Professional Documents
Culture Documents
Thrombosis and Acute Leukemia
Thrombosis and Acute Leukemia
Uploaded by
annisa edwarCopyright:
Available Formats
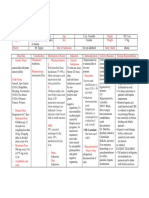
You might also like
- Board Stiff ThreeDocument440 pagesBoard Stiff Threewin co100% (1)
- DSM 5 MCQ PDFDocument480 pagesDSM 5 MCQ PDFeinstein100% (10)
- Mechanical VentilationDocument26 pagesMechanical VentilationNirupama Ks91% (11)
- The Coagulopathy of Cancer: ReviewDocument7 pagesThe Coagulopathy of Cancer: ReviewlucyishakNo ratings yet
- Management of Hemostatic Complications in Acute Leukemia: Guidance From The SSC of The ISTHDocument10 pagesManagement of Hemostatic Complications in Acute Leukemia: Guidance From The SSC of The ISTHCarlos Enrique Almonte MarínNo ratings yet
- Horowitz NA, Brenner B. - Thrombosis in Hematological Malignancies, Mechanisms and ImplicationsDocument5 pagesHorowitz NA, Brenner B. - Thrombosis in Hematological Malignancies, Mechanisms and ImplicationsFarid RakhmanNo ratings yet
- JCTH 7 154Document11 pagesJCTH 7 154Andreea AlexandruNo ratings yet
- Cancer-Associated Thrombosis: John Winters,, David GarciaDocument13 pagesCancer-Associated Thrombosis: John Winters,, David GarciaMichel CaballeroNo ratings yet
- Cancer CoagulationDocument7 pagesCancer CoagulationPPDSNeuroUnsri RSMHNo ratings yet
- CancerDocument3 pagesCancerEngr ShahzaibNo ratings yet
- Seminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerDocument14 pagesSeminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerJuan Camilo Morales TabordaNo ratings yet
- Trombocytopenia in CaDocument7 pagesTrombocytopenia in CaanisaNo ratings yet
- Mulatu Et Al 2020 Deep Venous Thrombosis Recurrence and Its Predictors at Selected Tertiary Hospitals in Ethiopia ADocument14 pagesMulatu Et Al 2020 Deep Venous Thrombosis Recurrence and Its Predictors at Selected Tertiary Hospitals in Ethiopia Amulatbirhanu100No ratings yet
- Debate - Thromboprophylaxis Should Be Considered in All Patients With Cancer - YesDocument3 pagesDebate - Thromboprophylaxis Should Be Considered in All Patients With Cancer - YesJosé Eduardo Cárdenas MendozaNo ratings yet
- The Mechanisms of Cancer-Associated Thrombosis: Anna Falanga, Marina Marchetti, Laura RussoDocument4 pagesThe Mechanisms of Cancer-Associated Thrombosis: Anna Falanga, Marina Marchetti, Laura RussoThomaz DamianiNo ratings yet
- Fichamento para Introduçao: Thromboembolism: A Public Health Concern. American Journal of Preventive Medicine, DefiniçãoDocument20 pagesFichamento para Introduçao: Thromboembolism: A Public Health Concern. American Journal of Preventive Medicine, Definiçãolarissam123No ratings yet
- Acuteleukemia: Hayley Rose-Inman,, Damon KuehlDocument18 pagesAcuteleukemia: Hayley Rose-Inman,, Damon KuehlJorge Tovar AvilaNo ratings yet
- ThromboDocument21 pagesThromboJayzel LaureanoNo ratings yet
- Biomolecules 12 00259Document14 pagesBiomolecules 12 00259Wilmar Leonardo Nieto RosasNo ratings yet
- Prevention of Venous Thromboembolism in Patients With CancerDocument12 pagesPrevention of Venous Thromboembolism in Patients With CancertheriversongsNo ratings yet
- Megan Wiese, MS, PA-C Naval Daver, MDDocument11 pagesMegan Wiese, MS, PA-C Naval Daver, MDFathiyya SalsabilaNo ratings yet
- Caso TEP Bibliografia Bis 2023Document7 pagesCaso TEP Bibliografia Bis 2023Viviana MorenoNo ratings yet
- Oncol Article JCRC 18Document9 pagesOncol Article JCRC 18EliDavidNo ratings yet
- TEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For ManagementDocument10 pagesTEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For Managementbenitez1228No ratings yet
- Portal Vein Thrombosis: ReviewDocument9 pagesPortal Vein Thrombosis: ReviewMahmoud AbouelsoudNo ratings yet
- Tom Asian 2015Document16 pagesTom Asian 2015p8crtgy9t5No ratings yet
- Blom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisDocument8 pagesBlom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisFarid RakhmanNo ratings yet
- Cerebral Venous Thrombosis From UptodateDocument20 pagesCerebral Venous Thrombosis From UptodatewbudyaNo ratings yet
- Platelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisDocument7 pagesPlatelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisEvan Nanda AdilistyaNo ratings yet
- Patogenesis, Diagnosis, Dan Penatalaksanaan Tromboemboli Vena Pada KankerDocument9 pagesPatogenesis, Diagnosis, Dan Penatalaksanaan Tromboemboli Vena Pada KankerHerlina ApriliaNo ratings yet
- Tromboprofilaxia para TEV Na CirroseDocument9 pagesTromboprofilaxia para TEV Na CirroseLeonardo FurtadoNo ratings yet
- Defining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsDocument7 pagesDefining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsZikry AuliaNo ratings yet
- Bloodbook 2017 660 PDFDocument7 pagesBloodbook 2017 660 PDFSambit DashNo ratings yet
- 234 FullDocument8 pages234 FullLaura Daniela MurilloNo ratings yet
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 pagesPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalNo ratings yet
- Deep Venous Thrombosis 2022. ANNALSDocument20 pagesDeep Venous Thrombosis 2022. ANNALSErnesto LainezNo ratings yet
- Winter 2006Document8 pagesWinter 2006dewiNo ratings yet
- European Guidelines On Perioperative Venous.5Document12 pagesEuropean Guidelines On Perioperative Venous.5ionut.andruscaNo ratings yet
- Acute Leukemia ThesisDocument8 pagesAcute Leukemia Thesisafcnftqep100% (2)
- Clinical Guide SEOM On Venous Thromboembolism in Cancer PatientsDocument12 pagesClinical Guide SEOM On Venous Thromboembolism in Cancer PatientsGaby ValenzuelaNo ratings yet
- Perspectives: Platelet Activation and Inhibition in Polycythemia Vera and Essential ThrombocythemiaDocument12 pagesPerspectives: Platelet Activation and Inhibition in Polycythemia Vera and Essential ThrombocythemiaJicko Street HooligansNo ratings yet
- Guideline Karsinoma HepatoselulerDocument11 pagesGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoNo ratings yet
- Radiotherapy-Associated Neutropenia and Thrombocytopenia: Analysis of Risk Factors and Development of A Predictive ModelDocument8 pagesRadiotherapy-Associated Neutropenia and Thrombocytopenia: Analysis of Risk Factors and Development of A Predictive ModelClaudiu PopescuNo ratings yet
- Cancer PDFDocument9 pagesCancer PDFMihaela IonescuNo ratings yet
- The Risk of Thrombosis in Patients With Acute Leukemia: Occurrence of Thrombosis at Diagnosis and During TreatmentDocument8 pagesThe Risk of Thrombosis in Patients With Acute Leukemia: Occurrence of Thrombosis at Diagnosis and During TreatmentArifah GulamanisNo ratings yet
- ITP ZakrzepicaDocument8 pagesITP ZakrzepicaMagdalena Górska-KosickaNo ratings yet
- Onco-Nephrology: Glomerular Diseases With Cancer: Jean-Franc Ois Cambier and Pierre RoncoDocument12 pagesOnco-Nephrology: Glomerular Diseases With Cancer: Jean-Franc Ois Cambier and Pierre RoncoGlauber LeitaoNo ratings yet
