Professional Documents
Culture Documents
Oral Candidiasis: A Short Review and A Case Report: December 2018
Oral Candidiasis: A Short Review and A Case Report: December 2018
Uploaded by
RAfii KerenOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Candidiasis: A Short Review and A Case Report: December 2018
Oral Candidiasis: A Short Review and A Case Report: December 2018
Uploaded by
RAfii KerenCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/336115724
Oral Candidiasis: A Short Review and a Case Report
Article · December 2018
CITATION READS
1 2,480
3 authors, including:
Syed Wali Peeran
Sebha University
128 PUBLICATIONS 167 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Oral hygiene practices and periodontal status among general population of Sebha, Libya View project
Periodontal immunology View project
All content following this page was uploaded by Syed Wali Peeran on 28 September 2019.
The user has requested enhancement of the downloaded file.
Oral Candidiasis: A Short Review and a Case Report
[PP: 11-14]
Dr. Syed Abid Bukhari
AFHJ, Jazan, KSA
Dr. Khalid Moashy
HOD and Consultant, AFHJ, Jazan, KSA
Dr. Syed Wali Peeran
(Corresponding Author)
AFHJ, Jazan, KSA
Abstract:
Candidiasis is a fungal infection caused by dimorphic yeasts which belong to the genus Candida.
Oral candidiasis (OC) is the commonest fungal infection affecting human beings. It affects the
oral mucosa. These lesions are caused by the yeast Candida albicans. We report a case of Saudi
male patient with oral candidiasis who was treated successfully with antifungal therapy.
Keywords: Candidiasis, fungal, infection, dimorphic yeasts, antifungal therapy
ARTICLE The paper received on: 20/10/2018 Accepted after review on: 04/12/2018 Published on: 04/12/2018
INFO
Cite this article as:
Bukhari, S.A., Moashy, K. & Peeran, S.W. (2018). Oral Candidiasis: A Short Review and a Case Report. Case
Reports in Odontology. 5(2), 11-14. Retrieved from www.casereportsinodontology.org
three groups; the acute candidiasis, chronic
1. Introduction candidiasis, and angular cheilitis.4
Candidiasis is a fungal infection 1. Acute Candidiasis
caused by dimorphic yeasts like fungi which a) Acute pseudomembranous candidiasis.
belong to the genus Candida. There are b) Acute atrophic (erythematous)
about 150 species of Candidia and over 20 candidiasis.
species of them can cause infection in 2. Chronic candidiasis.
humans, the most common of which is a) Chronic hyperplastic
Candida albicans. Inaddition, C. albicans, candidiasis(candidal leukoplakia)
C. glabrata, C. guillermondii, C. krusei, C. b) Denture induced candidiasis (chronic
parapsilosis C. tropicalis also cause atrophic(erythematous) candidiasis)
infections in human beings.1–3 Candida 3. Angular cheilitis (Stomatitis)
species inhabit the intestinal tract as well as The most widely used classification
vagina as commensals. They cause was developed by Holmtup and Axel and is
infections in immunosuppressed individuals as follows6:
and in healthy individuals with altered 1. Pseudomembranous candidiasis (Acute /
microbial flora.1 chronic)
Oral candidiasis (OC) is the 2. Erythematous candidiasis (Acute /
commonest fungal infection affecting human Chronic)
beings.4 It affects the oral mucosa. These 3. Candida associated lesions:
lesions are caused by the yeast Candida a) Denture stomatitis.
albicans.5,4 OC can be broadly placed under b) Angular cheilitis.
