Professional Documents
Culture Documents
Ajr 17 19185
Ajr 17 19185
Uploaded by
Bruno MeloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajr 17 19185
Ajr 17 19185
Uploaded by
Bruno MeloCopyright:
Available Formats
Cardiopulmonar y Imaging • Original Research
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
García-Garrigós et al.
Thoracic and Abdominal CT of Lung Cancer
Cardiopulmonary Imaging
Original Research
Best Protocol for Combined
Contrast-Enhanced Thoracic and
Abdominal CT for Lung Cancer:
A Single-Institution Randomized
Crossover Clinical Trial
Elena García-Garrigós1 OBJECTIVE. The purpose of this study was to evaluate the superiority of either of two pro-
Juan José Arenas-Jiménez1 tocols for combined contrast-enhanced thoracic and abdominal CT of patients with lung cancer
José Sánchez-Payá2 by comparing contrast enhancement, contrast-related artifacts, image quality, and radiation dose.
SUBJECTS AND METHODS. In this randomized controlled crossover clinical trial,
García-Garrigós E, Arenas-Jiménez JJ, 77 patients who underwent 203 CT examinations were enrolled. All patients underwent at
Sánchez-Payá J least two examinations performed with both protocols. Protocol A consisted of two acquisi-
tions: one 35-second delayed CT acquisition for the chest followed by a 70-second delayed
abdominal acquisition. Protocol B was a single 60-second delayed acquisition covering the
chest and the abdomen. Attenuation and noise of the aorta, pulmonary artery, and liver were
measured. Contrast-related artifacts, mediastinal lymph node visualization, liver enhance-
ment, and noise were visually scored. Dose-length product was recorded. Statistical analysis
was performed by t and chi-square tests and kappa statistics.
RESULTS. Contrast-related artifacts were more severe at all evaluated levels, and visu-
alization of lymph node regions was statistically significantly worse with protocol A. There
were no differences in enhancement or noise score of the liver. Tumor delineation and pleu-
ral findings were better evaluated with delayed phase images. Dose-length product was
Keywords: contrast injection protocol, CT, lung cancer,
pleural malignancy, radiation dose significantly higher with protocol A (645.0 vs 521.5 mGy · cm; p < 0.0001).
CONCLUSION. A single 60-second delayed acquisition for thoracic and abdominal
doi.org/10.2214/AJR.17.19185 contrast-enhanced CT is associated with less contrast artifact and affords better visualization
of lymph nodes at a lower radiation dose while acceptable vascular and hepatic contrast en-
Received October 18, 2017; accepted after revision
November 23, 2017.
hancement is maintained.
ontrast-enhanced CT of the chest concentration [7–11] and kilovoltage [12–14].
C
Based on a presentation at the 2017 World Congress of
Thoracic Imaging, Boston, MA.
and upper abdomen has an im- Protocols vary among institutions according
Supported by Fundación para el Fomento de la portant role in the initial workup to the technical characteristics of equipment
Investigación Sanitaria y Biomédica de la Comunitat and follow-up of lung cancer and and personal preferences of radiologists.
Valenciana (ISABIAL)-FISABIO (grant no. UGP-16-141). is one of the examinations most frequently Many parameters affecting the quality
1
requested of thoracic radiologists. Standard of examinations and their accuracy must be
Department of Radiology, Hospital General Universitario
de Alicante, Instituto de Investigación Sanitaria y
guidelines in the management of lung cancer taken into account when designing a con-
Biómedica de Alicante (ISABIAL), FISABIO Hospital [1–5] include both chest and upper abdomi- trast-enhanced CT protocol. These include
General Universitario de Alicante, Av Pintor Baeza 12, nal contrast-enhanced CT. CT acquisition parameters (length, kilovolt-
03010, Alicante, Spain. Address correspondence to The introduction of MDCT technology has age, milliamperage), patient characteristics
J. J. Arenas-Jiménez (arenas_jua@gva.es).
dramatically decreased scanning time, mak- (weight, height, cardiovascular condition),
2
Department of Epidemiology, Hospital General ing it necessary to adjust contrast injection and the contrast medium (quantity, concen-
Universitario de Alicante, Instituto de Investigación and scanning parameters to the capabilities of tration, rate of injection, delay) [6]. No single
Sanitaria y Biómedica de Alicante (ISABIAL), FISABIO these new technologies [6]. The role of iodin- standardized protocol exists for performing
Hospital General Universitario de Alicante, Alicante, Spain. ated contrast medium in these examinations combined thoracic and abdominal CT, and
Supplemental Data is to achieve adequate depiction of hilar and imaging guidelines for lung cancer lack spe-
Available online at www.ajronline.org. mediastinal vascular structures together with cific scanning protocol recommendations [1–
optimal enhancement of tumoral lesions and 5]. When a protocol is suggested, the level of
AJR 2018; 210:1226–1234
abdominal viscera. The literature on scan- evidence is low and primarily based on ex-
0361–803X/18/2106–1226 ning parameters for routine chest or combined pert opinion [15–18].
chest and abdominal CT is limited; a few re- In contemporary clinical practice with
© American Roentgen Ray Society ports have focused on the influence of contrast newer technologies, there are two commonly
1226 AJR:210, June 2018
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
Thoracic and Abdominal CT of Lung Cancer
accepted methods for performing combined
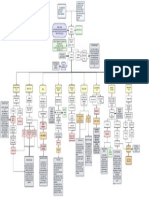
contrast-enhanced CT of the chest and abdo- Patients referred to department for combined chest and abdominal contrast-enhanced
CT as initial workup or follow-up of lung cancer
men. The first incorporates a single delayed 419 Patients (557 examinations)
acquisition that includes the chest and up-
per abdomen. The second method consists of Exclusion: Estimated glomerular filtration rate less than 60 mL/min, 40 (46)
two independent CT acquisitions: CT of the Iodinated contrast material allergy, 11 (13)
Injection protocol not achieved properly, 10 (11)
chest in an early phase after contrast injec- Underweight or overweight, 4 (7)
tion and CT of the upper abdomen including Declined by patient, 1 (1)
the liver in a portal phase. Protocol recom-
mendations [15–18] and literature including Patients with combined chest and abdominal contrast-enhanced CT as initial workup
data about scanning protocols [7–14, 19, 20] or follow-up of lung cancer
353 Patients (479 examinations)
also are divided on the use of one or two sep-
arate acquisitions for combined chest and ab- Exclusion: 276 Patients with only one CT scan
dominal CT. It is therefore unclear whether a
single delayed phase acquisition of the chest Final study population
and abdomen provides adequate vascular at- 77 Patients (203 examinations)
tenuation of the chest while maintaining ad-
equate image quality in the abdomen.
Fig. 1—Flowchart shows exclusion and inclusion criteria for study. Values in parentheses are number of CT
The purpose of our study was to evaluate examinations.
the superiority of either of two protocols (sin-
gle vs dual acquisition) for combined con- TABLE 1: Patient Demographic Data and Tumor Characteristics
trast-enhanced thoracic and abdominal CT
in patients with lung cancer by comparing Characteristic Value
contrast enhancement, contrast-related arti- Sex
facts, image quality, and radiation dose. The Male 55 (71.4)
double acquisition protocol included two in-
dependent acquisitions of the chest (ear- Female 22 (28.6)
ly phase) and the abdomen (delayed phase). Age (y) 64.1 (42–83)
The single scan acquisition included both the Weight (kg) 71.6 (50–100)
chest and abdomen in the delayed phase.
