Professional Documents
Culture Documents
Vestibular Disorder
Vestibular Disorder
Uploaded by
angel winnieOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vestibular Disorder
Vestibular Disorder
Uploaded by
angel winnieCopyright:
Available Formats
Rev Bras Otorrinolaringol
2006;72(3):388-93.
ORIGINAL ARTICLE
Circumstances and
consequences of falls in elderly
people with vestibular disorder
Fernando Freitas Ganança1, Juliana Maria
Gazzola2, Mayra Cristina Aratani3, Monica
Rodrigues Perracini4, Maurício Malavasi Keywords: vestibular disease, elderly, falls, dizziness.
Ganança5
Summary
A im: To investigate the circumstances and consequences
of falls in the chronically dizzy elderly and to correlate them
with the number of falls (one/two and more). Method:
Transversal descriptive analytic study with 64 patients aged
65 or over, with history of falls and diagnostic of chronic
vestibular dysfunction. We performed a descriptive analysis
and Qui-Square test (<0.05). Results: The sample
was constituted by a female majority (76.6%) with a mean
age of 73.62±5.69 years. The vestibular examination showed
peripheral vestibulopathy in 81.5% of the cases and the most
prevalent diagnostic hypothesis were benign paroxysmal
positional vertigo (43.8%) and metabolic inner ear disease
(42.2%). Recurrent falls were seen in 35 elderly (53.1%). In
relation to the last fall, 39.1% of the patients had fallen in their
homes, 51.6% of them occurred during the morning, 51.6%
with some propulsion mechanism, 53.1% when walking,
25.0% caused by dizziness and 23.4% by stumbling. Activity
restriction was significantly greater in patients that have
already had two and more falls, when compared with those
who had fallen only once (p=0.031). We found a significant
association between the number of falls and their causes
(p<0.001). Falls that have happened by slipping were more
frequent in the elderly that reported one fall (p=0.0265) and
falls that had happened because of dizziness were more
frequent in the elderly that complained of two or more falls
(p=0.0012). Conclusions: Fear and tendency to fall are
referred by the majority of chronically dizzy elderly. Fall
are more frequent in the morning, in the home and during
walking. The propulsion direction is mentioned by half of
the elderly and the most common cause for falls are dizziness
and stumbling. The number of falls is significantly associated
with activity restrictions after the last fall and with the causes
for falling (slipping and dizziness).
1
Physician, ENT specialist, Doctor in Medicine at UNIFESP - EPM. Affiliated Professor of Otoneurology at UNIFESP - EPM. Professor of the post-graduate course on
Neuromotor Rehabilitation Science at UNIBAN.
2
Physical therapist. Specialist in Gerontology, graduated at UNIFESP - EPM. Master in Sciences, graduate from the post-graduate course in Otorhinolaryngology and
Head & Neck Surgery at UNIFESP - EPM.
3
Physical therapist. Specialist in Gerontology, graduated at UNIFESP - EPM.
4
Physical therapist. Doctor in Rehabilitation Science - UNIFESP - EPM. Coordinating Professor of the Physical Therapy master’s degree course at UNICID.
5
Full Professor Otorhinolaryngology at UNIFESP - EPM. Senior Researcher in the stricto sensu Post-Graduate Program (Master’s degree) on Neuromotor Rehabilitation
Science at UNIBAN. Responsible for the Balance Metrics Unit of the Otorhinolaryngology Sector of the Fleury Diagnostic Medicine Center - Sao Paulo (SP).
Otoneurology Department at UNIFESP - EPM / Vestibular Rehabilitation Sector.
Correspondence: Dr. Fernando F. Ganança - Rua dos Otonis 700 Piso Superior Vila Clementino 04025-002 São Paulo SP.
Telephone (0xx11) 5575 2552 - E-mail: otoneuro@unifesp.epm.br.
Fapesp. Protocol number 03/10119-3
Paper submitted to the ABORL-CCF SGP (Management Publications System) on January 26th, 2005 and accepted for publication on April 5th, 2006.
BRAZILIAN JOURNAL OF OTORHINOLARYNGOLOGY 72 (3) MAY/JUNE 2006
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
388
INTRODUCTION lighting, slippery floors and others), risky behaviors (climb-
ing chairs) and the specific task in a given moment.7 When
Dizziness is a sensation of loss of body balance. demands on postural control are greater that the individual
It may be defined as erroneous perception, a movement capacity to deal with them, there is a fall8.
illusion or hallucination, a sensation of rotating spatial diso- No studies on the circumstances and consequences
rientation (vertigo) or non-rotating spatial disorientation of falls in the elderly with chronic vestibular diseases were
(instability, imbalance, fluctuation, oscillation, oscillopsy). found in national and international literature. Identifying
Different types of dizziness (rotatory and non-rotatory) in these characteristics may contribute to establish specific
the same individual are not rare. Both types may or may prevention strategies to reduce the rate of falls and its
not be vestibular disorders that can be demonstrated by complications.
otoneurological tests1. Dizziness results from primary or The aim of this study was to investigate the cir-
secondary functional disorders of the vestibular system in cumstances and consequences of falls in the elderly with
approximately 85% of cases2. chronic vestibular diseases, relating them to the number
Falls are the main complication of balance disorders of falls (one/two or more falls).