- Acute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHDocument8 pagesAcute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHd40sithuiNo ratings yet
- VTE TopicDocument9 pagesVTE Topicram7676No ratings yet
- Risk Stratification and Management of Intermediate-Risk Acute Pulmonary EmbolismDocument20 pagesRisk Stratification and Management of Intermediate-Risk Acute Pulmonary EmbolismLuis Javier Vera ZamoraNo ratings yet
- Cardiotoxicidad en Mieloma MultopleDocument10 pagesCardiotoxicidad en Mieloma MultopleJose Antonio Aguilar HidalgoNo ratings yet
- Jurnal Perdarahan Kanker 1Document9 pagesJurnal Perdarahan Kanker 1jefel umarNo ratings yet
- Ojim 2016091213324550Document10 pagesOjim 2016091213324550rianmg21No ratings yet
- Pages 4 7Document4 pagesPages 4 7andreas_251650No ratings yet
- Assessing Hypercoagulability and VTE Risk Using Thromboelastography and Khorana Score in Women With Cancers Receiving Chemotherapy 2024Document9 pagesAssessing Hypercoagulability and VTE Risk Using Thromboelastography and Khorana Score in Women With Cancers Receiving Chemotherapy 2024myqrwd464kNo ratings yet
- Acute Myeloid LeukemiaDocument11 pagesAcute Myeloid Leukemiafitra azraNo ratings yet
- Cancer and Liver Cirrhosis: Implications On Prognosis and ManagementDocument16 pagesCancer and Liver Cirrhosis: Implications On Prognosis and ManagementAlifia Ramadhanty PrameswariNo ratings yet
- Venous Thromboembolism in MalignancyDocument3 pagesVenous Thromboembolism in MalignancyAzmi FarhadiNo ratings yet
- Leunase and TrombolismDocument12 pagesLeunase and TrombolismSanta UlinaNo ratings yet
- Retinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionDocument4 pagesRetinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionmaryNo ratings yet
- Myelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentDocument11 pagesMyelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentTataNo ratings yet
- GastroprofilaxisDocument13 pagesGastroprofilaxisDaniel Alejandro Lecaros BarríaNo ratings yet
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsFrom EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsNo ratings yet
- Kadar Fibrinogen Sebagai Faktor Prognostik Pasien Perdarahan Intraserebral SpontanDocument5 pagesKadar Fibrinogen Sebagai Faktor Prognostik Pasien Perdarahan Intraserebral Spontanannisa edwarNo ratings yet
- Associations Between SeratoninDocument11 pagesAssociations Between Seratoninannisa edwarNo ratings yet
- EHMTI-0299. Serotonin As Biomarker of Ache Intensity in Chronic Tension HeadacheDocument1 pageEHMTI-0299. Serotonin As Biomarker of Ache Intensity in Chronic Tension Headacheannisa edwarNo ratings yet
- KDIGO BP Exec Summary FinalDocument11 pagesKDIGO BP Exec Summary Finalannisa edwarNo ratings yet
- Myofascial Trigger Points and Sensitization: An Updated Pain Model For Tension-Type HeadacheDocument11 pagesMyofascial Trigger Points and Sensitization: An Updated Pain Model For Tension-Type Headacheannisa edwarNo ratings yet
- Jnen 080 Sherifa Ahmad HamedDocument8 pagesJnen 080 Sherifa Ahmad Hamedannisa edwarNo ratings yet
- Routine Use of Vitamin K in The Treatment of Cirrhosis-Related Coagulopathy: Is It A-O-K? Maybe Not, We SayDocument6 pagesRoutine Use of Vitamin K in The Treatment of Cirrhosis-Related Coagulopathy: Is It A-O-K? Maybe Not, We Sayannisa edwarNo ratings yet
- Duty Dr. Iqbal - 1Document13 pagesDuty Dr. Iqbal - 1annisa edwarNo ratings yet
- Pathophysiological Mechanisms of Hepatic Encephalopathy: ReviewDocument5 pagesPathophysiological Mechanisms of Hepatic Encephalopathy: Reviewannisa edwarNo ratings yet
- Nurhayati, Female, 61 Yo, Neurology Ward: Chief Complaint: Present Illness HistoryDocument26 pagesNurhayati, Female, 61 Yo, Neurology Ward: Chief Complaint: Present Illness Historyannisa edwarNo ratings yet
- Firdaus Latif/Male/63 yo/MW 23: - Weakness and Fatigue Since 1 Month AgoDocument13 pagesFirdaus Latif/Male/63 yo/MW 23: - Weakness and Fatigue Since 1 Month Agoannisa edwarNo ratings yet
- Duration of Fasting During Acute Variceal BleedingDocument4 pagesDuration of Fasting During Acute Variceal Bleedingannisa edwarNo ratings yet
- Chronic Wound Managment HMIDocument37 pagesChronic Wound Managment HMIannisa edwarNo ratings yet
- Refit / Male / 24 Yo/ HCU 17: - Headache Increased Since 6 Hours AgoDocument14 pagesRefit / Male / 24 Yo/ HCU 17: - Headache Increased Since 6 Hours Agoannisa edwarNo ratings yet
- Asril Hepatoma (Autosaved)Document14 pagesAsril Hepatoma (Autosaved)annisa edwarNo ratings yet
- Menan - Dr. AnggitDocument19 pagesMenan - Dr. Anggitannisa edwarNo ratings yet
- Morning VidraDocument17 pagesMorning Vidraannisa edwarNo ratings yet
- Irwan/Male/ 42 Yo/ MW 17: Chief ComplaintDocument15 pagesIrwan/Male/ 42 Yo/ MW 17: Chief Complaintannisa edwarNo ratings yet
- Robert Georgy Ulimally/Male/51 YO/MW 21: Chief Complaint: Abdominal PainDocument14 pagesRobert Georgy Ulimally/Male/51 YO/MW 21: Chief Complaint: Abdominal Painannisa edwarNo ratings yet
- Morning AsriantiDocument15 pagesMorning Asriantiannisa edwarNo ratings yet
- Morning & Duty: 30 September 2021Document16 pagesMorning & Duty: 30 September 2021annisa edwarNo ratings yet
- Misnizar/female/46yo/FW 20: Chief Complaint: Fatigue and Weakness Since 3 Days AgoDocument13 pagesMisnizar/female/46yo/FW 20: Chief Complaint: Fatigue and Weakness Since 3 Days Agoannisa edwarNo ratings yet
- Morning Report 30-9Document15 pagesMorning Report 30-9annisa edwarNo ratings yet
- Guideline For Stress Ulcer Prophylaxis in The Intensive Care UnitDocument4 pagesGuideline For Stress Ulcer Prophylaxis in The Intensive Care Unitannisa edwarNo ratings yet
- Nursing Care Management of Patients With Anemia - 01Document38 pagesNursing Care Management of Patients With Anemia - 01Sionur 00No ratings yet
- FOLK MEDICINE ExtraDocument22 pagesFOLK MEDICINE ExtraPaul SavvyNo ratings yet
- Coronary Slow FlowDocument7 pagesCoronary Slow FlowradiomedicNo ratings yet
- Stock 8 Desember 2021Document102 pagesStock 8 Desember 2021Damaris Luisa DjadaNo ratings yet
- Ears Lecture GuideDocument56 pagesEars Lecture GuidemajNo ratings yet
- Statins and DiabetesDocument9 pagesStatins and DiabetesJonathan TorresNo ratings yet
- 2004, Vol.6, No.4, Pediatric Surgery PDFDocument95 pages2004, Vol.6, No.4, Pediatric Surgery PDFAnty Dewi Sarty RanyabarNo ratings yet
- History Taking HandbookDocument2 pagesHistory Taking Handbookyouservezeropurpose113No ratings yet
- NCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicDocument18 pagesNCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicSIJINo ratings yet
- Pain Assessment - Worksheet - Advanced PDFDocument4 pagesPain Assessment - Worksheet - Advanced PDFsaran segah RohanNo ratings yet
- Dermatology MiniOSCE 2Document352 pagesDermatology MiniOSCE 2Gmail JONo ratings yet
