Professional Documents
Culture Documents
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
Uploaded by
Ida NeniCopyright:
Available Formats
You might also like
- Tuberculosis, Smoking and Risk For Lung Cancer Incidence and MortalityDocument9 pagesTuberculosis, Smoking and Risk For Lung Cancer Incidence and MortalityarifahNo ratings yet
- Journal of Clinical Tuberculosis and Other Mycobacterial DiseasesDocument5 pagesJournal of Clinical Tuberculosis and Other Mycobacterial DiseasesputerinmNo ratings yet
- Jurnal Ke 2Document13 pagesJurnal Ke 2deroNo ratings yet
- Association Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalDocument5 pagesAssociation Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalairwanNo ratings yet
- Smoking Increases Risk of Recurrence After Successful Anti-Tuberculosis TreatmentDocument8 pagesSmoking Increases Risk of Recurrence After Successful Anti-Tuberculosis TreatmentRaditya Imam PratanaNo ratings yet
- Pulmonary Tuberculosis Specificities in Smokers: Egyptian Journal of Chest Diseases and TuberculosisDocument4 pagesPulmonary Tuberculosis Specificities in Smokers: Egyptian Journal of Chest Diseases and TuberculosisIntan TeraniaNo ratings yet
- Jurnal 10 HariantoDocument7 pagesJurnal 10 Hariantoaryzamelindah channelNo ratings yet
- JKMC, 2014 Issue2 (21-24)Document4 pagesJKMC, 2014 Issue2 (21-24)Jin SeonNo ratings yet
- Factors Associated With Mortality in Tuberculosis IranDocument4 pagesFactors Associated With Mortality in Tuberculosis IranMade NujitaNo ratings yet
- Mortality Among Tuberculosis Patients in The Democratic Republic of CongoDocument7 pagesMortality Among Tuberculosis Patients in The Democratic Republic of CongoGary Rios DionicioNo ratings yet
- Johanssen ReviewDocument16 pagesJohanssen Reviewsidra malikNo ratings yet
- Research On Prevalence of TB FinalDocument9 pagesResearch On Prevalence of TB FinalBontuNo ratings yet
- Which Patients Are Able To Adhere To Tuberculosis Treatment? A Study in A Rural Area in The Northwest Part of TurkeyDocument7 pagesWhich Patients Are Able To Adhere To Tuberculosis Treatment? A Study in A Rural Area in The Northwest Part of TurkeyAnonymous QPXAgjBwNo ratings yet
- Jact 12 I 2 P 142Document3 pagesJact 12 I 2 P 142Rosdiana Elizabeth Siburian0% (1)
- 1post-Class Quiz1 StudydesignsDocument14 pages1post-Class Quiz1 Studydesignssimplify8000No ratings yet
- Jurnal DR KrisDocument8 pagesJurnal DR KrisHiszom AsyhariNo ratings yet
- Bagi Retno Ariza Soeprihatini Soemarwoto (Inatime)Document6 pagesBagi Retno Ariza Soeprihatini Soemarwoto (Inatime)Dumora FatmaNo ratings yet
- Survival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorDocument10 pagesSurvival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorGetachew GemedaNo ratings yet
- Copd 2 263Document10 pagesCopd 2 263Vevi VarcetyNo ratings yet
- Title Subtle Presentation of Cryptic Tuberculosis in The ElderlyDocument25 pagesTitle Subtle Presentation of Cryptic Tuberculosis in The ElderlyHam FGNo ratings yet
- Diabetes Mellitus Among Tuberculosis Patients Admitted To The Pulmonarytuberculo PDFDocument5 pagesDiabetes Mellitus Among Tuberculosis Patients Admitted To The Pulmonarytuberculo PDFRinzyNo ratings yet
- EthiopiaDocument15 pagesEthiopiaVincentius Michael WilliantoNo ratings yet
- Boeck Ler 2009Document5 pagesBoeck Ler 2009l10n_assNo ratings yet
- Tuberculosis, Alcohol and Tobacco: Dangerous Liaisons: EditorialDocument2 pagesTuberculosis, Alcohol and Tobacco: Dangerous Liaisons: EditorialatikahanifahNo ratings yet
- Hubungan Pola Merokok Dengan Kejadian AsmaDocument11 pagesHubungan Pola Merokok Dengan Kejadian AsmaLivilia MiftaNo ratings yet
