Professional Documents
Culture Documents
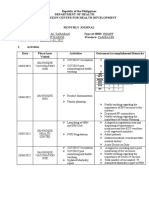
Schedule
Schedule
Uploaded by
Yogini GholapOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Schedule
Schedule
Uploaded by
Yogini GholapCopyright:
Available Formats
Schedule
General
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
BCG
Database ID 84_8 Year 2006
Since 1974, BCG vaccination has been included in the WHO Expanded Programme on Immunization (EPI)
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 31
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
Database ID 71_4 Year 2005
The regularly-reviewed EPI policy recommendation for BCG is to continue the use of the vaccine as it prevents severe TB in some, but not all children who have been
immunized. There should be no BCG booster doses. Should countries, based on cost-effectiveness considerations, decide to discontinue the use of BCG, WHO
recommends applying the criteria defined by the International Union against Tuberculosis and Lung Disease (IUATLD). The criteria essentially refer to the requirement
for an efficient case-notification system against a background of very low national prevalence figures for all forms of TB.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 27-29 October 2004 WHO/IVB/05.03 Page 24
14 February 2008 Page 1 of 59
Schedule
Database ID 1_14 Year 2004
Immunization of infants with Bacille Calmette-Guérin vaccine (BCG) can protect against TB meningitis and other severe forms of TB in children less than five years
old. BCG vaccine is not recommended after 12 months of age because the protection provided is variable and less certain.
The recommended method of prevention for children who are younger than 12 months old is to immunize them as soon after birth as possible with BCG vaccine.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 23
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
Database ID 6_13 Year 2004
If the infant does not have a scar and you cannot determine whether a dose of BCG has been given, immunize the infant with BCG vaccine.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 6: Holding an immunization session WHO/IVB/04.06 Page 10
Database ID 50_1 Year 2004
Unfortunately, the (BCG) vaccine does not fully meet the essential requirement of having a significant impact against the most common manifestation of TB, namely
pulmonary disease. Despite the shortcomings of this vaccine, WHO continues to recommend that a single dose of BCG be given to neonates or as soon as possible after
birth in countries with a high prevalence of TB.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 37, 38
Database ID 50_2 Year 2004
Since severe adverse effects of BCG vaccination are extremely rare even in asymptomatic, HIV-positive infants, all healthy neonates should be BCG-vaccinated, even
in areas endemic for HIV. However, where resources permit, long-term follow-up of BCG-vaccinated infants of known HIV-positive mothers is desirable for early
treatment, should disseminated BCG disease occur in children with rapid development of immunodeficiency.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 28
14 February 2008 Page 2 of 59
Schedule
Database ID 50_4 Year 2004
In cases where infants have been exposed to smear-positive pulmonary TB shortly after birth, BCG vaccination should be delayed until completion of 6 months of
prophylactic isoniazid treatment.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 28
Database ID 50_5 Year 2004
Countries with a low burden of TB may choose to limit BCG vaccination to neonates and infants of recognized high-risk groups for the disease or to skin-testnegative
older children. In some low-burden populations, BCG vaccination has been largely replaced by intensified case detection and supervised early treatment.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 28
Database ID 50_7 Year 2004
There is no proven benefit of repeated BCG vaccination against TB. This also applies to revaccination of BCG-vaccinated individuals who remain negative by
subsequent tuberculin testing.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 28 &
34
Database ID 50_11 Year 2004
In the absence of a scar in children in high-burden countries, BCG vaccination is indicated.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 34
Database ID 50_12 Year 2004
In low-burden countries, good protection against primary TB may also be achieved following vaccination of skin-test-negative adults. BCG vaccination of skin-
testpositive individuals, whether induced by environmental mycobacteria, Mtb or BCG does not improve immunity to TB.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 36
14 February 2008 Page 3 of 59
Schedule
Database ID 50_13 Year 2004
BCG vaccination is indicated
– for all infants living in areas where TB is highly endemic (concerning HIV, see below);
– for infants and children at particular risk of TB exposure in otherwise low-endemic areas;
– for persons exposed to multidrug-resistant Mtb (impact not established.)
BCG vaccination is contraindicated
– for persons with impaired immunity (symptomatic HIV infection, known or suspected congenital immunodeficiency, leukaemia, lymphoma or generalized malignant
disease);
– for patients under immunosupressive treatment (corticosteroids, alkylating agents, antimetabolites, radiation);
– in pregnancy.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 36
Database ID 50_15 Year 2004
Given the high risk of acquiring TB and the low risk of serious adverse events following BCG vaccination of HIV-exposed neonates, WHO maintains that, in HIV-
infected areas, all neonates be given BCG. Older infants or children suspected of being HIV-infected should not be vaccinated if they have symptomatic disease or
other evidence of immunosuppression.
BCG vaccine (WHO position paper) Weekly Epid. Record (2004, 79: 27-38) Page 38
Database ID 79_5 Year 2004
There are few population-based data on the effectiveness, or otherwise, of BCG vaccine in preventing severe tuberculosis in HIV-positive infants. Given the high
prevalence of HIV and tuberculosis in certain countries and of the current development of new tuberculosis vaccines, some of which are based on BCG, GACVS
advises no change in the current recommendations for BCG immunization of infants in countries with a high prevalence of tuberculosis and that population-based
studies should be undertaken to determine the efficacy and safety of BCG and related vaccines in HIV-negative and HIV-positive children in countries with a high
endemic rate of tuberculosis.
Global Advisory Committee on Vaccine Safety, 3–4 December 2003 Weekly Epid. Record (2004, 79: 16-20) Page 19
14 February 2008 Page 4 of 59
Schedule
Database ID 74_10 Year 2002
SAGE strongly endorses the continued used of BCG in national immunization services as a means of minimizing the harmful effects of tuberculosis infection in the first
year of life. SAGE recommends that the vaccine be used until there is an alternative improved anti-tuberculosis vaccine. In the meantime, national immunization
services are encouraged to maintain the highest possible coverage of infants.
SAGE reinforces WHO’s recommendation that no booster dose of BCG be given, as there is no evidence that booster doses are efficacious.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 14-15 June 2001 (WHO/V&B/02.07) Page 32
Cholera
Database ID 84_1 Year 2006
Although the whole-cell injectable vaccine (against cholera) is no longer recommended, it still is commercially available in some countries.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 4
Database ID 84_2 Year 2006
Since 1999, WHO recommends the use of killed oral WC/rBS vaccine as a tool to prevent cholera in populations at risk of a cholera epidemic. Such high-risk
populations may include, but are not limited to, refugees and urban slum residents.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 5
Database ID 84_4 Year 2006
The Ty21a (typhoind) vaccine is . . . to be swallowed every other day for one week. It can be taken simultaneously with the attenuated CVD103-HgR V. cholerae
vaccine.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 13
14 February 2008 Page 5 of 59
Schedule
Diptheria
Database ID 52_4 Year 2006
(A)ccording to WHO requirements, the potency of diphtheria vaccine used for the immunization of children shall be no less than 30 IU per single human dose. Vaccines
of lower potency are used for immunization of children aged =7 years and adults. This reduction of diphtheria toxoid potency minimizes reactogenicity at the injection
site but is still sufficient to provoke an antibody response in older children and adults.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 28
Database ID 52_6 Year 2006
The recommended schedule for vaccination against diphtheria varies considerably between countries. According to the WHO/EPI schedule, the primary series of
DTwP- or DTaP-containing vaccines should be administered in 3 doses, starting as early as 6 weeks of age and given with a minimum interval of 4 weeks. Where
resources permit, additional doses can be given after the completion of the primary series. Many national immunization programmes offer 1-2 booster doses, for
example one at 2 years of age and a second at age 4-7 years.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 29
Database ID 52_7 Year 2006
For previously un-immunized children aged 1-7 years, the recommended schedule (for diphtheria vaccine) is 2 doses 2 months apart, and a third dose after 6-12 months
using DTwP or DTaP. The recommended schedule for primary immunizations of older children, adolescents and adults using the dT combination is 2 doses -months
apart and a third dose after 6-12 months. People living in low-endemic or non-endemic areas should receive booster doses of DT approximately 10 years after
completing the primary series and subsequently every 10 years throughout life. Special attention should be paid to immunizing health-care workers who may have
occupational exposure to C. diphtheriae. Booster responses can still be elicited after intervals of 25-30 years, so repeat primary immunization is not required when
boosters are delayed.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 29
14 February 2008 Page 6 of 59
Schedule
Database ID 52_8 Year 2006
Unfortunately, diphtheria infection does not always confer protective immunity. Individuals recovering from the disease should therefore complete active immunization
with diphtheria toxoid during convalescence.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 29
Database ID 52_10 Year 2006
To compensate for the loss of natural boosting, industrialized countries should add childhood boosters of diphtheria toxoid to the primary immunization series of
infancy. The optimal timing for and the number of such booster doses should be based on epidemiological surveillance as well as on immunological and programmatic
considerations. Boosting at the age of 12 months, at school entry and just before leaving school are all possible options. In addition to these childhood immunizations,
people living in low-endemic or non-endemic areas may require booster injections of diphtheria toxoid at about 10-year intervals to maintain life-long protection.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 31
Database ID 52_11 Year 2006
To further promote immunity against diphtheria, diphtheria toxoid and tetanus toxoid rather than tetanus toxoid alone should be used when tetanus prophylaxis is
needed following injuries.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 25
Database ID 82_13 Year 2006
In accordance with the recommendations in the previous position paper on diphtheria, use of diphtheria–tetanus vaccine is preferable to single-antigen tetanus toxoid
vaccine. In future, the inclusion of other antigens, e.g. pertussis or Haemophilus influenzae type b (Hib), in booster doses should be considered.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
Database ID 83_1 Year 2006
Vaccines containing DT are used for children aged <7 years and dT-containing vaccines for individuals aged ≥7 years.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 198
14 February 2008 Page 7 of 59
Schedule
Database ID 83_2 Year 2006
As a rule, vaccine combinations containing diphtheria toxoid (D or d) and tetanus toxoid, rather than tetanus toxoid alone, should be used when immunization against
tetanus is indicated.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 198
Database ID 83_12 Year 2006
Both TT and dT can be used at any time during pregnancy.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 204
Database ID 83_18 Year 2006
See Appendix 83_18 for a summary table of immunizations with diphtheria–tetanus–pertussis (DTP) and diphtheria toxoid (Td) vaccines required to obtain long-term
protectiona against tetanus
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 207
Database ID 1_10 Year 2004
Immunizing infants and children with DTP or DT and adults with Td prevents tetanus.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 20
Database ID 2_7 Year 2004
Because it contains high levels of diphtheria toxoid, (DT) should not be given to children older than six years old or adults.
Td, or tetanus-diphtheria toxoids adult dose vaccine, is the same vaccine as DT, but with a lower diphtheria toxoid dose. It is suitable for children older than six years
old and adults, including pregnant women.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 12
14 February 2008 Page 8 of 59
Schedule
DPT
Database ID 52_6 Year 2006
The recommended schedule for vaccination against diphtheria varies considerably between countries. According to the WHO/EPI schedule, the primary series of
DTwP- or DTaP-containing vaccines should be administered in 3 doses, starting as early as 6 weeks of age and given with a minimum interval of 4 weeks. Where
resources permit, additional doses can be given after the completion of the primary series. Many national immunization programmes offer 1-2 booster doses, for
example one at 2 years of age and a second at age 4-7 years.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 29
Database ID 52_7 Year 2006
For previously un-immunized children aged 1-7 years, the recommended schedule (for diphtheria vaccine) is 2 doses 2 months apart, and a third dose after 6-12 months
using DTwP or DTaP. The recommended schedule for primary immunizations of older children, adolescents and adults using the dT combination is 2 doses -months
apart and a third dose after 6-12 months. People living in low-endemic or non-endemic areas should receive booster doses of DT approximately 10 years after
completing the primary series and subsequently every 10 years throughout life. Special attention should be paid to immunizing health-care workers who may have
occupational exposure to C. diphtheriae. Booster responses can still be elicited after intervals of 25-30 years, so repeat primary immunization is not required when
boosters are delayed.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 29
Database ID 83_18 Year 2006
See Appendix 83_18 for a summary table of immunizations with diphtheria–tetanus–pertussis (DTP) and diphtheria toxoid (Td) vaccines required to obtain long-term
protectiona against tetanus
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 207
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
14 February 2008 Page 9 of 59
Schedule
Database ID 61_2 Year 2005
In countries where the incidence of pertussis has been considerably reduced by successful immunization, a booster dose administered 1–6 years after the primary series
is warranted. The optimal timing of this booster dose as well as the possible need for additional booster doses of DTP depends on the epidemiological situation, and
should be assessed by individual national programmes.
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 31
Database ID 61_7 Year 2005
The main aim of pertussis vaccination is to reduce the risk of severe pertussis in infancy. The vaccine is usually administered in the national childhood immunization
programme as combined DTwP or DTaP vaccine, although the combination often includes additional vaccines (Haemophilus influenzae type b (Hib), hepatitis B
(HepB), poliovirus vaccine (IPV)). The optimal schedule and number of immunizations are not well defined but, in most countries, 3 primary doses are administered
with at least a 1-month interval to infants aged 2–6 months. A booster dose is commonly offered 1–6 years later. WHO recommends the primary series to be
administered at the age of 6, 10 and 14 weeks. National recommendations vary considerably, however.
