Professional Documents
Culture Documents
Heart Failure
Heart Failure
Uploaded by
Leni YulisCopyright:
Available Formats
You might also like
- Katherine Byrne, Tuberculosis and The Victorian: Literary ImaginationDocument5 pagesKatherine Byrne, Tuberculosis and The Victorian: Literary ImaginationMaria Eliza GiuboruncaNo ratings yet
- ARRYTHMIASDocument3 pagesARRYTHMIASitstheboyjayyNo ratings yet
- SMLE MapDocument1 pageSMLE MapNazem Abd RaboNo ratings yet
- CNS CNS CNSDocument46 pagesCNS CNS CNSqnmx7br6dsNo ratings yet
- AortaDocument1 pageAortaNoelle Grace Ulep BaromanNo ratings yet
- Anatomi Dan Fisiologi Sistem Kardiovaskular: Hendra FirmansyahDocument19 pagesAnatomi Dan Fisiologi Sistem Kardiovaskular: Hendra Firmansyahrandy sepasaciNo ratings yet
- List of Arteries of The Human BodyDocument9 pagesList of Arteries of The Human BodymohammedNo ratings yet
- Maternal ReviewerDocument2 pagesMaternal ReviewerLIZA CAMILLE R. ONDARONo ratings yet
- Cardiovascular Physiology: Lectures by Jan MachartDocument89 pagesCardiovascular Physiology: Lectures by Jan MachartFitri UlansariNo ratings yet
- Contoh Lain: Husenynov AUDIO - Mov - Google Drive - WebarchiveDocument10 pagesContoh Lain: Husenynov AUDIO - Mov - Google Drive - WebarchiveDomas Nurchandra PramudiantiNo ratings yet
- 2 2PharmaCHFDiureticsVISION-EDITED PDFDocument12 pages2 2PharmaCHFDiureticsVISION-EDITED PDFMarinelaNo ratings yet
- Portal Hypertension MindMapDocument1 pagePortal Hypertension MindMapjeeva pkpNo ratings yet
- Anatomy of The Heart: Anterior ViewDocument1 pageAnatomy of The Heart: Anterior ViewasjsANo ratings yet
- Closely Associated Associated W/: Manages Cholesterol PlaqueDocument1 pageClosely Associated Associated W/: Manages Cholesterol Plaquealnas2215630No ratings yet
- Unit 3 PhysioDocument107 pagesUnit 3 PhysioDhanush kannanNo ratings yet
- 4 - Biomechanics - Cardiovascular BiomechanicsDocument42 pages4 - Biomechanics - Cardiovascular Biomechanicsandirahmawan99No ratings yet
- 10 - Aortic Diseases (Illustrations Key)Document2 pages10 - Aortic Diseases (Illustrations Key)Asingwire BelindaNo ratings yet
- 1 1iwakirifisopatolclinliv14Document11 pages1 1iwakirifisopatolclinliv14alexandresarradeyNo ratings yet
- Coughdyspnea 2511 ArticleDocument1 pageCoughdyspnea 2511 ArticleGissele ParaisoNo ratings yet
- Right Ventricular Involvement PosterDocument1 pageRight Ventricular Involvement PosterAde JunadiNo ratings yet
- Hypertensive RetinopathyDocument4 pagesHypertensive RetinopathyNikithaNo ratings yet
- Aortic Regurgitation PathophysiologyDocument1 pageAortic Regurgitation Pathophysiologydana100% (1)
- The HeartDocument58 pagesThe HeartJULIUS NAKANYALANo ratings yet
- 2 AQA Biology Organisation Knowledge MAT Part 2 GCSEDocument4 pages2 AQA Biology Organisation Knowledge MAT Part 2 GCSEMN NgọcNo ratings yet
- AnatomyDocument1 pageAnatomyAnonymous hkWIKjoXFVNo ratings yet
- Heart DissectionDocument12 pagesHeart DissectionMary Joem Abigael TacaldoNo ratings yet
- Heart FailureDocument5 pagesHeart FailureHiba Suliman100% (1)
- Poster Transthoracic Echocardiography 160000352 V01 0322 LRDocument1 pagePoster Transthoracic Echocardiography 160000352 V01 0322 LRmariano.vicchio75No ratings yet
- Heart 3Document1 pageHeart 3shayna.katraNo ratings yet
- Animal TransportDocument26 pagesAnimal TransportRand HusseinNo ratings yet
- Tiếng Anh Chuyên Ngành - Trắc Nghiệm 2Document3 pagesTiếng Anh Chuyên Ngành - Trắc Nghiệm 2Nguyễn Thiện LuânNo ratings yet
- Untitled NotebookDocument12 pagesUntitled NotebookEvil QTNo ratings yet
- CVS Drugs NewDocument46 pagesCVS Drugs NewreemonsantoNo ratings yet
