Professional Documents
Culture Documents
Cardio Emergency Hemorrage
Cardio Emergency Hemorrage
Uploaded by
SN BundleOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardio Emergency Hemorrage
Cardio Emergency Hemorrage
Uploaded by
SN BundleCopyright:
Available Formats
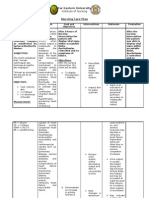
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
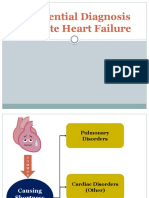
PULMONARY EDEMA Tachycardia and JVD
common complication of cardiac disorders common signs
common complication of cardiac disorders Incessant coughing
associated with acute decompensated HF foamy sputum
cardiogenic or noncardiogenic confused and then stuporous
lead to acute respiratory failure and death bloody sputum
level of consciousness decreases
ETIOLOGY crepitant crackles
Cardiogenic pulmonary edema diastolic (S3) gallop
left-sided heart failure thready pulse
Noncardiogenic pulmonary edema decreased cardiac output.
barbiturate or opiate poisoning breath sounds diminish
intravenous (IV) fluids infused in excessive
volumes or at an overly rapid rate DIAGNOSTIC FINDINGS
transfusion reaction I. ABG analysis
impaired pulmonary lymphatic drainage hypoxia with variable partial pressures of arterial
eclampsia carbon dioxide
inhalation of irritating gases metabolic acidosis
pneumonia II. B-type natriuretic peptide (BNP)
ARDS or shock lung
increase in value
III. Chest X-rays
PATHOPHYSIOLOGY
haziness of the lung fields
When the left ventricle begins to fail cardiomegaly
flood backs up into the pulmonary circulation
pleural effusion
pulmonary interstitial edema
Butterfly appearance
rapid increase in atrial pressure
IV. Pulse oximetry
acute increase in pulmonary venous pressure
decreasing levels of arterial oxygen saturation
increase in hydrostatic pressure forces fluid
V. Echocardiogram
out of the pulmonary capillaries
fluid around the heart
The fluid within the alveoli mixes with air
producing the classic sign of pulmonary edema congenital heart defects
frothy pink sputum decreased heart flow
large amounts of alveolar fluid create a diffusion block decreased pumping actions
hypoxemia VI. Cardiac catheterization
elevated central venous and pulmonary artery
elevated capillary wedge pressures.
VII. ECG
Previous or current myocardial infarction.
PREVENTION
assesses the degree of dyspnea
auscultates the lung fields and heart sounds
assesses the degree of peripheral edema
early indicators of developing pulmonary edema:
hacking cough
fatigue
weight gain
increased edema
decreased activity tolerance
alleviated by increasing dosages of diuretics
upright position with the feet and legs
reduces left ventricular workload
MEDICAL MANAGEMENT
CLINICAL MANIFESTATION High concentrations of oxygen by cannula or mask
BiPAP assisted ventilation
restless
If the patient’s arterial oxygen levels remain too
anxious low
sudden onset of breathlessness usually improves acid–base balance
sense of suffocation intubation
tachypneic with noisy breathing If patient becomes lethargic or somnolent
low oxygen saturation rates Bronchodilator
pale to cyanotic beta2-agonist
hands may be cool and moist anticholinergics
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 1 of 6
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
Diuretics Venous
blood pressure is closely monitored Arterial
intake and output, daily weights, serum Types of bleeding
electrolytes, and creatinine are carefully External hemorrhage
monitored. Internal hemorrhage
Vasodilators
contraindicated in patients who are hypotensive ETIOLOGY
IV nitroglycerin External hemorrhage may be caused by:
Nitroprusside penetrating trauma
Positive inotropic agents lacerations
Treatment of myocardial dysfunction Internal hemorrhage
enhance contractility blunt or penetrating trauma
promote vasoconstriction in peripheral vessels blood dyscrasias
digoxin ruptured aortic aneurysm
amrinone
Antiarrhythmics PATHOPHYSIOLOGY
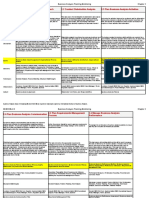
decreased cardiac output lead to hypovolemic shock
decrease peripheral vascular resistance, preload, filling of the vascular compartment; it occurs when
and afterload 15% to 20% of circulating blood volume is loss.