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 35
Database ID 1_10 Year 2004
Immunizing infants and children with DTP or DT and adults with Td prevents tetanus.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 20
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
Database ID 2_28 Year 2004
Wait at least four weeks between doses of OPV, DTP, Hib, and HepB vaccines.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 25
14 February 2008 Page 10 of 59
Schedule
Hepatitis A
Database ID 54_1 Year 2000
Currently, four inactivated vaccines against HAV are internationally available. All four vaccines are safe and effective, with long-lasting protection. None of the
vaccines are licensed for children less than one year of age.
The (HAV) vaccines are given parenterally, as a two-dose series, 6-18 months apart. The dose of vaccine, vaccination schedule, ages for which the vaccine is licensed,
and whether there is a paediatric and adult formulation varies from manufacturer to manufacturer.
Hepatitis A vaccines (WHO position paper ) Weekly Epid. Record (2000, 75: 38-44) Page 38 &
41
Database ID 54_9 Year 2000
In developed countries with low endemicity of hepatitis A and with high rates of disease in specific high-risk populations, vaccination of those populations against
hepatitis A may be recommended. The high-risk groups include injection-drug users, homosexual men, persons travelling to high-risk areas, and certain ethnic or
religious groups. However, it should be noted that vaccination programmes targeting specific high-risk groups may have little impact on the overall national incidence
of disease.
Hepatitis A vaccines (WHO position paper ) Weekly Epid. Record (2000, 75: 38-44) Page 43
Hepatitis B
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
14 February 2008 Page 11 of 59
Schedule
Database ID 39_26 Year 2005
(Considerations for hepatitis B vaccine schedule:)
• A determination of the role of perinatal transmission (useful for birth dose considerations) can be made based on the overall seroprevalance of HBsAg, age-specific
prevalence of HBsAg, and the prevalence of the HBeAg in pregnant women.
• Combination products may not be used at birth; therefore, programmes including the birth dose will need to include monovalent HepB vaccine in the supply.
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 45
Database ID 1_15 Year 2004
It is recommended that all infants receive three doses of hepatitis B vaccine during the first year of life. More recently, some countries have been using a combination
vaccine that includes vaccines for diphtheria, tetanus, pertussis, hepatitis B (hepB), and sometimes Haemophilus inflenzae type b (Hib). Programmatically, it is usually
easiest if the three doses of hepatitis B vaccine are given at the same time as the three doses of DTP. In countries where hepatitis B is highly endemic, where feasible, a
birth dose of hepB is included in the schedule to prevent perinatal hepatitis B infection.
Some countries also recommend immunizing adolescents, health workers and other risk groups.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 25
Database ID 2_11 Year 2004
Only monovalent HepB vaccine should be used as a birth dose, the dose given within the first week of life. Combination vaccines should not be used at birth, but may
be used in subsequent doses.
Do not use DTP-HepB+Hib as a birth dose. You may use the vaccine for subsequent doses.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 16 &
20
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
14 February 2008 Page 12 of 59
Schedule
Database ID 2_28 Year 2004
Wait at least four weeks between doses of OPV, DTP, Hib, and HepB vaccines.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 25
Database ID 2_35 Year 2004
Options for adding hepatitis B vaccine to childhood immunization schedules (Appendix 2_35.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 16
Database ID 55_2 Year 2004
(I)n countries where a high proportion of HBV infections are acquired perinatally, the first dose of hepatitis B vaccine should be given as soon as possible (<24 hours)
after birth.
In countries where a lower proportion of HBV infections are acquired perinatally, the relative contribution of perinatal HBV infection to the overall disease burden, and
the feasibility and cost-effectiveness of providing vaccination at birth, should be carefully considered before a decision is made on the optimal vaccination schedule.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 255
Database ID 55_4 Year 2004
(Hepatitis B vaccine catch-up) strategies targeted at older age groups or groups with risk factors for acquiring HBV infection should be considered as a supplement to
routine infant vaccination in countries of intermediate or low hepatitis B endemicity. In such settings, a substantial proportion of the disease burden may be attributable
to infections acquired by older children, adolescents and adults.
In countries of high endemicity, large-scale routine vaccination of infants rapidly reduces the transmission of HBV. In these circumstances, catch-up vaccination of
older children and adults has relatively little impact on chronic disease because most of them have already been infected.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 255
14 February 2008 Page 13 of 59
Schedule
Database ID 55_5 Year 2004
In highly endemic areas, HBV is most commonly spread from mother to child at birth, or from person to person in early childhood. In countries with low HBV
endemicity, sexual transmission and the use of contaminated needles, especially among injecting drug users, are the major routes of infection. However, perinatal
transmission may account for 15% of HBV-related deaths, even in low-endemic areas.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 257
Database ID 55_7 Year 2004
When immunizing against HBV at birth, only monovalent hepatitis B vaccine should be used: the other antigens found in combination vaccines are currently not
approved for use at birth (DTwP, DTaP, Hib, hepatitis A and IPV.)
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 258
Database ID 55_8 Year 2004
The minimum recommended interval between (hepatitis B vaccine) doses is four weeks. Longer dose intervals may increase the final anti-HBs titres but not the
seroconversion rates.
More than 3 doses of the vaccine are not required, regardless of duration (> 4 weeks) of the interval between them.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 259
Database ID 55_9 Year 2004
Recommended schedules for (hepatitis B) vaccination can be divided into those that include a birth-dose and those that do not. Schedules with a birth-dose call for the
first vaccination at birth, followed by a second and third dose at the time of the first and third diphtheria/tetanus/pertussis (DTP) vaccination, respectively (see Appendix
55_9, column II.) Alternatively, a four-dose schedule may be used where the dose at birth is followed by three additional doses; these doses may be given either as
monovalent vaccine or as a combination (e.g. with DTP and/or Hib) following the schedules commonly used for those vaccines (see Appendix 55_9, column III.) These
schedules will prevent most perinatally acquired infection.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 259
14 February 2008 Page 14 of 59
Schedule
Database ID 55_10 Year 2004
Some countries have chosen not to implement universal (hepatitis B) immunization and instead use comprehensive HBsAg screening of pregnant women with
immunization of newborn infants born to HBsAg-positive women. This strategy is usually not feasible in developing countries with high prevalence of disease and may
not be the most reliable and convenient option even in countries where HBsAg screening in pregnancy is well established.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 259
Database ID 55_11 Year 2004
When administered without the birth-dose, hepatitis B vaccine is usually given at the same time as DTP, either as a monovalent presentation or in combination with
DTP and/or Hib vaccine (see Appendix 55_9, column I) .
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 259
Database ID 55_12 Year 2004
Countries that opt for schedules with a birth-dose (of hepatitis B vaccine) should vaccinate preterm infants at birth and subsequently enter the respective national
hepatitis B vaccination schedule. However, if the birth weight is <2000 g, the vaccine dose at birth should not be counted towards the primary series, and three
additional doses should be given.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 260
Database ID 55_13 Year 2004
Immunocompromised children and adults can also benefit from vaccination (with hepatitis B vaccine.) However, the immune response may be reduced and additional
injections of the vaccine may be required. Where possible, the anti-HBs antibody titres should be followed up after immunization of immunocompromised individuals.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 260
14 February 2008 Page 15 of 59
Schedule
Database ID 55_17 Year 2004
All children and adolescents aged less than 18 years and not previously vaccinated should receive the (hepatitis B) vaccine. Hepatitis B vaccination is also indicated for
certain groups at high risk of contracting HBV infection, including persons with high-risk sexual behaviour, partners and household contacts of HBsAg-positive
persons, injecting drug users, persons who frequently require blood or blood products, recipients of solid organ transplantation, those at occupational risk of HBV
infection, including health care workers, as well as for international travellers to HBV-endemic countries.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 261
Database ID 55_19 Year 2004
Temporary immunity may be obtained using hepatitis B immune globulin (HBIG) for post-exposure prophylaxis.
HBIG prophylaxis may be indicated (i) for newborn infants whose mothers are HBsAg-positive, (ii) following percutaneous or mucous membrane exposure to HBsAg-
positive blood or body fluids, (iii) following sexual exposure to an HBsAg-positive person, and (iv) to protect patients from recurrent HBV infection following liver
transplantation. As a rule, HBIG should be used as an adjunct to hepatitis B vaccine. However, in full-term newborns, the protection against perinatally acquired
infection achieved by immediate (<24 hours) hepatitis B vaccination is not significantly improved by the addition of HBIG.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 261
Database ID 55_20 Year 2004
In countries of high disease endemicity (HBsAg prevalence >8%), HBV is mainly spread from mother to infant at birth or from child to child during early childhood (<5
years). In this epidemiological setting, schedules providing the first vaccine dose at birth are recommended.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 262
Database ID 55_21 Year 2004
Routine infant hepatitis B vaccination should also be given high priority in countries of intermediate or low HBV endemicity (HBsAg prevalence of >2-<8% or <2%,
respectively) because, even in these settings, an important proportion of chronic infections are acquired through HBV transmission during early childhood.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 262
14 February 2008 Page 16 of 59
Schedule
Database ID 55_22 Year 2004
Although HBsAg screening of all pregnant women and vaccination at birth only of infants born to HBsAg-positive mothers may be an option in areas with low HBV
transmission, this strategy may be only partially effective, since women at highest risk of infection often fail to attend prenatal clinics.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 262
Database ID 55_24 Year 2004
Catch-up vaccination (with hepatitis B vaccine of older age groups, including adolescents and adults) should be considered only if the continuity of the infant
vaccination programme can be ensured.
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 263
Database ID 73_2 Year 2003
WHO policy on hepatitis B vaccine: that it should be integrated into national immunization programmes in all countries, with target groups and strategies varying
according to the local epidemiology. For carrier prevalence equal to or greater than 2%, WHO recommended routine infant immunization and for countries with lower
carrier prevalence, immunization of adolescents could be considered as an addition or alternative to infant immunization.
(Page 25): For those countries with national hepatitis B immunization programmes that do not include immunization of infants, SAGE urges them to assess the
additional burden of hepatitis B disease that could be prevented if they were to implement an infant immunization programme as well.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 14–15 June 2002 WHO/V&B/03.06 Page 23
Database ID 20_2 Year 2001
Prevention of perinatal HBV transmission should be considered depending on the epidemiology of HBV transmission in a particular country.
In order to prevent HBV transmission from mother to infant, the first dose of HepB vaccine needs to be given as soon as possible after birth (preferably within 24
hours). In countries where a high proportion of chronic infections is acquired perinatally (e.g. South-East Asia), a birth dose should be given to infants. It is usually most
feasible to give HepB vaccine at birth when infants are born in hospitals. Efforts should also be made in these countries to give HepB vaccine as soon as possible after
delivery to infants delivered at home. In countries where a lower proportion of chronic infections is acquired perinatally (e.g. Africa), the highest priority is to achieve
high DTP3 and HepB3 vaccine coverage among infants. In these countries, use of a birth dose may also be considered after disease burden, cost-effectiveness, and
feasibility are evaluated.
Introducing hepatitis B vaccine into national immunization services WHO/V&B/01.28 Page 1
14 February 2008 Page 17 of 59
Schedule
Database ID 20_3 Year 2001
Catch up vaccination of older persons should be considered depending on the epidemiology of HBV transmission in a particular country. (Note: The Vaccine Fund
does not provide vaccine for catch-up immunization).
In countries with a high endemicity of chronic HBV infection (hepatitis B surface antigen [HBsAg] prevalence >8%), catch-up immunization is not usually
recommended because most chronic infections are acquired among children <5 years of age, and thus, routine infant vaccination will rapidly reduce HBV transmission.
In countries with lower endemicity of chronic HBV infection, a higher proportion of chronic infections may be acquired among older children, adolescents and adults;
catch-up immunization for these groups may be considered.
Introducing hepatitis B vaccine into national immunization services WHO/V&B/01.28 Page 2
Database ID 20_4 Year 2001
Monovalent HepB vaccines must be used to give the birth dose of HepB vaccine.
Combination vaccines that include HepB vaccine must not be used to give the birth dose of HepB vaccine because DTP and Hib vaccines are not recommended to be
given at birth.
Combination vaccines can be given whenever all of the antigens in the vaccine are indicated.
Introducing hepatitis B vaccine into national immunization services WHO/V&B/01.28 Page 2
Database ID 20_5 Year 2001
HepB vaccine schedules are very flexible; thus, there are multiple options for adding the vaccine to existing national immunization schedules without requiring
additional visits for immunization. (See Appendix 20_5.)