Case Reports in Odontology ISSN: 2410-0412
Volume: 05 Issue: 02 July-December, 2018
c) Median Rhomboid glossitis. department in the AFHJ, Jazan, KSA with a
The risk factors for OC include poor chief complaint of oral discomfort,
oral hygiene, impaired salivary gland discharge, inability to open his mouth and
function, use of drugs especially prolonged bad breath from the past two weeks. The
use of antibiotics, corticosteroid therapy, patient presented a non-contributory past
oral prosthesis including dentures, high medical except that he was diagnosed for
carbohydrate diet, stress and depression, use Post-traumatic stress disorder(PSTD) earlier.
of tobacco smoking, diabetes mellitus, (See Figure: 1). His past drug history and
Cushing’s syndrome, oral malignancies, dental history were nonsignificant. He had
altered nutritional states including iron no history of smoking. His vital signs were
deficiency, folate deficiency, irradiation and normal.
immunosuppressive conditions.4,7,8,910 OC is Intra-oral examination showed signs
diagnosed clinically. However biopsy in of discharge, a white moss like appearance,
cases of hyperplastic OC, and other ulcerative lesions of the lips, base of the
immunological methods such as PCR and tongue, buccal mucosa along with bad
ELISA are sometimes employed to breath and fissures at the angles of the
complement definitive diagnosis.11 OC mouth. The patient had a few missing teeth
lesions are white or erythematous, usually and had poor oral hygiene. An immediate
asymptomatic. It predominantly affects diagnosis of OC was done. He was treated
adults and shows no racial and sexual with a single dose of a combination of
predilection.12 A variety of remedies have systemic (200 mg Ketoconazole once daily
been employed in patients with OS which for 3 days) as well as local antifungal
include the use of mouthrinses such as therapy(Nystatin mouth-rinse for 7 days) .
Sodium hypochlorite, use of topical He responded to Antifungal therapy and
antifungal drugs such as miconazole, recovered completely without necessity of
clotrimazole, ketoconazole, nystatin further therapy. (See Figure: 2).
ointments and suspensions, use of systemic 3. Discussion& Conclusion
antifungal drugs Amphotericin B, Various members of Candida species
Clotrimazole, Fluconazole, Itraconazole, inhabit the oral cavity and are opportunistic
Ketoconazole, Nystatin .1,5,7 Recently fungi. They are associated with a number of
probiotic use of lactobacilli species oral diseases in human beings.22 OC is a
especially Lactobacillus rhamnosus and well-known entity and the lesions are
Lactobacillus casei have emerged as a new commonly seen. OC results from
frontier against the OC.13,14–17,18 Alternative physiological changes and homeostatic
therapies such as the employment of disturbances in the host immune system. In
photodynamic therapy, probiotics, the presence of a healthy and well balanced
prebiotics, use of medicinal plant extracts, host immune system Candida albicans
honey have also been reported to be of some behaves as a commensal in the oral
benefit.19,20,21 We report a case of OC ecosystem. It proliferates rapidly in cases of
occuring in a Saudi male patient who defects in cellular immune response in
reported being under stress. subjects and lead to biofilm infections in
2. Case Report immunocompromised individuals.123 In this
A 34-year old male patient of Saudi reported case the patient suffered from OC
origin reported to the outpatient dental with severe psychological stress.
Cite this article as: Bukhari, S.A., Moashy, K. & Peeran, S.W. (2018). Oral Candidiasis: A Short Review and a
Case Report. Case Reports in Odontology. 5(2), 11-14. Retrieved from www.casereportsinodontology.org
Page | 12
Case Reports in Odontology ISSN: 2410-0412
Volume: 05 Issue: 02 July-December, 2018
OC can result in aspiration Oral manifestations in patients with
pneumonia and fungemia1. Moreover Sjögren’s syndrome. J Rheumatol.
antifungal resistance due to the lesser 1998;25(5):906-910.
susceptibility of certain species, such as https://www.ncbi.nlm.nih.gov/pubmed/959
Candida glabrata and C. krusei, to 8889.
9. Ezenwa BN, Oladele RO, Akintan PE, et
antifungal drugs can be seen.23,24 Hence al. Invasive candidiasis in a neonatal
immediately attention with proper clinical intensive care unit in Lagos, Nigeria. Niger
diagnosis and judicious administration of Postgrad Med J. 2017;24(3):150-154.
antifungal drugs along with adequate doi:10.4103/npmj.npmj_104_17
attention to decrease in host immune 10. van Wyk C, Steenkamp V. Host factors
response if any is vital in handling OC when affecting oral candidiasis. South Afr J
it presents. Epidemiol Infect. 2011;26(1):18-21.