- Risk Factors For Interstitial Lung Disease 2018Document7 pagesRisk Factors For Interstitial Lung Disease 2018Mary CogolloNo ratings yet
- Environmental Toxins Harm Fetal Auditory PathwaysDocument4 pagesEnvironmental Toxins Harm Fetal Auditory PathwaysDinah Marie CarinoNo ratings yet
- Attique Corrected Paper 1Document12 pagesAttique Corrected Paper 1Mobin Ur Rehman KhanNo ratings yet
- Antibiotic Use and The Risk of Lung CancerDocument8 pagesAntibiotic Use and The Risk of Lung CancerBelajarNo ratings yet
- An Exploratory Study To Assess The Knowledge Regarding Side Effects of Anti - Tubercular Drugs and Its Self-Care Management Adapted by Tuberculosis PatientsDocument8 pagesAn Exploratory Study To Assess The Knowledge Regarding Side Effects of Anti - Tubercular Drugs and Its Self-Care Management Adapted by Tuberculosis Patientssaurabh kumar guptaNo ratings yet
- CAP - PrinaDocument12 pagesCAP - PrinaSalNo ratings yet
- Tobacco Smoke, Indoor Air Pollution and Tuberculosis: A Systematic Review and Meta-AnalysisDocument2 pagesTobacco Smoke, Indoor Air Pollution and Tuberculosis: A Systematic Review and Meta-AnalysisPutri ClaraNo ratings yet
- Cigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasDocument9 pagesCigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasMaria FulgensiaNo ratings yet
- THT JurnalDocument4 pagesTHT JurnalanugerahNo ratings yet
- (2020) Treatment Outcome of Tuberculosis Treatment Regimens in Kandahar, AfghanistanDocument7 pages(2020) Treatment Outcome of Tuberculosis Treatment Regimens in Kandahar, AfghanistanBilal Ahmad RahimiNo ratings yet
- Predictors of Tuberculosis (TBDocument11 pagesPredictors of Tuberculosis (TBchikomuezza19No ratings yet
- Marzieh Shareizaei - Et.alDocument7 pagesMarzieh Shareizaei - Et.alkang.asep008No ratings yet
- Pone 0142607 PDFDocument9 pagesPone 0142607 PDFNurul Muqarribah Pratiwi IshaqNo ratings yet
- Healthmed 15 1 Damir SecicDocument6 pagesHealthmed 15 1 Damir SecicEdoHNo ratings yet
- Update in TBC and Non TBCDocument5 pagesUpdate in TBC and Non TBCReynaVG19No ratings yet
- Treatment Outcome and Mortality: Their Predictors Among HIV/TB Co-Infected Patients From IranDocument5 pagesTreatment Outcome and Mortality: Their Predictors Among HIV/TB Co-Infected Patients From Iranali aliNo ratings yet
- Avicenna JMedDocument5 pagesAvicenna JMedJehangir AllamNo ratings yet
- Tobacco ExposureDocument12 pagesTobacco ExposureHenny WijayaNo ratings yet
- Penjelasan JurnalDocument12 pagesPenjelasan JurnalPramestiNo ratings yet
- Never Smokers With Lung Cancer in Morocco: Epidemiology and Gender DifferencesDocument6 pagesNever Smokers With Lung Cancer in Morocco: Epidemiology and Gender DifferencesIJPHSNo ratings yet
- Tuberkulosis Paru Dan Analisis Faktor-Faktor Yang Mempenyaruhi Tingginya Angka Kejadiannya Di Indonesia Tahun 2007Document8 pagesTuberkulosis Paru Dan Analisis Faktor-Faktor Yang Mempenyaruhi Tingginya Angka Kejadiannya Di Indonesia Tahun 2007Bagus Ayu PurnamasariNo ratings yet
- Smoking: Effects On Multiple Sclerosis Susceptibility and Disease ProgressionDocument10 pagesSmoking: Effects On Multiple Sclerosis Susceptibility and Disease Progressionfarah maulida martaNo ratings yet
- Tuberculosis: A Global Health Problem: EditorialDocument3 pagesTuberculosis: A Global Health Problem: EditorialzihanNo ratings yet
- Pengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotoDocument8 pagesPengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotohompalahompalaNo ratings yet
- Rujukan Peneltian Yag Menggunakan FisherDocument8 pagesRujukan Peneltian Yag Menggunakan FisherDwi YulNo ratings yet