Height (cm) 166.3 (150–182)
Subjects and Methods Histologic result
This prospective randomized controlled cross- Adenocarcinoma 40 (51.9)
over clinical trial was reviewed and approved by Squamous 20 (26.0)
the institutional review board and local ethics
Small cell 15 (19.5)
committee. Written informed consent was ob-
tained from all participants in the study. Non–small cell (not otherwise specified) 2 (2.6)
Stage
Patient Population IA 6 (7.8)
From May to December 2015, patients referred to
IB 5 (6.5)
our department for combined chest and abdominal
contrast-enhanced CT as initial workup or follow- IIA 4 (5.2)
up of lung cancer were enrolled in the study. Patients IIB 2 (2.6)
were excluded if they had an estimated glomerular IIIA 7 (9.1)
filtration rate less than 60 mL/min, if they had an
IIIB 4 (5.2)
allergy to iodinated contrast material, or if the con-
trast injection protocol could not be achieved as re- IV 49 (63.6)
quired owing to inadequate vein access, extravasa- Treatment
tion, or any other problem during contrast injection. Chemotherapy 43 (55.8)
Patients weighing less than 50 kg or more than 100
Chemoradiotherapy 17 (22.1)
kg were excluded. When the patients were enrolled,
they were initially randomized to one of the two Surgery 13 (16.9)
scanning protocols, A or B. On each subsequent im- Surgery and chemotherapy 3 (3.9)
aging visit, the other protocol was used. Radiotherapy 1 (1.3)
We initially enrolled 419 patients in the study
Note—Values are number of patients with percentage in parentheses or mean with range in parentheses.
for a total of 557 CT examinations. The patient Stage is based on the system set out in the 7th edition of the American Joint Committee on Cancer lung cancer
enrollment flowchart is shown in Figure 1. After staging manual.
AJR:210, June 2018 1227
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
García-Garrigós et al.
exclusions, the final study population consisted 16 × 1.5 mm; pitch, 1.2; rotation time, 0.6 sec- CT images at a PACS workstation (Centricity
of 203 scans of 77 patients. Patient characteris- ond; reference tube current–time product, 170 PACS Universal Viewer 6.0, GE Healthcare). They
tics, histologic results, staging, and treatments are mAs at 110 kVp. Automatic tube current modula- were instructed to begin reading at the 5-mm ab-
detailed in Table 1. The number of CT examina- tion (CARE Dose 4D, Siemens Healthcare) was dominal series to avoid interpretation bias due to
tions per patient ranged from two to six; 101 were switched on for all examinations. knowledge of the imaging protocols, which can be
performed with protocol A and 102 with proto- Image reconstruction was performed with a more apparent in chest series.
col B. Weight and height were obtained from pa- medium-smooth soft-tissue kernel (B30) at a slice Quantitative assessment—Quantitative assess-
tient clinical charts. There were no statistically thickness of 5 mm without overlap and a slice ment was performed by placing a circular ROI of
significant differences in patient sex, age, weight, thickness of 2 mm with 1.2-mm interval (one in- approximately 1.5 cm2 in the 5-mm-thickness re-
or height in the two protocol groups. dependent series each for the chest and another for constructions and measuring attenuation values in
the abdomen) and with a high-spatial-frequency Hounsfield units. Thoracic vascular attenuation
CT Protocols reconstruction kernel (B70) at a slice thickness of measurements were performed in the pulmonary
All CT scans were obtained with a 16-MDCT 2 mm with 1.2-mm interval for the chest. Finally, trunk at the level of the bifurcation and in the as-
scanner (Somatom Emotion 16, Siemens Health- five series were reconstructed for each patient and cending and descending thoracic aorta, all at the
care). Protocol A consisted of two acquisitions, sent to the PACS in the same order for all patients same slice level. Abdominal attenuation measure-
one of the chest ending at the lung bases beginning independently of the scanning protocol used. All ments were in the left hepatic lobe, anterior and
35 seconds after the initiation of contrast admin- images were reviewed at a PACS workstation at posterior right hepatic lobes, right erector spinae
istration. This was followed by a 70-second de- window settings appropriate for viewing the lung muscle, spleen, and aorta at the level of the main
layed abdominal acquisition starting at the dome parenchyma (level, −700 HU; width, 1500 HU) and portal vein, all at the same slice level.
of the diaphragm and extending inferiorly. In this the mediastinum (level, 50 HU; width, 400 HU). The size of the ROI in the muscle was adapted
way there was always overlap of the two acquisi- All patients received a standardized IV injection to avoid inclusion of fat in the measurement. Ves-
tions. In protocol B, the acquisition coverage was through a power injector consisting of iomeprol sels, bile ducts, focal steatosis, and other focal le-
the same as in protocol A, but a single acquisition (Iomeron, Bracco) with either 350 or 400 mg I/mL sions were avoided when placing the ROI in the
was performed at 60-second delay. at a dose of 0.5 g I/kg body weight fixed 40-sec- liver and spleen. When there was clearly promi-
In both protocols scanning was performed in ond duration of injection followed by a 30-mL sa- nent diffuse hepatic steatosis, liver attenuation
the craniocaudal orientation with the patient in line chaser at the same rate as for the contrast medi- measurements from that patient were excluded
supine position with arms above the head. Acqui- um. Contrast concentration was not controlled and from analysis by consensus of the two readers. SD
sition began approximately 2 cm above the lung was subject to availability at the time of the CT ex- of the measurement of the anterior right hepatic
apices to include the supraclavicular regions and amination. No specific instructions were given to lobe was registered as image noise. Mean attenu-
extended through the upper abdomen to include the technicians to choose a specific concentration. ation of the liver was calculated as the average of
the whole liver. Dose-length product provided by the CT scanner the three hepatic measurements. Contrast-to-noise
Scan parameters for protocol A were as fol- was recorded for each examination. ratio (CNR) and signal-to-noise ratio (SNR) of the
lows: collimation, 16 × 1.5 mm; pitch, 1.2; ro- liver were calculated according to the following
tation time, 0.6 second; reference tube current– Image Analysis formulas [13, 21]: CNR = (mean attenuation of the
time products, 150 mAs for the chest and 200 Two thoracic radiologists (10 and 20 years of liver − ROI attenuation of the muscle) / noise of
mAs for the abdomen at 110 kVp. Scan param- thoracic CT interpretation experience) blinded to the liver; SNR = mean attenuation of the liver /
eters for protocol B were as follows: collimation, the acquisition protocol independently reviewed noise of the liver.
A B
Fig. 2—57-year-old man with squamous lung carcinoma.
A and B, Axial contrast-enhanced helical CT scans obtained with protocols A (A) and B (B) show severe perivenous artifact limiting evaluation of lymph node at 4R nodal
station (arrow). Protocol B (B) shows absence of perivenous artifacts and excellent delimitation of node at 4R station (arrow).