Programmatically, it is usually easiest if the 3 doses of HepB vaccine are given at the same time as the 3 doses of DTP (Option I). This schedule will prevent infections
acquired during early childhood, which account for most of the HBV-related disease burden in high endemic countries, and also will prevent infections acquired later in
life. However, this schedule will not prevent perinatal HBV infections because it does not include a dose of HepB vaccine at birth. Two schedule options can be used to
prevent perinatal HBV infections: a 3-dose schedule of monovalent HepB vaccine, with the 1st dose given at birth and the 2nd and 3rd doses given at the same time as
the 1st and 3rd doses of DTP vaccine (Option II); or a 4-dose schedule in which a birth dose of monovalent HepB vaccine is followed by 3 doses of a combination
vaccine, e.g. DTP HepB (Option III).
The 3-dose schedule (Option II) is less expensive, but may be more complicated to administer, because infants receive different vaccines at the 2nd immunization visit
than at the 1st and 3rd visits. The 4-dose schedule (Option III) may be easier to administer programmatically, but is more costly, and vaccine supply issues may make it
unfeasible.
Introducing hepatitis B vaccine into national immunization services WHO/V&B/01.28 Page 2
14 February 2008 Page 18 of 59
Schedule
Database ID 36_1 Year 2001
In order to prevent perinatal HBV transmission the first dose of hepatitis B vaccine should be given as soon as possible after birth, preferably within 24 hours.
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 6
s and parents
Database ID 36_2 Year 2001
• In all countries: Achieving a high level of completion of the hepatitis B vaccine series among all infants should be the highest priority. This has the greatest overall
impact on the prevalence of chronic HBV infection in children, regardless of whether it is feasible to administer a birth dose.
• In countries where a high proportion of chronic HBV infections is acquired perinatally (e.g. in south-east Asia): A birth dose should be given to infants who are
delivered in hospitals when hepatitis B vaccine is introduced. Efforts should also be made in these countries to give hepatitis B vaccine as soon as possible after birth to
infants delivered at home.
• In countries where a lower proportion of chronic HBV infections is acquired perinatally (e.g. in Africa): The administration of a birth dose may be considered after
evaluating:
- the relative contribution of perinatal HBV infections to the overall disease burden;
- the feasibility and cost-effectiveness of providing a birth dose.
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 7
s and parents
Database ID 36_3 Year 2001
Monovalent hepatitis B vaccine MUST BE USED for the birth dose.
· Combination vaccines that include hepatitis B vaccine MUST NOT BE USED to give the birth dose of hepatitis B vaccine because DTP and Hib vaccines should not
be administered at birth.
· Either monovalent hepatitis B vaccine or combination vaccines may be used for later doses in the hepatitis B vaccine schedule. Combination vaccines can be given
whenever all the antigens in the vaccines are indicated.
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 9
s and parents
14 February 2008 Page 19 of 59
Schedule
Database ID 36_7 Year 2001
All infants aged under 1 year should receive a full series of hepatitis B vaccine. The need for catch-up immunization of older age groups and for targeted risk groups
varies between countries.
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 12
s and parents
Database ID 36_9 Year 2001
Programmatically, it is usually easiest if the three doses of hepatitis B vaccine are given at the same time as the three doses of DTP (See Appendix 36_9 for options for
adding hepatitis B vaccine to childhood immunization schedules.)
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 13
s and parents
HIB
Database ID 82_13 Year 2006
In accordance with the recommendations in the previous position paper on diphtheria, use of diphtheria–tetanus vaccine is preferable to single-antigen tetanus toxoid
vaccine. In future, the inclusion of other antigens, e.g. pertussis or Haemophilus influenzae type b (Hib), in booster doses should be considered.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
14 February 2008 Page 20 of 59
Schedule
Database ID 2_28 Year 2004
Wait at least four weeks between doses of OPV, DTP, Hib, and HepB vaccines.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 25
Database ID 21_5 Year 2001
Combination vaccines that contain Hib conjugate vaccine:
• can be used anytime all of the antigens in the vaccine are indicated by the schedule;
• cannot be used before 6 weeks of age (e.g. for the birth dose of hepatitis B vaccine) because the immunogenicity of the DTP and Hib components will be reduced if
given before this age.
Introducing Haemophilus influenzae type b (Hib) conjugate vaccine into national immunization services WHO/V&B/01.29 Page 2
Database ID 21_6 Year 2001
Immunization of infants with Hib conjugate vaccine is usually accomplished by giving the vaccine at the same ages as DTP vaccine, either as a separate injection or in
combination.
In general, infants should receive a primary dose schedule of 3 doses of Hib conjugate vaccine in the first year of life. Doses of Hib conjugate vaccine should be
administered at least 4 weeks apart.
Children older than one year of age require only a single dose of Hib conjugate vaccine.
Introducing Haemophilus influenzae type b (Hib) conjugate vaccine into national immunization services WHO/V&B/01.29 Page 2
Database ID 21_7 Year 2001
Booster doses of Hib conjugate vaccine may be given to children in the second year of life, but successful control of Hib disease does not require a booster dose.
Introducing Haemophilus influenzae type b (Hib) conjugate vaccine into national immunization services WHO/V&B/01.29 Page 2
Database ID 15_3 Year 2000
Hib vaccine is indicated in children from the age of 6 weeks up to 18 months.
Introduction of Haemophilus influenzae type b vaccine into immunization programmes WHO/V&B/00.05 Page 5
14 February 2008 Page 21 of 59
Schedule
Database ID 15_5 Year 2000
In general, the scheduling practices below are followed for Hib immunization:
- The first dose is given to children at six weeks of age or older.
- Three doses are given. Most Hib vaccines require three doses, and in the remainder of this document, a three-dose primary series will be considered routine. One
conjugate is licensed for a two-dose primary series, but is not marketed widely.
Introduction of Haemophilus influenzae type b vaccine into immunization programmes WHO/V&B/00.05 Page 6
Database ID 15_11 Year 2000
In most countries, the primary series of Hib immunizations protect children through their most susceptible period and thus, in general, a booster is not needed. Although
boosters may be considered when Hib disease is a substantial problem for children older than 12 months, some countries do not use booster doses even under these
circumstances because of the increased cost and administrative complexity.
Introduction of Haemophilus influenzae type b vaccine into immunization programmes WHO/V&B/00.05 Page 10
Influenza
Database ID 84_6 Year 2006
A trivalent live cold-adapted vaccine (Flumist) has been developed for intra-nasal spray delivery . . .
The vaccine has been licensed in the USA for vaccination of persons from 5-49 years of age, in view of side effects in younger children (wheezing, nasal congestion)
and absence of data in the elderly. The vaccine is safe, effective, and shows remarkable genetic stability, but it has to be kept at -18°C.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 18
14 February 2008 Page 22 of 59
Schedule
Database ID 56_1 Year 2005
Based on data from industrialized countries, and listed in order of priority, the following groups of individuals may be targeted for vaccination (against influenza) in
order to reduce the incidence of severe illness and premature death.
1. Residents of long-term care facilities for elderly people and the disabled.
2. Elderly non-institutionalized individuals with chronic conditions such as pulmonary and cardiovascular illness, metabolic diseases including diabetes mellitus and
renal dysfunction, and various types of immunosuppression, including people with acquired immunodeficiency syndrome (AIDS) and transplant recipients.
3. All adults and children aged >6 months with any of the conditions mentioned above.
4. Elderly individuals who are above a nationally defined age limit, irrespective of other risk factors. Although the appropriate age for general vaccination may be
considerably lower in countries with poor living conditions, most countries define the age limit to be >65 years.
5. Other groups defined on the basis of national data and capacities, such as contacts of high-risk people, pregnant women, health-care workers and others with key
functions in society, as well as children 6-23 months of age.
Influenza vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 279-287) Page 286
Database ID 56_8 Year 2005
In terms of protective efficacy, the live influenza vaccines appear to be comparable with the TIVs (trivalent, inactivated influenza vaccines.) However, CAIV-T (cold-
adapted influenza vaccine) is licensed only for healthy people aged 5-49 years, given reports of an increase in reactive airway disease in vaccinees <5 years of age and
insufficiently documented protective efficacy in older people.
Influenza vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 279-287) Page 285
14 February 2008 Page 23 of 59
Schedule
JE
Database ID 88_2 Year 2006
The most effective immunization strategy in JE endemic settings is a one time campaign in the primary target population, as defined by local epidemiological data,
followed by incorporation of the JE vaccine into the routine immunization programme. This approach has a greater public health impact than either strategy separately
(page 331.)
The most effective immunization strategy in JE-endemic settings is one time catch-up campaigns including child health weeks or multi-antigen campaigns in the locally-
defined primary target population, followed by incorporation of the JE vaccine into the routine immunization programme. This approach has a greater public health
impact than either strategy separately (page 339.)
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 331&3
WHO Position Paper 39
Database ID 88_3 Year 2006
Both the mouse-brain derived and the cell culture-based vaccines are considered efficacious and to have an acceptable safety profile for use in children. However, with
the mouse-brain derived vaccine, rare cases of potentially fatal acute disseminated encephalomyelitis (ADEM) and hypersensitivity reactions have been reported among
vaccinated children in endemic regions and in travellers from nonendemic locations. Because of the rarity of these adverse events, and the high benefit-to-risk ratio of
routine vaccination, the introduction of immunization against JE in public health programmes should not be deferred (page 332.)
The three types of JE vaccines that are currently in largescale use are considered efficacious and acceptably safe for use in children. However, following immunization
with the mouse brain-derived vaccine, rare cases of potentially fatal ADEM and hypersensitivity reactions have been reported among children in endemic regions and in
travellers from non-endemic locations. An increased awareness of these specific adverse events is recommended, for example when assessing the actual risk of JE for
the individual traveller. However, because of the rarity of these adverse events, and the greater benefit to risk ratio of routine vaccination, the introduction of
immunization against JE in public health programmes should not be deferred (page 339.)
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 332&3
WHO Position Paper 39
14 February 2008 Page 24 of 59
Schedule
Database ID 88_4 Year 2006
The cell culture-based, live attenuated (JE) vaccine appears to require fewer doses for longterm protection, is in most cases less expensive, and seems to represent an
attractive alternative to the mouse brainderived vaccine. However, more needs to be known on its safety and efficacy when used in immunodeficient people, as well as
on the impact of co-administrating this vaccine with other vaccines (page 332.)
The live attenuated vaccine induces protection for several years after 1 or 2 doses, whereas durable protection by the mouse brain-derived vaccine may require 2-3
initial doses followed by boosters at intervals of approximately 3 years. As the price per dose of the mouse brain-derived vaccine in most countries is higher than that of
the live attenuated vaccine, the need for repeated doses renders the former vaccine unaffordable in many JE-endemic countries (page 339)
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 332&3
WHO Position Paper 39
Database ID 88_5 Year 2006
When immunizing children 1-3 years of age, the mouse brain-derived vaccine provides adequate protection throughout childhood following 2 primary doses 4 weeks
apart and boosters after 1 year and subsequently at 3-yearly intervals until the age of 10-15 years. Equally good childhood protection is obtained by a single dose of the
cell-culture based, live attenuated vaccine followed by a single booster given at an interval of about 1 year (page 332).
For epidemiological, programmatic and economic reasons, JE immunization schedules differ widely from one country to the other. In general, using the mouse
brainderived vaccine, adequate childhood protection is achieved following immunization of children as of 1 year of age with 2 primary doses 4 weeks apart followed by
boosters after 1 year and subsequently at 3-yearly intervals up to the age of 10-15 years. Using the cell culture-based, live attenuated vaccine, equally good childhood
protection is provided by a single dose of vaccine followed by a booster
given at an interval of about 1 year (page 340).
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 332&3
WHO Position Paper 40
Database ID 88_10 Year 2006
Although experience from Thailand shows that JE vaccination of children aged 6-12 months may be highly efficacious as well, in most epidemiological settings primary
immunization should be given at the age of 1-3 years. Given the mostly infrequent occurrence of JE in infancy and the likely interference with passively acquired
maternal antibodies during the first months of life, vaccination is not recommended for children before the age of 6 months.
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 336
WHO Position Paper
14 February 2008 Page 25 of 59
Schedule
Database ID 88_11 Year 2006
In people whose immunity is unlikely to be boosted by natural infection, repeated boosters are required for sustained immunity.
Since the optimal number and timing of booster doses depend on the frequency of natural boosting with JE virus and possibly with related flaviviruses, the schedule for
routine JE immunization has been difficult to standardize. Many Asian countries have adopted a schedule of 2 primary doses preferably 4 weeks apart, followed by a
booster after 1 year. In some countries, subsequent boosters are recommended, usually at about 3-year intervals up to the age of 10-15 years.
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 336
WHO Position Paper
Database ID 88_12 Year 2006
For travellers aged >1 year visiting rural areas of endemic countries for at least 2 weeks, the established current practise is to administer 3 primary doses at days 0, 7 and
28; alternatively 2 primary doses preferably 4 weeks apart. When continued protection is required, boosters should be given after 1 year and then every 3 years.
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 336
WHO Position Paper
Database ID 88_16 Year 2006
(For cell culture-derived, live attenuated JE vaccine,) carefully planned studies are required to establish firm recommendations on the optimal immunization schedule.
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 338
WHO Position Paper
Database ID 88_17 Year 2006
Neither hypersensitivity reactions nor acute encephalitis have been associated with this (cell culture-derived, live attenuated JE) vaccine. However, for immunization of
pregnant women or immunodeficient individuals, the live attenuated vaccine should be replaced by one of the inactivated JE vaccines until further evidence has been
generated.