- Inflammatory Potential of Diet and Risk of Laryngeal Cancer in A Case-Control Study From ItalyDocument8 pagesInflammatory Potential of Diet and Risk of Laryngeal Cancer in A Case-Control Study From ItalyFrizka ApriliaNo ratings yet
- A Randomized Controlled Trial of Smoking Cessation Methods in Patients Newly-Diagnosed With Pulmonary TuberculosisDocument9 pagesA Randomized Controlled Trial of Smoking Cessation Methods in Patients Newly-Diagnosed With Pulmonary TuberculosisAkhirul NuzulNo ratings yet
- Pulmonary Tuberculosis and Diabetes Mellitus: Co-Existence of Both Diseases in Patients Admitted in A Teaching Hospital in The Southwest of IranDocument4 pagesPulmonary Tuberculosis and Diabetes Mellitus: Co-Existence of Both Diseases in Patients Admitted in A Teaching Hospital in The Southwest of IranrutnomleniNo ratings yet
- Drug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaDocument16 pagesDrug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaaulianmediansyahNo ratings yet
- BBH 101h Written Report TBDocument11 pagesBBH 101h Written Report TBapi-608299493No ratings yet
- 2020 Article 63656Document10 pages2020 Article 63656SarmadNo ratings yet
- The Burden of Bacteriologically Negative TB DiagnosisDocument9 pagesThe Burden of Bacteriologically Negative TB DiagnosisMeiyanti MeiyantiNo ratings yet
- Jurnal TBC Inter 1Document5 pagesJurnal TBC Inter 1sekti lindaNo ratings yet
- Risk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewDocument11 pagesRisk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewKorwin TitlaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- Gsi Bioinfo Day1Document1 pageGsi Bioinfo Day1Ida NeniNo ratings yet
- Tips For A Reduction of False Positives in Manual RT-PCR Diagnostics of Sars-Cov-2Document7 pagesTips For A Reduction of False Positives in Manual RT-PCR Diagnostics of Sars-Cov-2Ida NeniNo ratings yet
- Tiket Garuda Rute Bengkulu - Jakarta 22 Oct 2021 (Ida)Document2 pagesTiket Garuda Rute Bengkulu - Jakarta 22 Oct 2021 (Ida)Ida NeniNo ratings yet
- Example Management ReviewDocument14 pagesExample Management ReviewIda NeniNo ratings yet
- Schedule Training QHSE 2021-Aljabar T&CDocument14 pagesSchedule Training QHSE 2021-Aljabar T&CIda NeniNo ratings yet
- Life-Cycle Environmental Impact Assessment of Mineral IndustriesDocument8 pagesLife-Cycle Environmental Impact Assessment of Mineral IndustriesIda NeniNo ratings yet
- Em Oranau: A Revision of The System of Nomenclature For Influenza Viruses: A WHO MemorandumDocument7 pagesEm Oranau: A Revision of The System of Nomenclature For Influenza Viruses: A WHO MemorandumIda NeniNo ratings yet
- Article WJPR 1438667348Document40 pagesArticle WJPR 1438667348Ida NeniNo ratings yet
- Interim Guidelines For Collecting & Handling of Clinical Specimens For COVID - Oct 25, 21Document9 pagesInterim Guidelines For Collecting & Handling of Clinical Specimens For COVID - Oct 25, 21Ida NeniNo ratings yet
- Intuitive Eating Is Associated With Glycemic Control in Type 2 DiabetesDocument12 pagesIntuitive Eating Is Associated With Glycemic Control in Type 2 DiabetesiaiafgdoNo ratings yet
- Moa PCMDocument32 pagesMoa PCMHinaRaviNo ratings yet
- Musculoskeletal Ultrasound For Interventional PhysiatryDocument15 pagesMusculoskeletal Ultrasound For Interventional PhysiatryHoussem BejaouiNo ratings yet
- Growth Hormone Deficiency - A Case ReportDocument3 pagesGrowth Hormone Deficiency - A Case ReportAyiek WicaksonoNo ratings yet
- Diagnosis Banding Kejang DemamDocument7 pagesDiagnosis Banding Kejang DemamCesaNo ratings yet
- Principles For Aseptic Technique - Information For Healthcare Workers - December 2021Document5 pagesPrinciples For Aseptic Technique - Information For Healthcare Workers - December 2021ebubechukwu echefuNo ratings yet