1228 AJR:210, June 2018
TABLE 2: Quantitative Analysis Results for Protocols A and B Qualitative analysis—Qualitative analysis was
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
Thoracic and Abdominal CT of Lung Cancer
performed in 5-mm-thick reconstructions. Perive-
Protocol A Protocol B
(n = 101) (n = 102) nous artifacts at three levels (subclavian and axil-
lary veins on the side of injection, supraclavicular
Characteristic Reader Mean SD Mean SD p region on the side of injection, and bilateral bra-
Pulmonary artery attenuation (HU) 1 331.8 75.6 200.6 23.8 0.000 chiocephalic veins or superior vena cava) were
graded as follows: 1, no artifact; 2, artifact present
2 329.5 73.1 199.7 22.9 0.000
not interfering with evaluation; 3, severe artifact
Pulmonary artery noise (HU) 1 12.5 2.5 10.1 2.1 0.000 limiting evaluation. Similarly, evaluation of poten-
2 13.4 2.6 10.6 1.9 0.000 tial lymph nodes adjacent to the vessels in the axil-
Ascending aorta attenuation (HU) 1 317.2 50.8 203.0 28.4 0.000 lary and subclavian regions, supraclavicular region,
levels 2R and 2L, and level 4R was graded accord-
2 312.5 57.2 202.3 27.5 0.000
ing to the following scale: 1, excellent, vessels and
Descending aorta attenuation (HU) 1 297.1 48.7 193.1 32.4 0.000 surrounding tissue clearly defined; 2, good, some
2 295.4 51.7 194.9 30.8 0.000 evident artifacts present but not limiting evaluation;
Abdominal aorta attenuation (HU) 1 166.7 22.2 185.5 25.7 0.000 3, poor, severe artifacts potentially limiting lymph
node margins and subsequent measurements.
2 167.2 20.2 183.6 24.2 0.000
Presence of possible atelectasis associated with
Anterior right hepatic lobe attenuation (HU)a 1 118.6 14.1 122.2 14.3 0.081 the tumor was evaluated. When it was found, ob-
2 117.5 18.1 120.6 16.7 0.208 servers were asked to grade tumor delineation
Anterior right hepatic lobe noise (HU) 1 12.2 2.6 12.3 3.0 0.752 from surrounding tissues in the chest series on
the following scale: 1, excellent delineation of
2 11.9 2.1 12.4 2.7 0.154
the tumor; 2, acceptable differentiation of tumor
Posterior right hepatic lobe attenuation (HU)a 1 113.9 13.4 117.2 13.7 0.090 margins from possible atelectasis; and 3, bad de-
2 113.5 13.0 116.2 13.8 0.161 lineation of the tumor. They also evaluated the
Left hepatic lobe attenuation (HU)a 1 120.9 15.5 124.1 14.3 0.129 presence of pleural effusion; when they found it,
they graded visualization of pleural thickening or
2 119.8 14.4 124.8 13.4 0.011
nodules according to the following scale: 1, excel-
Mean hepatic attenuation (HU)a 1 117.8 13.5 121.2 12.4 0.070 lent definition; 2, acceptable definition; 3, poor
2 116.9 13.8 120.5 13.1 0.059 definition. In the same way, they were asked to de-
Splenic attenuation (HU) 1 118.3 12.5 134.5 19.0 0.000 termine the visual assessment of the liver on the
following scale: 1, excellent definition; 2, accept-
2 118.6 11.7 134.5 17.2 0.000
able definition; 3, poor definition.
Hepatic contrast-to-noise ratioa 1 5.7 1.8 6.1 2.1 0.240 The presence of hepatic metastases was evaluat-
2 5.7 1.6 5.7 1.8 0.892 ed, and if there were any suspicious lesions, quali-
Hepatic signal-to-noise ratioa 1 10.1 2.6 10.5 2.9 0.432 tative analysis of tumor conspicuity was performed
independently in the thoracic and abdominal series
2 10.1 2.2 10.1 2.5 0.889
with the same criteria as for the liver. Finally, noise
Dose-length product (mGy · cm) 645.0 159.9 521.5 96.7 0.000 in the liver images was subjectively graded on the
an = 100 in protocol A and n = 101 in protocol B owing to exclusion of one patient with diffuse hepatic steatosis.
following 5-point scale: 1, no appreciable noise;
A B
Fig. 3—64-year-old man with lung adenocarcinoma.
A and B, Axial contrast-enhanced helical CT scans were obtained with protocols A (A) and B (B). Protocol A (A) shows poor tumor delineation (asterisk) from pleural
effusion (arrowhead) and 4R lymph node (arrow). Perivenous artifact is present at superior vena cava. Scan obtained 3 months later using protocol B (B) shows excellent
differentiation of the tumor (asterisk), pleural effusion (arrowhead), and 4R lymph node (arrow).
AJR:210, June 2018 1229
2, minimum noise; 3, average noise not disturb- TABLE 3: Qualitative Analysis Results for Protocols A and B
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
García-Garrigós et al.
ing liver evaluation; 4, above average noise; 5, too
Grade Protocol A (n = 101) Protocol B (n = 102) p
much noise, potentially limiting evaluation.
Presence or absence of pulmonary embolism Axillary lymph nodes 0.000
was assessed on 2-mm-thickness images. When Reader 1
present it was classified as central (segmental or
1 2 (2.0) 27 (26.5)
proximal pulmonary arteries), peripheral, or both.
2 1 (1.0) 38 (37.3)
Statistical Analysis 3 98 (97.0) 37 (36.3)
The two protocol groups were compared by Reader 2 0.000
chi-square test for sex and age and unpaired t test
1 1 (1.0) 35 (34.3)
for weight and height. The quantitative measure-
ments between the two protocol groups and be- 2 2 (2.0) 35 (34.3)
tween iodine concentrations were compared by 3 98 (97.0) 32 (31.4)
t test. A paired t test was used to compare consec- Supraclavicular lymph nodes
utive measurements between the two protocols in
Reader 1 0.000
the same patient. The qualitative analysis results
were compared between protocols by chi-square 1 0 (0.0) 58 (56.9)
test. Weighted kappa statistics were used to mea- 2 16 (15.8) 35 (34.3)
sure the degree of agreement between observers 3 85 (84.2) 9 (8.8)
in evaluation of qualitative variables. Statistical
Reader 2 0.000
analysis was performed with the software package
SPSS Statistics (version 21, IBM). Statistical sig- 1 0 (0.0) 71 (69.6)
nificance was set at 0.05. 2 19 (18.8) 22 (21.6)
3 82 (81.2) 9 (8.8)
Results
2R Lymph nodes
Quantitative Assessment
The mean enhancement of the pulmonary Reader 1 0.000
artery, ascending aorta, and descending aorta 1 6 (5.9) 102 (100.0)
was significantly greater with protocol A than 2 37 (36.7) 0 (0.0)
with protocol B for both independent observ-
3 58 (57.4) 0 (0.0)
ers (Table 2). Pulmonary artery enhancement
was less than 150 HU in two examinations Reader 2
performed with protocol B and less than 211 1 6 (5.9) 99 (97.0)
HU in five performed with protocol A. There 2 28 (27.7) 2 (2.0)
were no statistically significant differences
3 67 (66.3) 1 (1.0)
in any abdominal liver attenuation measure-
ments or in calculated abdominal CNR and 4R Lymph nodes
SNR measurements except for left hepatic Reader 1 0.000
lobe attenuation by reader 2, which was high- 1 5 (5.0) 102 (100.0)
er with protocol B (Table 2). There was statis-
2 41 (40.6) 0 (0.0)
tically significant greater enhancement of the
spleen and abdominal aorta with protocol B. 3 55 (54.5) 0 (0.0)
When paired t test analysis was performed on Reader 2 0.000
a subset of 182 consecutive examinations (91 1 5 (5.0) 102 (100.0)
paired consecutive examinations with proto-
2 35 (34.6) 0 (0.0)
col A and B in the same patients), differenc-
es between protocols were also statistically 3 61 (60.4) 0 (0.0)
significant in the thoracic vessels, spleen, and Hepatic parenchymal enhancement
abdominal aorta for both readers. Reader 1 0.474
Regarding the effect of contrast iodine
1 97 (96.0) 97 (95.1)
concentration, pulmonary artery attenuation
with protocol A showed greater enhance- 2 3 (3.0) 5 (4.9)
ment with the lower concentration of iodinat- 3 1 (1.0) 0 (0.0)
ed contrast medium. There was otherwise no Reader 2 0.745
statistically significant difference in vascular
1 97 (96.0) 97 (95.1)
or parenchymal enhancement between the
two iodine concentration groups (Table S1). 2 4 (4.0) 5 (4.9)
Dose-length product was statistically 3 0 (0.0) 0 (0.0)
significant higher with protocol A than with (Table 3 continues on next page)
1230 AJR:210, June 2018
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
Thoracic and Abdominal CT of Lung Cancer
TABLE 3: Qualitative Analysis Results for Protocols A and B (continued) TABLE 4: Kappa Correlation B etween
Readers in Q ualitative
Grade Protocol A (n = 101) Protocol B (n = 102) p Variables Assessment
Hepatic noise
Variable κ
Reader 1 0.204
Axillary lymph nodes 0.760
1 0 (0.0) 0 (0.0)
Supraclavicular lymph nodes 0.800
2 32 (31.7) 34 (33.3)
2R Lymph nodes 0.845
3 69 (68.3) 65 (63.7)
4R Lymph nodes 0.854
4 0 (0.0) 3 (2.9)
Hepatic parenchymal enhancement 0.884
5 0 (0.0) 0 (0.0)
Hepatic noise 0.556
Reader 2 0.697
Axillary vein artifact 0.710
1 0 (0.0) 0 (0.0)
Supraclavicular vein artifact 0.715
2 44 (44.0) 40 (39.2)
Vena cava artifact 0.881
3 56 (55.0) 60 (58.8)
4 1 (1.0) 2 (2.0)
tistically significant (Table 3). Subsequently,
5 0 (0.0) 0 (0.0) mediastinal lymph nodes levels were judged
Axillary artifact to be evaluated worse with protocol A than
Reader 1 0.000
with B. Neither liver assessment score nor
subjective noise grade exhibited statistical-
1 1 (1.0) 17 (16.7) ly significant differences between protocols
2 0 (0.0) 46 (45.1) (Table 3).