Japanese encephalitis vaccines (WHO position paper) Weekly Epid. Record (2006, 81: 331-340) Page 338
WHO Position Paper
14 February 2008 Page 26 of 59
Schedule
Measles
Database ID 89_18 Year 2007
SAGE accepted the proposal (of its working group on measles) to maintain the current recommendation for administration of the first dose of measles vaccine at 9
months in settings where the transmission is widespread and mortality is high. Where transmission has been substantially reduced (for example, following high quality
nationwide SIAs), increasing the age from 9 months to 12 months represents a rational and desirable policy change. However, before implementing a change, policy-
makers should review local data on the actual age at which infants
receive measles vaccine, the coverage expected at 12 months compared with 9 months, age-specific measles incidence and review the immunogenicity and effectiveness
of measles vaccine administered at 9 months compared with 12 months.
Conclusions and recommendations from the meeting of the immunization Strategic Advisory Group of Experts (SAGE) - November 2006 Weekly Epid. Record (2006, 82: 1-16) Page 13
Database ID 89_19 Year 2007
With respect to introducing a routine second dose of measles vaccine, SAGE emphasizes the principle that this should be considered only in settings where high
coverage of the first dose has been achieved and sustained and where measles transmission has been reduced to a low level, indicating a well functioning routine
immunization programme. Criteria that could be used to determine if the routine programme is strong enough and the coverage sufficiently high to benefit from a
routine second dose require further analysis and consultation.
Conclusions and recommendations from the meeting of the immunization Strategic Advisory Group of Experts (SAGE) - November 2006 Weekly Epid. Record (2006, 82: 1-16) Page 13
Database ID 89_20 Year 2007
With respect to the optimal interval between SIAs (for measles), SAGE noted a number of examples where delays in conducting follow-up SIAs have led to large
outbreaks (for example, in Brazil, Kenya and Uganda). SAGE agreed with the approach developed by the Regional Office for the Americas and adapted by the
Technical Advisory Group on Measles in the African Region that follow-up SIAs should be conducted before the estimated number of susceptible children reaches the
size of a birth cohort. This approach has been found to be programmatically useful and sufficiently accurate to prevent large outbreaks.
Conclusions and recommendations from the meeting of the immunization Strategic Advisory Group of Experts (SAGE) - November 2006 Weekly Epid. Record (2006, 82: 1-16) Page 14
14 February 2008 Page 27 of 59
Schedule
Database ID 80_3 Year 2006
It is recommended that (measles vaccine) be administered as from the age of nine months, when most children have lost the protection afforded by maternal antibodies.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 3
Database ID 80_7 Year 2006
Appendix 80_7 indicates the relationship between routine measles vaccination coverage and the recommended interval between follow-up supplementary immunization
campaigns.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 6
Database ID 80_9 Year 2006
Supplementary immunization activities -SIAs, (measles):
_ All children in the target-age group should be vaccinated, regardless of their history of measles immunization or illness.
_ In normal circumstances the lower age limit for measles vaccination during SIAs should be nine months. However, children as young as six months should be
vaccinated if a significant proportion of measles cases occur in children aged six to nine months. Children who are vaccinated before the age of nine months should
receive another dose at nine months in order to ensure protection, as up to half of those vaccinated earlier do not develop immunity.
_ Catch-up SIAs should target children aged up to 15 years at the inception of accelerated measles control activities. With regard to follow-up SIAs, the target-age
group should include those children born since the last campaign.
_ The best time to schedule measles SIAs is during seasons of low transmission, as determined on the basis of local experience and reviews of epidemiological data.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 8
Database ID 87_1 Year 2006
A second opportunity for measles immunization is essential to ensure protection against measles.
WHO/UNICEF joint statement - Global plan for reducing measles mortality 2006-2010 WHO/IVB/05.11 Page 2
14 February 2008 Page 28 of 59
Schedule
Database ID 87_4 Year 2006
In conflict or emergency areas, WHO and UNICEF have a commitment to ensure that, at a minimum, measles vaccine and vitamin A supplements are administered.
(WHO/UNICEF joint
statement: reducing measles mortality in emergencies, 2002.)
WHO/UNICEF joint statement - Global plan for reducing measles mortality 2006-2010 WHO/IVB/05.11 Page 3
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
Database ID 1_3 Year 2004
To reduce the risk of infection in hospitals, all children between the ages of six and nine months who have not received measles vaccine and who are admitted to a
hospital should be immunized against measles. If the children’s parents do not know whether they have received measles vaccine, the child should still be immunized.
If a child has received measles vaccine before nine months of age, a second dose should be administered at nine months or as soon as possible after nine months.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 8
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
Database ID 2_27 Year 2004
Note: an infant with known or suspected HIV infection and/or signs and symptoms of AIDS should receive measles vaccine at six months and then again at nine months
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
14 February 2008 Page 29 of 59
Schedule
Database ID 24_3 Year 2004
In complex emergencies, immunization should include all children from 6 months through 14 years of age. At a minimum, children from 6 months through 4 years of
age must be immunized. The choice of the ages covered will be influenced by vaccine availability, funding, human resources and local measles epidemiology.
Reducing measles mortality in emergencies (WHO/UNICEF Joint Statement) WHO/V&B/04.03 Page 3
Database ID 58_4 Year 2004
Immunization against measles is recommended for all susceptible children and adults for whom measles vaccination is not contraindicated.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 131
Database ID 58_5 Year 2004
Asymptomatic HIV infection is an indication, not a contraindication, for measles vaccination. Ideally, the vaccine should be offered as early as possible in the course of
HIV infection. In areas where measles is prevalent, or during outbreaks, individuals with early signs of HIV-induced immunosuppression may also be considered for
vaccination.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 131
Database ID 58_6 Year 2004
The recommended age for measles vaccination depends on the local measles epidemiology as well as on programmatic considerations. In most developing countries,
high attack rates and serious disease among infants necessitate early vaccination, usually at 9 months of age, despite the relatively low (80-85%) seroconversion rates
following vaccination in this age group. Unless severely immunocompromised, HIV-infected infants should receive measles vaccine at 6 months of age, followed by an
additional dose at 9 months.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 131
14 February 2008 Page 30 of 59
Schedule
Database ID 58_7 Year 2004
In most industrialized countries, national health systems are consistently able to provide measles vaccine to a high proportion of infants, with a concomitant reduction in
measles virus circulation. The probability of an infant being exposed to measles before his or her first birthday is low. It is therefore recommended that measles
vaccination be deferred until a child is 12-15 months old, when seroconversion rates in excess of 90% may be expected.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 131
Database ID 58_9 Year 2004
In countries with measles elimination goals, a one-time only measles SIA (supplementary immunization activity) should be considered, targeting all children aged 9
months to 14 years, regardless of disease history or previous vaccination status. Efforts are also needed to target specific groups of young adults who may be at
increased risk for measles infection, including military recruits, university students, health care workers, refugees and international travellers to measles-endemic areas.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 132
Meningococcal
Database ID 59_1 Year 2002
Current internationally marketed meningococcal vaccines are based either on combinations of group-specific capsular polysaccharides (A and C or A,C,Y, and W135)
or on a conjugate between group C specific polysaccharide and a protein carrier. The polysaccharide vaccines are safe and highly immunogenic, although the group C
component is ineffective in children under two years of age. On the other hand, the recently introduced serogroup C conjugate vaccine is safe and efficacious even in
the youngest children.
Current internationally available meningococcal polysaccharide vaccines are safe and effective for individuals aged two years or more and are recommended for routine
immunization of specific risk groups above this age.
Meningococcal vaccines: polysaccharide and polysaccharide conjugate vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 331-339) Page 330 &
332
14 February 2008 Page 31 of 59
Schedule
Database ID 59_10 Year 2002
In addition to their use in emergency mass campaigns, meningococcal vaccines are also recommended for groups in which a particularly high risk of disease has been
documented. These include those attending army units, training camps, or boarding schools, travellers to epidemic areas, and persons with immunological predisposition
to meningococcal disease (such as asplenia and inherited immunological deficiencies).
Meningococcal vaccines: polysaccharide and polysaccharide conjugate vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 331-339) Page 338
Database ID 59_13 Year 2002
In older children and adolescents group C disease may be prevented by a single dose of (group C conjugate meningococcal) vaccine. Where disease in children above
two years of age is the main concern, or where resources are limited, several years of protection may be achieved by single injection of the combined groups A and C
polysaccharide vaccine.
Meningococcal vaccines: polysaccharide and polysaccharide conjugate vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 331-339) Page 338
MMR
Database ID 1_5 Year 2004
Mumps vaccine should be given in combination with measles and rubella vaccines (MMR).
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 11
Database ID 66_9 Year 2000
Rubella vaccine is usually administered at age 12-15 months, but can also be administered to children as young as 9 months of age. In most countries, the vaccine is
given as MR or MMR, and the age of administration is chosen based on the appropriate age for measles vaccination. It may also be administered to older children,
adolescents, students, child care personnel, health care workers, military personnel and adult men in contact with women of childbearing age.
Rubella vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 161-169) Page 166
14 February 2008 Page 32 of 59
Schedule
Mumps
Database ID 1_5 Year 2004
Mumps vaccine should be given in combination with measles and rubella vaccines (MMR).
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 11
Database ID 60_4 Year 2001
If a large proportion of the population remains seronegative for mumps, care should be taken to vaccinate adults considered to be at special risk.
Mumps virus vaccines (WHO position paper) Weekly Epid. Record (2001, 76: 345-356) Page 346
Database ID 60_6 Year 2001
Mumps vaccines are recommended for use in a 1-dose schedule, given at age 12-18 months.
(Page 355) Control of mumps can be achieved through high routine coverage with an effective mumpscontaining vaccine administered at age 12-18 months.
Mumps virus vaccines (WHO position paper) Weekly Epid. Record (2001, 76: 345-356) Page 352
Database ID 60_12 Year 2001
Due to its known low effectiveness, the Rubini-strain (mumps) vaccine should not be used in national immunization programmes. Persons previously immunized with
the Rubini-strain vaccine should receive a dose of an effective mumps vaccine to ensure protection.
Mumps virus vaccines (WHO position paper) Weekly Epid. Record (2001, 76: 345-356) Page 354
14 February 2008 Page 33 of 59
Schedule
Database ID 60_19 Year 2001
A second (mumps) opportunity is not required in countries where coverage with the first dose is sufficiently high (i.e. > 95%). If a second opportunity is required, it
could be administered through a second routine dose, or by implementing periodical catch-up campaigns. Finally, if an initial catch-up campaign is implemented, the
target age group should be determined according to mumps susceptibility. In most unvaccinated populations, most children acquire mumps infections before the age of
10 years.
Mumps virus vaccines (WHO position paper) Weekly Epid. Record (2001, 76: 345-356) Page 355
Pentavalent and Hexavalent
Database ID 39_26 Year 2005
(Considerations for hepatitis B vaccine schedule:)
• A determination of the role of perinatal transmission (useful for birth dose considerations) can be made based on the overall seroprevalance of HBsAg, age-specific
prevalence of HBsAg, and the prevalence of the HBeAg in pregnant women.
• Combination products may not be used at birth; therefore, programmes including the birth dose will need to include monovalent HepB vaccine in the supply.
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 45
Database ID 2_11 Year 2004
Only monovalent HepB vaccine should be used as a birth dose, the dose given within the first week of life. Combination vaccines should not be used at birth, but may
be used in subsequent doses.
Do not use DTP-HepB+Hib as a birth dose. You may use the vaccine for subsequent doses.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 16 &
20
14 February 2008 Page 34 of 59
Schedule
Database ID 55_7 Year 2004
When immunizing against HBV at birth, only monovalent hepatitis B vaccine should be used: the other antigens found in combination vaccines are currently not
approved for use at birth (DTwP, DTaP, Hib, hepatitis A and IPV.)
Hepatitis B vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 255-263) Page 258
Database ID 20_4 Year 2001
Monovalent HepB vaccines must be used to give the birth dose of HepB vaccine.
Combination vaccines that include HepB vaccine must not be used to give the birth dose of HepB vaccine because DTP and Hib vaccines are not recommended to be
given at birth.
Combination vaccines can be given whenever all of the antigens in the vaccine are indicated.
Introducing hepatitis B vaccine into national immunization services WHO/V&B/01.28 Page 2
Database ID 21_5 Year 2001
Combination vaccines that contain Hib conjugate vaccine:
• can be used anytime all of the antigens in the vaccine are indicated by the schedule;
• cannot be used before 6 weeks of age (e.g. for the birth dose of hepatitis B vaccine) because the immunogenicity of the DTP and Hib components will be reduced if
given before this age.
Introducing Haemophilus influenzae type b (Hib) conjugate vaccine into national immunization services WHO/V&B/01.29 Page 2
Database ID 36_3 Year 2001
Monovalent hepatitis B vaccine MUST BE USED for the birth dose.