- Streptoccocus BHA: Gagal Jantung KananDocument2 pagesStreptoccocus BHA: Gagal Jantung KananSetyawan Aditya Pambudi SNo ratings yet
- VHD'S: Mitral Stenosis Aortic Stenosis Rheumatic FeverDocument2 pagesVHD'S: Mitral Stenosis Aortic Stenosis Rheumatic Feverkilladim992No ratings yet
- Physiology Revision CVS Part 3Document20 pagesPhysiology Revision CVS Part 3Gauri BendreNo ratings yet
- Cardiovascular ShockDocument3 pagesCardiovascular Shockkavindeep15122004No ratings yet
- Pathophysio CRF2 - RevisedDocument1 pagePathophysio CRF2 - Reviseddeborah malnegroNo ratings yet
- Heart ConditionsDocument1 pageHeart ConditionsNirmesh ThanabalanNo ratings yet
- A18 BODY FLUIDS in Human BodyDocument1 pageA18 BODY FLUIDS in Human Bodyservoculus machatteNo ratings yet
- Anatomy Physiology of The CV SystemDocument29 pagesAnatomy Physiology of The CV SystemMaedehNo ratings yet
- Im NotesDocument1 pageIm NotesNicole GayetaNo ratings yet
- Science - Circulatory SystemDocument1 pageScience - Circulatory SystemMUHAMMAD AZKA GHULAM IDRUS 2020bNo ratings yet
- Netter's Anatomy Coloring 2345Document1 pageNetter's Anatomy Coloring 2345Andreea GheorgheNo ratings yet
- FL 2.4 KardiodinamikaDocument29 pagesFL 2.4 KardiodinamikanazhifatihananNo ratings yet
- The HeartDocument15 pagesThe HeartNursyNurseNo ratings yet
- Pa Tho Physiology of Congestive Heart FailureDocument3 pagesPa Tho Physiology of Congestive Heart FailureErin MarieNo ratings yet
- Compare & Contrast Map (Point-to-Point)Document1 pageCompare & Contrast Map (Point-to-Point)طفوف محمد.No ratings yet
- Female InfertilityDocument1 pageFemale InfertilityHawraa AbbasNo ratings yet
- Cardio CostanzoDocument71 pagesCardio CostanzoShellz2428No ratings yet
- Cirsoid Aneurysm OF THE Uterus: Specific Arteriographic: Read As I8o/oo Mm. HG But Fellto Io/8o MMDocument7 pagesCirsoid Aneurysm OF THE Uterus: Specific Arteriographic: Read As I8o/oo Mm. HG But Fellto Io/8o MMLouis HadiyantoNo ratings yet
- Arterial Anatomy of The Female Genital Tract - Variations and Relevance To Transcatheter Embolization of The UterusDocument12 pagesArterial Anatomy of The Female Genital Tract - Variations and Relevance To Transcatheter Embolization of The UterusFelipe Wei Ning WangNo ratings yet
- Arterial Line Waveform Interpretation UHL Childrens Intensive Care GuidelineDocument5 pagesArterial Line Waveform Interpretation UHL Childrens Intensive Care GuidelineDhony100% (1)
- Fisiologia CardiovascularDocument72 pagesFisiologia CardiovascularANDRES GUARDIA CAYONo ratings yet
- DPJG - In: .In?:..:om:'.ye..nDocument4 pagesDPJG - In: .In?:..:om:'.ye..ndonnaNo ratings yet
- Biology O Level Summary NotesDocument4 pagesBiology O Level Summary NotesAdriana MuzfirahNo ratings yet
- Pathophysiology of Chronic Renal Failure (Condensed) Part 2Document1 pagePathophysiology of Chronic Renal Failure (Condensed) Part 2deborah malnegro100% (5)
- Portal HypertensionDocument1 pagePortal HypertensionSEELAM HEPSIBANo ratings yet
- ICBA NotesDocument60 pagesICBA NotesAndrew EldeiryNo ratings yet
- Grade 6 - Specific Outcomes: Can Affect Human Development From Conception Through BirthDocument49 pagesGrade 6 - Specific Outcomes: Can Affect Human Development From Conception Through Birthapi-253059746No ratings yet
- 13 B 2 NDocument7 pages13 B 2 NRay Ramilo100% (1)
- I Slams War On TerrorDocument0 pagesI Slams War On TerrorkhalidpandithNo ratings yet
- (Instructor Version) : Packet Tracer - Ipv6 Dynamic Routing - EigrpDocument3 pages(Instructor Version) : Packet Tracer - Ipv6 Dynamic Routing - EigrpJangjung gmail.comNo ratings yet
