Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
264 viewsLiver Cancer
Liver Cancer
Uploaded by
Joyce Ann CumlatThe liver document discusses the diagnosis and treatment of primary and secondary liver cancers. It notes that the liver is the largest solid organ located in the right side of the abdomen. Primary liver cancers include hepatocellular carcinoma and cholangiocarcinoma. Secondary cancers often spread to the liver from the lung, kidney, breast, or intestines. Diagnosis involves blood tests, imaging like CT/MRI, and biopsy. Treatment depends on cancer type and stage but may include surgery, radiation, chemotherapy, embolization, or liver transplantation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Gastritis PPTDocument86 pagesGastritis PPTWayan Hery75% (4)
- Colorectal CancerDocument3 pagesColorectal CancerAriane May Rubio50% (2)
- Colorectal CancerDocument14 pagesColorectal Cancershaqtim100% (2)
- Ewing's SarcomaDocument16 pagesEwing's SarcomaChacha Zakiya100% (1)
- Case Study Colorectal CancerDocument23 pagesCase Study Colorectal CancerLeogalvez BedanoNo ratings yet
- A Case Study On Rectal AdenocarcinomaDocument62 pagesA Case Study On Rectal AdenocarcinomaEyySiEffVee100% (1)
- Crohn's DiseaseDocument46 pagesCrohn's Diseaseuttarasingh100% (3)
- Liver CancerDocument2 pagesLiver CancerPrincess Barnuevo100% (2)
- Colorectal CancerDocument7 pagesColorectal Cancerjames garciaNo ratings yet
- Casestudy Gastric CarcinomaDocument53 pagesCasestudy Gastric CarcinomaAngelaTrinidadNo ratings yet
- AML Case StudyDocument66 pagesAML Case StudyNoel Christian PeraltaNo ratings yet
- 13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsDocument31 pages13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsRena SafitriNo ratings yet
- Liver CancerDocument16 pagesLiver CancerMark James MelendresNo ratings yet
- Case Study Mastectomy RevisedDocument13 pagesCase Study Mastectomy RevisedJessa BorreNo ratings yet
- Mastectomy (Case Analysis)Document7 pagesMastectomy (Case Analysis)Lester_Ocuaman_2248No ratings yet
- Prostatectomy: Surgical Prostate Gland Tumour Urine UrethraDocument36 pagesProstatectomy: Surgical Prostate Gland Tumour Urine Urethranosebleed_ms3691100% (1)
- Mastectomy Case StudyDocument9 pagesMastectomy Case StudyAura Regene AtienzaNo ratings yet
- Case Study MastectomyDocument26 pagesCase Study MastectomyIcheAnne Nilay100% (2)
- Final EditDocument43 pagesFinal EditMary Rose LinatocNo ratings yet
- Cholecystectomy (: Laparoscopic GallstonesDocument4 pagesCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalNo ratings yet
- PANCREATITISDocument38 pagesPANCREATITISVEDHIKAVIJAYANNo ratings yet
- ABDOMINAL ObjectiveDocument9 pagesABDOMINAL ObjectiveXing-Jin RomeroNo ratings yet
- Ortho Case StudyDocument17 pagesOrtho Case StudyAndrea Sibayan SorianoNo ratings yet
- Lung CancerDocument2 pagesLung CancerAurea Jasmine DacuycuyNo ratings yet
- Hiatal Hernia AchalasiaDocument22 pagesHiatal Hernia AchalasiaDhen MarcNo ratings yet
- Casereport-Modified Radical MastectomyDocument33 pagesCasereport-Modified Radical MastectomyMayflor de LunaNo ratings yet
- Rectal CarcinomaDocument16 pagesRectal Carcinomabuddy557No ratings yet
- Benign Tumors of The StomachDocument55 pagesBenign Tumors of The Stomachapi-19641337No ratings yet
- Treatments and Drugs: by Mayo Clinic StaffDocument23 pagesTreatments and Drugs: by Mayo Clinic StaffJr D BayzNo ratings yet
- Prostate CancerDocument6 pagesProstate CancerfheisanzNo ratings yet
- 2 Acute CholecystitisDocument21 pages2 Acute CholecystitisEtteh MaryNo ratings yet
- Open CholecystectomyDocument7 pagesOpen CholecystectomyMonique CastroNo ratings yet
- Pancretic Cancer Case Study - BurkeDocument52 pagesPancretic Cancer Case Study - Burkeapi-282999254No ratings yet
- Case Study CholecystitisDocument27 pagesCase Study CholecystitisBandana RajpootNo ratings yet
- Cancer CaDocument6 pagesCancer CaRocco WalksNo ratings yet
- CholecystectomyDocument6 pagesCholecystectomyTom Bayubs-tucsNo ratings yet
- Skin Cancer: I. Overview of The DisorderDocument3 pagesSkin Cancer: I. Overview of The DisorderSung ChiiNo ratings yet
- Example Case StudyDocument7 pagesExample Case StudyTerrena Lyn BlackmanNo ratings yet
- By: Vismin Prince Magno: Liver CancerDocument17 pagesBy: Vismin Prince Magno: Liver Cancerhedokido100% (1)
