Professional Documents
Culture Documents
Caa Hemorrhage
Caa Hemorrhage
Uploaded by
Gabriel Septiana CitraCopyright:
Available Formats
You might also like
- Segmconference2023 10-3-23 Ip-SpeakersDocument9 pagesSegmconference2023 10-3-23 Ip-Speakersapi-698589423No ratings yet
- Alarm Fatigue: Use of An Evidence-Based Alarm Management StrategyDocument8 pagesAlarm Fatigue: Use of An Evidence-Based Alarm Management StrategyMister BigglesworthNo ratings yet
- Caltech Coursera - Drugs&Brain - Report - Posting 8 Feb 2013Document12 pagesCaltech Coursera - Drugs&Brain - Report - Posting 8 Feb 2013Parker333No ratings yet
- Time - The Science of Weight Loss - 2019 PDFDocument99 pagesTime - The Science of Weight Loss - 2019 PDFSigitWibowo100% (5)
- Cerebral Amyloid Angiopathy A Systematic Review 2011Document9 pagesCerebral Amyloid Angiopathy A Systematic Review 2011Jaime Arevalo PanduroNo ratings yet
- What Research Shows: NARTH's Response To The APA Claims On HomosexualityDocument4 pagesWhat Research Shows: NARTH's Response To The APA Claims On Homosexualitybmx0No ratings yet
- Maruna and Mann 2006Document23 pagesMaruna and Mann 2006stephanieNo ratings yet
- Laura StephenDocument23 pagesLaura Stephenpepebyluis100% (1)
- Cerebral Amyloid AngiopathyDocument2 pagesCerebral Amyloid AngiopathyPaolo Giordano100% (1)
- A Meta-Analysis of Pornography Consumption and Actual Acts of Sexual Aggression in General Population StudiesDocument23 pagesA Meta-Analysis of Pornography Consumption and Actual Acts of Sexual Aggression in General Population Studiesaroa100% (1)
- Cardiac Amyloidosis: Name: Salam Majzoub Preceptor: Dr. Lama FaddoulDocument47 pagesCardiac Amyloidosis: Name: Salam Majzoub Preceptor: Dr. Lama Faddoulsalam majzoubNo ratings yet
- Colizzi Et Al., 2015 - Psychiatry - ResDocument8 pagesColizzi Et Al., 2015 - Psychiatry - ResdojabrNo ratings yet
- Peds 2013-2958Document11 pagesPeds 2013-2958Sean SubtesteNo ratings yet
- Pornography and Sexual Deviance: A Report of the Legal and Behavioral Institute, Beverly Hills, CaliforniaFrom EverandPornography and Sexual Deviance: A Report of the Legal and Behavioral Institute, Beverly Hills, CaliforniaNo ratings yet
- The Impact of Shock Wave Therapy at VariDocument9 pagesThe Impact of Shock Wave Therapy at VariArifSurtonoNo ratings yet
- 2020 - Slavin Et Al. Child Sexual Abuse and Compulsive Sexual Behavior - A Systematic Literature ReviewDocument21 pages2020 - Slavin Et Al. Child Sexual Abuse and Compulsive Sexual Behavior - A Systematic Literature ReviewAnapsi02100% (1)
- Bad Guidelines Management of Adults With Delusional InfestationDocument18 pagesBad Guidelines Management of Adults With Delusional InfestationRBGBGB RBGNo ratings yet
- Pubertal Suppression For Transgender Youth0897877001603408698Document15 pagesPubertal Suppression For Transgender Youth0897877001603408698Antorcha CANo ratings yet
- Exposing The Myth ofDocument7 pagesExposing The Myth ofnowayborngay0% (1)
- Tau Opa ThiesDocument22 pagesTau Opa ThiesIrina OdajiuNo ratings yet
- Homosexuality and The Scientific Evidence PDFDocument274 pagesHomosexuality and The Scientific Evidence PDFanon_113431634No ratings yet
- Alzheimers-Disease-Genetics-Fact-Sheet 0Document8 pagesAlzheimers-Disease-Genetics-Fact-Sheet 0api-285676076No ratings yet
- Imploding Gay Power: by Philip IrvinDocument4 pagesImploding Gay Power: by Philip IrvinnowayborngayNo ratings yet
- Fence Sitters: Parents' reactions to sexual ambiguities in their newborn children - מתוך מאמרה של מאירה וייסDocument18 pagesFence Sitters: Parents' reactions to sexual ambiguities in their newborn children - מתוך מאמרה של מאירה וייספרופסור מאירה וייסNo ratings yet
- Methylphenidate Side Effect Profile Is Influenced by Genetic Variation in The Attention-Deficit/Hyperactivity Disorder-Associated CES1 GeneDocument10 pagesMethylphenidate Side Effect Profile Is Influenced by Genetic Variation in The Attention-Deficit/Hyperactivity Disorder-Associated CES1 GeneMerari Lugo Ocaña100% (1)
- Am I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlDocument9 pagesAm I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlBlack HoleNo ratings yet
- Clinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956Document14 pagesClinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956abelim01100% (1)
- Debate On HomosexualsDocument2 pagesDebate On HomosexualsLiQinghuaNo ratings yet
- Polls On Attitudes On Homosexuality & Gay MarriageDocument88 pagesPolls On Attitudes On Homosexuality & Gay MarriageAmerican Enterprise InstituteNo ratings yet
- PEP Web - Stoller A Contribution To The Study of Gender IdentityDocument5 pagesPEP Web - Stoller A Contribution To The Study of Gender IdentityRamon Ferreira100% (1)
- PSYC-The Psychopathology of Everyday Life-Argumentative EssayDocument11 pagesPSYC-The Psychopathology of Everyday Life-Argumentative EssayHarrison MolloyNo ratings yet
- Discussing Potentials in Dimensional and Clinical Staging Models of Schizophrenia Diagnosis and How They Relate To The Problem of StigmaDocument14 pagesDiscussing Potentials in Dimensional and Clinical Staging Models of Schizophrenia Diagnosis and How They Relate To The Problem of StigmaGeorgeBaker100% (1)
- Gilman, Ken, Kenneth, Peter - Advances Pertaining To The Pharmacology and Interactions of Irreversible Nonselective Monoamine Oxidase InhibitorsDocument9 pagesGilman, Ken, Kenneth, Peter - Advances Pertaining To The Pharmacology and Interactions of Irreversible Nonselective Monoamine Oxidase Inhibitors朗博Cuauhtlatoa100% (1)
- Trans Pulse 2011Document3 pagesTrans Pulse 2011Daily XtraNo ratings yet
- Manual For Early Infant Male Circumcision Under Local AnaesthesiaDocument140 pagesManual For Early Infant Male Circumcision Under Local AnaesthesiaSabbir AhmedNo ratings yet
- Aust N Z J Psychiatry 2014 Gitlin 89 90Document3 pagesAust N Z J Psychiatry 2014 Gitlin 89 90KThreopusNo ratings yet
- Conversion Therapy: Consensus StatementDocument3 pagesConversion Therapy: Consensus StatementAlexandria Firdaus Al-farisyNo ratings yet
- Andropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneDocument14 pagesAndropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneYariCárdenasNo ratings yet
- Overview of Igg4 - Related Disease: Introduction - History, Definition, and Diagnostic CriteriaDocument6 pagesOverview of Igg4 - Related Disease: Introduction - History, Definition, and Diagnostic CriteriaStefan PopoviciNo ratings yet
- Victor Cline's Study PDFDocument22 pagesVictor Cline's Study PDFsolay12No ratings yet
- Vasculitis: VASCULITIS Is A Primary Inflammatory Disease Process of The VasculatureDocument43 pagesVasculitis: VASCULITIS Is A Primary Inflammatory Disease Process of The VasculaturelihayatiNo ratings yet
- Detransition Related Needs and Support A Cross Sectional Online SurveyDocument20 pagesDetransition Related Needs and Support A Cross Sectional Online SurveyZara LauraNo ratings yet
- Affidavit of Michelle CretellaDocument12 pagesAffidavit of Michelle CretellaDavid Hart0% (1)
- What Does It Mean To Be A Woman Research Paper 3Document16 pagesWhat Does It Mean To Be A Woman Research Paper 3api-608687083100% (1)