3 100 (99.0) 39 (38.2) Agreement between observers was good
Reader 2 0.000
to excellent for the qualitative variables, ex-
cept for hepatic noise evaluation, which had a
1 1 (1.0) 25 (24.5) kappa value of 0.556 (Table 4). Tumor delin-
2 2 (2.0) 43 (42.2) eation was evaluated by readers 1 and 2 using
3 98 (97.0) 34 (33.3) both protocols for 19 readings in 14 patients.
Protocol B performed better than protocol A
Supraclavicular artifact
(Fig. 3) in 13 cases interpreted by reader 1
Reader 1 0.000 and 10 cases by reader 2. In contrast, only
1 2 (2.0) 47 (46.1) one reading performed better with protocol
2 7 (6.9) 47 (46.1) A than with protocol B.
The thoracic phase was compared with
3 92 (91.1) 8 (7.8)
the abdominal phase of protocol A for
Reader 2 0.000 grading of pleural findings, including pleu-
1 0 (0.0) 66 (64.7) ral thickening and nodules associated with
2 18 (17.8) 27 (26.5) pleural effusions in 37 examinations. In 18
cases, both observers scored pleural findings
3 83 (82.2) 9 (8.8)
better during the abdominal phase of proto-
Caval artifact col A (Fig. 4). Mean scores for both proto-
Reader 1 0.000 col B and the abdominal phase of protocol
1 2 (2.0) 98 (96.1) A (reader 1, 1.28; reader 2, 1.19) were better
than for the early phase of protocol A (read-
2 34 (33.7) 4 (3.9)
er 1, 1.83; reader 2, 1.72; p < 0.001), a score
3 65 (64.4) 0 (0.0) of 1 being excellent definition and 3 poor
Reader 2 0.000 definition of pleural findings.
1 2 (2.0) 96 (94.1) Hepatic metastases were evaluated by
both observers for 20 examinations of nine
2 32 (31.7) 6 (5.9)
patients. There was no interobserver dis-
3 67 (66.3) 0 (0.0) agreement on lesion detectability between
Note—Values in parentheses are percentages. protocols A and B. Nine examinations were
performed with protocol A. In three of them,
B (645.0 ± 159.9 vs 521.5 ± 96.7 mGy · cm; Visual Assessment both thoracic and abdominal phases were
p < 0.0001) because of overlap of thoracic and Contrast-related perivenous artifacts (Fig. graded 1 by both observers. In the other six
abdominal acquisitions and a higher reference 2) were more severe with protocol A for all examinations, observers scored the abdomi-
tube current–time product for the abdomen. levels evaluated, and the difference was sta- nal phase better than the thoracic phase.
AJR:210, June 2018 1231
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
García-Garrigós et al.
Pulmonary embolism was diagnosed in specifically, whether a single delayed acqui- subclavian, and brachiocephalic veins and the
eight patients, five with protocol A (one cen- sition of the chest and abdomen provides ad- superior vena cava [6, 25].
tral, four both central and peripheral) and equate vascular enhancement in the chest As expected, there were obvious differ-
three with protocol B (one central, one pe- while maintaining image quality in the ab- ences in contrast enhancement of thoracic
ripheral, and one both central and peripher- domen. In this setting, we conducted a ran- vessels between the two protocols; greater
al). When available, previous CT scans were domized trial to evaluate these protocols and attenuation was found in the early phase of
reviewed for potentially missed pulmonary determine whether differences exist between protocol A than in protocol B for all levels
emboli, although none were discovered. these scanning options. analyzed. In the vast majority of patients, at-
A primary concern with use of an ear- tenuation values for the aorta and pulmonary
Discussion ly phase in contrast-enhanced chest CT, is artery were greater than 200 HU with pro-
Contrast-enhanced CT of the chest and the presence of perivenous artifacts caused tocol A, a level acceptable for angiographic
upper abdomen plays an essential role in by concentrated contrast medium entering studies. For protocol B, levels were greater
staging and follow-up of lung cancer. How- through the superior vena cava. When se- than 150 HU in most patients, a value con-
ever, appropriate recommendations for the vere, these artifacts can blur perivascular sidered acceptable for routine chest scanning
optimal scanning protocol are lacking. The structures and limit evaluation of mediastinal [17]. More than 93% of patients undergoing
goals of the radiologist in combined contrast- lymph nodes, particularly the superior medi- protocol A had attenuation greater than 211
enhanced CT of the chest and abdomen are astinal chains. Use of a saline chaser bolus HU, a value that Wittram [26] suggested is
to achieve optimal contrast opacification of after contrast injection reduces contrast dose the theoretic minimum attenuation required
systemic and pulmonary vessels, avoid con- and artifacts in the chest [22, 23], although to see pulmonary venous thromboemboli;
trast-related artifacts, and obtain adequate this has no effect on liver enhancement [24]. only 35% of patients receiving protocol B did
contrast enhancement of lesions, the liver, In our series, the frequency of substantial so. From our point of view, however, attenu-
and other viscera. contrast-related perivenous artifacts in proto- ation values achieved in protocol B are suit-
In clinical practice, two distinct protocols col A was greater than that in other studies able for routine clinical evaluation of the me-
exist for combined contrast-enhanced chest [8, 22, 23]. However, most of the patients in diastinal and vascular structures with chest
and abdominal CT. The first is similar to that those studies received a lower total dose of io- CT. It can be assumed that protocol B is less
used in classic single-detector scanners with dine and had shorter injection times than our effective for detecting pulmonary emboli,
one early (20- to 35-second delayed) acquisi- patients did. Regarding contrast-related peri- but in general we are not seeking pulmonary
tion for the chest and a second delayed por- venous artifacts, our results show benefits of emboli when performing CT for lung cancer
tal venous phase for the abdomen. The sec- a 60-second delayed chest scan. The reasons evaluation. Although unsuspected pulmo-
ond protocol consists of a single acquisition for this are likely twofold. On one hand, the nary embolism involving peripheral pulmo-
covering the whole chest and upper abdomen contrast delay with saline push promotes ap- nary arteries is fairly frequent in this popula-
with a scanning delay that includes the liv- propriate contrast washout and clearing of the tion [27], this would not make us change our
er during the portal venous phase. However, veins [23]. On the other hand, contrast medi- primary imaging objectives.
information is lacking about the advantages um is already recirculating, resulting in op- One of the advantages of delayed scan-
and disadvantages of these protocols, more timal, homogeneous enhancement of jugular, ning of the chest is theoretic optimal contrast
A B
Fig. 4—48-year-old woman with lung adenocarcinoma and metastatic pleural effusion.
