Professional Documents
Culture Documents
Balantidum Coli: EBON, SISON - 2017
Balantidum Coli: EBON, SISON - 2017
Uploaded by
Abcd ReyesCopyright:
Available Formats
You might also like
- Test Bank For Anatomy and Physiology: An Integrative Approach 3Rd Edition, by Mckinley DR., Michael, Valerie Oâ ™loughlin, Theresa BidleDocument36 pagesTest Bank For Anatomy and Physiology: An Integrative Approach 3Rd Edition, by Mckinley DR., Michael, Valerie Oâ ™loughlin, Theresa Bidlesublunardisbench.2jz85100% (23)
- Balantidium Coli: Disease, Epidemiology and Laboratory DiagnosisDocument38 pagesBalantidium Coli: Disease, Epidemiology and Laboratory DiagnosisSanty PatNo ratings yet
- Medical Biology 3 - BR - 2020Document70 pagesMedical Biology 3 - BR - 2020Yusuf Yağız TimurNo ratings yet
- 1.3 Hemoflagellates and Ciliates (Limpin)Document4 pages1.3 Hemoflagellates and Ciliates (Limpin)arvinkennethdelacruzNo ratings yet
- (PARA) 1.5 - Blood and Tissue FlagellatesDocument6 pages(PARA) 1.5 - Blood and Tissue FlagellatesGuia De GuzmanNo ratings yet
- Parasitology-Lec 5 TrematodesDocument5 pagesParasitology-Lec 5 Trematodesapi-3743217100% (2)
- AmebaDocument53 pagesAmebaapi-19916399No ratings yet
- IntProt PDFDocument15 pagesIntProt PDFWasilla MahdaNo ratings yet
- The Intestinal ProtozoaDocument15 pagesThe Intestinal ProtozoaKHURT MICHAEL ANGELO TIUNo ratings yet
- Amoeba Notes 2015Document6 pagesAmoeba Notes 2015Ivy FlorentinoNo ratings yet
- Protista (Subdivision Protozoa) : Bütschlii), or Pathogenic (E. Histolytica)Document6 pagesProtista (Subdivision Protozoa) : Bütschlii), or Pathogenic (E. Histolytica)Primo GeorgeNo ratings yet
- Free-Living Amoebas & Ciliates (Lab)Document10 pagesFree-Living Amoebas & Ciliates (Lab)Xie LianNo ratings yet
- Activity 2Document2 pagesActivity 2Cyril LumibaoNo ratings yet
- Medical Biology 3Document42 pagesMedical Biology 3Malik MohamedNo ratings yet
- Introduction To ParasitologyDocument79 pagesIntroduction To ParasitologyLeeShauran100% (7)
- PROTOZOA (Sarcodina) : ProtozoologyDocument7 pagesPROTOZOA (Sarcodina) : ProtozoologyReyven Niña DyNo ratings yet
- OkieDocument3 pagesOkieFebeval CastilloNo ratings yet
- ClinPara FlagellatesDocument10 pagesClinPara FlagellatesStephen YorNo ratings yet
- Para Lec Lesson2Document9 pagesPara Lec Lesson2Tolentino, Edron E.No ratings yet
- ClinPara AmoebaDocument8 pagesClinPara AmoebaStephen YorNo ratings yet
- Clinical+Parasitology-Module+10 2Document12 pagesClinical+Parasitology-Module+10 2Geresh MagsinoNo ratings yet
- Micro ParasitesDocument4 pagesMicro ParasitesKrisha Marie BadilloNo ratings yet
- Balantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansDocument2 pagesBalantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansMichael Vincent P.No ratings yet
- Amoeba PrefinalsDocument5 pagesAmoeba PrefinalsKervy Jay AgraviadorNo ratings yet
- FINALS Intestinal NematodesDocument17 pagesFINALS Intestinal NematodesLoveyysolonNo ratings yet
- Supplemental Readings On ProtozoansDocument18 pagesSupplemental Readings On Protozoansferrerjericho300No ratings yet
- Worksheet 5 - Diagnostic Features of Medically Important ProtozoansDocument6 pagesWorksheet 5 - Diagnostic Features of Medically Important ProtozoansKyra ErniNo ratings yet
- Amoeba paraDocument9 pagesAmoeba paraHANNA CASANDRA GARCIANo ratings yet
- Tabular Parasitology MICROPARADocument19 pagesTabular Parasitology MICROPARAJerlyn FranciscoNo ratings yet
- 7 - Nematodes (Aphasmids and Phasmids)Document9 pages7 - Nematodes (Aphasmids and Phasmids)Scarlet WitchNo ratings yet
- Amoeba: Ms. Helga SyDocument7 pagesAmoeba: Ms. Helga Syanti romantic txtNo ratings yet
- Parasitic Amoebas by Dr. C. J. Castro PDFDocument4 pagesParasitic Amoebas by Dr. C. J. Castro PDFMiguel CuevasNo ratings yet
- BZ Lab 4.0Document7 pagesBZ Lab 4.0Alexa Jean D. HonrejasNo ratings yet
- PARASITOLOGY (Quizlet)Document9 pagesPARASITOLOGY (Quizlet)Allyssa AniNo ratings yet
- Nonpathogenic Amoebae - FlagellatesDocument20 pagesNonpathogenic Amoebae - FlagellatesHend AtijaniNo ratings yet
- Intestinal and Commensal AmoebaDocument9 pagesIntestinal and Commensal AmoebaFuture TrekingNo ratings yet
- Lesson 5 Plasmodium SPPDocument8 pagesLesson 5 Plasmodium SPPAnya IgnacioNo ratings yet
- Introduction To Parasitology PDFDocument17 pagesIntroduction To Parasitology PDFArianna Aparte AvenidoNo ratings yet
- Plasm OdiumDocument12 pagesPlasm OdiumtqurroNo ratings yet
- Parasitology Ciliates FlagellatesDocument4 pagesParasitology Ciliates FlagellatesarvinkennethdelacruzNo ratings yet
- Nematodes 2Document7 pagesNematodes 2Ericsson CarabbacanNo ratings yet