· Combination vaccines that include hepatitis B vaccine MUST NOT BE USED to give the birth dose of hepatitis B vaccine because DTP and Hib vaccines should not
be administered at birth.
· Either monovalent hepatitis B vaccine or combination vaccines may be used for later doses in the hepatitis B vaccine schedule. Combination vaccines can be given
whenever all the antigens in the vaccines are indicated.
Introduction of hepatitis B vaccine into childhood immunization services. Management guidelines, including information for health worker WHO/V&B/01.31 Page 9
s and parents
14 February 2008 Page 35 of 59
Schedule
Pertussis
Database ID 82_13 Year 2006
In accordance with the recommendations in the previous position paper on diphtheria, use of diphtheria–tetanus vaccine is preferable to single-antigen tetanus toxoid
vaccine. In future, the inclusion of other antigens, e.g. pertussis or Haemophilus influenzae type b (Hib), in booster doses should be considered.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
Database ID 61_2 Year 2005
In countries where the incidence of pertussis has been considerably reduced by successful immunization, a booster dose administered 1–6 years after the primary series
is warranted. The optimal timing of this booster dose as well as the possible need for additional booster doses of DTP depends on the epidemiological situation, and
should be assessed by individual national programmes.
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 31
Database ID 61_7 Year 2005
The main aim of pertussis vaccination is to reduce the risk of severe pertussis in infancy. The vaccine is usually administered in the national childhood immunization
programme as combined DTwP or DTaP vaccine, although the combination often includes additional vaccines (Haemophilus influenzae type b (Hib), hepatitis B
(HepB), poliovirus vaccine (IPV)). The optimal schedule and number of immunizations are not well defined but, in most countries, 3 primary doses are administered
with at least a 1-month interval to infants aged 2–6 months. A booster dose is commonly offered 1–6 years later. WHO recommends the primary series to be
administered at the age of 6, 10 and 14 weeks. National recommendations vary considerably, however.
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 35
14 February 2008 Page 36 of 59
Schedule
Database ID 61_8 Year 2005
Children whose (pertussis) vaccination series has been interrupted should have their series resumed, without repeating previous doses.
In some countries, an additional vaccine dose is now offered to health-care workers and young parents. Only aP vaccines are used for vaccination of older children and
adults. (page 36: Local reactions tend to increase with age and the number of injections.) (page 37: In order to reduce the reactogenicity of booster injections, aP
vaccines with reduced antigen concentration have been formulated for use in adolescents and adults.)
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 35
Database ID 61_9 Year 2005
All infants, including HIV-positive individuals, should be immunized against pertussis.
Pertussis vaccines (WHO position paper) Weekly Epid. Record (2005, 80: 31-39) Page 35
Pneumococcal
Database ID 89_10 Year 2007
Consistent with WHO’s position on new vaccines, PCV-7 (7-serotype conjugate pneumococcal vaccine) can be easily integrated into routine vaccination schedules, and
it may be administered at the same time, though at a different site, as other vaccines in infant immunization programmes, including DTP, hepatitis B, Hib and polio
vaccines. Routine immunization with PCV-7 should be initiated before the age of 6 months to maximize the benefits of the vaccine and may start as early as 6 weeks of
age.
Conclusions and recommendations from the meeting of the immunization Strategic Advisory Group of Experts (SAGE) - November 2006 Weekly Epid. Record (2006, 82: 1-16) Page 9
14 February 2008 Page 37 of 59
Schedule
Database ID 89_11 Year 2007
Clinical efficacy has been demonstrated in 2 schedules (for PCV-7, the 7-serotype conjugate pneumococcal vaccine) : a 6-week, 10-week, 14-week schedule and a 2-
month, 4-month, 6-month schedule, which was followed by a booster dose at 12-15 months of age. Further information on the cost effectiveness of other potential
schedules (for example, using different
numbers of doses or different intervals between doses, and with and without boosters) should be obtained. Other schedules (such as 2 doses in a primary series plus a
booster dose) are being used in some countries, whose experiences may be important as GAVI-supported countries begin introducing PCV-7 or review its use. Although
a late dose (around the first birthday) may be challenging operationally for GAVI-eligible countries, there may be suitable opportunities when a dose of PCV-7 could be
given, such as at the same time as measles vaccination. Countries should evaluate this information once it is available and select the most appropriate schedule based on
the anticipated impact, cost effectiveness and programmatic feasibility.
Conclusions and recommendations from the meeting of the immunization Strategic Advisory Group of Experts (SAGE) - November 2006 Weekly Epid. Record (2006, 82: 1-16) Page 9
Database ID 92_1 Year 2007
The 23-valent (pneumococcal ) vaccine is primarily designed for use in older children and adults who are at high risk for pneumococcal disease.
It is not licensed for use in children aged <2 years
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 94
Database ID 92_2 Year 2007
PCV-7 (7-valent polysaccharide–protein conjugate pneumococcal) vaccine is highly immunogenic in all age groups, but it is currently licensed for use only in children
aged <5 years, including infants aged <12 months.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 94
Database ID 92_5 Year 2007
Trials in several developing countries have demonstrated the efficacy of a 3-dose schedule for infants without a subsequent booster dose. This schedule is compatible
with the schedules of national immunization programmes in many developing countries. The benefit of administering an additional dose in the second year of life
requires further investigation in these settings. Similarly, consideration of alternative PCV-7 vaccination schedules - including delaying the administration of a third
dose so it may be given along with measles vaccination or in the second year of life - should be guided by future research findings.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 95
14 February 2008 Page 38 of 59
Schedule
Database ID 92_6 Year 2007
When the vaccine is first introduced into routine childhood immunization programmes a single catch-up dose of PCV-7 may be given to previously unvaccinated
children aged 12-24 months and to children aged 2-5 years who are at high risk.
(Page 98) - When the vaccine is initially introduced into childhood immunization programmes, a single catch-up dose of PCV-7 may be given to previously
unvaccinated children aged 12-24 months and to children aged 2-5 years considered to be at high risk. It is not known whether re-vaccination is necessary later in life.
(Page 103) - When PCV-7 is first introduced into routine childhood immunization programmes, maximum individual and community-level protection can be achieved
by also providing a single catch-up dose of the vaccine to previously unvaccinated children who are aged 12-24 months and to children aged 2-5 years who are
considered to be at high risk.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 95&98
Database ID 92_12 Year 2007
The primary series of PCV-7 consists of 3 intramuscular doses administered to infants at intervals of at least 4 weeks, starting at the age of 6 weeks or later.
Vaccination at the age of 6 weeks, 10 weeks and 14 weeks in infants in developing countries is as immunogenic as vaccination at 2 months, 4 months and 6 months in
industrialized countries. A booster dose administered after 12 months of age may improve the immune response and may especially affect pneumococcal
nasopharyngeal carriage. Some industrialized countries have adopted a schedule based on delivering 2 doses during infancy (for example, at 2 months and 4 months)
and a third dose at 12-13 months.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 98
Database ID 92_16 Year 2007
To maximize the benefits of the vaccine, routine immunization with PCV-7 should be initiated before 6 months of age and may start as early as 6 weeks of age.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 103
14 February 2008 Page 39 of 59
Schedule
Database ID 92_17 Year 2007
There are 2 schedules that have proven clinical efficacy: a 6 week–10 week–14 week series and a 2 month–4 month–6 month series; this latter series is followed by a
booster dose at 12–15 months of age.
Countries should evaluate information on impact and scheduling once it is available and select the most appropriate schedule based on anticipated impact, cost
effectiveness and programmatic feasibility.
Pneumococcal conjugate vaccine for childhood immunization (WHO position paper) Weekly Epid. Record (2006, 82: 93-104) Page 103
Database ID 84_7 Year 2006
The polyvalent PS (polysaccharide) vaccine (against Streptococcus pneumoniae) is recommended for healthy people over 65 years of age, particularly those living in
institutions. Randomized controlled trials in healthy elderly people in industrialized countries have, however, failed to show a beneficial effect of the vaccine, so that
recommendation for its use in the elderly is based on data from observational studies showing a significant protective effect against invasive (bacteraemic)
pneumococcal disease, but not pneumonia.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 27
Database ID 62_1 Year 2003
(P)oor immunogenicity of polysaccharide (pneumococcal) vaccines in early childhood precludes the use of the 23-valent pneumococcal vaccine in the high-risk group
of children under 2 years of age.
Pneumococcal vaccines (WHO position paper) Weekly Epid. Record (2003, 78: 110-119) Page 111
Database ID 62_4 Year 2003
The duration of protection following immunization with the 23-valent polysaccharide vaccine is estimated at 5 years, or more, in healthy adults. However, the duration
may be considerably shorter in some high-risk groups for pneumococcal disease. Revaccination using the polysaccharide vaccine is not routinely recommended.
(Page 116) Revaccination using the polysaccharide vaccine is not routinely recommended, but immunocompromised children who have received polysaccharide
vaccine may be revaccinated after 3 years. The safety of three or more doses of the polysaccharide vaccine is not known.
Pneumococcal vaccines (WHO position paper) Weekly Epid. Record (2003, 78: 110-119) Page 112
14 February 2008 Page 40 of 59
Schedule
Database ID 62_8 Year 2003
A single dose of the 23-valent polysaccharide vaccine is recommended for selected groups above 2 years of age at increased risk of pneumococcal disease. These
groups include the healthy elderly (over 65 years of age), particularly those living in institutions.
Pneumococcal vaccines (WHO position paper) Weekly Epid. Record (2003, 78: 110-119) Page 116
Database ID 62_12 Year 2003
The polyvalent polysaccharide vaccine is recommended for selected groups above 2 years of age with increased risk of pneumococcal disease. Such groups include the
healthy elderly (over 65 years old), particularly those living in institutions, patients suffering from chronic organ failure, diabetes, nephrotic syndrome and certain
immunodeficiencies, particularly those with functional or anatomical asplenia.
Recent meta-analyses on the efficacy and effectiveness of the pneumococcal polysaccharide vaccine have raised doubts about the benefit of the vaccine in the elderly
population. However, these vaccines continue to be recommended for this group based on evidence from observational studies that show a beneficial effect against
pneumococcal disease associated with bacteraemia.
Pneumococcal vaccines (WHO position paper) Weekly Epid. Record (2003, 78: 110-119) Page 118
Polio
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
Database ID 1_7 Year 2004
OPV is recommended for both routine immunization and supplementary campaigns for polio eradication. IPV is also an effective vaccine. But OPV is less expensive,
safe, and easy for health workers and volunteers to administer.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 15
14 February 2008 Page 41 of 59
Schedule
Database ID 2_6 Year 2004
(Supplementary immunization with OPV) is usually conducted in large scale campaigns (National Immunization Days) where two doses of OPV, one month apart, are
given to all children under five years of age regardless of how many doses they have received in the past. Many rounds of National immunization days maybe
conducted in a country however there is no risk associated with receiving multiple doses of OPV.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 11
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
Database ID 2_23 Year 2004
If a child has diarrhoea when you give OPV, administer an extra dose: that is, a fifth dose at least four weeks after he or she has received the last dose in the schedule.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 25
Database ID 2_28 Year 2004
Wait at least four weeks between doses of OPV, DTP, Hib, and HepB vaccines.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 25
Database ID 2_37 Year 2004
WHO does not, as of July 2003, recommend the adoption of IPV, either alone or in a sequential schedule, in developing countries for the following reasons: unresolved
issues related to the immunogenicity of IPV when administered at birth, six, ten and 14 weeks of age in the EPI vaccination schedule, the continued focal circulation of
wild poliovirus on two continents, the relatively high cost of IPV and the operational complexities of introducing a vaccine which requires syringes and needles, while
OPV is given orally.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 10
14 February 2008 Page 42 of 59
Schedule
Database ID 72_8 Year 2004
Although IPV is deemed to be safe, its efficacy is somewhat unclear, such that WHO is not currently recommending its use for countries with recent endemics or risk of
importation.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 7-9 July 2003 WHO/IVB/ 04.12 Page 73
Rabies
Database ID 93_11 Year 2007
Pre-exposure rabies vaccination requires IM doses of
1 ml or 0.5 ml, depending on the vaccine type, given on
days 0, 7 and 28 (day 28 preferable, but administration
may be advanced towards day 21 if time is limited).