A, Axial contrast-enhanced helical CT scan obtained with protocol B shows excellent definition of pleural thickening at costal and mediastinal pleura (arrows) graded 1
by both observers.
B, Axial early phase contrast-enhanced CT scan obtained with protocol A 3 months after A shows acceptable definition of pleural thickening (arrows) graded 2 by both
observers.
1232 AJR:210, June 2018
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
Thoracic and Abdominal CT of Lung Cancer
opacification of tumoral lesions due to tim- hancement and quality. Moreover, attenua- Conclusion
ing of the contrast bolus, greater contrast dis- tion of the spleen and abdominal aorta was For patients with lung cancer, a single
tribution occurring in the extravascular in- even higher with protocol B. 60-second delayed acquisition for contrast-
terstitial space. In thoracic imaging, this is As also shown in other studies [8, 9], use enhanced CT of the chest and abdomen is
particularly relevant for evaluation of pleural of protocol A resulted in a higher degree of preferable to two separate acquisitions. It
thickening, tumoral lesions accompanying enhancement of the pulmonary artery with decreases contrast-related perivenous ar-
pleural effusions, and differentiation and de- a lower iodine contrast concentration. How- tifact, facilitates evaluation of mediastinal
lineation of lung tumors. The British Thorac- ever, iodine concentration has been found [9, lymph node stations and pleural lesions, and
ic Society statement on malignant mesothe- 33] to have no effect on liver enhancement. improves tumor delineation. These bene-
lioma [16] recommends a 60-second delayed The primary advantage of higher concentra- fits are achieved while the same abdominal
scan for this specific reason. Pleural thicken- tion of contrast medium is allowing a lower enhancement and quality are maintained at
ing or nodules can be difficult to distinguish injection rate to provide the same amount of lower but acceptable thoracic vascular en-
during the early phases of contrast-enhanced iodine injected for a specific time. hancement and a lower radiation dose.
chest CT owing to lack of contrast enhance- Finally, although the primary purpose of
ment. This is particularly true in compari- our study was to acquire scientific evidence Acknowledgments
sons of data from pulmonary CT angiog- and establish imaging protocol recommen- We thank Aaron Frodsham and Mariana
raphy with data from routine thoracic CT dations for CT of the chest in lung cancer, Planells Alduvin for assistance in the lin-
during the venous phase, as shown in a recent our results can be extrapolated to routine guistic revision process.
report [28] on the diagnostic performance of contrast-enhanced CT of the chest, abdomen,
routine CT in patients with suspected pleural and pelvis for other neoplasms. References
malignancy. Using 60-second delayed scan- Our study had limitations. First, we fo- 1. Ettinger DS, Wood D, Aisner DL, et al. NCCN
ning, Raj et al. [29] found greater contrast of cused on comparing a primary variable in Clinical Practice Guidelines in Oncology (NCCN
pleural surfaces using higher doses of con- the combined chest and abdominal CT scan Guidelines): non-small cell lung cancer, version
trast medium. In our series, images from the protocol, which is the delay after the start of 8.2017. www.nccn.org/professionals/physician_gls/
abdominal phase in either protocol A or pro- contrast administration. It can be argued that pdf/nscl.pdf. July 14, 2017. Accessed August 8, 2017
tocol B scored better than the early phase of variation of other variables could overcome 2. Novello S, Barlesi F, Califano R, et al. Metastatic
the chest scan. Regarding delineation of lung some of the problems detected in the evalu- non-small-cell lung cancer: ESMO clinical prac-
tumors, their appearance and differentiation ation of the images. However, the contrast in- tice guidelines for diagnosis, treatment and fol-
from atelectasis is variable. According to our jection parameters (overall contrast dose, de- low-up. Ann Oncol 2016; 27(suppl 5):v1–v27
results, however, in 14 patients with persis- livery rate, injection duration, saline chaser 3. Silvestri GA, Gonzalez AV, Jantz MA, et al. Meth-
tent tumoral lesions and atelectasis on two volume and rate) and the scanning parameters ods for staging non-small cell lung cancer: diagno-
consecutive scans, protocol B was superior (tube voltage and current, pitch, and others) sis and management of lung cancer, 3rd ed—Ameri-
to protocol A in most cases. were selected according to established clini- can College of Chest Physicians evidence-based
To our knowledge, no study has system- cal practices and existing evidence in the liter- clinical practice guidelines. Chest 2013; 143(5
atically evaluated the need for an arterial ature. Second, 110-kV tube voltage was used suppl):e211S–e250S
phase of the liver in imaging of metastases because of our existing manufacturer volt- 4. National Institute for Health and Care Excellence
of lung cancer. Therefore, these CT scans are age configuration. When designing the study, website. Lung cancer: diagnosis and manage-
usually obtained only in the portal phase [9, we chose the 16-MDCT among the available ment—clinical guideline CG121. www.nice.org.
19]. In our series, liver lesion definition was scanners at our institution for being one of the uk/guidance/cg121. Published April 2011. Ac-
considered better in the delayed abdominal most commonly used scanners at radiology cessed June 1, 2017
phase than in the thoracic phase in 66% of facilities. Scanning times are similar for most 5. Lim E, Baldwin D, Beckles M, et al. Guidelines
scans showing metastases in both phases. 16-MDCT scanners, although that tube volt- on the radical management of patients with lung
For adequate tumor–to–normal liver con- age is not so broadly extended. The lower tube cancer. Thorax 2010; 65(suppl 3):1–27
trast, the most important factors to be con- voltage compared with 120 kV could increase 6. Bae KT. Intravenous contrast medium administra-
sidered are the total amount of iodine deliv- attenuation values. Although further studies tion and scan timing at CT: considerations and ap-
ered and body weight [6, 19]. For this reason, are necessary for confirmation, we routinely proaches. Radiology 2010; 256:32–61
protocols for patients with cancer must take perform similar scanning protocols with other 7. Loubeyre P, Debard I, Nemoz C, Minh VA. Using
into consideration the contrast dose adapted scanners using both 100 kV and 120 kV with thoracic helical CT to assess iodine concentration
to the patient’s specific body characteristics, similar clinically acceptable results. The same in a small volume of nonionic contrast medium
as in our study. Although other body size in- applies to tube current, which was fairly high during vascular opacification: a prospective study.
