Professional Documents
Culture Documents
National Guidelines For Analysis of Cerebrospinal Uid For Bilirubin in Suspected Subarachnoid Haemorrhage
National Guidelines For Analysis of Cerebrospinal Uid For Bilirubin in Suspected Subarachnoid Haemorrhage
Uploaded by
MWOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
National Guidelines For Analysis of Cerebrospinal Uid For Bilirubin in Suspected Subarachnoid Haemorrhage
National Guidelines For Analysis of Cerebrospinal Uid For Bilirubin in Suspected Subarachnoid Haemorrhage
Uploaded by
MWCopyright:
Available Formats
Review Article
National guidelines for analysis of cerebrospinal uid for bilirubin in
suspected subarachnoid haemorrhage
UK National External Quality Assessment Scheme for Immunochemistry Working Group
Abstract
Correspondence It is crucially important to detect subarachnoid haemorrhage (SAH) in all patients in
Dr Robert Beetham whom it has occurred in order to select patients for angiography and preventative
Dept of Clinical Biochemistry
surgery. A computed tomography (CT) scan is positive in up to 98% of patients with
Frenchay Hospital
Bristol BS16 1LE, UK SAH presenting within 12 h but is positive in only 50% of patients presenting within 1
E-mail: week.
robert.beetham@north-bristol.swest.nhs.uk Cerebrospinal uid (CSF) bilirubin spectrophotometry can be used to determine the
need for angiography in those few CT-negative patients in whom clinical suspicion of
a SAH remains high; it may remain positive for up to 2 weeks after the event. The
lumbar puncture (LP) should only be performed 412 h after the onset of presenting
symptoms. Whenever possible, collect four sequential CSF specimens. Always
ensure that the last CSF sample taken is sent for bilirubin analysis. Protect the CSF
from light and avoid vacuum tube transport systems if possible.
Always use spectrophotometry in preference to visual inspection. All CSF specimens
are precious and should be analysed no matter how they were transported, where
necessary with appropriate notice of the caveats regarding oxyhaemoglobin.
Centrifuge the specimen at 42000 rpm for 5 min as soon as possible after receipt in
the laboratory and in any case within 1 h of collection. Store the supernatant at 48C in
the dark until analysis.
An increase in CSF bilirubin is the key nding which supports the occurrence of SAH,
but it is not speci c for this. In most positive cases bilirubin will occur with
oxyhaemoglobin. Oxyhaemoglobin occurring on its own is dif cult to interpret and
may be increased as a result of in vitro haemolysis of red cells introduced into the
CSF during lumbar puncture. This process is exacerbated by vacuum tube transport
systems. Results should be interpreted in the light of other investigations (e.g. if scan
shows bilirubin then measure serum bilirubin and CSF oxyhaemoglobin and protein)
and other confounding variables such as the time elapsed from presentation to LP.
Ann Clin Biochem 2003; 40: 481–488
Introduction The initial investigation, the demonstration of blood
on a computed tomography (CT) scan, will, in experi-
enced hands, be positive in 98% of patients with SAH
Subarachnoid haemorrhage (SAH) is spontaneous presenting within the ¢rst 12 h after an event,4 but
arterial bleeding into the subarachnoid space, usually positivity falls with time to about 50% in patients
from a cerebral aneurysm.1 Patients who have bled, presenting after 1 week.5 Patients with a positive CT
and in whom the diagnosis is initially missed, often usually proceed to catheter angiography to con¢rm
present with a further bleed, in a poorer condition and the presence of an aneurysm and locate its site so that
with a worse outcome than those in whom the correct it can be treated to prevent a re-bleed. Catheter angio-
diagnosis is made promptly.2,3 It is thus crucially graphy, a resource-intensive and invasive procedure,
important to detect SAH in all patients in whom it has carries a small but de¢nite risk of morbidity and
occurred. mortality.6 There is thus a need for a procedure to
© 2003 The Association of Clinical Biochemists 481
482 Beetham et al.
detect those CT-negative patients presenting with CSF sample with an increased erythrocyte count as
a history suggestive of SAH who actually have there is no other reliable way for distinguishing
sustained a SAH 4 and to eliminate the diagnosis in between SAH and a traumatic lumbar puncture. It is
the remainder without the need for catheter angio- also of value in the investigation of CSF with a normal
graphy. Best estimates are that a UK hospital may see red cell count from a patient presenting several days
up to 150 patients per annum with symptoms of SAH after an event, by which time the cells may no longer
who are CT-negative; some 2-3% of these will be be present.
proven to have a ruptured aneurysm.4 We now propose guidelines for the specimen
Following haemorrhage into the CSF, red blood cells requirements, transport, handling, analysis of CSF
undergo lysis and phagocytosis; the liberated oxyhae- and interpretation in patients with a suspected SAH
moglobin is converted in vivo in a time-dependent but a negative CT scan. Notes to these guidelines,
manner into bilirubin 7 and sometimes methae- printed as Appendix 1, provide the reasoning behind
moglobin.8 Of these three pigments, only bilirubin our recommendations.
arises solely from in vivo conversion. Oxyhaemoglobin
and methaemoglobin may both be produced in vitro as
well as in vivo.9
Bilirubin may be detected in CSF by spectro-
Specimen requirements and transport
photometry or by visual inspection for the yellow dis- A protocol for specimen requirements and transport is
coloration (xanthochromia) it imparts to CSF. Evidence provided in Appendix 2, although modi¢cation may be
clearly indicates that visual inspection is not a required to meet local needs. Readers should also refer
reliable method.10,11 Spectrophotometry to detect to Appendix 1, Notes to the Guidelines. Essentially, the
bilirubin is of particular value in the investigation of a requirements are:
Ann Clin Biochem 2003; 40: 481–488
National guidelines for CSF analysis for bilirubin in suspected subarachnoid haemorrhage 483
. Whenever possible, collect four sequential specimens. the analysis to be undertaken without dilution, and
will be determined by local requirements.