References doi:10.1080/10158782.2011.11441414
1. Ohshima T, Ikawa S, Kitano K, Maeda N. A 11. Coronado-Castellote L, Jiménez-Soriano
Proposal of Remedies for Oral Diseases Y. Clinical and microbiological diagnosis
Caused by Candida: A Mini Review. Front of oral candidiasis. J Clin Exp Dent.
Microbiol. 2018;9:1522. 2013;5(5):e279-e286.
doi:10.3389/fmicb.2018.01522 doi:10.4317/jced.51242
2. Candidiasis. Centers for Disease Control 12. Meira HC, De Oliveira BM, Pereira IF,
and Prevention. Naves MD, Mesquita RA, Santos VR. Oral
https://www.cdc.gov/fungal/diseases/candi candidiasis: A retrospective study of 276
diasis/index.html. Published May 4, 2018. Brazilian patients. J Oral Maxillofac
Accessed November 10, 2018. Pathol. 2017;21(3):351-355.
3. Halim N, Kalkur C, Rangare A. oral doi:10.4103/jomfp.JOMFP_77_16
candidiasis: a review. Journal of Indian 13. Miyazima TY, Ishikawa KH, Mayer M,
Dental Association. 2017;11(8):12-16. Saad S, Nakamae A. Cheese supplemented
http://publication.ida.org.in/IndexMain.htm with probiotics reduced the Candida levels
#/viewArticle/21625. Accessed November in denture wearers-RCT. Oral Dis.
10, 2018. 2017;23(7):919-925.
4. Akpan A. Oral candidiasis. Postgrad Med doi:10.1111/odi.12669
J. 2002;78(922):455-459. 14. Ishikawa KH, Mayer MPA, Miyazima TY,
doi:10.1136/pmj.78.922.455 et al. A multispecies probiotic reduces oral
5. Singh A, Verma R, Murari A, Agrawal A. Candida colonization in denture wearers. J
Oral candidiasis: An overview. J Oral Prosthodont. 2015;24(3):194-199.
Maxillofac Pathol. 2014;18(Suppl 1):S81- doi:10.1111/jopr.12198
S85. doi:10.4103/0973-029X.141325 15. Hatakka K, Ahola AJ, Yli-Knuuttila H, et
6. Williams D, Lewis M. Pathogenesis and al. Probiotics reduce the prevalence of oral
treatment of oral candidosis. J Oral candida in the elderly--a randomized
Microbiol. 2011;3(1):5771. controlled trial. J Dent Res.
doi:10.3402/jom.v3i0.5771 2007;86(2):125-130.
7. Lira A de LS de, Torres AC. Relationship doi:10.1177/154405910708600204
between oral candidiasis and users of 16. Ai R, Wei J, Ma D, et al. A meta-analysis
dental prostheses. Braz J Oral Sci. of randomized trials assessing the effects
2018;17:1-11. of probiotic preparations on oral
doi:10.20396/bjos.v17i0.8652906 candidiasis in the elderly. Arch Oral Biol.
8. Soto-Rojas AE, Villa AR, Sifuentes- 2017;83:187-192.
Osornio J, Alarcón-Segovia D, Kraus A. doi:10.1016/j.archoralbio.2017.04.030
Cite this article as: Bukhari, S.A., Moashy, K. & Peeran, S.W. (2018). Oral Candidiasis: A Short Review and a
Case Report. Case Reports in Odontology. 5(2), 11-14. Retrieved from www.casereportsinodontology.org
Page | 13
Case Reports in Odontology ISSN: 2410-0412
Volume: 05 Issue: 02 July-December, 2018
17. Song Y-G, Lee S-H. Inhibitory effects of Figures & Legends:
Lactobacillus rhamnosus and Lactobacillus
casei on Candida biofilm of denture
surface. Arch Oral Biol. 2017;76:1-6.
doi:10.1016/j.archoralbio.2016.12.014
18. Matsubara VH, Wang Y, Bandara HMHN,
Mayer MPA, Samaranayake LP. Probiotic
lactobacilli inhibit early stages of Candida
albicans biofilm development by reducing
their growth, cell adhesion, and
filamentation. Appl Microbiol Biotechnol.
