Professional Documents
Culture Documents
Palupi - Jurnal EBN
Palupi - Jurnal EBN
Uploaded by
sri lestariCopyright:
Available Formats
You might also like
- Test Bank For Oral Pharmacology For The Dental Hygienist 2nd Edition 2 e Mea A Weinberg Cheryl Westphal Theile James Burke FineDocument16 pagesTest Bank For Oral Pharmacology For The Dental Hygienist 2nd Edition 2 e Mea A Weinberg Cheryl Westphal Theile James Burke Finexavianhatmgzmz9No ratings yet
- Complementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)From EverandComplementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)No ratings yet
- Basic Training For: Barangay Health Workers Barangay Nutrition ScholarDocument16 pagesBasic Training For: Barangay Health Workers Barangay Nutrition ScholarMario Hipolito100% (5)
- NBHS 1104 Topic 1Document16 pagesNBHS 1104 Topic 1hema angleNo ratings yet
- BMJ 33 2 193Document5 pagesBMJ 33 2 193Ami Novianti SubagyaNo ratings yet
- Hypertonic (3%) Saline Vs 0.9% Saline Nebulization For Acute Viral Bronchiolitis: A Randomized Controlled TrialDocument5 pagesHypertonic (3%) Saline Vs 0.9% Saline Nebulization For Acute Viral Bronchiolitis: A Randomized Controlled TrialMukesh Kumar GuptaNo ratings yet
- Solucion A en BronquiolitisDocument6 pagesSolucion A en BronquiolitisLuis Sanchez CarranzaNo ratings yet
- Pneumonia 5Document6 pagesPneumonia 5furqan92No ratings yet
- Bersihan MukosilierDocument58 pagesBersihan MukosilierbennyrolandnababanNo ratings yet
- Wet CoughDocument2 pagesWet CoughphobicmdNo ratings yet
- Clinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceDocument5 pagesClinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceSarah DaniswaraNo ratings yet
- Medical Therapeutics Journal Appraisal 3B 2009-70197: 1. Is It Relevant?Document4 pagesMedical Therapeutics Journal Appraisal 3B 2009-70197: 1. Is It Relevant?Maria Christina SalazarNo ratings yet
- Pemilihan Terapi Empirik Pada Balita Pneumonia Berdasarkan Lama Rawat (Lenght of Stay/Los) Dan Komplikasi Dari Gambaran RadiologiDocument8 pagesPemilihan Terapi Empirik Pada Balita Pneumonia Berdasarkan Lama Rawat (Lenght of Stay/Los) Dan Komplikasi Dari Gambaran RadiologiChristyNatalytaTariganNo ratings yet
- Boursiani 2017Document5 pagesBoursiani 2017Carlos Urkieta MonetaNo ratings yet
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoNo ratings yet
- Early Versus Late Caffeine Therapy Administration in Preterm Neonates An Updated Systematic Review and Meta-AnalysisDocument10 pagesEarly Versus Late Caffeine Therapy Administration in Preterm Neonates An Updated Systematic Review and Meta-AnalysisFrancisco C. Belloso HornaNo ratings yet
- Early N Late Caffein TherapyDocument10 pagesEarly N Late Caffein TherapyasritasuriNo ratings yet
- Chamnanvanakij, 2005Document6 pagesChamnanvanakij, 2005Fatma ElzaytNo ratings yet
- The Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalDocument7 pagesThe Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalZablon KodilaNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyJonathan MarkNo ratings yet
- 2 PBDocument4 pages2 PBSuryati HusinNo ratings yet
- Paediatric Pneumonia 2016 - 17Document13 pagesPaediatric Pneumonia 2016 - 17JENNY MARGOT HIDALGO QUISPENo ratings yet
- Tachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionDocument2 pagesTachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionAli BabaNo ratings yet
- Evidence Based Nursing: Batch 2011Document7 pagesEvidence Based Nursing: Batch 2011Eimhie Lee CasiNo ratings yet
- Characteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDocument8 pagesCharacteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDrnNo ratings yet
- Journal Pediatric IndiaDocument5 pagesJournal Pediatric IndiaHhhNo ratings yet
- The Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine OsmolalityDocument7 pagesThe Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine Osmolalitysafdar aliNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- Post-Standardization of Routine Creatinine Assays Are They Suitable Foir Clinical ApplicationsDocument9 pagesPost-Standardization of Routine Creatinine Assays Are They Suitable Foir Clinical ApplicationsmichelNo ratings yet
- Dr. Tofayel Ahmed IMO Department of Paediatrics, JRRMCHDocument26 pagesDr. Tofayel Ahmed IMO Department of Paediatrics, JRRMCHTofayel AhmedNo ratings yet
- Clinical Analisis of Sputum Gram StainsDocument7 pagesClinical Analisis of Sputum Gram Stainspelcastre r.No ratings yet
- Evaluation Lung B LineDocument1 pageEvaluation Lung B LineBhanu KumarNo ratings yet
- Efficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisDocument4 pagesEfficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisFiaz medicoNo ratings yet
- Utility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDocument6 pagesUtility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDr. Asaad Mohammed Ahmed BabkerNo ratings yet
- Journal Pediatric Shock BaruDocument6 pagesJournal Pediatric Shock BaruHhhNo ratings yet