- Chap 118Document5 pagesChap 118theodoruskevinNo ratings yet
- CH 38 - Bowel EliminationDocument10 pagesCH 38 - Bowel EliminationJose GonzalezNo ratings yet
- Arf & CRFDocument55 pagesArf & CRFPramidi VarijaNo ratings yet
- 117 Picu Nursing Research Priorities in The Uk and IrelandDocument1 page117 Picu Nursing Research Priorities in The Uk and IrelandDaniella AwurumibeNo ratings yet
- Multimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoDocument11 pagesMultimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoIJAR JOURNALNo ratings yet
- NCM 107 Postpartum Assessment BenitezDocument2 pagesNCM 107 Postpartum Assessment BenitezJaye Aprile Adrianne KuizonNo ratings yet
- Discussion About Labor and DeliveryDocument3 pagesDiscussion About Labor and DeliveryStudent NurseNo ratings yet
- Questions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Document13 pagesQuestions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Afni YunitaNo ratings yet
- J Jds 2020 05 016Document5 pagesJ Jds 2020 05 016Kim Chi NguyễnNo ratings yet
- Sequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4Document6 pagesSequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4kingpintamNo ratings yet
- Haemostasis and Thrombosis: An Overview: H. RascheDocument5 pagesHaemostasis and Thrombosis: An Overview: H. Rascheshinichi kudoNo ratings yet
- Nootropil Injection SMPC 2016 02 04Document11 pagesNootropil Injection SMPC 2016 02 04MarkusNo ratings yet
- Acsms Resources For The Exercise Physiologist 2nd Edition Ebook PDFDocument61 pagesAcsms Resources For The Exercise Physiologist 2nd Edition Ebook PDFjames.keeter432100% (48)
- Restless Leg Syndrome ...Document5 pagesRestless Leg Syndrome ...RidaNo ratings yet
- 6.2 Lesson Plan DIPLOMA in OncologyDocument14 pages6.2 Lesson Plan DIPLOMA in OncologyedrinsneNo ratings yet
- Prosthetic Rehabilitation OF Maxillary Defects: A ReviewDocument12 pagesProsthetic Rehabilitation OF Maxillary Defects: A ReviewragulNo ratings yet
- Resume Charlie Castro 2Document13 pagesResume Charlie Castro 2JasonV.PanayNo ratings yet
- Reni-Infectious Disease 100 SoalDocument61 pagesReni-Infectious Disease 100 SoalNur akilaNo ratings yet
- Slide Rehab MedikDocument18 pagesSlide Rehab MedikElfan Mahfuzh SmavenNo ratings yet
- Routes of Drug AdministrationDocument23 pagesRoutes of Drug Administrationrosalyn sugayNo ratings yet
- Acute Calculous CholecystitisDocument9 pagesAcute Calculous CholecystitisNoel LoayzaNo ratings yet
- Optical Coherence Tomography (OCT) in Neurologic DiseasesDocument232 pagesOptical Coherence Tomography (OCT) in Neurologic DiseasesirodalexandraNo ratings yet
- Covid 19 AwarenessDocument13 pagesCovid 19 AwarenessAsorihm MhirosaNo ratings yet
- Examination of Peripheral Nerve InjuriesDocument9 pagesExamination of Peripheral Nerve InjuriessarandashoshiNo ratings yet
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
Uploaded by
Ida NeniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
High Risk Behaviors Addiction: Association Between Tuberculosis and Smoking
Uploaded by
Ida NeniCopyright:
Available Formats
International Journal of
High Risk Behaviors
& Addiction
Association Between Tuberculosis and Smoking
Roya Alavi-Naini 1, Batool Sharifi-Mood 1, Maliheh Metanat 1*
1 Infectious Diseases and Tropical Medicine Research Center, Zahedan University of Medical Sciences, Zahedan, IR Iran
A R T I C LE I N FO A B S TR AC T
Article type: Background: The association between smoking and tuberculosis (TB), which has been
Original Article proven in multiple studies with different study population ethnicity, has not yet re-
ceived sufficient attention in terms of TB control.
