Professional Documents
Culture Documents
Report 43: Quantifying The Impact of Vaccine Hesitancy in Prolonging The Need For Non-Pharmaceutical Interventions To Control The COVID-19 Pandemic
Report 43: Quantifying The Impact of Vaccine Hesitancy in Prolonging The Need For Non-Pharmaceutical Interventions To Control The COVID-19 Pandemic
Uploaded by
will1329Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Report 43: Quantifying The Impact of Vaccine Hesitancy in Prolonging The Need For Non-Pharmaceutical Interventions To Control The COVID-19 Pandemic
Report 43: Quantifying The Impact of Vaccine Hesitancy in Prolonging The Need For Non-Pharmaceutical Interventions To Control The COVID-19 Pandemic
Uploaded by
will1329Copyright:
Available Formats
24 March 2021 Imperial College COVID-19 response team
Report 43: Quantifying the impact of vaccine hesitancy in prolonging
the need for Non-Pharmaceutical Interventions to control the
COVID-19 pandemic
Daniela Olivera Mesa, Alexandra B Hogan, Oliver J Watson, Giovanni D Charles, Katharina Hauck, Azra
C Ghani, Peter Winskill1
WHO Collaborating Centre for Infectious Disease Modelling, MRC Centre for Global Infectious Disease
Analysis, Jameel Institute (J-IDEA), Imperial College London
1
Correspondence: Peter Winskill, p.winskill@imperial.ac.uk
Summary
Vaccine hesitancy – a delay in acceptance or refusal of vaccines despite availability – has the potential
to threaten the successful roll-out of SARS-CoV-2 vaccines globally. Here, we evaluate the potential
impact of vaccine hesitancy on the control of the pandemic and the relaxation of non-pharmaceutical
interventions (NPIs) by combining an epidemiological model of SARS-CoV-2 transmission with data on
vaccine hesitancy from population surveys. Our findings suggest that the mortality over a 2-year
period could be up to 8 times higher in countries with high vaccine hesitancy compared to an ideal
vaccination uptake if NPIs are relaxed. Alternatively, high vaccine hesitancy could prolong the need
for NPIs to remain in place. Addressing vaccine hesitancy with behavioural interventions is therefore
an important priority in the control of the COVID-19 pandemic.
SUGGESTED CITATION
D Olivera Mesa, AB Hogan, OJ Watson et al. Quantifying the impact of vaccine hesitancy in prolonging the need
for Non-Pharmaceutical Interventions to control the COVID-19 pandemic. Imperial College London (24-03-2021),
doi: https://doi.org/10.25561/87096.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives
4.0 International License.
DOI: https://doi.org/10.25561/87096 Page 1 of 13
24 March 2021 Imperial College COVID-19 response team
1. Introduction
The COVID-19 pandemic has simultaneously resulted in high global mortality and major economic
disruptions. As a control measure, non-pharmaceutical interventions (NPIs) such as social distancing
and mobility restrictions have been put in place worldwide and have successfully reduced
transmission of the virus. However, these interventions are unsustainable in the long-term (1) and
current hopes to control the pandemic rely heavily on vaccination.
In December 2020, the first vaccine against SARS-CoV-2 was approved; by March 2021, 12 vaccines
had been licensed (2) and more than 300 million vaccination doses administered worldwide (3). Their
reported efficacy against symptomatic disease ranges from 50% to over 95% (4-8). Given the high
basic reproduction number for SARS-CoV-2 (estimates range between 3-4)(1) high levels of vaccine
uptake will be required to achieve herd immunity (9), particularly if children are not vaccinated during
the first phase of roll-out.
One major concern that threatens to limit the impact of vaccination is vaccine hesitancy (10).
Population surveys have found that between 14% (11) and 27% (12) of adults say that they will not
accept a vaccine if available, whilst between 14%(11) and 19% (12) say that they are uncertain. There
is a large variation in vaccine hesitancy between countries , with the proportion saying that they
would get a SARS-Cov-2 vaccine if it became available, ranging from 40% for France (12) to 89% for
China (11). In many countries, vaccine hesitancy is heterogenous across sub-populations depending
on gender, age, ethnicity, religion, or socioeconomic status (11-13). The key drivers of SARS-CoV-2
vaccine hesitancy are related to concerns about the accelerated pace of vaccine development (13),
side-effects (12), and the spread of misinformation about the pandemic (10).
To understand the likely impact of vaccine hesitancy on future control of the pandemic, we use a
mathematical model of SARS-CoV-2 transmission (9) to explore vaccine hesitancy through its impact
on population coverage. We capture the effect of reduced coverage using three measured levels of
vaccine hesitancy based on self-reported intention to be vaccinated from recent behavioural survey
data (12). Low, medium, and high hesitancy levels result in optimistic, neutral and pessimistic
scenarios respectively. Hesitancy levels are further disaggregated by age-group to capture variation in
attitudes with respect to age. The hesitancy scenarios are compared to an ideal counterfactual
assuming no vaccine hesitancy, in which we assume that a small proportion (2%) of the population
will be ineligible to be vaccinated due to contraindications. We model each scenario with both a high
and a moderate vaccine efficacy profile that represents the range of efficacies of currently approved
vaccines. Informed by current vaccine roll-out in high-income countries, we assume that vaccination
started in January 2021 and is implemented at a rate that results in a total campaign of 10 months to
fully vaccinate the population above 15 years old, with no vaccine hesitancy (the duration of the
campaign is shorter in scenarios with vaccine hesitancy, due to assuming the same roll-out speed but
lower uptake).