- Steroids For Airway EdemaDocument7 pagesSteroids For Airway EdemaDamal An NasherNo ratings yet
- Corticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Document8 pagesCorticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Bela Bagus SetiawanNo ratings yet
- Articulos BronquiolitisDocument18 pagesArticulos BronquiolitisLaura López Del Castillo LalydelcaNo ratings yet
- Jurnal 3Document5 pagesJurnal 3Anonymous Us5v7C6QhNo ratings yet
- 1 s2.0 S0272638619311151 MainDocument17 pages1 s2.0 S0272638619311151 Main吴善统No ratings yet
- Jurnal ThyphoidDocument10 pagesJurnal ThyphoidAndrea ChristantyNo ratings yet
- Jurnal TBCDocument6 pagesJurnal TBCLorinsya Ollin100% (1)
- Alammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalDocument8 pagesAlammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalTinara HusniaNo ratings yet
- Alammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalDocument8 pagesAlammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalTinara HusniaNo ratings yet
- Parkinson IJSRDocument5 pagesParkinson IJSRtyaguspritaNo ratings yet
- A Study On Ventilator Associated Pneumonia inDocument4 pagesA Study On Ventilator Associated Pneumonia inAl MuzakkiNo ratings yet
- Hidrocortisona Vs Choque SepticoDocument12 pagesHidrocortisona Vs Choque SepticoMarisolCamposNo ratings yet
- NIH Public Access: Corticosteroids For Bacterial KeratitisDocument19 pagesNIH Public Access: Corticosteroids For Bacterial KeratitisDede YadedeNo ratings yet
- Journal Homepage: - : IntroductionDocument3 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Targeted O2 Neonatal ResusDocument13 pagesTargeted O2 Neonatal ResusWikan SariNo ratings yet
- Children NebulizerDocument8 pagesChildren NebulizerAnggi CalapiNo ratings yet
- Can Lactate Clearance Predict Mortality in Critically Ill Children?Document6 pagesCan Lactate Clearance Predict Mortality in Critically Ill Children?Sam Aguilar FigueroaNo ratings yet
- Antimicrobial Agent and ChemoteraphyDocument4 pagesAntimicrobial Agent and ChemoteraphyRaina96No ratings yet
- Randomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDocument5 pagesRandomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDiego AndradeNo ratings yet
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaNo ratings yet
- Does Combined Oral Dexamethasone 2011Document3 pagesDoes Combined Oral Dexamethasone 2011Diana Vanessa SuarezNo ratings yet
- 2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisDocument15 pages2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisPamela Mamani FloresNo ratings yet
- GoogleDocument13 pagesGooglesintaraNo ratings yet
- Zgddekzz 23 11 1097Document6 pagesZgddekzz 23 11 1097arieza nur pratamaNo ratings yet
- Gobi NathDocument5 pagesGobi NathRaihan IlyasaNo ratings yet
- Penundaan Pemotongan TalipusatDocument14 pagesPenundaan Pemotongan Talipusatmaya maeNo ratings yet
- Las Nebulizaciones Con Solucion Salina HipertonicaDocument6 pagesLas Nebulizaciones Con Solucion Salina HipertonicaAlisson De Berduccy TroncosoNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Power Point Consumer Health EducationDocument81 pagesPower Point Consumer Health EducationAlbert Ian CasugaNo ratings yet
- Functional Capacity&Lung FunctionDocument11 pagesFunctional Capacity&Lung Functionandika pradanaNo ratings yet
- Bio T4 DLP KSSM Chapter 11Document59 pagesBio T4 DLP KSSM Chapter 11fadilahNo ratings yet
- MBBS Pain Symposium 2022Document10 pagesMBBS Pain Symposium 2022Morgan BaileyNo ratings yet
- Systemic and Local Applications of Steroids in Endodontics: An Update ReviewDocument8 pagesSystemic and Local Applications of Steroids in Endodontics: An Update ReviewJorge OrbeNo ratings yet
- Brokenshire College: Form C. Informed Consent Assessment FormDocument2 pagesBrokenshire College: Form C. Informed Consent Assessment Formgeng gengNo ratings yet
- R.A. No. 11223 - Universal Health Care ActDocument5 pagesR.A. No. 11223 - Universal Health Care ActCeline100% (2)
- Medical Devices Act - M 3 en PDFDocument42 pagesMedical Devices Act - M 3 en PDFDewa GedeNo ratings yet
- Apollo Proton Cancer Centre (Medical Oncology) For Kenyan PatientsDocument10 pagesApollo Proton Cancer Centre (Medical Oncology) For Kenyan PatientsApollo Information CentreNo ratings yet
- Jointly Team: SMLE GroupDocument22 pagesJointly Team: SMLE GroupAkpevwe EmefeNo ratings yet
- Sindrom Reconstructive ImunaDocument7 pagesSindrom Reconstructive ImunaAlexandra PaunNo ratings yet
- American Handbook of Psychiatry - Volume I - The Foundations of PsychiatryDocument3,272 pagesAmerican Handbook of Psychiatry - Volume I - The Foundations of Psychiatrydark thanos100% (2)
- Pascual Janine Krista E. NCPDocument3 pagesPascual Janine Krista E. NCPCzarina Mae LomboyNo ratings yet
- Pathophysiology of Acute Renal FailureDocument2 pagesPathophysiology of Acute Renal Failureminangsung minangnengNo ratings yet
- Scrotal Swelling FadhlyDocument52 pagesScrotal Swelling FadhlyfadhlyNo ratings yet
- RPD NewDocument4 pagesRPD Newapi-632682404No ratings yet