Morphine A loss of effective circulating blood volume causes:
reduce anxiety and dyspnea inadequate organ
dilate the systemic venous bed
can compromise respirations
resuscitation equipment available in case the Bleeding
patient stops breathing
NURSING MANAGEMENT Hypovolemia
positioned upright
preferably with the legs dangling over the side of hypoperfusion
the bed
decreasing venous return Cellular anerobic metabolism + Lactic acidosis
decreasing right ventricular SV
decreasing lung congestion ↓coag. proteases
nurse gives the patient simple, concise information in a
reassuring voice
bedside commode Coagulopathy & Hge
decrease the energy required by the patient
monitor urine output ↓tissue perfusion + BS – gut & Muscle↓
indwelling urinary catheter may be inserted
continuous ECG monitoring
frequent measurement of vital signs Underperfused muscle
Administer supplemental oxygen as ordered, first step
in treatment hypothermia
Assess the patient’s condition frequently and document
his or her responses to treatment.
Monitor ABG and pulse oximetry values, and in the HgE hypoperfusion acidosis
patient with a pulmonary artery catheter, pulmonary
end-diastolic and PAWPs
Watch for complications
Monitor vital signs every 15 to 30 minutes while
administering nitroprusside in dextrose 5% in water by
IV drip.
Discard unused nitroprusside solution after 4
hours. tissue perfusion
Watch for arrhythmias in patients receiving digoxin
marked respiratory depression in those receiving
morphine
sodium restrictions and high potassium diet DEATH
HEMORRHAGE
CLINICAL MANIFESTATION
loss of a large amount of blood internally or externally in
a short period. cool, moist skin
Source of bleeding: decreasing blood pressure
Capillary increasing heart rate
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 2 of 6
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
delayed capillary refill BLOOD TRANSFUSION
decreasing urine volume Administration of blood and blood components
Apprehension treat decreased hemoglobin (Hb) level and hematocrit
Signs of internal bleeding (HCT).
Ecchymoses
occult or frank blood in urine PACKED BT
Obvious bleeding from wound or orifices Packed RBCs contain:
cellular debris
used when patient has a normal blood
volume
DIAGNOSTIC FINDINGS Perioperative and emergency blood salvage
decreased hematocrit and hemoglobin (most common indication for bt)
Guaiac testing may detect occult blood in stool. Washed packed RBCs
commonly used for patients previously sensitized
MEDICAL MANAGEMENT to transfusions
I. Fluid Replacement
two large-gauge IV catheters are inserted SELF SUPPLIED BT
in an uninjured extremity autotransfusion or autologous transfusion
Blood samples are obtained for analysis, typing, patient’s own blood is collected, filtrated, and
and cross-matching reinfused.
isotonic electrolyte solutions Autologous transfusion may be indicated for:
colloids elective surgery
blood component therapy nonelective surgery
perioperative and emergency blood salvage
Packed red blood cells
during and after thoracic or cardiovascular surgery
II. Control of External Hemorrhage
and hip, knee, or liver resection
Direct, firm pressure is applied:
perioperative and emergency blood salvage for
over the bleeding area
traumatic injury of the lungs, liver, chest wall,
the involved artery at a site that is proximal to
heart, pulmonary vessels, spleen, kidneys, inferior
the wound
vena cava, and iliac, portal, or subclavian veins
the injured part is elevated to stop venous and
capillary bleeding, if possible. TRANSFUSING BLOOD AND BLOOD COMPONENTS
the extremity is immobilized to control blood loss
If the injured area is an extremity
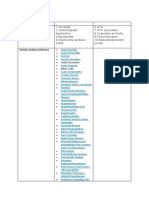
Packed Sed blood cells (rBCs)
tourniquet is applied to an extremity
To restore or maintain oxygen-carrying
when the external hemorrhage cannot be
compatibilityABO and Rh Indications
capacity
controlled in any other way
applied just proximal to the wound To correct anemia and surgical blood loss
The patient is tagged with a skin marking pencil or To increase RBC mass
on adhesive tape on the forehead with a “T,” To improve RBC exchange
stating the location of the tourniquet and the ABO compatibility:
time applied Type A receives type A or O
the tourniquet remains in place until the patient is type B receives type B or O
in the operating room type AB receives type AB or O
suffered a traumatic amputation type O receives type O
Time of tourniquet application and removal should Rh match necessary
be documented
considerationNursing
III. Control of Internal Bleeding Use a blood administration set to infuse
blood within 4 hours.