in the elderly. A fall is defined as an unintentional event
resulting in a change of position to a lower level com- METHODS
pared to the individual’s initial position, with no intrinsic
determining factor such as a cerebral vascular accident or An analytical descriptive cross-sectional study ap-
syncope or an unavoidable accident3,4. proved by the Federal University of Sao Paulo - Sao Paulo
In study done in metropolitan Sao Paulo, Perracini Medical School (UNIFESP - EPM) Research Ethics Com-
and Ramos5 found that the prevalence of falls among eld- mittee, protocol number 01214/05. This paper is part of a
erly people was about 30% and that the rate of recurrent study financed by the Sao Paulo State Research Support
falls was 11% in that group. Although most falls (30 to 50%) Foundation (FAPESP), process number 03/10119-3.
cause minor injuries that do not require medical care, 10 The sample included male and female patients
to 15% of falls cause serious injuries, the most common from the UNIFESP - EPM Otoneurology Outpatient Clinic
being hip fracture (1% to 2%). Approximately 25% of falls aged 65 years and over, with chronic vestibular disease,
in that community cause immediate limitation of activities characterized by complaints of dizziness and/or imbalance
either due to physical harm or to fear of falling4. and/or dazing and/or other non-specific sensations of diz-
In a study on the incidence of falls in individuals ziness with at least three months duration. The evaluation
with vestibular dysfunction, those with bilateral vestibular was not made during a crisis of vertigo.
deficits fell more often compared to patients with unilat- Exclusion criteria included elderly patients with
eral involvement (respectively 51.1% and 30%). Patients poor or incapacitating visual and auditory acuity which
with unilateral vestibular deficits aged over 75 years had limited activities of daily life even with corrective lenses
a higher rate of falls compared to patients aged below 65 and/or hearing aids, those that had undergone upper and/
years. However, in patients with bilateral vestibular defi- or lower limb amputation and patients that could not walk
cits, the rate of falls in patients aged 75 years and above independently or were confined to wheelchairs.
was lower compared to patients aged less than 74 years, Patients initially underwent otoneurological clini-
probably due to increased demands to use attention and a cal evaluation, which includes the clinical history, the
reduction of activities, with less exposure to situations of otorhinolaryngological physical examination, audiometry,
risk. No difference was found in the incidence of falls in imitanciometry and vestibular examination using vecto-
patients with unilateral vestibular dysfunction and patients electronystagmography according to criteria described in
aged 65 years or more. There was a significantly higher literature9,10.
number of falls in patients with bilateral vestibular dys- Patients were inquired about falls during the year
function in the 65 to 74 years age group compared to the preceding the study. Information was collected about the
elderly in the community within the same age group6. place, time, lighting, direction, causes and activities at the
Falls frequently result from a sum of intrinsic and moment of the fall; information was also gathered about
extrinsic risk factors; it is difficult to restrict a fall to a whether the fall led to restrictions on activities of daily life.
single risk factor or cause. Fall-related intrinsic factors in The last event was investigated when there were recurrent
the elderly are loss of mobility, functional incapacity to falls (two or more falls). Patients were also inquired about
undertake activities of daily life, reduced lower limb mus- the tendency to fall and fear of falls.
cle strength, balance disorders, complaints of dizziness, Statistical analysis was descriptive analysis. For the
psychotropic medication, visual, auditory and/or cognitive analysis of inference, the variable “number of falls” was
deficits, postural hypotension, gait disorders and chronic compared with the variables place, time, lighting, direction
diseases. Extrinsic factors are environmental risks (poor and causes of the fall, activities at the moment of the fall
and if the fall led to restrictions on activities of daily life;
BRAZILIAN JOURNAL OF OTORHINOLARYNGOLOGY 72 (3) MAY/JUNE 2006
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
389
the Chi-squared test was used to calculate these variables activities of daily life after the last fall.
(c2). Fisher’s accuracy test was used to identify the associa- There was a significant association between number
tion between variables of contingency tables where 25% of falls and restriction of activities after the last fall
of cells had less than five occurrences. The Chi-squared (p=0.031). Restriction of activities was significantly higher
test was used to analyze the association between frequen- in elderly patients with vestibular diseases that had had
cies of a sample with two categories, followed by Yates’ two or more falls (78.6%), compared to those with only
correction. The statistical test significance level was 5% one fall (21.4%).
(a ≤ 0,05). A significant association was found between the
Analysis was done using the software SPSS 10.0 number and the causes of falls (p < 0.001). There was
under Windows11. a statistically significant difference between the number
of falls and slipping (p=0,026), among other causes of
RESULTS falls; there was an increased rate of slipping in patients
that reported falls. Falls due to dizziness or vertigo were
Our sample included 64 elderly patients with a more frequent in patients that reported two or more falls
diagnosis of chronic vestibular syndrome monitored in during the study period, which was statistically significant
our outpatient department. Average age was 73.62 years, (p=0.001) as seen on Table 2.
standard deviation (SD) of 5.69; the maximum age was There was no significant association between the
89 years. Fifteen (23.4%) were male and 49 (76.6%) were variable number of falls and the variables place, time,
female. lighting and direction of fall.