- Knowledge, Awareness and Attitude Towards Organ Donation Among Undergraduate Medical Students of HaryanaDocument5 pagesKnowledge, Awareness and Attitude Towards Organ Donation Among Undergraduate Medical Students of HaryanaVinissha JeyarajNo ratings yet
- 74 Anaesthesia For Intestinal Obstruction in Children 1Document6 pages74 Anaesthesia For Intestinal Obstruction in Children 1Dr. Anish GolchhaNo ratings yet
- Discharge Instruction: Fitriani Pratiwi M.PDDocument13 pagesDischarge Instruction: Fitriani Pratiwi M.PDSaniaNo ratings yet
- Ecografo Aloka Modelo SSD-3500Document34 pagesEcografo Aloka Modelo SSD-3500EmilioPerezBallesterosNo ratings yet
- Mothers Knowledge and Practices of Minor IllnessesDocument17 pagesMothers Knowledge and Practices of Minor IllnessesSTANN KAZIPETNo ratings yet
- Unusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewDocument4 pagesUnusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewMirachel AugustNo ratings yet
- Documentation Dissection: New Patient Visit OafDocument3 pagesDocumentation Dissection: New Patient Visit OaftestNo ratings yet
- Effects of Computer AddictionDocument11 pagesEffects of Computer AddictionErich Trinidad33% (3)
- Daftar Harga Airway PT. Surgika 2017Document16 pagesDaftar Harga Airway PT. Surgika 2017Syaofi SofiNo ratings yet
- 2011 Fundchap9-Firesafety11-1Document19 pages2011 Fundchap9-Firesafety11-1api-272722550No ratings yet
- Postnatal Care PDF 66142082148037Document64 pagesPostnatal Care PDF 66142082148037veronia widayantiNo ratings yet
- Breaking Ground On ADHD Diagnosis in PakistanDocument1 pageBreaking Ground On ADHD Diagnosis in PakistanAnum Rizwan FazalNo ratings yet
- Drug Study Amoxicillin PDFDocument4 pagesDrug Study Amoxicillin PDFMc SantosNo ratings yet
- Symptoms of Ovarian CancerDocument3 pagesSymptoms of Ovarian Cancerwwe_jhoNo ratings yet
- Bartholin's Gland Cyst MarsupializationDocument3 pagesBartholin's Gland Cyst MarsupializationIndra JayaNo ratings yet
- PERCEPTION-COORDINATION-PRE-TEST RationalizationDocument11 pagesPERCEPTION-COORDINATION-PRE-TEST Rationalizationdrei yanNo ratings yet
Thrombosis and Acute Leukemia
Thrombosis and Acute Leukemia
Uploaded by
annisa edwarOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thrombosis and Acute Leukemia
Thrombosis and Acute Leukemia
Uploaded by
annisa edwarCopyright:
Available Formats
Hematology
ISSN: (Print) 1607-8454 (Online) Journal homepage: https://www.tandfonline.com/loi/yhem20
Thrombosis and acute leukemia
Erick Crespo-Solís
To cite this article: Erick Crespo-Solís (2012) Thrombosis and acute leukemia, Hematology,
17:sup1, s169-s173, DOI: 10.1179/102453312X13336169156852
To link to this article: https://doi.org/10.1179/102453312X13336169156852
Published online: 12 Nov 2013.
Submit your article to this journal
Article views: 1041
View related articles
Citing articles: 2 View citing articles
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=yhem20
Thrombosis and acute leukemia
Erick Crespo-Solı́s
Clı́nica de Leucemia Aguda, Departamento de Hematologı́a y Oncologı́a, Instituto Nacional de Ciencias Médicas
y Nutrición Salvador Zubirán, Mexico City, Mexico
Thrombosis is a common complication in patients with acute leukemia. While the presence of central
venous lines, concomitant steroids, the use of Escherichia coli asparaginase and hereditary thrombophilic
abnormalities are known risk factors for thrombosis in children, information on the pathogenesis, risk
factors, and clinical outcome of thrombosis in adult patients with acute lymphoid leukemia (ALL) or acute
myeloid leukemia (AML) is still scarce. Expert consensus and guidelines regarding leukemia-specific risk
factors, thrombosis prevention, and treatment strategies, as well as optimal type of central venous catheter
in acute leukemia patients are required. It is likely that each subtype of acute leukemia represents a
different setting for the development of thrombosis and the risk of bleeding. This is perhaps due to a
combination of different disease-specific pathogenic mechanisms of thrombosis, including the type of
chemotherapy protocol chosen, the underlying patients health, associated risk factors, as well as the
biology of the disease itself. The risk of thrombosis may also vary according to ethnicity and prevalence of
hereditary risk factors for thrombosis; thus, it is advisable for Latin American, Asian, and African countries
to report on their specific patient population.
Keywords: Acute leukemia, Thrombosis, Risk factors
Thrombosis and Cancer Prophylaxis with low-molecular-weight heparin
Thrombosis is a common complication in cancer (LMWH) or unfractionated heparin is indicated in
patients and the association between these two patients with cancer undergoing major surgery. This
entities has been known for centuries. Deep venous same prophylactic measures may benefit medical
thrombosis and pulmonary embolism (PE) are the oncology patients admitted to the hospital with an
most common cancer-associated thrombotic events. acute illness.3 However, prophylaxis may represent a
Cancer patients account for 20% of all patients with risk per se in patients with acute leukemia with very
venous thromboembolism (VTE), and in recent years, low platelet counts or with coagulation disorders.
the reported incidence has been as high as 28% of Initial treatment of VTE consists of anticoagulant
hospitalized cancer patients.1 therapy; LMWH or unfractionated heparin are the
The mortality rate in patients with cancer and preferred frontline drugs. Secondary prophylaxis with
thrombosis is higher (16.3%) than in those without vitamin K antagonists can also be initiated on the
thrombosis (6.3%), particularly in patients who same day as heparin therapy. Treatment must be
develop PE (24.8%).2 Some tumor types are more adjusted to maintain an international normalized ratio
likely to be associated with the development of within 2.0–3.0. The annual incidence of recurrent VTE
thromboses: pancreas, brain, ovary, and lung. About in patients without cancer is 8%, but in patients with
10% of patients with idiopathic VTE will be diagnosed cancer, this rate increases two- to threefold. This could
with cancer within the following 10 years (more than be a consequence of the difficulty in maintaining
75% will be diagnosed within the first year).3 an optimal international normalized ratio in these
A validated scoring system predicting the develop- patients, due to drug interactions, anorexia, malnutri-
ment of VTE in cancer patients has been proposed, tion, liver dysfunction, and poor gastrointestinal
and is appropriate for solid tumors;4 yet, its para- tolerance,3 as well as the presence of tumor-related
meters such as high leucocyte or platelet counts, are prothrombotic factors such as mechanical vascular
not useful for patients with acute leukemia. compression or an increase in molecular activators of
coagulation due to the overexpression of tissue factor
by malignant cells.