dexes have been suggested [30], body weight in both protocols. Weight-based tube volt- AJR 2000; 174:783–787
at doses of 0.5–0.6 g I/kg is the most fre- age and current should be applied in routine 8. Setty BN, Sahani DV, Ouellette-Piazzo K, Hahn
quently used owing to its simplicity [17, 19, practice. Third, while reading the images, the PF, Shepard JA. Comparison of enhancement, im-
31, 32]. Contrast enhancement, noise, calcu- observers could suspect which protocol was age quality, cost, and adverse reactions using 2
lated CNR and SNR, and visual assessment used in each case, leading to possible interpre- different contrast medium concentrations for rou-
of the liver were not different for the portal tation bias. To partially overcome this prob- tine chest CT on 16-slice MDCT. J Comput Assist
phases of the two protocols, making both ab- lem, the readers were asked to begin reading Tomogr 2006; 30:818–822
dominal phases equivalent in terms of en- during the abdominal phase. 9. Behrendt FF, Mahnken AH, Stanzel S, et al. Intra-
AJR:210, June 2018 1233
Downloaded from www.ajronline.org by 2001:8a0:e046:1401:1568:53a6:a1e5:a44e on 01/02/21 from IP address 2001:8a0:e046:1401:1568:53a6:a1e5:a44e. Copyright ARRS. For personal use only; all rights reserved
García-Garrigós et al.
individual comparison of contrast media concen- 18. Williams S. General techniques for examinations first-pass direct versus delayed-phase indirect
trations for combined abdominal and thoracic discussing CT, biopsy and MRI. In: Nicholson T, multidetector CT venography. Clin Imaging 2015;
MDCT. AJR 2008; 191:145–150 ed. Recommendations for cross-sectional imag- 39:412–416
10. Mühlenbruch G, Behrendt FF, Eddahabi MA, et ing in cancer management, 2nd ed. London, UK: 26. Wittram C. How I do it: CT pulmonary angiogra-
al. Which iodine concentration in chest CT? A Royal College of Radiologists, 2014 phy. AJR 2007; 188:1255–1261
prospective study in 300 patients. Eur Radiol 19. Fleischmann D, Kamaya A. Optimal vascular and 27. Shinagare AB, Okajima Y, Oxnard GR, et al. Un-
2008; 18:2826–2832 parenchymal contrast enhancement: the current state suspected pulmonary embolism in lung cancer
11. Behrendt FF, Plumhans C, Keil S, et al. Contrast of the art. Radiol Clin North Am 2009; 47:13–26 patients: comparison of clinical characteristics
enhancement in chest multidetector computed to- 20. García Garrigós E, Arenas Jiménez JJ, Sánchez and outcome with suspected pulmonary embo-
mography: intraindividual comparison of 300 Payá J, Sirera Matilla M, Gayete Cara À. Com- lism. Lung Cancer 2012; 78:161–166
mg/ml versus 400 mg/ml iodinated contrast me- puted tomography protocols used in staging bron- 28. Tsim S, Stobo DB, Alexander L, Kelly C, Blyth
dium. Acad Radiol 2009; 16:144–149 chopulmonary carcinoma: results of a national KG. The diagnostic performance of routinely ac-
12. Sigal-Cinqualbre AB, Hennequin R, Abada HT, survey. Radiologia 2016; 58:460–467 quired and reported computed tomography imag-
Chen X, Paul JF. Low-kilovoltage multi-detector 21. Szucs-Farkas Z, Strautz T, Patak MA, et al. Is ing in patients presenting with suspected pleural
row chest CT in adults: feasibility and effect on body weight the most appropriate criterion to se- malignancy. Lung Cancer 2017; 103:38–43
image quality and iodine dose. Radiology 2004; lect patients eligible for low-dose pulmonary CT 29. Raj V, Kirke R, Bankart MJ, Entwisle J. Multidetec-
231:169–174 angiography? Analysis of objective and subjective tor CT imaging of pleura: comparison of two contrast
13. Mayer C, Meyer M, Fink C, et al. Potential for ra- image quality at 80 kVp in 100 patients. Eur infusion protocols. Br J Radiol 2011; 84:796–799
diation dose savings in abdominal and chest CT Radiol 2009; 19:1914–1922 30. Awai K, Kanematsu M, Kim T, et al. The optimal
using automatic tube voltage selection in combi- 22. Hopper KD, Mosher TJ, Kasales CJ, TenHave TR, body size index with which to determine iodine
nation with automatic tube current modulation. Tully DA, Weaver JS. Thoracic spiral CT: delivery dose for hepatic dynamic CT: a prospective multi-
AJR 2014; 203:292–299 of contrast material pushed with injectable saline center study. Radiology 2016; 278:773–781
14. Lurz M, Lell MM, Wuest W, et al. Automated tube solution in a power injector. Radiology 1997; 31. Yamashita Y, Komohara Y, Takahashi M, et al.
voltage selection in thoracoabdominal computed 205:269–271 Abdominal helical CT: evaluation of optimal dos-
tomography at high pitch using a third-generation 23. Haage P, Schmitz-Rode T, Hübner D, Piroth W, es of intravenous contrast material—a prospective
dual-source scanner: image quality and radiation Günther RW. Reduction of contrast material dose randomized study. Radiology 2000; 216:718–723
dose performance. Invest Radiol 2015; 50:352–360 and artifacts by a saline flush using a double pow- 32. Johnson PT, Fishman EK. IV contrast selection
15. Hopper KD, Singapuri K, Finkel A. Body CT and er injector in helical CT of the thorax. AJR 2000; for MDCT: current thoughts and practice. AJR
oncologic imaging. Radiology 2000; 215:27–40 174:1049–1053 2006; 186:406–415
16. British Thoracic Society Standards of Care Com- 24. Takao H, Nojo T, Ohtomo K. Use of a saline chas- 33. Rengo M, Caruso D, De Cecco CN, et al. High
mittee. BTS statement on malignant mesothelioma er in abdominal computed tomography: a system- concentration (400 mgI/mL) versus low concen-
in the UK, 2007. Thorax 2007; 62(suppl 2):1–19 atic review. Clin Imaging 2009; 33:261–266 tration (320 mgI/mL) iodinated contrast media in
17. Bae KT. Optimization of contrast enhancement in 25. Sundaram B, Kuriakose JW, Stojanovska J, multi detector computed tomography of the liver:
thoracic MDCT. Radiol Clin North Am 2010; Watcharotone K, Parker RA, Kazerooni EA. Tho- a randomized, single centre, non-inferiority study.
48:9–29 racic central venous evaluation: comparison of Eur J Radiol 2012; 81:3096–3101
F O R YO U R I N F O R M AT I O N
A data supplement for this article can be viewed in the online version of the article at: www.ajronline.org.