- FNM104 Prelim ReviewerDocument8 pagesFNM104 Prelim ReviewerjelciumNo ratings yet
- Aits 2223 FT Vi Jeem OfflineDocument15 pagesAits 2223 FT Vi Jeem OfflineSuvrajyoti TaraphdarNo ratings yet
- The Separation and Synthesis of Lipidic 1,2-And 1,3-Diols From Natural Phenolic Lipids For The Complexation and Recovery of BoronDocument23 pagesThe Separation and Synthesis of Lipidic 1,2-And 1,3-Diols From Natural Phenolic Lipids For The Complexation and Recovery of BoronNanasaheb PatilNo ratings yet
- Exploring Combinations and The Pascal Triangle Through MusicDocument17 pagesExploring Combinations and The Pascal Triangle Through MusicWayne Pedranti100% (2)
- Ruskin Bonds "THE KITE MAKER"Document14 pagesRuskin Bonds "THE KITE MAKER"Dhruti Galgali38% (8)
- Job Opportunities Sydney 7082017Document10 pagesJob Opportunities Sydney 7082017Dianita CorreaNo ratings yet
- Every Office Has OneDocument2 pagesEvery Office Has OneVeronicaGelfgrenNo ratings yet
- Souvenir Program ContractDocument1 pageSouvenir Program ContractAnthony GonzalesNo ratings yet
- Cronin 1992Document15 pagesCronin 1992Marcela GonzálezNo ratings yet
- IB Chemistry - SL Topic 7 Questions 1Document19 pagesIB Chemistry - SL Topic 7 Questions 1vaxor16689No ratings yet
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- Technical InstructionsDocument6 pagesTechnical InstructionsSadinjana LakshanNo ratings yet
- Environmental ScienceDocument2 pagesEnvironmental Sciencegillianbernice.alaNo ratings yet
- Water Flow Meter South AfricaDocument2 pagesWater Flow Meter South AfricaH2oNetNo ratings yet
- University of The Philippines Open University Faculty of Management and Development Studies Master of Management ProgramDocument10 pagesUniversity of The Philippines Open University Faculty of Management and Development Studies Master of Management ProgramRoldan TalaugonNo ratings yet
- NIOS Class 12 Psychology Chapter 10 EmotionsDocument4 pagesNIOS Class 12 Psychology Chapter 10 Emotionsmanahil dollNo ratings yet
- Chapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020Document33 pagesChapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020temesgen yohannesNo ratings yet
- Organisational Analysis of Hero Motocorp and Eicher Motors: Group 9Document7 pagesOrganisational Analysis of Hero Motocorp and Eicher Motors: Group 9Rupanshi JaiswalNo ratings yet
- Transmission Structures and Foundations:: CourseDocument8 pagesTransmission Structures and Foundations:: CoursejulianobiancoNo ratings yet
- Importing Google Earth Data Into A GISDocument15 pagesImporting Google Earth Data Into A GISJONAMNo ratings yet
- Buying Guide Truck Scales EN v11 Low PDFDocument80 pagesBuying Guide Truck Scales EN v11 Low PDFBồ Công AnhNo ratings yet
- Multimedia Chapter 1 and 2Document22 pagesMultimedia Chapter 1 and 2tsegab bekeleNo ratings yet
- Questions Energy Surfaces and Spontaneous ReactionsDocument2 pagesQuestions Energy Surfaces and Spontaneous Reactionshernys NietoNo ratings yet
- Psycholinguistics: What It Is? - Language, Speech and Communication.Document4 pagesPsycholinguistics: What It Is? - Language, Speech and Communication.Edo PrasetiaNo ratings yet
- Nutr1020 Dietary AnalysisDocument4 pagesNutr1020 Dietary Analysisapi-318180415No ratings yet
Heart Failure
Heart Failure
Uploaded by
Leni YulisOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Heart Failure
Heart Failure
Uploaded by
Leni YulisCopyright:
Available Formats
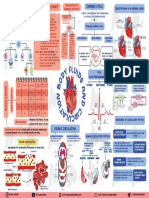
Risk Factor
Systemic Inflammation of
Coronary Hypertension/ Myocarditis, Stenosis AV Valve
Systemic Factors