. The specimen for spectrophotometry should always
be the last fraction of CSF to be taken, and ideally at . The specimen should be protected from light.
least the fourth.
. Use of pneumatic tube systems to transport the
. The volume requested must be that which enables specimen to the laboratory should be avoided.12
Figure 1(a) to (e). Representative spectro-
photometric scans showing net bilirubin absor-
bance (NBA) at 476 nm above a tangential
baseline, as described in the text. (a) Normal
cerebrospinal uid with essentially no bilirubin;
scan and baseline (not drawn) are super-
imposable. (b) NBA within the reference range.
(c) Oxyhaemoglobin with zero NBA. (d)
Oxyhaemoglobin with NBA within the reference
range. (e) Oxyhaemoglobin with an increased
NBA. (In practice, such scans are best
visualized lling the whole of an A4 page in
landscape mode.)
Ann Clin Biochem 2003; 40: 481–488
484 Beetham et al.
. A simultaneous blood specimen should be taken for Reporting and interpretation
serum bilirubin and total protein measurement.
The following is the most appropriate advice that we
. Record the timing of sampling relative to that of
can provide regarding reporting and suggested inter-
possible haemorrhage. This should be no less than
12 h. pretative comments. Readers should refer to Appendix
1, Notes to the Guidelines, for further details. For each
It is advised that prospective protocols are discussed case, the ¢nal interpretation should take into account
with users of the service. the known dynamic production of haem pigments
following a bleed, as outlined in the Introduction.
Specimen handling Thus, most positive cases exhibit both oxyhaemo-
globin and bilirubin. Oxyhaemoglobin occurring on
The specimen designated for spectrophotometry its own may, unusually, be found early on after a bleed
should be centrifuged at 42000 rpm for 5 min as soon (particularly if the absorbance of the oxyhaemoglobin
as possible after receipt in the laboratory and in any peak is su¤ciently great to obscure a small but signif-
case within 1h of collection. The supernatant should icant amount of bilirubin ^ see below). Bilirubin
be stored in the dark at 48C until analysis. occurring on its own would not be expected within the
¢rst few days, but becomes an increasingly possible
¢nding as the second week progresses.
Analysis
. Perform a zero-order spectrophotometric scan on NBA 40.007 AU and no oxyhaemoglobin present
the supernatant between 350 and 600 nm using a Report as: `No signi¢cant bilirubin and no oxyhaemo-
recording spectrophotometer and a cuvette with a globin present. No evidence to support subarachnoid
1-cm path length. Use an initial full-scale de£ection haemorrhage.’
(FSD) of 0.1 absorbance units (AU). If any peaks
exceed 0.1 AU, scale as appropriate but never use a NBA 40.007 AU and oxyhaemoglobin present but NOA
FSD less than 0.1 AU. 50.1 AU
. The specimen should not be diluted. Report as: `Oxyhaemoglobin present but no signi¢cant
bilirubin. Oxyhaemoglobin on its own has a low
Inspect the scan and identify and record the presence
predictive value for subarachnoid haemorrhage but
of the following haem pigments:
does not exclude.’
. Oxyhaemoglobin: absorbance maximum between
410 and 418 nm. NBA 40.007 AU and NOA 50.1 AU
. Bilirubin: either a broad peak in the range 450 to Report as: `Oxyhaemoglobin present but no signi¢cant
460 nm or a shoulder adjacent to an oxyhae- bilirubin. NB The concentration of oxyhaemoglobin
moglobin peak if present. may mask a small but signi¢cant increase in bilirubin.
. Methaemoglobin: the rarest pigment, and if present Subarachnoid haemorrhage not excluded.’
usually manifest as a broader peak than oxyhae-
moglobin, occurring between 403 and 410 nm. NBA 40.007 AU and no oxyhaemoglobin present
(a) Serum bilirubin 420 mmol/L and CSF protein
Calculate the net bilirubin absorbance (NBA) 41.0 g/L.
according to Chalmers’ modi¢cation13 to the original Report as: `Increased CSF bilirubin but no oxyhae-
method of Chalmers and Kiley14 as follows: moglobin. Consistent with subarachnoid haemor-
. Draw a predicted baseline which forms a tangent to rhage.’ (NB This would be an unusual pattern within
the scan between 350 and 400 nm and again the ¢rst week after an event.)
between 430 and 530 nm. This baseline should (b) Serum bilirubin 420 mmol/ L and CSF protein
never cut the scan. 41.0 g/L.
. Measure the absorbance of the scan above this Apply formula to calculate an adjusted NBA (see
predicted baseline at 476 nm; this is the NBA. If the Appendix 3).
baseline forms a tangent to the scan before 476 nm, If adjusted NBA 50.007 AU, report as: `Increased
then the measured NBA is by de¢nition zero. CSF bilirubin but no oxyhaemoglobin. Consistent with
subarachnoid haemorrhage.’ (NB This would be an
. Also measure the absorbance of any oxyhae-
unusual pattern within the ¢rst week after an event).
moglobin peak above this predicted baseline; this is
If adjusted NBA 50.007 AU, report as: `Increased
the net oxyhaemoglobin absorbance (NOA).
CSF bilirubin but probably totally accounted for by
Illustrative zero-order spectra are shown in Figs 1(a) increase in serum bilirubin. No oxyhaemoglobin. Not
to (e). supportive of subarachnoid haemorrhage.’