- Introduction To Cestodes and Minor CestodesDocument8 pagesIntroduction To Cestodes and Minor CestodesJustin TayabanNo ratings yet
- AMOEBADocument74 pagesAMOEBAhuyenthanh1807No ratings yet
- AMOEBADocument11 pagesAMOEBAMicaella RemilloNo ratings yet
- Parasitic AmoebaDocument23 pagesParasitic AmoebaJethrö MallariNo ratings yet
- Para Lab 11Document3 pagesPara Lab 11api-3743217No ratings yet
- Parasites by Apple TanDocument16 pagesParasites by Apple TanOlivia LimNo ratings yet
- Significance of Commensal Amebae in StoolDocument12 pagesSignificance of Commensal Amebae in StoolNicolle PanchoNo ratings yet
- Lecture 3 para Summer 2023-1Document47 pagesLecture 3 para Summer 2023-1محمود سليمانNo ratings yet
- Disease Causing OrganismsDocument4 pagesDisease Causing OrganismsANKITA GAYENNo ratings yet
- (PARA) Coccidia - Dedace2013Document3 pages(PARA) Coccidia - Dedace2013Marion YouthforChrist Acojido100% (1)
- Ameba and E.histolyticaDocument18 pagesAmeba and E.histolyticapenonia.abegailashleyNo ratings yet
- ECHINOCOCCUSDocument5 pagesECHINOCOCCUSGhina RizwanNo ratings yet
- 745 MycoplasmaDocument79 pages745 MycoplasmadrbhaveshparmarNo ratings yet
- Kingdom Monera ZoologyDocument2 pagesKingdom Monera ZoologyBASI, HEINDRICH LLOYD M.No ratings yet
- Parasaytology 2 DRDocument104 pagesParasaytology 2 DRMampise DepyeNo ratings yet
- Short Writing Assignment 4Document5 pagesShort Writing Assignment 4Troi JeraoNo ratings yet
- Reviewer On EukaryotesDocument6 pagesReviewer On EukaryotesAlaica Joice B. JaboneteNo ratings yet
- Para Protozoa Part2Document19 pagesPara Protozoa Part2BSMLS2AMERCADO ARJAYA.No ratings yet
- Camp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.From EverandCamp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.No ratings yet
- Community Needs AssessmentDocument5 pagesCommunity Needs AssessmentAbcd ReyesNo ratings yet
- Entrepreneurship: The Philippine Environment For EntrepreneurshipDocument44 pagesEntrepreneurship: The Philippine Environment For EntrepreneurshipAbcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - Human Body Lesson 1Document8 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - Human Body Lesson 1Abcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - The Language of Anatomy Lesson 1Document4 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - The Language of Anatomy Lesson 1Abcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATOPHYSIOLOGY Laboratory Lecture Cardiovasculas System Lesson 9Document13 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATOPHYSIOLOGY Laboratory Lecture Cardiovasculas System Lesson 9Abcd ReyesNo ratings yet
- Legionella Pneumophila Bartonella Spp. Campylobacter Jejuni Helicobacter PyloriDocument1 pageLegionella Pneumophila Bartonella Spp. Campylobacter Jejuni Helicobacter PyloriAbcd ReyesNo ratings yet
- Bacteroides Spp. Porphyromonas Spp. Fusobacterium Spp. Prevotella SPPDocument2 pagesBacteroides Spp. Porphyromonas Spp. Fusobacterium Spp. Prevotella SPPAbcd ReyesNo ratings yet
- GC1 - Week 1 - Lesson 3 4 LECTUREDocument35 pagesGC1 - Week 1 - Lesson 3 4 LECTUREAbcd ReyesNo ratings yet
- Corynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPDocument1 pageCorynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPAbcd ReyesNo ratings yet
- General Chemistry 1 - Week 1: Mr. Daryl Vince D. Romerosa - SST1Document41 pagesGeneral Chemistry 1 - Week 1: Mr. Daryl Vince D. Romerosa - SST1Abcd Reyes100% (1)
- Mathematics in Our WorldDocument42 pagesMathematics in Our WorldAbcd ReyesNo ratings yet
- IIIII mp3Document10 pagesIIIII mp3Abcd ReyesNo ratings yet
- General Chemistry 1: Learner'S Packet inDocument13 pagesGeneral Chemistry 1: Learner'S Packet inAbcd ReyesNo ratings yet
- Pre-Learning Concept CheckDocument4 pagesPre-Learning Concept CheckAbcd ReyesNo ratings yet
- Dancing With Yin Yang Chap6 ANS LRDocument34 pagesDancing With Yin Yang Chap6 ANS LRmarianetlaNo ratings yet
- Discovery-Driven Research and Bioinformatics in Nuclear Receptor andDocument10 pagesDiscovery-Driven Research and Bioinformatics in Nuclear Receptor andtaoufik akabliNo ratings yet
- Hypnotic Regression TherapyDocument8 pagesHypnotic Regression TherapyAdithya MakkattilNo ratings yet
- Physiology MCQsDocument7 pagesPhysiology MCQsNatukunda DianahNo ratings yet
- Endothelial Dysfunction in Diabetic Erectile DysfunctionDocument11 pagesEndothelial Dysfunction in Diabetic Erectile DysfunctionILham SyahNo ratings yet
- Ref. 1002120 Spintrol H N Lot. 3576Document4 pagesRef. 1002120 Spintrol H N Lot. 3576Edwin josé Nicaragua RíosNo ratings yet