- DocxDocument12 pagesDocxJojo JacobNo ratings yet
- Bwdi DR, Chemist&Stp Final ListDocument226 pagesBwdi DR, Chemist&Stp Final ListzaheerbcNo ratings yet
- Encefalopatía Hepatica PDFDocument7 pagesEncefalopatía Hepatica PDFsukardo5426No ratings yet
- AlzheimerDocument2 pagesAlzheimerCho HyeyeonNo ratings yet
- Case Presentation: BY MeghaDocument13 pagesCase Presentation: BY Meghalibrian_pallavi3942No ratings yet
- Maya Rotation ChecklistDocument1 pageMaya Rotation Checklistapi-434982019No ratings yet
- Prof. Services v. AganaDocument77 pagesProf. Services v. AganaRechel De TorresNo ratings yet
- Al Jabry Pharmacy LLC: Deef Pharmaceutical Industries Co. KsaDocument1 pageAl Jabry Pharmacy LLC: Deef Pharmaceutical Industries Co. Ksamdgayas70No ratings yet
- Delirium and Acute Confusional States - Prevention, Treatment, and Prognosis - UpToDateDocument18 pagesDelirium and Acute Confusional States - Prevention, Treatment, and Prognosis - UpToDateKarina CabayNo ratings yet
- Lung Cancer Pathology and DiagnosisDocument28 pagesLung Cancer Pathology and DiagnosismadvincyNo ratings yet
- Instrucciones Post Extraccion INGLESDocument1 pageInstrucciones Post Extraccion INGLESAlessandro Matias GonzalezNo ratings yet
Palupi - Jurnal EBN
Palupi - Jurnal EBN
Uploaded by
sri lestariOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Palupi - Jurnal EBN
Palupi - Jurnal EBN
Uploaded by
sri lestariCopyright:
Available Formats
822
RESEARCH ARTICLE
Comparison of 3% saline and 0.9% normal saline nebulization as diluent in
children with bronchiolitis
Shobha Sapkota1, Ammara Kaleem2, Suffura Huma3, Muhammad Aleem Ud Din4, Shabbir Ahmad5, Sobia ShahAlam6
Abstract
Objective: To compare the outcome in terms of mean time to disappearance of cough, wheezing, crackles and length of
hospital stay in patients treated with sodium chloride 3% with sodium chloride 0.9% as nebulisation diluent in children for
suffering from bronchiolitis.
Methods: The prospective study was conducted at the Department of Paediatric Medicine Sheikh Zayed Hospital, Lahore,
Pakistan, from November 2014 to April 2015, and comprised children aged between 6 weeks and 24 months having
bronchiolitis. Group A received 3% sodium chloride and Group B received 0.9% of the same solution. Duration of cough,
wheezing, crackles and duration of stay at hospital were compared between the groups. Data was analysed using SPSS 17.
Results: Of the 100 patients, there were 50(50%) in Group A with a mean age of 7.17±4.46 months, and as many in Group
B with a mean age of 6.6±3.74 months. Overall, there were 55(55%) boys and 45(45%) girls. Mean cough and wheezing
remission time as well as length of hospital stay was significantly different between the groups (p<0.05).
Conclusion: In children having bronchiolitis, 3% saline as nebuliser solution was found to be more effective than 0.9% saline
solution.
Keywords: 3% saline solution, Bronchiolitis, Wheezing, Crepitations, Hospital stay. (JPMA 71: 822; 2021)
DOI: https://doi.org/10.47391/JPMA.569
Introduction nature of the mucus. It also rehydrates mucus secretion
Respiratory syncytial virus is commonly responsible for through water-flow and stimulates by releasing
causing bronchiolitis in paediatric patients aged <1 year. prostaglandin.6 Further, theoretically, it is helpful for
Infants aged <3 years are more prone to having reducing bronchial wall oedema. It is economical in the
complications related to disease nature. Premature babies, way of shorter hospital stay and low cost of treatment.7
chronic lung disease, heart defects, overcrowding and There is no local data, but international data shows
exposing the baby to smoke are well-established risk conflicting results to show which of the diluents is better.
factors complicating the disease.1 Supportive measures, Cochrane meta-analysis comprising 28 trials reported 14%
including hydration, oxygenation and continuing feed, are less hospitalisation with hypertonic saline, and the hospital
the mainstay of treatment.2 Research has enumerated stay was 10 hours shorter with hypertonic saline.7 One
variation in results regarding investigation, management, study reported less time for stay in hospital with 3% sodium
admission to hospital and duration of time spent in hospital chloride (NaCl) solution.8 Howeever, two studies2,9 while
in patients of bronchiolitis, and, hence, there is room for comparing hypertonic saline and normal saline both with
improvement in disease management.3 Adrenaline, salbutamol showed no significant benefit. The current
bronchodilators, corticosteroids, anti-cholinergic, anti- study was planned to compare the outcome in terms of
bacterial, physical therapy for lung and pulmonary mean time to disappearance of cough, wheezing, crackles
surfactant have been components of intervention so far. and length of hospital stay in paediatric bronchiolitis
Precise and specific treatment of bronchiolitis is under patients treated with NaCl 3% and NaCl 0.9%.