Ann Clin Biochem 2003; 40: 481–488
National guidelines for CSF analysis for bilirubin in suspected subarachnoid haemorrhage 485
(c) CSF protein 41.0 g/L, whatever the serum If adjusted NBA 50.007 AU, report as: `Increased
bilirubin. CSF bilirubin but probably totally accounted for by an
Report as: `Increased CSF bilirubin, but no oxy- increased serum bilirubin. Oxyhaemoglobin present
haemoglobin. This ¢nding may be consistent with: which on its own has a low predictive value for sub-
subarachnoid haemorrhage; an increased bilirubin arachnoid haemorrhage, although does not totally
accompanying the increased CSF protein; or other exclude.’
source of CSF blood. Interpret result with caution in (c) CSF protein 41.0 g/L, whatever the serum bili-
relation to subarachnoid haemorrhage, especially if rubin.
within ¢rst week of event.’ Report as: `Increased CSF bilirubin with oxyhae-
moglobin present. This ¢nding may be consistent
with: subarachnoid haemorrhage; an increased bili-
NBA 40.007 AU and oxyhaemoglobin present but NOA rubin accompanying the increased CSF protein; or
other source of CSF blood.’
40.1 AU
(a) Serum bilirubin 420 mmol/L and CSF protein
41.0 g/L. NBA 40.007 AU and NOA 40.1 AU
Report as: `Increased CSF bilirubin with oxyhae - (a) CSF protein 41.0 g/L, whatever the serum
moglobin present. Consistent with subarachnoid bilirubin.
haemorrhage.’ Report as: `Increased CSF bilirubin with oxyhae-
(b) Serum bilirubin 420 mmol/L and CSF protein moglobin present. Consistent with subarachnoid
41.0 g/L. haemorrhage.’
Apply formula (Appendix 3) to calculate adjusted (b) CSF protein 41.0 g/L, whatever the serum bili-
NBA. rubin.
If adjusted NBA 50.007 AU, report as: `Increased Report as: `Increased CSF bilirubin with oxyhae-
CSF bilirubin with oxyhaemoglobin present. Con- moglobin present. This ¢nding may be consistent
sistent with subarachnoid haemorrhage.’ with: subarachnoid haemorrhage; an increased
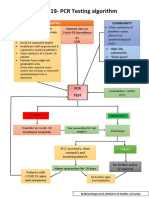
Figure 2. Bilirubin absorbance in cerebrospinal uid (CSF) for detection of subarachnoid bleeding. CT ˆcomputed tomography;
‡ve ˆ positive; 7ve ˆ negative; NOA ˆ net oxyhaemoglobin absorbance; NBA ˆ net bilirubin absorbance. (NB. The disposition of
specimens for microbiological examination and total protein will be subject to local arrangement.)
Ann Clin Biochem 2003; 40: 481–488
486 Beetham et al.
bilirubin accompanying the increased CSF protein; or Acknowledgements
other source of CSF blood.’ The UK NEQAS for Immunochemistry working group
consisted of: R Beetham, MN Fahie-Wilson,
Methaemoglobin detected I Holbrook, ID Watson, PR Wenham, PAE White,
This is an unusual ¢nding and probably related to P Thomas, AM Ward, A Cruickshank, G Keir,
artefactual conversion of oxyhaemoglobin. Therefore, W Egner and K Allen.
when methaemoglobin is present the signi¢cance of The working group acknowledge with thanks the
the ¢nding is the same as if oxyhaemoglobin had been assistance of D O’Connell, H Gunawardena and
detected. Report as under 2, 3, 5 and 6, substituting PLM Lynch in the provision of data used by the group
methaemoglobin for oxyhaemoglobin. and thank D O’Connell for assistance with Fig. 1. It also
NB When reporting on spectrophotometry, bear in acknowledges the formulation of guidelines by other
mind that: (a) a normal erythrocyte count in a CSF groups, particularly the All Wales Audit Group and the
taken de¢nitely between 12 and 72 h after an event is Northern Ireland Audit Group.
evidence against a SAH; and (b) spectrophotometric
¢ndings on a CSF taken at a second or subsequent
lumbar puncture some hours or more after the Appendix 1. Notes to the guidelines
previous puncture only re£ect the probability that (a) In addition to the oxyhaemoglobin which appears
blood has been introduced traumatically into the after a SAH, it also commonly arises either from the in
subarachnoid space at an earlier puncture. vitro lysis of red cells in the CSF obtained following
puncture, or from the trauma of the puncture itself. As
Decision tree explained in note (g) below, such oxyhaemoglobin
may interfere with the detection of bilirubin and is a
A decision tree (see Fig. 2) outlines the steps involved in confounding element in interpretation. Therefore,
producing the key laboratory information for the every e¡ort should be made to eliminate it. It is for
detection of a subarachnoid bleed. (A colour version of this reason that CSF taken for spectrophotometry
Fig. 2 is available from the corresponding author.) should be collected into a separate container to those
in which the ¢rst few mL of £uid are placed, and
Standards based on these guidelines also why transport by pneumatic tube is not
recommended.
. The laboratory should provide instructions for (b) As explained in note (j), even small increases
users which provide details of requesting, specimen above the reference range are su¤cient to be consis-
requirements, transport and interpretation (see tent with a SAH and therefore indicate the need for
example in Appendix 2). angiography. Dilution of the specimen will decrease
. There should be in place Standard Operating the certainty with which such increases may be
Procedures (SOPs) for specimen handling, analysis, detected.
reporting and interpretation. (c) Stability studies have shown that CSF stored in a
. The laboratory must participate in an appropriate plastic tube and exposed to spring daylight through a
external quality assurance scheme. north-facing window showed a bilirubin decay rate of
. It is unlikely that a laboratory will build up su¤- at least 0.005 AU/h. CSF specimens must therefore be
cient expertise unless a minimum of 25 specimens protected from light to avoid this phenomenon, which
are analysed annually. may lead to false negative results.