Article history: Objectives: The aim of the present study was to determine the association between TB
Received: 18 Apr 2012 and cigarette smoking in southeastern Iran, an endemic area for tuberculosis.
Revised: 15 May 2012 Patients and Methods: This prospective case-control study conducted at a University-
Accepted: 20 May 2012 Affiliated Hospital (Boo-Ali Hospital, Zahedan, and Southeastern Iran) from March 2007
to March 2012 enrolled 253 TB patients and 312 healthy controls. Factors including his-
Keywords: tory of cigarette smoking, duration of smoking, number of cigarettes smoked per day,
Tuberculosis consumption of other drugs (parenteral and non-parenteral), and family history of tu-
Smoking berculosis and smoking, were evaluated in both cases and controls. Univarate and multi-
variate logistic regressions were performed to compare TB cases and controls. The odds
ratio (OR) and 95% confidence intervals (CI) were also estimated.
Results: The results of the study revealed a significant difference between TB and control
groups in relation to smoking (P < 0.0001). In multivariate logistic regression, cigarette
smokers were 3.1 (95% CI: 1.4-10.3) times more frequent in TB patients compared with con-
trols. Other factors that showed significant differences between TB patients and controls
were the use of non-parenteral drugs (OR = 3.6, 95% CI: 2.2-21.4), family history of TB (OR
= 6.6, 95% CI: 2.3-18.2), family history of smoking (OR = 2.8, 95% CI: 1.1-8.4), and smoking
history of more than 10 years (OR = 1.6, 95% CI: 1.2-9.8).
Conclusions: The present study evidenced the association between TB and smoking. It is
therefore recommended to include interventions for smoking cessation in the current
TB control practice. Copyright c 2012, Zahedan University of Medical Sciences; Published by Kowsar.
Implication for health policy/practice/research/medical education:
The aim of this study is to determine the association between TB and cigarette smoking in an endemic area for tuberculosis. In gen-
eral, the findings of this research are indicative of strong association between TB and smoking. These results prompt for including
interventions for smoking cessation in the current tuberculosis control practice.
Please cite this paper as:
Alavi-Naini R, Sharifi-Mood B, Metanat M. Association Between Tuberculosis and Smoking. Int J High Risk Behav Addict. 2012; 1(2): 71-4.
DOI: 10.5812/ijhrba.5215
1. Background in low- or middle-income countries, where the burden
of TB is also very high (1). The World Health Organization
Tuberculosis (TB) is one of the leading causes of death
reported that smoking causes 9% of all deaths worldwide
worldwide and remains a major public health burden
(2). Tobacco smoking has been shown to associate with
in many developing countries. Approximately 1.3 billion
TB infection. Moreover, cigarette smoking is also associ-
people smoke tobacco products and most of them live
ated with negative prognosis of TB (3). Smoking may af-
fect many organ systems, but the lungs suffer by far the
* Corresponding author: Maliheh Metanat, Infectious Diseases and Trop-
ical Medicine, Research Center Zahedan University of Medical Sciences, Za- most damage. Smoking damages the lungs and impacts
hedan, IR Iran. Tel: +98-5413228101, Fax: +98-5413228101, E-mail: malihemeta- the body’s immune system, making smokers more sus-
nat@yahoo.com. ceptible to TB infection. The occurrence of TB has been
Copyright c 2012, Zahedan University of Medical Sciences; Published by Kowsar.