debate among experts and is not supported by recent
inconclusive data.4 Patients and methods
Many studies are in favour of beneficial effects of The prospective study was conducted at the Department
hypertonic 3% saline for the treatment of bronchiolitis as of Paediatrics, Sheikh Zayed Hospital, Lahore, Pakistan,
it increases the clearance of mucus5 by breaking the ionic from November 2014 to April 2015.
bonds in the mucus, decreasing the thickness and elastic After approval from the institutional ethics review
committee, the sample size was calculated at 95%
1Kirtipur Hospital, Kathmandu, Nepal; 2,3,5Azra Naheed Medical College, Lahore,
confidence interval (CI), 80% power of test with an
Pakistan; 4Sahara Medical College, Narowal, Pakistan; 6Ghurki Trust Teaching expected duration of hospital stay taken from literature.10
Hospital, Lahore, Pakistan. The smaple was raised from among the in-patients using
Correspondence: Ammara Kaleem. Email: ammarakaleem08@hotmail.com
Vol. 71, No. 3, March 2021
823 S. Sapkota, A. Kaleem, S. Huma, et al.
consecutive convenient sampling method. Those included Table-1: Baseline characteristics.
were bronchiolitis patients with age between 6 weeks and Variables 0.9% saline group 3% saline group p-value
24 months of either gender. Those excluded were children (n=50) (n=50)
having any underlying cardiovascular disease by history Age (months) 0-6 30(60%) 25(50%) 0.256
and medical record, prior history of wheezing, history of 6-12 17(34%) 17(34%)
eczema, allergies of the respiratory tract, including asthma >12 3(6%) 8(16%)
and rhinitis, hypoxia with oxygen saturation (SpO2) <85% Mean±SD 6.6±3.74 7.17±4.46
without oxygenation by pulse oximetry, deterioration in Gender Male 27(54%) 28(56%) 0.841
consciousness, Glasgow Coma Scale (GCS) <15/15, use of Female 23(46%) 22(44%)
bronchodilators within the preceding four hours, use of Gestation Preterm 10(20%) 14(28%) 0.349
Term 40(80%) 36(72%)
corticosteroids therapy within the preceding 48 hours,
Weight(kg) <5th percentile 11(22%) 18(36%) 0.516
consolidation of lungs on X-ray chest and family history of >5th percentile 39(78%) 32(64%)
asthma, atopy. Mean ±SD 6.67±2.52 7.04±3.24
Height (cm) <5th percentile 5(10%) 10(20%) 0.965
No randomisation was done. After informed consent was
>5th percentile 45(90%) 40(80%)
taken from each child’s parent in the local language, the Mean ±SD 66.30±6.25 66.36±7.25
subjects were divided into Group A 3% NaCl nebulisation Oxygen saturation 93.18±3.46 94.40±3.49 0.079
and Group 2 0.9% NaCl nebulisation. Nebulization was
cm: Centimetre, kg: Kilograms, SD: Standard deviation
done by 2ml of the diluent in addition to salbutamol 2.5mg
after every four hours. Nebulisations were supported with Table-2: Results of disappearance of symptoms and time period of stay in hospital in
both groups.
oxygen inhalation at 6-8 litre per min. Treatment was
provided till the patient was allowed to go home. Variables 0.9% saline group 3% saline group p-value
Disappearance of wheeze(mean days) 2.9±0.8 1 2.47±0.72 0.006
Data was noted in a predesigned proforma That included Disappearance of crackle (mean days) 3.34±1.07 3.1±0.79 0.206
name, age, gender and address of the patient. Weight, Disappearance of cough( mean days) 5.0±0.78 4.2±0.77 0.000
height and SpO2 by pulse oximeter were measured. Data Time period for hospital stay 6.12±0.90 5.04±0.92 0.000
regarding manifestations of the disease, including cough, Age <6 m 6.26±0.86 5±0.95 0.000
rhonchi, crepitations and duration of hospital stay, the Age >6 m 5.9±0.91 5±0.91 0.002
Wang clinical score11 were observed and documented by Male 6.15±0.81 4.89±0.87 0.000
Female 6.09±0.99 5.23±0.97 0.005
fully trained registrars on duty every 8 hours, which was
Preterm 6.10±0.94 5.11±1.06 0.000
later converted to days from first nebulisation to the order Term 6±0.66 4.8±0.66 0.000
of discharge in round on disappearance of all the signs and Weight < 5th percentile 6.36±0.67 5.5±0.924 0.012
symptoms of bronchiolitis. Weight >5th percentile 6.05±0.94 4.78±0.832 0.000
Height <5th percentile 6.4±0.54 5.10±0.56 0.001
Time to disappearance of symptoms and length of hospital Height >5th percentile 6.09±0.925 5.03±1.04 0.000
stay were also recorded.
Data was analysed using SPSS 17. Qualitative data, like
gender, was expressed as frequencies and percentages.
Age, weight, height, time to disappearance of symptoms
and stay in hospital were expressed mean and standard
deviation (SD). The difference in terms of hospital stay and
duration of disappearance of symptoms was analyzed
using independent t-test. Pearson Chi square test was used
when needed. P<0.05 was taken as significant.
Results
Of the 100 patients, there were 50(50%) in Group A with a
mean age of 7.17±4.46 months, and as many in Group B
with a mean age of 6.6±3.74 months. Overall, there were
55(55%) boys and 45(45%) girls (Table 1).