internal hemorrhage is suspected if:
tachycardia Administer only with normal saline solution.
falling blood pressure Keep in mind that an RBC transfusion isn’t
thirst appropriate for anemias treatable by
apprehension nutritional or drug therapies.
cool and moist skin
leukocyte-poor RBCs
delayed capillary refill
packed RBC, plasma, and platelets are given at a Same as packed RBCs
To prevent febrile reactions from leukocyte
Indications
rapid rate
arterial blood gas specimens are obtained antibodies
evaluate pulmonary function and tissue To treat immunocompromised patients
perfusion To restore RBCs to patients who have had
establish baseline hemodynamic parameters two or more nonhemolytic febrile reactions
supine position
monitored closely until hemodynamic or circulatory
parameters improve
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 3 of 6
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
Nursing ABO and Rh
CompatibilityABO and Rh
Same as packed RBCs ABO compatibility required
Rh match necessary Rh match not required
compatibility
Use blood administration tubing.
It may require a 40-micron filter suitable for Use a blood administration set to infuse.
Nursing consideration
hard-spun, leukocyte-poor RBCs. Add normal saline solution to each bag of
cryoprecipitate, as necessary, to facilitate
consideration
Use only with normal saline solution.
transfusion.
Keep in mind that cells expire 24 hours
after washing. Keep in mind that cryoprecipitate must be
administered within 6 hours of thawing.
Platelets Before administering, check lab studies to
Same as packed RBCs confirm a deficiency of one of the specific
To prevent febrile reactions from leukocyte clotting factors present in cryoprecipitate.
Indications
antibodies Be aware that patients with hemophilia A or
To treat immunocompromised patients vonVIII
Factor Willebrand’s
concentratedisease should only be
Recombinant
To restore RBCs to patients who have had To treat hemophilia A
Indications
two or more nonhemolytic febrile reactions To treat von Willebrand's disease
compatibilityABO and Rh
ABO identical when possible
Rh-negative recipients should receive Rh
negative platelets when possible
Administer by I.V. injection using a filter
needle or use the administration set
supplied by the manufacturer.
considerationNursing
Use a filtered component drip
administration set to infuse.
If ordered, administer prophylactic
pretransfusion medications, such as
antihistamines or antipyretics, to reduce Albumin 5% (buffered saline)
chills, fever, and allergic reactions. To replace volume lost because of shock
Complete transfusion within 20 minutes or from burns, trauma, surgery, or infections
Fresh frozen plasma (FFP) Uncoagulated
Indications
To treat hypoproteinemia (with or without
To correct a coagulation factor deficiency edema)
To replace a specific factor when that factor
Indications
isn't available
To reverse Warfarin
To treat thrombotic thrombocytopenic
considerationNursing
purpura Use the administration set supplied by the
manufacturer and set rate based on patient
compatibilityABO and Rh
ABO compatibility required
condition and response.
Rh match not required Keep in mind that albumin isn’t to be used
to treat severe anemia.
Administer cautiously in cardiac and
pulmonary disease because heart failure
may result from volume overload.
considerationNursing
Use a blood administration set.
TRANSFUSION OF PACKED RED BLOOD CELLS
Complete transfusion within 20 minutes or
I. Preprocedure
at the fastest rate the patient can tolerate.
Confirm that the transfusion has been prescribed
Monitor patient for signs and symptoms of
hypocalcemia because the citric acid in Check that patient’s blood has been typed and
FFP may bind to calcium. cross-matched.
Remember that FFP must be infused within Verify that patient has signed a written consent
Cryoprecipitate Insoluble plasma portion of FFP form
To treat factor VIII deficiency and fibrinogen Explain procedure to patient
disorders Take patient’s temperature, pulse, respiration,
Indications
To treat significant factor XIII deficiency blood pressure and assess fluid volume status
Note if signs of increased fluid overload present
Use hand hygiene and wear gloves
Use appropriately sized needle for insertion in a
peripheral vein
Use blood filter to screen out fibrin clots
Do not vent blood container
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 4 of 6
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
II. Procedure Check blood product for any unusual color or
Obtain packed red blood cells after the IV line is clumps
started Make sure that platelets or FFP units are given
Double-check labels with another nurse or immediately after they are obtained
physician Infuse each unit of FFP over 30–60 minutes per
Confirm patient’s identification patient tolerance
Check blood for gas bubbles and any unusual Infuse each unit of platelets as fast as patient can
color or cloudiness tolerate to diminish platelet clumping during
Make sure that PRBC transfusion is initiated within administration.