Weekly epidemiological record No. 49/50, 2007, 82, 425-436 Page 432
Database ID 84_10 Year 2006
This type of vaccine (inactivated rabies vaccine) is still unfortunately manufactured and used in South-East Asia, but the number of countries doing so has been
decreasing during the past 10 years in accordance with the WHO recommendations to replace them by cell-cultured vaccines.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 89
Database ID 84_13 Year 2006
It is well known that rabies PEP [post-exposure prophylaxis] with vaccine alone is not always sufficient, especially in cases of severe exposure (category 3) where
concommittant passive immunization with rabies immunoglobulins (RIG) is strongly recommended.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 90
14 February 2008 Page 43 of 59
Schedule
Database ID 64_1 Year 2002
Post-exposure treatment, including when necessary specific rabies immune globulin, is recommended for all cases of potential (rabies) infection.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 110
Database ID 64_3 Year 2002
The indication for post-exposure vaccination with or without rabies immune globulin depends on the type of contact with the rabid animal. Types of contact are:
category I .touching or feeding animals, licks on the skin; category II .nibbling of uncovered skin, minor scratches or abrasions without bleeding, licks on broken skin;
category III . Single or multiple transdermal bites or scratches, contamination of mucous membrane with saliva from licks. For category I no treatment is required,
whereas for category II immediate vaccination and for category III immediate vaccination and administration of rabies immune globulin are recommended in addition to
immediate washing and flushing of all bite wounds and scratches. Depending on vaccine type, the post-exposure schedule prescribes intramuscular doses of 1 ml or 0.5
ml given as 4-5 doses over 4 weeks. For rabies-exposed patients who have previously undergone complete pre-exposure vaccination or post-exposure treatment with
cell-derived rabies vaccines, 2 intramuscular doses of a cell-derived vaccine separated by 3 days are sufficient. Rabies immune globulin treatment is not necessary in
such cases. The same rules apply to persons vaccinated against rabies who have demonstrated neutralizing antibody titres of at least 0.5 IU/ml.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 117
Database ID 64_4 Year 2002
Factors that should be taken into consideration when deciding whether or not to initiate (post-exposure rabies) treatment are the category of exposure, the presence of
rabies in the area where the contact occurred or from which the animal came, and the animal species involved. Also, the vaccination status and clinical features of the
animal involved, the type of vaccine used and the availability of the animal for observation must be considered, as should be, if available, the results of laboratory
testing of the animal.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 119
Database ID 64_9 Year 2002
Veterinary rabies vaccines should not be used for humans.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 118
14 February 2008 Page 44 of 59
Schedule
Database ID 64_11 Year 2002
Pre-exposure (rabies) vaccination may be performed with any of the modern cell-derived vaccines and is recommended for anyone at increased risk of exposure to
rabies virus. Traditionally, this recommendation includes laboratory staff, veterinarians, animal handlers, wildlife officers with frequent exposure to potentially infected
animals as well as visitors to highly rabies-enzootic areas who may be exposed to rabies hosts. However, according to age-stratified studies of incidence, those at
greatest risk are probably children living in rabies-enzootic regions of the developing world.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 116
Database ID 64_12 Year 2002
The pre-exposure (rabies vaccine) schedule requires intramuscular doses of 1 ml or 0.5 ml, depending on the vaccine type, given on days 0, 7 and 28. Major vaccine
manufacturers recommend 1 booster dose after 1 year, and to ensure protection in persons at continued risk, booster vaccinations every 5 years, or ideally, at intervals
dictated by regular testing for antirabies antibodies (titres >0.5 IU/ml required for protection).
On the other hand, studies with the human diploid cell vaccine and the purified Vero cell rabies vaccine have shown that 10 years after a pre-exposure series followed
by a single booster dose after 1 year, more than 96% of the vaccines still have neutralizing antibodies against rabies virus.
Rabies vaccines (WHO position paper) Weekly Epid. Record (2002, 77: 109-119) Page 117
Rubella
Database ID 1_9 Year 2004
For prevention of CRS, women of childbearing age are the primary target group for rubella immunization. Immunizing women between the ages of 15 and 40 will
rapidly reduce the incidence of CRS without affecting childhood transmission of the rubella virus.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 18
Database ID 72_14 Year 2004
(SAGE) urges consideration of men as an additional rubella immunization target, important for rapid control of both rubella and CRS.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 7-9 July 2003 WHO/IVB/ 04.12 Page 81
14 February 2008 Page 45 of 59
Schedule
Database ID 66_9 Year 2000
Rubella vaccine is usually administered at age 12-15 months, but can also be administered to children as young as 9 months of age. In most countries, the vaccine is
given as MR or MMR, and the age of administration is chosen based on the appropriate age for measles vaccination. It may also be administered to older children,
adolescents, students, child care personnel, health care workers, military personnel and adult men in contact with women of childbearing age.
Rubella vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 161-169) Page 166
Tetanus
Database ID 52_11 Year 2006
To further promote immunity against diphtheria, diphtheria toxoid and tetanus toxoid rather than tetanus toxoid alone should be used when tetanus prophylaxis is
needed following injuries.
Diphtheria vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 24-32) Page 25
Database ID 80_16 Year 2006
In order to prevent neonatal tetanus, women should receive a minimum of two doses of tetanus toxoid (TT) vaccine, administered at least four weeks apart.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 15
Database ID 82_11 Year 2006
It was generally agreed (by SAGE members) that (for tetanus vaccine) there is no maximum interval between the primary series and a booster dose and that there is no
need to re-start interrupted immunization schedules. Vaccination of school-age children would also help to sustain MNT (maternal and neonatal tetanus) elimination.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
14 February 2008 Page 46 of 59
Schedule
Database ID 82_12 Year 2006
SAGE recommended the following (regarding tetanus immunization schedules):
A 5-dose childhood immunization schedule should be promoted. The primary series of 3 doses would be given in infancy, with a booster dose ideally at age 4-7 years
and another booster dose in adolescence (e.g. at age 12-15 years). The exact timing of the booster doses should be flexible to take account of the most appropriate
health service contacts in different countries and of integration with other vaccines and other interventions such as bednet distribution, vitamin A therapy and
deworming. In some countries, these boosters could be given through school-based approaches, but efforts to reach those not attending school will be important. A sixth
dose should be recommended for adults, for example in the first pregnancy or for military recruits.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
Database ID 82_13 Year 2006
In accordance with the recommendations in the previous position paper on diphtheria, use of diphtheria–tetanus vaccine is preferable to single-antigen tetanus toxoid
vaccine. In future, the inclusion of other antigens, e.g. pertussis or Haemophilus influenzae type b (Hib), in booster doses should be considered.
Conclusions and recommendations from the Strategic Advisory Group of Experts (SAGE) - 10-11 April 2006 Weekly Epid. Record (2006, 81: 210-20) Page 217
Database ID 83_1 Year 2006
Vaccines containing DT are used for children aged <7 years and dT-containing vaccines for individuals aged ≥7 years.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 198
Database ID 83_2 Year 2006
As a rule, vaccine combinations containing diphtheria toxoid (D or d) and tetanus toxoid, rather than tetanus toxoid alone, should be used when immunization against
tetanus is indicated.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 198
14 February 2008 Page 47 of 59
Schedule
Database ID 83_4 Year 2006
A childhood tetanus immunization schedule of 5 doses is recommended. WHO recommends that the primary series of 3 doses should be given in infancy (aged <1
year). Where pertussis is of particular risk to young infants, DTP immunization should be started at age 6 weeks and 2 subsequent doses should be given at intervals of
at least 4 weeks (e.g. at weeks 10 and 14). The exact timing of the booster doses should be flexible to take account of the most appropriate health service contacts in
different countries. Ideally, a booster dose should be offered at age 4-7 years followed by another booster in adolescence, e.g. at age 12-15 years. Where a high
percentage of children, including girls, attend school, school-based immunization programmes should be used where feasible to deliver the booster doses. Special
efforts to reach school nonattenders will be needed.
In addition to the childhood vaccination programme, an extra tetanus toxoid-containing dose to adults will provide additional assurance of long-lasting, possibly lifelong
protection. Therefore, a sixth dose should be recommended for adults, e.g. at the time of the first pregnancy or during military service. Those who receive their first
tetanus vaccine doses as adolescents or adults require a total of only 5 appropriately spaced doses to obtain the same long-term protection.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 199 &
206
Database ID 83_5 Year 2006
Even after many years, an interrupted primary- or boosterdose (tetanus vaccine) schedule should not be restarted; the schedule is simply continued with the next dose
that is due.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 206
Database ID 83_11 Year 2006
The interval between the tetanus toxoidcontaining doses should be at least 4 weeks. Longer intervals may increase the magnitude and duration of the immune response,
but should not be a reason to delay immunization.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 203
Database ID 83_12 Year 2006
Both TT and dT can be used at any time during pregnancy.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 204
14 February 2008 Page 48 of 59
Schedule
Database ID 83_14 Year 2006
The “high-risk approach” to control neonatal tetanus should be part of the neonatal tetanus elimination strategy in countries where the elimination target (<1 case per
1000 live births at district level) has not yet been reached. This approach targets all women of childbearing age and consists of campaign-style immunization
(supplementary immunization activities, or SIAs) with 3 doses of TT (or dT) with an interval of at least 4 weeks between doses 1 and 2, and of at least 6 months
between doses 2 and 3. Promotion of clean deliveries is part of this approach. In addition to the 3 doses provided in the SIAs, 2 further boosters are needed to provide
long-term protection to women with no documented receipt of tetanus toxoid-containing vaccines in childhood.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 205
Database ID 83_15 Year 2006
Although adequately immunized people should have sufficient protection against tetanus, treating physicians may give a dose of tetanus toxoid-containing vaccine in the
case of an injury, in addition to other preventive measures. Depending on the severity of the injury and on the reliability of the history of previous tetanus vaccinations,
the vaccine should be given if the last dose was administered more than 10 years ago (or 5 years in the case of severe injuries)*. The immunization schedule should be
completed as soon as possible for those who have not received all doses of the basic schedule.
In addition, passive immunization using tetanus antitoxin, preferably of human origin, may be needed for prophylaxis (e.g. in cases of dirty wounds in incompletely
immunized individuals). Such antitoxin is also essential in the treatment of tetanus cases and should be readily available in all countries. From page 200: While tetanus
antitoxin should be readily available in all countries, its use cannot substitute for the need to achieve and sustain high tetanus vaccination coverage.
* Summary guide to tetanus prophylaxis in routine wound management. In: Heymann DL, ed. Control of communicable diseases manual, 18th ed. Washington, DC,
American Public Health Association, 2004:532; Surgical care at the district hospital. Geneva, World Health Organization, 2003:4-12.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 205
Database ID 83_16 Year 2006
For previously non-immunized adolescents and adults, the recommended schedule is 2 (tetanus vaccine) doses administered at least 4 weeks apart followed by a third
dose administered at least 6 months after the second, and subsequent boosters at least 1 year apart. Those who receive their first tetanus vaccine doses as adolescents or
adults require a total of only 5 appropriately spaced doses to obtain long-term protection.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 206
14 February 2008 Page 49 of 59
Schedule
Database ID 83_17 Year 2006
In countries where MNT remains a public health problem, pregnant women for whom reliable information on previous tetanus vaccinations is not available should
receive at least 2 doses of tetanus toxoid-containing vaccine (normally dT) with an interval of at least 4 weeks between the doses. To ensure protection for a minimum
of 5 years, a third dose should be given at least 6 months later. A fourth and fifth dose should be given at intervals of at least 1 year, e.g. during subsequent pregnancies,
in order to ensure long-term protection. Pregnant women who have received only 3 doses of DTP in early infancy should receive 2 doses of a tetanus toxoid-containing
vaccine with a minimal interval of 4 weeks. Those who received 4 doses of tetanus vaccine during their childhood need only 1 booster dose, which should be given at
the first opportunity. In both scenarios, to provide protection throughout childbearing age, a sixth dose would be needed after at least 1 year.
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 207
Database ID 83_18 Year 2006
See Appendix 83_18 for a summary table of immunizations with diphtheria–tetanus–pertussis (DTP) and diphtheria toxoid (Td) vaccines required to obtain long-term
protectiona against tetanus
Tetanus vaccine (WHO position paper) Weekly Epid. Record (2006, 81: 198-208) Page 207
Database ID 1_10 Year 2004
Immunizing infants and children with DTP or DT and adults with Td prevents tetanus.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 20
Database ID 1_11 Year 2004
Neonatal tetanus can be prevented by immunizing women of childbearing age with tetanus toxoid, either during pregnancy or outside of pregnancy. This protects the
mother and enables tetanus antibodies to be transferred to her baby.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 20
Database ID 1_12 Year 2004
People who recover from tetanus do not have natural immunity and can be infected again and therefore need to be immunized.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 20
14 February 2008 Page 50 of 59
Schedule
Database ID 2_7 Year 2004
Because it contains high levels of diphtheria toxoid, (DT) should not be given to children older than six years old or adults.
Td, or tetanus-diphtheria toxoids adult dose vaccine, is the same vaccine as DT, but with a lower diphtheria toxoid dose. It is suitable for children older than six years
old and adults, including pregnant women.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 12
Database ID 2_8 Year 2004
A three-dose course of TT or Td provides protection against maternal and neonatal tetanus for at least five years. A maximum of five doses will protect women
throughout their childbearing years.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 12
Database ID 6_9 Year 2004
At any immunization session, especially outreach, you should offer routine TT immunization to pregnant women.
Some countries also have a policy of providing TT immunization to non-pregnant or recently pregnant women during routine infant immunization sessions.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 6: Holding an immunization session WHO/IVB/04.06 Page 12
Database ID 7_1 Year 2004
A woman should receive no more than five doses of TT
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 7: Monitoring and using your data WHO/IVB/04.06 Page 7
Database ID 41_17 Year 2003
If a child was unprotected (against neonatal tetanus at birth) the mother should receive a does of TT during the same visit and should be followed up with a subsequent
TT dose if needed for protection. The same applies for mothers whose children were protected at birth but who remain eligible for another TT dose.