The average number of diseases per individual
was 3.98 (SD = 1.77), with a maximum of eight associ-
ated diseases. The most prevalent were circulatory system
diseases (78.1%) followed by osteomuscular system and
connective tissue diseases (67.2%), and nutritional endo-
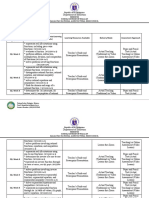
Table 1. Absolute and relative frequency of fall places in elderly patients
crine and metabolic diseases (54.7%). The average number
with chronic vestibular dysfunction (n = 64).
of medical drugs used was 4.08 drugs (SD = 2.38), with
maximum of ten drugs.
Place of the fall Absolute Relative
Results of the vestibular test showed peripheral Frequency (n) Frequency (%)
syndrome (81.5%), no abnormalities (11.1%) and central
At home (external environment) 13 20,3
vestibular syndrome (7.4%). The most frequent vestibu-
At home (internal environment) 21 32,8
lar disorders were benign paroxysmal positional vertigo
(43.8%) and metabolic diseases of the labyrinth (42.2%). Out of home (familiar place) 25 39,1
Seven patients (10.9%) used walking support de- Out of home (unfamiliar place) 5 7,8
vices. Of the 64 elderly patients, 34 (53.1%) had reported
recurrent falls. Fear of falls and the tendency to fall were re-
ported by most patients (73.4% and 82.8%, respectively).
The most common time for a fall was the morning Table 2. Distribution of the number of falls related to the causes of falls
in elderly patients with chronic vestibular dysfunction (n = 64).
(51.6%), followed by the afternoon (34.4%), the evening
(12.5%) and dawn (1.6%).
Number of falls
The reported direction of the fall was propulsion in
51.6% of the patients, retropulsion in 15.6%, right lateral in CAUSES One fall Two or more falls Total
15.6%, left lateral in 12.5% and no answer in 4.7%. n (%) n (%) n (%)
The fall places are described on Table 1. Falls in Tripping 11 (73,3) 4 (26,7) 15 (100,0)
the bathroom were 38.1% of fall that occurred at home. In Slipping 11 (84,6) 2 (15,4) 13 (100,0)
most cases the house was well lighted (85.9%).
Syncope/Dark-
The most frequent tasks at the moment of the fall ening of vision
1 (14,3) 6 (85,7) 7 (100,0)
were walking (53.1%), climbing up or down stairs (10.9%),
Dizziness/Ver-
change of posture (9.4%) and taking a bath (6.3%). tigo
1 (6,3) 15 (93,8) 16 (100,0)
Vertigo was most common cause of falls (25.0%),
Others 6 (46,2) 7 (53,8) 13 (100,0)
followed by tripping over (23.4%), slipping (20.3%), syn-
cope/blackout (10.8%) and others (20.5%). “Other” causes Total 30 (46,9) 34 (53,1) 64 (100,0)
Fisher’s exact test
include reduced attention at the moment of the fall (7.9%), p < 0.001
weakening of the knees (7.9%) and an unexpected hurdle Corrected Chi-squared test (Yates)
(4.7%). Number of falls and slipping (p = 0.026)
Fourteen patients (21.9%) reported restriction of Number of falls and dizziness/vertigo (p = 0.001)
BRAZILIAN JOURNAL OF OTORHINOLARYNGOLOGY 72 (3) MAY/JUNE 2006
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
390
DISCUSSION signs and/or symptoms mediated by repeated exposure
to sensory stimulation as the day elapses20.
Patients in this study had a relatively high average Half our sample reported falls facing forward (pro-
age (73.62 years), similar to that found by other authors that pulsion). The difficulty of elderly with vestibular diseases
also consider aging as a possible factor of loss of vestibular to use hip reactive strategies in an attempt to control the
function, leading to multiple associated otoneurological center of gravity to find a support base in a situation of
symptoms such as vertigo and other forms of dizziness, strong and fast disturbance, could explain most of the falls
imbalance, hearing loss, tinnitus, and others12,13. in the forward direction23-25. In this approach, the line of
Women were 76.6% of our sample, similar to litera- vision moves with the position of the head, which might
ture findings. Dizziness is more frequent in women in a make it more difficult for the elderly with vestibular dis-
2:114 ratio; women also seem to fall more frequently5,15. eases to stabilize the visual field.
A variety of diseases may cause dizziness in the Among the causes of falls in our study patients,
elderly, but metabolic and vascular etiologies are the main vertigo was first (25.0%), followed by tripping (23.4%)
causes, due either to primary or secondary injury to the and slipping (20.3%). Tripping and slipping were also
vestibular system16,17. Our findings corroborate this con- significant causes in Berg et al.’s20 study of the elderly, at
clusion, as we 78.1% of our sample had some circulatory 34.0% and 25.0%, respectively. The increased prevalence
system disease and 54.7% an endocrine nutritional and of vertigo as a cause of falls probably is due to vestibular
metabolic disease. disease that was present in elderly patients in our study.