DOI: https://doi.org/10.25561/87096 Page 2 of 13
24 March 2021 Imperial College COVID-19 response team
2. Results
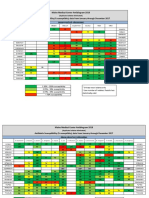
We first sought to determine the public health impact of vaccination and vaccine hesitancy as NPIs
are lifted. To do so, we allowed the time-varying reproductive number in the absence of immunity Rt,
to be increased in steps such that the effective reproductive number Reff, accounting for vaccine-
induced immunity, remains at the threshold value of 1 with the assumption of ideal vaccination uptake
(Figure 1 a, c). In this ideal scenario, NPIs can be fully lifted at the end of the vaccination period with
a high efficacy vaccine (94% efficacy, Figure 1a). However, with a moderate efficacy vaccine (63%
efficacy), some NPIs or other population-level behavioural changes may need to remain to control the
epidemic (Figure 1 c). In the presence of vaccine hesitancy, lifting NPIs and relying on vaccine-induced
immunity for control is predicted to lead to periodic outbreaks determined by the duration of naturally
induced immunity, with the outbreak size greater at higher levels of vaccine hesitancy (Figure 1 b, d).
For a high efficacy vaccine, even under the optimistic vaccine hesitancy scenario, daily deaths per
million at the peak of the first outbreak are projected to be 8.7 times higher than under the ideal
scenario (Figure 1b). This translates to a cumulative impact of 236 more deaths per million population
in the two years after vaccination begins. For a vaccine of moderate efficacy, in an optimistic vaccine
hesitancy scenario, the cumulative impact of vaccine hesitancy is projected to lead to 305 extra deaths
per million population over this period.
DOI: https://doi.org/10.25561/87096 Page 3 of 13
24 March 2021 Imperial College COVID-19 response team
24 March 2021 Imperial College COVID-19 response team
Figure 1. Projected COVID-19 dynamics for different vaccine hesitancy levels. Panels a-b show a high vaccine
efficacy (94% against infection, 98% against hospitalisation and death), panels c-d moderate vaccine efficacy
(63% against infection, 85% against hospitalisation and death). Panels a and c show the reproductive number Rt
profile, which represents the level of NPI stringency, with lower numbers indicating higher stringency. In this
illustrative example, we assume that a first wave of transmission occurred at the beginning of 2020 with an Rt
of 2.5. This was followed by NPIs leading to a reduction in Rt to 1, followed by an Rt of 1.5 as NPIs are lifted
leading to a second wave of transmission in the latter half of 2020. After vaccination is introduced at the
beginning of 2021, NPIs in all scenarios are lifted according to a schedule based on coverage under the ideal
scenario (no vaccine hesitancy, 98% of individuals 15 years plus are vaccinated). Panels b and d show projected
deaths per million under four vaccine hesitancy scenarios: Ideal (no hesitancy, black), optimistic (low hesitancy,
orange), neutral (medium hesitancy, purple), pessimistic (high hesitancy, blue). In each scenario, final
vaccination coverage per age group and deaths vary according to vaccine hesitancy. Dashed lines indicate the
vaccination rollout period in the ideal scenario.
DOI: https://doi.org/10.25561/87096 Page 4 of 13
24 March 2021 Imperial College COVID-19 response team
These adverse impacts of vaccine hesitancy on transmission, symptomatic disease, hospitalisations,
and deaths affect vaccinated as well as unvaccinated individuals because of imperfect vaccine efficacy
(Figure 2). Under the pessimistic scenario for vaccine hesitancy, the resulting lower vaccination
coverage is projected to lead to a 33% and 46% increase in hospitalisations in the vaccinated
population for the high and moderate vaccine efficacy profile, respectively, and a 18% and 46%
increase in deaths in the vaccinated population, compared to an ideal vaccination scenario (Figure 2).
Figure 2. Public health impact of vaccine hesitancy. High vaccine efficacy is shown on the left and moderate
vaccine efficacy on the right. The annotated numbers are the cumulative deaths a) and hospitalisations b) per
million individuals for the vaccinated and unvaccinated populations at the end of the projection horizon (1
January 2021 - 31 December 2022). Vaccination coverage of individuals aged 15 years and older is highest in
the ideal scenario at 98%, and lowest in the pessimistic scenario because of vaccine hesitancy.
As an alternative way to assess the impact of vaccine hesitancy on the pandemic, we evaluated the
degree to which other NPIs would need to remain in place given the real-time achieved vaccine
coverage in order to prevent further epidemics (i.e. keep Reff<1, Figure 3). For the high efficacy vaccine,
under the ideal scenario, we predict that NPIs could be fully lifted by the end of 2021 whilst keeping
transmission under control. However, even under the optimistic scenario with low vaccine hesitancy,
limited NPIs or other behavioural modifications might need to remain in place, with Rt having to
DOI: https://doi.org/10.25561/87096 Page 5 of 13
24 March 2021 Imperial College COVID-19 response team
remain below 2.4 to prevent further epidemics, 79% of the assumed R0 of 3. For the more pessimistic
scenarios of vaccine hesitancy, and for lower vaccine efficacy, these differences become more
pronounced. A difference of ~35% in the effective reproductive number could represent the closure
of educational institutions or limiting interaction between households to achieve control of the
epidemic (14); both of which are not sustainable or desirable.