Atherosclerosis Pulmonary Endocarditis, and Semiluron Valve
Hypertension Rheumatism
HEART FAILURE
ECG
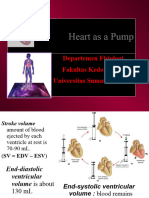
Decreased Cardiac Output related Less Volume of The left ventricle fails to pump
Artery Blood
The right ventricle fails to
to decreased ventricular filling blood from the lungs pump blood from the lungs
(preload) as evidence by
high blood pressure
Pulmonary circulation
Diastolic pressure rises
Offload the pressure Chest X-Ray
Short Tem: Renin release
Sympathetic
- Patient demonstrates adequate cardiac output as
evidenced by blood pressure and pulse rate and
rhythm within normal parameters for patient; strong Angiotensin I is
peripheral pulses; and an ability to tolerate activity Fluid pushed into the alveoli Right atrium dam
Converted to
without symptoms of dyspnea, syncope, or chest pain. vasodilator Angiotensin II
-Patient exhibits warm, dry skin, eupnea with absence therapy
of pulmonary crackles. Cough
-Patient remains free of side effects from the Systemic vein
medications used to achieve adequate cardiac output. Reduced oxygen dam
supply
Long term: Vasoconstriction of Increased blood
Increased
aldosteron
-Patient explains actions and precautions to take for blood vessels pressure
Secression
cardiac disease. Accumulation of
lactic acid
Dyspnea
Reabsorption Na +
GFR H2O in the extracle
room
Enlarged hepatic
veins
INDEPENDENT NURSING INTERVENTIONS:
The balance of Na
- Record intake and output. If patient is acutely ill, measure hourly urine in blood changes
Hepatomegaly
output and note decreases in output.
Impaired gas exchage related to
- For patients with increased preload, limit fluids and sodium as ordered.
ventilation-perfusion inequality as
- Place on cardiac monitor; monitor for dysrhythmias, especially atrial Pain acute
fibrillation.
evidenced by cannot catch her
- Position patient in semi-Fowler’s to high-Fowler’s Edema breath Portal vessel
pressure
COLLABORATIVE INTERVENTIONS:
-Examine laboratory data, especially arterial blood gases and electrolytes,
including potassium. Fluid Volume Excess related to Fluid pushed into the
- Monitor laboratory tests such as complete blood count, sodium level, and excessive fluid intake as evidence by abdominal cavity
serum creatinine. generalized edema
- Administer medications as prescribed, noting side effects and toxicity. Diuretic Therapy
- Review results of EKG and chest Xray.
OUTCOME MET: Ascites
Short Tem:
- Patient demonstrates adequate cardiac output as
evidenced by blood pressure and pulse rate and Short Term: Short Term:
rhythm within normal parameters for patient; strong - Patient is normovolemic as evidenced by urine output After 2 hours of nursing intervention the patient will able to : Anxiety related to
peripheral pulses; and an ability to tolerate activity greater than or equal to 30 mL/hr. -maintain optimal gas exchange as evidenced by usual mental status, breathlessness from
without symptoms of dyspnea, syncope, or chest pain. - Patient has balanced intake and output and stable weight. unlabored respirations at 12-20 per minute, oximetry results within normal inadequare oxygenation
-Patient exhibits warm, dry skin, eupnea with absence limits, blood gases with normal range and baseline HR for patient.
- Patient maintains HR 60 to 100 beats/min.
of pulmonary crackles. -Patient maintains clear lung fields and remains free signs of respiratory
-Patient remains free of side effects from the - Patient has clear lung sounds as manifested by absence of
medications used to achieve adequate cardiac output. pulmonary crackles. distress.