Otoneurological clinical data in our sample was We also noticed that the most frequent tasks at the
similar to findings in other studies18,19. There was a pre- moment of the fall were walking, climbing or going down
dominance of peripheral vestibular disorders, and the stairs, activities involving postural transference and bath-
more frequent vestibular conditions. According to Ganança ing. Cohen22 observed that for patients aged between 35
et al.2, benign paroxysmal positional vertigo is the most and 82 years and with vestibular diseases, raising from a
common vestibular disease in the elderly, particularly in chair was difficult for 94.0%, walking over level surfaces
females. was difficult for 81.0% and bathing and climbing stairs
Our sample was different from population studies was difficult for 75.0% of these patients. These tasks re-
on the elderly in that the rate of recurrent falls was 29.2%, quire good functional body balance systems; when these
compared to a survey done among the elderly in metro- systems are dysfunctional, such activities become a chal-
politan Sao Paulo in which the prevalence of recurrent falls lenge, compromising control of posture and consequently
was 11.0%5. For Herdman et al.6, dizziness of vestibular facilitating falls21,26.
origin may be a predisposing factor of falls and recurrent Falls are strongly associated with the decline of
falls, as vestibular dysfunction limits control of posture, physical function due to aging; functionally, this means
leading to instability and body misalignment. that there is a reduction or loss of the capability to un-
In our study, 21.9% of patients had restriction of dertake the demands of daily life and its environmental
activities of daily life after the last fall, which is in agree- challenges5.
ment with Nevitt,4 who found that serious injury or activity Restriction of activities was significantly higher in
limitations reached 25.0% in patients with a history of falls, elderly patients with vestibular diseases that had suffered
due to physical damage or fear of falling. two or more falls compared to patients that had had only
Most falls described by patients with vestibular dis- one fall. Restriction of activities may be, at least tempo-
eases in our study had occurred out of home in a known rarily, a consequence of trauma, fear of falling, medical
place (36.1%). Berg et al.20 studied falls in independent orders and/or coexisting diseases4,27. Functional motor
elderly people and showed that falls occurred mostly at activities related to cephalic movement balance control
home in an external environment (35.0%). For the elderly may cause dizziness in patients with vestibular diseases,
with chronic vestibular dysfunction, tasks seem to become further increasing restriction of activities.
more difficult when the environment requires greater In our study, slipping was the most frequent cause
control of posture21. Out of home, there is an increased of falls in elderly patients reporting one fall, whereas diz-
demand on the stabilization of the visual field, head and ziness and vertigo were more frequent in elderly patients
thoracic movements, and most of all a dynamic balance that reported two or more falls during our study period.
to face any eventual obstacle22. These findings suggest that elderly patients with vestibular
Falls in patients with vestibular diseases in our diseases and with a higher susceptibility to body imbalance
study occurred mostly during the morning (51.6%), differ- usually have falls related to vestibular disorders. These
ent from Jekins et al.’s12 study, where 52.0% of falls were findings also underline the importance of fall prevention
found to have happened during the afternoon. This may by control of extrinsic factors such as environmental risk,
be related to a reduction or disappearance of vestibular which may cause slipping.
BRAZILIAN JOURNAL OF OTORHINOLARYNGOLOGY 72 (3) MAY/JUNE 2006
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
391
In line with evidence in literature, Perracini7 sug- 8. Perracini MR. Prevenção e Manejo de Quedas. In: Ramos LR, Toniolo
gests a number of interventions that may be recommended Neto J. Geriatria e Gerontologia. Guias de Medicina Ambulatorial e
Hospitalar / Unifesp-Escola Paulista de Medicina. São Paulo: Editora
for dealing with risk factors for falls in the elderly, such Manole; 2005. p.193-208.
as: 1) muscle strengthening programs for the quadriceps 9. Ganança MM, Caovilla HH, Munhoz MSL, Silva MLG, Frazza MM. As
and ankle dorsal flexor muscles; 2) balance training to etapas da equilibriometria. In: Ganança MM, Caovilla HH, Munhoz
integrate sensory information, to control stability limits, to MSL, Silva MLG. Equilibriometria Clínica. Série Otoneurologia. São
Paulo: Editora Atheneu; 1999. p.41-114.
control thoracic rotation and to increase the effectiveness 10. Ganança MM, Caovilla HH, Munhoz MSL, Silva MLG, Ganança
of movement strategies; 3) prescription and/or adapta- FF, Ganança CF. A vertigem explicada. RBM Rev Bras Med
tion of walking support devices; 4) adaptation of correc- 1999c;56(Espec):2-20.
tive lenses; 5) prescription and adequate use of hearing 11. The SPSS Statistical package for the social sciences: base users guide
[computer program]. Version 10.0. Chicago: SPSS; 1999.
aids; 6) adequate psychotropic medication; 7) changes in 12. Jekins HA, Furman JM, Gulya AJ, HonrubiaV, Linthicum FH, Mirka A.
the environment and adaptations as needed done by an Dysequilibrium of aging. Otolaryngol Head Neck Surg 1989;100:272-
occupational therapist; 8) specific physical therapy and 82.
pharmacological management of chronic degenerative 13. Caovilla HH et al. Presbivertigem, Presbiataxia, Presbizumbido e
Presbiacusia. In: Silva MLG et al. Quadros Clínicos Otoneurológicos
diseases. mais Comuns. São Paulo: Atheneu; 2001. p. 153-8.