Figure 3. Stringency of NPIs required to control the epidemic under different vaccine hesitancy scenarios.
Reproductive number profiles are estimated to keep R eff<1 such that epidemic impact is the same for each
scenario as in the ideal scenario. A lower reproductive number corresponds to more stringent NPIs. Continuous
lines represent profiles for a high efficacy vaccine and dashed lines represent profiles for a moderate efficacy
vaccine. The vertical dotted lines show the period of vaccination in the ideal scenario.
Our illustrative examples above are comparable to the waves of COVID-19 outbreaks in Europe.
However, vaccine hesitancy varies between countries (Figure 4a). To evaluate the impact of these
variations, we chose three European countries with different vaccine acceptance views: France,
Germany, and the United Kingdom (UK). For each country, we modelled the trajectory of the pandemic
under an ideal vaccination and a neutral vaccine hesitancy scenario. For a vaccine with high efficacy,
we project 1.3, 4.5 and 8.7 times more deaths in 2021/2022 in a scenario with hesitancy compared to
an ideal scenario in the UK, Germany and France respectively (Figure 4).
DOI: https://doi.org/10.25561/87096 Page 6 of 13
24 March 2021 Imperial College COVID-19 response team
Figure 4. Impact of vaccine hesitancy for three European countries. a) Reported vaccine acceptance per age group in France, Germany and the United Kingdom reproduced
from Jones et al.(12). b) Cumulative death ratios per age group compared to the ideal vaccine uptake scenario, by country and vaccine efficacy profile. The ratio compares
cumulative deaths projected over a two-year period after vaccination starts for two scenarios: An ideal scenario, where 98% of the population older than 15 years gets
vaccinated and a vaccine hesitancy scenario, where coverage for people over 15 years old is based on vaccine acceptance from a). SARS-CoV-2 dynamics were fitted for each
country for 2020, simulations were generated for a vaccination campaign starting Jan 2021 and lasting 10 months.
DOI: https://doi.org/10.25561/87096 Page 7 of 13
24 March 2021 Imperial College COVID-19 response team
3. Discussion
Our findings show the considerable impact of vaccine hesitancy, detailing the considerable mortality
that could be averted with increased vaccine coverage. However, our analysis necessarily makes many
simplifying assumptions, and it is important to note that the future trajectory of the epidemic will
depend on the complex interactions between vaccination uptake, behaviour, and government
interventions. First, we have assumed homogenous mixing between vaccine hesitant individuals.
However, as has been seen for other diseases, COVID-19 vaccine hesitancy is heterogenous and
clustered within population subgroups (15). Transmission is more likely to be sustained within clusters
with low vaccine coverage (16, 17) and therefore future outbreaks may be limited to these sub-
populations. Secondly, self-reported attitudes to COVID-19 vaccines are changing over time (11, 12)
and levels may improve as confidence grows in the vaccination programmes. Thirdly, we do not
account for immune escape from the vaccine due to new variants arising. Whilst second generation
vaccines will likely become available to address this issue, it is currently unclear whether some of the
high levels of vaccine uptake observed in early vaccine roll-outs would be sustained in subsequent
booster programmes.
Getting vaccinated is an individual choice, but these individual choices have population wide effects
that are likely to challenge current efforts to control COVID-19. Our findings suggest that vaccine
hesitancy may have a substantial impact on the pandemic trajectory, deaths, and hospitalization. To
prevent such adverse outcomes, NPIs would need to stay in place longer, or possibly indefinitely,
resulting in high economic and social costs (18, 19). Reducing vaccine hesitancy is therefore an
important public health priority. Interventions that aim to build trust, for example with community-
based public education or via positive role-models, are proven efficacious approaches to address
hesitancy (20). There is an ongoing debate about vaccine passports as a condition to travel, or a
vaccination requirement for employees (21). Such interventions may be effective because they
incentivize individuals to get vaccinated, but they are controversial in libertarian democracies because
they curtail personal freedom and individual choice about medical treatments. The alternative will be
to accept some level of disease, hospitalisation and deaths given the level of vaccine coverage
achieved whilst allowing NPIs to be lifted, given that NPIs are not a sustainable long-term method for
control.
DOI: https://doi.org/10.25561/87096 Page 8 of 13
24 March 2021 Imperial College COVID-19 response team
4. Methods
4.1 Vaccine hesitancy data
Attitudes towards COVID-19 vaccination were obtained from the Imperial College London YouGov
Covid 19 Behaviour Tracker Data(12). This data set includes weekly surveys about people’s behaviours
in response to COVID-19 (including vaccines) as well as standard demographic questions on age,
gender, and household structure.
We extracted the survey results from February 8th - February 15th , 2021 for 10 European countries.
To assess vaccine hesitancy, we used data from one question pertaining to COVID-19 vaccine
acceptance in which participants were asked to what extent they would definitely get a COVID-19
vaccine, if it became available to them next week. Answers were obtained on a numeric scale ranging
from “Strongly agree -– 1” to “Strongly disagree – 5”. We grouped survey results into 5-year age
groups and categorised three vaccine acceptance levels for each group - high, middle, and low vaccine
hesitancy - where vaccine acceptance was the proportion of individuals whose answers were “1”, “1
or 2” and “1,2 or 3” respectively.