- Cancer Case StudyDocument15 pagesCancer Case StudyRobin HaliliNo ratings yet
- Seminar On MastectomyDocument8 pagesSeminar On Mastectomypooja singhNo ratings yet
- Peritoneal Carcinomatosis Grand Case StudyDocument69 pagesPeritoneal Carcinomatosis Grand Case StudyBeverly Joy RubiNo ratings yet
- Prostate CancerDocument19 pagesProstate CancersamwelNo ratings yet
- B. Pathophysiology: Clinical Aspects of Cancer DiagnosisDocument10 pagesB. Pathophysiology: Clinical Aspects of Cancer DiagnosisAbigael Patricia GutierrezNo ratings yet
- Liver CancerDocument28 pagesLiver CancerHealth Education Library for PeopleNo ratings yet
- Choledocholithiasis: A Case Study ofDocument5 pagesCholedocholithiasis: A Case Study ofJanelle Kate SaleNo ratings yet
- HBV HCV Cirrhosis Gender Perinatal Transmission Age Family HX RaceDocument2 pagesHBV HCV Cirrhosis Gender Perinatal Transmission Age Family HX RaceKaycee TolingNo ratings yet
- Prostatic CancerDocument4 pagesProstatic CancerParixit DasNo ratings yet
- Colon CancerDocument17 pagesColon CancerYaska MusaNo ratings yet
- Breast CancerDocument24 pagesBreast CancerElvis DuotNo ratings yet
- Esophageal CancerDocument40 pagesEsophageal Cancerapi-282115150No ratings yet
- Ovarian New GrowthDocument7 pagesOvarian New GrowthRegiena Tamargo100% (1)
- Lung Ca Case Presentation PDFDocument28 pagesLung Ca Case Presentation PDFapi-276417422100% (2)
- Colorectal CancerDocument8 pagesColorectal Cancerjorgeacct100% (3)
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- RAFIN - Management of The Client With Cervical - Ovarian-Cancer and HysterectomyDocument12 pagesRAFIN - Management of The Client With Cervical - Ovarian-Cancer and HysterectomyCezanne CruzNo ratings yet
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Liver CancerDocument44 pagesLiver CancerEjay Jacob Ricamara50% (2)
- Jordanian Surgical Society - PPT LastDocument166 pagesJordanian Surgical Society - PPT LastNessreen Jamal100% (1)
- Cancer of LiverDocument14 pagesCancer of LiverRani SujithNo ratings yet
- Multiple Sclerosis 1Document31 pagesMultiple Sclerosis 1Joyce Ann CumlatNo ratings yet
- Ii. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Document6 pagesIi. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Joyce Ann CumlatNo ratings yet
- PATHOPHYSIOLOGYDocument5 pagesPATHOPHYSIOLOGYJoyce Ann CumlatNo ratings yet
- Gland (Or Hypophysis), A Bean-Sized Organ Suspended From It by A Stem CalledDocument3 pagesGland (Or Hypophysis), A Bean-Sized Organ Suspended From It by A Stem CalledJoyce Ann CumlatNo ratings yet
- Digestion and The Digestive SystemDocument4 pagesDigestion and The Digestive SystemIzelwyn DaguioNo ratings yet
- Abdominal PainDocument7 pagesAbdominal PainKartikey ChauhanNo ratings yet
- Liver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisDocument35 pagesLiver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisMohd Johari Mohd ShafuwanNo ratings yet
- Helminth Revision 2Document1 pageHelminth Revision 2FarlogyNo ratings yet
- Chapter 006Document42 pagesChapter 006api-263755297No ratings yet
- Anatomy of StomachDocument58 pagesAnatomy of StomachSkinny tuberNo ratings yet
- Resume Ebrahim RadinniaDocument2 pagesResume Ebrahim RadinniaSepideh MirzaeiNo ratings yet
- Major Organs of The Human Body:: Stomach and IntestinesDocument12 pagesMajor Organs of The Human Body:: Stomach and IntestinesMiraNo ratings yet
- Bile Duct InjuryDocument62 pagesBile Duct InjuryShashidhara Puttaraj100% (1)
- 3.3 ColicDocument3 pages3.3 ColicGeorges Ramon Livio ProdigsonNo ratings yet
- Alumy SuspensiDocument5 pagesAlumy SuspensiThytin MartHa PeliYanNo ratings yet
- Ulcerative ColitisDocument5 pagesUlcerative ColitisVenice Jame SanchezNo ratings yet
- The Digestive SystemDocument3 pagesThe Digestive SystemabcNo ratings yet
- NGT FeedingDocument8 pagesNGT FeedingSheng GosepNo ratings yet
- Update On DiarrheaDocument12 pagesUpdate On DiarrheantnquynhproNo ratings yet
- Jaundice 23-24pdfDocument25 pagesJaundice 23-24pdfmyarjddbzNo ratings yet
- Abdominal ExaminationDocument56 pagesAbdominal ExaminationAnggreani PutriNo ratings yet
- Chapter 6 NutritionDocument101 pagesChapter 6 NutritionNUR FAEZAHNo ratings yet
- Quiz 4Document12 pagesQuiz 4abezareljvenNo ratings yet