Correspondence to: E. Crespo-Solı́s, Clı́nica de Leucemia Aguda,
Departamento de Hematologı́a y Oncologı́a, Instituto Nacional de Ciencias The Italian Society for Haemostasis and Thrombosis
Médicas y Nutrición Salvador Zubirán, Vasco de Quiroga #15, Sección XVI, recommends LMWH for the first 6 months in patients
Tlalpan, CP 14000 Mexico City. Mexico. Email: erickerickmx@
yahoo.com.mx with VTE and hematological malignancies. In patients
ß W. S. Maney & Son Ltd 2012
DOI 10.1179/102453312X13336169156852 Hematology 2012 VOL . 17 SUPPL . 1 S 169
Crespo-Solı́s Thrombosis in patients with acute leukemia
with severe and prolonged thrombocytopenia, the use protocol had an incidence of 10%. Several risk factors
of LMWH is preferable to oral anticoagulant therapy.5 were evaluated in the multivariate analysis. Only
Recommendations for treatment of thrombosis in the concomitant administration of Escherichia coli
patients with cancer are mostly based on studies of asparaginase/prednisone to leukemic children with a
patients with solid tumors.3,5,6 Guidelines for prophy- prothrombotic risk factor was found to increase the
laxis and management of VTE based on prospective risk of thrombosis (odds ratio: 34.5; 95% confidence
studies conducted in acute leukemia patients are interval: 4.39–271.42; P50.0008). Interestingly, the
lacking. differences in thrombosis rates were observed only
during induction chemotherapy.18
Thrombosis and Acute Leukemia The incidence of thrombosis also varies according
Patients with acute leukemia present both an to the study period (before or after 1990). The overall
increased risk of hemorrhage, as well as of thrombo- incidence of VTE in studies conducted or reported
sis. The incidence of thrombosis varies between 2 and before or after 1990 is 1.8 and 4.7%, respectively. This
36%.7–14 may be possibly explained by improved diagnostic
Relevant aspects regarding patients with acute methods, different chemotherapy regimens or an
leukemia and thrombosis are as follows:
increase in suspicion and confirmation of the
1. association between central catheters and throm-
bosis and its clinical variability on presentation diagnosis of thrombosis.15 Regarding the site of
(symptomatic or asymptomatic); thrombosis, a reported 52% of patients with central
2. association between L-asparaginase during induc- nervous system thromboembolism have venous sinus
tion chemotherapy and thrombosis in patients with involvement. Thrombosis may affect overall survival,
acute lymphoid leukemia (ALL); quality of life, and cognitive function. There are no
3. recognition of thrombosis as a frequent and
perhaps underestimated complication in patients data regarding the recurrence of thrombosis in this
with acute promyelocytic leukemia (APL); population. Patients are reported to have residual
4. inconsistencies among reports in the literature neurological deficits or seizure disorders. Associated
regarding risk factors for thrombosis (gender, age, morbidity is approximately 15–20% in cases of cen-
leukemia subtype, catheter characteristics, comor- tral nervous system (CNS) thrombosis.15
bidity, and genetic mutations) and their impact on
L-asparaginase decreases plasminogen, fibrinogen,
overall survival.
and antithrombin, resulting in impaired thrombin
ALL inhibition which may contribute to the asparaginase-
As with any other disease, patients with ALL develop related dose-limiting toxicity.19-21 Changes in anti-
thromboses as a result of an interaction of factors. thrombin (AT) and fibrinogen during induction che-
According to current evidence, the main contributors motherapy with L-asparaginase were reported in a
include the disease itself, the type of administer- retrospective study of 214 adult patients with ALL.22
ed chemotherapy, central venous catheters (CVC), The median AT levels decreased from 120 to 59%
genetic abnormalities, as well as an acquired predis- after the fourth L-asparaginase infusion. AT levels
position. Most published studies are in pediatric below 60% were found in 50% of cases. Fibrinogen
patients. As reported by Athale and Chan,15 the levels decreased from 2.9 g/l at diagnosis, to 1.9 g/l
average incidence of thrombosis in children with ALL before the first infusion, they continued to decrease
is 3%. According to a prospective study in adults with after the first 10 days of induction therapy and
ALL, the incidence of thrombosis increases to 9.6%.10 reached a median value of 1.1 g/l at the time of the
Variation in the incidence of thrombosis depends on fourth L-asparaginase infusion. Infusion of AT
several factors, such as the study design, prospective concentrate was followed by a significant increase in
versus retrospective,16,17 whereby the former tend to AT levels, from 61 to 88%. Fibrinogen levels
report higher incidences of thrombotic phenomena. significantly increased after fibrinogen concentrate
Furthermore, studies designed to detect asymptomatic administration, from 1 to 1.4 g/l. Fresh frozen plasma
thrombosis have also reported increased thrombosis was not effective in significantly ameliorating AT or
incidence rates.15 The incidence of thrombosis is also fibrinogen levels. The incidence of thrombosis was
related to the treatment regimen. 9.8% during induction therapy and all thrombotic
The German group has reported different inci- events occurred within 2–35 days after the first
dence rates of thrombosis when comparing patients injection of L-asparaginase during induction che-
receiving the Berlin–Frankfurt–Münster (BFM) or motherapy. No mention of catheter-related throm-
the Cooperative Study Group for Childhood Acute boses was made, but 25% of thrombotic events
Lymphoblastic Leukemia (COALL) chemotherapy developed in the upper limbs. The use of oral
protocols. Patients receiving the COALL protocol contraceptives was more frequent in women with
had a 0.8% incidence of thrombosis during induction thrombosis than in those without. Other factors such
chemotherapy, whereas patients receiving the BFM as familial thrombophilia, previous thrombosis, age,
S170 Hematology 2012 VOL . 17 SUPPL . 1
Crespo-Solı́s Thrombosis in patients with acute leukemia
AT levels ,60%, fibrinogen levels ,0.5 g/l and low patients is challenging, because of the considerable
doses of heparin were similar between groups of risk of hemorrhage due to severe thrombocytopenia
patients with and without thrombosis. The complete and coagulation and/or fibrinolysis abnormalities. A
remission rate was similar in patients with and patient with bleeding and PE is not an uncommon
without thrombosis, but thrombus development was picture for clinicians treating AML, especially at
associated with a decreased median overall survival diagnosis and during the induction phase.
(19 months versus 53 months), as well as a decreased Thromboses are treated with LMWH. Monitoring
disease-free survival (14 months versus 58 months). of anti-Xa and maintenance of peak levels between
Some studies have reported a genetic prothrombo- 0.5 and 1 IU/ml in patients with renal failure, obesity,
tic predisposition as an important host factor in pregnancy, and children, as well as close observation
the development of VTE in children with ALL,23 of the platelet count are mandatory. LMWH should
whereas others have failed to demonstrate such an be decreased by 50%, if the platelet count drops to
association.24 Whether to administer primary antic- 50610(9)/l or below, or temporarily discontinued if
oagulant prophylaxis with LMWH to children with ,20610(9)/l.37
ALL during induction chemotherapy, remains con- Important data obtained by Ku et al.11 in a
troversial. A recent retrospective study of 80 children population-based cohort, was used to determine the
with ALL,25 demonstrated an incidence of genetic incidence of thrombosis in an American population
thrombophilia of 22.5% (factor II G20210A and (California) of 5394 patients with AML or ALL. The
factor V Leiden). These patients received prophylac- 2-year cumulative incidence of VTE was 5.2%,
tic enoxaparin, but 7.5% developed thromboembolic comparable to that in patients with solid tumors.
events. VTE was not detected in patients with factor Interestingly, 64% of thrombotic events developed
V Leiden, suggesting that ALL patients with the PT within the first 3 months of the leukemia diagnosis.
gene mutation are at increased risk of developing Risk factors for VTE in AML included female
clotting complications in comparison with those gender, older age, the number of chronic comorbid-
harboring the factor V Leiden mutation. ities, and the presence of an indwelling catheter. In
All patients with acute leukemia require placement ALL patients, the 2-year cumulative incidence of
of a CVC for cytotoxic chemotherapy administration. VTE was 4.5%. Risk factors for VTE included the
All types of CVCs are associated with infection and presence of a central venous catheter, older age, and
thrombosis. Actually, thrombosis is a risk factor for the number of chronic comorbidities. As opposed to
developing infection of the CVC and this association AML patients in whom survival was not affected by
has been documented for over 25 years.26,27 Autopsy VTE, ALL individuals had a 40% increase in the risk
and venographic studies have demonstrated that soon of death during the first year after diagnosis.