In Group B, mean time of disappearance of wheeze was
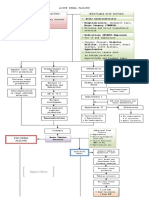
2.9±0.8 days and it was 2.47±07 days in Group A. Mean Figure: : Line graph showing percentage of infants remaining in hospital in both
duration of disappearance of crackles was 3.34±1 days in groups.
J Pak Med Assoc
Comparison of 3% saline and 0.9% normal saline nebulization as diluent in …….. 824
Table-3: Stratification of time for stay in hospital in 3% saline in terms of different resulted in marked reduction in time for settling cough,
variables. wheeze and crepitations (p<0.05). Moreover, duration of
Time for hospital stay in terms of: p-value hospital stay was also reduced in 3% NaCl solution
Age <6 months 5.08±0.95 0.763 nebulisation group (p<0.01).10
>6months 5±0.91 There are certain limitations to the current study. the
Gender Male 4.89±0.87 0.208
physical findings were assessed by registrars on duty and
Female 5.23±0.97
Gestation age Preterm 5.11±1.06 0.389
there was no randomisation of the subjects which could
Term 4.86±0.66 have led to bias in results. Moreover, diagnosis of
Weight <5th percentile 5.5±0.924 0.007 bronchiolitis was clinical without any viral antigen studies.
>5th percentile 4.78±0.832 Finally, we did not included infants of out-patient
Height <5th percentile 5.1±0.568 0.821 department (OPD) having bronchiolitis.
>5th percentile 5.03±1.04
Conclusion
Group B and it was 3.1±0.8 in Group A. Cough disappeared The 3% NaCl inhalation in combination with salbutamol
in 5.0±0.8 days in Group B and in 4.2±0.8 days in Group A. was found to be better than 0.9% NaCl solution. Pulmonary
Mean hospital stay was 6.12±0.9 days in Group B and it was symptoms were resolved more quickly and reduced the
5.04±0.92 days in Group A. The time spent for stay in economic burden due to less time for hospital stay.
hospital was significantly shorter in Group A compared to
Disclaimer: The first author was working at the Shaikh
Group B (p<0.05) (Figure). Significant difference was also
Zayed Hospital, Lahore, during the study period.
noted in mean time for hospital stay in relation to age,
gender, gestational age, weight and height between the Conflict of interest: None.
groups (p<0.05) (Table 2). Source of Funding: None.
Effectiveness of 3% NaCl saline was not significant for References
various variables (Table 3). 1. Grewal S, Ali S, McConnell DW, Vandermeer B, Klassen TP. A random-
ized trial of nebulized 3% hypertonic saline with epinephrine in the
Discussion treatment of acute bronchiolitis in the emergency department. Arch
Nebulisations with bronchodilators and normal saline have Pediatr Adolesc Med 2009;163:1007-12. doi: 10.1001/archpediatrics.
2009.196.
been widely used in the treatment of bronchiolitis. Studies
2. Sharma BS, Gupta MK, Rafik SP. Hypertonic (3%) saline vs 0.93%
have documented varying degree of success using saline nebulization for acute viral bronchiolitis: a randomized con-
terbutaline, salbutamol and adrenaline. Recent studies trolled trial. Indian Pediatr 2013;50:743-7. doi: 10.1007/s13312-013-
have observed better response in terms of decrease in the 0216-8.
duration of symptoms and time for stay in hospital using 3. Zorc JJ, Hall CB. Bronchiolitis: recent evidence on diagnosis and man-
agement. Pediatrics 2010;125:342-9. doi: 10.1542/peds.2009-2092.
3% NaCl with normal saline.12
4. Mathew JL. Hypertonic saline nebulization for bronchiolitis. Indian
It has been documented that although hypertonic saline Pediatr 2008;45:987-9.
5. Ralston S, Hill V, Martinez M. Nebulized hypertonic saline without
decreased the number of admissions to hospital (28.9%), adjunctive bronchodilators for children with bronchiolitis. Pediatrics
the duration of hospital stay and assessment score for 2010;126:e520-5. doi: 10.1542/peds.2009-3105.
respiratory distress were unaffected when compared with 6. Pandit S, Dhawan N, Thakur D. Utility of Hypertonic Saline in the
normal saline13 which is in contrast with the current study. Management of Acute Bronchiolitis in Infants: A Randomised Con-
Similarly, another study in Istanbul revealed contradictory trolled Study. Int J Clin Pediatr 2013;2:24-9 doi: 10.4021/ijcp96w
7. Zhang L, Mendoza-Sassi RA, Wainwright C, Klassen TP. Nebulised hy-
results showing unremarkable differences between the pertonic saline solution for acute bronchiolitis in infants. Cochrane
study groups regarding disease management and hospital Database Syst Rev 2017;12:CD006458. doi: 10.1002/
stay (p>0.05).14 Two other studies15,16 reported no 14651858.CD006458.pub4.
noticeable difference between the two nebulisation 8. Al-Ansari K, Sakran M, Davidson BL, El Sayyed R, Mahjoub H, Ibrahim
K. Nebulized 5% or 3% hypertonic or 0.9% saline for treating acute
groups.