. The nature of the analytical service which a (d) Current consensus is that CSF should not be
laboratory provides, e.g. whether it is available only examined for bilirubin earlier than 12 h after an event.
within certain hours or at all times, will be depen- This is based on two strands of evidence:
dent upon local needs. In particular, these will be
determined by the tertiary centre’s referral policy, (i) That bilirubin forms 9-15 h after a bleed.7 We
access to its beds and availability of angiography. have been unable to review the evidence on which
Both the analytical and interpretative aspects of the this statement has been made.
service should be provided together. (ii) That in a series of 111 patients positive for blood
on CT, all subject to lumbar puncture after 12 h,
. To meet the requirements of clinical governance, all
xanthochromia was present in all.19 This evi-
spectrophotometric scans should be kept in an
dence must be reviewed with caution due to the
appropriate form for recall for a minimum of 2
ambiguous de¢nition of xanthochromia.
years.
. Spectrophotometers should be serviced regularly It is also commonly believed that xanthochromia
and undergo regular absorption and wavelength will be evident in all patients up to 2 weeks following a
checks. bleed. Again, this is based on an inappropriate
Ann Clin Biochem 2003; 40: 481–488
National guidelines for CSF analysis for bilirubin in suspected subarachnoid haemorrhage 487
group ^ those who were positive for blood on CT.19 four patients, one of whom was angiography-positive)
In patients who are negative for blood on CT who that no clear indication of its signi¢cance could be
may be negative due to late presentation or small obtained. Very recent work, which needs to be
bleeds, we cannot be certain about this period of 2 con¢rmed, has implicated high levels of iodine (widely
weeks. In our experience, we have detected an used as a skin disinfectant) as being involved in in vitro
increased CSF bilirubin in two patients subsequently methaemoglobin formation.
shown to have ruptured aneurysms, in whom the
CSF was taken at 11 and 14 days after the onset of Appendix 2. Exemplar protocol for the
symptoms.
(e) Derivative spectroscopy has been found to be of collection, handling and transport to the
value by some analysts, but requires considerable laboratory of cerebrospinal uid requiring
experience in interpretation. It is therefore not spectrophotometric scanning for the
recommended.
(f) We have con¢rmed that, on 58 CSF specimens detection of bilirubin
with bilirubin NBA 0.003- 0.251 AU (24 of which Principle
contained oxyhaemoglobin in addition to bilirubin), This test is performed to try to identify those patients
there was no signi¢cant di¡erence between the NBA who have had a SAH but in whom the CT scan is
obtained by the original Chalmers and Kiley method14 negative. The spectrophotometric scan detects bili-
and that by the modi¢cation of Chalmers.13 rubin in CSF, and this ¢nding is consistent with a bleed
(g) Out of 740 spectrophotometric scans reviewed into the CSF.
from CT-negative patients in four participating The formation of bilirubin after haemorrhage is a
centres, 425 had no oxyhaemoglobin and NBA time -dependent process and bilirubin may not be
40.007 AU. Angiograms were performed in 31 of detectable soon after the event (e.g. onset of severe
these 425 patients and no aneurysms were found. headache). On current evidence, it is recommended
(h) From the same series, 204 CSF samples were that CSF is not sampled until at least 12 h after a
reported as containing oxyhaemoglobin with NBA suspected event. The opening pressure should always
40.007 AU. Twenty-nine of these patients had angio- be recorded when performing a lumbar puncture.
graphy, and in only two instances was an aneurysm Lumbar puncture is contra-indicated in patients with
found. Oxyhaemoglobin thus has a low predictive papilloedema, focal neurological de¢cit or reduced
value for SAH. However, we recognize that rarely, consciousness.
early on after a bleed, oxyhaemoglobin may be present Please indicate on the request form:
without bilirubin.
(i) Experiments using a combination of increasing . Clinical indication for request
bilirubin and oxyhaemoglobin concentrations have . Result of CT scan
indicated that oxyhaemoglobin causes an under- . Time of onset of symptoms/event
estimation of NBA by approximately 0.001 AU for . Time of lumbar puncture
every 0.030 AU of NOA. To prevent undue complexity, . If the di¡erential diagnosis includes meningitis
we incorporate this into interpretation for NOA
40.1 AU. Specimens
(j) Originally, Chalmers and Kiley14 indicated a . Cerebrospinal £uid may also be required for micro-
reference range for NBA of 0 to 0.007 AU; values of biological examination and for protein and glucose
0.010 to 0.015 AU were classed as equivocal and estimation. Su¤cient CSF will therefore be needed
values 40.015 AU as positive. In the series quoted for all of these required investigations.
above, CSFs from three patients with proven ruptured . Label three 28-mL sterile universal containers and
aneurysms yielded NBAs of 0.008, 0.015 and one yellow-top £uoride EDTA tube with the patient’s
0.016 AU. In addition, we are aware of three CT- name, hospital number, ward, date of birth, the
positive patients with proven aneurysms whose CSFs time that the CSF was obtained and the sequence
yielded NBAs of 0.008, 0.012 and 0.019 AU.We there- order of sampling.
fore recommend that NBA values 40.007 AU are a . The ¢rst specimen should be a minimum of 0.5 mL of
clear indication for angiography. In the series quoted CSF placed in a yellow-top £uoride EDTA tube for
above, 27 patients with NBA 40.007 AU proceeded to glucose and protein estimations. This specimen
angiography, of which 12 were found to have should be sent to the clinical biochemistry depart-
aneurysms. ment.