- Patient verbalizes awareness of causative factors and Long Term:
Long term: behaviors essential to correct fluid excess. Upon Discharge the patient will be able to: Short Term: After 2 hours of nursing interventions, the
-Patient explains actions and precautions to take for -Participates in procedures to optimize oxygenation and in management patient will be able to:
cardiac disease. Long Term: regimen within level of capability/condition. a. Verbalize awareness of feelings of anxiety
-Patient explains measures that can be taken to treat or -Patient manifests resolution or absence of symptoms of respiratory b. Demonstrate reduced anxiety levels
prevent fluid volume excess. distress.
-Patient describes symptoms that indicate the need to Long Term: Upon discharge, the patient will be able
to:
consult with health care provider.
a. Identify at least 2 healthy ways to deal with
anxiety.
INDEPENDENT NURSING INTERVENTIONS:
OUTCOME MET:
Short Term: -Assess respiratory rate, depth and effort including the use of accessory muscles,
- Patient is normovolemic as evidenced by urine output nasal flaring and abnormal breathing patterns. INDEPENDENT NURSING INTERVENTIONS:
greater than or equal to 30 mL/hr. -Observe for nail beds, cyanosis in skin, especially note the color of the tongue 1. Assess for signs of anxiety:
- Patient has balanced intake and output and stable INDEPENDENT NURSING INTERVENTIONS:
and oral mucous membrane. a. Feelings of panic, fear, and uneasiness.
weight. b. Tachycardia
- Patient maintains HR 60 to 100 beats/min. - Monitor fluid status closely: Auscultate lungs, compare daily body -Monitor oxygen saturation continuously using pulse oximetry.
c. Cold or sweaty hands or feet
- Patient has clear lung sounds as manifested by weights, and monitor intake and output. -Monitor chest x-ray results d. Shortness of breath
absence of pulmonary crackles. - Position patient, or teach patient how to assume a position, that -Position patient with head of the bed elevated, in a semi-fowler’s position as e. Restlessness
- Patient verbalizes awareness of causative factors and facilitates breathing (increase number of pillows, elevate the head of tolerated. Rationale: Dyspnea can become much worse with anxiety since it causes rapid, shallow breathing.
behaviors essential to correct fluid excess. bed), or patient may prefer to sit in a comfortable armchair to sleep.
-Encourage or assist with ambulation as per physician’s order.
- Assess for skin breakdown, and institute preventive measures THERAPEUTIC INTERVENTIONS:
(frequent changes of position, positioning to avoid -Instruct and encourage patient in diaphragmatic breathing and effective
Long Term: 1. Encourage the use of relaxation techniques
pressure, leg exercises). coughing.
-Patient explains measures that can be taken to treat or Rationale: To reduce panic and fear and to consciously produce the body’s relaxed state characterized by
prevent fluid volume excess. - Teach patient to adhere to a low-sodium diet by reading food labels -Assess home environment for irritants that impair gas exchange. slower breathing, lower blood pressure, and a sense of calmness.
-Patient describes symptoms that indicate the need to and avoiding commercially prepared convenience foods. 2. Administer oxygen during the acute stage
consult with health care provider. - Assist patient to adhere to any fluid restriction by planning the fluid Collaborative Interventions: Rationale: to diminish the work of breathing and to increase comfort
distribution throughout the day while maintaining dietary preferences. -Administer oxygen by the method prescribed
COLLABORATIVE INTERVENTIONS:
- Administer diuretics early in the morning so that diuresis does not
disturb nighttime rest.
- Monitor IV fluids closely; contact physician or pharmacist about the
possibility of double-concentrating any medications.
Outcome Met
Short Term:
After 2 hours of nursing intervention the patient was able to : Outcomes was met
-maintain optimal gas exchange as evidenced by usual mental status, unlabored Short Term: After 2 hours of nursing interventions, the patient will be able to:
a. Verbalize awareness of feelings of anxiety
respirations at 12-20 per minute, oximetry results within normal limits, blood gases b. Demonstrate reduced anxiety levels as evidenced by a calm demeanor
with normal range and baseline HR for patient. and cooperative behavior
-Patient maintains clear lung fields and remains free signs of respiratory distress.
Long Term: Long Term: Upon discharge, the patient will be able to”
Upon Discharge the patient will be able to: a. Identify 2 healthy ways to deal with anxiety such as relaxation
techniques
-Demonstrates diaphragmatic breathing.