- NCM 116Document32 pagesNCM 116Yeany IddiNo ratings yet
- Drug StudyDocument9 pagesDrug StudyJonica CamposNo ratings yet
- Digestive System Lesson Plan SCDocument5 pagesDigestive System Lesson Plan SCJustine PamaNo ratings yet
- CSEC Biology DigestionDocument53 pagesCSEC Biology DigestionKemoy FrancisNo ratings yet
- 6 Day Pediatric PancreatitisDocument16 pages6 Day Pediatric PancreatitisShreyash Haritwal100% (1)
- Anatomi Radiologi Barium Studies For GITDocument52 pagesAnatomi Radiologi Barium Studies For GITRio ArbiansyahNo ratings yet
- Inflammtory Bowel Disease (Ibd)Document30 pagesInflammtory Bowel Disease (Ibd)SnehaNo ratings yet
- The Digestive System Parts and FunctionsDocument6 pagesThe Digestive System Parts and FunctionsDixie MerinNo ratings yet
- Vagus Indigestionعسر الهضم المسبب باصابة العصب الحائرDocument27 pagesVagus Indigestionعسر الهضم المسبب باصابة العصب الحائرAli H. Sadiek أ.د. علي حسن صديق100% (3)
Liver Cancer
Liver Cancer
Uploaded by
Joyce Ann Cumlat0 ratings0% found this document useful (0 votes)
264 views44 pagesThe liver document discusses the diagnosis and treatment of primary and secondary liver cancers. It notes that the liver is the largest solid organ located in the right side of the abdomen. Primary liver cancers include hepatocellular carcinoma and cholangiocarcinoma. Secondary cancers often spread to the liver from the lung, kidney, breast, or intestines. Diagnosis involves blood tests, imaging like CT/MRI, and biopsy. Treatment depends on cancer type and stage but may include surgery, radiation, chemotherapy, embolization, or liver transplantation.
Original Description:
Original Title
207139670-Liver-Cancer-Ppt
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe liver document discusses the diagnosis and treatment of primary and secondary liver cancers. It notes that the liver is the largest solid organ located in the right side of the abdomen. Primary liver cancers include hepatocellular carcinoma and cholangiocarcinoma. Secondary cancers often spread to the liver from the lung, kidney, breast, or intestines. Diagnosis involves blood tests, imaging like CT/MRI, and biopsy. Treatment depends on cancer type and stage but may include surgery, radiation, chemotherapy, embolization, or liver transplantation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
264 views44 pagesLiver Cancer
Liver Cancer
Uploaded by
Joyce Ann CumlatThe liver document discusses the diagnosis and treatment of primary and secondary liver cancers. It notes that the liver is the largest solid organ located in the right side of the abdomen. Primary liver cancers include hepatocellular carcinoma and cholangiocarcinoma. Secondary cancers often spread to the liver from the lung, kidney, breast, or intestines. Diagnosis involves blood tests, imaging like CT/MRI, and biopsy. Treatment depends on cancer type and stage but may include surgery, radiation, chemotherapy, embolization, or liver transplantation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 44
The liver is the largest solid organ of the body.
It is located on the right side of the abdomen.
The liver is triangular in shape and is divided into a
right and left lobe, the right lobe being the larger of
the two.
It provides several important functions to the body
including:
Filtering the blood to remove and process toxins.
Synthesizing and excreting bile, which is important in
processing fat from our diet.
Helping regulate blood sugar (glucose) levels.
Producing factors that play an important role in blood
clotting.
Prognosis is poor, with overall 5-year survival
of 5%.
If untreated , death occurs in 6-8 weeks
Most common presenting
symptom is right upper quadrant
abdominal pain, usually dull or
aching and may radiate to the
right shoulder.
Right upper quadrant mass,
abdominal distention, fever,
malaise, weight loss, and
anorexia become evident.
Jaundice is present in few
patients at diagnosis in primary
liver cancer. In
cholangiocarcinoma, the
presenting symptom is usually
obstructive jaundice.
If there is portal vein obstruction,
ascites and esophageal varices
occour.
Serum, bilirubin, alkaline phosphatase, and serum
transaminases are all increased.
Alpha-fetoprotein: Principal tumor marker for
hepatocellular carcinoma – elevated in 70% to 95% of
patients with the disease.