- Resource - Bad Actors in Conversion Therapy PDFDocument5 pagesResource - Bad Actors in Conversion Therapy PDFBrianna JanuaryNo ratings yet
- Treatment of Hypoglycemia in ChildrenDocument16 pagesTreatment of Hypoglycemia in ChildrenKamuiShirouNo ratings yet
- ALZHEIMER'S DISEASE - Colour & MagnetoDocument11 pagesALZHEIMER'S DISEASE - Colour & MagnetoDr Vaishali MathapatiNo ratings yet
- PDF - Why Dont We Prescribe MAOIsDocument11 pagesPDF - Why Dont We Prescribe MAOIsSarwar Baig100% (1)
- Vasculitic NeuropathiesDocument20 pagesVasculitic NeuropathiesHITIPHYSIONo ratings yet
- Background: Alpha ThalassemiaDocument24 pagesBackground: Alpha ThalassemiacristieristiieNo ratings yet
- Adolescent Sexuaiity: Judith Marks Mishne D.S.WDocument2 pagesAdolescent Sexuaiity: Judith Marks Mishne D.S.WRAHMANo ratings yet
- Update On The Efficacy of Pharmacotherapy For Social Anxiety Disorder: A Meta-AnalysisDocument12 pagesUpdate On The Efficacy of Pharmacotherapy For Social Anxiety Disorder: A Meta-AnalysisAnaaaerobios100% (1)
- Bilateral Thalamic LesionsDocument10 pagesBilateral Thalamic LesionsOralBoardsNo ratings yet
- Gay Affirmative Therapy PerlmanDocument11 pagesGay Affirmative Therapy PerlmanPsico Orientador100% (1)
- Management of IncontinenceDocument91 pagesManagement of IncontinenceVahid Msmi100% (1)
- Negative Symptoms in SchizophreniaDocument15 pagesNegative Symptoms in Schizophreniasyahrizon thomasNo ratings yet
- Sexual and Gender Identity DisordersDocument5 pagesSexual and Gender Identity DisordersKiana TehraniNo ratings yet
- Familial Non-Medullary Thyroid CancerDocument19 pagesFamilial Non-Medullary Thyroid CancerMikeyNo ratings yet
- Should Homosexuality Be LegalizedDocument4 pagesShould Homosexuality Be LegalizedSamamaSuhailNo ratings yet
- Males and Eating Disorders: William HarrymanDocument14 pagesMales and Eating Disorders: William HarrymanWilliam HarrymanNo ratings yet
- The Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis ResearchDocument29 pagesThe Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis Researchapi-246003035No ratings yet
- Angiopathy StrokeDocument7 pagesAngiopathy Strokearia tristayanthiNo ratings yet
- Noc110069 346 351Document6 pagesNoc110069 346 351Carlos AlvaradoNo ratings yet
- Main PDFDocument9 pagesMain PDFAmalia Gh,No ratings yet
- RCT Simvastatin AlzheimerDocument8 pagesRCT Simvastatin AlzheimerGabriel Septiana CitraNo ratings yet
- D Dimer Level in COVID 19 Infection A Systematic ReviewDocument12 pagesD Dimer Level in COVID 19 Infection A Systematic ReviewGabriel Septiana CitraNo ratings yet
- Abcde2 TiaDocument7 pagesAbcde2 TiaGabriel Septiana CitraNo ratings yet
- Surveillance IchDocument6 pagesSurveillance IchGabriel Septiana CitraNo ratings yet
- 2001 Prevalence of and Risk Factors For Carpal Tunnel Syndrome in A Rural PopulationDocument9 pages2001 Prevalence of and Risk Factors For Carpal Tunnel Syndrome in A Rural PopulationGabriel Septiana CitraNo ratings yet
- Company Profile: Sistema Inteligente de Color, Descubrir Tu Valor ExcepcionalDocument4 pagesCompany Profile: Sistema Inteligente de Color, Descubrir Tu Valor ExcepcionalOmar Stalin Lucio RonNo ratings yet
- Original Article /artículo Original: Muhlenbergia Angustata (Poaceae), Puno, PerúDocument10 pagesOriginal Article /artículo Original: Muhlenbergia Angustata (Poaceae), Puno, PerúBet MACNo ratings yet
- Adverse Childhood ExperiencesDocument8 pagesAdverse Childhood ExperiencesMa. Alicia Jimenez MartinezNo ratings yet
- AAO 2015 Atropine For Myopia DR Donald Tan 11-16-15 RedactedDocument15 pagesAAO 2015 Atropine For Myopia DR Donald Tan 11-16-15 RedactedunonounoNo ratings yet
- Final Year MBBS Video Lectures Links (Version - 1)Document7 pagesFinal Year MBBS Video Lectures Links (Version - 1)noorNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
- Evidence Based Validation of Traditional Medicines 2021Document1,135 pagesEvidence Based Validation of Traditional Medicines 2021shubham panditNo ratings yet
- Solitaire FR BrochureDocument2 pagesSolitaire FR Brochuredsk778894No ratings yet
- Motivation Dabur IndiaDocument84 pagesMotivation Dabur IndiaGuman SinghNo ratings yet
- HeadacheDocument22 pagesHeadacheAlma SunagawaNo ratings yet
- PHIN Laboratory Result ELR v231Document86 pagesPHIN Laboratory Result ELR v231anujaks_rlbNo ratings yet
- Community Medicine (PSM)Document7 pagesCommunity Medicine (PSM)Shashwathi MNo ratings yet
- Month 12 ProgressionDocument11 pagesMonth 12 Progressiongreg hofmanNo ratings yet
- Universal Crescent Power P LTD EIA Report Part IDocument66 pagesUniversal Crescent Power P LTD EIA Report Part ImanishxlriNo ratings yet
- - 113後中醫第2次模考試題及解答 頁面 3Document12 pages- 113後中醫第2次模考試題及解答 頁面 3liu634paulNo ratings yet
- CR Piopneumothoraks Nicky FIXdDocument62 pagesCR Piopneumothoraks Nicky FIXdPutri RahmawatiNo ratings yet
- Handbook Technology TransferDocument15 pagesHandbook Technology Transferzakarya wadiNo ratings yet
- SCIENCE-DRRR - Q1 - W5 - Mod2-Hazard-Its-Impact-Identification-and-Risk-Assessment-08082020Document27 pagesSCIENCE-DRRR - Q1 - W5 - Mod2-Hazard-Its-Impact-Identification-and-Risk-Assessment-08082020Stephanie PacquiaoNo ratings yet
- ABYIPDocument5 pagesABYIPJayson Guerrero100% (4)
- EczemaDocument1 pageEczemaKaniz WahabNo ratings yet
- FITT 1 Updated HandoutsDocument25 pagesFITT 1 Updated HandoutsJolina VillalobosNo ratings yet
- Chlorhexidine Gluconate 0.2% W/V Mouth Wash: Class: IndicationsDocument3 pagesChlorhexidine Gluconate 0.2% W/V Mouth Wash: Class: IndicationsAnonymous Bt6favSF4YNo ratings yet
- Lipoma ExcisionDocument4 pagesLipoma ExcisionNikolaus TalloNo ratings yet
- 10 STD Science BookDocument338 pages10 STD Science BookmkprabhuNo ratings yet
- IHDW GuidelinesDocument32 pagesIHDW GuidelinesCezara ZahariaNo ratings yet
- Cardiovascular Disease AssignmentDocument3 pagesCardiovascular Disease Assignmentapi-308874632No ratings yet
Caa Hemorrhage
Caa Hemorrhage
Uploaded by
Gabriel Septiana CitraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Caa Hemorrhage
Caa Hemorrhage
Uploaded by
Gabriel Septiana CitraCopyright:
Available Formats
Cerebral amyloid angiopathy with and
without hemorrhage
Evidence for different disease phenotypes
Andreas Charidimou, ABSTRACT
MD, PhD Objective: To gain insight into different cerebral amyloid angiopathy (CAA) phenotypes and mech-
Sergi Martinez-Ramirez, anisms, we investigated cortical superficial siderosis (CSS), a new imaging marker of the disease,
MD and its relation with APOE genotype in patients with pathologically proven CAA, who presented
Ashkan Shoamanesh, MD with and without intracerebral hemorrhage (ICH).
Jamary Oliveira-Filho,
Methods: MRI scans of 105 patients with CAA pathologic confirmation and MRI were analyzed
MD
for CSS (focal, #3 sulci; disseminates, $4 sulci) and other imaging markers. We compared path-
Matthew Frosch, PhD
ologic, imaging, and APOE genotype data between subjects with vs without ICH, and investigated
Anastasia Vashkevich, BA
associations between CSS and APOE genotype.