shown to be linked to altered immune response and
Alavi-Naini R et al. Tuberculosis and Smoking
multiple defects in immune cells such as macrophages, Boo-Ali Hospital were recruited during the study period
monocytes and CD4 lymphocytes (4). Other mechanisms, and were matched for age and sex to TB patients. The in-
such as mechanical disruption of cilia function and hor- clusion criteria for normal healthy subjects were the ab-
monal effects, could also appear secondarily to smoking sence of clinical symptoms and signs suggestive for active
(5). Therefore, all these factors may contribute to the pulmonary tuberculosis and normal chest X-ray. Factors
increased susceptibility of an individual to develop TB including history of cigarette smoking, smoking dura-
infection. Several studies found that significantly more tion, number of cigarettes smoked per day, consumption
current smokers developed TB and subsequently died of other drugs (parenteral and non-parenteral), and fam-
within the follow-up period than non-smokers (6-8). It ily history of tuberculosis and smoking were registered
is possible that smoking increases the risk of relapse, by for both TB cases and controls. Comparison between TB
facilitating the persistence of M. Tuberculosis infection smokers and TB non-smokers were performed using the
after treatment and augments the risk for any residual M. SPSS 17.0 software version (IBM Corp., Armonk, NY, US)
Tuberculosis bacilli to promote infection that would lead and results with a P < 0.05 were considered statistically
to disease (3). Several cross-sectional case-control stud- significant. Both univariate and multivariate logistic re-
ies have reported the smoking - TB association (2,9,10). gressions were performed to compare cases and controls.
The most important cohort study on this matter was The odds ratio (OR) and 95% confidence intervals (95% CI)
conducted in India from 1991 to 2003, which presented were also estimated.
a strong evidence of this association (11). The necessity to
verify the certitude of cigarette smoking - TB association 4. Results
in the southeastern Iranian population constituted the
Among the 253 TB patients, 123 (48.6%) were males. Nine-
rationale for the present research.
ty seven (38.3%) of TB patients were more than 50 years old
2. Objectives
and 104 (41.1%) were cigarette smokers. One hundred fifty
four (49.3%) out of 312 controls were male and 116 (37.2%)
The aim of the present study was to determine the asso- of them were more than 50 years old. Cigarette smokers
ciation between TB and cigarette smoking in southeast- accounted 57 individuals (18.3%) in the control group.
ern Iran, an endemic area for tuberculosis. In univariate analysis, there was a significant difference
between TB and control group, in relation to smoking (P
3. Patients and Methods = 0.0001). One hundred and six of the TB smokers (42%)
had a history of non-parenteral consumption of drugs,
This prospective case-control study was conducted at a
especially opiate. Only 12 (4.7%) TB patients were intra-
university-affiliated hospital (Boo-Ali Hospital, Zahedan,
venous drug users. In the control group, 51 (16.3%) were
and southeastern Iran) from March 2007 to March 2012.
non-parenteral drug users and 10 (3.2%) used parenteral
Diagnosis of pulmonary TB patients was established on
drugs. There were no statistically significant differences
clinical findings, positive sputum smear for acid fast ba-
between the group of TB patients and controls according
cilli and the results of chest X-ray. Only patients who were
to use of parenteral drugs (P > 0.05), but a significant dif-
confirmed by microbial culture were included into the
ference was shown for non-parenteral drugs (P = 0.0001).
study. Therefore, 253 TB patients were included in the fi-
Human immunodeficiency virus (HIV) infections are not
nal analysis. Three hundred and twelve normal healthy
prevalent in southeastern Iran and tests for HIV detec-
subjects who underwent the physical examination at
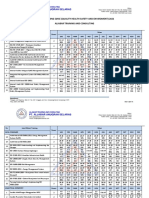
Table 1. General Characteristics of Tuberculosis Patients and Controls a
TB b Patients, No. (%) Controls, No. (%) P value
Age > 50, y 97 (38.3) 116 (37.2) 0.79
Sex, Male 123 (48.6) 154 (49.3) 0.87
Cigarette smokers 104 (41.1) 57 (18.3) 0.0001
Parental drug users 12 (4.7) 10 (3.2) 0.66
Non-parenteral drug users 106 (42) 51 (16.3) 0.0001
Smoked at least 30 cigarettes per day 65 (25.7) 58 (18.6) 0.051
Smoked for at least 10 years 78 (30.8) 68 (21.8) 0.016
HIV b positive 3 (1.2) 1 (0.3) -
Lived with anyone with TB b 53 (21) 12 (3.9) 0.0001
Lived with anyone who smoke 61 (24.3) 33 (10.6) 0.0001
a Patients and controls numbers are presented as absolute values and percentages, P < 0.05 was considered statistically significant
b Abbreviations: TB, tuberculosis; HIV, human immunodeficiency virus
72 Int J High Risk Behav Addict. 2012; 1(2)
Tuberculosis and Smoking Alavi-Naini R et al.