WHO–recommended standards for surveillance of selected vaccine-preventable diseases WHO/V&B/03.01 Page 27
14 February 2008 Page 51 of 59
Schedule
Typhoid
Database ID 84_4 Year 2006
The Ty21a (typhoind) vaccine is . . . to be swallowed every other day for one week. It can be taken simultaneously with the attenuated CVD103-HgR V. cholerae
vaccine.
State of the art of new vaccines: research and development WHO/IVB/06.01 Page 13
Database ID 67_2 Year 2000
Immunization of school-age children is recommended in areas where typhoid fever in these age groups is a significant public health problem, and particularly where
antibiotic-resistant S. typhi strains are prevalent. In those settings immunization against typhoid fever will be required until socioeconomic improvements finally
interrupt transmission of S. typhi. Where appropriate the use of typhoid vaccines should be harmonized with the administration of tetanus and diphtheria vaccines.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 258
Database ID 67_6 Year 2000
To maintain protection, revaccination (with the Vi polysaccharide vaccine) is recommended every 3 years.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 262
Database ID 67_7 Year 2000
Protection (provided by the Ty21a vaccine) is markedly influenced by the number of doses and their spacing. When the vaccine is given in 3 doses 2 days apart,
protective immunity is achieved 7 days after the last dose. In endemic areas a booster dose is recommended every 3 years. Travellers from non-endemic to endemic
regions are recommended a booster on a yearly basis. There are currently no field trial data to document the efficacy of this vaccine in children aged < 3 years.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 262
14 February 2008 Page 52 of 59
Schedule
Database ID 67_8 Year 2000
The (Ty21a typhoid) vaccine is usually administrated orally as entericcoated capsules and is registered for use from 6 years of age.
A liquid formulation of the Ty21a (Ty21a typhoid) vaccine can be taken by children as young as 2 years and has proved more immunogenic than the capsular
formulation.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 262
Database ID 67_12 Year 2000
Primary immunization with this (old inactivated whole-cell) parenteral (typhoid) vaccine consists of 2 doses given 4 weeks apart; a single booster dose is recommended
every 3 years.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 263
Database ID 67_14 Year 2000
For the occasional small-scale vaccination in countries of low typhoid endemicity and for individual protection of short-term visitors to highly-endemic areas, either of
the 2 modern (typhoid) vaccines is recommended. It should be noted, however, that the vaccines do not provide complete protection and should not replace hygiene
precautions.
Typhoid vaccines (WHO position paper) Weekly Epid. Record (2000, 75: 257-264) Page 263
Varicella
Database ID 68_2 Year 1998
(Varicella) vaccine may be offered in any country to individual adolescents and adults without a history of varicella, in particular to those at increased risk of
contracting or spreading the infection. This use in adolescents and adults entails no risk of an epidemiological shift, as childhood exposure to VZV remains unaffected.
Varicella vaccines (WHO position paper) Weekly Epid. Record (1998, 73: 241-248) Page 241
14 February 2008 Page 53 of 59
Schedule
Database ID 68_5 Year 1998
From a logistic as well as an epidemiological point of view, the optimal age for varicella vaccination is 12-24 months.
In Japan and several other countries 1 dose of the (varicella) vaccine is considered sufficient, regardless of age. In the United States, 2 doses, 4-8 weeks apart, are
recommended for adolescents and adults, in whom 78% were found to have seroconverted after the first, and 99% after the second dose of the vaccine. Children below
13 years receive only 1 dose.
Varicella vaccines (WHO position paper) Weekly Epid. Record (1998, 73: 241-248) Page 245
Vitamin A
Database ID 80_14 Year 2006
(V)itamin A distribution linked with measles SIAs should only serve to complement routine distribution activities. In communities where VAD (vitamin A deficiency)
exists, all infants and children aged 6 to 59 months should be given vitamin A during SIAs.
The minimum interval between doses of vitamin A is one month.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 12
Database ID 80_26 Year 2006
One month prior to SIA, the country should consider suspending the administration of prophylactic Vitamin A in routine services nationwide, and resume administering
it one month after SIA.
• Take all children aged between 6 to 59 months to receive vitamin A drops.
• Six months after the last dose of vitamin A every child should receive an additional dose.
Global field guide for planning and implementing measles supplementary immunization activities WHO/IVB/04.24 Page 39
14 February 2008 Page 54 of 59
Schedule
Database ID 1_20 Year 2004
Vitamin A supplementation can be combined with immunization services for children and women when health officials know or suspect that vitamin A deficiency is
present in an area or among a certain population. Vitamin A may be given at the same time as immunization.
Opportunities for linking Vitamin A and routine immunization are shown in Appendix 1_20.
The optimal interval between (Vitamin A) doses is 4-6 months. The minimum recommended safe interval between doses is one month. The interval between doses can
be reduced to treat clinical vitamin A deficiency and measles cases.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 1: Target diseases WHO/IVB/04.06 Page 35
Database ID 6_7 Year 2004
If your country provides vitamin A supplementation during routine immunization, you must screen mothers and children younger than 5-years-old for vitamin A
supplementation at every immunization contact.
Ideally, infants and children should receive vitamin A doses of 100 000 IU (6-11 months) or 200 000 IU (12-59 months) every 4-6 months. Repeat supplementary
doses should never be less than 4 weeks apart unless the child is being treated for measles or eye signs of VAD.
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 6: Holding an immunization session WHO/IVB/04.06 Page 11
Database ID 58_11 Year 2004
Vitamin A supplementation has been shown to markedly reduce measles-associated mortality in developing countries and should always be given to measles patients in
areas where vitamin A deficiency is prevalent.
Measles vaccines (WHO position paper) Weekly Epid. Record (2004, 79: 130-142) Page 134
Database ID 72_10 Year 2004
The current strategy is for no (vitamin A) supplementation within the first six months of life.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 7-9 July 2003 WHO/IVB/ 04.12 Page 74
14 February 2008 Page 55 of 59
Schedule
Database ID 74_22 Year 2002
SAGE supports the continued use of opportunities to include vitamin A supplementation in routine and supplementary immunization services, including the contact with
measles immunization at 9 months of age and the treatment of childhood illnesses as per IMCI guidelines.
Coverage data need to be improved.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 14-15 June 2001 (WHO/V&B/02.07) Page 50
Yellow Fever
Database ID 39_5 Year 2005
WHO recommends the following schedule for infants (Appendix 39_5).
Vaccine introduction guidelines. Adding a vaccine to a national immunization programme: decision and implementation WHO/IVB/05.18 Page 32
Database ID 77_4 Year 2005
GACVS reiterates that particular care should be taken that the (17D yellow fever) vaccine is received only by those travellers who are truly at risk of exposure to yellow
fever. In addition, vaccine providers should give careful consideration to the risks and benefits for elderly travellers and should routinely enquire about a history of
thymus disorder, irrespective of the age of the subject. Where a history of thymus disorder is reported, alternative prevention measures should be considered.
Global Advisory Committee on Vaccine Safety, 2–3 December 2004 Weekly Epid. Record (2005, 80: 3-7) Page 7
Database ID 2_19 Year 2004
Typical immunization schedule for children (see Appendix 2_19.)
Immunization in practice: a practical resource guide for Health workers – 2004 update_____Module 2: The vaccines WHO/IVB/04.06 Page 24
14 February 2008 Page 56 of 59
Schedule
Database ID 72_12 Year 2004
Yellow fever vaccination for the purposes of international travel is geared towards protecting non-infected countries from importation of the virus. Thus a conservative
approach is still deemed necessary and 10-year booster shots should be maintained in this situation. However, in endemic countries, it is preferable to prioritize efforts
to achieve good primary coverage rather than booster doses.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 7-9 July 2003 WHO/IVB/ 04.12 Page 76
Database ID 79_4 Year 2004
(GACVS stated that) particular care should be taken that the (yellow fever) vaccine is received only by those travellers truly at risk for yellow fever exposure.
Furthermore, care should be taken that routine yellow fever vaccination programmes are not jeopardized by risk–benefit ratios that may be inapplicable to the target
populations in endemic countries.
Global Advisory Committee on Vaccine Safety, 3–4 December 2003 Weekly Epid. Record (2004, 79: 16-20) Page 19
Database ID 69_4 Year 2003
YF (yellow fever) vaccine should be offered to all travellers to and from at-risk areas, unless they belong to the group of individuals for whom YF vaccination is
contraindicated. There is currently insufficient scientific evidence to support a change in the International health regulations for travelers to endemic areas demanding
proof of valid YF vaccination within the preceding ten years. However, in at-risk countries, vaccination resources should be directed to ensuring good primary
vaccination coverage rather than to providing booster doses.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 350
Database ID 69_12 Year 2003
All persons aged 9 months or older and living in YF (yellow fever) at-risk areas should receive YF vaccine. Highest priority should be given to those persons most
likely to be exposed, such as forestry and agricultural workers, and to those living in villages or towns with a history of previous outbreaks. Immigrants to such regions
from non-endemic areas should also be vaccinated against YF.
Travellers should be vaccinated at least 10 days before arrival in the at risk area.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 356
14 February 2008 Page 57 of 59
Schedule
Database ID 69_16 Year 2003
In countries at risk of YF (yellow fever), YF vaccine is recommended for use in all children aged at least 9-12 months of age. In addition, preventive vaccination of
older children and adults is recommended in at risk areas. Vaccination for YF is also recommended for travellers aged above 9 months who plan to visit areas at risk for
YF.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 357
Database ID 69_18 Year 2003
According to the International health regulations and the WHO International certificate of vaccination, a boosterdose of YF (yellow fever) vaccine is required every 10
years. However, in most cases, the duration of protection following the first dose of YF vaccine seems to be at least 30-35 years and possibly lifelong. For this reason, it
has been proposed to limit vaccination against YF to a single dose. In order to clarify this matter, WHO organized a consultation with a group of YF experts in March
2003. This group reviewed relevant literature and available data and concluded that, at present, the evidence for protective immunity beyond 10 years was insufficient to
justify a change in the current YF vaccination policy for international travellers. However, in at-risk countries, vaccination resources should be directed to ensuring
good primary vaccination coverage rather than to providing booster doses. For the purposes of international travel, only YF vaccinations performed at nationally
authorized YF vaccination sites and using WHO pre-qualified YF vaccines may be entered into the International Certificate of Vaccination.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 358
Database ID 69_19 Year 2003
Given the very rare, but potentially severe, adverse effects, YF (yellow fever) vaccine for travellers should be administered on strict indications only, particularly in the
elderly. Restriction of YF vaccination to authorized centres is likely to promote the appropriate use of YF vaccine.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 358
Database ID 69_24 Year 2003
The (YF) vaccine is also widely used for the protection of travelers to YF-endemic areas.
Yellow fever vaccine (WHO position paper) Weekly Epid. Record (2003, 78: 349-359) Page 350
14 February 2008 Page 58 of 59
Schedule
Database ID 73_7 Year 2003
The issue of deaths following YF (yellow fever) vaccination was highly sensitive where few YF cases exist, and vaccination should be postponed in such countries.
WHO believed the vaccine to be safe but more data were necessary.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 14–15 June 2002 WHO/V&B/03.06 Page 61
Database ID 74_25 Year 2002
(SAGE recommends that the) policy of vaccinating persons who are going to travel to areas where yellow fever is endemic should be continued.