Risk factors for falls should be identified to allow 14. Campos CAH. Principais quadros clínicos no adulto e idoso. In:
prevention and rehabilitation by specific interventions. We Ganança MM. Vertigem tem cura? São Paulo: Lemos Editorial; 1998.
highlight the need for further studies to help identify risk p.49-57.
15. Campebell JA, Spears GF, Borrie MJ. Examination by logistic regres-
factors for falls in the elderly with vestibular diseases. sion modelling of the variables which increase the relative risk of
elderly women falling compared to elderly men. J Clin Epidemiol
CONCLUSION 1990;42:1415-20.
16. Mangabeira Albernaz PL. Aspectos otoneurológicos na velhice. Acta
The majority of elderly patients that have a diagnosis Awho 1982;1(3):93-5.
17. Ganança MM, Caovilla HH, Munhoz MSL, Silva MLG, Settanni FAP,
of chronic vestibular disease report fear of falls and a ten- Ganaça FF, et al. As tonturas e sintomas associados. In: Munhoz MSL,
dency to fall. Falls are more frequent during the morning, Ganança MM, Caovilla HH, Silva MLG. Casos clínicos otoneurológicos
out of home and during walking. Half the patients report típicos e atípicos. São Paulo: Editora Atheneu; 2001.p.1-22.
the propulsive direction, and the most common causes are 18. Caovilla HH, Ganança MM, Munhoz MSL, Silva MLG, Frazza MM.
O valor da nistagmografia computadorizada. Rev Bras Med Otor-
vertigo and tripping over something. The number of falls rinolaringol 1997;4(5):158-63.
is associated with restriction of activities after the last fall, 19. Whitney SL, Wrisley DM, Furman JM. Concurrent validity of the Berg
and with the causes of the fall (slipping and dizziness). Balance Scale and Dynamic Gait Index in people with vestibular
dysfunction. Physiother Res Int 2003;8(4):178-86.
20. Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and conse-
REFERENCES quences of falls in independent community-dwelling older adults.
Age Ageing. 1997;26(4):261-8.
1. Ganança MM, Caovilla HH. Desequilíbrio e reequilíbrio. In: Ganança
21. Ganança FF, Perracini MR, Ganança CF. Reabilitação dos Distúrbios
MM. Vertigem tem cura? São Paulo: Lemos Editorial; 1998. p.13-9.
do Equilíbrio Corporal. In: Ganança MM. Vertigem: abordagens
2. Ganança MM, Caovilla HH, Munhoz MSL, Silva MLG. Alterações
diagnósticas e terapêuticas. São Paulo: Lemos Editorial; 2002. p.16.
da audição e do equilíbrio corporal no idoso. RBM Rev Bras Med.
22. Cohen H. Vestibular rehabilitation reduces functional disability.
1999;56(10):995-1011.
Otolaryngol Head Neck Surg 1992 Nov;107(5):638-43.
3. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among
23. Ganança MM, Munhoz MSL, Caovilla HH, Silva MLG, Ganança FF,
elderly persons living in the community. N Engl J Med. 1988 Dec
Perracini MR, et al. Conceitos e algoritmos terapêuticos. In: Ganança
29;319(26):1701-7.
MM, Munhoz MSL, Caovilla HH, Silva MLG. Condutas na Vertigem.
4. Nevitt MC. Falls in the elderly: risk factors and prevention. In: Masdeu
São Paulo: Grupo Editoral Moreira Jr.; 2004. p.55-112.
JC, Sudarsky L, Wolfson L. Gait disorders of aging. Falls and thera-
24. Perracini MR. Equilíbrio e controle postural em idosos. Rev Bras
peutic strategies. Philadelphia: Lippincott-Raven Publishers; 1997.
Postura Mov 1998;2(4):130-42.
p.13-36.
25. Horak FB, Shupert C. Função do sistema vestibular no controle
5. Perracini MR, Ramos LR. Fatores associados a quedas em uma
postural. In: Herdman SJ. Reabilitação vestibular. São Paulo: Editora
coorte de idosos residentes na comunidade. Rev Saúde Pública
Manole; 2002. p.25-51.
2002;6(36):709-16.
26. Whitney SL. Management of the elderly person with vestibular
6. Herdman SJ, Blatt P, Schubert MC, Tusa RJ. Falls in patients with
dysfunction. In: Herdman S. Vestibular Rehabilitation. United States
vestibular deficits. Am J Otol 2000 Nov;21(6):847-51.
of America: Contemporary Perspectives Rehabilitation; 2000. p.510-
7. Carvalhaes N, Rossi E, Paschoal S, Perracini N, Perracini MR, Rodrigues
33.