- Classifying PlantsDocument2 pagesClassifying PlantsJanelle BerkemeierNo ratings yet
- SUBHADIPA - MAJUMDERComparative Account of Aortic Arch2020!04!03Aortic Arch Comparative PDFDocument11 pagesSUBHADIPA - MAJUMDERComparative Account of Aortic Arch2020!04!03Aortic Arch Comparative PDFTharun BharadwajNo ratings yet
- Anat Table Conference - Nervous TissueDocument12 pagesAnat Table Conference - Nervous TissuePeter ThompsonNo ratings yet
- By: Prof Saeed Abuel Makarem & DR - Sanaa AlshaarawiDocument24 pagesBy: Prof Saeed Abuel Makarem & DR - Sanaa AlshaarawiRakesh Kumar RanjanNo ratings yet
- Guide Questions Answers: Muscles Contract, They Contribute To Gross and FineDocument7 pagesGuide Questions Answers: Muscles Contract, They Contribute To Gross and FinePrancheska Abigayle Peneyra SantiagoNo ratings yet
- Lecture Planner (Biology) - Neev 2025Document1 pageLecture Planner (Biology) - Neev 2025prathamgptt.1234No ratings yet
- Persistent Elevation of Intraocular Pressure Following Intravitreal Injection of BevacizumabDocument4 pagesPersistent Elevation of Intraocular Pressure Following Intravitreal Injection of Bevacizumab6jprsrbhkcNo ratings yet
- Answers To End of Chapter Questions Chapter 14 HomeostasisDocument2 pagesAnswers To End of Chapter Questions Chapter 14 HomeostasisAnand EnkhjinNo ratings yet
- Biology Form One NotesDocument135 pagesBiology Form One NotesstationarymurietNo ratings yet
- 4HB0 Getting Started Guide 2017 (9-1)Document32 pages4HB0 Getting Started Guide 2017 (9-1)NoaNo ratings yet
- Concise Review: Mesenchymal Stem Cells and Translational Medicine: Emerging IssuesDocument8 pagesConcise Review: Mesenchymal Stem Cells and Translational Medicine: Emerging IssuesLorenzo Maria CerviNo ratings yet
- Disseminated Intravascular Coagulopathy DICDocument24 pagesDisseminated Intravascular Coagulopathy DICMassimiliano MalerbaNo ratings yet
- Art Vampire Bat ExhibitDocument15 pagesArt Vampire Bat ExhibitAlejo RuilovaNo ratings yet
- Iferika JR Histology Slide Compilation-1Document197 pagesIferika JR Histology Slide Compilation-1ikembachinomso06No ratings yet
- Summative Test-G8-Quarter-4Document13 pagesSummative Test-G8-Quarter-4Charmaine CanonoNo ratings yet
- Id KezDocument129 pagesId KezAxi AxiNo ratings yet
- K12 BIO1 EXER2 - Plant-Cell PDFDocument9 pagesK12 BIO1 EXER2 - Plant-Cell PDFZina CuldoraNo ratings yet
- Implantation & Second WeekDocument18 pagesImplantation & Second WeekCabdiladif Ahmed McrfNo ratings yet
- Reinforcement in Checking Vital SignsDocument7 pagesReinforcement in Checking Vital SignsFarah FildzahNo ratings yet
- Ib Biology Mark Scheme PhotosynthesisDocument8 pagesIb Biology Mark Scheme Photosynthesisafbsyebpu100% (2)
- Charity Kapenda Muselema: Term 3 - NeurophysiologyDocument50 pagesCharity Kapenda Muselema: Term 3 - NeurophysiologyHomeground entertainmentNo ratings yet
- Cardiovascular Physiology Practice QuestionsDocument4 pagesCardiovascular Physiology Practice QuestionsHayley Welsh100% (1)
- T3-Blood Groups, Products and PlateletsDocument41 pagesT3-Blood Groups, Products and Plateletsdanielnsy28No ratings yet
Balantidum Coli: EBON, SISON - 2017
Balantidum Coli: EBON, SISON - 2017
Uploaded by
Abcd ReyesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Balantidum Coli: EBON, SISON - 2017
Balantidum Coli: EBON, SISON - 2017
Uploaded by
Abcd ReyesCopyright:
Available Formats
UERMMMCI: CAHP (BATCH 2019) Two Developmental stages of ciliates and flagellates in GIT
PARASITOLOGY – FINALS - Cyst
Reference: Lecture notes prepared by Prof. Eduardo - Infective stage to man
EBON 2017 - Sturdy – able to survive in chlorinated water
- Trophozoites
CILIATES AND FLAGELLATES - Pathogenic stage
Outline: - Can‟t survive outside environment for long
period of time
I. Flow Cyst trophozoite EXCYSTATION
II. Introduction Trophozoites cyst ENCYSTATION
III. Balantidum coli
IV. Mastigophora flagellates Balantidum coli
- Giardia Intestinalis / Giardia duodenalis / INTRODUCTION
lambia Parasites of pig but can cause disease to man
- Chilomastix mesnili 1857 – Malmstem
V. Trichomonads - First to recognized B. coli in 2 humans with dysentery
- Dientamoeba fragilis (blood and mucus in stool)
- Trichomonas vaginalis - First name given: “Paramecium coli” due to several cilia
- Trichomonas tenax 1861 – Leuckart
- Trichomonas hominis - First saw the morphology similarly with that parasites
from pig‟s intestine
Flow STEIN
- Renamed: “balantidium coli”I looks like a bag with furs
Introduction - “balanto” – greek word “bag”
Habitat: Colon, Cecum, LI