4.2 Mathematical model
We used a previously developed mathematical model for SARS-CoV-2 transmission and vaccination
(9). The age-structured deterministic SEIR-type compartmental model incorporates an age specific
probability of infection determined by age-based contact matrices as well as the disease clinical
pathway, which includes hospitalisation, oxygen support and intensive care needs. Vaccination is
modelled as an additional dimension disaggregating the population into those who have not received
the vaccine, have received the vaccine but are not yet protected, have received the vaccine and are
protected and those who have received the vaccine but are no-longer protected (if vaccine-derived
immunity is not life-long). In this model only those who are currently infected do not receive the
vaccine. Protection due to vaccination is modelled at two stages in the model; 1) reducing the
probability of infection upon exposure (efficacy against infection) and 2) reducing the probability of
hospitalisation being indicated after developing disease (efficacy against hospitalisation and death).
Parameters for SARS-CoV-2 infection, health care capacity, age-distribution and contact patterns are
based on previous work (9, 22) . Vaccine induced immunity was assumed lifelong, while natural
immunity was assumed to last for an average of one year (23). To produce simulations representing
the different vaccines approved to date, each scenario was run for two vaccines: one with high efficacy
(94% efficacy against infection(4)) and one with moderate efficacy (63% efficacy against infection(5)).
For both vaccines we assume an additional 60% efficacy against hospitalisation for breakthrough
infections, resulting in an overall vaccine efficacy against hospitalisation and death of 98% for the high
efficacy vaccine and 85% for the moderate efficacy vaccine. A summary of key parameters is given in
Table S1. The model code is freely available at https://github.com/mrc-ide/nimue.
To mimic current vaccine rollout plans, vaccination is introduced in the population at the beginning of
January 2021. We assumed that only individuals aged 15 years and above are vaccinated and that
vaccination occurs at a constant rate that results in 98% of the adult population and hence 80% of the
population being vaccinated after ten months under the ideal vaccine hesitancy scenario. For other
vaccine hesitancy scenarios, we implement the same rate of vaccination (given that this is constrained
DOI: https://doi.org/10.25561/87096 Page 9 of 13
24 March 2021 Imperial College COVID-19 response team
not by vaccine uptake but by the supply and delivery of vaccines) such that the final lower level of
coverage is achieved earlier than ten months. Vaccines are allocated prioritising older age groups
first: with 80+ years vaccinated first and then sequentially including additional age groups in 5-year
age-bands down to 15-19 years.
4.3 Simulations
To simulate a representative pre-vaccination scenario, we generated a scenario in which Rt was 2.5
up to April 2020, subsequently decreased to 1 to represent the impact of NPIs against the first wave,
and then rose to 1.5 during the latter half of 2020 to represent a second wave. Following the
introduction of vaccination in January 2021, we set Rt to increase in 5 fixed steps. The time for each
step increase was determined by estimating when vaccination coverage had reached levels such that
the effective reproduction number in the presence of vaccination was one (Reff=1). This coverage was
estimated based on the following equation:
1
𝐶𝑜𝑣𝑒𝑟𝑎𝑔𝑒 ∗ 𝑒𝑓𝑓𝑖𝑐𝑎𝑐𝑦 = 1 −
𝑅𝑡
At the end of the vaccination period, Rt remained at a value such that the effective reproduction
number continued at the threshold value of 1, taking into account final vaccination coverage and
vaccine efficacy.
We consider four potential scenarios for vaccine coverage per age group:
1) Ideal: 98% coverage for all age groups 15+.
2) Optimistic: Final coverage per age group is given by vaccine acceptance from the low vaccine
hesitancy level.
3) Neutral: Final coverage per age group is given by vaccine acceptance from the middle vaccine
hesitancy level.
4) Pessimistic: Final coverage per age group is given by vaccine acceptance from the high vaccine
hesitancy level.
When analysing the impact of lifting NPIs, the Rt profile following the introduction of vaccination was
generated based on an ideal scenario for vaccination uptake. Conversely, when evaluating the degree
to which NPIs would need to remain in place, the Rt profile after the introduction of vaccination was
set up based on each one of the vaccine coverage scenarios described above.
Simulations for the representative scenario were run using a U.K representative contact matrix
(https://github.com/sbfnk/socialmixr) and epidemics were seeded at the end February 2020 with 20
cases. As an output for each simulation, we estimated the number of deaths and hospitalisations
associated with COVID-19 over the two-year period from 1 January 2021 to 31 December 2022.
To generate country specific simulations, we parameterise the model with data on the population size
and age distribution of the country (https://population.un.org/wpp/) and representative contact
matrices obtained from a systematic review of social contact surveys through the socialmixR package
(https://github.com/sbfnk/socialmixr) . The model was then fitted to reported daily cases and deaths
DOI: https://doi.org/10.25561/87096 Page 10 of 13
24 March 2021 Imperial College COVID-19 response team
up to December 31st, 2020 by varying three parameters - the start date of the epidemic, the initial R0
and the effect size of changes in mobility on transmission (using mobility data from Google
(https://www.google.com/covid19/mobility )). Model fitting was performed using a Metropolis
Hastings MCMC based sampling scheme as previously described(24). The resulting fit generates an Rt
trajectory up to the introduction vaccination in January 2021, after which, Rt was set to increase by
10 fixed steps, up to the theoretical herd immunity threshold based on an ideal vaccination schedule
(as described above). The pandemic trajectory was evaluated for two scenarios: An ideal scenario and
a neutral vaccine hesitancy scenario (as described above), using country specific data on vaccine
hesitancy and demography.
5. Data availability
All data used in this study are from publicly accessible sources and the results generated are available
from the corresponding author on reasonable request.