(k) While there is documented evidence for the . Microbiology requires at least 5 mL of CSF divided
production of methaemoglobin following SAH, it was into two sequentially numbered, sterile 28-mL
such an uncommon ¢nding in the series quoted (in universal containers labelled `second’ and `third’.
Ann Clin Biochem 2003; 40: 481–488
488 Beetham et al.
These two specimens must be delivered to the References
microbiology department as soon as possible. Use of
1 Vermeulen M, van Gijn J. The diagnosis of subarachnoid
the pneumatic tube delivery system should be avoided. haemorrhage. J Neurol Neurosurg Psychiatry 1990; 53: 365-72
. A further minimum of 1 mL of CSF should be placed 2 Mayer PL, Awad IA, Todor R. Misdiagnosis of symptomatic cerebral
in the ¢nal (labelled `fourth’) sterile 28-mL aneurysm; prevalence and correlation with outcome at four
universal container for the spectrophotometric institutions. Stroke 1996; 27: 1558-63
scan. (NB 1mL is about 20 drops from the Luer 3 Jacobsson KE, Saveland H, Hillman J, Edner G, Zygmunt S,
connector on a needle). Protect this sample from Pellettieri L. Warning leak and management outcome in aneurysmal
the light by placing it in a thick brown envelope subarachnoid haemorrhage. J Neurosurg 1996: 85: 995-9
outside the usual plastic specimen bag. 4 van der Wee N, Rinkel GE, Hasan D, van Gijn J. Detection of
. A blood specimen should be taken at the same time subarachnoid haemorrhage on early CT: is lumbar puncture still
needed after a negative scan? J Neurol Neurosurg Psychiatry
for serum bilirubin, total protein and glucose esti-
1995; 58: 357-9
mation, which are needed to aid interpretation.
5 van Gijn J, van Dongen KJ. The time course of aneurysmal
NB. These samples must also be delivered to the clinical haemorrhage on computed tomograms. Neuroradiology 1982; 23:
biochemistry department as soon as possible. Use of the 153-6
pneumatic tube delivery system should be avoided. 6 Dion JE, Gates PC, Fox AJ, Barnett HJM, Blom RJ. Clinical events
If this procedure is not followed, analysis is likely to following neuroangiography: a prospective study. Stroke 1987; 18:
be compromised. 997-1004
Text in italics indicates those details subject to local 7 Fishman RA. Cerebral Fluid in Diseases of the Nervous System.
requirements. London: WB Saunders, 1980
8 Wahlgren NG, Lindquist C. Haem derivatives in the cerebrospinal
uid after intracranial haemorrhage. Eur Neurol 1987; 26: 216-21
Appendix 3. Adjustment of net bilirubin 9 Fahie-Wilson M, Park D. Spectrophotometric examination of CSF in
absorbance for an increase in serum suspected subarachnoid haemorrhage – what should we look for?
In: Martin SM, Halloran SP, eds. Proceedings of the XVI
bilirubin International Congress of Clinical Chemistry, 1996 Jul 8-12,
The predicted absorbance (PA) of a CSF at 476 nm due London. London: Association of Clinical Biochemists, 1996: 85
to bilirubin can be calculated according to the 10 Kjellin KG, Söderström CE. Diagnostic signi cance of CSF
following equation:15^17 spectrophotometry in cerebrovascular diseases. J Neurol Sci
1974; 23: 359-69
11 Marden NA, Thomas PH, Stansbie D. Is the naked eye as sensitive
CSF total protein …g=L† as the spectrophotometer for detecting xanthochromia in
PA ˆ
Serum total protein …g=L† cerebrospinal uid? In: Martin SM, ed. Proceedings of the National
Meeting, 2001 April 30-May 4, London. London: Association of
£ serum bilirubin (mmol=L) £ 0.042 AU
Clinical Biochemists, 2001: 53
…1† 12 Wenham PR, Hanson T, Ashby JP. Interference in spectro-
photometric analysis of cerebrospinal uid by haemolysis induced
Then adjusted NBA ˆ measured NBA ¡ PA by transport through a pneumatic tube system. Ann Clin Biochem
2001; 38: 371-5
…2† 13 Chalmers AH. Cerebrospinal uid xanthochromia testing simpli ed.
Clin Chem 2001; 47: 147-8
We recommend use of this formula because it has 14 Chalmers AH, Kiley M. Detection of xanthochromia in cerebrospinal
been validated for use: uid. Clin Chem 1998; 44: 1740-2
15 Kjellin KG. The binding of xanthochromic compounds in the
(a) in neonatal jaundice,18 albeit often at higher bili- cerebrospinal uid. J Neurol Sci 1969; 9: 597-601
rubin concentrations than are encountered in 16 Kronholm V, Lintrup J. Spectrophotometric investigations of the
adults, and cerebrospinal uid in the near-ultraviolet region. Acta Psychiatr
(b) in a group of 12 patients with increased serum Scand 1960; 35: 314-29
bilirubin and CSF protein up to 1.0 g/L, in whom 17 Wahlgren NG, Bergstrom K. Determination of haem derivatives in
predicted7actual NBA produced a mean value of the cerebrospinal uid – a semi-quantitative method. J Neurol
70.002 AU. Neurosurg Psychiatry 1983; 46: 653-8
18 Hellström B, Kjellin KG. The diagnostic value of spectrophotometry
We do not recommend adjustment of NBAwhere the of the cerebrospinal uid in the newborn period. Develop Med Child
CSF bilirubin is increased due to an increased CSF Neurol 1971; 6: 789-97
protein concentration alone, or where there is an 19 Vermeulen M, Hasan D, Blijenberg BG, Hijdra A, van Gijn J.