You might also like
- Katherine Byrne, Tuberculosis and The Victorian: Literary ImaginationDocument5 pagesKatherine Byrne, Tuberculosis and The Victorian: Literary ImaginationMaria Eliza GiuboruncaNo ratings yet
- ARRYTHMIASDocument3 pagesARRYTHMIASitstheboyjayyNo ratings yet
- SMLE MapDocument1 pageSMLE MapNazem Abd RaboNo ratings yet
- CNS CNS CNSDocument46 pagesCNS CNS CNSqnmx7br6dsNo ratings yet
- AortaDocument1 pageAortaNoelle Grace Ulep BaromanNo ratings yet
- Anatomi Dan Fisiologi Sistem Kardiovaskular: Hendra FirmansyahDocument19 pagesAnatomi Dan Fisiologi Sistem Kardiovaskular: Hendra Firmansyahrandy sepasaciNo ratings yet
- List of Arteries of The Human BodyDocument9 pagesList of Arteries of The Human BodymohammedNo ratings yet
- Maternal ReviewerDocument2 pagesMaternal ReviewerLIZA CAMILLE R. ONDARONo ratings yet
- Cardiovascular Physiology: Lectures by Jan MachartDocument89 pagesCardiovascular Physiology: Lectures by Jan MachartFitri UlansariNo ratings yet
- Contoh Lain: Husenynov AUDIO - Mov - Google Drive - WebarchiveDocument10 pagesContoh Lain: Husenynov AUDIO - Mov - Google Drive - WebarchiveDomas Nurchandra PramudiantiNo ratings yet
- 2 2PharmaCHFDiureticsVISION-EDITED PDFDocument12 pages2 2PharmaCHFDiureticsVISION-EDITED PDFMarinelaNo ratings yet
- Portal Hypertension MindMapDocument1 pagePortal Hypertension MindMapjeeva pkpNo ratings yet
- Anatomy of The Heart: Anterior ViewDocument1 pageAnatomy of The Heart: Anterior ViewasjsANo ratings yet
- Closely Associated Associated W/: Manages Cholesterol PlaqueDocument1 pageClosely Associated Associated W/: Manages Cholesterol Plaquealnas2215630No ratings yet
- Unit 3 PhysioDocument107 pagesUnit 3 PhysioDhanush kannanNo ratings yet
- 4 - Biomechanics - Cardiovascular BiomechanicsDocument42 pages4 - Biomechanics - Cardiovascular Biomechanicsandirahmawan99No ratings yet
- 10 - Aortic Diseases (Illustrations Key)Document2 pages10 - Aortic Diseases (Illustrations Key)Asingwire BelindaNo ratings yet
- 1 1iwakirifisopatolclinliv14Document11 pages1 1iwakirifisopatolclinliv14alexandresarradeyNo ratings yet
- Coughdyspnea 2511 ArticleDocument1 pageCoughdyspnea 2511 ArticleGissele ParaisoNo ratings yet
- Right Ventricular Involvement PosterDocument1 pageRight Ventricular Involvement PosterAde JunadiNo ratings yet
- Hypertensive RetinopathyDocument4 pagesHypertensive RetinopathyNikithaNo ratings yet
- Aortic Regurgitation PathophysiologyDocument1 pageAortic Regurgitation Pathophysiologydana100% (1)
- The HeartDocument58 pagesThe HeartJULIUS NAKANYALANo ratings yet
- 2 AQA Biology Organisation Knowledge MAT Part 2 GCSEDocument4 pages2 AQA Biology Organisation Knowledge MAT Part 2 GCSEMN NgọcNo ratings yet
- AnatomyDocument1 pageAnatomyAnonymous hkWIKjoXFVNo ratings yet
- Heart DissectionDocument12 pagesHeart DissectionMary Joem Abigael TacaldoNo ratings yet
- Heart FailureDocument5 pagesHeart FailureHiba Suliman100% (1)
- Poster Transthoracic Echocardiography 160000352 V01 0322 LRDocument1 pagePoster Transthoracic Echocardiography 160000352 V01 0322 LRmariano.vicchio75No ratings yet
- Heart 3Document1 pageHeart 3shayna.katraNo ratings yet
- Animal TransportDocument26 pagesAnimal TransportRand HusseinNo ratings yet
- Tiếng Anh Chuyên Ngành - Trắc Nghiệm 2Document3 pagesTiếng Anh Chuyên Ngành - Trắc Nghiệm 2Nguyễn Thiện LuânNo ratings yet
- Untitled NotebookDocument12 pagesUntitled NotebookEvil QTNo ratings yet