2016;100(14):6415-6426.
doi:10.1007/s00253-016-7527-3
19. Annigeri RG, Mangala GK, Thimmasetty
J, Sharma N, Kanjani V, Sravya G.
Evaluation of tulasi extract mouthwash in
the management of oral candidiasis.
Nagaraj T, ed. JCRI. 2018;5(2):30-34.
doi:10.15713/ins.jcri.203
20. Pflipsen M, Zenchenko Y. Nutrition for
oral health and oral manifestations of poor
nutrition and unhealthy habits. Gen Dent.
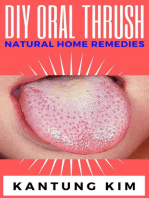
2017;65(6):36-43. Figure 1: Clinical picture showing OC
https://www.ncbi.nlm.nih.gov/pubmed/290
99364.
21. Rodrigues CF, Rodrigues ME, Henriques
MCR. Promising alternative therapeutics
for oral candidiasis. Curr Med Chem. May
2018.
doi:10.2174/092986732566618060110233
3
22. Imron Nasution A. Virulence Factor and
Pathogenicity of Candida albicans in Oral
Candidiasis. G Patil S, ed. WJOUD.
2013;4:267-271. doi:10.5005/jp-journals-
10015-1243
23. Silva S, Rodrigues C, Araújo D, Rodrigues
M, Henriques M. Candida Species
Biofilms’ Antifungal Resistance. Journal
of Fungi. 2017;3(1):8.
doi:10.3390/jof3010008
24. Niimi M, Firth NA, Cannon RD. Figure 2: One Week post Antifungal therapy
Antifungal drug resistance of oral fungi.
Odontology. 2010;98(1):15-25.
doi:10.1007/s10266-009-0118-3
Cite this article as: Bukhari, S.A., Moashy, K. & Peeran, S.W. (2018). Oral Candidiasis: A Short Review and a
Case Report. Case Reports in Odontology. 5(2), 11-14. Retrieved from www.casereportsinodontology.org
Page | 14
View publication stats
You might also like
- Drug-Induced Oral Candidiasis - A Case ReportDocument4 pagesDrug-Induced Oral Candidiasis - A Case ReportFajarRahmantiyoNo ratings yet
- Candida-Associated Cheilitis: Online Images in The Medical SciencesDocument2 pagesCandida-Associated Cheilitis: Online Images in The Medical Sciencesfelaxis fNo ratings yet
- Pseudomembranous Candidiasis Induced byDocument5 pagesPseudomembranous Candidiasis Induced byGenevieve Florencia Natasya SaraswatiNo ratings yet
- Current Treatment of Oral Candidiasis A Literature ReviewDocument8 pagesCurrent Treatment of Oral Candidiasis A Literature ReviewRonaldo PutraNo ratings yet
- Fmicb 06 01391 PDFDocument10 pagesFmicb 06 01391 PDFChellaPremitaNo ratings yet
- Candida-Associated Denture StomatitisDocument5 pagesCandida-Associated Denture StomatitisAyik DarkerThan BlackNo ratings yet
- 204-Article Text-650-2-10-20200909Document9 pages204-Article Text-650-2-10-20200909Ridha AprillahNo ratings yet
- Health Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Document5 pagesHealth Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Kamado NezukoNo ratings yet
- Health Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Document5 pagesHealth Notions, Volume 4 Number 2 (February 2020) Issn 2580-4936Kamado NezukoNo ratings yet
- Risk Factors Related To Oral Candidiasis in Patients With Primary Sjögren's SyndromeDocument6 pagesRisk Factors Related To Oral Candidiasis in Patients With Primary Sjögren's SyndromeEdith TrejoNo ratings yet
- Clinical Characteristics of Patients With Oral CandidiasisDocument8 pagesClinical Characteristics of Patients With Oral CandidiasisHilya Aliva AufiaNo ratings yet