Alison Ayres, BA
Jonathan Rosand, MD, Results: Our cohort consisted of 54 patients with CAA with symptomatic lobar ICH and 51 with-
MSc out ICH. APOE genotype was available in 53 patients. More than 90% of pathology samples in
Mahmut Edip Gurol, both groups had neuritic plaques, whereas neurofibrillary tangles were more commonly present in
MD the patients without ICH (87% vs 42%, p , 0.0001). There was a trend for patients with CAA
Steven M. Greenberg, with ICH to more commonly have APOE e2 (48.7% vs 21.4%, p 5 0.075), whereas patients
MD, PhD without ICH were more likely to be APOE e4 carriers (85.7% vs 53.9%, p 5 0.035). Dissemi-
Anand Viswanathan, nated CSS was considerably commoner in patients with ICH (33.3% vs 5.9%, p , 0.0001). In
MD, PhD logistic regression, disseminated CSS was associated with APOE e2 (but not APOE e4) (odds ratio
5.83; 95% confidence interval 1.49–22.82, p 5 0.011).
Conclusions: This neuropathologically defined CAA cohort suggests that CSS and APOE e2 are
Correspondence to related to the hemorrhagic expression of the disease; APOE e4 is enriched in nonhemorrhagic
Dr. Charidimou:
acharidimou@mgh.harvard.edu CAA. Our study emphasizes the concept of different CAA phenotypes, suggesting divergent
pathophysiologic mechanisms. Neurology® 2015;84:1206–1212
GLOSSARY
AD 5 Alzheimer disease; BG 5 basal ganglia; CAA 5 cerebral amyloid angiopathy; CI 5 confidence interval; CMB 5 cerebral
microbleed; CSO 5 centrum semiovale; CSS 5 cortical superficial siderosis; EPVS 5 enlarged perivascular spaces; FLAIR 5
fluid-attenuated inversion recovery; ICH 5 intracerebral hemorrhage; IQR 5 interquartile range; MGH 5 Massachusetts
General Hospital; NFT 5 neurofibrillary tangle; OR 5 odds ratio; PVS 5 perivascular spaces; STRIVE 5 Standards for
Reporting Vascular Changes on Neuroimaging; SWI 5 susceptibility-weighted imaging; T2*-GRE 5 T2*-weighted
gradient-recalled echo; WMH 5 white matter hyperintensities.
Sporadic cerebral amyloid angiopathy (CAA) is a small vessel disease that preferentially involves
small cortical and leptomeningeal arteries due to progressive amyloid-b deposition in their
walls.1,2 CAA occurs frequently in elderly people, and is a common and important cause of
symptomatic lobar intracerebral hemorrhage (ICH).1–3 However, CAA might present without
major lobar ICH, but instead with cognitive impairment (either chronic or rapidly progressive),
or transient focal neurologic symptoms.4 CAA is almost invariably found in Alzheimer disease
(AD), but in most cases is relatively mild.5
CAA is also associated with characteristic MRI biomarkers, including strictly lobar cerebral mi-
crobleeds (CMBs), cortical superficial siderosis (CSS),6 centrum semiovale (CSO) perivascular
spaces (PVS), and white matter hyperintensities (WMH).1,7 These neuroimaging markers
Editorial, page 1190
From the Department of Brain Repair and Rehabilitation (A.C.), UCL Institute of Neurology and The National Hospital for Neurology
and Neurosurgery, London, UK; and the Hemorrhagic Stroke Research Program, Stroke Research Center, Department of Neurology (A.C.,
S.M.-R., A.S., J.O.-F., A. Vashkevich, A.A., J.R., M.E.G., S.M.G., A. Viswanathan), C.S. Kubik Laboratory for Neuropathology (M.F.),
Division of Neurocritical Care and Emergency Neurology (J.R.), and Center for Human Genetic Research (J.R.), Massachusetts General
Hospital, Harvard Medical School, Boston.
Go to Neurology.org for full disclosures. Funding information and disclosures deemed relevant by the authors, if any, are provided at the end of the article.
1206 © 2015 American Academy of Neurology
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
probably reflect related but distinct aspects of ,1 cm) or samples from clot evacuations not containing any
assessable vessels; (2) autopsy studies not grading CAA; and (3)
CAA pathophysiology. CSS in particular is an
known alternative causes for lobar ICH. A total of 192 patients
interesting recently recognized form of CAA- were eligible for analysis. Patients with no pathologic evidence of
related hemorrhage, which likely reflects CAA (n 5 54), clinical/imaging presentations not characteristic of
repeated episodes of blood leaking into the sub- CAA (3 cases with deep ICH and 9 with ischemic stroke at baseline),
no T2 or T2*-GRE MRI (n 5 18), T2/T2*-GRE MRI of
arachnoid space from brittle and fragile CAA- insufficient quality (n 5 2), and irretrievable sequences (n 5 1)
affected vessels. CSS has been shown to carry a were excluded.
high risk of future symptomatic lobar ICH.6,8,9 Demographic and clinical information was obtained from
prospective databases and medical records using standardized data
Genetic factors, such as APOE genotype,
collection forms. Variables of interest were age, sex, history of
are important in the pathophysiology of hypertension, antithrombotic drug use, and clinical presentation
CAA.10,11 APOE e4 appears to enhance vascu- at baseline. APOE genotype was determined in a subset of pa-
lar amyloid-b deposition in a dose-dependent tients who provided blood samples and consented to genetic test-
ing as previously described,15 and without knowledge of clinical
fashion,12 while APOE e2 promotes vasculo-
or neuroimaging data.
pathic changes that can lead to vessel rup- The original clinical presentation of patients was ascertained
ture.13 To gain further insights into different from all available neuroimaging, pathologic, and clinical data,
CAA phenotypes and potential mechanisms,14 and was determined as either symptomatic lobar ICH confirmed
on neuroimaging or nonhemorrhagic (including cognitive
we investigated associations between neuroi- impairment, transient focal neurologic episodes, or other neuro-
maging markers of the disease, APOE geno- logic symptoms). Cases of inflammatory CAA were included in
type, and pathologic findings in patients the analysis when an MRI outside the acute phase ($1 month)
was available. To investigate the stability of the non-ICH CAA
with CAA presenting with and without symp-
clinical phenotypes, we extrapolated follow-up information from
tomatic ICH. We hypothesized that (1) hem- prospective databases and medical records on incident sympto-
orrhagic markers of CAA (CSS and lobar matic ICH.
CMBs) would be more strongly associated
Standard protocol approvals, registrations, and patient
with APOE e2 genotype; (2) hemorrhagic consents. The study received ethical approval by the institu-
markers of disease severity in CAA (CSS and tional review board of MGH.
lobar CMBs) and APOE e2 genotype would Pathologic data collection. Morphologic assessment was per-
be more common in patients presenting with formed in routine hematoxylin & eosin staining and the presence
symptomatic ICH than in those presenting or absence and severity of vascular amyloid-b deposition was
confirmed by immunohistochemical detection or Congo red
without ICH; and (3) neurofibrillary tangles staining. CAA presence and severity was assessed in all available
(NFTs) will be more common in nonhemor- vessels. Cases were considered positive for CAA when they had at
rhagic compared to hemorrhagic CAA, least 1 leptomeningeal or cortical vessel with amyloid-b reported,
whereas amyloid plaques might be invariably providing enough information to reliably classify CAA severity
using the Vonsattel grading system16,17 and were classified as mild
present in the 2 groups due to their close (Vonsattel grade 1) or moderate to severe (Vonsattel grades 2–4).
molecular pathogenesis. Where available from neuropathology reports, we also systemat-
ically extracted information on neuritic plaques and NFTs as-
sessed in routinely immunostained sections for amyloid-b and
METHODS Case selection and clinical data collection.
phosphorylated tau and recorded as present or absent.
We included all eligible patients from Massachusetts General Hospi-
tal (MGH) identified retrospectively by a systematic keyword search Neuroimaging data and analysis. Imaging for all patients
of pathology reports and prospective clinical databases. Cases were included T2-weighted, FLAIR, T2*-GRE, or SWI. MRI were
defined as subjects with both pathology-proven CAA (from reviewed blinded to clinical, histopathologic, and genetic data by
routinely collected brain biopsy, biopsy at hematoma evacuation, trained observers, according to Standards for Reporting Vascular
or autopsy) and adequate brain MRI sequences for the study. Data Changes on Neuroimaging (STRIVE).18
search covered patients seen at the hospital between 1997 and The presence and number of CMBs was evaluated on axial
2012. An additional overlapping search through established T2*-GRE or SWI images according to current consensus criteria7
prospective datasets of patients with lobar hemorrhages (ICH or and categorized as lobar (i.e., cortical-subcortical), deep (i.e., basal
CMB) was performed to confirm identification of all potential ganglia [BG], thalami, brainstem), or cerebellar. The presence
eligible cases for the study. Among more than 3,200 retrieved and number of macro ICHs (.5 mm in diameter on T2*-
cases, we initially included those having (1) a pathology report GRE/SWI)19 was also noted.