bronchiolitis In Infants. J Pediatr 2010;157:630-4. Doi:
10.1016/j.jpeds.2010.04.074
A Cochrane review concluded that patients who received
9. Kuzik BA, Flavin MP, Kent S, Zielinski D, Kwan CW, Adeleye A, et al. Ef-
nebulisation with 3% NaCl solution spent 10 hours less in fect of inhaled hypertonic saline on hospital admission rate in chil-
hospital compared to the group receiving normal saline dren with viral bronchiolitis: a randomized trial. CJEM
nebulisation.7 Another database revealed less time for 2010;12:477-84. doi: 10.1017/s1481803500012690.
hospital stay in patients with hypertonic saline than in 10. Luo Z, Liu E, Luo J, Li S, Zeng F, Yang X, et al. Nebulized hypertonic
saline/salbutamol solution treatment in hospitalized children with
patients treated with normal saline.17 A study illustrated
mild to moderate bronchiolitis. Pediatr Int 2010;52:199-202. doi:
that when 3% NaCl solution was used with salbutamol, it 10.1111/j.1442-200X.2009.02941.x
Vol. 71, No. 3, March 2021
825 S. Sapkota, A. Kaleem, S. Huma, et al.
11. Wang EE, Milner R, Allen U, Maj H. Bronchodilators for treatment of 15. Bulkow LR, Singleton RJ, Karron RA, Harrison LH. Risk factors for se-
mild bronchiolitis: a factorial randomised trial. Arch Dis Child vere respiratory syncytial virus infection among Alaska native chil-
1992;67:289-93. doi: 10.1136/adc.67.3.289. dren. Pediatrics 2002;109:210-6. doi: 10.1542/peds.109.2.210.
12. Sarrell EM, Tal G, Witzling M, Someck E, Houri S, Cohen HA, et al. Neb- 16. Broughton S, Roberts A, Fox G, Pollina E, Zuckerman M, Chaudhry S,
ulized 3% hypertonic saline solution treatment in ambulatory chil- et al. Prospective study of healthcare utilisation and respiratory mor-
dren with viral bronchiolitis decreases symptoms. Chest bidity due to RSV infection in prematurely born infants. Thorax
2002;122:2015-20. doi: 10.1378/chest.122.6.2015. 2005;60:1039-44. doi: 10.1136/thx.2004.037853.
13. Wu S, Baker C, Lang ME, Schrager SM, Liley FF, Papa C, et al. Nebulized 17. Wang ZY, Li XD, Sun AL, Fu XQ. Efficacy of 3% hypertonic saline in
hypertonic saline for bronchiolitis: a randomized clinical trial. JAMA bronchiolitis: A meta-analysis. Exp Ther Med 2019;18:1338-44. doi:
Pediatr 2014;168:657-63. doi: 10.1001/jamapediatrics.2014.301. 10.3892/etm.2019.7684.
14. Koker O, Ozdogan S, Kose G, Yildirmak ZY. Comparison of the effica-
cies of normal saline versus hypertonic saline in the management of
acute bronchiolitis’. Int J Contemp Pediatr 2016;3:795-800. DOI:
10.18203/2349-3291.ijcp20162353
J Pak Med Assoc
You might also like
- Test Bank For Oral Pharmacology For The Dental Hygienist 2nd Edition 2 e Mea A Weinberg Cheryl Westphal Theile James Burke FineDocument16 pagesTest Bank For Oral Pharmacology For The Dental Hygienist 2nd Edition 2 e Mea A Weinberg Cheryl Westphal Theile James Burke Finexavianhatmgzmz9No ratings yet
- Complementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)From EverandComplementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)No ratings yet
- Basic Training For: Barangay Health Workers Barangay Nutrition ScholarDocument16 pagesBasic Training For: Barangay Health Workers Barangay Nutrition ScholarMario Hipolito100% (5)
- NBHS 1104 Topic 1Document16 pagesNBHS 1104 Topic 1hema angleNo ratings yet
- BMJ 33 2 193Document5 pagesBMJ 33 2 193Ami Novianti SubagyaNo ratings yet
- Hypertonic (3%) Saline Vs 0.9% Saline Nebulization For Acute Viral Bronchiolitis: A Randomized Controlled TrialDocument5 pagesHypertonic (3%) Saline Vs 0.9% Saline Nebulization For Acute Viral Bronchiolitis: A Randomized Controlled TrialMukesh Kumar GuptaNo ratings yet
- Solucion A en BronquiolitisDocument6 pagesSolucion A en BronquiolitisLuis Sanchez CarranzaNo ratings yet
- Pneumonia 5Document6 pagesPneumonia 5furqan92No ratings yet
- Bersihan MukosilierDocument58 pagesBersihan MukosilierbennyrolandnababanNo ratings yet
- Wet CoughDocument2 pagesWet CoughphobicmdNo ratings yet
- Clinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceDocument5 pagesClinical Profile, Etiology, and Management of Hydropneumothorax: An Indian ExperienceSarah DaniswaraNo ratings yet
- Medical Therapeutics Journal Appraisal 3B 2009-70197: 1. Is It Relevant?Document4 pagesMedical Therapeutics Journal Appraisal 3B 2009-70197: 1. Is It Relevant?Maria Christina SalazarNo ratings yet
- Pemilihan Terapi Empirik Pada Balita Pneumonia Berdasarkan Lama Rawat (Lenght of Stay/Los) Dan Komplikasi Dari Gambaran RadiologiDocument8 pagesPemilihan Terapi Empirik Pada Balita Pneumonia Berdasarkan Lama Rawat (Lenght of Stay/Los) Dan Komplikasi Dari Gambaran RadiologiChristyNatalytaTariganNo ratings yet