- Oropharyngeal Candidiasis: Review of Its Clinical Spectrum and Current TherapiesDocument18 pagesOropharyngeal Candidiasis: Review of Its Clinical Spectrum and Current TherapiesDelbert GradyNo ratings yet
- 588 Article+Text 1884 1 10 20220107Document9 pages588 Article+Text 1884 1 10 20220107Dave PutraNo ratings yet
- Chronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFDocument3 pagesChronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFGita Dwi DesianiNo ratings yet
- Diagnosis and Treatment of Oral CandidosisDocument7 pagesDiagnosis and Treatment of Oral CandidosisYerly Ramirez MuñozNo ratings yet
- Angular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanDocument2 pagesAngular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanindahdwitasariNo ratings yet
- Oral Candidiasis An Opportunistic Infection A ReviewDocument5 pagesOral Candidiasis An Opportunistic Infection A ReviewDino JalerNo ratings yet
- Odontogenic Infections Microbiology and ManagementDocument5 pagesOdontogenic Infections Microbiology and ManagementJeninNo ratings yet
- Potencial Malignizante de CandidiasisDocument16 pagesPotencial Malignizante de CandidiasissolcitoNo ratings yet
- Suppression of Streptococcus Mutans and Candida Albicans by Probioticsan in Vitro StudyDocument8 pagesSuppression of Streptococcus Mutans and Candida Albicans by Probioticsan in Vitro StudyTahir AliNo ratings yet
- Dental Caries A Microbiological Approach 2476 213X 1000118Document16 pagesDental Caries A Microbiological Approach 2476 213X 1000118NOVITANo ratings yet
- Oral Candidiasis - A Review PDFDocument18 pagesOral Candidiasis - A Review PDFChristian Rodriguez BermudezNo ratings yet
- 2428 FullDocument4 pages2428 FullEdith TrejoNo ratings yet
- Pathophysiology of Sinusitis of Odontogenic OriginDocument7 pagesPathophysiology of Sinusitis of Odontogenic OriginErin NettaNo ratings yet
- Occurrence of Candida Albicans in Periodontitis PDFDocument7 pagesOccurrence of Candida Albicans in Periodontitis PDFAbdoNo ratings yet
- Immunological Effectiveness of Immuno - and Biocorrective Treatment of Dental Diseases in Pregnant WomenDocument4 pagesImmunological Effectiveness of Immuno - and Biocorrective Treatment of Dental Diseases in Pregnant WomenCentral Asian StudiesNo ratings yet
- Jurnal Gingivitis Vivian 190631174Document5 pagesJurnal Gingivitis Vivian 190631174VivianNo ratings yet
- Seminario Biologia 2Document11 pagesSeminario Biologia 2Daniela Rizo AlvarezNo ratings yet
- CandidiasisDocument6 pagesCandidiasismirayanti astariNo ratings yet
- Case Report-Hypothyroidism, Adenoid Hypertrophy and GingivitisDocument7 pagesCase Report-Hypothyroidism, Adenoid Hypertrophy and GingivitisDeepak GawandeNo ratings yet
- 10.2478 - Aoj 2022 0006Document12 pages10.2478 - Aoj 2022 0006Cindy SuNo ratings yet
- Ganoderma Lucidum Against Candida AlbicansDocument8 pagesGanoderma Lucidum Against Candida AlbicansCsikós IlonaNo ratings yet
- The Topical Effect of Chlorhexidine and Povidone-Iodine in The Repair of Oral Wounds. A ReviewDocument7 pagesThe Topical Effect of Chlorhexidine and Povidone-Iodine in The Repair of Oral Wounds. A ReviewMario CastroNo ratings yet