containing explicit information regarding CAA assessment and (2) CSS was defined as linear residues of chronic blood products in
available brain MRI sequences of adequate quality including T2- the superficial layers of the cerebral cortex showing a characteristic
weighted, T2*-weighted gradient-recalled echo (T2*-GRE), or gyriform pattern of low signal on T2*-GRE/SWI; T1-weighted
susceptibility-weighted imaging (SWI) and fluid-attenuated and FLAIR images were used for anatomical confirmation of the gyral
inversion recovery (FLAIR) sequences. After reviewing all location of these signal hypointensities.20 The distribution and severity
neuroimaging, pathologic, and clinical data available, we excluded of CSS was classified as focal (restricted to #3 sulci) or disseminated
subjects with (1) small brain biopsy samples (greater diameter ($4 sulci).6 Areas of CSS were $2 unaffected sulci away from any
Neurology 84 March 24, 2015 1207
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
lobar ICH, at multiple axial levels; CSS contiguous or potentially p 5 0.336). Although the prevalence of neuritic pla-
anatomically connected with any lobar ICH were not included in ques was similar in the 2 groups, neuritic plaques in
these categories.20
isolation (i.e., with no tangles) were much more fre-
PVS were assessed in line with STRIVE definitions18 and
rated on axial T2-weighted MRI, using a validated 4-point visual
quent in the ICH patients than in the patients with
rating scale in the BG and CSO as previously described.21,22 CAA without ICH (53% vs 13%, p , 0.0001). More
Periventricular and deep WMH were visually assessed on than 90% of pathology samples in both groups had
axial FLAIR images on the 4-point Fazekas rating scale for each, neuritic plaques, whereas NFTs were more commonly
adding up to a total score on a 7-point scale.23 present in the patients without ICH (87% vs 42%, p ,
Statistical analysis. Categorical variables were analyzed using 0.0001). These associations remained consistent in
Pearson x2 or Fisher exact test, and continuous variables by the logistic regression models controlling for age.
2-sample t test (for normal distributions) and Wilcoxon rank sum Comparisons of clinical and imaging character-
(for non-normal distributions). We compared demographic, istics between patients with CAA with vs without
genetic, pathologic, and imaging characteristics of CAA patients
ICH are summarized in table 2. There was a trend
with and without ICH. Variables for APOE e2 and e4 were each
coded as the number of alleles per participant (0, 1, or 2).
for patients with CAA and ICH to more often have
Separate logistic regression models were used to assess the APOE e2 (48.7% vs 21.4%, p 5 0.075), whereas
relationship between APOE genotype and CSS (presence or patients without ICH were more likely to be car-
burden), as well as CMB count (linear regression). As riers of APOE e4 (85.7% vs 53.9%, p 5 0.035).
sensitivity analyses, these models were predetermined to adjust The 2 groups were similar in imaging markers of
for age and clinical presentation of CAA. Significance level was set
cerebral small vessel disease, including WMH bur-
at 0.05. Stata software (version 11.2, StataCorp., College Station,
TX) was used. The manuscript was prepared with reference to the
den, high degree of CSO–enlarged PVS (EPVS)
STROBE guidelines.24 and BG-EPVS, and lobar CMB counts (table 2).
However, the prevalence of CSS was higher in pa-
RESULTS Our final cohort consisted of 105 patients tients with ICH (51.9% vs 19.6%, p 5 0.001),
with pathologic evidence of CAA: 52 from autopsies, especially disseminated CSS (33.3% vs 5.9%,
22 from brain biopsies, and 31 with pathologic sam- p , 0.0001). Representative MRIs are shown in
ples from hematoma evacuations. Fifty-four patients the figure.
were admitted with symptomatic, spontaneous lobar Among subjects with available genetic testing
ICH, while 51 patients were admitted without any (n 5 53), APOE e2 (but not e4) allele was overrepre-
symptomatic ICH. Patients without ICH presented sented in cases with disseminated CSS, in the whole
with cognitive impairment (n 5 42), transient focal cohort (p 5 0.013), and in the CAA subgroup with
neurologic episodes (n 5 3), or a combination of other ICH (table 3). In logistic regression, disseminated CSS
symptoms (n 5 6, including altered mental status, or was associated with APOE e2 (odds ratio [OR] 5.83;
seizures, with findings consistent with inflammatory 95% confidence interval [CI] 1.49–22.82, p 5 0.011).
CAA). The median Clinical Dementia Rating score These results remained consisted and of similar effect
of patients without ICH and available data (n 5 27) size in a sensitivity analysis adjusting for age and clin-
was 1 (interquartile range [IQR] 0.5–2). ical presentation with symptomatic ICH (OR 4.97;
Table 1 indicates the severity of CAA and the pres- 95% CI 1.11–22.21, p 5 0.036) and in models fur-
ence or absence of neuritic plaques and NFTs in the 2 ther adjusting for the presence of vasculopathic
groups. In general, mild (Vonsattel grade 1) or moder- changes on pathology. There was no association
ate to severe (Vonsattel grades 2–4) CAA were equally between CSS (burden or presence) and APOE e4.
represented in the cohorts (p . 0.2 for both compar- There was no association between CMB counts and
isons). There was no difference in the presence of vas- APOE genotype.
culopathic changes (vessel-within-vessel appearance and Follow-up data were available in all patients pre-
vessel wall necrosis) in the 2 groups (29.6% vs 24%, senting without ICH at baseline. During a median
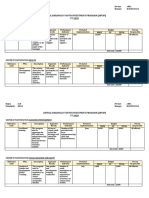
Table 1 Cerebral amyloid angiopathy with and without intracerebral hemorrhage: Severity and associations with neuritic plaques and
tanglesa
CAA severity (Vonsattel
grade)
Grade 1 Grade 2–4 Vasculopathic changes NP alone NT alone NP and NT No NP or NT
CAA with ICH, n (%) 7 (13) 47 (87) 16 (29.6) 19 (52.8) 0 15 (41.7) 3 (5.6)
CAA without ICH, n (%) 11 (21.6) 40 (78.4) 12 (24) 6 (13) 1 (2.2) 39 (84.8) 0
Abbreviations: CAA 5 cerebral amyloid angiopathy; ICH 5 intracerebral hemorrhage; NP 5 neuritic plaques; NT 5 neuritic tangles.
a
Data on neuritic plaques and tangles were available in 36/54 patients with ICH and 46/51 patients without ICH.
1208 Neurology 84 March 24, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Table 2 Comparison of clinical, imaging, and genetic characteristics between pathologically proven CAA with vs without ICH cohorts
Whole CAA cohort (n 5 105) CAA with ICH (n 5 54) CAA without ICH (n 5 51) p Value
Age, y, mean (95% CI) 72.7 (71.1–74.2) 71.6 (69.4–73.7) 73.9 (71.5–76.2) 0.148
Female, n (%) 55 (52.4) 33 (63.1) 22 (43.1) 0.065
Hypertension, n (%) 66 (64.7) 30 (57.8) 36 (72) 0.131
Antithrombotic drug use, n (%) 40 (44.4) 15 (36.6) 25 (51) 0.170
a
APOE e2, n (%) 22 (41.5) 19 (48.7) 3 (21.4) 0.075
a
APOE e4, n (%) 33 (62.3) 21 (53.9) 12 (85.7) 0.035
Time from MRI to pathology, mo, median (IQR) 5.3 (0.3–31.4) 1.3 (0.2–11) 23.3 (1.4–50.7) 0.0002
Severe (Fazekas 5–6) WMH, n (%) 21 (20) 13 (24.1) 8 (15.7) 0.283
High-grade CSO-EPVS (>20), n (%) 57 (54.8) 29 (54.7) 28 (54.9) 0.985
High-grade BG-EPVS (>20), n (%) 25 (24) 11 (20.8) 14 (27.5) 0.424
Lobar CMB presence, n (%) 63 (60) 36 (66.7) 27 (52.9) 0.151
Lobar CMB count, median (IQR) 2 (0–27) 3 (0–23) 2 (0–31) 0.411
Presence of CSS, n (%) 38 (39.2) 28 (51.9) 10 (19.6) 0.001
Focal CSS, n (%) 17 (16.2) 10 (18.5) 7 (13.7) 0.505
Disseminated CSS, n (%) 21 (20) 18 (33.3) 3 (5.9) ,0.0001
Abbreviations: BG 5 basal ganglia; CAA 5 cerebral amyloid angiopathy; CI 5 confidence interval; CMB 5 cerebral microbleed; CSO 5 centrum semiovale;
CSS 5 cortical superficial siderosis; EPVS 5 enlarged perivascular spaces; ICH 5 intracerebral hemorrhage; IQR 5 interquartile range; WMH 5 white
matter hyperintensities.
a
APOE genotype was available in 53 CAA patients: 39 with ICH and 14 without ICH.
follow-up time of 3 years (IQR 1.1–5.6 years), 2 of of CAA with symptomatic ICH in our study had a
51 patients (3.9%, 95% CI 0.5–13.5%) experienced fairly similar vascular amyloid burden and preva-
a symptomatic lobar ICH. One of these 2 patients lence of CAA-associated vasculopathic changes com-
had focal CSS at baseline MRI. pared to cases without ICH, although this could
have been influenced by sampling bias. In addition,
DISCUSSION The major findings from this study the 2 groups had a similar profile of putative neuro-
show that patients with CAA presenting with ICH imaging biomarkers of CAA severity, including lobar
are more likely to have CSS (particularly dissemi- CMBs, WMH, and CSO-EPVS. It thus seems likely
nated) and the APOE e2 genotype compared to that additional biological pathways from those
CAA patients presenting without ICH. By contrast, involved in amyloid-b accumulation in cortical
APOE e4 is enriched in nonhemorrhagic CAA. In and leptomeningeal vessels play a role in determin-
addition, there was an overall higher burden of ing clinical expression.