- Boursiani 2017Document5 pagesBoursiani 2017Carlos Urkieta MonetaNo ratings yet
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoNo ratings yet
- Early Versus Late Caffeine Therapy Administration in Preterm Neonates An Updated Systematic Review and Meta-AnalysisDocument10 pagesEarly Versus Late Caffeine Therapy Administration in Preterm Neonates An Updated Systematic Review and Meta-AnalysisFrancisco C. Belloso HornaNo ratings yet
- Early N Late Caffein TherapyDocument10 pagesEarly N Late Caffein TherapyasritasuriNo ratings yet
- Chamnanvanakij, 2005Document6 pagesChamnanvanakij, 2005Fatma ElzaytNo ratings yet
- The Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalDocument7 pagesThe Effect of Cerebrospinal Fluid's Biochemical and Cellular Properties On Ventriculoperitoneal Shunt SurvivalZablon KodilaNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyJonathan MarkNo ratings yet
- 2 PBDocument4 pages2 PBSuryati HusinNo ratings yet
- Paediatric Pneumonia 2016 - 17Document13 pagesPaediatric Pneumonia 2016 - 17JENNY MARGOT HIDALGO QUISPENo ratings yet
- Tachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionDocument2 pagesTachypnea Is A Useful Predictor of Pneumonia in Children With Acute Respiratory InfectionAli BabaNo ratings yet
- Evidence Based Nursing: Batch 2011Document7 pagesEvidence Based Nursing: Batch 2011Eimhie Lee CasiNo ratings yet
- Characteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDocument8 pagesCharacteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDrnNo ratings yet
- Journal Pediatric IndiaDocument5 pagesJournal Pediatric IndiaHhhNo ratings yet
- The Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine OsmolalityDocument7 pagesThe Influence of Storage Time and Temperature On The Measurement of Serum, Plasma and Urine Osmolalitysafdar aliNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- Post-Standardization of Routine Creatinine Assays Are They Suitable Foir Clinical ApplicationsDocument9 pagesPost-Standardization of Routine Creatinine Assays Are They Suitable Foir Clinical ApplicationsmichelNo ratings yet
- Dr. Tofayel Ahmed IMO Department of Paediatrics, JRRMCHDocument26 pagesDr. Tofayel Ahmed IMO Department of Paediatrics, JRRMCHTofayel AhmedNo ratings yet
- Clinical Analisis of Sputum Gram StainsDocument7 pagesClinical Analisis of Sputum Gram Stainspelcastre r.No ratings yet
- Evaluation Lung B LineDocument1 pageEvaluation Lung B LineBhanu KumarNo ratings yet
- Efficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisDocument4 pagesEfficacy of Nebulised Epinephrine Versus Salbutamol in Hospitalised Children With BronchiolitisFiaz medicoNo ratings yet
- Utility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDocument6 pagesUtility of The Sputum Cytology Applying MGG and Pap Stains in Monitoring Sudanese Patients Complaining of Bronchial AsthmaDr. Asaad Mohammed Ahmed BabkerNo ratings yet
- Journal Pediatric Shock BaruDocument6 pagesJournal Pediatric Shock BaruHhhNo ratings yet
- Steroids For Airway EdemaDocument7 pagesSteroids For Airway EdemaDamal An NasherNo ratings yet
- Corticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Document8 pagesCorticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Bela Bagus SetiawanNo ratings yet
- Articulos BronquiolitisDocument18 pagesArticulos BronquiolitisLaura López Del Castillo LalydelcaNo ratings yet
- Jurnal 3Document5 pagesJurnal 3Anonymous Us5v7C6QhNo ratings yet
- 1 s2.0 S0272638619311151 MainDocument17 pages1 s2.0 S0272638619311151 Main吴善统No ratings yet
- Jurnal ThyphoidDocument10 pagesJurnal ThyphoidAndrea ChristantyNo ratings yet
- Jurnal TBCDocument6 pagesJurnal TBCLorinsya Ollin100% (1)
- Alammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalDocument8 pagesAlammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalTinara HusniaNo ratings yet
- Alammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalDocument8 pagesAlammar Et Al 2023 The Effect of Corticosteroids On Sinus Microbiota in Chronic Rhinosinusitis Patients With NasalTinara HusniaNo ratings yet
- Parkinson IJSRDocument5 pagesParkinson IJSRtyaguspritaNo ratings yet
- A Study On Ventilator Associated Pneumonia inDocument4 pagesA Study On Ventilator Associated Pneumonia inAl MuzakkiNo ratings yet
- Hidrocortisona Vs Choque SepticoDocument12 pagesHidrocortisona Vs Choque SepticoMarisolCamposNo ratings yet
- NIH Public Access: Corticosteroids For Bacterial KeratitisDocument19 pagesNIH Public Access: Corticosteroids For Bacterial KeratitisDede YadedeNo ratings yet
- Journal Homepage: - : IntroductionDocument3 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Targeted O2 Neonatal ResusDocument13 pagesTargeted O2 Neonatal ResusWikan SariNo ratings yet