30 minutes Observe patient closely throughout transfusion for
after removal of PRBCs from blood bank any signs of adverse reaction
refrigerator. Monitor vital signs at the end of transfusion
For the first 15 minutes, run the transfusion slowly Flush line with saline after transfusion
—no faster than 5 mL/min. III. Postprocedure
If no adverse effects occur during the first 15 Obtain vital signs and auscultate breath sounds
minutes, increase the flow rate unless patient Dispose of used materials properly
is at high risk for circulatory overload Document procedure in patient’s medical record
Monitor closely for 15–30 minutes to detect signs Monitor patient for response to and effectiveness
of reaction of procedure
Note that administration time does not exceed 4 platelet count may be ordered 1 hour after
hours because of increased risk of bacterial platelet transfusion
proliferation. If patient is at risk for transfusion-associated
Be alert for signs of adverse reactions circulatory overload
Change blood tubing after every 2 units monitor closely for 6 hours after transfusion
decrease chance of bacterial contamination
III. Postprocedure On additional information:
Obtain vital signs and breath sounds 1. FFP requires ABO but not Rh compatibility
If signs of increased fluid overload present 2. Platelets are not typically crossmatched for ABO
Diuretic compatibility.
Dispose of used materials properly 3. Never add medications to blood or blood products.
Document procedure in patient’s medical record
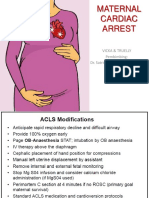
Monitor patient for response to and effectiveness CARDIAC ARREST
of procedure. the heart is unable to pump and circulate blood to the
If, patient is at risk, monitor for at least 6 body’s organs and tissues
hours for signs of transfusion transfusion- caused by a dysrhythmia
associated circulatory overload pulseless electrical activity
monitor for signs of delayed hemolytic
reaction ETIOLOGY
acute MI
On additional information: V-fib
1. Never add medications to blood or blood products
V-tach
2. if blood is too thick to run freely, normal saline may be
severe trauma
added to the unit
3. If blood must be warmed, use an inline blood warmer with hypovolemia
a monitoring system. metabolic disorders
brain injury
TRANSFUSION OF PLATELETS OR FRESH-FROZEN respiratory arrest
PLASMA drowning
I. Preprocedure drug overdose
Confirm that the transfusion has been prescribed
Verify that patient has signed a written consent CLINICAL MANIFESTATION
form ineffective respiratory gasping
Explain procedure to patient pupils of the eyes begin dilating in less than a minute
Take patient’s VS seizures may occur
Note if signs of increased fluid overload present Pallor and cyanosis
Use hand hygiene and wear gloves Immediate loss of consciousness
Use a 22-gauge or larger needle for placement in Absence of palpable pulses and heart sounds
a large vein
II. Procedure
Obtain platelets or fresh-frozen plasma (FFP) from NURSING MANAGEMENT
the blood bank Determine responsiveness and notify the practitioner
Double-check labels with another nurse or and resuscitation team.
physician Initiate CPR.
Monitor cardiac rhythm.
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 5 of 6
NURS 19 Pulmonary Edema, Hemorrhage, Cardiac arrest
AY 2021- 09/16/2021
2022
Midterm Exam
Assist with ET intubation and mechanical ventilation.
Follow ACLS protocols; administer medications as
ordered.
Assist with defibrillation for ventricular fibrillation or
pulseless ventricular tachycardia.
Administer a patent I. V. line if it is not already in place.
Administer emergency drugs, as ordered.
Provide client and family teaching
Promote family coping.
Address the possibility of organ donation with the
client's family, keeping in mind that this is a difficult time
for them.