NFT pathology in the non-hemorrhagic CAA The most distinctive neuroimaging feature
group. APOE genotype might partly influence these between the 2 groups was the much higher prevalence
relationships: APOE e2 was found to be associated of disseminated CSS in patients with CAA and ICH.
with both symptomatic ICH clinical phenotype and The prevalence of CSS in our histopathology-
disseminated CSS. confirmed CAA-ICH group is in line with the re-
Our results provide new insights into the clinical ported prevalence in a previous imaging study of
and imaging spectrum of sporadic CAA, pointing to CAA-ICH.20 In addition, the presence of CSS in
different disease phenotypes.14 While sporadic CAA the group without ICH (10%) is more in line with
is commonly found in the elderly, it is currently recent imaging studies evaluating CSS in a memory
unknown why only a fraction of people with CAA clinic setting and AD.25
pathology develop symptomatic disease, and why Although the pathophysiologic mechanisms
some present with symptomatic ICH, while others underlying CSS in CAA are not yet fully understood,
only develop cognitive impairment or other clinical observational data suggest that CSS represents blood
symptoms. A previous comparative postmortem his- residues related to blood leaking episodes into the
topathologic study found that the brain features subarachnoid space from CAA-affected vessels.6,20,26
from patients with CAA that are most consistently A secondary mechanism due to leakage or expansion
related to ICH are severe degree of vascular amyloid of a lobar ICH into the subarachnoid space cannot be
deposition and the presence of fibrinoid necrosis fully excluded; however, similar to other studies, CSS
(with or without microaneurysms).16 However, cases was mostly found distant from any ICH (and often in
Neurology 84 March 24, 2015 1209
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Figure Representative MRIs of patients with pathologic evidence of cerebral amyloid angiopathy with and without symptomatic intracerebral
hemorrhage
(A) A 73-year-old woman with cerebral amyloid angiopathy (CAA)–intracerebral hemorrhage (ICH) and disseminated cortical superficial siderosis on T2*-
weighted gradient-recalled echo (T2*-GRE) (left). Her APOE genotype was e2/e4. (B) Multiple strictly lobar cerebral microbleeds (but no siderosis) on T2*-
GRE MRI (left) in a 73-year-old woman with cognitive impairment and e4/e4 APOE genotype. Note the comparable white matter hyperintensities burden on
fluid-attenuated inversion recovery MRI (middle panels) and centrum semiovale perivascular spaces on T2-weighted images (right panels) in the 2 patients.
Both cases had severe CAA with vasculopathic changes (vessel-within-vessel appearance) on pathology.
the opposite hemisphere), and was also detected even in 24 patients (47.1%).8 A European multicenter
in cases without any ICH. Two recent studies have study of patients with probable or possible CAA
identified CSS as a particular risk factor for subse- (n 5 118) found that CSS was a significant predictor
quent ICH in CAA.8,9 In a cohort of 51 patients with of time until ICH.9 The ICH risk at 4 years was
CAA-related CSS and a median follow-up of 35.3 28.9% (95% CI 7.7–76.7%) and 74% (95% CI
months, new intracranial hemorrhages were observed 44.1–95.7) for patients with focal and disseminated
CSS, respectively, compared to 25% (95% CI 7.6–
28.3%) for patients without siderosis (log-rank test:
Table 3 APOE allele prevalences according to cortical superficial siderosis
p 5 0.0031).9 A small autopsy series of 6 CAA cases
burden in patients with cerebral amyloid angiopathy with or without
intracerebral hemorrhage showed that multiple leptomeningeal arteries (and
not parenchymal cortical vessels) can rupture into
CSS burden the subarachnoid space and the brain parenchyma,
No CSS Focal CSS Disseminated CSS
leading to large lobar hemorrhages.27,28 These obser-
vations might explain the relationship between dis-
Whole CAA cohort, n (%)
seminated CSS and CAA with ICH, as well as why
APOE e2 7 (29.2) 3 (25) 12 (70.6)
patients with disseminated CSS have the highest risk
APOE e4 18 (75) 6 (50) 9 (52.9) of future ICH.9
CAA with ICH, n (%) Our study demonstrates that there might be
APOE e2 7 (46.7) 1 (11.1) 11 (73.3) APOE genotype-specific effects on the imaging and
APOE e4 9 (60) 4 (44.4) 8 (53.3)
clinical expression of CAA-related disease. While
APOE e4 seems to be more associated with CAA
CAA without ICH, n (%)
without ICH, APOE e2 is linked more strongly with
APOE e2 0 (0) 2 (66.7) 1 (50)
bleeding and CSS. The APOE e2 allele is reported to
APOE e4 9 (100) 2 (66.7) 1 (50) be associated with CAA-related lobar ICH, possibly
Abbreviations: CAA 5 cerebral amyloid angiopathy; CSS 5 cortical superficial siderosis; due to the disease-related vasculopathic changes seen
ICH 5 intracerebral hemorrhage. with this allele,13,29 and recently with CSS in a cohort
1210 Neurology 84 March 24, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
of CAA defined by clinicoradiographic criteria.30 unavailability of APOE genotype data in all patients.
APOE e4 (presence and number) is also associated The differences in Alzheimer pathology between
with sporadic CAA and ICH risk.31–33 Our study groups could potentially be explained by a longer
raised the interesting possibility that APOE e2 influ- duration of disease (taking time from MRI to
ences pathways causing both CSS and ICH. After pathology as a surrogate for disease duration) in pa-
accounting for the presence of vasculopathic changes, tients with CAA without ICH or the different char-
the apparent relation of APOE e2 to CSS was not acteristics between the 2 groups (including APOE e4
reduced, suggesting that vascular amyloid load and prevalence). Molecular imaging studies assessing
how extensively the vessel wall architecture is disrup- amyloid and tau burden in vivo38 may help resolve
ted is not the sole driving force underlying these path- this question. Furthermore, the degree and evolu-
ways and hence, clinical phenotypes. However, any tion of cognitive impairment in patients with CAA
mechanistic links are clearly complex and need to be without ICH (data limited in our study) could influ-
treated with caution, as APOE genotype alone might ence pathologic findings, especially NFTs and amy-
not be necessary or sufficient to drive these effects. It loid plaques presence. Finally, the cross-sectional
is important to note that links may differ according to design of the current study did not allow us to assess
the presence or absence of AD pathology, particularly potential causality of the reported associations.
for APOE e2, which has been associated with a Results from this neuropathologic-defined cohort
reduced risk of late-onset Alzheimer dementia.31 This of patients with CAA with and without ICH provide
observation is in line with the differential associations evidence for distinct disease phenotypes, and suggest
between neuritic plaques and NFTs in our patients that CSS and APOE e2 are related to the hemorrhagic
with CAA with and without ICH. There is significant expression of the disease. Our study emphasizes the
variation in the pathologic appearance of CAA and its widening spectrum of CAA, with clinical phenotypes
influence on AD pathology,34,35 further highlighting reflecting different neuroimaging and genetic fea-
the concept of different phenotypes of CAA. It is tures, and suggests divergent pathophysiologic mech-
important to acknowledge though that the overrepre- anisms. Although these findings require external
sentation of NFTs among the patients with CAA validation in larger CAA cohorts, they may be rele-
without ICH might also reflect a bias issue, since vant for future biomarker studies and disease-
by definition these cases presented with cognitive modifying CAA trials.
impairment, partly driven by NFT pathology.