increased serum bilirubin concentration and the CSF Xanthochromia after subarachnoid haemorrhage needs no
protein is greater than 1.0 g/L, because of lack of revisitation. J Neurol Neurosurg Psychiat 1989; 52: 826-8
validation. Accepted for publication 27 March 2003
Ann Clin Biochem 2003; 40: 481–488
You might also like
- NN10600-000 72s2Document24 pagesNN10600-000 72s2tommiyauNo ratings yet
- Handle Large Messages in Apache KafkaDocument59 pagesHandle Large Messages in Apache KafkaBùi Văn KiênNo ratings yet
- Cruickshank Et Al 2008 Revised National Guidelines For Analysis of Cerebrospinal Fluid For Bilirubin in SuspectedDocument25 pagesCruickshank Et Al 2008 Revised National Guidelines For Analysis of Cerebrospinal Fluid For Bilirubin in Suspectedshaun tanNo ratings yet
- CSF XanthochromiaDocument3 pagesCSF XanthochromiaShaikh Ghassan AbidNo ratings yet
- Standards For Analysis of Cerebrospinal Fluid CSF For XanthochromiaDocument2 pagesStandards For Analysis of Cerebrospinal Fluid CSF For XanthochromiaanggaririnNo ratings yet
- Xanthochromia in The Cerebrospinal FL Uid: Image of The MomentDocument3 pagesXanthochromia in The Cerebrospinal FL Uid: Image of The MomentNutthawut JuldenNo ratings yet
- Ainsley H. Chalmers and Michelle Kiley (Departments of HaemaDocument3 pagesAinsley H. Chalmers and Michelle Kiley (Departments of HaemaswasahmedNo ratings yet
- 10.1515 - CCLM 2021 1320Document5 pages10.1515 - CCLM 2021 1320geo4maryNo ratings yet
- Utility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020Document6 pagesUtility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020tufis02No ratings yet
- Int J Lab Hematology - 2022 - Marinov - Validation of A Single Tube 3 Colour Immature Red Blood Cell Screening Assay ForDocument7 pagesInt J Lab Hematology - 2022 - Marinov - Validation of A Single Tube 3 Colour Immature Red Blood Cell Screening Assay ForMaria SousaNo ratings yet
- Ok 2Document7 pagesOk 2cydolusNo ratings yet
- 4-Hematology Analyzer - Detecting Erroneous Blood CountsDocument23 pages4-Hematology Analyzer - Detecting Erroneous Blood CountsRajeshNo ratings yet
- Performance Evaluation of The Body Fluid Mode On The Platform Sysmex XE-5000 Series Automated Hematology AnalyzerDocument9 pagesPerformance Evaluation of The Body Fluid Mode On The Platform Sysmex XE-5000 Series Automated Hematology AnalyzerbalkisNo ratings yet
- Briggs2006 PDFDocument10 pagesBriggs2006 PDFRonal WinterNo ratings yet
- Sysmex ScattergramsDocument7 pagesSysmex ScattergramsRuxandra Mesaros100% (1)
- Sop CBCDocument3 pagesSop CBCYousef AlshawafahNo ratings yet
- Pie 2018Document5 pagesPie 2018Tina HerreraNo ratings yet
- 2 The Use of The Laboratory: 1 Introducing Clinical BiochemistryDocument2 pages2 The Use of The Laboratory: 1 Introducing Clinical BiochemistryAmelia PebriantiNo ratings yet
- Indications Trephine BiopsyDocument6 pagesIndications Trephine Biopsyoki harisandiNo ratings yet
- El Examen de Sedimento de Orina Proporciona Más Información Diagnóstica en AKI Que Biomarcadores. 2022Document3 pagesEl Examen de Sedimento de Orina Proporciona Más Información Diagnóstica en AKI Que Biomarcadores. 2022Edwin Fabian Paz UrbanoNo ratings yet
- Erythrocyte and Plasma Volume MeasurementDocument6 pagesErythrocyte and Plasma Volume MeasurementMillenial AcousticsNo ratings yet
- CSF, UF 1000i, 2015Document11 pagesCSF, UF 1000i, 2015balkisNo ratings yet
- Evaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationDocument9 pagesEvaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationbalkisNo ratings yet
- Endourology and Stones Predictive Value of Leukocytosis For Infectious Complications After Percutaneous NephrolithotomyDocument5 pagesEndourology and Stones Predictive Value of Leukocytosis For Infectious Complications After Percutaneous NephrolithotomyJufrialdy AldyNo ratings yet
- Renal BiopsyDocument4 pagesRenal BiopsyDeshan AdikariNo ratings yet
- Efficacy of Ascitic Acid Dipstick Leukocyte Esterase Activity in Early Diagnosis of Spontaneous Bacterial PeritonitisDocument6 pagesEfficacy of Ascitic Acid Dipstick Leukocyte Esterase Activity in Early Diagnosis of Spontaneous Bacterial PeritonitisIJAR JOURNALNo ratings yet
- Pathophysiology of Ischaemic Stroke: Insights From Imaging, and Implications For Therapy and Drug DiscoveryDocument11 pagesPathophysiology of Ischaemic Stroke: Insights From Imaging, and Implications For Therapy and Drug DiscoveryryanafitrianaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument10 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- 10 1111@ijlh 12760Document6 pages10 1111@ijlh 12760Hedo HidayatNo ratings yet