PERAS, L. Pulmonary Edema, Hemorrhage, Cardiac arrest 6 of 6
You might also like
- Undercover by John Bevere TagalogDocument5 pagesUndercover by John Bevere TagalogAngela Bainca Amper86% (21)
- Internal Medicine NotesDocument54 pagesInternal Medicine NotesHayley Welsh75% (4)
- General and Specific ObjectivesDocument8 pagesGeneral and Specific ObjectivesBea Simagala95% (21)
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- General PsychologyDocument4 pagesGeneral PsychologyDaniel C. Dequiña100% (1)
- Toronto Notes Respirology PDFDocument40 pagesToronto Notes Respirology PDFJaya Semara Putra75% (4)
- Afib NCPDocument3 pagesAfib NCPGen RodriguezNo ratings yet
- Congestive Heart Failure Pathophysiology Schematic DiagramDocument3 pagesCongestive Heart Failure Pathophysiology Schematic DiagramJasleen KaurNo ratings yet
- Neonatal Heart DiseaseDocument8 pagesNeonatal Heart DiseaseDelphy VargheseNo ratings yet
- Elearning in Aviation SuzanneDocument35 pagesElearning in Aviation SuzannejuanNo ratings yet
- Activity #3: Pathophysiology and Nursing Care PlanDocument6 pagesActivity #3: Pathophysiology and Nursing Care PlanMonette Abalos MendovaNo ratings yet
- Pulmonary Edema: Moderator - Asso Prof DR Arun Kumar Presentor - DR Kannan GDocument39 pagesPulmonary Edema: Moderator - Asso Prof DR Arun Kumar Presentor - DR Kannan GGrace JasminNo ratings yet
- Congestive Heart Failure (CHF) : Causes DiagnosisDocument6 pagesCongestive Heart Failure (CHF) : Causes DiagnosisSOPHIA LOISE TEJANO FULACHENo ratings yet
- Patent Ductus Arteriosus 6. Aortic Stenosis: Signs and Symptoms: Signs and SymptomsDocument3 pagesPatent Ductus Arteriosus 6. Aortic Stenosis: Signs and Symptoms: Signs and SymptomsKIANA LOUISE ROMANONo ratings yet
- Sindromatologi DyspneuDocument18 pagesSindromatologi DyspneuMeylan TaebenuNo ratings yet
- Cor Pulmonale PATHOPHYSIOLOGYDocument2 pagesCor Pulmonale PATHOPHYSIOLOGYChloie Marie RosalejosNo ratings yet
- Pathophysiology 1Document5 pagesPathophysiology 1Genevive Alcantara MartinNo ratings yet
- Resp 180214084710Document72 pagesResp 180214084710Karla Geraldine Carhuas VeliNo ratings yet
- IM-Heart Failure Concept MapDocument16 pagesIM-Heart Failure Concept MapTrisNo ratings yet
- 03 CopdDocument7 pages03 CopdahmedNo ratings yet
- Acute Respiratory Distress Syndrome - NursingDocument14 pagesAcute Respiratory Distress Syndrome - Nursingyellowbyuns0% (1)
- Ahmad Soboh - Bridging PBL Midterm ExamDocument42 pagesAhmad Soboh - Bridging PBL Midterm ExamAhmad SobihNo ratings yet
- Pathophysiology-LCHFDocument2 pagesPathophysiology-LCHFNicole Villanueva, BSN - Level 3ANo ratings yet
- Group 1 6 Problem Emergency Medicine Block Monday, 30 Oct 2017Document121 pagesGroup 1 6 Problem Emergency Medicine Block Monday, 30 Oct 2017Jonathan TandajuNo ratings yet
- CHF PathoDocument2 pagesCHF PathoZy HallasgoNo ratings yet
- Maternal Cardiac ArrestDocument28 pagesMaternal Cardiac ArrestTruelly ChanantaNo ratings yet
- PathophysiologyDocument34 pagesPathophysiologyeunams_1195% (20)
- Acute Respiratory Distress Syndrome (ARDS) : Chest X-Ray Chest CT Scan BronchosDocument4 pagesAcute Respiratory Distress Syndrome (ARDS) : Chest X-Ray Chest CT Scan BronchosJulyan ValenzaNo ratings yet
- 15 - Respiratory FailureDocument33 pages15 - Respiratory FailureSelin SakarNo ratings yet
- Acute Pulmonary Oedema: D S J B. CDocument6 pagesAcute Pulmonary Oedema: D S J B. CAmatystNo ratings yet