Ultrasonography, computed tomography (CT), and
magnetic resonance imaging (MRI) are used to detect
cancer and assess if the tumor can be surgically
removed.
Arteriography helps determine resectability of liver
tumor.
Percutaneous needle biopsy or biopsy through
ultrasonography may be done.
Laparoscopy with liver biopsy may be performed.
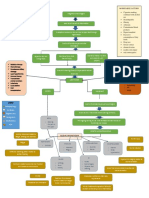
1. Choice of treatment depends on
Whether tumor is primary or secondary
Type and extent of tumor
Concomitant diseases
Liver functions
Patient status
2.Pretreatment therapy
Anemia, clotting deficits, and fluid and
electrolyte abnormalities should be corrected
Vitamin A, C, D, and B complex can reduce
effect of jaundice
Pruritus can be relieved with good hygiene
and by avoiding products that dry skin and by
using oil-based lotions, antihistamines;
cholestyramine
Nutritional improvement is critical
Cancer that starts in the liver.
There are two main types:
Hepatocellular carcinoma (HCC) – starts in the
main cell of the liver (hepatocytes).
Cholangiocarcinoma – starts in the bile duct.
Hepatocellular carcinoma (HCC) is by far the
most common type of primary liver cancer.
Primary liver tumors usually are associated with
chronic liver disease, hepatitis B and C
infections, and cirrhosis.
Angiosarcoma is a rare liver cancer starting in
the blood vessels.
Liver cancer is much common particularly in
sub-Saharan Africa and Southeast Asia.
Liver cancer is the fifth most common cancer.
Metastases are often from:
Lung
Kidney
Breast
Intestinal tract
Infection with Hepatitis B
Liver scarring (cirrhosis) due to Hepatitis B or
C, inflammation or genetic disorders such as
haemochromatosis or alpha 1-antitrypsin
deficiency
Alcohol drinking over a long period of time
Diabetes
Smoking
High-fat diet
Being overweight or obese
Cancer that starts in other part of the body but has spread
(metastasized) to the liver.
Most common types to spread to the liver start I the
digestive sytem:
Bowel
Pancreas
Esophagus
Stomach
Others that also commonly spread to the liver:
Breast
Ovary
Kidney
Lung
Secondary cancer is sometimes found at he same time that
the primary cancer is diagnosed.
Sometimes he primary cancer can’t b
found, this is known as Cancer of
Unknown Primary (CUP).
The early manifestations of malignancy of the liver
include:
Pain
Continuous dull ache in the right upper quadrant,
epigastrium, or back
Weight loss
Loss of strength
Anorexia
Anemia
The liver may be enlarged and irregular on palpation.
Jaundice is present (only if the larger bile ducts are
occluded by the pressure of malignant nodules obstruct
the portal veins of if tumor tissue is seeded in the
peritoneal cavity.)
Metastases from other primary sites are
found in the liver in about half of all advanced
cancer cases (Bacon & Di Bisceglie, 2000).
By way of portal systems or lymphatic
channels, or by direct extension from an
abdominal tumor, malignant tumors are likely
to reach the liver eventually.
The liver apparently is an ideal place for these
malignant cells to thrive.
The liver cancer diagnosis is based on:
Clinical signs and symptoms
History
Physical examination
Results of laboratory
X-ray studies
Increased serum levels of bilirubin, alkaline
phosphatase, AST, GGT, and lactic
dehydrogenase may occur.
Leukocytosis (increased white blood cells).
Erythrocytosis (increased red blood cells).
Hypercalcemia, hypoglycemia, and
hypocholesterolemia may also be seen on
laboratory assessment.
There are two markers that are useful to
distinguish between metastatic liver disease
and primary liver cancer:
The serum level of alpha fetoprotein (AFP),
which serves as a tumor marker.
Levels of carciembryonic antigen (CEA), a
marker of advanced cancer of the digestive
tract, maybe elevated.
X-rays
Liver scans
CT scans
Ultrasound studies
MRI
Arteriography
Laparoscopy
Confirmation of a tumor’s histology can be
made by biopsy under imaging guidance (CT
scan or ultrasound) or laparoscopically.
Local or systemic dissemination of the tumor
by needle biopsy or refine-needle biopsy can
occur but is rare.
Primary HCC diagnosis should be confirmed
by frozen section at the time of laparotomy.
Radiation therapy and chemotherapy have
been used in treating cancer of the liver with
varying degrees of success.
The use of external beam radiation for the
treatment of liver tumors has been limited by
the radiosensitivity of normal hepatocytes.
More effective ways of delivering radiations to
tumors of the liver include:
Intravenous or intraarterial injections of
antibodies tagged with radioactive isotopes that
specifically attack tumor-associated antigens.
Percutaneous placement of a high-intensity
source for interstitial radiation therapy.
Chemotherapy has been used to improve
quality of life and pro-long survival.