- HaematologyDocument11 pagesHaematologyIkram AzmanNo ratings yet
- The Diagnostic Use of ADVIA 2120i Siemens and An "APL Criteria" CanDocument9 pagesThe Diagnostic Use of ADVIA 2120i Siemens and An "APL Criteria" CananggaririnNo ratings yet
- Histoneur Hepatology PDFDocument7 pagesHistoneur Hepatology PDFmarianNo ratings yet
- Cardiac Output Estimation Using Ballistocardiography: A Feasibility Study in Healthy SubjectsDocument9 pagesCardiac Output Estimation Using Ballistocardiography: A Feasibility Study in Healthy SubjectsshucksmaamNo ratings yet
- Comparison of Cerebellomedullary and Lumbar CSF in Dogs With Neurological Disease Jvim.15700Document6 pagesComparison of Cerebellomedullary and Lumbar CSF in Dogs With Neurological Disease Jvim.15700hematologiaNo ratings yet
- New QuantitiesDocument6 pagesNew Quantities20100117 Bùi Thùy VyNo ratings yet
- Diagnosis of Brucella: Prepared By: Bahaa Mostafa Kamel 415Document6 pagesDiagnosis of Brucella: Prepared By: Bahaa Mostafa Kamel 415Bahaa ShaabanNo ratings yet
- Feline Blood Film 230902 043358Document13 pagesFeline Blood Film 230902 04335897namithaNo ratings yet
- Science: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsDocument6 pagesScience: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsnivmastNo ratings yet
- 12 White Blood Cell Counting Techniques in BirdsDocument5 pages12 White Blood Cell Counting Techniques in BirdsPablo LópezNo ratings yet
- 01 STR 8 5 613Document5 pages01 STR 8 5 613Seblewengel AbateNo ratings yet
- Yield of Induced Sputum in Clinically Diagnosed Pulmonary TuberculosisDocument7 pagesYield of Induced Sputum in Clinically Diagnosed Pulmonary TuberculosisIJAR JOURNALNo ratings yet
- Clasificacion de Biopsias Ellis Et Al.Document6 pagesClasificacion de Biopsias Ellis Et Al.tatianaNo ratings yet
- Ann Clin Biochem-2009-Guy-468-76Document9 pagesAnn Clin Biochem-2009-Guy-468-76keyssiNo ratings yet
- Cerebrospinal FluidDocument16 pagesCerebrospinal FluidSolomon Fallah Foa SandyNo ratings yet
- Review Article Perfusion Imaging in Ischaemic StrokeDocument4 pagesReview Article Perfusion Imaging in Ischaemic Strokesepty_auliaNo ratings yet
- Optimal Blood Pressure During CPBDocument7 pagesOptimal Blood Pressure During CPBAdy WarsanaNo ratings yet
- Neonatal Neurosonography: A Pictorial Essay: EuroradiologyDocument13 pagesNeonatal Neurosonography: A Pictorial Essay: EuroradiologyAnom RahartoNo ratings yet
- Leaders Bone Marrow Aspiration: BjbainDocument7 pagesLeaders Bone Marrow Aspiration: BjbaintmrezatandiNo ratings yet
- Design and Analysis of HSC-BPPV Diagnostic ManeuveDocument11 pagesDesign and Analysis of HSC-BPPV Diagnostic ManeuveSelinay YAȘANo ratings yet
- Clinical Biochemistry: E. Schapkaitz, S. RaburabuDocument7 pagesClinical Biochemistry: E. Schapkaitz, S. RaburabuMunawwar SaukaniNo ratings yet
- EASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced ReaderDocument1 pageEASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced Readerchiara valentina luglioNo ratings yet
- Letter To The Editor: Comparison Between Automated and Microscopic Analysis in Body Fluids CytologyDocument3 pagesLetter To The Editor: Comparison Between Automated and Microscopic Analysis in Body Fluids CytologybalkisNo ratings yet
- Zhang 2000Document6 pagesZhang 2000hoangkiett0904No ratings yet
- JR2 RizaDocument3 pagesJR2 RizaCitra DewiNo ratings yet
- 10.1515 - Labmed 2023 0064Document9 pages10.1515 - Labmed 2023 0064Arturo Eduardo Huarcaya OntiverosNo ratings yet
- Basics of Kidney Biopsy: A Nephrologist's Perspective: Review ArticleDocument11 pagesBasics of Kidney Biopsy: A Nephrologist's Perspective: Review ArticleBilal MaloukaNo ratings yet
- BlacT Package InsertDocument2 pagesBlacT Package InsertaliborabasNo ratings yet
- XN 3000 VS BeckmanDocument8 pagesXN 3000 VS BeckmanZied FehriNo ratings yet
- Kjtcs 47 124Document5 pagesKjtcs 47 124dalozpa23No ratings yet
- HaematologiDocument10 pagesHaematologigroup3akademikNo ratings yet
- 10 0000@www Jrheum Org@32@5@828Document5 pages10 0000@www Jrheum Org@32@5@828Yasser AlghrafyNo ratings yet
- Clinical Neuroanatomical TechniquesDocument6 pagesClinical Neuroanatomical TechniquesMWNo ratings yet
- Cha 10Document2 pagesCha 10MWNo ratings yet
- CovidpcrtestingalgorithmDocument1 pageCovidpcrtestingalgorithmMWNo ratings yet
- Original Article: Macroenzyme Detection by Polyethylene Glycol PrecipitationDocument7 pagesOriginal Article: Macroenzyme Detection by Polyethylene Glycol PrecipitationMWNo ratings yet
- Color Atlas of BrainDocument8 pagesColor Atlas of BrainMWNo ratings yet