- Internal Medicine NotesDocument54 pagesInternal Medicine NotesKiara Govender100% (1)
- Supan-Clinical Case AnalysisDocument7 pagesSupan-Clinical Case AnalysisAjay SupanNo ratings yet
- Power Point Panic AttackDocument7 pagesPower Point Panic Attackfrancis00090No ratings yet
- Gagal NapasDocument49 pagesGagal NapasimaderadityaNo ratings yet
- Dyspnoea 2Document1 pageDyspnoea 2Shubham TarapureNo ratings yet
- P EmbolismDocument29 pagesP EmbolismCommandoCitotz100% (2)
- Pemicu 6 KGD AldiDocument134 pagesPemicu 6 KGD AldiFirdaus AldyNo ratings yet
- Congenital Heart DisorderDocument4 pagesCongenital Heart DisorderElle RosalesNo ratings yet
- Acute Respiratory Failure Concept MapDocument1 pageAcute Respiratory Failure Concept Mapjenievysenerez100% (1)
- Heart FailureDocument7 pagesHeart FailureLovely CacapitNo ratings yet
- Under Supervision DR/ Mariam Sabry: Ulmonary DemaDocument28 pagesUnder Supervision DR/ Mariam Sabry: Ulmonary DemaMohamed ElsyaedNo ratings yet
- Dyspnea - DR AllenDocument50 pagesDyspnea - DR AllenalmiraerickaiNo ratings yet
- Neonatal EmergenciesDocument21 pagesNeonatal EmergenciesRNo ratings yet
- Pulmonary EdemaDocument50 pagesPulmonary EdemaStacy LuceroNo ratings yet
- All PathoDocument2 pagesAll PathoroseasNo ratings yet
- Pulmonary Edema: Topic OutlineDocument2 pagesPulmonary Edema: Topic OutlineKdamnz100% (1)
- CAD NCP Decreased Cardiac OutputDocument3 pagesCAD NCP Decreased Cardiac OutputLeizel Apolonio100% (3)
- Symptoms of CvsDocument25 pagesSymptoms of CvsstudymedicNo ratings yet
- Essential Basics of General Medicine Faculty of Dentistry Cairo UniversityDocument104 pagesEssential Basics of General Medicine Faculty of Dentistry Cairo Universitybavly waidyNo ratings yet
- Institute of Nursing: Far Eastern UniversityDocument3 pagesInstitute of Nursing: Far Eastern UniversityaleccespirituNo ratings yet
- Approach To DyspneaDocument9 pagesApproach To DyspneaMuhammad LukmanNo ratings yet
- 2023 UsDocument10 pages2023 UswisgeorgekwokNo ratings yet
- Problem Based Learning Cardiovascular System: 2nd GroupDocument47 pagesProblem Based Learning Cardiovascular System: 2nd GroupClaudia Narinda R. PNo ratings yet
- LI 8 - Differential Diagnosis of Acute Heart FailureDocument11 pagesLI 8 - Differential Diagnosis of Acute Heart Failure19-034 Jefry Junaidi PurbaNo ratings yet
- Disnea - Rosen - 230526 - 125351Document10 pagesDisnea - Rosen - 230526 - 125351Pablo BetancourtNo ratings yet
- Pathophysiology DyspneaDocument1 pagePathophysiology DyspneaJoseph LimNo ratings yet
- Congestive Heart Failure BloodDocument27 pagesCongestive Heart Failure BloodmarvinawatiNo ratings yet
- Diagnostic Diferential Medicina InternaDocument6 pagesDiagnostic Diferential Medicina InternaLary ArNo ratings yet
- ARDS (Acute Respiratory Distress Syndrome) : EarlyDocument1 pageARDS (Acute Respiratory Distress Syndrome) : EarlyDora Elena HurtadoNo ratings yet
- Pulmonary Embolism: Presented By: Miss. M.K.Kaku Nursing TutorDocument9 pagesPulmonary Embolism: Presented By: Miss. M.K.Kaku Nursing TutorKaku ManishaNo ratings yet
- Perivascular DiseasesDocument5 pagesPerivascular DiseasesKathleen Ellize BetchaydaNo ratings yet
- Supplementary Material 1c Acute Respiratory FailureDocument5 pagesSupplementary Material 1c Acute Respiratory FailureJanela Chriselle B. TICARNo ratings yet
- ACC Jimmy AsafDocument152 pagesACC Jimmy AsafFikriYTNo ratings yet
- CHF and CardiomyopathiesDocument8 pagesCHF and CardiomyopathiesDan HoNo ratings yet