after the insertion of a catheter, practically all will
develop a fibrin sheath.28,29 APL
Different diagnostic methods have been used to APL patients present a particular scenario, whereby
demonstrate that the aforementioned fibrin sheaths fatal hemorrhages due to disseminated intravascular
are always colonized by cocci.30–32 The type of coagulation were the major cause of early death be-
catheter-related thrombosis may be due to either fore the use of all trans-retinoic acid as part of the
clotting of the lumen (13–93%) or the development of induction treatment. Currently, the rate of fatal he-
mural thrombi in the vessel where the catheter is morrhages ranges between 2.4 and 6.5%.38 Increased
placed (12–74%).33–35 fibrinolysis has been documented and overexpression
Approximately, a third of CVC-related thromboses of annexin A2 may be one of the underlying
are symptomatic. Factors favoring the development of mechanisms, conditioning the hemorrhagic complica-
CVC-related thromboses include malignancy, throm- tions in these patients. Abnormally high levels of
bophilia, endothelial cell injury due to the CVC itself or annexin A2 on APL cells increase plasmin generation
to chemotherapy, the position of the catheter in the that in turn, activates fibrinolysis. Furthermore,
vascular system and the number of catheter lumens.34 annexin II mRNA levels are reduced after treatment
The most important sequelae are pulmonary emboli, with all trans-retinoic acid39 and arsenic trioxide.40
post-phlebitic syndrome, and infection, with an esti- Thrombosis is probably an underestimated complica-
mated frequency of 6, 15–35, and 18%, respectively.33 tion in APL patients.41 Concomitant hemorrhage and
thrombosis have also been reported during induction
Acute Myeloid Leukemia (AML) chemotherapy. A retrospective study of 34 consecutive
Additional risk factors for VTE in AML patients APL patients in a single referral center in Israel,
include the increased expression of tissue factor in reported an incidence of severe thrombosis of 12%.
leukemic cells, its activation on cellular surfaces, and Life-threatening bleeding occurred in 29% of patients.
hyperleukocytosis.36 Treatment of VTE in AML The most consistent hemostatic abnormality was
Hematology 2012 VOL . 17 SUPPL . 1 S 171
Crespo-Solı́s Thrombosis in patients with acute leukemia
Haemostasis and Thrombosis (SISET). Thromb Res.
decreased fibrinogen (,150 mg/dl) in 61% of cases. On 2009;124:e32–40.
multivariate analysis, only the leukocyte count 6 Louzada ML, Majeed H, Wells PS. Efficacy of low-molecular-
(,30610(9)/ml) reached statistical significance as a weight-heparin versus vitamin K antagonists for long term
treatment of cancer-associated venous thromboembolism in
predictor of bleeding. Interestingly, none of the hemo- adults: a systematic review of randomized controlled trials.
static parameters (platelet, fibrinogen, PT, and APTT) Thromb Res. 2009;123:837–44.
7 Ziegler S, Sperr WR, Knöbl P, Lehr S, Weltermann A, Jäger U,
were identified as risk factors for bleeding or et al. Symptomatic venous thromboembolism in acute leuke-
thrombosis. Of note, three out six patients with mia: incidence, risk factors and impact on prognosis. Thromb
Res. 2005;115:59–64.
thrombotic events were found to be thrombophilic.42 8 Mohren M, Markmann I, Jentsch-Ullrich K, Koenigsmann M,
There is a case report of a patient with APL who Lutze G, Franke A. Increased risk of venous thromboembolism
in patients with acute leukemia. Br J Cancer. 2006;94:200–2.
developed splenic, renal, and intestinal infarction 9 de Stefano V, Sorà F, Rossi E, Chiusolo P, Laurenti L, Fianchi
due to severe acquired protein C deficiency; no evi- L, et al. The risk of thrombosis in patients with acute leukemia:
dence of disseminated intravascular coagulation was ocurrence of thrombosis at diagnosis and during treatment. J
Thromb Haemost. 2005;3:1985–92.
documented.43 In an Italian study,44 patients with 10 Melillo L, Grandone E, Colaizzo D, Cappucci F, Valvano MR,
thrombosis had a higher white blood cell count and an Cascavilla N. Symptomatic venous thromboembolism and
thrombophilic status in adult acute leukemia: a single center
increased prevalence of the short PML/RARA iso- experience of 114 patients at diagnosis. Acta Haematol.
form (bcr3), FLT3/ITD, CD2, and CD5 expression. 2007;117:215–20.
11 Ku GH, White RH, Chew HK, Harvey DJ, Zhou H, Wun T.
The PETHEMA study45 did not confirm these Venous thromboembolism in patients with acute leukemia.
thrombosis risk factors. Instead, the identified risk Incidence, risk factors and effect on survival. Blood.
2009;113:3911–7.
factors included: fibrinogen ,170 mg/dl, an M3 12 Athale UH, Chan AK. Thrombosis in children with acute
variant at diagnosis and tranexamic acid prophylaxis lymphoblastic leukemia Part I. Epidemiology of thrombosis in
children with acute lymphoblastic leukemia. Thromb Res.
during induction chemotherapy. 2003;11:125–31.
13 Athale U, Siciliano S, Thabane L, Pai N, Cox S, Lathia A, et al.
Conclusions Epidemiology and clinical risk factors predisposing to throm-
boembolism in children with cancer. Pediatr Blood Cancer.
Thrombosis is a common complication in patients 2008;51:792–7.
with acute leukemia. Most of the information on ALL 14 Caruso V, Lacoviello L, di Castelnuevo A, Storti S, Mariani G,
de Gaetano G, et al. Thrombotic complications in childhood
patients has been obtained from studies in children acute lymphoblastic leukemia: a meta-analysis of 17 prospective
and the information in adult patients remains scant. studies comprising 1752 pediatric patients. Blood.
Expert consensus and guidelines on risk factors, 2006;108:2216–22.
15 Payne JH, Vora AJ. Thrombosis and acute lymphoblastic
optimum catheter care, use and management, preven- leukemia. Br J Haematol. 2007;138:430–45.
tion and treatment of thrombosis are required. The 16 Korte W, Fledges A, Baumgartner C, Ullmann S, Niederer V,
Schmid L. Increased thrombin generation during fibrinogen
role of newer anticoagulants needs to be explored in and platelet recovery as an explanation for hypercoagulability
multicenter clinical trials, and risk factors should be in children with L-asparaginase therapy for ALL or NHL: a
preliminary report. Klin Padiatr. 1994;206:331–3.
standardized, in order to understand the disease’s 17 Sutor AH, Mall V, Thomas KB. Bleeding and thrombosis in
pathogenesis and provide adequate treatment to these children with acute lymphoblastic leukemia, treated according
to the ALL-BFM-90 ptrotocol. Klin Padiatr. 1999;211:201–4.
patients within a complicated setting of thrombosis 18 Nowak-Göttl U, Heinecke A, von Kries R, Nürnberger W,
and hemorrhage. Münchow N, Junker R. Thrombotic events revisited in children
with acute lymphoblastic leukemia. Impact of concomitant
Ideally, guidelines should be based on prospectively Escherichia coli asparaginase/prednisone administration.
designed studies conducted only in patients with acute Thromb Res. 2001;103:165–72.
leukemia. Furthermore, they should be designed sepa- 19 Silverman LB, Gelber RD, Dalton VK, Asselin BL, Barr RD,
Clavell LA, et al. Improved outcome for children with acute
rately, according to leukemia subtype (ALL, AML, lymphoblastic leukemia: results of the Dana-Farber
and APL). It is very probable that each acute leukemia Consortium Protocol 91-01. Blood. 2001;97:1211–8.
20 Mitchell L, Hoogendoorn H, Giles AR, Vegh P, Andrew M.
subtype represents a different physiopathogenic set- Increased endogenous thrombin generation in children with
ting favoring the development of thrombosis. ALL: risk of thrombotic complications in L-asparaginase
induced antithrombin deficiency. Blood. 1994;83:386–91.
21 Bushman JE, Palmieri D, Whinna HC, Church FC. Insight into
References the mechanism of asparaginase-induced depletion of antith-
rombin III in treatment of childhood ALL. Leuk Res.
1 Khorana AA. Venous thromboembolism and prognosis in 2000;24:559–65.
cancer. Thromb Res. 2010;125:490–3. 22 Hunault-Berger M, Chevallier P, Delain M, Bulabois CE,
2 Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman Bologna S, Bernard M, et al. Changes in antithrombin and
GH, James P. Frequency, risk factors, and trendsfor venous fibrinogen levels during induction chemotherapy with L-
thromboembolism among hospitalized cancer patients. Cancer. asparaginase in adult patients with acute lymphoblastic
2007;110:2339–46. leukemia or lymphoblastoc lymphoma. Use of supportive
3 Lee AY. Epidemiology and management of venous throm- coagulation therapy and clinical outcome: the CAPELAL
boembolism in patients with cancer. Thromb Res. study. Haematologica. 2008;93;1488–94.