Although the natural history of patients with AUTHOR CONTRIBUTIONS
symptomatic CAA mainly presenting with cognitive A. Charidimou: project concept and design, imaging and data analysis,
write up. S. Martinez-Ramirez: data collection, imaging analysis, critical
impairment (i.e., without ICH at baseline) has not revisions. A. Shoamanesh: critical revisions. J. Oliveira-Filho: data collec-
been fully investigated, our data suggest that this tion, critical revisions. M. Frosch: data collection, critical revisions. Anas-
CAA phenotype may have a lower risk of developing tasia Vashkevich: data collection and management. Alison Ayres: data
collection and management. J. Rosand: funding, data collection, critical
ICH compared to CAA cases with a history of ICH.
revisions. Mahmut Edip Gurol: data collection. Steven M. Greenberg:
It is important to note that patients with CAA with- funding, data collection, critical revisions. A. Viswanathan: project con-
out major ICH (microbleeds or CSS-only CAA) pre- cept and design, write up, critical revisions.
senting to stroke services with symptoms other than
cognitive impairment (e.g., transient focal neurologic ACKNOWLEDGMENT
episodes) might still be at significant risk of future The authors thank Dr. David J. Werring, Prof. Martin Brown, and the Bogue
Research Fellowships (UCL) for supporting Dr. Andreas Charidimou’s visiting
bleeding.9,36,37 This topic requires further investiga- fellowship at the Hemorrhagic Stroke Research Program, Harvard Medical
tion in prospective studies. School, Boston, MA.
Major strengths of the study include the large
sample of patients with histopathologically con- STUDY FUNDING
firmed CAA and available MRI sequences, the sys- Supported by NIH grants K23AG028726-05, P50AG005134-30,
2R01AG26484, 5R01AG026484-10, and 5K23AG028726-05.
tematic evaluation of MRI scans for a range of
neuroimaging biomarkers of small vessel disease, DISCLOSURE
and the testing of a prespecified hypothesis. The The authors report no disclosures relevant to the manuscript. Go to
main limitations, inherent to any clinical- Neurology.org for full disclosures.
pathology series in CAA, include (1) the difference
in pathology sampling between autopsied brains Received July 30, 2014. Accepted in final form November 12, 2014.
and biopsies/hematomas; (2) the biases regarding
REFERENCES
which patients get biopsied or autopsied, which
1. Charidimou A, Gang Q, Werring DJ. Sporadic cerebral
might be skewed towards end stage or advanced dis- amyloid angiopathy revisited: recent insights into patho-
ease; and (3) potential selection bias due to the physiology and clinical spectrum. J Neurol Neurosurg Psy-
requirement for both pathology and MRI and the chiatry 2012;83:124–137.
Neurology 84 March 24, 2015 1211
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
2. Viswanathan A, Greenberg SM. Cerebral amyloid angiop- 21. Charidimou A, Jaunmuktane Z, Baron JC, et al. White mat-
athy in the elderly. Ann Neurol 2011;70:871–880. ter perivascular spaces: an MRI marker in pathology-proven
3. Vinters HV. Cerebral amyloid angiopathy: a critical cerebral amyloid angiopathy? Neurology 2014;82:57–62.
review. Stroke 1987;18:311–324. 22. Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS,
4. Greenberg SM, Vonsattel JP, Stakes JW, Gruber M, Wardlaw JM. Enlarged perivascular spaces on MRI are a fea-
Finklestein SP. The clinical spectrum of cerebral amyloid ture of cerebral small vessel disease. Stroke 2010;41:450–454.
angiopathy: presentations without lobar hemorrhage. 23. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA.
Neurology 1993;43:2073–2079. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and
5. Ellis RJ, Olichney JM, Thal LJ, et al. Cerebral amyloid normal aging. AJR Am J Roentgenol 1987;149:351–356.
angiopathy in the brains of patients with Alzheimer’s dis- 24. von Elm E, Altman DG, Egger M, Pocock SJ,
ease: the CERAD experience, part XV. Neurology 1996; Gotzsche PC, Vandenbroucke JP. The Strengthening the
46:1592–1596. Reporting of Observational Studies in Epidemiology
6. Linn J, Halpin A, Demaerel P, et al. Prevalence of super- (STROBE) statement: guidelines for reporting observa-
ficial siderosis in patients with cerebral amyloid angiopa- tional studies. Lancet 2007;370:1453–1457.
thy. Neurology 2010;74:1346–1350. 25. Zonneveld HI, Goos JD, Wattjes MP, et al. Prevalence of
7. Greenberg SM, Vernooij MW, Cordonnier C, et al. Cere- cortical superficial siderosis in a memory clinic population.
bral microbleeds: a guide to detection and interpretation. Neurology 2014;82:698–704.
Lancet Neurol 2009;8:165–174. 26. Linn J, Herms J, Dichgans M, et al. Subarachnoid hemosid-
8. Linn J, Wollenweber FA, Lummel N, et al. Superficial erosis and superficial cortical hemosiderosis in cerebral amy-
siderosis is a warning sign for future intracranial hemor- loid angiopathy. AJNR Am J Neuroradiol 2008;29:184–186.
rhage. J Neurol 2013;260:176–181. 27. Takeda S, Yamazaki K, Miyakawa T, et al. Subcortical
9. Charidimou A, Peeters AP, Jager R, et al. Cortical super- hematoma caused by cerebral amyloid angiopathy: does
ficial siderosis and intracerebral hemorrhage risk in cerebral the first evidence of hemorrhage occur in the subarachnoid
amyloid angiopathy. Neurology 2013;81:1666–1673. space? Neuropathology 2003;23:254–261.
10. Greenberg SM, Rebeck GW, Vonsattel JP, Gomez-Isla T, 28. Takeda S, Hinokuma K, Yamazaki K, et al. The hemor-
Hyman BT. Apolipoprotein E epsilon 4 and cerebral hem- rhage caused by sporadic-type cerebral amyloid angiopathy
orrhage associated with amyloid angiopathy. Ann Neurol occurs primarily in the cerebral sulci. Neuropathology
1995;38:254–259. 2012;32:38–43.
11. Greenberg SM, Briggs ME, Hyman BT, et al. Apolipo- 29. Nicoll JA, Burnett C, Love S, et al. High frequency of
protein E epsilon 4 is associated with the presence and apolipoprotein E epsilon 2 allele in hemorrhage due to cere-
earlier onset of hemorrhage in cerebral amyloid angiopa- bral amyloid angiopathy. Ann Neurol 1997;41:716–721.
thy. Stroke 1996;27:1333–1337. 30. Shoamanesh A, Martinez-Ramirez S, Oliveira-Filho J,
12. Rannikmae K, Samarasekera N, Martinez-Gonzalez NA, et al. Interrelationship of superficial siderosis and micro-
Al-Shahi Salman R, Sudlow CL. Genetics of cerebral amy- bleeds in cerebral amyloid angiopathy. Neurology 2014;
loid angiopathy: systematic review and meta-analysis. 83:1838–1843.
J Neurol Neurosurg Psychiatry 2013;84:901–908. 31. Verghese PB, Castellano JM, Holtzman DM. Apolipopro-
13. Greenberg SM, Vonsattel JP, Segal AZ, et al. Association tein E in Alzheimer’s disease and other neurological dis-
of apolipoprotein E epsilon2 and vasculopathy in cerebral orders. Lancet Neurol 2011;10:241–252.
amyloid angiopathy. Neurology 1998;50:961–965. 32. Alonzo NC, Hyman BT, Rebeck GW, Greenberg SM.
14. Charidimou A, Jager HR. Developing biomarkers for Progression of cerebral amyloid angiopathy: accumulation
cerebral amyloid angiopathy trials: do potential disease of amyloid-beta40 in affected vessels. J Neuropathol Exp
phenotypes hold promise? Lancet Neurol 2014;13: Neurol 1998;57:353–359.
538–540. 33. Rannikmae K, Kalaria RN, Greenberg SM, et al. APOE
15. Brouwers HB, Biffi A, McNamara KA, et al. Apolipopro- associations with severe CAA-associated vasculopathic
tein E genotype is associated with CT angiography spot changes: collaborative meta-analysis. J Neurol Neurosurg
sign in lobar intracerebral hemorrhage. Stroke 2012;43: Psychiatry 2014;85:300–305.
2120–2125. 34. Allen N, Robinson AC, Snowden J, Davidson YS,
16. Vonsattel JP, Myers RH, Hedley-Whyte ET, Ropper AH, Mann DM. Patterns of cerebral amyloid angiopathy define
Bird ED, Richardson EP Jr. Cerebral amyloid angiopathy histopathological phenotypes in Alzheimer’s disease. Neu-
without and with cerebral hemorrhages: a comparative his- ropathol Appl Neurobiol 2014;40:136–148.
tological study. Ann Neurol 1991;30:637–649. 35. Attems J, Jellinger KA, Lintner F. Alzheimer’s disease
17. Greenberg SM, Vonsattel JP. Diagnosis of cerebral amy- pathology influences severity and topographical distribu-
loid angiopathy: sensitivity and specificity of cortical tion of cerebral amyloid angiopathy. Acta Neuropathol
biopsy. Stroke 1997;28:1418–1422. 2005;110:222–231.
18. Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging 36. Charidimou A, Peeters A, Fox Z, et al. Spectrum of tran-
standards for research into small vessel disease and its con- sient focal neurological episodes in cerebral amyloid angi-
tribution to ageing and neurodegeneration. Lancet Neurol opathy: multicentre magnetic resonance imaging cohort
2013;12:822–838. study and meta-analysis. Stroke 2012;43:2324–2330.
19. Kidwell CS, Greenberg SM. Red meets white: do micro- 37. van Etten ES, Auriel E, Haley KE, et al. Incidence of
bleeds link hemorrhagic and ischemic cerebrovascular dis- symptomatic hemorrhage in patients with lobar micro-
ease? Neurology 2009;73:1614–1615. bleeds. Stroke 2014;45:2280–2285.
20. Charidimou A, Jager RH, Fox Z, et al. Prevalence and 38. Xia CF, Arteaga J, Chen G, et al. [(18)F]T807, a novel tau
mechanisms of cortical superficial siderosis in cerebral positron emission tomography imaging agent for Alz-
amyloid angiopathy. Neurology 2013;81:626–632. heimer’s disease. Alzheimers Dement 2013;9:666–676.
1212 Neurology 84 March 24, 2015
ª 2015 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Segmconference2023 10-3-23 Ip-SpeakersDocument9 pagesSegmconference2023 10-3-23 Ip-Speakersapi-698589423No ratings yet
- Alarm Fatigue: Use of An Evidence-Based Alarm Management StrategyDocument8 pagesAlarm Fatigue: Use of An Evidence-Based Alarm Management StrategyMister BigglesworthNo ratings yet
- Caltech Coursera - Drugs&Brain - Report - Posting 8 Feb 2013Document12 pagesCaltech Coursera - Drugs&Brain - Report - Posting 8 Feb 2013Parker333No ratings yet
- Time - The Science of Weight Loss - 2019 PDFDocument99 pagesTime - The Science of Weight Loss - 2019 PDFSigitWibowo100% (5)
- Cerebral Amyloid Angiopathy A Systematic Review 2011Document9 pagesCerebral Amyloid Angiopathy A Systematic Review 2011Jaime Arevalo PanduroNo ratings yet
- What Research Shows: NARTH's Response To The APA Claims On HomosexualityDocument4 pagesWhat Research Shows: NARTH's Response To The APA Claims On Homosexualitybmx0No ratings yet
- Maruna and Mann 2006Document23 pagesMaruna and Mann 2006stephanieNo ratings yet
- Laura StephenDocument23 pagesLaura Stephenpepebyluis100% (1)
- Cerebral Amyloid AngiopathyDocument2 pagesCerebral Amyloid AngiopathyPaolo Giordano100% (1)
- A Meta-Analysis of Pornography Consumption and Actual Acts of Sexual Aggression in General Population StudiesDocument23 pagesA Meta-Analysis of Pornography Consumption and Actual Acts of Sexual Aggression in General Population Studiesaroa100% (1)
- Cardiac Amyloidosis: Name: Salam Majzoub Preceptor: Dr. Lama FaddoulDocument47 pagesCardiac Amyloidosis: Name: Salam Majzoub Preceptor: Dr. Lama Faddoulsalam majzoubNo ratings yet
- Colizzi Et Al., 2015 - Psychiatry - ResDocument8 pagesColizzi Et Al., 2015 - Psychiatry - ResdojabrNo ratings yet
- Peds 2013-2958Document11 pagesPeds 2013-2958Sean SubtesteNo ratings yet
- Pornography and Sexual Deviance: A Report of the Legal and Behavioral Institute, Beverly Hills, CaliforniaFrom EverandPornography and Sexual Deviance: A Report of the Legal and Behavioral Institute, Beverly Hills, CaliforniaNo ratings yet
- The Impact of Shock Wave Therapy at VariDocument9 pagesThe Impact of Shock Wave Therapy at VariArifSurtonoNo ratings yet
- 2020 - Slavin Et Al. Child Sexual Abuse and Compulsive Sexual Behavior - A Systematic Literature ReviewDocument21 pages2020 - Slavin Et Al. Child Sexual Abuse and Compulsive Sexual Behavior - A Systematic Literature ReviewAnapsi02100% (1)
- Bad Guidelines Management of Adults With Delusional InfestationDocument18 pagesBad Guidelines Management of Adults With Delusional InfestationRBGBGB RBGNo ratings yet
- Pubertal Suppression For Transgender Youth0897877001603408698Document15 pagesPubertal Suppression For Transgender Youth0897877001603408698Antorcha CANo ratings yet
- Exposing The Myth ofDocument7 pagesExposing The Myth ofnowayborngay0% (1)
- Tau Opa ThiesDocument22 pagesTau Opa ThiesIrina OdajiuNo ratings yet
- Homosexuality and The Scientific Evidence PDFDocument274 pagesHomosexuality and The Scientific Evidence PDFanon_113431634No ratings yet
- Alzheimers-Disease-Genetics-Fact-Sheet 0Document8 pagesAlzheimers-Disease-Genetics-Fact-Sheet 0api-285676076No ratings yet
- Imploding Gay Power: by Philip IrvinDocument4 pagesImploding Gay Power: by Philip IrvinnowayborngayNo ratings yet
- Fence Sitters: Parents' reactions to sexual ambiguities in their newborn children - מתוך מאמרה של מאירה וייסDocument18 pagesFence Sitters: Parents' reactions to sexual ambiguities in their newborn children - מתוך מאמרה של מאירה וייספרופסור מאירה וייסNo ratings yet
- Methylphenidate Side Effect Profile Is Influenced by Genetic Variation in The Attention-Deficit/Hyperactivity Disorder-Associated CES1 GeneDocument10 pagesMethylphenidate Side Effect Profile Is Influenced by Genetic Variation in The Attention-Deficit/Hyperactivity Disorder-Associated CES1 GeneMerari Lugo Ocaña100% (1)
- Am I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlDocument9 pagesAm I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlBlack HoleNo ratings yet
- Clinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956Document14 pagesClinical Significance of A Proposed Developmental Trauma Disorder Diagnosis - Results of An International Survey of Clinicians - 2020 11 09 232956abelim01100% (1)
- Debate On HomosexualsDocument2 pagesDebate On HomosexualsLiQinghuaNo ratings yet
- Polls On Attitudes On Homosexuality & Gay MarriageDocument88 pagesPolls On Attitudes On Homosexuality & Gay MarriageAmerican Enterprise InstituteNo ratings yet
- PEP Web - Stoller A Contribution To The Study of Gender IdentityDocument5 pagesPEP Web - Stoller A Contribution To The Study of Gender IdentityRamon Ferreira100% (1)
- PSYC-The Psychopathology of Everyday Life-Argumentative EssayDocument11 pagesPSYC-The Psychopathology of Everyday Life-Argumentative EssayHarrison MolloyNo ratings yet
- Discussing Potentials in Dimensional and Clinical Staging Models of Schizophrenia Diagnosis and How They Relate To The Problem of StigmaDocument14 pagesDiscussing Potentials in Dimensional and Clinical Staging Models of Schizophrenia Diagnosis and How They Relate To The Problem of StigmaGeorgeBaker100% (1)
- Gilman, Ken, Kenneth, Peter - Advances Pertaining To The Pharmacology and Interactions of Irreversible Nonselective Monoamine Oxidase InhibitorsDocument9 pagesGilman, Ken, Kenneth, Peter - Advances Pertaining To The Pharmacology and Interactions of Irreversible Nonselective Monoamine Oxidase Inhibitors朗博Cuauhtlatoa100% (1)
- Trans Pulse 2011Document3 pagesTrans Pulse 2011Daily XtraNo ratings yet
- Manual For Early Infant Male Circumcision Under Local AnaesthesiaDocument140 pagesManual For Early Infant Male Circumcision Under Local AnaesthesiaSabbir AhmedNo ratings yet
- Aust N Z J Psychiatry 2014 Gitlin 89 90Document3 pagesAust N Z J Psychiatry 2014 Gitlin 89 90KThreopusNo ratings yet
- Conversion Therapy: Consensus StatementDocument3 pagesConversion Therapy: Consensus StatementAlexandria Firdaus Al-farisyNo ratings yet
- Andropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneDocument14 pagesAndropause: Current Concepts: Keywords: Androgen Deficiency in Ageing Male, Late Onset Hypogonadism, TestosteroneYariCárdenasNo ratings yet
- Overview of Igg4 - Related Disease: Introduction - History, Definition, and Diagnostic CriteriaDocument6 pagesOverview of Igg4 - Related Disease: Introduction - History, Definition, and Diagnostic CriteriaStefan PopoviciNo ratings yet
- Victor Cline's Study PDFDocument22 pagesVictor Cline's Study PDFsolay12No ratings yet
- Vasculitis: VASCULITIS Is A Primary Inflammatory Disease Process of The VasculatureDocument43 pagesVasculitis: VASCULITIS Is A Primary Inflammatory Disease Process of The VasculaturelihayatiNo ratings yet
- Detransition Related Needs and Support A Cross Sectional Online SurveyDocument20 pagesDetransition Related Needs and Support A Cross Sectional Online SurveyZara LauraNo ratings yet
- Affidavit of Michelle CretellaDocument12 pagesAffidavit of Michelle CretellaDavid Hart0% (1)
- What Does It Mean To Be A Woman Research Paper 3Document16 pagesWhat Does It Mean To Be A Woman Research Paper 3api-608687083100% (1)
- Resource - Bad Actors in Conversion Therapy PDFDocument5 pagesResource - Bad Actors in Conversion Therapy PDFBrianna JanuaryNo ratings yet
- Treatment of Hypoglycemia in ChildrenDocument16 pagesTreatment of Hypoglycemia in ChildrenKamuiShirouNo ratings yet
- ALZHEIMER'S DISEASE - Colour & MagnetoDocument11 pagesALZHEIMER'S DISEASE - Colour & MagnetoDr Vaishali MathapatiNo ratings yet
- PDF - Why Dont We Prescribe MAOIsDocument11 pagesPDF - Why Dont We Prescribe MAOIsSarwar Baig100% (1)
- Vasculitic NeuropathiesDocument20 pagesVasculitic NeuropathiesHITIPHYSIONo ratings yet
- Background: Alpha ThalassemiaDocument24 pagesBackground: Alpha ThalassemiacristieristiieNo ratings yet
- Adolescent Sexuaiity: Judith Marks Mishne D.S.WDocument2 pagesAdolescent Sexuaiity: Judith Marks Mishne D.S.WRAHMANo ratings yet
- Update On The Efficacy of Pharmacotherapy For Social Anxiety Disorder: A Meta-AnalysisDocument12 pagesUpdate On The Efficacy of Pharmacotherapy For Social Anxiety Disorder: A Meta-AnalysisAnaaaerobios100% (1)
- Bilateral Thalamic LesionsDocument10 pagesBilateral Thalamic LesionsOralBoardsNo ratings yet
- Gay Affirmative Therapy PerlmanDocument11 pagesGay Affirmative Therapy PerlmanPsico Orientador100% (1)
- Management of IncontinenceDocument91 pagesManagement of IncontinenceVahid Msmi100% (1)
- Negative Symptoms in SchizophreniaDocument15 pagesNegative Symptoms in Schizophreniasyahrizon thomasNo ratings yet
- Sexual and Gender Identity DisordersDocument5 pagesSexual and Gender Identity DisordersKiana TehraniNo ratings yet
- Familial Non-Medullary Thyroid CancerDocument19 pagesFamilial Non-Medullary Thyroid CancerMikeyNo ratings yet
- Should Homosexuality Be LegalizedDocument4 pagesShould Homosexuality Be LegalizedSamamaSuhailNo ratings yet
- Males and Eating Disorders: William HarrymanDocument14 pagesMales and Eating Disorders: William HarrymanWilliam HarrymanNo ratings yet
- The Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis ResearchDocument29 pagesThe Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis Researchapi-246003035No ratings yet
- Angiopathy StrokeDocument7 pagesAngiopathy Strokearia tristayanthiNo ratings yet
- Noc110069 346 351Document6 pagesNoc110069 346 351Carlos AlvaradoNo ratings yet
- Main PDFDocument9 pagesMain PDFAmalia Gh,No ratings yet
- RCT Simvastatin AlzheimerDocument8 pagesRCT Simvastatin AlzheimerGabriel Septiana CitraNo ratings yet
- D Dimer Level in COVID 19 Infection A Systematic ReviewDocument12 pagesD Dimer Level in COVID 19 Infection A Systematic ReviewGabriel Septiana CitraNo ratings yet
- Abcde2 TiaDocument7 pagesAbcde2 TiaGabriel Septiana CitraNo ratings yet
- Surveillance IchDocument6 pagesSurveillance IchGabriel Septiana CitraNo ratings yet
- 2001 Prevalence of and Risk Factors For Carpal Tunnel Syndrome in A Rural PopulationDocument9 pages2001 Prevalence of and Risk Factors For Carpal Tunnel Syndrome in A Rural PopulationGabriel Septiana CitraNo ratings yet
- Company Profile: Sistema Inteligente de Color, Descubrir Tu Valor ExcepcionalDocument4 pagesCompany Profile: Sistema Inteligente de Color, Descubrir Tu Valor ExcepcionalOmar Stalin Lucio RonNo ratings yet
- Original Article /artículo Original: Muhlenbergia Angustata (Poaceae), Puno, PerúDocument10 pagesOriginal Article /artículo Original: Muhlenbergia Angustata (Poaceae), Puno, PerúBet MACNo ratings yet
- Adverse Childhood ExperiencesDocument8 pagesAdverse Childhood ExperiencesMa. Alicia Jimenez MartinezNo ratings yet
- AAO 2015 Atropine For Myopia DR Donald Tan 11-16-15 RedactedDocument15 pagesAAO 2015 Atropine For Myopia DR Donald Tan 11-16-15 RedactedunonounoNo ratings yet
- Final Year MBBS Video Lectures Links (Version - 1)Document7 pagesFinal Year MBBS Video Lectures Links (Version - 1)noorNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
- Evidence Based Validation of Traditional Medicines 2021Document1,135 pagesEvidence Based Validation of Traditional Medicines 2021shubham panditNo ratings yet
- Solitaire FR BrochureDocument2 pagesSolitaire FR Brochuredsk778894No ratings yet
- Motivation Dabur IndiaDocument84 pagesMotivation Dabur IndiaGuman SinghNo ratings yet
- HeadacheDocument22 pagesHeadacheAlma SunagawaNo ratings yet
- PHIN Laboratory Result ELR v231Document86 pagesPHIN Laboratory Result ELR v231anujaks_rlbNo ratings yet
- Community Medicine (PSM)Document7 pagesCommunity Medicine (PSM)Shashwathi MNo ratings yet
- Month 12 ProgressionDocument11 pagesMonth 12 Progressiongreg hofmanNo ratings yet
- Universal Crescent Power P LTD EIA Report Part IDocument66 pagesUniversal Crescent Power P LTD EIA Report Part ImanishxlriNo ratings yet
- - 113後中醫第2次模考試題及解答 頁面 3Document12 pages- 113後中醫第2次模考試題及解答 頁面 3liu634paulNo ratings yet
- CR Piopneumothoraks Nicky FIXdDocument62 pagesCR Piopneumothoraks Nicky FIXdPutri RahmawatiNo ratings yet
- Handbook Technology TransferDocument15 pagesHandbook Technology Transferzakarya wadiNo ratings yet
- SCIENCE-DRRR - Q1 - W5 - Mod2-Hazard-Its-Impact-Identification-and-Risk-Assessment-08082020Document27 pagesSCIENCE-DRRR - Q1 - W5 - Mod2-Hazard-Its-Impact-Identification-and-Risk-Assessment-08082020Stephanie PacquiaoNo ratings yet
- ABYIPDocument5 pagesABYIPJayson Guerrero100% (4)
- EczemaDocument1 pageEczemaKaniz WahabNo ratings yet
- FITT 1 Updated HandoutsDocument25 pagesFITT 1 Updated HandoutsJolina VillalobosNo ratings yet
- Chlorhexidine Gluconate 0.2% W/V Mouth Wash: Class: IndicationsDocument3 pagesChlorhexidine Gluconate 0.2% W/V Mouth Wash: Class: IndicationsAnonymous Bt6favSF4YNo ratings yet
- Lipoma ExcisionDocument4 pagesLipoma ExcisionNikolaus TalloNo ratings yet
- 10 STD Science BookDocument338 pages10 STD Science BookmkprabhuNo ratings yet
- IHDW GuidelinesDocument32 pagesIHDW GuidelinesCezara ZahariaNo ratings yet
- Cardiovascular Disease AssignmentDocument3 pagesCardiovascular Disease Assignmentapi-308874632No ratings yet