R. Quedas. Anais do Congresso Paulista de Geriatria e Gerontologia
27. Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of
- GERP’98; 1998 Jan; São Paulo, Brasil. São Paulo, p. 5-18, 1998.
falling and fall-related efficacy in relationship to functioning among
community-living elders. J Gerontol 1994;49(3):M140-M147.
BRAZILIAN JOURNAL OF OTORHINOLARYNGOLOGY 72 (3) MAY/JUNE 2006
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
392
You might also like
- Problem Set 3 Solution PDFDocument10 pagesProblem Set 3 Solution PDFHOUSSAME NAIMNo ratings yet
- 10 1097@NRL 0b013e31817533a3 PDFDocument10 pages10 1097@NRL 0b013e31817533a3 PDFV RakeshreddyNo ratings yet
- Lab. 3 - Beam Bending - 2020 Sem. 2: TheoryDocument3 pagesLab. 3 - Beam Bending - 2020 Sem. 2: TheoryFahim KhandakarNo ratings yet
- Falls in Older People: Epidemiology, Risk Factors and Strategies For PreventionDocument5 pagesFalls in Older People: Epidemiology, Risk Factors and Strategies For Preventiongiovanni senzaterraNo ratings yet
- Auris Nasus Larynx: Eeva Tuunainen, Jyrki Rasku, Pirkko Ja Ntti, Ilmari PyykkoDocument7 pagesAuris Nasus Larynx: Eeva Tuunainen, Jyrki Rasku, Pirkko Ja Ntti, Ilmari PyykkoSandi IrvantaNo ratings yet
- Dominance Wave Propagation During Binocular Rivalry in Mil - 2019 - Vision ReseaDocument8 pagesDominance Wave Propagation During Binocular Rivalry in Mil - 2019 - Vision ReseaAaryan R SinghNo ratings yet
- The Falling Elderly: Epidemiology Psychological TraumaDocument5 pagesThe Falling Elderly: Epidemiology Psychological TraumasugarmelodiesNo ratings yet
- Clinical Review - FullDocument5 pagesClinical Review - FullVita MadmoNo ratings yet
- Occasional Whiplash: Review Injury: A ReappraisalDocument4 pagesOccasional Whiplash: Review Injury: A ReappraisalSandara ParkNo ratings yet
- Vision Therapy For Binocular DysfunctionDocument7 pagesVision Therapy For Binocular DysfunctionGian Carlo Giusto BurboaNo ratings yet
- Peripheral Vestibular Dysfunction Is Prevalent in Older Adults Experiencing Multiple Non-Syncopal Falls Versus Age-Matched Non-Fallers: A Pilot StudyDocument6 pagesPeripheral Vestibular Dysfunction Is Prevalent in Older Adults Experiencing Multiple Non-Syncopal Falls Versus Age-Matched Non-Fallers: A Pilot StudyMuhammad YudhaNo ratings yet
- Vertigo and Dizziness in The ElderlyDocument6 pagesVertigo and Dizziness in The ElderlyCarmen DélanoNo ratings yet
- Tinetti 1Document6 pagesTinetti 10998884821k28kNo ratings yet
- Alla Et Al, 2020Document12 pagesAlla Et Al, 2020Rahmi LubisNo ratings yet
- 2016 Epidemiologia Da Migrânea VestibularDocument6 pages2016 Epidemiologia Da Migrânea VestibularGloria CantoNo ratings yet
- Migraine Associated Vertigo: Yoon-Hee Cha, M.D., Robert W. Baloh, M.DDocument6 pagesMigraine Associated Vertigo: Yoon-Hee Cha, M.D., Robert W. Baloh, M.DnoraNo ratings yet
- Guidelines For The Management of Epilepsy in The Elderly: Acta Neurologica Belgica October 2006Document7 pagesGuidelines For The Management of Epilepsy in The Elderly: Acta Neurologica Belgica October 2006adityaNo ratings yet
- West Virginia Medical Journal June2012Document6 pagesWest Virginia Medical Journal June2012nabiyaNo ratings yet
- Articlee OooDocument6 pagesArticlee OooLAL DIME 1No ratings yet
- Referat Motion SicknessDocument49 pagesReferat Motion SicknessGaluh Eka TantriNo ratings yet
- Vertigo 2 PDFDocument7 pagesVertigo 2 PDFyolan ariyanaNo ratings yet
- Etter To The Editor: The Value of Cycloplegia in Optometric Refraction of Adults in A Population StudyDocument2 pagesEtter To The Editor: The Value of Cycloplegia in Optometric Refraction of Adults in A Population StudyPhillip NyambaloNo ratings yet
- Herpes Zoster Ophthalmicus Clinical Presentation and Risk Factors For Loss of VisionDocument7 pagesHerpes Zoster Ophthalmicus Clinical Presentation and Risk Factors For Loss of VisionWTF AttaNo ratings yet
- GBS 2Document179 pagesGBS 2m3510No ratings yet
- Corneal Collagen Cross-Linking in The Stabilization of KeratoconusDocument9 pagesCorneal Collagen Cross-Linking in The Stabilization of KeratoconusPunam RazputriNo ratings yet