May also be used as a therapy after surgical
resection of hepatic tumors.
Systemic chemotherapy and regional
infusion are used to administer antineoplastic
agents.
An implantable pump is used to deliver high-
concentration chemotherapy to the liver
through the hepatic artery.
Percutaneous biliary drainage is used to bypass
biliary ducts obstructed by the liver, pancreatic,
or bile ducts in patients with inoperable tumors
or those who are poor surgical risks.
Complications include sepsis, leakage of bile,
hemorrhage, and reobstruction of the biliary
system.
Observe patient for fever and chills, bile
drainage around the catheter, changes in vital
signs, and evidence of biliary obstruction,
including increased pain or pressure, pruritus,
and recurrence of jaundice.
Hyperthermia: heat by laser or radiofrequency
energy is directed to tumors to cause necrosis of
the tumors while sparing normal tissue.
Cryosurgery is a newer treatment modality.
Embolization of arterial blood flow to the tumor;
effective in small tumors; injection of small
particulate embolic or chemotherapeutic agents
may be used to cause tumor necrosis.
Immunotherapy: lymphocytes with antitumor
reactivity are administered.
Surgical resection is a treatment of choice when HCC is
confined to one lobe of the liver
When the primary site can be completely excised &
metastasis is limited, hepatic resection can be performed
Metastases to the liver are rarely limited or solitary
Surgeons have capitalized on the regenerative capacity of
the liver cells removing 90% of it
The presence of cirrhosis limits the ability of the liver to
regenerate
Staging of liver tumors aid in predicting the chances of
surgical cure
Nutritional, fluid and general physical status is assessed in
preparation for a surgery
Patients aided psychologically in preparing for the surgery
Extensive diagnostic studies may be performed
as well as Specific studies that may include:
Liver scans
Liver biopsy
Cholangiography
Selective Hepatic angiography
Percutaneous needle biopsy
Peritoneoscopy
Laparoscopy
Ultrasound
CT scans
MRI
Blood tests, Particularly determinations of
serum alkaline phosphate, AST, and GGT
Primary tumor (T)
TX- Primary tumor
To- No evidence of primary tumor
T1-Solitary tumor without vascular invasion
T2-Solitary tumor without vascular invasion or
multiple tumors
-none more than 5 cm
T3-Multiple tumors more than 5 cm or tumor
involving a major branch of the portal or hepatic
vein(s)
T4-Tumor(s) with direct invasion of adjacent organs
other than the gallbladder or with perforation of
visceral peritoneum
NX -Regional lymph nodes cannot be
assessed
N0 -No regional lymph node metastasis
N1 -Regional lymph node metastasis
Mx -Distant metastasis cannot be assessed
Mo -No distant metastasis
M1 -Distant Metastasis
Stage I T1 No Mo
Stage II T2 No Mo
Stage IIIA T3 No Mo
Stage IIIB T4 No Mo
Stage IIIC Any T N1 Mo
Stage IV Any T Any N M1
Removal of a lobe of
the liver is the most
common surgical
procedure.
For right liver
lobectomy or an
extended right
lobectomy a
thoracoabdominal
incision wll be used.
An extensive
abdominal incision is
made for a left
lobectomy.
Cyrosurgery
(cyroablation), tumors
are destroyed by liquid
itrogen at -196⁰C.
This technique ha been
used alone.
Its efficacy is still being
evaluated
Procedure involves total removal of the
diseased liver and its replacement with
a healthy liver in the same anatomic
location (orthotopic liver
transplantation [OLT]).
It is not a routine procedure and it may
be accompanied by complications.
Recurrence of primary liver malignancy
has been reported.
The patient with small tumors may
have a good prognosis after
transplantation.
Established therapeutic modality rather
than experimental procedure to treat
these disorders.
To prepare the patient and family for
liver transplantation, nurses in all
settings must understand the process
and procedure of liver transplantation.
The postoperative complication rate is high
because of technical complications or
infections.
Immediate postoperative complications may
include:
Bleeding – common in postoperative period
Infection – leading cause f death in liver
transplantation.
Rejection – a key concern.
Assess for problems related to
cardiopulmonary involvement, vascular
complications, and respiratory and liver
dysfunction.
Give careful attention to metabolic
abnormalities (glucose, protein, and lipids).
Provide close monitoring and care for the first 2
or 3 days.
Encourage early ambulation, and initiate other
postoperative care measures.
Closely monitor the patient undergoing
cryosurgery for hypothermia, hemorrhage, bile
leak, and myoglobinuria.
Instruct patient about the importance of follow-
up visits.
Encourage patient to resume activities as soon
as possible, but caution patient to avoid
activities that may damage the pump.
Teach patient about signs of complications,
and encourage patient to notify nurse or
physician if problems or questions occur.
Provide reassurance and instructions to
patient and family to reduce fear.