Morphology Disease: Balantidiasis
Opportunistic pathogen
Life Cycle - Pathophysiology
MORPHOLOGY
Laboratory Diagnosis
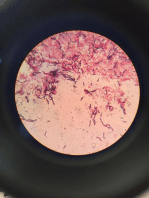
1. Trophozoite
Tissue invader
Epidemiology
30-150 micrometer in length
PVC Cy (cystosome or mouth)
Micronucleus - reproduction
INTRODUCTION Macronucleus
Recall: - metabolism and growth
- „sausage shape‟ tapered anterior end surface
Sarcodina – Amoeba covered with cilia
Mastigophora – Flagellates CV (contractile vacuole)
Ciliophora – Ciliates
Apicomplexa – Sporozoa, Ciccidians
Sporozoa
- e.g. Malarial parasite
Coccidians
- e.g. Toxoplasma & Cryptosporidia
Types of Nucleus of Protozoa
- Entamoeba histolytica
- Pseudopod
- Karyosome (nucleolus)
- Nuclear chromatin (chromatin granules) Figure 1. B. coli trophozoite (Image obtained from
- “fine chromatin granules with small central www.cdc.gov/dpdx)
granules” 2. Cysts
- Entamoeba coli Size: 45-65 micrometer
- Larger chromatin granules than E. histolytica Micronucleus - reproduction
- Eccentric karyosome Macronucleus - metabolism and growth
- G. lamblia CV (contractile vacuole)
- “large central karyosome” Without cilia
- D. fragilis
- ”clusters of 4-8 chromatin granules”
EBON, SISON | 2017 1
LABORATORY DIAGNOSIS up to EPIDEMIOLOGY
Specimen: stool
Test: concentration wet preparation to visualize the cilia.(s.a
Zinc flotation method
Epdiemiology
- Areas with poor sanitation
- Close contact with pigs or pig‟s feces
- Overcrowded institution (e.g. asylum, prisons,
orphanage)
- Bolivia
- Papua New Guinea
- Philippines In 2005, a study was done on pigs in southern
Figure 2. Cysts of B. coli (Image obtained from
& northern PH. Revealed 66.1% prevalence of B. coli
www.cdc.gov/dpdx)
infection in pigs‟
LIFE CYCLE
Cecum & colon Mastigophora (Flagellates)
Characteristics:
- Flagella (one or more) move in “counter clockwise”
Invade mucosa & multiply by binary fission or conjugation
fashion creating a rapid movement.
- All reproduce ASEXUALLY (binary fission)
Secretion of hyaluronidase then digests epithelium causing
Ulceration of the intestinal mucosa/
Members:
- Chilomastix mesnii
Encystation in rectum
- Giardia duodenalis
- Trichomonads:
Ingestion of contaminated water excystation in small intestine\
o Dientamoeba fragilis
o Trichomonas spp
PATHOPHYSIOLOGY
Characteristics of ulcer produced: - Trypanosoma spp
- Larger compared to amoeba - Leishmania spp
- Multiple
- Wide neck Classification:
- Round or oval base - Blood and tissue
Incubation period 4 to 5 days for Balantidiasis o Leishmania & trypanosoma
S/Sx: - Intestinal
- Watery stool or with blood and pus o G. dudodenalis & C. mesnili
- Nausea - Trichomonads
- Anorexia o D. fragilis, T. vaginalis
- Tenesmus
- Abdominal pain Giardia intestinalis / Giardia duodenalis or Giardia lambia
INTRODUCTION up to MORPHOLOGY
- Diarrhea
History:
Clinical manifestations:
- 1859 – first describe by Lamb
o 80% of infected are asymptomatic carriers (serve as
The father of microbiology – Anton Van leeuwenhoek
reservoir)
- 1681 – discovered G. duodenalis in his stool
o Chronic-colitis – non bloody diarrhea, abdominal
Disease: Giardiasis
cramps, halitosis
o Fulminating balantidiasis – mucoid and bloody stool,
1. Trophozoites
weight loss
12-15 micrometer length
Tissues invaded
2 nuclei with large karyosome
- Mesenteric nodes
Medial bodies
- Appendix
Axoneme
- Cecum (habitat)
2 ventral flagella
- Extraintestinal
Adhesive disc/sucking disc
- Lungs
4 pairs of flagella
- Liver
2 anterior
- GU
2 posterior
Possible pathway to the lungs
2 caudal
- Lymphatic system
2 ventral
- Hepatic portal circuit
o As the trophozoites mature to cyst the flagella
- Perforation of the colon and spread thru the peritoneal
and sucking discs are lost.
cavity
“Smiley face”
Note: the presence of cilia in the lungs, will challenge you, thus,
Motility: “falling leaf” motion
examine accurately
EBON, SISON | 2017 2
LABORATORY DIAGNOSIS
Specimen: stool
3 stool sample taken every 2 days interval
Look for Charcot-leyden crystals (products from eosinophils)
Figure 3. Trophozoites of G.lambia ((Image obtained from
www.cdc.gov/dpdx)
LIFE CYCLE
Stomach gastric acid stimulates excystation
IFA, ELISA
Attached to intestinal villi (duodenum and jejunum) via sucking String test (Entero test)
disc - Use a gelatin capsule with an attached thread
- One end is attached to the inner aspect of the
Will cause Flattening of villi, crypt hyperplasia, decrease patient‟s cheek
lactase enzyme, bile salts taken up for excystation and bacterial - The capsule is swallowed
growth - Thread is withdrawn and shaken in saline to release the
trophozoite.