Table 2. Multivariate Analysis of Common Risk Factors Related to Smoking in Tuberculosis Patients Compared to Controls a
OR b 95% CI b P value
Cigarette smokers 3.1 1.4 - 10.3 0.001
Smoked at least 30 cigarettes a day 1.2 1.1 - 4.8 0.09
Smoked for at least 10 years 1.6 1.2 - 9.8 0.05
Non-parenteral drug users 3.6 2.2 - 21.4 0.012
b
Lived with anyone with TB 6.6 2.3 - 18.2 0.001
Lived with anyone who smoke 2.8 1.1 - 8.4 0.03
a
P < 0.05 was considered statistically significant.
b Abbreviations: CI, confidence interval; OR, odd ratio; TB, tuberculosis
tion were not requested for all patients. Therefore, only a quarter of all male deaths in middle age (6). Smoking
three out of 38 TB patients and one out of 24 controls, (OR = 2.53, 95% CI: 1.23–5.21) and living in an area where
with a high risk behavior, were reported positive for HIV the family health program was not implemented (OR =
infection. Family history of TB and smoking were the two 3.61, 95% CI: 1.46–8.93) were found to be independently
other risk factors that showed significant differences in associated with the relapse of TB, as indicated by the re-
TB patients and controls (P < 0.05) (Table 1). In multivari- port of Batista et al. in the northeast region of Brazil (13).
ate logistic regression (Table 2), cigarette smokers were 3.1 Similarly to our study, other researches carried out in the
(95% CI: 1.4-10.3) times more frequent in TB patients com- United Kingdom, Taiwan and China, revealed the strong
parer to controls. Other factors that presented significant association between TB and smoking, and the reduction
differences between TB patients and controls were the of TB risks by smoking cessation (9,12,14-16). Smoking
use of non-parenteral drugs (OR = 3.6, 95% CI: 2.2-21.4), a has been shown to significantly associate with a delay in
family history of TB (OR = 6.6, 95% CI: 2.3-18.2), a family his- sputum smear conversion time. In addition, exposure to
tory of smoking (OR = 2.8, 95% CI: 1.1-8.4), and history of second-hand smoke can also increase the risk for both TB
smoking for more than 10 years (OR = 1.6; 95% CI: 1.2-9.8). infection and development of active TB disease, among
children and adults. Therefore, TB patients who smoke at
5. Discussion home are also placing their families at a greater risk of
TB infection. Similar to other researches, the association
As mentioned previously, smoking is a well-recognized
between TB and smoking was demonstrated in our study.
major risk factor for the development of lung cancer,
It is therefore recommended to include interventions for
chronic obstructive pulmonary disease and other re-
smoking cessation in the current TB control practice.
spiratory infections, especially TB (10). While the rates
Acknowledgments
of smoking have declined in developed countries dur-
ing the past few decades, they have continued to rise in
less developed countries. As demonstrated in our study, We want to express our thanks to the Deputy of Re-
cigarette smoking was three times more frequent in TB search of the Zahedan University of Medical Sciences, for
patients, compared to healthy individuals. Common risk financial support. We also wish to bring our appreciation
factors related to smoking, such as smoking for more to Mrs. S. Mirfakhrai and Mrs. B. Pour-Afghan for technical
than 10 years, familial TB history, familial smoking his- support.
tory, and the use of non-parenteral drugs, were more
frequent in TB patients, compared with controls. Smok- Authors’ Contribution
ing has been associated with TB and mortality from TB
R Alavi-Naini carried out the design, coordinated the
in several studies (2,6,7,12). A 14-year prospective cohort
study and prepared the manuscript. B Sharifi-Mood pro-
study (1992–2006) carried out in South Korea from 1992 to
vided assistance in the design of the study and statistical
2006 revealed evidences that smoking increases the inci-
analysis. Maliheh Metanat edited the manuscript. All au-
dence of TB, the mortality rates from this disease, and TB
thors have read and approved the content of the manu-
recurrence (7). The adjusted risk of TB deaths among bidi
script.
