Professional Documents
Culture Documents
ACLS Acute Coronary Syndrome & Strokes
ACLS Acute Coronary Syndrome & Strokes
Uploaded by
S D0 ratings0% found this document useful (0 votes)
107 views6 pages2020 American Heart Association acs algorithm
Original Title
ACLS acute coronary syndrome & strokes
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document2020 American Heart Association acs algorithm
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
0 ratings0% found this document useful (0 votes)
107 views6 pagesACLS Acute Coronary Syndrome & Strokes
ACLS Acute Coronary Syndrome & Strokes
Uploaded by
S D2020 American Heart Association acs algorithm
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
You are on page 1of 6
ce
; AMERICAN
American ASO CTON
Heart of CRITICAL-CARE
Association. NURSES
Acute Coronary
Syndromes and Stroke
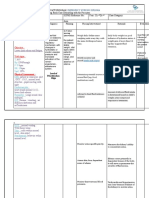
Acute Coronary Syndromes Algorithm
Symptoms sugges e of ischemia or infarction
7
EMS assessment and care and hospital preparation
* Assess ABCs. Be prepared to provide CPR and defibrillation
* Administer aspirin and consider oxygen, nitroglycerin, and morphine if needed
* Obtain 12-lead ECG; if ST elevation:
— Notify receiving hospital with transmission or interpretation; note ti
and first medical contact :
* Provide prehospital notification; on arrival, transport to ED/
* Notified hospital should mobilize resources to resp
° If considering prehospital fibrinolysis, |
Concurrent ED/cath lab assessment Immediate ED/cath lab
(<10 minutes) general treatment
* Activate STEMI team upon EMS notification * IfO2 sat <90%, start:
* Assess ABCs; give oxygen if needed 4L/min, titrate
* Establish IV access * Aspirin 162 to:
Perform brief, targeted history, ou
fi i
2020 American Heart Association. 20-1120
2020 American Heart Assocation N-1029 (of). Pinte
ST elevation or new or
presumably new LBBB;
strongly suspicious
for injury
ST-elevation MI (STEMI)
Vi
© Start adjunctive
therapies as indicated
© Donotdelay reperfusion
hours |
$12 hours
Guidelines
briana
A
CA ELT CEA tel tats Algorithm (continued)
Non-ST-el
validat
(ie, TIMI
ST depression or dynamic
T-wave inversion, transient
ST elevation; strongly
suspicious for ischemia
and/or high-risk score
High-risk NSTE-ACS
Troponin elevated or
high-risk patient
Consider early invasive
strategy if:
| « Refractory ischemic
chest discomfort
» Recurrent/persistent
ST deviation
Ventricular tachycardia
« Hemodynamic
instability
Signs of heart failure
Start adjunctive therapies
(eg. nitroglycerin, heparin)
as indicated
See AHA/ACC NSTE-ACS
Reperfusion goals:
Therapy defined by
center criteria
« FMC-to-bal
(PC of
patient and
loon inflation
10 Ss
(NSTE-ACS)
Determine risk using
| aie
q
levation ACS
ited score
or GRACE)
Normal ECG or
nondiagnostic changes
in ST segment or
T wave; low-risk score
Low-/intermediate-
risk NSTE-ACS
Consider admission
to ED chest pain unit
or to appropriate bed
for further monitoring
and possible
intervention
pee
Fibrinolytic Contraindications for STEMI
Contraindications for fibrinolytic use in STEMI consistent with
the 2013 ACCF/AHA Guideline for the Management of ST-Elevation
Myocardial Infarction*
Absolute Contraindications
¢ Any prior intracranial hemorrhage
Known structural cerebral vascular lesion (eg, arteriovenous
malformation)
Known malignant intracranial neoplasm (primary or metastatic)
Ischemic stroke within 3 months
— Exceptacute ischemic stroke within 4.5 hours
Suspected aortic dissection
Active bleeding or bleeding diathesis (excluding menses)
Significant closed head trauma or facial trauma within 3 months
Intracranial or intraspinal surgery within 2 months
|| * Severe uncontrolled hypertension (unresponsive to emergency
therapy)
¢ For streptokinase, prior treatment within the previous 6 months
Relative Contraindications
* History of chronic, severe, poorly controlled hypertension
¢ Significant hypertension on presentation (systolic blood pressure
greater than 180 mm Hg or diastolic blood pressure greater than
110 mm Hg)
History of prior ischemic stroke more than 3 months
¢ Dementia
| * Known intracranial pathology not covered in absolute contraindications
| © Traumatic or prolonged (more than 10 minutes) CPR
° Major surgery (less than 3 weeks)
| © Recent (within 2 to 4 weeks) internal bleeding
| © Noncompressible vascular punctures
| © Pregnancy
* Active peptic ulcer
* Oralanticoagulant therapy
*Viewed as advisory for clinical decisi
Abbreviations: CPR, cardiopulm
| infarction.
i ke
Identify signs and symptoms of possi strol
Activate emergency responst
v
Critical EMS assessments and actions
Assess ABCs; give oxygenif needed
Initiate stroke protocol
Perform physical exam “ !
Perform validated prehospital stroke screen and stroke severity tool
« Establish time of symptom onset (last known normal)
* Triage to most appropriate stroke center
* Check glucose; treatifindicated “ i %
* Provide prehospital notification; on arrival, transport to brain imaging suite
Note: Refer to the expanded EMS stroke algorithm.