Encystation in large intestines
EPIDEMIOLOGY
PATHOPHYSIOLOGY Reservoir host:
Flattening of villi lead to decreased in absorption - Human
Crypt hyperplasia associated with increased enterocyte - Dogs
migration rate - Beaver
- Can lead to lactose deficiency. Vehicles:
- Extremely large no. of trop may lead to direct physical - Water
blockage of nutrient uptake esp fat soluble substances - Resistant traditional 5%chlorine
(Vitamin B12) Malabsorption syndrome - Survive at 62C, survive in lakes (3 months)
Clinical manifestations - Uncooked contaminated vegetables and fruits
- 50% of infected are asymptomatic carriers. Worldwide
- Acute giardiasis: less nutrient and H20 absorption > Philippines – 1.6 to 22%
“traveler” diarrhea, flatulence with odor of rotten egg- The first published study showed that 86% of
like smell (1-2 weeks) isolates belongs to genotype assemblage B.
- Chronic giardiasis – depends on number of Results of experiment done in Animals
trophozoites (diarrhea, malabsorption syndrome, fatty - Malabsorption caused diarrhea not active secretion
stool) e.g. enterotoxin of bacteria
Crypt and villus astrophy lactase deficient Vitro
- Human milk kills trophozoites
Available lactose used for bacterial growth
Chilomastix mesnili
Bacterial growth & excystation used bile salt MORPHOLOGY
1. Cysts
Decreased in bile salt 6-10 micrometer
Thick cyst wall
Less uptake of lipid Cystosome (“open safety pin” or “shepherds crook”
Lemon shape with hyaline protrusion
Steatorrhea Large nucleus with central karyosome
Host immunity
- Mostly humoral
- Due to the exhibition of Ag variation
- Expressed 180 different Antigens over 6-12 generations
IgM & sIgA plays important role Patient with sIgA
deficiency + with duodenal or jejunal diverticula
(congenital) = chronic giardiasis
EBON, SISON | 2017 3
Life cycle:
- Proposed transmission: via helminths ova Enterobius
and Ascaris
- Ingestion
- Binary fission
- Trophozoite in the feces
- Cycle continue
Clinical manifestations:
- Diarrhea
- Abdominal pain
- Anorexia
- Fatigue
Figure 4. Cyst of Chilomastix mesnili (Image obtained from
- Probably acts as low-grade irritant of intestinal mucosal
www.cdc.gov/dpdx)
surfaces that may lead to inflammation.
2. Trophozoites:
- 1977 – 1st case reported in Thailand
12-20 micrometer
Laboratory Diagnosis
Pear shape
Difficult to identify in fresh wet mount can be mistaken
3 flagella
with
1 flagellum (longer)
WBC
Large nucleus with central karyosome located
Faecal debris
anteriorly
Intestinal cells
Cytostome (“ open safety pin” & “sheperds crook”)
o Formed stool – trophozoite not motile
Spiral groove
o Watery stool – actively motile
Figure. 5 Trophozoite of Chilomastix mesnili (Image obtained from
www.cdc.gov/dpdx)
Trichomonads
Characteristics: Figure 6. Trophozoite of Dientamoeba fragilis (Image obtained
- Anaerobic from www.cdc.gov/dpdx)
- Cyst not formed
- Transmission: direct contact
- Possess 4-6 flagella at the apical pole
- Axostyle present
Dientamoeba fragilis
INTRODUCTION up to LABORATORY DIAGNOSIS
Di – 2
Ent – intestine
Amoeba – with pseudopod
Fragilis – fragile
Formerly under Family Endamoebidae
Habitat: cecum & upper colon
Structure of Trichomonas
Reasons for transfer to Family Trichomonads:
- Four anterior flagella (jerky motility)
Structures:
- Nucleus
- Has different nucleus
- Axostyle (central rod)
- Exist as trophozoite only
- Posterior flagellum (T. hominis)
- Has extra spindle
- Undulating membrane
- Closely related to Genus Histomonas (
Amoeboflagellates)
Trichomonas tenax (tetra trichomonas buccalis)
Characteristics
Commensals in mouth of humans and pirates
- No cystic stage
Found in tartar, defect of caries? Teeth
- 5-15 micrometer
- 2 nuclei
- Clusters of 4-8 chromatin granules
- Uses trichrome strain
EBON, SISON | 2017 4
Trichomonas vaginalis - Vulva itching or swelling
MORPHOLOGY up to LIFE CYCLE - Burning sensation/vaginal itching (15-20%)
Nucleus - Abundant “frothy” yellow green vaginal discharge (50-
Flagella 75%)
Undulating membrane (half of the body) - Punctate cervical microhemorrhages (25%)
Life cycle:
Female: Complications
- Vagina - Premature delivery due to premature rupture of the
- Skene‟s gland (urethra) membrane (PPROM)
Male: - Baby may have low birth weight (<5.5 lbs. at birth )
- Urethra - Predisposing factors to:
Note: Pass thru sexual intercourse with multiple partners. HIV infection (presence of open
- Prefers alkaline pH wound)
- Can live outside the host up to 30 minutes Cervical cancer (2001)
- May survive in a host (esp. men) >two years
- Menopause (6-7 pH) LABORATORY DIAGNOSIS up to PVC
- Use of birth control pills Pelvic examination
- Prolonged used of antibiotic. - “strawberry cervix” vaginal wall have erythema and
punctuate hemorrhages
- T. vaginalis adhere to vaginal squamous epithelial.
“Strawberry cervix” is due to extensive inflammation
and erosion of vaginal or urethral epithelium
- N. gc adhere to endocervix columnar epithelium
Methods of specimen collection
Female:
- Self obtained low vaginal swab (SOLV)
- High vaginal swab
Male:
- Get the scanty transparent or white
Figure 6. Trophozoite of Trichomonas vaginalis (Image obtained discharge
from www.cdc.gov/dpdx) Treatment:
o Sometimes men may need no treatment as the
infection is likely to resolve itself in a couple of weeks.