- Prevalence of Blindness in Patients With Uveitis: Original ResearchDocument4 pagesPrevalence of Blindness in Patients With Uveitis: Original ResearchMuhammad RaflirNo ratings yet
- Presntation f1Document25 pagesPresntation f1Bushra JavedNo ratings yet
- Myopia and Associated PathologicalDocument11 pagesMyopia and Associated PathologicalWing Yan LamNo ratings yet
- Diseases of The Diaphragm, Chest Wall, Pleura, and MediastinumDocument16 pagesDiseases of The Diaphragm, Chest Wall, Pleura, and Mediastinumjpma2197No ratings yet
- Ooa90020 543 547Document5 pagesOoa90020 543 547Sugi ArthaNo ratings yet
- International Journal of GerontologyDocument5 pagesInternational Journal of GerontologyKaye Antonette AntioquiaNo ratings yet
- 0701 CB MigraineDocument4 pages0701 CB MigraineEcaterina PozdircăNo ratings yet
- Complications of Upper Cervical Spine Trauma in Elderly Subjects. A Systematic Review of The LiteratureDocument12 pagesComplications of Upper Cervical Spine Trauma in Elderly Subjects. A Systematic Review of The Literaturebec medNo ratings yet
- 4 Arlies (Edited)Document9 pages4 Arlies (Edited)116045 IRMA YULIANINo ratings yet
- Acute DizzinessDocument14 pagesAcute DizzinesstsyrahmaniNo ratings yet
- Jaha 119 014546Document8 pagesJaha 119 014546HendrawanDianAgungWicaksanaNo ratings yet
- Mal de Debarquement SyndromeDocument5 pagesMal de Debarquement SyndromeFelipeAsenjoÁlvarezNo ratings yet
- Hayleys12877 015 0068 2 PDFDocument12 pagesHayleys12877 015 0068 2 PDFFitria Indah LestariNo ratings yet
- Banderas RojasDocument5 pagesBanderas RojasLucía TrilloNo ratings yet
- (1479683X - European Journal of Endocrinology) Prevalence and Natural History of Adrenal IncidentalomasDocument13 pages(1479683X - European Journal of Endocrinology) Prevalence and Natural History of Adrenal IncidentalomasClaudiaNo ratings yet
- NB02005Document3 pagesNB02005Noor MohammadNo ratings yet
- Characterization of Congenital Anomalies in Individuals With Choanal AtresiaDocument5 pagesCharacterization of Congenital Anomalies in Individuals With Choanal AtresiaAndi SanapatiNo ratings yet
- Overactive Bladder Syndrome and Nocturia: Chapter OutlineDocument27 pagesOveractive Bladder Syndrome and Nocturia: Chapter OutlineZakia DrajatNo ratings yet
- Pediatric Intracranial Aneurysms. Experience of 47 Cases.: Corresponding AuthorDocument8 pagesPediatric Intracranial Aneurysms. Experience of 47 Cases.: Corresponding AuthorVoicu AndreiNo ratings yet
- Women With Epilepsy: Clinically Relevant Issues: A B C D, E, FDocument8 pagesWomen With Epilepsy: Clinically Relevant Issues: A B C D, E, FAnum SasmitaNo ratings yet
- WhiplashInjury CEACCPDocument5 pagesWhiplashInjury CEACCPCarlosNo ratings yet
- Cervical DystoniaDocument5 pagesCervical DystoniaOmar ElsahartyNo ratings yet
- Necessity of EEG and CT Scan For Accurate Diagnosis of Idiopathic (Partial / Generalised) Seizures in ChildrenDocument4 pagesNecessity of EEG and CT Scan For Accurate Diagnosis of Idiopathic (Partial / Generalised) Seizures in ChildrenInternational Organization of Scientific Research (IOSR)No ratings yet
- Guillain Barre SyndromeDocument2 pagesGuillain Barre SyndromeTheresia Avila KurniaNo ratings yet
- Clinical Study of Concomitant StrabismusDocument6 pagesClinical Study of Concomitant StrabismusCarlos OrtegaNo ratings yet
- Spinal Cord InjuryDocument16 pagesSpinal Cord Injuryzwecker4458No ratings yet
- Inouye 2007Document8 pagesInouye 2007Veridiana Assencio SilvaNo ratings yet
- Evaluation of First Seizure and Newly Diagnosed.4Document31 pagesEvaluation of First Seizure and Newly Diagnosed.4veerraju tvNo ratings yet
- Status Epilepticus: Correspondence: Hpg9v@virginia - EduDocument12 pagesStatus Epilepticus: Correspondence: Hpg9v@virginia - EduGerardo Lerma BurciagaNo ratings yet
- Contin Educ Anaesth Crit Care Pain-2006-Fines-37-40Document4 pagesContin Educ Anaesth Crit Care Pain-2006-Fines-37-40PattolaNo ratings yet
- Which EEG Patterns Warrant Treatment in Critically IllDocument13 pagesWhich EEG Patterns Warrant Treatment in Critically IllRosiane Da Silva FontanaNo ratings yet