Report of the Strategic Advisory Group of Experts (SAGE) - Geneva, 14-15 June 2001 (WHO/V&B/02.07) Page 63
14 February 2008 Page 59 of 59
You might also like
- Business Plan For Orthopedic HospitalDocument5 pagesBusiness Plan For Orthopedic HospitalDarshan More100% (1)
- Medical ReportDocument5 pagesMedical ReportShoaib Mirza0% (1)
- Geeky Medics DocumentationDocument3 pagesGeeky Medics DocumentationGus LionsNo ratings yet
- Non-Specific Effects of Bacillus Calmette-Guérin: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument18 pagesNon-Specific Effects of Bacillus Calmette-Guérin: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDaniel TurudicNo ratings yet
- Microorganisms 10 02483Document15 pagesMicroorganisms 10 02483Robert StryjakNo ratings yet
- Best Practive Clinical 2021Document17 pagesBest Practive Clinical 2021cdsaludNo ratings yet
- Neonatal Immunization Rationale Current State andDocument10 pagesNeonatal Immunization Rationale Current State andNancy CVNo ratings yet
- ContraindicationsDocument17 pagesContraindicationsAndyanYugatamaNo ratings yet
- Exploring The Limitations of BCG VaccineDocument7 pagesExploring The Limitations of BCG Vaccinenajdah_220754970No ratings yet
- Stage Gating Criteria Tables 2021Document39 pagesStage Gating Criteria Tables 2021bilou hertNo ratings yet
- Research Proposal EdittedDocument47 pagesResearch Proposal EdittedSkyNo ratings yet
- Prevention of Group B Streptococcal Early-Onset Disease in Newborns - ACOGDocument66 pagesPrevention of Group B Streptococcal Early-Onset Disease in Newborns - ACOGxemdoan044No ratings yet
- Vaccines 11 01459Document18 pagesVaccines 11 01459Robert StryjakNo ratings yet
- Recommendations For Term and Late Preterm Infants at Risk For Perinatal Bacterial InfectionDocument5 pagesRecommendations For Term and Late Preterm Infants at Risk For Perinatal Bacterial InfectionAbdi KebedeNo ratings yet
- Epi L 4 MW 2013Document91 pagesEpi L 4 MW 2013Nigus AfessaNo ratings yet
- Materi Prof. Dr. Dr. Sri Rezeki H. Hadinegoro SpAK Catch Up ImmunizationDocument36 pagesMateri Prof. Dr. Dr. Sri Rezeki H. Hadinegoro SpAK Catch Up ImmunizationFatmaNo ratings yet
- Vaccine AdministrationDocument60 pagesVaccine AdministrationpradipkshetriNo ratings yet
- Oral Polio Influences Immune Response To BCG VaccinationDocument9 pagesOral Polio Influences Immune Response To BCG Vaccinationromeoenny4154No ratings yet
- The Pfizer BioNTech (BNT162b2) COVID-19 Vaccine - What You Need To KnowDocument5 pagesThe Pfizer BioNTech (BNT162b2) COVID-19 Vaccine - What You Need To KnowdianavemNo ratings yet
- Rezky. Anshar. 1Document9 pagesRezky. Anshar. 1rezkyNo ratings yet
- BCG Vaccine and COVID-19 Implications For Infection Prophylaxis and Cancer ImmunotherapyDocument4 pagesBCG Vaccine and COVID-19 Implications For Infection Prophylaxis and Cancer ImmunotherapysovalaxNo ratings yet
- UKHSA Guidelines On VZ Post Exposure ProphylaxisDocument25 pagesUKHSA Guidelines On VZ Post Exposure ProphylaxisShehzadAlamNo ratings yet
- WHO 2019 nCoV Vaccines SAGE Recommendation BIBP 2021.1 EngDocument7 pagesWHO 2019 nCoV Vaccines SAGE Recommendation BIBP 2021.1 EngDiane LigmanNo ratings yet
- A Simple and Rapid Identification Method For Mycobacterium Bovis BCG With Loop-Mediated Isothermal AmplificationDocument12 pagesA Simple and Rapid Identification Method For Mycobacterium Bovis BCG With Loop-Mediated Isothermal AmplificationEdgar DíazNo ratings yet
- Estreptoco NeonatosDocument14 pagesEstreptoco NeonatosJuan Diego MarulandaNo ratings yet
- Invasive Bacterial Disease Trends and Characterization of Group B Streptococcal Isolates Among Young Infants in Southern Mozambique, 2001-2015Document16 pagesInvasive Bacterial Disease Trends and Characterization of Group B Streptococcal Isolates Among Young Infants in Southern Mozambique, 2001-2015Justino WaveleNo ratings yet
- 2024 What Is Next For BCG Revaccination To Prevent Tuberculosis. LancetDocument2 pages2024 What Is Next For BCG Revaccination To Prevent Tuberculosis. LancetcomprademaxNo ratings yet
- BCG Vaccine: Immunizations For TravelersDocument12 pagesBCG Vaccine: Immunizations For Travelerseric lauwrenzNo ratings yet
- How To Deal With Cab in BCG Shortage EraDocument43 pagesHow To Deal With Cab in BCG Shortage Erap'eng matchima h.No ratings yet
- WHO 2019 nCoV Vaccines SAGE Recommendation BBV152 2022.1 EngDocument10 pagesWHO 2019 nCoV Vaccines SAGE Recommendation BBV152 2022.1 EngJjNo ratings yet
- Recommend Ations: S GK, SS, S M, K C, S A, S K D, S V, A KS, S S, S K, H K P, SB, B JP, GVB, P GDocument11 pagesRecommend Ations: S GK, SS, S M, K C, S A, S K D, S V, A KS, S S, S K, H K P, SB, B JP, GVB, P Ga hNo ratings yet
- WHO IVB 15.09 EngDocument59 pagesWHO IVB 15.09 EngAbdul AhadNo ratings yet
- Antibiotic Stewardship in Perinatal and Neonatal Care Ramasethu2017Document6 pagesAntibiotic Stewardship in Perinatal and Neonatal Care Ramasethu2017María Cristina RomanoNo ratings yet
- Journal OctoberDocument4 pagesJournal OctoberCyrenne TababanNo ratings yet
- CHN Ebr 1Document2 pagesCHN Ebr 1nissieNo ratings yet
- Tuberculosis 6: New Vaccines For TuberculosisDocument10 pagesTuberculosis 6: New Vaccines For TuberculosisDinesh NerkarNo ratings yet
- Readersdpiis2468042722000069token &OriginRegion Us East 1&OriginCreationDocument13 pagesReadersdpiis2468042722000069token &OriginRegion Us East 1&OriginCreationMelanie Anaud Magro-AmosNo ratings yet
- Who Can Take The Pfizer-Biontech Covid-19 Vaccine?Document4 pagesWho Can Take The Pfizer-Biontech Covid-19 Vaccine?Hazel EstayanNo ratings yet
- BCG For Sars Cov 2Document3 pagesBCG For Sars Cov 2dickypranataNo ratings yet
- Defining The Recipe For An Optimal Rotavirus Vaccine Introduction in A High-Income Country in Europe STANDAERTDocument23 pagesDefining The Recipe For An Optimal Rotavirus Vaccine Introduction in A High-Income Country in Europe STANDAERTRoxana Ștefania DrăganNo ratings yet
- Neonatal Immunization: Hepatitis B Vaccine Can Prevent Hepatitis B and Its ConsequencesDocument3 pagesNeonatal Immunization: Hepatitis B Vaccine Can Prevent Hepatitis B and Its ConsequencesMahmoud AbouelsoudNo ratings yet
- Vaccines 10 00472Document17 pagesVaccines 10 00472IdmNo ratings yet
- Vaccines 10 00246Document17 pagesVaccines 10 00246john paul carasNo ratings yet
- Comparison of BCG Vaccination at Birth and at 3 MonthDocument3 pagesComparison of BCG Vaccination at Birth and at 3 Monthromeoenny4154No ratings yet
- Kenya National Immunization Policy Guidelines Version SignedDocument100 pagesKenya National Immunization Policy Guidelines Version SignedHarriet Temba100% (1)
- Sars-Cov-2 A Public Health Emergency: Challenges in Vaccination in Indian SetupDocument5 pagesSars-Cov-2 A Public Health Emergency: Challenges in Vaccination in Indian Setupgaurav pandeyNo ratings yet
- 1 s2.0 S1198743X19300813 MainDocument5 pages1 s2.0 S1198743X19300813 MainNia KurniawanNo ratings yet
- Trial of BCG Vaccines in South India For Tuberculosis Prevention: First ReportDocument9 pagesTrial of BCG Vaccines in South India For Tuberculosis Prevention: First ReportMarisa LisnawatiNo ratings yet
- Exploring BCG Vaccination As A Novel Approach To Prevent R - 2023 - eClinicalMedDocument3 pagesExploring BCG Vaccination As A Novel Approach To Prevent R - 2023 - eClinicalMedronaldquezada038No ratings yet
- Strepto 2020Document12 pagesStrepto 2020Jordana NahsanNo ratings yet
- Cacth - Up Immunization in ChildhoodDocument35 pagesCacth - Up Immunization in ChildhoodYesi SaputriNo ratings yet
- Abscence of Scar FormationDocument9 pagesAbscence of Scar FormationRizzzzzzzzzzNo ratings yet
- Comment: Bcg-Induced Trained Immunity: Can It Offer Protection Against Covid-19?Document3 pagesComment: Bcg-Induced Trained Immunity: Can It Offer Protection Against Covid-19?edison aruquipaNo ratings yet
- Operational Guidelines For PCV IntroductionDocument104 pagesOperational Guidelines For PCV IntroductionSK SARFARAZ UDDINNo ratings yet
- VSD Covid Vaccine Sab SB Protocol 508Document28 pagesVSD Covid Vaccine Sab SB Protocol 508yoshbriantitoNo ratings yet
- Bookshelf NBK550970Document17 pagesBookshelf NBK550970Lucas WillianNo ratings yet
- Universalimmunisationprogram 171120044520Document22 pagesUniversalimmunisationprogram 171120044520Gagan GargNo ratings yet
- Yellow Fever DeclineDocument10 pagesYellow Fever Declinecalvinmagara1307No ratings yet
- Preparing For The Coronavirus Disease COVID19 Vaccination Evidence Plans and ImplicationsJournal of Korean Medical ScienceDocument20 pagesPreparing For The Coronavirus Disease COVID19 Vaccination Evidence Plans and ImplicationsJournal of Korean Medical Sciencecarla laureanoNo ratings yet
- WebpdfDocument471 pagesWebpdfyogui1965No ratings yet
- Childhood Immunization in Pakistan: Salient PointsDocument3 pagesChildhood Immunization in Pakistan: Salient PointsTanveer SajidNo ratings yet
- 1642214359314013Document6 pages1642214359314013cersei.seri.sera.10No ratings yet
- Cvs Adjustments During Exercise by DR Sadia ZafarDocument23 pagesCvs Adjustments During Exercise by DR Sadia ZafarMudassar RoomiNo ratings yet
- CyclophosphamideDocument3 pagesCyclophosphamideChen Boon TeyNo ratings yet
- Pathophysiology of Our Case Study Viral Myocarditis Secondary To Dengue FeverDocument2 pagesPathophysiology of Our Case Study Viral Myocarditis Secondary To Dengue FevercarmaxetaNo ratings yet
- Classification On Mammography-Ultrasound 21 Sept BaruDocument319 pagesClassification On Mammography-Ultrasound 21 Sept BaruAswin ChristantoNo ratings yet
- BCPSDocument7 pagesBCPSdrmohaddes hossainNo ratings yet
- BIFIDOBACTERIUMDocument22 pagesBIFIDOBACTERIUMShashi Sharma100% (2)
- Fever With RashDocument48 pagesFever With RashAnand VermaNo ratings yet
- Ocular Manifestation of Systemic DiseasesDocument58 pagesOcular Manifestation of Systemic DiseasesUmar AzlanNo ratings yet
- Cap 88-7 Fanaroff & Martin's Neonatal Perinatal Medicine (11-22)Document12 pagesCap 88-7 Fanaroff & Martin's Neonatal Perinatal Medicine (11-22)AlejandraSevillaNo ratings yet
- Malignant MelanomaDocument31 pagesMalignant MelanomakityamuwesiNo ratings yet
- Congential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersDocument7 pagesCongential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersNichole CollinsNo ratings yet
- Brain Case Studies AssignmentDocument6 pagesBrain Case Studies AssignmentBrianNo ratings yet
- Reiki GuidelinesDocument2 pagesReiki Guidelinesgold starNo ratings yet
- Mapeh-10 Quater 1 ExamDocument5 pagesMapeh-10 Quater 1 ExamKIRBY ANN GALABINNo ratings yet
- Meanma Maligna PDFDocument4 pagesMeanma Maligna PDFNur Aisyah Soedarmin IieychaNo ratings yet
- Capstone Project Desktop Version 270519Document22 pagesCapstone Project Desktop Version 270519api-385688041No ratings yet
- SIGN Data Collection SheetsDocument6 pagesSIGN Data Collection Sheetsasi basseyNo ratings yet
- Goljan Transcribed NotesDocument59 pagesGoljan Transcribed NotesJiyeon JeonNo ratings yet
- Eye & Ear IrrigationDocument34 pagesEye & Ear IrrigationdaisyNo ratings yet
- Perianesthesia Nursing Core Curriculum e Book Preprocedure Phase I and Phase II Pacu Nursing Ebook PDF VersionDocument62 pagesPerianesthesia Nursing Core Curriculum e Book Preprocedure Phase I and Phase II Pacu Nursing Ebook PDF Versionronald.robotham754100% (45)
- Anabolic Androgenic SteroidsDocument70 pagesAnabolic Androgenic Steroidsfaqed ilzakira100% (2)
- ACT274Document6 pagesACT274Verónica SilveriNo ratings yet
- Book Reviews: Diagnostic Handbook of OtorhinolaryngologyDocument1 pageBook Reviews: Diagnostic Handbook of OtorhinolaryngologyVernika AngelinaNo ratings yet
- Isbb Post Test 200 Items Uph Isabela 2docx 240215 235725Document15 pagesIsbb Post Test 200 Items Uph Isabela 2docx 240215 235725thegr8 GNo ratings yet
- Treatment Irritable Bowel SyndromeDocument2 pagesTreatment Irritable Bowel SyndromeCésar AndraskiNo ratings yet
- Drugs of Abuse: Reymark C. Adorada MAPEH TeacherDocument40 pagesDrugs of Abuse: Reymark C. Adorada MAPEH Teacherreymark adoradaNo ratings yet
- 17.2 Inheritance Igcse Cie Biology Ext Theory QPDocument11 pages17.2 Inheritance Igcse Cie Biology Ext Theory QPivannn510510No ratings yet