CHARACTERISTICS
Characteristics: o Metronidazole one megadose taken orally
“Clean-up organism” o Tinidazole
Feeds on: o Most curable STI
- Cell debris o Pregnant:
- Pus - 1st trimester – tropical clotrimazole
- Bacteria - 2nd and 3rd trimester – metronidazole orally
o Home remedies:
PATHOGENESIS - Sitz bath with lemon and vinegar
Incubation period: 4 to 28 days - Lactobacillus acido good bacteria
PVC:
Adhere to vaginal squamous epithelial cell and release protein - Practice monogamy
enzyme (digest tissue) - Avoid intercourse during treatment
- Notify his or her partner so they can be treated to avoid
Triggers: extensive inflammation and erosion of vaginal or re-infection.
urethral epithelium - Avoid unprotected sexual contact (condoms reduce
risk only, not 100% protective)
Effects: redness, swelling, pain, itching, pus, exudation. - Take shower after intercourse
- Don‟t share towels or underwears.
Symptoms: in male - Frequently co-exist with other STI
- Mild white or transparent discharge from the penis
(50-60%)
- Itching of the urethra (25%)
- Burning sensation after urination or ejaculation (12-
25%)
- Holds infections for years, asymptomatic (50-90%)
- Some may develop:
Prostitis
Epididymitis
Symptoms: in female
- Discomfort or pain during intercourse
EBON, SISON | 2017 5
You might also like
- Test Bank For Anatomy and Physiology: An Integrative Approach 3Rd Edition, by Mckinley DR., Michael, Valerie Oâ ™loughlin, Theresa BidleDocument36 pagesTest Bank For Anatomy and Physiology: An Integrative Approach 3Rd Edition, by Mckinley DR., Michael, Valerie Oâ ™loughlin, Theresa Bidlesublunardisbench.2jz85100% (23)
- Balantidium Coli: Disease, Epidemiology and Laboratory DiagnosisDocument38 pagesBalantidium Coli: Disease, Epidemiology and Laboratory DiagnosisSanty PatNo ratings yet
- Medical Biology 3 - BR - 2020Document70 pagesMedical Biology 3 - BR - 2020Yusuf Yağız TimurNo ratings yet
- 1.3 Hemoflagellates and Ciliates (Limpin)Document4 pages1.3 Hemoflagellates and Ciliates (Limpin)arvinkennethdelacruzNo ratings yet
- (PARA) 1.5 - Blood and Tissue FlagellatesDocument6 pages(PARA) 1.5 - Blood and Tissue FlagellatesGuia De GuzmanNo ratings yet
- Parasitology-Lec 5 TrematodesDocument5 pagesParasitology-Lec 5 Trematodesapi-3743217100% (2)
- AmebaDocument53 pagesAmebaapi-19916399No ratings yet
- IntProt PDFDocument15 pagesIntProt PDFWasilla MahdaNo ratings yet
- The Intestinal ProtozoaDocument15 pagesThe Intestinal ProtozoaKHURT MICHAEL ANGELO TIUNo ratings yet
- Amoeba Notes 2015Document6 pagesAmoeba Notes 2015Ivy FlorentinoNo ratings yet
- Protista (Subdivision Protozoa) : Bütschlii), or Pathogenic (E. Histolytica)Document6 pagesProtista (Subdivision Protozoa) : Bütschlii), or Pathogenic (E. Histolytica)Primo GeorgeNo ratings yet
- Free-Living Amoebas & Ciliates (Lab)Document10 pagesFree-Living Amoebas & Ciliates (Lab)Xie LianNo ratings yet
- Activity 2Document2 pagesActivity 2Cyril LumibaoNo ratings yet
- Medical Biology 3Document42 pagesMedical Biology 3Malik MohamedNo ratings yet
- Introduction To ParasitologyDocument79 pagesIntroduction To ParasitologyLeeShauran100% (7)
- PROTOZOA (Sarcodina) : ProtozoologyDocument7 pagesPROTOZOA (Sarcodina) : ProtozoologyReyven Niña DyNo ratings yet
- OkieDocument3 pagesOkieFebeval CastilloNo ratings yet
- ClinPara FlagellatesDocument10 pagesClinPara FlagellatesStephen YorNo ratings yet
- Para Lec Lesson2Document9 pagesPara Lec Lesson2Tolentino, Edron E.No ratings yet
- ClinPara AmoebaDocument8 pagesClinPara AmoebaStephen YorNo ratings yet
- Clinical+Parasitology-Module+10 2Document12 pagesClinical+Parasitology-Module+10 2Geresh MagsinoNo ratings yet
- Micro ParasitesDocument4 pagesMicro ParasitesKrisha Marie BadilloNo ratings yet
- Balantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansDocument2 pagesBalantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansMichael Vincent P.No ratings yet
- Amoeba PrefinalsDocument5 pagesAmoeba PrefinalsKervy Jay AgraviadorNo ratings yet
- FINALS Intestinal NematodesDocument17 pagesFINALS Intestinal NematodesLoveyysolonNo ratings yet
- Supplemental Readings On ProtozoansDocument18 pagesSupplemental Readings On Protozoansferrerjericho300No ratings yet
- Worksheet 5 - Diagnostic Features of Medically Important ProtozoansDocument6 pagesWorksheet 5 - Diagnostic Features of Medically Important ProtozoansKyra ErniNo ratings yet
- Amoeba paraDocument9 pagesAmoeba paraHANNA CASANDRA GARCIANo ratings yet