- Oral Candidiasis Causes Types and Treatment PDFDocument12 pagesOral Candidiasis Causes Types and Treatment PDFTiborNo ratings yet
- IntJHealthAlliedSci8129-4857065 012057Document4 pagesIntJHealthAlliedSci8129-4857065 012057tito cuadrosNo ratings yet
- Medical Mycology Case Reports: SciencedirectDocument5 pagesMedical Mycology Case Reports: SciencedirectDr.Sudarsan SenNo ratings yet
- 2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesDocument22 pages2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesK KNo ratings yet
- Aparna. K Et AlDocument7 pagesAparna. K Et AlAparna SanathNo ratings yet
- Heim 2017Document13 pagesHeim 2017Muhamad SaifuddinNo ratings yet
- Podj 4 PDFDocument3 pagesPodj 4 PDFNur Sita DewiNo ratings yet
- Periodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisDocument6 pagesPeriodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisPhuong ThaoNo ratings yet
- Oral Candidiasis An Overview and Case ReportDocument7 pagesOral Candidiasis An Overview and Case ReportPutri NingrumNo ratings yet
- 2022 - TenOrio - Oral Manifestations of Autoimmune Polyglandular Syndrome Type 1Document5 pages2022 - TenOrio - Oral Manifestations of Autoimmune Polyglandular Syndrome Type 1NATALIA SILVA ANDRADENo ratings yet
- Antibiotics in Endodontics: A ReviewDocument16 pagesAntibiotics in Endodontics: A ReviewHisham HameedNo ratings yet
- Oral and Dental HealthDocument10 pagesOral and Dental HealthannisaramadantiNo ratings yet
- Dental Caries A Microbiological ApproachDocument15 pagesDental Caries A Microbiological ApproachAnnabella NatashaNo ratings yet
- OJDOH - Antimicrobial Resistance &stewardship ProgramDocument7 pagesOJDOH - Antimicrobial Resistance &stewardship Programshayma rafatNo ratings yet
- Jpedo 4Document5 pagesJpedo 4Super LonelyNo ratings yet
- NtionvioletDocument10 pagesNtionvioletGeorgi GugicevNo ratings yet
- Candidiasis - Red and White Manifestations in The Oral CavityDocument8 pagesCandidiasis - Red and White Manifestations in The Oral CavityFajarRahmantiyoNo ratings yet
- Cabt 10 I 1 P 1Document5 pagesCabt 10 I 1 P 1Hanifah Nailul AmaniaNo ratings yet
- CBL 10 - Gigi & Mulut PDFDocument35 pagesCBL 10 - Gigi & Mulut PDFanon_977064336No ratings yet
- Management of Oral Manifestations in A Case of Cushing's HabitusDocument4 pagesManagement of Oral Manifestations in A Case of Cushing's HabitusAzzNo ratings yet
- SciDentJ43142-2157287 055932Document6 pagesSciDentJ43142-2157287 055932Michael TrumanjayaNo ratings yet
- Chronic Mucocutaneous Candidiasis: A Case ReportDocument4 pagesChronic Mucocutaneous Candidiasis: A Case Reportselandia nisrinaNo ratings yet
- JDDM 2 129Document5 pagesJDDM 2 129Widhi Satrio NugrohoNo ratings yet
- Diagnostics 12 01600 v2Document15 pagesDiagnostics 12 01600 v2dayuNo ratings yet
- Prescribing Antibiotics in Odontology and Stomatology Recommenda 2003Document5 pagesPrescribing Antibiotics in Odontology and Stomatology Recommenda 2003Fernando Lopez EncisoNo ratings yet
- 261 773 1 PB PDFDocument8 pages261 773 1 PB PDFDr Monal YuwanatiNo ratings yet
- Phys Mcqs Nervous SystemDocument23 pagesPhys Mcqs Nervous SystemYusraNo ratings yet