6. Acknowledgements
All authors acknowledge funding from the MRC Centre for Global Infectious Disease Analysis
(reference MR/R015600/1), jointly funded by the UK Medical Research Council (MRC) and the UK
Foreign, Commonwealth & Development Office (FCDO), under the MRC/FCDO Concordat agreement
and is also part of the EDCTP2 programme supported by the European Union. KH acknowledges
funding by Community Jameel. PW and ABH acknowledge funding from the Imperial College Research
Fellowship scheme. ACG, DOM and GDC acknowledge funding from The Wellcome Trust (no.
215143/Z/18/Z to DOM).
DOI: https://doi.org/10.25561/87096 Page 11 of 13
24 March 2021 Imperial College COVID-19 response team
7. References
1. Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, et al. Estimating the effects
of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257-61.
2. LSHTM Vaccine Centre. COVID-19 vaccine tracker 2021 [updated 16 February 2021. Available
from: https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/#.
3. Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, et al. Coronavirus
(COVID-19) Vaccinations Our World in Data 2021 [updated 17 February 2021. Available from:
https://ourworldindata.org/covid-vaccinations#.
4. Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and Efficacy of
the BNT162b2 mRNA Covid-19 Vaccine. New England Journal of Medicine. 2020;383(27):2603-15.
5. Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy
of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four
randomised controlled trials in Brazil, South Africa, and the UK. The Lancet. 2021;397(10269):99-111.
6. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and Safety of the
mRNA-1273 SARS-CoV-2 Vaccine. New England Journal of Medicine. 2020;384(5):403-16.
7. Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS,
et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19
vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia. The Lancet.
8. Sinovac Biotech Ltd. Sinovac Announces Phase III Results of Its COVID-19 Vaccine. 2021.
9. Hogan AB, Winskill P, Watson OJ, Walker PGT, Whittaker C, Baguelin M, et al. Report 33:
Modelling the allocation and impact of a COVID-19 vaccine. Imperial College London; 2020 September
25
10. Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-
19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour. 2021.
11. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of
potential acceptance of a COVID-19 vaccine. Nature Medicine. 2021;27(2):225-8.
12. Jones SP, Imperial College London, YouGov Plc. Imperial College London YouGov Covid Data
Hub. YouGov Plc; 2020.
13. Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, et al. COVID-19 vaccine
hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II.
Psychological Medicine. 2020:1-15.
14. Brauner JM, Mindermann S, Sharma M, Johnston D, Salvatier J, Gavenčiak T, et al. Inferring
the effectiveness of government interventions against COVID-19. Science. 2021;371(6531):eabd9338.
15. de Figueiredo A. Sub-national forecasts of COVID-19 vaccine acceptance across the UK: a
large-scale cross-sectional spatial modelling study. medRxiv2020.
16. Truelove SA, Graham M, Moss WJ, Metcalf CJE, Ferrari MJ, Lessler J. Characterizing the impact
of spatial clustering of susceptibility for measles elimination. Vaccine. 2019;37(5):732-41.
17. Salathé M, Bonhoeffer S. The effect of opinion clustering on disease outbreaks. Journal of the
Royal Society, Interface. 2008;5(29):1505-8.
18. Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic
implications of the coronavirus pandemic (COVID-19): A review. International journal of surgery
(London, England). 2020;78:185-93.
19. Mandel A, Veetil V. The Economic Cost of COVID Lockdowns: An Out-of-Equilibrium Analysis.
Economics of Disasters and Climate Change. 2020;4(3):431-51.
20. Vergara RJD, Sarmiento PJD, Lagman JDN. Building public trust: a response to COVID-19
vaccine hesitancy predicament. Journal of Public Health. 2021.
21. Brown RCH, Kelly D, Wilkinson D, Savulescu J. The scientific and ethical feasibility of immunity
passports. The Lancet Infectious Diseases. 2021;21(3):e58-e63.
DOI: https://doi.org/10.25561/87096 Page 12 of 13
24 March 2021 Imperial College COVID-19 response team
22. Walker PGT, Whittaker C, Watson OJ, Baguelin M, Winskill P, Hamlet A, et al. The impact of
COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science.
2020;369(6502):413-22.
23. Hall V, Foulkes S, Charlett A, Atti A, Monk E, Simmons R, et al. Do antibody positive healthcare
workers have lower SARS-CoV-2 infection rates than antibody negative healthcare workers? Large
multi-centre prospective cohort study (the SIREN study), England: June to November 2020. medRxiv.
2021:2021.01.13.21249642.
24. Watson OJ, Alhaffar M, Mehchy Z, Whittaker C, Akil Z, Imperial College COVID-19 Response
Team, et al. Report 31: Estimating the burden of COVID-19 in Damascus, Syria: an analysis of novel
data sources to infer mortality under-ascertainment Imperial College London; 2020 15 September.