- Tabular Parasitology MICROPARADocument19 pagesTabular Parasitology MICROPARAJerlyn FranciscoNo ratings yet
- 7 - Nematodes (Aphasmids and Phasmids)Document9 pages7 - Nematodes (Aphasmids and Phasmids)Scarlet WitchNo ratings yet
- Amoeba: Ms. Helga SyDocument7 pagesAmoeba: Ms. Helga Syanti romantic txtNo ratings yet
- Parasitic Amoebas by Dr. C. J. Castro PDFDocument4 pagesParasitic Amoebas by Dr. C. J. Castro PDFMiguel CuevasNo ratings yet
- BZ Lab 4.0Document7 pagesBZ Lab 4.0Alexa Jean D. HonrejasNo ratings yet
- PARASITOLOGY (Quizlet)Document9 pagesPARASITOLOGY (Quizlet)Allyssa AniNo ratings yet
- Nonpathogenic Amoebae - FlagellatesDocument20 pagesNonpathogenic Amoebae - FlagellatesHend AtijaniNo ratings yet
- Intestinal and Commensal AmoebaDocument9 pagesIntestinal and Commensal AmoebaFuture TrekingNo ratings yet
- Lesson 5 Plasmodium SPPDocument8 pagesLesson 5 Plasmodium SPPAnya IgnacioNo ratings yet
- Introduction To Parasitology PDFDocument17 pagesIntroduction To Parasitology PDFArianna Aparte AvenidoNo ratings yet
- Plasm OdiumDocument12 pagesPlasm OdiumtqurroNo ratings yet
- Parasitology Ciliates FlagellatesDocument4 pagesParasitology Ciliates FlagellatesarvinkennethdelacruzNo ratings yet
- Nematodes 2Document7 pagesNematodes 2Ericsson CarabbacanNo ratings yet
- Introduction To Cestodes and Minor CestodesDocument8 pagesIntroduction To Cestodes and Minor CestodesJustin TayabanNo ratings yet
- AMOEBADocument74 pagesAMOEBAhuyenthanh1807No ratings yet
- AMOEBADocument11 pagesAMOEBAMicaella RemilloNo ratings yet
- Parasitic AmoebaDocument23 pagesParasitic AmoebaJethrö MallariNo ratings yet
- Para Lab 11Document3 pagesPara Lab 11api-3743217No ratings yet
- Parasites by Apple TanDocument16 pagesParasites by Apple TanOlivia LimNo ratings yet
- Significance of Commensal Amebae in StoolDocument12 pagesSignificance of Commensal Amebae in StoolNicolle PanchoNo ratings yet
- Lecture 3 para Summer 2023-1Document47 pagesLecture 3 para Summer 2023-1محمود سليمانNo ratings yet
- Disease Causing OrganismsDocument4 pagesDisease Causing OrganismsANKITA GAYENNo ratings yet
- (PARA) Coccidia - Dedace2013Document3 pages(PARA) Coccidia - Dedace2013Marion YouthforChrist Acojido100% (1)
- Ameba and E.histolyticaDocument18 pagesAmeba and E.histolyticapenonia.abegailashleyNo ratings yet
- ECHINOCOCCUSDocument5 pagesECHINOCOCCUSGhina RizwanNo ratings yet
- 745 MycoplasmaDocument79 pages745 MycoplasmadrbhaveshparmarNo ratings yet
- Kingdom Monera ZoologyDocument2 pagesKingdom Monera ZoologyBASI, HEINDRICH LLOYD M.No ratings yet
- Parasaytology 2 DRDocument104 pagesParasaytology 2 DRMampise DepyeNo ratings yet
- Short Writing Assignment 4Document5 pagesShort Writing Assignment 4Troi JeraoNo ratings yet
- Reviewer On EukaryotesDocument6 pagesReviewer On EukaryotesAlaica Joice B. JaboneteNo ratings yet
- Para Protozoa Part2Document19 pagesPara Protozoa Part2BSMLS2AMERCADO ARJAYA.No ratings yet
- Camp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.From EverandCamp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.No ratings yet
- Community Needs AssessmentDocument5 pagesCommunity Needs AssessmentAbcd ReyesNo ratings yet
- Entrepreneurship: The Philippine Environment For EntrepreneurshipDocument44 pagesEntrepreneurship: The Philippine Environment For EntrepreneurshipAbcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - Human Body Lesson 1Document8 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - Human Body Lesson 1Abcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - The Language of Anatomy Lesson 1Document4 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATHOPHYSIOLOGY Laboratory - Lecture - The Language of Anatomy Lesson 1Abcd ReyesNo ratings yet
- (BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATOPHYSIOLOGY Laboratory Lecture Cardiovasculas System Lesson 9Document13 pages(BMED66) HUMAN ANATOMY & PHYSIOLOGY WITH PATOPHYSIOLOGY Laboratory Lecture Cardiovasculas System Lesson 9Abcd ReyesNo ratings yet
- Legionella Pneumophila Bartonella Spp. Campylobacter Jejuni Helicobacter PyloriDocument1 pageLegionella Pneumophila Bartonella Spp. Campylobacter Jejuni Helicobacter PyloriAbcd ReyesNo ratings yet
- Bacteroides Spp. Porphyromonas Spp. Fusobacterium Spp. Prevotella SPPDocument2 pagesBacteroides Spp. Porphyromonas Spp. Fusobacterium Spp. Prevotella SPPAbcd ReyesNo ratings yet
- GC1 - Week 1 - Lesson 3 4 LECTUREDocument35 pagesGC1 - Week 1 - Lesson 3 4 LECTUREAbcd ReyesNo ratings yet
- Corynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPDocument1 pageCorynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPAbcd ReyesNo ratings yet
- General Chemistry 1 - Week 1: Mr. Daryl Vince D. Romerosa - SST1Document41 pagesGeneral Chemistry 1 - Week 1: Mr. Daryl Vince D. Romerosa - SST1Abcd Reyes100% (1)
- Mathematics in Our WorldDocument42 pagesMathematics in Our WorldAbcd ReyesNo ratings yet
- IIIII mp3Document10 pagesIIIII mp3Abcd ReyesNo ratings yet
- General Chemistry 1: Learner'S Packet inDocument13 pagesGeneral Chemistry 1: Learner'S Packet inAbcd ReyesNo ratings yet
- Pre-Learning Concept CheckDocument4 pagesPre-Learning Concept CheckAbcd ReyesNo ratings yet
- Dancing With Yin Yang Chap6 ANS LRDocument34 pagesDancing With Yin Yang Chap6 ANS LRmarianetlaNo ratings yet
- Discovery-Driven Research and Bioinformatics in Nuclear Receptor andDocument10 pagesDiscovery-Driven Research and Bioinformatics in Nuclear Receptor andtaoufik akabliNo ratings yet
- Hypnotic Regression TherapyDocument8 pagesHypnotic Regression TherapyAdithya MakkattilNo ratings yet
- Physiology MCQsDocument7 pagesPhysiology MCQsNatukunda DianahNo ratings yet
- Endothelial Dysfunction in Diabetic Erectile DysfunctionDocument11 pagesEndothelial Dysfunction in Diabetic Erectile DysfunctionILham SyahNo ratings yet
- Ref. 1002120 Spintrol H N Lot. 3576Document4 pagesRef. 1002120 Spintrol H N Lot. 3576Edwin josé Nicaragua RíosNo ratings yet
- Classifying PlantsDocument2 pagesClassifying PlantsJanelle BerkemeierNo ratings yet
- SUBHADIPA - MAJUMDERComparative Account of Aortic Arch2020!04!03Aortic Arch Comparative PDFDocument11 pagesSUBHADIPA - MAJUMDERComparative Account of Aortic Arch2020!04!03Aortic Arch Comparative PDFTharun BharadwajNo ratings yet
- Anat Table Conference - Nervous TissueDocument12 pagesAnat Table Conference - Nervous TissuePeter ThompsonNo ratings yet
- By: Prof Saeed Abuel Makarem & DR - Sanaa AlshaarawiDocument24 pagesBy: Prof Saeed Abuel Makarem & DR - Sanaa AlshaarawiRakesh Kumar RanjanNo ratings yet
- Guide Questions Answers: Muscles Contract, They Contribute To Gross and FineDocument7 pagesGuide Questions Answers: Muscles Contract, They Contribute To Gross and FinePrancheska Abigayle Peneyra SantiagoNo ratings yet
- Lecture Planner (Biology) - Neev 2025Document1 pageLecture Planner (Biology) - Neev 2025prathamgptt.1234No ratings yet
- Persistent Elevation of Intraocular Pressure Following Intravitreal Injection of BevacizumabDocument4 pagesPersistent Elevation of Intraocular Pressure Following Intravitreal Injection of Bevacizumab6jprsrbhkcNo ratings yet
- Answers To End of Chapter Questions Chapter 14 HomeostasisDocument2 pagesAnswers To End of Chapter Questions Chapter 14 HomeostasisAnand EnkhjinNo ratings yet
- Biology Form One NotesDocument135 pagesBiology Form One NotesstationarymurietNo ratings yet
- 4HB0 Getting Started Guide 2017 (9-1)Document32 pages4HB0 Getting Started Guide 2017 (9-1)NoaNo ratings yet
- Concise Review: Mesenchymal Stem Cells and Translational Medicine: Emerging IssuesDocument8 pagesConcise Review: Mesenchymal Stem Cells and Translational Medicine: Emerging IssuesLorenzo Maria CerviNo ratings yet
- Disseminated Intravascular Coagulopathy DICDocument24 pagesDisseminated Intravascular Coagulopathy DICMassimiliano MalerbaNo ratings yet
- Art Vampire Bat ExhibitDocument15 pagesArt Vampire Bat ExhibitAlejo RuilovaNo ratings yet
- Iferika JR Histology Slide Compilation-1Document197 pagesIferika JR Histology Slide Compilation-1ikembachinomso06No ratings yet
- Summative Test-G8-Quarter-4Document13 pagesSummative Test-G8-Quarter-4Charmaine CanonoNo ratings yet
- Id KezDocument129 pagesId KezAxi AxiNo ratings yet
- K12 BIO1 EXER2 - Plant-Cell PDFDocument9 pagesK12 BIO1 EXER2 - Plant-Cell PDFZina CuldoraNo ratings yet
- Implantation & Second WeekDocument18 pagesImplantation & Second WeekCabdiladif Ahmed McrfNo ratings yet
- Reinforcement in Checking Vital SignsDocument7 pagesReinforcement in Checking Vital SignsFarah FildzahNo ratings yet
- Ib Biology Mark Scheme PhotosynthesisDocument8 pagesIb Biology Mark Scheme Photosynthesisafbsyebpu100% (2)
- Charity Kapenda Muselema: Term 3 - NeurophysiologyDocument50 pagesCharity Kapenda Muselema: Term 3 - NeurophysiologyHomeground entertainmentNo ratings yet
- Cardiovascular Physiology Practice QuestionsDocument4 pagesCardiovascular Physiology Practice QuestionsHayley Welsh100% (1)
- T3-Blood Groups, Products and PlateletsDocument41 pagesT3-Blood Groups, Products and Plateletsdanielnsy28No ratings yet