- Children NebulizerDocument8 pagesChildren NebulizerAnggi CalapiNo ratings yet
- Can Lactate Clearance Predict Mortality in Critically Ill Children?Document6 pagesCan Lactate Clearance Predict Mortality in Critically Ill Children?Sam Aguilar FigueroaNo ratings yet
- Antimicrobial Agent and ChemoteraphyDocument4 pagesAntimicrobial Agent and ChemoteraphyRaina96No ratings yet
- Randomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDocument5 pagesRandomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDiego AndradeNo ratings yet
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaNo ratings yet
- Does Combined Oral Dexamethasone 2011Document3 pagesDoes Combined Oral Dexamethasone 2011Diana Vanessa SuarezNo ratings yet
- 2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisDocument15 pages2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisPamela Mamani FloresNo ratings yet
- GoogleDocument13 pagesGooglesintaraNo ratings yet
- Zgddekzz 23 11 1097Document6 pagesZgddekzz 23 11 1097arieza nur pratamaNo ratings yet
- Gobi NathDocument5 pagesGobi NathRaihan IlyasaNo ratings yet
- Penundaan Pemotongan TalipusatDocument14 pagesPenundaan Pemotongan Talipusatmaya maeNo ratings yet
- Las Nebulizaciones Con Solucion Salina HipertonicaDocument6 pagesLas Nebulizaciones Con Solucion Salina HipertonicaAlisson De Berduccy TroncosoNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Power Point Consumer Health EducationDocument81 pagesPower Point Consumer Health EducationAlbert Ian CasugaNo ratings yet
- Functional Capacity&Lung FunctionDocument11 pagesFunctional Capacity&Lung Functionandika pradanaNo ratings yet
- Bio T4 DLP KSSM Chapter 11Document59 pagesBio T4 DLP KSSM Chapter 11fadilahNo ratings yet
- MBBS Pain Symposium 2022Document10 pagesMBBS Pain Symposium 2022Morgan BaileyNo ratings yet
- Systemic and Local Applications of Steroids in Endodontics: An Update ReviewDocument8 pagesSystemic and Local Applications of Steroids in Endodontics: An Update ReviewJorge OrbeNo ratings yet
- Brokenshire College: Form C. Informed Consent Assessment FormDocument2 pagesBrokenshire College: Form C. Informed Consent Assessment Formgeng gengNo ratings yet
- R.A. No. 11223 - Universal Health Care ActDocument5 pagesR.A. No. 11223 - Universal Health Care ActCeline100% (2)
- Medical Devices Act - M 3 en PDFDocument42 pagesMedical Devices Act - M 3 en PDFDewa GedeNo ratings yet
- Apollo Proton Cancer Centre (Medical Oncology) For Kenyan PatientsDocument10 pagesApollo Proton Cancer Centre (Medical Oncology) For Kenyan PatientsApollo Information CentreNo ratings yet
- Jointly Team: SMLE GroupDocument22 pagesJointly Team: SMLE GroupAkpevwe EmefeNo ratings yet
- Sindrom Reconstructive ImunaDocument7 pagesSindrom Reconstructive ImunaAlexandra PaunNo ratings yet
- American Handbook of Psychiatry - Volume I - The Foundations of PsychiatryDocument3,272 pagesAmerican Handbook of Psychiatry - Volume I - The Foundations of Psychiatrydark thanos100% (2)
- Pascual Janine Krista E. NCPDocument3 pagesPascual Janine Krista E. NCPCzarina Mae LomboyNo ratings yet
- Pathophysiology of Acute Renal FailureDocument2 pagesPathophysiology of Acute Renal Failureminangsung minangnengNo ratings yet
- Scrotal Swelling FadhlyDocument52 pagesScrotal Swelling FadhlyfadhlyNo ratings yet
- RPD NewDocument4 pagesRPD Newapi-632682404No ratings yet
- DocxDocument12 pagesDocxJojo JacobNo ratings yet
- Bwdi DR, Chemist&Stp Final ListDocument226 pagesBwdi DR, Chemist&Stp Final ListzaheerbcNo ratings yet
- Encefalopatía Hepatica PDFDocument7 pagesEncefalopatía Hepatica PDFsukardo5426No ratings yet
- AlzheimerDocument2 pagesAlzheimerCho HyeyeonNo ratings yet
- Case Presentation: BY MeghaDocument13 pagesCase Presentation: BY Meghalibrian_pallavi3942No ratings yet
- Maya Rotation ChecklistDocument1 pageMaya Rotation Checklistapi-434982019No ratings yet
- Prof. Services v. AganaDocument77 pagesProf. Services v. AganaRechel De TorresNo ratings yet
- Al Jabry Pharmacy LLC: Deef Pharmaceutical Industries Co. KsaDocument1 pageAl Jabry Pharmacy LLC: Deef Pharmaceutical Industries Co. Ksamdgayas70No ratings yet
- Delirium and Acute Confusional States - Prevention, Treatment, and Prognosis - UpToDateDocument18 pagesDelirium and Acute Confusional States - Prevention, Treatment, and Prognosis - UpToDateKarina CabayNo ratings yet
- Lung Cancer Pathology and DiagnosisDocument28 pagesLung Cancer Pathology and DiagnosismadvincyNo ratings yet
- Instrucciones Post Extraccion INGLESDocument1 pageInstrucciones Post Extraccion INGLESAlessandro Matias GonzalezNo ratings yet