DOI: https://doi.org/10.25561/87096 Page 13 of 13
You might also like
- Increases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesDocument4 pagesIncreases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesKyle Becker95% (19)
- HIV Awareness Survey QuestionnaireDocument3 pagesHIV Awareness Survey QuestionnaireSean Patrick Razo0% (1)
- Dynamic Optimization of COVID-19 Vaccine PrioritizDocument27 pagesDynamic Optimization of COVID-19 Vaccine PrioritizCristian Fernando Sanabria BautistaNo ratings yet
- Vaccination and NPIsDocument10 pagesVaccination and NPIsPaulos ZelekeNo ratings yet
- Modelling of COVID-19 Vaccination Strategies and Herd ImmunityDocument8 pagesModelling of COVID-19 Vaccination Strategies and Herd ImmunitydewiNo ratings yet
- Bosetti Et Al - Epidemio in Partially Vaccinated Pop - 2021.06.28-Text and SupplementDocument39 pagesBosetti Et Al - Epidemio in Partially Vaccinated Pop - 2021.06.28-Text and SupplementCaterina MariniNo ratings yet
- Mathematical Modelling of COVID-19 Transmission and Mitigation Strategies in The Population of Ontario, CanadaDocument9 pagesMathematical Modelling of COVID-19 Transmission and Mitigation Strategies in The Population of Ontario, CanadaGuillermo Rodriguez LopezNo ratings yet
- Ijerph 18 07491Document10 pagesIjerph 18 07491Corneliu PaschanuNo ratings yet
- 1 s2.0 S0264410X23000348 MainDocument12 pages1 s2.0 S0264410X23000348 MainJose Luis Isazañ JoseNo ratings yet
- Vaccinate With Confidence and Finish StrongDocument4 pagesVaccinate With Confidence and Finish StrongBillNo ratings yet
- The Lancet Regional Health - Europe: Hermann BrennerDocument2 pagesThe Lancet Regional Health - Europe: Hermann BrennerRahmanu ReztaputraNo ratings yet
- Vaccine Surveillance Report - Week 37 v2Document33 pagesVaccine Surveillance Report - Week 37 v2Abby EscorzaNo ratings yet
- Summary of Guidance For Minimizing The Impact of COVID-19 On Individual Persons, Communities, and Health Care Systems - United States, August 2022Document8 pagesSummary of Guidance For Minimizing The Impact of COVID-19 On Individual Persons, Communities, and Health Care Systems - United States, August 2022PANAMA GREEN BUILDING COUNCILNo ratings yet
- Deb PDocument19 pagesDeb PJean M Huaman FiallegaNo ratings yet
- COVID Vaccine Hesitancy Around WorldDocument15 pagesCOVID Vaccine Hesitancy Around WorldMohd ZahiNo ratings yet
- PIIS0140673621015890Document2 pagesPIIS0140673621015890Anastasija LevcenkoNo ratings yet
- CEA COVID-19 Vaccine in ColombiaDocument10 pagesCEA COVID-19 Vaccine in Colombiaangel.paternina423No ratings yet
- Eabf1374 FullDocument12 pagesEabf1374 FullNiatazya Mumtaz SagitaNo ratings yet
- Cost Utility of Vaccination Against COVID-19 in BrazilDocument8 pagesCost Utility of Vaccination Against COVID-19 in BrazilTatiana DutraNo ratings yet
- Group 3 PR2Document21 pagesGroup 3 PR2jaxxNo ratings yet
- Vaccine: Michele Kohli, Michael Maschio, Debbie Becker, Milton C. WeinsteinDocument8 pagesVaccine: Michele Kohli, Michael Maschio, Debbie Becker, Milton C. Weinsteinfareha riazNo ratings yet
- Covid ImpactDocument9 pagesCovid ImpactAlejandro Gabriel ArancibiaNo ratings yet
- Hesitancy Towards A COVID-19 Vaccine and Prospects For Herd ImmunityDocument51 pagesHesitancy Towards A COVID-19 Vaccine and Prospects For Herd ImmunityA009Karin Kurniati NurfatmahNo ratings yet
- Worldwide Bayesian Causal Impact Analysis of Vaccine Administration On Deaths and Cases Associated With Covid-19: A Bigdata Analysis of 145 CountriesDocument65 pagesWorldwide Bayesian Causal Impact Analysis of Vaccine Administration On Deaths and Cases Associated With Covid-19: A Bigdata Analysis of 145 CountriesendrioNo ratings yet
- UK Vaccine Surveillance Report Week 42Document29 pagesUK Vaccine Surveillance Report Week 42Cam SlaterNo ratings yet
- Concepts in Disaster MedicineDocument8 pagesConcepts in Disaster MedicinedaniaNo ratings yet
- 2021 PSL CovidDocument10 pages2021 PSL CovidRalph Gerard SangalangNo ratings yet
- Imperial College COVID19 NPI Modelling 16-03-2020Document20 pagesImperial College COVID19 NPI Modelling 16-03-2020Zerohedge100% (11)
- 1 s2.0 S1755436524000240 MainDocument10 pages1 s2.0 S1755436524000240 Main7fkqx7zh7pNo ratings yet
- Controlo Da Pandemia em Portugal Na Fase Da VacinaçãoDocument15 pagesControlo Da Pandemia em Portugal Na Fase Da VacinaçãopedromelaoNo ratings yet
- Fimmu 13 782198Document11 pagesFimmu 13 782198Suryati HusinNo ratings yet
- The Journal of Infectious DiseasesDocument19 pagesThe Journal of Infectious DiseasesmagfirahNo ratings yet
- Julianromero Whitepaperpt7Document13 pagesJulianromero Whitepaperpt7api-527610130No ratings yet