Refer patient for home care.
Assist patient and family in making decisions
about hospice care, and initiate referrals.
Encourage patient to discuss end-of-life care.
Therapeutic Interventions
Radiation therapy can help reduce pain and
discomfort.
Liver cancer is radiosensitive, but treatment
is restricted by the limited radiation tolerance
of normal liver.
Hyperthermia has been used to treat hepatic
metastases.
Management of ascites and edema through
fluid restriction, albumin, and diuretics.
Chemotherapy is used as an adjuvant therapy
after surgical resection of liver cancer.
Systemic chemotherapy is the only treatment
applicable once the cancer has spread outside the
liver.
Regional infusion chemotherapy by implantable
pump has been used to deliver a high concentration of
chemotherapy directly to the liver through the
hepatic artery.
Hepatic artery occlusion and embolization with
chemotherapeutic agents is another possible
method.
Immunotherapy is currently under investigation.
Surgery is the best treatment but is only feasible in
25% of cases, after extent of tumor and hepatic
reserve have been considered.
Surgical resection may be along anatomic divisions of
the liver or nonanatomic resections.
Freezing hepatic tumors by cryosurgery is a new
modalilty that preserves normal liver.
Liver transplantation has been performed to treat
liver tumors, but results have been poor because of
the high rate of recurrent primary liver malignancy. It
is now recommended that the patient be treated
before and after transplantation with chemotherapy
and radiation therapy.
Percutaneous transhepatic biliary drainage
(PTBD) is used to drain obstructed biliary ducts
in patients with inoperable tumors or in patients
considered poor surgical risks. A percutaneous
catheter drains the biliary tree to relieve
jaundice, decrease pruritus, and decrease
anorexia.
Percutaneous or endoscopic placement of
internal stents may also be used as palliative
treatment for a patient with obstructed bile
ducts with a terminal diagnosis.
Assess the patient’s response to pain control
measures.
Monitor vital signs, intake and output, and daily
weights to detect fluid balance.
Measure and record abdominal girth daily.
Monitor laboratory values for liver function.
Note subtle changes in mental status indicating
hepatic encephalopathy.
Monitor for signs of malnutrition, including
weight loss, loss of strength, anemia.
Administer pain control agents as ordered, keeping in
mind decreased liver metabolism. Monitor signs of drug
toxicity.
Provide nonpharmacologic methods of pain relief, such as
massage and guided imagery.
Position the patient for comfort – usually in semi –
Fowler’s position.
Encourage the patient to eat small meals and
supplementary liquid feedings.
Asses and report factors that may increase nutritional
needs: Increased body temperature, pain, signs of
infection, stress level. Encourage additional calories as
tolerated.
Restrict sodium and fluid intake as prescribed.
If the patient has PTBD, monitor catheter exit site for
bleeding or bile drainage, and asses drainage in bag
for color, amount, consistency. The drainage initially
may have some blood mixed with bile but should clear
within a few hours.
Flush catheter if ordered
Check for and report signs of peritonitis from bile leaking
into abdomen: Fever, chills, abdominal pain and
tenderness, distention.
Provide psychological support to patient and family to
help them cope with uncertain prognosis.
Instruct the patient and family on preparation
for surgery, reinforcement and clarify proposed
surgical procedure, and review postoperative
instructions.
Instruct the patient to recognize and report signs
and symptoms of complication.
Instruct the patient in continued surveillance for
recurrence.
Instruct the patient and family in care of any
tubes or drains.