2003;110:167–72. 23 Nowak-Gottl U, Wermes C, Junker R, Koch HG, Schobess R,
4 Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis Fleischhack G, et al. Prospective evaluation of the thrombotic
CW. Development and validation of a predictive model for risk in children with ALL carrying the MTHFR TT 677
chemotherapy-associated thrombosis. Blood. 2008;111:4902–7. genotype, the prothrombine G20210A variant and further
5 Imberti D, di Nisio M, Donati MB, Falanga A, Ghirarduzzi A, prothrombotic risk factors. Blood. 1999;93:1595–9.
Guarneri D, et al. Treatment of venous thromboembolism in 24 Mitchell LG, Andrew M, Hanna K, Abshire T, Halton J,
patients with cancer: guidelines of the Italian Society for Anderson R, et al. A prospective cohort study determining the
S172 Hematology 2012 VOL . 17 SUPPL . 1
Crespo-Solı́s Thrombosis in patients with acute leukemia
prevalence of thrombotic events in children with ALL and a 34 Hurtubise MR, Bottino JC, Lawson M, McCredie KB.
central venous line who are treated with L-aparaginase: results Restoring patency of occluded central venous catheters. Arch
of the Prophylactic Antithrombin Replacement in Kids with Surg. 1980;115:212–3.
ALL Treated with sparaginase (PARKAA) study. Cancer. 35 Beckers MM, Ruven HJ, Seldenrijk CA, Prins MH, Biesma
2003;97:508–16. DH. Risk of thrombosis and infections of central venous
25 Harlev D, Zaidman I, Sarig G, Ben Arush MW, Brenner B, catheters and totally implanted access ports in patients treated
Elhasid R. Prophylactic therapy with enoxaparin in children for cancer. Thromb Res. 2010;125:318–21.
with acute lymphoblastic leukemia and inherited thrombophilia 36 Oehadian A, Iqhal M, Sumantri R. Deep vein thrombosis in
during L-asparaginase treatment. Thromb Res. 2010;126:93–7. acute myelogenous leukemia. Acta Med Indones-Indones J
26 Press OW, Ramsey PG, Larson EB, Fefer A, Hickman RO. Intern Med. 2009;41:200–4.
Hickman catheter infections in patients with malignancies. 37 Falanga A, Rickles FR. Management of thrombohemorrhagic
Medicine (Baltimore). 1984;63:189–200. syndrome (THS) in hematologic malignancies. Hematology.
27 Raad II, Luna M, Khalil SA, Costerton JW, Lam C, Bodey 2007;165–71.
GP. The relationship between the thrombotic and infection 38 Falanga A, Marchetti M. Venous thromboembolism in the
complications of central venous catheters. JAMA. hematological malignancies. J Clin Oncol. 2009;27:4848–57.
1994;271:1014–6. 39 Menell JS, Cesarman GM, Andrew T, McLaughlin MA, Lev
28 Balestreri L, de Cicco M, Matorio M, Coran F, Morassut S. EA, Hajjar KA. Annexin II and bleeding in acute promyelo-
Central venous catheter-related thrombosis in clinically asymp- cytic leukemia. N Eng J Med. 1999;340:994–1004.
tomatic oncologic patients: a plebography study. Eur J Radiol. 40 Liu YH, Wang ZY, Shen WH. Influence of arsenic trioxide and
1995;20:108–11. daunorubicin on the expression of annexin II and fibrinolytic
29 de Cicco M, Matorio M, Balstreri L, Panarello G, Fantin D, activity in NB4 cells. Zhongua Xue Ye Xue Za Zhi.
Morassut S, et al. Central venous thrombosis: an early and 2010;12:813–6. Chinese.
frequent complication in cancer patients bearing long-term 41 Sanz MA, Montesinos P. Open issues on bleeding and
silastic catéter. A prospective study. Thromb Res. 1997;86:101– thrombosis in acute promyelocytic leukemia Thromb Res.
13. 2010;125 Suppl 2:S51–4.
30 Starkhammar H, Bengtsson M, Morales O. Fibrin sleeve 42 Dally N, Hoffman R, Haddad N, Sarig G, Rowe JM, Brenner
formation after long term brachial catheterization with B. Predictive factors of bleeding and thrombosis during
implantable port device. A prospective study. Eur J Surg. induction therapy in acute promyelocytic leukemia — a single
1992;158:481–4. center experience in 34 patients. Thromb Res. 2005;116:109–14.
31 Raad I, Custerton W, Sabharwal U, Sacilowski M, Anaissie E, 43 Kwaan HC, Huyck T. Thromboembolic and bleeding compli-
Bodey GP. Ultrastructural analysis of indwelling vascular cations in acute leukemia. Expert Rev Hematol. 2010;6:719–30.
catheters: a quantitative relationship between luminal coloniza- 44 Breccia M, Avvisati G, Latagliata R, Carmosino I, Guarini A,
tion during of placement. J Infect Dis. 1993;168:400–7. de Propris MS, et al. Occurrence of thrombotic events in acute
32 Tenney JH, Moody MR, Newman KA, Schimpff SC, Wade JC, promyelocytic leukemia correlates with consistent immunophe-
Costerton JW, et al. Adherent microorganisms on luminal notyping and molecular features. Leukemia. 2007;21:79–83.
surfaces of a long-term intravenous catheters. Importance of 45 Montesinos P, de la Serna J, Vellenga E, Rayon C, Bergua J,
Staphylococcus epidermidis in patient with cancer. Arch Intern Parody R, et al. Incidence and risk factors for thrombosis in
Med. 1986;146:1949–54. patients with acute promyelocytic leukemia. Experience of the
33 Kuter DJ. Thrombotic complications of central venous PETHEMA LPA96 and LPA99 Protocols. Blood (ASH Ann
catheters in cancer patients. The Oncologist. 2004;9:207–16. Meet Abstr). 2006;108:1503.