- Government 211016 134210Document27 pagesGovernment 211016 134210KemNo ratings yet
- Modelling To Support A Future Covid 19 StrategyDocument9 pagesModelling To Support A Future Covid 19 StrategyKeith LynchNo ratings yet
- Preprint Modelling of COVID-19 Vaccination Strategies and Herd Immunity, in Scenarios of Limited and Full Vaccine SupplyDocument29 pagesPreprint Modelling of COVID-19 Vaccination Strategies and Herd Immunity, in Scenarios of Limited and Full Vaccine SupplyArifin SiregarNo ratings yet
- Honors 221 Essay 2 FinalDocument6 pagesHonors 221 Essay 2 Finalapi-487217658No ratings yet
- The Lancet Advierte A Gobiernos y Asesores Porqué Ahora La Fase 4 Es Más Importante Que La Fase 3Document3 pagesThe Lancet Advierte A Gobiernos y Asesores Porqué Ahora La Fase 4 Es Más Importante Que La Fase 3Urgente24No ratings yet
- Topic11 VaccinationIDocument14 pagesTopic11 VaccinationIHelen LugoNo ratings yet
- Vaccine: SciencedirectDocument10 pagesVaccine: SciencedirectNenqx Inthandt C'bunqxzu TheaNo ratings yet
- Perkiraan COVID-19 Infections, Hospitalizations, and DeathsDocument4 pagesPerkiraan COVID-19 Infections, Hospitalizations, and Deathsabdullatif503No ratings yet
- The Effect of The COVID-19 Vaccine On Daily Cases and Deaths Based On Global Vaccine DataDocument12 pagesThe Effect of The COVID-19 Vaccine On Daily Cases and Deaths Based On Global Vaccine DataCorneliu PaschanuNo ratings yet
- MainDocument9 pagesMainSURYONONo ratings yet
- Comment: The Lancet Infectious Diseases, Frank Sandmann andDocument2 pagesComment: The Lancet Infectious Diseases, Frank Sandmann andAbdón Guerra FariasNo ratings yet
- Analysis of The Potential Impact of Durability Timing and Transmission Blocking of COVID19 Vaccine On Morbidity and mortalityEClinicalMedicine PDFDocument14 pagesAnalysis of The Potential Impact of Durability Timing and Transmission Blocking of COVID19 Vaccine On Morbidity and mortalityEClinicalMedicine PDFAnang SetiawanNo ratings yet
- White Paper - Effective-Covid19-Control-through-carrier-tracking-and-non-pharmaceutical-interventions-v2.0-2Document45 pagesWhite Paper - Effective-Covid19-Control-through-carrier-tracking-and-non-pharmaceutical-interventions-v2.0-2Daniel SloanNo ratings yet
- Running Head: Benefits of The Covid-19 Vaccine 1Document7 pagesRunning Head: Benefits of The Covid-19 Vaccine 1bonnieNo ratings yet
- Hesitancy in co-WPS OfficeDocument6 pagesHesitancy in co-WPS OfficeNorhani PanayamanNo ratings yet
- SceirdDocument9 pagesSceirdGiaWay HsuNo ratings yet
- Estimation of Vaccine Efficacy and Critical Vaccination Coverage in Partially Observed OutbreaksDocument9 pagesEstimation of Vaccine Efficacy and Critical Vaccination Coverage in Partially Observed OutbreaksAri SiswadiNo ratings yet
- Covid 19 Transmission Vaccinated CasesDocument9 pagesCovid 19 Transmission Vaccinated CasesrNo ratings yet
- MeaslesDocument4 pagesMeaslesChetan SharmaNo ratings yet
- COVID-19 Vaccine and Guillain-Barré Syndrome: Let's Not Leap To AssociationsDocument10 pagesCOVID-19 Vaccine and Guillain-Barré Syndrome: Let's Not Leap To AssociationsAsok DattaNo ratings yet
- COVID-19 Vaccine Surveillance Report: Week 2Document55 pagesCOVID-19 Vaccine Surveillance Report: Week 2Kosta GavrasNo ratings yet
- Coronavirus: Arm Yourself With Facts: Symptoms, Modes of Transmission, Prevention & TreatmentFrom EverandCoronavirus: Arm Yourself With Facts: Symptoms, Modes of Transmission, Prevention & TreatmentRating: 5 out of 5 stars5/5 (1)
- Infectious Diseases in Solid-Organ Transplant Recipients: A practical approachFrom EverandInfectious Diseases in Solid-Organ Transplant Recipients: A practical approachOriol ManuelNo ratings yet
- Beyond One Health: From Recognition to ResultsFrom EverandBeyond One Health: From Recognition to ResultsJohn A. HerrmannNo ratings yet
- Everything You Should Know About the Coronavirus: How it Spreads, Symptoms, Prevention & Treatment, What to Do if You are Sick, Travel InformationFrom EverandEverything You Should Know About the Coronavirus: How it Spreads, Symptoms, Prevention & Treatment, What to Do if You are Sick, Travel InformationNo ratings yet
- Evaluation of Stability of Directly Standardized Rates For Sparse Data Using Simulation MethodsDocument9 pagesEvaluation of Stability of Directly Standardized Rates For Sparse Data Using Simulation Methodswill1329No ratings yet
- PHDS Guidance - AggregationDocument22 pagesPHDS Guidance - Aggregationwill1329No ratings yet
- PHDS Guidance - Assigning Deprivation CategoriesDocument7 pagesPHDS Guidance - Assigning Deprivation Categorieswill1329No ratings yet