1234 AJR:210, June 2018
You might also like
- Amundson Active EngagementDocument13 pagesAmundson Active EngagementAna Nirvana100% (1)
- Ineffective Health MaintenanceDocument2 pagesIneffective Health MaintenanceBlessie Fernandez100% (1)
- Ajr 09 3543Document5 pagesAjr 09 3543Jakaria Khan SakibNo ratings yet
- The Unofficial Guide To RadiologyDocument59 pagesThe Unofficial Guide To RadiologywanwaqiuddinNo ratings yet
- Lung Nodule Detection by Microdose CT Versus Chest RadiographyDocument9 pagesLung Nodule Detection by Microdose CT Versus Chest RadiographyTatiana RecinosNo ratings yet
- Comparison of Long-Term Results of Percutaneous Treatment Techniques For Hepatic Cystic Echinococcosis Types 2 and 3bDocument7 pagesComparison of Long-Term Results of Percutaneous Treatment Techniques For Hepatic Cystic Echinococcosis Types 2 and 3bSandu AlexandraNo ratings yet
- Nagar Et Al 2012 Reperfusion Phenomenon Masking Acute and Subacute Infarcts at Dynamic Perfusion CT Confirmation byDocument10 pagesNagar Et Al 2012 Reperfusion Phenomenon Masking Acute and Subacute Infarcts at Dynamic Perfusion CT Confirmation byAnonymous Bu43ZUNo ratings yet
- Clear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalDocument8 pagesClear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalBastian VizcarraNo ratings yet
- Ajr 19 21383Document10 pagesAjr 19 21383chachaNo ratings yet
- Ajr 09 4032Document7 pagesAjr 09 4032Roshi_11No ratings yet
- Jurnal CT ScanDocument12 pagesJurnal CT ScanJefri Rudolf WomsiworNo ratings yet
- Effect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current ModulationDocument6 pagesEffect of Patient Size On Radiation Dose of Abdominal MDCT With Automatic Tube Current Modulationdestian ryanNo ratings yet
- Methods of Colostomy Construction No Effect On.6Document8 pagesMethods of Colostomy Construction No Effect On.6Charles CardosoNo ratings yet
- Johnson2010 Article FourDimensionalAnalysisOfAortiDocument2 pagesJohnson2010 Article FourDimensionalAnalysisOfAortiST. Fatimah KadirNo ratings yet
- Tissue Plasminogen Activator and Thrombin.17Document2 pagesTissue Plasminogen Activator and Thrombin.17ellie<3No ratings yet
- Prevalence of Solid Tumors in Incidentally Detected Homogeneous Renal Masses Measuring 20 HU On Portal Venous Phase CTDocument5 pagesPrevalence of Solid Tumors in Incidentally Detected Homogeneous Renal Masses Measuring 20 HU On Portal Venous Phase CTGordana PuzovicNo ratings yet
- Scanning Beyond Anatomic Limits of The Thorax in Chest CT - Findings, Radiation Dose, and Automatic Tube Current ModulationDocument6 pagesScanning Beyond Anatomic Limits of The Thorax in Chest CT - Findings, Radiation Dose, and Automatic Tube Current Modulationdestian ryanNo ratings yet
- Computed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaDocument6 pagesComputed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaGordana PuzovicNo ratings yet
- VitalSigns LectureNotes v2Document47 pagesVitalSigns LectureNotes v2diegoNo ratings yet
- Effects of Peer-Led Interventions For Patients With Cancer: A Meta-AnalysisDocument23 pagesEffects of Peer-Led Interventions For Patients With Cancer: A Meta-AnalysisMuthya GhitaNo ratings yet
- Pediatric Kidney MeasurementDocument7 pagesPediatric Kidney MeasurementKevin SurjadiNo ratings yet
- Jaffe Et Al 2012 Radiation Dose For Routine Clinical Adult Brain CT Variability On Different Scanners at One InstitutionDocument6 pagesJaffe Et Al 2012 Radiation Dose For Routine Clinical Adult Brain CT Variability On Different Scanners at One InstitutionHamza ArjahNo ratings yet
- UntitledDocument10 pagesUntitledJanne NgoNo ratings yet
- Ajr 10 5540Document9 pagesAjr 10 5540Pepe pepe pepeNo ratings yet
- Solid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaDocument11 pagesSolid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaTạ Minh ZSNo ratings yet
- CTA ExtremityDocument8 pagesCTA Extremityrio trisonaNo ratings yet
- Comparison of Gadolinium-Enhanced Fat-Saturated T1 - Weighted FLAIR and Fast Spin - Echo MRI of The Spine at 3 T For Evaluation of Extradural LesionsDocument7 pagesComparison of Gadolinium-Enhanced Fat-Saturated T1 - Weighted FLAIR and Fast Spin - Echo MRI of The Spine at 3 T For Evaluation of Extradural Lesionsanon_302681452No ratings yet
- AJR Chest Radiography in The ICU Parte I 2012Document9 pagesAJR Chest Radiography in The ICU Parte I 2012wfranelicNo ratings yet
- Chest Radiography in The ICUDocument9 pagesChest Radiography in The ICUNicolás HonoresNo ratings yet
- Ajr 11 7450Document7 pagesAjr 11 7450Ahmad Ibrahim SalemNo ratings yet
- Classification Revised For Lung Adenocarcinoma: Fighting Tuberculosis in SiberiaDocument24 pagesClassification Revised For Lung Adenocarcinoma: Fighting Tuberculosis in SiberiaYantoNo ratings yet
- Ajr 14 12810Document5 pagesAjr 14 12810Eka JuliantaraNo ratings yet
- Lung 2021 DohDocument39 pagesLung 2021 Dohbonn maNo ratings yet
- A Correlative Study of Solitary Thyroid Nodules.18Document6 pagesA Correlative Study of Solitary Thyroid Nodules.18Nan NaanNo ratings yet
- Handler 1979Document3 pagesHandler 1979KarimNo ratings yet
- Lee Et Al 2012 The Utility of Sonography For The Triage of Blunt Abdominal Trauma Patients To Exploratory LaparotomyDocument7 pagesLee Et Al 2012 The Utility of Sonography For The Triage of Blunt Abdominal Trauma Patients To Exploratory LaparotomyThesisaurus IDNo ratings yet
- Herbert JJDocument4 pagesHerbert JJYong Hye JungNo ratings yet
- 227 Full PDFDocument3 pages227 Full PDFanon_629352389No ratings yet
- Oral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTDocument4 pagesOral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTnataliayobeantoNo ratings yet
- Procedures Pro 2 Sept06-1934-Article PDFDocument4 pagesProcedures Pro 2 Sept06-1934-Article PDFMarNo ratings yet
- Cushing's SyndromeDocument1 pageCushing's SyndromeAmber BlodduweddNo ratings yet
- Cancellation of Elective Surgical Cases in A.12Document5 pagesCancellation of Elective Surgical Cases in A.12KhalilSemlaliNo ratings yet
- MR Angiography at 3 T of Peripheral Arterial Disease: A Randomized Prospective Comparison of Gadoterate Meglumine and GadobutrolDocument11 pagesMR Angiography at 3 T of Peripheral Arterial Disease: A Randomized Prospective Comparison of Gadoterate Meglumine and GadobutrolKevin AdrianNo ratings yet
- MRI of Small Hepatocellular Carcinoma: Typical Features Are Less Frequent Below A Size Cutoff of 1.5 CMDocument8 pagesMRI of Small Hepatocellular Carcinoma: Typical Features Are Less Frequent Below A Size Cutoff of 1.5 CMTaffy GultomNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Anam - 2016 - J. - Phys. - Conf. - Ser. - 694 - 012030Document7 pagesAnam - 2016 - J. - Phys. - Conf. - Ser. - 694 - 012030Hamza ArjahNo ratings yet
- Gray-Matter Volume Estimate Score - A Novel Semi-Automatic Method Measuring Early Ischemic Change On CTDocument7 pagesGray-Matter Volume Estimate Score - A Novel Semi-Automatic Method Measuring Early Ischemic Change On CTkartini ciatawiNo ratings yet
