings yet
- 01-System Devices Configuration - Rev GDocument36 pages01-System Devices Configuration - Rev GPABITRA PATRANo ratings yet
- Phar3003 - 3017 Online Timetable v4Document3 pagesPhar3003 - 3017 Online Timetable v4Ashley LeeNo ratings yet
- Seminar ReportDocument13 pagesSeminar Reportgunjan pratapNo ratings yet