- CVS Drugs NewDocument46 pagesCVS Drugs NewreemonsantoNo ratings yet
- Streptoccocus BHA: Gagal Jantung KananDocument2 pagesStreptoccocus BHA: Gagal Jantung KananSetyawan Aditya Pambudi SNo ratings yet
- VHD'S: Mitral Stenosis Aortic Stenosis Rheumatic FeverDocument2 pagesVHD'S: Mitral Stenosis Aortic Stenosis Rheumatic Feverkilladim992No ratings yet
- Physiology Revision CVS Part 3Document20 pagesPhysiology Revision CVS Part 3Gauri BendreNo ratings yet
- Cardiovascular ShockDocument3 pagesCardiovascular Shockkavindeep15122004No ratings yet
- Pathophysio CRF2 - RevisedDocument1 pagePathophysio CRF2 - Reviseddeborah malnegroNo ratings yet
- Heart ConditionsDocument1 pageHeart ConditionsNirmesh ThanabalanNo ratings yet
- A18 BODY FLUIDS in Human BodyDocument1 pageA18 BODY FLUIDS in Human Bodyservoculus machatteNo ratings yet
- Anatomy Physiology of The CV SystemDocument29 pagesAnatomy Physiology of The CV SystemMaedehNo ratings yet
- Im NotesDocument1 pageIm NotesNicole GayetaNo ratings yet
- Science - Circulatory SystemDocument1 pageScience - Circulatory SystemMUHAMMAD AZKA GHULAM IDRUS 2020bNo ratings yet
- Netter's Anatomy Coloring 2345Document1 pageNetter's Anatomy Coloring 2345Andreea GheorgheNo ratings yet
- FL 2.4 KardiodinamikaDocument29 pagesFL 2.4 KardiodinamikanazhifatihananNo ratings yet
- The HeartDocument15 pagesThe HeartNursyNurseNo ratings yet
- Pa Tho Physiology of Congestive Heart FailureDocument3 pagesPa Tho Physiology of Congestive Heart FailureErin MarieNo ratings yet
- Compare & Contrast Map (Point-to-Point)Document1 pageCompare & Contrast Map (Point-to-Point)طفوف محمد.No ratings yet
- Female InfertilityDocument1 pageFemale InfertilityHawraa AbbasNo ratings yet
- Cardio CostanzoDocument71 pagesCardio CostanzoShellz2428No ratings yet
- Cirsoid Aneurysm OF THE Uterus: Specific Arteriographic: Read As I8o/oo Mm. HG But Fellto Io/8o MMDocument7 pagesCirsoid Aneurysm OF THE Uterus: Specific Arteriographic: Read As I8o/oo Mm. HG But Fellto Io/8o MMLouis HadiyantoNo ratings yet
- Arterial Anatomy of The Female Genital Tract - Variations and Relevance To Transcatheter Embolization of The UterusDocument12 pagesArterial Anatomy of The Female Genital Tract - Variations and Relevance To Transcatheter Embolization of The UterusFelipe Wei Ning WangNo ratings yet
- Arterial Line Waveform Interpretation UHL Childrens Intensive Care GuidelineDocument5 pagesArterial Line Waveform Interpretation UHL Childrens Intensive Care GuidelineDhony100% (1)
- Fisiologia CardiovascularDocument72 pagesFisiologia CardiovascularANDRES GUARDIA CAYONo ratings yet
- DPJG - In: .In?:..:om:'.ye..nDocument4 pagesDPJG - In: .In?:..:om:'.ye..ndonnaNo ratings yet
- Biology O Level Summary NotesDocument4 pagesBiology O Level Summary NotesAdriana MuzfirahNo ratings yet
- Pathophysiology of Chronic Renal Failure (Condensed) Part 2Document1 pagePathophysiology of Chronic Renal Failure (Condensed) Part 2deborah malnegro100% (5)
- Portal HypertensionDocument1 pagePortal HypertensionSEELAM HEPSIBANo ratings yet
- ICBA NotesDocument60 pagesICBA NotesAndrew EldeiryNo ratings yet
- Grade 6 - Specific Outcomes: Can Affect Human Development From Conception Through BirthDocument49 pagesGrade 6 - Specific Outcomes: Can Affect Human Development From Conception Through Birthapi-253059746No ratings yet
- 13 B 2 NDocument7 pages13 B 2 NRay Ramilo100% (1)
- I Slams War On TerrorDocument0 pagesI Slams War On TerrorkhalidpandithNo ratings yet