- Rcog2018 1e20645 NORMALDocument1 pageRcog2018 1e20645 NORMALberlianromaNo ratings yet
- Validation of The Oscillometric Blood Pressure MonDocument6 pagesValidation of The Oscillometric Blood Pressure MonPkarlNo ratings yet
- PROPELLER Technique To Improve Image Quality of MRI of The ShoulderDocument8 pagesPROPELLER Technique To Improve Image Quality of MRI of The ShoulderDhoni AvantasiaNo ratings yet
- The Ideal Male Nipple-Areola ComplexDocument7 pagesThe Ideal Male Nipple-Areola ComplexAngga Putra Kusuma KusumaNo ratings yet
- Necrotizing EnterocolitingDocument8 pagesNecrotizing Enterocolitingtrie dolleNo ratings yet
- Eye Lens Dose During CT ExamDocument7 pagesEye Lens Dose During CT ExamSamu SimamesaNo ratings yet
- Sainani 2009Document10 pagesSainani 2009Patricia BezneaNo ratings yet
- J Jacc 2021 06 019Document24 pagesJ Jacc 2021 06 019Jesús MorenoNo ratings yet
- Montagne Et Al 2012 Computed Tomography of The Normal Adrenal GlandsDocument4 pagesMontagne Et Al 2012 Computed Tomography of The Normal Adrenal GlandsAndreea CreangaNo ratings yet
- Swensen Et Al 2013 High Resolution CT of The Lungs Findings in Various Pulmonary DiseasesDocument9 pagesSwensen Et Al 2013 High Resolution CT of The Lungs Findings in Various Pulmonary Diseasesjeetchoudhary7890No ratings yet
- Cytopathology Regulations - Dr. Fadi Abdul-KarimDocument15 pagesCytopathology Regulations - Dr. Fadi Abdul-Karimyousrazeidan1979No ratings yet
- Exopthal 7Document7 pagesExopthal 7Perdana SihiteNo ratings yet
- CA Adrenal 2018Document16 pagesCA Adrenal 2018Daniela JimenezNo ratings yet
- HNP3Document9 pagesHNP3dev darma karinggaNo ratings yet
- Atlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrom EverandAtlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrieder BerrNo ratings yet
- Daniele Bernardi-Ruggero Bertelli - Bitcoin Price Forecast Using Quantitative Models - 2021 MarDocument20 pagesDaniele Bernardi-Ruggero Bertelli - Bitcoin Price Forecast Using Quantitative Models - 2021 MarBruno MeloNo ratings yet
- Battle of The Bots Flash Loans Miner Extractable Value and Efficient Settlement Christine Reseach PaperDocument22 pagesBattle of The Bots Flash Loans Miner Extractable Value and Efficient Settlement Christine Reseach PaperBruno MeloNo ratings yet
- Mudrex Crypto Market Outlook 4th April 2023Document5 pagesMudrex Crypto Market Outlook 4th April 2023Bruno MeloNo ratings yet
- Crypto Market Outlook Report - April 25, 2023Document8 pagesCrypto Market Outlook Report - April 25, 2023Bruno MeloNo ratings yet
- FP Koornneef - MSC Thesis - P5Document105 pagesFP Koornneef - MSC Thesis - P5Bruno MeloNo ratings yet
- FP Koornneef - Presentation - P5Document85 pagesFP Koornneef - Presentation - P5Bruno MeloNo ratings yet
- Strip o Ce Façade: Converted Building Vacant o Ce Building Unit Design Construction in StepsDocument3 pagesStrip o Ce Façade: Converted Building Vacant o Ce Building Unit Design Construction in StepsBruno MeloNo ratings yet
- Reconfigurable Interlocking FurnitureDocument14 pagesReconfigurable Interlocking FurnitureBruno MeloNo ratings yet
- Oliver-Maskell2007 Article PreroutedFPGACoresForRapidSystDocument7 pagesOliver-Maskell2007 Article PreroutedFPGACoresForRapidSystBruno MeloNo ratings yet
- Thermodynamic - Tables and GraphicsDocument46 pagesThermodynamic - Tables and GraphicsBruno MeloNo ratings yet
- 2022 LIFE and The Circular EconomyDocument104 pages2022 LIFE and The Circular EconomyBruno MeloNo ratings yet
- FreeBitcoin Script Roll 10000 100 Real HagshDocument4 pagesFreeBitcoin Script Roll 10000 100 Real HagshBruno MeloNo ratings yet
- Impact of Stress Management On Learning in A Classroom Setting PDFDocument58 pagesImpact of Stress Management On Learning in A Classroom Setting PDFnoronisa talusobNo ratings yet
- FSSC - FSSC 22000 V6 - 2023Document43 pagesFSSC - FSSC 22000 V6 - 2023posteraq374100% (1)
- Assessment Tool For Day Care Center and Day Care WorkerDocument34 pagesAssessment Tool For Day Care Center and Day Care WorkerMarrah Alora IliganNo ratings yet
- Low Vision PrinciplesDocument272 pagesLow Vision Principlesmariam mhNo ratings yet
- Duration of Dual Antiplatelet Therapy: Current ControversiesDocument8 pagesDuration of Dual Antiplatelet Therapy: Current ControversiesRajendra ChavanNo ratings yet
- KP Medical AstrologyDocument68 pagesKP Medical Astrologyaarivalagan100% (2)
- EFA DubaiDocument70 pagesEFA DubaiLifelinesafety ConsultantsNo ratings yet
- Medical Scenarios Updated 2023Document87 pagesMedical Scenarios Updated 2023tato sernaNo ratings yet
- A6013 v1 SD Influenza Ag BrochureDocument2 pagesA6013 v1 SD Influenza Ag BrochureYunescka MorenoNo ratings yet
- What Is ABA TherapyDocument8 pagesWhat Is ABA TherapyrushnaNo ratings yet
- Risk For Falls NCPDocument1 pageRisk For Falls NCPandayaannedhesireeNo ratings yet
- Week 7 Guide Questions AnswersDocument7 pagesWeek 7 Guide Questions AnswersKathleenMarieAlforteNo ratings yet
- DECON SPORE 200 Plus Disinfectant VEL 029 SDS North America English NAE 1Document7 pagesDECON SPORE 200 Plus Disinfectant VEL 029 SDS North America English NAE 1alex portilloNo ratings yet
- OBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Document7 pagesOBSTETRIC NURSING Hand Out UPANG INHOUSE 2022Mary Ann G. CorsanesNo ratings yet
- Psychosocial Narrative ReportDocument2 pagesPsychosocial Narrative ReportChonnie TiaNo ratings yet
- The Dynamics of Disease TransmissionDocument18 pagesThe Dynamics of Disease TransmissionJ MNo ratings yet
- Laudit, Arnel Z.Document30 pagesLaudit, Arnel Z.Japs De la CruzNo ratings yet
- Teaching and Learning Approaches in Early Childhood Programme CSZD 2143Document10 pagesTeaching and Learning Approaches in Early Childhood Programme CSZD 2143Tamira VanteciaNo ratings yet
- 8.medication Treatment SheetDocument1 page8.medication Treatment SheetDienizs LabiniNo ratings yet
- Worksheet Activity No. 5: Petri Dishes Colonies Size Color Shape A B C D E F GDocument2 pagesWorksheet Activity No. 5: Petri Dishes Colonies Size Color Shape A B C D E F GAlejandro, Severly Jane B.No ratings yet
- SOP On Operation and Calibration of Water BathDocument5 pagesSOP On Operation and Calibration of Water Bathfawaz khalilNo ratings yet
- New FFDocument81 pagesNew FFTesfahun GetachewNo ratings yet
- Orthodontic Study Models and Its Uses: Prachodh C ADocument36 pagesOrthodontic Study Models and Its Uses: Prachodh C Avicky100% (1)
- Red EyeDocument6 pagesRed EyeafatNo ratings yet
- Care of Client With Respiratory System DisordersDocument17 pagesCare of Client With Respiratory System DisordersAYTONA, JAMAICA F.No ratings yet
- AISA CP Handbook 2016Document83 pagesAISA CP Handbook 2016Rhea EscleoNo ratings yet
- Nursing School & College GuidelinesDocument16 pagesNursing School & College GuidelinesKaren SyiemNo ratings yet
- Gingivitis 2020Document91 pagesGingivitis 2020زيد العراقيNo ratings yet