You might also like
- Gastritis PPTDocument86 pagesGastritis PPTWayan Hery75% (4)
- Colorectal CancerDocument3 pagesColorectal CancerAriane May Rubio50% (2)
- Colorectal CancerDocument14 pagesColorectal Cancershaqtim100% (2)
- Ewing's SarcomaDocument16 pagesEwing's SarcomaChacha Zakiya100% (1)
- Case Study Colorectal CancerDocument23 pagesCase Study Colorectal CancerLeogalvez BedanoNo ratings yet
- A Case Study On Rectal AdenocarcinomaDocument62 pagesA Case Study On Rectal AdenocarcinomaEyySiEffVee100% (1)
- Crohn's DiseaseDocument46 pagesCrohn's Diseaseuttarasingh100% (3)
- Liver CancerDocument2 pagesLiver CancerPrincess Barnuevo100% (2)
- Colorectal CancerDocument7 pagesColorectal Cancerjames garciaNo ratings yet
- Casestudy Gastric CarcinomaDocument53 pagesCasestudy Gastric CarcinomaAngelaTrinidadNo ratings yet
- AML Case StudyDocument66 pagesAML Case StudyNoel Christian PeraltaNo ratings yet
- 13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsDocument31 pages13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsRena SafitriNo ratings yet
- Liver CancerDocument16 pagesLiver CancerMark James MelendresNo ratings yet
- Case Study Mastectomy RevisedDocument13 pagesCase Study Mastectomy RevisedJessa BorreNo ratings yet
- Mastectomy (Case Analysis)Document7 pagesMastectomy (Case Analysis)Lester_Ocuaman_2248No ratings yet
- Prostatectomy: Surgical Prostate Gland Tumour Urine UrethraDocument36 pagesProstatectomy: Surgical Prostate Gland Tumour Urine Urethranosebleed_ms3691100% (1)
- Mastectomy Case StudyDocument9 pagesMastectomy Case StudyAura Regene AtienzaNo ratings yet
- Case Study MastectomyDocument26 pagesCase Study MastectomyIcheAnne Nilay100% (2)
- Final EditDocument43 pagesFinal EditMary Rose LinatocNo ratings yet
- Cholecystectomy (: Laparoscopic GallstonesDocument4 pagesCholecystectomy (: Laparoscopic GallstonesAlexia BatungbacalNo ratings yet
- PANCREATITISDocument38 pagesPANCREATITISVEDHIKAVIJAYANNo ratings yet
- ABDOMINAL ObjectiveDocument9 pagesABDOMINAL ObjectiveXing-Jin RomeroNo ratings yet
- Ortho Case StudyDocument17 pagesOrtho Case StudyAndrea Sibayan SorianoNo ratings yet
- Lung CancerDocument2 pagesLung CancerAurea Jasmine DacuycuyNo ratings yet
- Hiatal Hernia AchalasiaDocument22 pagesHiatal Hernia AchalasiaDhen MarcNo ratings yet
- Casereport-Modified Radical MastectomyDocument33 pagesCasereport-Modified Radical MastectomyMayflor de LunaNo ratings yet
- Rectal CarcinomaDocument16 pagesRectal Carcinomabuddy557No ratings yet
- Benign Tumors of The StomachDocument55 pagesBenign Tumors of The Stomachapi-19641337No ratings yet
- Treatments and Drugs: by Mayo Clinic StaffDocument23 pagesTreatments and Drugs: by Mayo Clinic StaffJr D BayzNo ratings yet
- Prostate CancerDocument6 pagesProstate CancerfheisanzNo ratings yet
- 2 Acute CholecystitisDocument21 pages2 Acute CholecystitisEtteh MaryNo ratings yet
- Open CholecystectomyDocument7 pagesOpen CholecystectomyMonique CastroNo ratings yet
- Pancretic Cancer Case Study - BurkeDocument52 pagesPancretic Cancer Case Study - Burkeapi-282999254No ratings yet
- Case Study CholecystitisDocument27 pagesCase Study CholecystitisBandana RajpootNo ratings yet
- Cancer CaDocument6 pagesCancer CaRocco WalksNo ratings yet
- CholecystectomyDocument6 pagesCholecystectomyTom Bayubs-tucsNo ratings yet
- Skin Cancer: I. Overview of The DisorderDocument3 pagesSkin Cancer: I. Overview of The DisorderSung ChiiNo ratings yet
- Example Case StudyDocument7 pagesExample Case StudyTerrena Lyn BlackmanNo ratings yet
- By: Vismin Prince Magno: Liver CancerDocument17 pagesBy: Vismin Prince Magno: Liver Cancerhedokido100% (1)
- Cancer Case StudyDocument15 pagesCancer Case StudyRobin HaliliNo ratings yet
- Seminar On MastectomyDocument8 pagesSeminar On Mastectomypooja singhNo ratings yet
- Peritoneal Carcinomatosis Grand Case StudyDocument69 pagesPeritoneal Carcinomatosis Grand Case StudyBeverly Joy RubiNo ratings yet
- Prostate CancerDocument19 pagesProstate CancersamwelNo ratings yet
- B. Pathophysiology: Clinical Aspects of Cancer DiagnosisDocument10 pagesB. Pathophysiology: Clinical Aspects of Cancer DiagnosisAbigael Patricia GutierrezNo ratings yet
- Liver CancerDocument28 pagesLiver CancerHealth Education Library for PeopleNo ratings yet
- Choledocholithiasis: A Case Study ofDocument5 pagesCholedocholithiasis: A Case Study ofJanelle Kate SaleNo ratings yet