- Case Report: Excessive Calcium Ingestion Leading To Milk-Alkali SyndromeDocument3 pagesCase Report: Excessive Calcium Ingestion Leading To Milk-Alkali SyndromeMWNo ratings yet
- Validation Vs VerificationDocument46 pagesValidation Vs VerificationMW100% (2)
- Case ReportDocument3 pagesCase ReportMWNo ratings yet
- WHO Practical GuideDocument113 pagesWHO Practical GuideMWNo ratings yet
- Short ReportDocument4 pagesShort ReportMWNo ratings yet
- Reference Intervals - Direct Priori MethodDocument5 pagesReference Intervals - Direct Priori MethodMWNo ratings yet
- AACB 2013 Lab QCDocument9 pagesAACB 2013 Lab QCMW100% (1)
- Hazardous Materials Operating GuideDocument128 pagesHazardous Materials Operating GuidenhishamNo ratings yet
- Understanding and Responding To Self-Harm by Allan HouseDocument9 pagesUnderstanding and Responding To Self-Harm by Allan HousesimasNo ratings yet
- Identifikasi Kondisi Dan Penanganan Bangunan Pelengkap Infrastruktur JalanDocument6 pagesIdentifikasi Kondisi Dan Penanganan Bangunan Pelengkap Infrastruktur JalanFarhanNo ratings yet
- Implications of Covid-19 For Mental Health.Document3 pagesImplications of Covid-19 For Mental Health.Lina CasasNo ratings yet
- Base Oils: Technical Data Sheet NEXBASE 3043Document2 pagesBase Oils: Technical Data Sheet NEXBASE 3043Axel Mahya AvichenaNo ratings yet
- Political Science Assignment: POL QDocument4 pagesPolitical Science Assignment: POL QEktaNo ratings yet
- Abs Sire Directory 23Document40 pagesAbs Sire Directory 23sfranjul64No ratings yet
- True or False (8 PTS.) : Bio 11 2 Lecture LE Mock Exam October 2015Document8 pagesTrue or False (8 PTS.) : Bio 11 2 Lecture LE Mock Exam October 2015Alexander Miguel SyNo ratings yet
- STEB Asia - Biskuat FIFA Promo 2021Document4 pagesSTEB Asia - Biskuat FIFA Promo 2021imeldaNo ratings yet
- Hearst Demystifying Media Fireside Chat - The Bloomberg Way With Matthew WinklerDocument16 pagesHearst Demystifying Media Fireside Chat - The Bloomberg Way With Matthew WinklerDemystifying MediaNo ratings yet
- Microsoft-Case StudyDocument26 pagesMicrosoft-Case StudyHiten GuptaNo ratings yet
- Customer Satisfaction and Employee InvolvementDocument36 pagesCustomer Satisfaction and Employee InvolvementMaria Rebecca Toledo SalarNo ratings yet
- Analysis and Design of A Charge Pump Circuit For High CurrentDocument4 pagesAnalysis and Design of A Charge Pump Circuit For High CurrenthsharghiNo ratings yet
- SKYPAD Pocket Firmware Instructions PDFDocument3 pagesSKYPAD Pocket Firmware Instructions PDFAbelito FloresNo ratings yet
- Creation, Torah, and Revealed Wisdom in Some Second Temple Sapiential Texts (Sirach, 4qinstruction, 4Q185, and 4Q525) : A Response To John KampenDocument24 pagesCreation, Torah, and Revealed Wisdom in Some Second Temple Sapiential Texts (Sirach, 4qinstruction, 4Q185, and 4Q525) : A Response To John KampenKent Jerson CasianoNo ratings yet
- The Pavilion Lounge: A Cricket Themed LoungeDocument34 pagesThe Pavilion Lounge: A Cricket Themed LoungeShreya DGNo ratings yet
- Benevision N22/N19/N17/N15/ N12: Quick Reference GuideDocument40 pagesBenevision N22/N19/N17/N15/ N12: Quick Reference GuideVinoth RaviNo ratings yet
- Prevalence of Interpersonal Violence Against Athletes in The Sport Context (2017)Document5 pagesPrevalence of Interpersonal Violence Against Athletes in The Sport Context (2017)Juan Kmilo Martinez FernandezNo ratings yet
- CSC 218 Notes 3Document8 pagesCSC 218 Notes 3Musa JubrilNo ratings yet
- Assignment 2 Lesson Plan AnalysisDocument14 pagesAssignment 2 Lesson Plan Analysisapi-373008418No ratings yet
- Janome 900CPX Coverstitch Sewing Machine Instruction ManualDocument26 pagesJanome 900CPX Coverstitch Sewing Machine Instruction ManualiliiexpugnansNo ratings yet
- Neos 100Document34 pagesNeos 100David Bustamante ReyNo ratings yet
- Lesson Plan Year 3 LNS Pets WorldDocument6 pagesLesson Plan Year 3 LNS Pets WorldtgDeanNo ratings yet
- Helsinki Finnish Linus Torvalds Linux KernelDocument6 pagesHelsinki Finnish Linus Torvalds Linux KernelArnav PrasadNo ratings yet
- Draft Minutes Apr 5, 2023Document5 pagesDraft Minutes Apr 5, 2023PPSMU PAMPANGA PPONo ratings yet
- Inductive and Deductive ReasoningDocument6 pagesInductive and Deductive Reasoningkiahjessie100% (3)
- The Nature of Human Resource ManagementDocument14 pagesThe Nature of Human Resource ManagementEmerito PerezNo ratings yet
- Modal Testing of A Flexible Wing On A Dynamically Active Test Fixture Using The Fixed Base Correction MethodDocument22 pagesModal Testing of A Flexible Wing On A Dynamically Active Test Fixture Using The Fixed Base Correction Methodscramjet007No ratings yet