- Comparators Briefing - TechnicalDocument6 pagesComparators Briefing - Technicalwill1329No ratings yet
- PHDS Guidance - Confidence IntervalsDocument15 pagesPHDS Guidance - Confidence Intervalswill1329No ratings yet
- Comparators Briefing - OverviewDocument2 pagesComparators Briefing - Overviewwill1329No ratings yet
- 2021 10 06 COVID19 Report 46 SupplementDocument58 pages2021 10 06 COVID19 Report 46 Supplementwill1329No ratings yet
- Report 44: Recent Trends in Sars-Cov-2 Variants of Concern in EnglandDocument36 pagesReport 44: Recent Trends in Sars-Cov-2 Variants of Concern in Englandwill1329No ratings yet
- Figures and Tables Report 46: Factors Driving Exten Sive Spatial A ND T Emporal FL Uctuations in COV ID 19 Fat Ality Rat Es in Brazilian HospitalsDocument45 pagesFigures and Tables Report 46: Factors Driving Exten Sive Spatial A ND T Emporal FL Uctuations in COV ID 19 Fat Ality Rat Es in Brazilian Hospitalswill1329No ratings yet
- Report 46: Factors Driving Extensive Spatial and Temporal Fluctuations in COVID 19 Fatality Rates in Brazilian HospitalsDocument20 pagesReport 46: Factors Driving Extensive Spatial and Temporal Fluctuations in COVID 19 Fatality Rates in Brazilian Hospitalswill1329No ratings yet
- ER TUnited-Kingdom 2021-10-09Document3 pagesER TUnited-Kingdom 2021-10-09will1329No ratings yet
- Fungal Infections - InfestationsDocument48 pagesFungal Infections - InfestationsMoayad NawaflehNo ratings yet
- Chapter 1-Introduction To CholeraDocument28 pagesChapter 1-Introduction To CholeraWako MiesaNo ratings yet
- Daftar Penyakit Kompetensi 4ADocument12 pagesDaftar Penyakit Kompetensi 4ARoy Sandy PermanaNo ratings yet
- Apollo Blood Donation CardDocument3 pagesApollo Blood Donation Cardlovebhardwaj13No ratings yet
- Common Zoonotic Diseases Affecting Pets and People: Kristen Hammett, DVMDocument22 pagesCommon Zoonotic Diseases Affecting Pets and People: Kristen Hammett, DVMSandrea SalazarNo ratings yet
- J Clin Virol 2020Document4 pagesJ Clin Virol 2020Alejandro Jiménez BlasNo ratings yet
- NGO News Digest NESWSLETTER Issue No. 26-1Document14 pagesNGO News Digest NESWSLETTER Issue No. 26-1tafadzwa123No ratings yet
- Worm InfestationDocument1 pageWorm InfestationMRS CHAKRAPANINo ratings yet
- Balanopostitis and Penyle Edema Atypical Manifestation of Primary SipilisDocument2 pagesBalanopostitis and Penyle Edema Atypical Manifestation of Primary SipilisTeja LaksanaNo ratings yet
- Hse Bulletin: Cold & FluDocument2 pagesHse Bulletin: Cold & FluRanjan PradhanNo ratings yet
- K Park 24 TH Edition ChangesDocument8 pagesK Park 24 TH Edition ChangesAnkit ChoudharyNo ratings yet
- Infection and Response - KnowITDocument64 pagesInfection and Response - KnowITdawud khanNo ratings yet
- Microbiology and ParasitologyDocument5 pagesMicrobiology and ParasitologyChester Riogelon100% (2)
- Rubella IgG 1301Z-WebDocument6 pagesRubella IgG 1301Z-WebvolvoproNo ratings yet
- 2018 MMC AntibiogramDocument2 pages2018 MMC Antibiogramaman570570No ratings yet
- BrochureDocument7 pagesBrochuretanjir.22110205No ratings yet
- Lassa FeverDocument2 pagesLassa FeverDauda Muize AdewaleNo ratings yet
- Case Study of LeptospirosisDocument4 pagesCase Study of Leptospirosisbuzz Q75% (4)
- Revathi Papsmear ProcedureDocument50 pagesRevathi Papsmear ProcedureRevathi DadamNo ratings yet
- March, To It Now Being The Vast Majority of Our Sequenced CasesDocument6 pagesMarch, To It Now Being The Vast Majority of Our Sequenced Cases01 LudviaNo ratings yet
- Lesson Plan On Typhoid FeverDocument39 pagesLesson Plan On Typhoid FeverValarmathi100% (7)
- Concepts of Infection ControlDocument53 pagesConcepts of Infection ControlBimal Dey100% (1)
- Identifying and Investigating OutbreaksDocument74 pagesIdentifying and Investigating OutbreaksCesarNo ratings yet
- Registration-No.I1690002157557311866-REGISTRATION SYSTEM FOR MOVEMENT TO UTTARAKHAND STATEDocument2 pagesRegistration-No.I1690002157557311866-REGISTRATION SYSTEM FOR MOVEMENT TO UTTARAKHAND STATEsidharth bajajNo ratings yet
- Part I Travel Documents Issued by Third Countries and Territorial Entities en 0Document124 pagesPart I Travel Documents Issued by Third Countries and Territorial Entities en 0drlazyboyNo ratings yet
- ISAK Insider 01Document2 pagesISAK Insider 01Satoe TohiNo ratings yet
- IMUNISASIDocument26 pagesIMUNISASINadia KhoiriyahNo ratings yet
- Meningitis - Introduction and ManagementDocument27 pagesMeningitis - Introduction and ManagementAmmo KhanNo ratings yet
- Bowel Isolation Technique Power PointDocument14 pagesBowel Isolation Technique Power PointMichael LesterNo ratings yet