- HBV HCV Cirrhosis Gender Perinatal Transmission Age Family HX RaceDocument2 pagesHBV HCV Cirrhosis Gender Perinatal Transmission Age Family HX RaceKaycee TolingNo ratings yet
- Prostatic CancerDocument4 pagesProstatic CancerParixit DasNo ratings yet
- Colon CancerDocument17 pagesColon CancerYaska MusaNo ratings yet
- Breast CancerDocument24 pagesBreast CancerElvis DuotNo ratings yet
- Esophageal CancerDocument40 pagesEsophageal Cancerapi-282115150No ratings yet
- Ovarian New GrowthDocument7 pagesOvarian New GrowthRegiena Tamargo100% (1)
- Lung Ca Case Presentation PDFDocument28 pagesLung Ca Case Presentation PDFapi-276417422100% (2)
- Colorectal CancerDocument8 pagesColorectal Cancerjorgeacct100% (3)
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- RAFIN - Management of The Client With Cervical - Ovarian-Cancer and HysterectomyDocument12 pagesRAFIN - Management of The Client With Cervical - Ovarian-Cancer and HysterectomyCezanne CruzNo ratings yet
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Liver CancerDocument44 pagesLiver CancerEjay Jacob Ricamara50% (2)
- Jordanian Surgical Society - PPT LastDocument166 pagesJordanian Surgical Society - PPT LastNessreen Jamal100% (1)
- Cancer of LiverDocument14 pagesCancer of LiverRani SujithNo ratings yet
- Multiple Sclerosis 1Document31 pagesMultiple Sclerosis 1Joyce Ann CumlatNo ratings yet
- Ii. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Document6 pagesIi. Pathophysiology Causative Agents:: Alternative Learning Activities Level 3Joyce Ann CumlatNo ratings yet
- PATHOPHYSIOLOGYDocument5 pagesPATHOPHYSIOLOGYJoyce Ann CumlatNo ratings yet
- Gland (Or Hypophysis), A Bean-Sized Organ Suspended From It by A Stem CalledDocument3 pagesGland (Or Hypophysis), A Bean-Sized Organ Suspended From It by A Stem CalledJoyce Ann CumlatNo ratings yet
- Digestion and The Digestive SystemDocument4 pagesDigestion and The Digestive SystemIzelwyn DaguioNo ratings yet
- Abdominal PainDocument7 pagesAbdominal PainKartikey ChauhanNo ratings yet
- Liver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisDocument35 pagesLiver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisMohd Johari Mohd ShafuwanNo ratings yet
- Helminth Revision 2Document1 pageHelminth Revision 2FarlogyNo ratings yet
- Chapter 006Document42 pagesChapter 006api-263755297No ratings yet
- Anatomy of StomachDocument58 pagesAnatomy of StomachSkinny tuberNo ratings yet
- Resume Ebrahim RadinniaDocument2 pagesResume Ebrahim RadinniaSepideh MirzaeiNo ratings yet
- Major Organs of The Human Body:: Stomach and IntestinesDocument12 pagesMajor Organs of The Human Body:: Stomach and IntestinesMiraNo ratings yet
- Bile Duct InjuryDocument62 pagesBile Duct InjuryShashidhara Puttaraj100% (1)
- 3.3 ColicDocument3 pages3.3 ColicGeorges Ramon Livio ProdigsonNo ratings yet
- Alumy SuspensiDocument5 pagesAlumy SuspensiThytin MartHa PeliYanNo ratings yet
- Ulcerative ColitisDocument5 pagesUlcerative ColitisVenice Jame SanchezNo ratings yet
- The Digestive SystemDocument3 pagesThe Digestive SystemabcNo ratings yet
- NGT FeedingDocument8 pagesNGT FeedingSheng GosepNo ratings yet
- Update On DiarrheaDocument12 pagesUpdate On DiarrheantnquynhproNo ratings yet
- Jaundice 23-24pdfDocument25 pagesJaundice 23-24pdfmyarjddbzNo ratings yet
- Abdominal ExaminationDocument56 pagesAbdominal ExaminationAnggreani PutriNo ratings yet
- Chapter 6 NutritionDocument101 pagesChapter 6 NutritionNUR FAEZAHNo ratings yet
- Quiz 4Document12 pagesQuiz 4abezareljvenNo ratings yet
- NCM 116Document32 pagesNCM 116Yeany IddiNo ratings yet
- Drug StudyDocument9 pagesDrug StudyJonica CamposNo ratings yet
- Digestive System Lesson Plan SCDocument5 pagesDigestive System Lesson Plan SCJustine PamaNo ratings yet
- CSEC Biology DigestionDocument53 pagesCSEC Biology DigestionKemoy FrancisNo ratings yet
- 6 Day Pediatric PancreatitisDocument16 pages6 Day Pediatric PancreatitisShreyash Haritwal100% (1)
- Anatomi Radiologi Barium Studies For GITDocument52 pagesAnatomi Radiologi Barium Studies For GITRio ArbiansyahNo ratings yet
- Inflammtory Bowel Disease (Ibd)Document30 pagesInflammtory Bowel Disease (Ibd)SnehaNo ratings yet
- The Digestive System Parts and FunctionsDocument6 pagesThe Digestive System Parts and FunctionsDixie MerinNo ratings yet
- Vagus Indigestionعسر الهضم المسبب باصابة العصب الحائرDocument27 pagesVagus Indigestionعسر الهضم المسبب باصابة العصب الحائرAli H. Sadiek أ.د. علي حسن صديق100% (3)