Hematology 2012 VOL . 17 SUPPL . 1 S 173
You might also like
- Board Stiff ThreeDocument440 pagesBoard Stiff Threewin co100% (1)
- DSM 5 MCQ PDFDocument480 pagesDSM 5 MCQ PDFeinstein100% (10)
- Mechanical VentilationDocument26 pagesMechanical VentilationNirupama Ks91% (11)
- The Coagulopathy of Cancer: ReviewDocument7 pagesThe Coagulopathy of Cancer: ReviewlucyishakNo ratings yet
- Management of Hemostatic Complications in Acute Leukemia: Guidance From The SSC of The ISTHDocument10 pagesManagement of Hemostatic Complications in Acute Leukemia: Guidance From The SSC of The ISTHCarlos Enrique Almonte MarínNo ratings yet
- Horowitz NA, Brenner B. - Thrombosis in Hematological Malignancies, Mechanisms and ImplicationsDocument5 pagesHorowitz NA, Brenner B. - Thrombosis in Hematological Malignancies, Mechanisms and ImplicationsFarid RakhmanNo ratings yet
- JCTH 7 154Document11 pagesJCTH 7 154Andreea AlexandruNo ratings yet
- Cancer-Associated Thrombosis: John Winters,, David GarciaDocument13 pagesCancer-Associated Thrombosis: John Winters,, David GarciaMichel CaballeroNo ratings yet
- Cancer CoagulationDocument7 pagesCancer CoagulationPPDSNeuroUnsri RSMHNo ratings yet
- CancerDocument3 pagesCancerEngr ShahzaibNo ratings yet
- Seminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerDocument14 pagesSeminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerJuan Camilo Morales TabordaNo ratings yet
- Trombocytopenia in CaDocument7 pagesTrombocytopenia in CaanisaNo ratings yet
- Mulatu Et Al 2020 Deep Venous Thrombosis Recurrence and Its Predictors at Selected Tertiary Hospitals in Ethiopia ADocument14 pagesMulatu Et Al 2020 Deep Venous Thrombosis Recurrence and Its Predictors at Selected Tertiary Hospitals in Ethiopia Amulatbirhanu100No ratings yet
- Debate - Thromboprophylaxis Should Be Considered in All Patients With Cancer - YesDocument3 pagesDebate - Thromboprophylaxis Should Be Considered in All Patients With Cancer - YesJosé Eduardo Cárdenas MendozaNo ratings yet
- The Mechanisms of Cancer-Associated Thrombosis: Anna Falanga, Marina Marchetti, Laura RussoDocument4 pagesThe Mechanisms of Cancer-Associated Thrombosis: Anna Falanga, Marina Marchetti, Laura RussoThomaz DamianiNo ratings yet
- Fichamento para Introduçao: Thromboembolism: A Public Health Concern. American Journal of Preventive Medicine, DefiniçãoDocument20 pagesFichamento para Introduçao: Thromboembolism: A Public Health Concern. American Journal of Preventive Medicine, Definiçãolarissam123No ratings yet
- Acuteleukemia: Hayley Rose-Inman,, Damon KuehlDocument18 pagesAcuteleukemia: Hayley Rose-Inman,, Damon KuehlJorge Tovar AvilaNo ratings yet
- ThromboDocument21 pagesThromboJayzel LaureanoNo ratings yet
- Biomolecules 12 00259Document14 pagesBiomolecules 12 00259Wilmar Leonardo Nieto RosasNo ratings yet
- Prevention of Venous Thromboembolism in Patients With CancerDocument12 pagesPrevention of Venous Thromboembolism in Patients With CancertheriversongsNo ratings yet
- Megan Wiese, MS, PA-C Naval Daver, MDDocument11 pagesMegan Wiese, MS, PA-C Naval Daver, MDFathiyya SalsabilaNo ratings yet
- Caso TEP Bibliografia Bis 2023Document7 pagesCaso TEP Bibliografia Bis 2023Viviana MorenoNo ratings yet
- Oncol Article JCRC 18Document9 pagesOncol Article JCRC 18EliDavidNo ratings yet
- TEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For ManagementDocument10 pagesTEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For Managementbenitez1228No ratings yet
- Portal Vein Thrombosis: ReviewDocument9 pagesPortal Vein Thrombosis: ReviewMahmoud AbouelsoudNo ratings yet
- Tom Asian 2015Document16 pagesTom Asian 2015p8crtgy9t5No ratings yet
- Blom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisDocument8 pagesBlom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisFarid RakhmanNo ratings yet
- Cerebral Venous Thrombosis From UptodateDocument20 pagesCerebral Venous Thrombosis From UptodatewbudyaNo ratings yet
- Platelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisDocument7 pagesPlatelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisEvan Nanda AdilistyaNo ratings yet
- Patogenesis, Diagnosis, Dan Penatalaksanaan Tromboemboli Vena Pada KankerDocument9 pagesPatogenesis, Diagnosis, Dan Penatalaksanaan Tromboemboli Vena Pada KankerHerlina ApriliaNo ratings yet
- Tromboprofilaxia para TEV Na CirroseDocument9 pagesTromboprofilaxia para TEV Na CirroseLeonardo FurtadoNo ratings yet
- Defining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsDocument7 pagesDefining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsZikry AuliaNo ratings yet
- Bloodbook 2017 660 PDFDocument7 pagesBloodbook 2017 660 PDFSambit DashNo ratings yet
- 234 FullDocument8 pages234 FullLaura Daniela MurilloNo ratings yet
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 pagesPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalNo ratings yet
- Deep Venous Thrombosis 2022. ANNALSDocument20 pagesDeep Venous Thrombosis 2022. ANNALSErnesto LainezNo ratings yet
- Winter 2006Document8 pagesWinter 2006dewiNo ratings yet
- European Guidelines On Perioperative Venous.5Document12 pagesEuropean Guidelines On Perioperative Venous.5ionut.andruscaNo ratings yet
- Acute Leukemia ThesisDocument8 pagesAcute Leukemia Thesisafcnftqep100% (2)
- Clinical Guide SEOM On Venous Thromboembolism in Cancer PatientsDocument12 pagesClinical Guide SEOM On Venous Thromboembolism in Cancer PatientsGaby ValenzuelaNo ratings yet
- Perspectives: Platelet Activation and Inhibition in Polycythemia Vera and Essential ThrombocythemiaDocument12 pagesPerspectives: Platelet Activation and Inhibition in Polycythemia Vera and Essential ThrombocythemiaJicko Street HooligansNo ratings yet
- Guideline Karsinoma HepatoselulerDocument11 pagesGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoNo ratings yet
- Radiotherapy-Associated Neutropenia and Thrombocytopenia: Analysis of Risk Factors and Development of A Predictive ModelDocument8 pagesRadiotherapy-Associated Neutropenia and Thrombocytopenia: Analysis of Risk Factors and Development of A Predictive ModelClaudiu PopescuNo ratings yet
- Cancer PDFDocument9 pagesCancer PDFMihaela IonescuNo ratings yet
- The Risk of Thrombosis in Patients With Acute Leukemia: Occurrence of Thrombosis at Diagnosis and During TreatmentDocument8 pagesThe Risk of Thrombosis in Patients With Acute Leukemia: Occurrence of Thrombosis at Diagnosis and During TreatmentArifah GulamanisNo ratings yet
- ITP ZakrzepicaDocument8 pagesITP ZakrzepicaMagdalena Górska-KosickaNo ratings yet
- Onco-Nephrology: Glomerular Diseases With Cancer: Jean-Franc Ois Cambier and Pierre RoncoDocument12 pagesOnco-Nephrology: Glomerular Diseases With Cancer: Jean-Franc Ois Cambier and Pierre RoncoGlauber LeitaoNo ratings yet
- Acute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHDocument8 pagesAcute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHd40sithuiNo ratings yet
- VTE TopicDocument9 pagesVTE Topicram7676No ratings yet
- Risk Stratification and Management of Intermediate-Risk Acute Pulmonary EmbolismDocument20 pagesRisk Stratification and Management of Intermediate-Risk Acute Pulmonary EmbolismLuis Javier Vera ZamoraNo ratings yet
- Cardiotoxicidad en Mieloma MultopleDocument10 pagesCardiotoxicidad en Mieloma MultopleJose Antonio Aguilar HidalgoNo ratings yet
- Jurnal Perdarahan Kanker 1Document9 pagesJurnal Perdarahan Kanker 1jefel umarNo ratings yet
- Ojim 2016091213324550Document10 pagesOjim 2016091213324550rianmg21No ratings yet
- Pages 4 7Document4 pagesPages 4 7andreas_251650No ratings yet
- Assessing Hypercoagulability and VTE Risk Using Thromboelastography and Khorana Score in Women With Cancers Receiving Chemotherapy 2024Document9 pagesAssessing Hypercoagulability and VTE Risk Using Thromboelastography and Khorana Score in Women With Cancers Receiving Chemotherapy 2024myqrwd464kNo ratings yet