- Cognitive and Psychopathological Aspects of Ehlers DanlosDocument5 pagesCognitive and Psychopathological Aspects of Ehlers DanlosKarel GuevaraNo ratings yet
- Neuhauser Lempert 2004 Vertigo and Dizziness Related To Migraine A Diagnostic ChallengeDocument9 pagesNeuhauser Lempert 2004 Vertigo and Dizziness Related To Migraine A Diagnostic ChallengeliviaekasofianiNo ratings yet
- Comorbidities and Risk Factors Associated With Insomnia in The Elderly PopulationDocument9 pagesComorbidities and Risk Factors Associated With Insomnia in The Elderly PopulationKhairunnisa Ayu KresnandaNo ratings yet
- Vertigo and Dizziness: Challenges For Epidemiological ResearchDocument6 pagesVertigo and Dizziness: Challenges For Epidemiological ResearchKim AntelNo ratings yet
- Intro Mass SpecDocument2 pagesIntro Mass SpecHuy Đặng Anh0% (1)
- Amos Rapoport Meaning of Built Environment HighlightedDocument251 pagesAmos Rapoport Meaning of Built Environment HighlightedBhavani U KulkarniNo ratings yet
- 1 s2.0 S0022247X14006933 MainDocument12 pages1 s2.0 S0022247X14006933 MainValentin MotocNo ratings yet
- Cooperating With OthersDocument7 pagesCooperating With Otherswarren basconNo ratings yet
- Republic of The Philippines: M11GM-Ia-1) M11GM-Ia-2)Document5 pagesRepublic of The Philippines: M11GM-Ia-1) M11GM-Ia-2)Ana Bianca De GuzmanNo ratings yet
- Seminar PPT P S Manoj KumarDocument26 pagesSeminar PPT P S Manoj KumarManu P S50% (2)
- Processes in CounselingDocument26 pagesProcesses in CounselingQueenie Ann Ramirez MalaboNo ratings yet
- Mbala Et Les Contes Populaires BURSSENS - 1991Document11 pagesMbala Et Les Contes Populaires BURSSENS - 1991Glodi NtangeNo ratings yet
- Jason Van Tatenhove Transcript July 7Document23 pagesJason Van Tatenhove Transcript July 7Daily KosNo ratings yet
- Flowin Open ChannelsDocument22 pagesFlowin Open ChannelsSushma ThakurNo ratings yet
- File PDFDocument1 pageFile PDFtehtarikNo ratings yet
- CV BIKKU BARNWAL - CompressedDocument5 pagesCV BIKKU BARNWAL - CompressedBikku BarnwalNo ratings yet
- Topic 2-Leadership and MotivDocument31 pagesTopic 2-Leadership and MotivHundassa Likassa100% (1)
- Analisis Lingkungan Bisnis Dalam Meningkatkan Keunggulan Bersaing Café KopilabsDocument9 pagesAnalisis Lingkungan Bisnis Dalam Meningkatkan Keunggulan Bersaing Café KopilabsFitrina SaidNo ratings yet
- 2023 LO Grade 10 Term 2 MG FinalDocument10 pages2023 LO Grade 10 Term 2 MG FinalsheronmoyoshalomNo ratings yet
- Layout, Flow Process, Koordinator Wilayah & Inbound OutboundDocument11 pagesLayout, Flow Process, Koordinator Wilayah & Inbound OutboundHackiem MeazzaNo ratings yet
- DPP - 01 (Video Solution) - Kinematics NJ - 247Document5 pagesDPP - 01 (Video Solution) - Kinematics NJ - 247jayeshmali9459No ratings yet
- Problems: Photovoltaics: EUB - 7 - 133 Renewable Energy Technologies 1Document6 pagesProblems: Photovoltaics: EUB - 7 - 133 Renewable Energy Technologies 1mdmarufur100% (1)
- Remedws AljabarDocument6 pagesRemedws AljabarMariany UnknownNo ratings yet
- ch.2 Electric Potential and Capacitor - NotesDocument10 pagesch.2 Electric Potential and Capacitor - Notesnandank44373No ratings yet
- Science9 q2 Mod6 Molar MasDocument32 pagesScience9 q2 Mod6 Molar MasKristine Ibarreta-JazulNo ratings yet
- Basic Theories of PaDocument25 pagesBasic Theories of Panaja firdausNo ratings yet
- Hes D6501-03 General Test Methods For CoatingDocument28 pagesHes D6501-03 General Test Methods For CoatingPreetam KumarNo ratings yet
- 1.4.18. 2020 An Investigation On Botan Bridge Cllapse During ConstructionDocument6 pages1.4.18. 2020 An Investigation On Botan Bridge Cllapse During ConstructionJuan BravoNo ratings yet
- Dma Dissertation TopicsDocument5 pagesDma Dissertation TopicsBuyCheapPapersUK100% (1)
- Ebook Ebook PDF Research Methods and Statistics A Critical Thinking Approach 4th Edition PDFDocument41 pagesEbook Ebook PDF Research Methods and Statistics A Critical Thinking Approach 4th Edition PDFkaren.cambell302100% (37)
- Kids Playing Music PowerPoint TemplatesDocument48 pagesKids Playing Music PowerPoint TemplatesKyou KazuneNo ratings yet
- Cycle - 02Document8 pagesCycle - 02aaryangargNo ratings yet