- (Instructor Version) : Packet Tracer - Ipv6 Dynamic Routing - EigrpDocument3 pages(Instructor Version) : Packet Tracer - Ipv6 Dynamic Routing - EigrpJangjung gmail.comNo ratings yet
- FNM104 Prelim ReviewerDocument8 pagesFNM104 Prelim ReviewerjelciumNo ratings yet
- Aits 2223 FT Vi Jeem OfflineDocument15 pagesAits 2223 FT Vi Jeem OfflineSuvrajyoti TaraphdarNo ratings yet
- The Separation and Synthesis of Lipidic 1,2-And 1,3-Diols From Natural Phenolic Lipids For The Complexation and Recovery of BoronDocument23 pagesThe Separation and Synthesis of Lipidic 1,2-And 1,3-Diols From Natural Phenolic Lipids For The Complexation and Recovery of BoronNanasaheb PatilNo ratings yet
- Exploring Combinations and The Pascal Triangle Through MusicDocument17 pagesExploring Combinations and The Pascal Triangle Through MusicWayne Pedranti100% (2)
- Ruskin Bonds "THE KITE MAKER"Document14 pagesRuskin Bonds "THE KITE MAKER"Dhruti Galgali38% (8)
- Job Opportunities Sydney 7082017Document10 pagesJob Opportunities Sydney 7082017Dianita CorreaNo ratings yet
- Every Office Has OneDocument2 pagesEvery Office Has OneVeronicaGelfgrenNo ratings yet
- Souvenir Program ContractDocument1 pageSouvenir Program ContractAnthony GonzalesNo ratings yet
- Cronin 1992Document15 pagesCronin 1992Marcela GonzálezNo ratings yet
- IB Chemistry - SL Topic 7 Questions 1Document19 pagesIB Chemistry - SL Topic 7 Questions 1vaxor16689No ratings yet
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- Technical InstructionsDocument6 pagesTechnical InstructionsSadinjana LakshanNo ratings yet
- Environmental ScienceDocument2 pagesEnvironmental Sciencegillianbernice.alaNo ratings yet
- Water Flow Meter South AfricaDocument2 pagesWater Flow Meter South AfricaH2oNetNo ratings yet
- University of The Philippines Open University Faculty of Management and Development Studies Master of Management ProgramDocument10 pagesUniversity of The Philippines Open University Faculty of Management and Development Studies Master of Management ProgramRoldan TalaugonNo ratings yet
- NIOS Class 12 Psychology Chapter 10 EmotionsDocument4 pagesNIOS Class 12 Psychology Chapter 10 Emotionsmanahil dollNo ratings yet
- Chapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020Document33 pagesChapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020temesgen yohannesNo ratings yet
- Organisational Analysis of Hero Motocorp and Eicher Motors: Group 9Document7 pagesOrganisational Analysis of Hero Motocorp and Eicher Motors: Group 9Rupanshi JaiswalNo ratings yet
- Transmission Structures and Foundations:: CourseDocument8 pagesTransmission Structures and Foundations:: CoursejulianobiancoNo ratings yet
- Importing Google Earth Data Into A GISDocument15 pagesImporting Google Earth Data Into A GISJONAMNo ratings yet
- Buying Guide Truck Scales EN v11 Low PDFDocument80 pagesBuying Guide Truck Scales EN v11 Low PDFBồ Công AnhNo ratings yet
- Multimedia Chapter 1 and 2Document22 pagesMultimedia Chapter 1 and 2tsegab bekeleNo ratings yet
- Questions Energy Surfaces and Spontaneous ReactionsDocument2 pagesQuestions Energy Surfaces and Spontaneous Reactionshernys NietoNo ratings yet
- Psycholinguistics: What It Is? - Language, Speech and Communication.Document4 pagesPsycholinguistics: What It Is? - Language, Speech and Communication.Edo PrasetiaNo ratings yet
- Nutr1020 Dietary AnalysisDocument4 pagesNutr1020 Dietary Analysisapi-318180415No ratings yet