- Principles of Lesion Localization in Neurology - University of MiamiDocument35 pagesPrinciples of Lesion Localization in Neurology - University of MiamiErick AlbanNo ratings yet
- Memory Complaint Scale (MCS)Document9 pagesMemory Complaint Scale (MCS)IcaroNo ratings yet
- Chapter 5 MemoryDocument55 pagesChapter 5 MemoryNadine Chanelle QuitorianoNo ratings yet
- Medication Management Ini ElderlyDocument57 pagesMedication Management Ini ElderlySyafi'ah Bakaruddin100% (2)
- ArthritisDocument22 pagesArthritisअनुरूपम स्वामीNo ratings yet
- Drug Study DisudrinDocument1 pageDrug Study DisudrinGrant Kenneth Dumo AmigableNo ratings yet
- AlgesiaDocument1 pageAlgesiaSaf DicamNo ratings yet
- Molecular Trojan Horses For Blood-Brain Barrier Drug DeliveryDocument7 pagesMolecular Trojan Horses For Blood-Brain Barrier Drug Deliveryjohn snowNo ratings yet
- Hematology and Coagulation Essentials HandbookDocument78 pagesHematology and Coagulation Essentials HandbookSadat NazirNo ratings yet
- The Iraqi Doctor With Highest Academic Rank According To International StandardsDocument1 pageThe Iraqi Doctor With Highest Academic Rank According To International StandardsAamir Jalal Al-MosawiNo ratings yet
- Rad PathologyDocument178 pagesRad PathologyJames MoralesNo ratings yet
- Buerger Disease 1Document27 pagesBuerger Disease 1nadiaNo ratings yet
- Radio PDFDocument124 pagesRadio PDFAshwaq A Bani AtaNo ratings yet
- CNS 35-50Document16 pagesCNS 35-50ahmedsalah565vvvNo ratings yet
- Chapter 12 - DnaDocument23 pagesChapter 12 - Dnaapi-246719131No ratings yet
- Medicinal Plants and Their Traditional UsesDocument11 pagesMedicinal Plants and Their Traditional UsesEditor IJTSRDNo ratings yet
- OB Ward DRUG STUDYDocument1 pageOB Ward DRUG STUDYMaria Francheska OsiNo ratings yet
- Management of Patients With Nonmalignant Hematologic DisordersDocument97 pagesManagement of Patients With Nonmalignant Hematologic DisordersJulia Rae Delos SantosNo ratings yet
- ALZHEIMERDocument9 pagesALZHEIMERKhem Limoso100% (2)
- Drug Study PantoprazoleDocument2 pagesDrug Study PantoprazoleFlauros Ryu Jabien100% (3)
- AtelectasisDocument2 pagesAtelectasisiMaibelle BelleNo ratings yet
- Preoperative Evaluation For Non-Cardiac Surgery: AK GhoshDocument6 pagesPreoperative Evaluation For Non-Cardiac Surgery: AK GhoshAshvanee Kumar SharmaNo ratings yet
- Extrapulmonary Tuberculosis-An Update On The Diagnosis, Treatment and Drug ResistanceDocument24 pagesExtrapulmonary Tuberculosis-An Update On The Diagnosis, Treatment and Drug ResistanceApt. Mulyadi PrasetyoNo ratings yet
- RosiglitazoneDocument2 pagesRosiglitazoneAngelica Alburo PenionNo ratings yet
- Adult Physical AssessmentDocument185 pagesAdult Physical AssessmentD. Melba S.S ChinnaNo ratings yet
- FAQCo WINforcitizensDocument5 pagesFAQCo WINforcitizensRaj AgrawalNo ratings yet
- Lecture Notes: Clinical Chemistry of LiverDocument38 pagesLecture Notes: Clinical Chemistry of LivershehnilaNo ratings yet
- VADEMECUMDocument48 pagesVADEMECUMCentellas IvarNo ratings yet
- Psychiatric Nursing: BenzodiazepinesDocument8 pagesPsychiatric Nursing: BenzodiazepinesDiane AbanillaNo ratings yet