- Playground Design: Bridges in Mathematics Grade 4 Unit 8Document2 pagesPlayground Design: Bridges in Mathematics Grade 4 Unit 8api-289120259No ratings yet
- Affidavit of Susie Barlow Describing Experiences in FLDSDocument5 pagesAffidavit of Susie Barlow Describing Experiences in FLDSborninbrooklyn100% (1)
- Simon The Sportsman: Activity TypeDocument3 pagesSimon The Sportsman: Activity TypeEkaterina DatsenkoNo ratings yet
- Jamaica Cultural Immersion Program FINALDocument2 pagesJamaica Cultural Immersion Program FINALLinda zubyNo ratings yet
- BABOK V2 - All ChaptersDocument20 pagesBABOK V2 - All ChaptersSmith And YNo ratings yet
- APAC LocalizationsDocument15 pagesAPAC LocalizationsDhinakaranNo ratings yet
- Case Study RubricDocument2 pagesCase Study Rubricreem.alrshoudiNo ratings yet
- The New Elliot Wave RuleDocument40 pagesThe New Elliot Wave RuleUlisses76100% (3)
- Top 10 Machine Learning AlgorithmsDocument12 pagesTop 10 Machine Learning AlgorithmsUmang SoniNo ratings yet
- Research Proposal G5Cheating Behavior in ExamR 03Document44 pagesResearch Proposal G5Cheating Behavior in ExamR 03Davidson BravoNo ratings yet
- Endocrine System ActivityDocument5 pagesEndocrine System ActivityDavid IzaguirreNo ratings yet
- The Cask of AmontilladoDocument43 pagesThe Cask of AmontilladoZechaina Udo100% (2)
- Agilent 54600B Oscilloscope Data SheetDocument8 pagesAgilent 54600B Oscilloscope Data SheetAlejandro CasasNo ratings yet
- Cath SAP 5Document47 pagesCath SAP 5Angel AliNo ratings yet
- Characteristics That Define Our VictoryDocument5 pagesCharacteristics That Define Our VictoryLouie BiasongNo ratings yet
- Partisan Politics and Public Finance: Changes in Public Spending in The Industrialized Democracies, 1955-1989Document21 pagesPartisan Politics and Public Finance: Changes in Public Spending in The Industrialized Democracies, 1955-1989SumardiNo ratings yet
- AlstomGroup - JD For Software EngineerDocument3 pagesAlstomGroup - JD For Software EngineerPraveen PremachandranNo ratings yet
- The Knowledge of First AidDocument9 pagesThe Knowledge of First AidMoon MyNo ratings yet
- Illustrated Catalogue of The Historical and World-Renowned Collection of Torture Instruments, Etc. From The Royal Castle of NurembergDocument104 pagesIllustrated Catalogue of The Historical and World-Renowned Collection of Torture Instruments, Etc. From The Royal Castle of NurembergCesar Maxiumivich Montoya100% (2)
- Filología Neotestamentaria 50 - V.v.a.ADocument184 pagesFilología Neotestamentaria 50 - V.v.a.AGaspard de la Nuit100% (1)
- Richik Dadhich 1742 Ugiv Crime and Punishment CA3Document3 pagesRichik Dadhich 1742 Ugiv Crime and Punishment CA3Richik DadhichNo ratings yet
- Outline and Notes - Biography of The Dollar-KarminDocument7 pagesOutline and Notes - Biography of The Dollar-KarminBankingLinguisticCheckmatesNo ratings yet
- Intro To Genetic EngineeringDocument84 pagesIntro To Genetic EngineeringMhimi ViduyaNo ratings yet
- PUBLIC LEADERSHIP (1) NewDocument13 pagesPUBLIC LEADERSHIP (1) NewHanief GuswantoroNo ratings yet
- Kuwait - Trademark Law No. 68 of 1980Document7 pagesKuwait - Trademark Law No. 68 of 1980Ramesh KannanNo ratings yet
- Leppänen Et Al. - 2023 - When Do Novel Business Models Lead To High Performance A Configurational Approach To Value DriversDocument31 pagesLeppänen Et Al. - 2023 - When Do Novel Business Models Lead To High Performance A Configurational Approach To Value Driverspeterrammel97No ratings yet