Y
ED or brain imaging suite*
Immediate general and neurologic assessment by hospital or stroke team
* Activate stroke team upon EMS notification
* Prepare for emergent CT scan or MRI of brain upon arrival
* Stroke team meets EMS on arrival
* Assess ABCs; give oxygen if needed
* Obtain IV access and perform laboratory assessments
* Check glucose; treat ifindicated
* Review patient history, medications, and procedures
* Establish time of symptom onset or last known normal
* Perform physical exam and neurologic examination, including NIH Stroke Scale
rCi eurological Scale
: and go, ‘straight to the brain imaging suite.
_<_ Does brain imaging >
\ showhemorrhage? >
a
Consider alteplase
Initiate
intracranial
hemorrhage
rotocol
Consider EVT
* Perform CTA
* Perform CTP as indicated
Emergency Medical Ser
Acute Stroke LOTT Te)
Transport time
| to EVT-capable
stroke center will ‘
not disqualify for
thrombolytic,
g Total transport
| time from scene
| to nearest CSC
is <30 min total
and within
maximum time
permitted by EMS.
ice LT)
Se ery
tren)
Pouca’
Presentation
=gastowrf
PNT ea CU CUCU in Acute Ischemic Stroke
Options to Treat Arterial Hypertension in Patients With Acute Ischemic
Stroke Who Are Candidates for Emergency Reperfusion Therapy’
{0}
COR2b LOE
Patient otherwise eligible for emergency reperfusion therapy except that
BP is >185/110 mm Hg:
* Labetalol 10-20 mg IV over 1-2 minutes, may repeat 1 time; or
* Nicardipine 5 mg/h lV, titrate up by 2.5 mg/h every 5-15 minutes,
maximum 15 mg/h; when desired BP reached, adjust to maintain
proper BP limits; or
¢ Clevidipine 1-2 mg/h lV, titrate by doubling the dose every
2-5 minutes until desired BP reached; maximum 21 mg/h
¢ Other agents (eg, hydralazine, enalaprilat) may also be considered
If BP is not maintained <185/110 mm Hg, do not administer alteplase
Management of BP during and after alteplase or other emergency
| | reperfusion therapy to maintain BP <180/105 mm Hg:
| | ° Monitor BP every 15 minutes for 2 hours from the start of alteplase
therapy, then every 30 minutes for 6 hours, and then every hour
for 16 hours
If systolic BP >180-230 mm Hg or diastolic BP >105-120 mm Hg:
° Labetalol 10 mg IV followed by continuous IV infusion 2-8 mg/min; or
° Nicardipine 5 mg/h lV, titrate up to desired effect by 2.5 mg/h every
5-15 minutes, maximum 15 mg/h; or
* Clevidipine 1-2 mg/h lV, titrate by doubling the dose every
2-5 minutes until desired BP reached; maximum 21 mg/h
!f BP not controlled or diastolic BP >140 mm Hg, consider IV sodium
nitroprusside
Abbreviations: AIS, acute ischemic stroke; BP, blood pressure; COR, Class of
Recommendation; IV, intravenous; LOE, Level of Evidence.
Different treatment options may be appropriate in patients who have comorbid conditions
that may benefit from rapid reductions in BP, such as acute coronary heart failure, aortic
dissection, or preeclampsia/eclampsia.
Data derived from Jauch et al.? i
1. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients
with acute ischemic stroke: 2019 update to the 2018 guidelines for the early men agate
of acute ischemic stroke: a guideline for healthcare professionals from the America
Association/American Stroke Association. Stroke. 2019:50(12):e344-e418. dot: 10-1 e
STR.0000000000000211 . Col
. Jauch EC, Saver JL, Adams HP Jr, etal; for the American Heart Association suroke Cos s
Council on Cardiovascular Nursing, Council on Peripheral Vascular Diseaceiees sos
Clinical Cardiology. Guidelines for the early management of patients itt \20o
stroke: a guideline for healthcare professionals from the American Hea
Stroke Association. Stroke. 2013;44(3):870-947. doi:
10.1161/STR.0b013e3182
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CBAHI Survey Questions October 2021Document5 pagesCBAHI Survey Questions October 2021S D67% (3)
- Professor: Dr. Felina C. YoungDocument8 pagesProfessor: Dr. Felina C. YoungS DNo ratings yet
- Log Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date AreaDocument3 pagesLog Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date AreaS DNo ratings yet
- Log Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaDocument4 pagesLog Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaS DNo ratings yet
- Sara Sappari ArabaniDocument3 pagesSara Sappari ArabaniS DNo ratings yet
- April 21st 2020 Muhc Code BlueDocument20 pagesApril 21st 2020 Muhc Code BlueS DNo ratings yet
- Log Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaDocument3 pagesLog Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaS DNo ratings yet
- Dueich Germany LearningjsjsjjsjsDocument1 pageDueich Germany LearningjsjsjjsjsS DNo ratings yet
- Budget Planning: Nur-Ailyn Sabri Isnaji, RN Lorena Jain Kuhutan, RN Salman Cosain Hamidi, RNDocument7 pagesBudget Planning: Nur-Ailyn Sabri Isnaji, RN Lorena Jain Kuhutan, RN Salman Cosain Hamidi, RNS DNo ratings yet
- Log Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaDocument2 pagesLog Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaS DNo ratings yet