- Acute Myeloid LeukemiaDocument11 pagesAcute Myeloid Leukemiafitra azraNo ratings yet
- Cancer and Liver Cirrhosis: Implications On Prognosis and ManagementDocument16 pagesCancer and Liver Cirrhosis: Implications On Prognosis and ManagementAlifia Ramadhanty PrameswariNo ratings yet
- Venous Thromboembolism in MalignancyDocument3 pagesVenous Thromboembolism in MalignancyAzmi FarhadiNo ratings yet
- Leunase and TrombolismDocument12 pagesLeunase and TrombolismSanta UlinaNo ratings yet
- Retinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionDocument4 pagesRetinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionmaryNo ratings yet
- Myelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentDocument11 pagesMyelodysplastic Syndromes: Diagnosis, Prognosis, and TreatmentTataNo ratings yet
- GastroprofilaxisDocument13 pagesGastroprofilaxisDaniel Alejandro Lecaros BarríaNo ratings yet
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsFrom EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsNo ratings yet
- Kadar Fibrinogen Sebagai Faktor Prognostik Pasien Perdarahan Intraserebral SpontanDocument5 pagesKadar Fibrinogen Sebagai Faktor Prognostik Pasien Perdarahan Intraserebral Spontanannisa edwarNo ratings yet
- Associations Between SeratoninDocument11 pagesAssociations Between Seratoninannisa edwarNo ratings yet
- EHMTI-0299. Serotonin As Biomarker of Ache Intensity in Chronic Tension HeadacheDocument1 pageEHMTI-0299. Serotonin As Biomarker of Ache Intensity in Chronic Tension Headacheannisa edwarNo ratings yet
- KDIGO BP Exec Summary FinalDocument11 pagesKDIGO BP Exec Summary Finalannisa edwarNo ratings yet
- Myofascial Trigger Points and Sensitization: An Updated Pain Model For Tension-Type HeadacheDocument11 pagesMyofascial Trigger Points and Sensitization: An Updated Pain Model For Tension-Type Headacheannisa edwarNo ratings yet
- Jnen 080 Sherifa Ahmad HamedDocument8 pagesJnen 080 Sherifa Ahmad Hamedannisa edwarNo ratings yet
- Routine Use of Vitamin K in The Treatment of Cirrhosis-Related Coagulopathy: Is It A-O-K? Maybe Not, We SayDocument6 pagesRoutine Use of Vitamin K in The Treatment of Cirrhosis-Related Coagulopathy: Is It A-O-K? Maybe Not, We Sayannisa edwarNo ratings yet
- Duty Dr. Iqbal - 1Document13 pagesDuty Dr. Iqbal - 1annisa edwarNo ratings yet
- Pathophysiological Mechanisms of Hepatic Encephalopathy: ReviewDocument5 pagesPathophysiological Mechanisms of Hepatic Encephalopathy: Reviewannisa edwarNo ratings yet
- Nurhayati, Female, 61 Yo, Neurology Ward: Chief Complaint: Present Illness HistoryDocument26 pagesNurhayati, Female, 61 Yo, Neurology Ward: Chief Complaint: Present Illness Historyannisa edwarNo ratings yet
- Firdaus Latif/Male/63 yo/MW 23: - Weakness and Fatigue Since 1 Month AgoDocument13 pagesFirdaus Latif/Male/63 yo/MW 23: - Weakness and Fatigue Since 1 Month Agoannisa edwarNo ratings yet
- Duration of Fasting During Acute Variceal BleedingDocument4 pagesDuration of Fasting During Acute Variceal Bleedingannisa edwarNo ratings yet
- Chronic Wound Managment HMIDocument37 pagesChronic Wound Managment HMIannisa edwarNo ratings yet
- Refit / Male / 24 Yo/ HCU 17: - Headache Increased Since 6 Hours AgoDocument14 pagesRefit / Male / 24 Yo/ HCU 17: - Headache Increased Since 6 Hours Agoannisa edwarNo ratings yet
- Asril Hepatoma (Autosaved)Document14 pagesAsril Hepatoma (Autosaved)annisa edwarNo ratings yet
- Menan - Dr. AnggitDocument19 pagesMenan - Dr. Anggitannisa edwarNo ratings yet
- Morning VidraDocument17 pagesMorning Vidraannisa edwarNo ratings yet
- Irwan/Male/ 42 Yo/ MW 17: Chief ComplaintDocument15 pagesIrwan/Male/ 42 Yo/ MW 17: Chief Complaintannisa edwarNo ratings yet
- Robert Georgy Ulimally/Male/51 YO/MW 21: Chief Complaint: Abdominal PainDocument14 pagesRobert Georgy Ulimally/Male/51 YO/MW 21: Chief Complaint: Abdominal Painannisa edwarNo ratings yet
- Morning AsriantiDocument15 pagesMorning Asriantiannisa edwarNo ratings yet
- Morning & Duty: 30 September 2021Document16 pagesMorning & Duty: 30 September 2021annisa edwarNo ratings yet
- Misnizar/female/46yo/FW 20: Chief Complaint: Fatigue and Weakness Since 3 Days AgoDocument13 pagesMisnizar/female/46yo/FW 20: Chief Complaint: Fatigue and Weakness Since 3 Days Agoannisa edwarNo ratings yet
- Morning Report 30-9Document15 pagesMorning Report 30-9annisa edwarNo ratings yet
- Guideline For Stress Ulcer Prophylaxis in The Intensive Care UnitDocument4 pagesGuideline For Stress Ulcer Prophylaxis in The Intensive Care Unitannisa edwarNo ratings yet
- Nursing Care Management of Patients With Anemia - 01Document38 pagesNursing Care Management of Patients With Anemia - 01Sionur 00No ratings yet
- FOLK MEDICINE ExtraDocument22 pagesFOLK MEDICINE ExtraPaul SavvyNo ratings yet
- Coronary Slow FlowDocument7 pagesCoronary Slow FlowradiomedicNo ratings yet
- Stock 8 Desember 2021Document102 pagesStock 8 Desember 2021Damaris Luisa DjadaNo ratings yet
- Ears Lecture GuideDocument56 pagesEars Lecture GuidemajNo ratings yet
- Statins and DiabetesDocument9 pagesStatins and DiabetesJonathan TorresNo ratings yet
- 2004, Vol.6, No.4, Pediatric Surgery PDFDocument95 pages2004, Vol.6, No.4, Pediatric Surgery PDFAnty Dewi Sarty RanyabarNo ratings yet
- History Taking HandbookDocument2 pagesHistory Taking Handbookyouservezeropurpose113No ratings yet
- NCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicDocument18 pagesNCM 116: Care of Clients With Problems in Nutrition and Gastrointestinal, Metabolism and Endocrine,, Acute and ChronicSIJINo ratings yet
- Pain Assessment - Worksheet - Advanced PDFDocument4 pagesPain Assessment - Worksheet - Advanced PDFsaran segah RohanNo ratings yet
- Dermatology MiniOSCE 2Document352 pagesDermatology MiniOSCE 2Gmail JONo ratings yet
- Knowledge, Awareness and Attitude Towards Organ Donation Among Undergraduate Medical Students of HaryanaDocument5 pagesKnowledge, Awareness and Attitude Towards Organ Donation Among Undergraduate Medical Students of HaryanaVinissha JeyarajNo ratings yet
- 74 Anaesthesia For Intestinal Obstruction in Children 1Document6 pages74 Anaesthesia For Intestinal Obstruction in Children 1Dr. Anish GolchhaNo ratings yet
- Discharge Instruction: Fitriani Pratiwi M.PDDocument13 pagesDischarge Instruction: Fitriani Pratiwi M.PDSaniaNo ratings yet
- Ecografo Aloka Modelo SSD-3500Document34 pagesEcografo Aloka Modelo SSD-3500EmilioPerezBallesterosNo ratings yet
- Mothers Knowledge and Practices of Minor IllnessesDocument17 pagesMothers Knowledge and Practices of Minor IllnessesSTANN KAZIPETNo ratings yet
- Unusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewDocument4 pagesUnusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewMirachel AugustNo ratings yet
- Documentation Dissection: New Patient Visit OafDocument3 pagesDocumentation Dissection: New Patient Visit OaftestNo ratings yet
- Effects of Computer AddictionDocument11 pagesEffects of Computer AddictionErich Trinidad33% (3)
- Daftar Harga Airway PT. Surgika 2017Document16 pagesDaftar Harga Airway PT. Surgika 2017Syaofi SofiNo ratings yet
- 2011 Fundchap9-Firesafety11-1Document19 pages2011 Fundchap9-Firesafety11-1api-272722550No ratings yet
- Postnatal Care PDF 66142082148037Document64 pagesPostnatal Care PDF 66142082148037veronia widayantiNo ratings yet
- Breaking Ground On ADHD Diagnosis in PakistanDocument1 pageBreaking Ground On ADHD Diagnosis in PakistanAnum Rizwan FazalNo ratings yet
- Drug Study Amoxicillin PDFDocument4 pagesDrug Study Amoxicillin PDFMc SantosNo ratings yet
- Symptoms of Ovarian CancerDocument3 pagesSymptoms of Ovarian Cancerwwe_jhoNo ratings yet
- Bartholin's Gland Cyst MarsupializationDocument3 pagesBartholin's Gland Cyst MarsupializationIndra JayaNo ratings yet
- PERCEPTION-COORDINATION-PRE-TEST RationalizationDocument11 pagesPERCEPTION-COORDINATION-PRE-TEST Rationalizationdrei yanNo ratings yet