smokers was 2.60 (95% CI: 2.02 - 3.33) times higher than for
Financial Disclosure
never-smokers, in a prospective study in Mumbai, India,
with a 4 years duration from 1999 to 2003. In this study,
approximately 32% of TB deaths could be attributable to None declared.
bidi smoking (11). In another study carried out in south-
ern India, smoking, which increases the incidence of clin- Funding/Support
ical TB, was the cause of half of the male TB deaths, and of This study was a part of a research project that was fi-
Int J High Risk Behav Addict. 2012; 1(2) 73
Alavi-Naini R et al. Tuberculosis and Smoking
nancially supported by the Research Council of Zahedan rean men and women. Am J Epidemiol. 2009;170(12):1478-85.
8. Lam TH, Ho SY, Hedley AJ, Mak KH, Peto R. Mortality and smoking
University.
in Hong Kong: case-control study of all adult deaths in 1998. BMJ.
References
2001;323(7309):361.
9. Tocque K, Bellis MA, Beeching NJ, Syed Q, Remmington T, Da-
vies PD. A case-control study of lifestyle risk factors associated
with tuberculosis in Liverpool, North-West England. Eur Respir J.
1. Shafey O, Fernandez E, Thun M, Schiaffino A, Dolwick S, Cokki-
nides V. Cigarette advertising and female smoking prevalence
2001;18(6):959-64.
in Spain, 1982-1997: case studies in International Tobacco Surveil-
lance. Cancer. 2004;100(8):1744-9.
10. Malin AS, McAdam KP. Escalating threat from tuberculosis: the
third epidemic. Thorax. 1995;50(Suppl 1):S37-42.
2. Zarocostas J. Twenty four risk factors responsible for nearly half
of annual deaths, says WHO. BMJ. 2009;339:b4439.
11. Pednekar MS, Gupta PC. Prospective study of smoking and tuber-
culosis in India. Prev Med. 2007;44(6):496-8.
3. Davies PD, Yew WW, Ganguly D, Davidow AL, Reichman LB, Dhe-
12. Lin HH, Ezzati M, Chang HY, Murray M. Association between to-
da K, et al. Smoking and tuberculosis: the epidemiological as-
sociation and immunopathogenesis. Trans R Soc Trop Med Hyg.
bacco smoking and active tuberculosis in Taiwan: prospective
cohort study. Am J Respir Crit Care Med. 2009;180(5):475-80.
2006;100(4):291-8.
13. d’Arc Lyra Batista J, de Fatima Pessoa Militao de Albuquerque M,
4. Altet MN, Alcaide J, Plans P, Taberner JL, Salto E, Folguera LI, et al.
de Alencar Ximenes RA, Rodrigues LC. Smoking increases the risk
of relapse after successful tuberculosis treatment. Int J Epidemiol.
Passive smoking and risk of pulmonary tuberculosis in children
immediately following infection. A case-control study. Tuber
Lung Dis. 1996;77(6):537-44.
2008;37(4):841-51.
14. Wang J, Shen H. Review of cigarette smoking and tuberculosis
5. Buskin SE, Gale JL, Weiss NS, Nolan CM. Tuberculosis risk factors
in adults in King County, Washington, 1988 through 1990. Am J
in China: intervention is needed for smoking cessation among
tuberculosis patients. BMC Public Health. 2009;9:292.
Public Health. 1994;84(11):1750-6.
15. Lin HH, Murray M, Cohen T, Colijn C, Ezzati M. Effects of smok-
6. Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortal-
ing and solid-fuel use on COPD, lung cancer, and tuberculosis in
China: a time-based, multiple risk factor, modelling study. Lan-
ity from tuberculosis and other diseases in India: retrospective
study of 43000 adult male deaths and 35000 controls. Lancet.
cet. 2008;372(9648):1473-83.
2003;362(9383):507-15.
16. Wen CP, Chan TC, Chan HT, Tsai MK, Cheng TY, Tsai SP. The reduc-
tion of tuberculosis risks by smoking cessation. BMC Infect Dis.
7. Jee SH, Golub JE, Jo J, Park IS, Ohrr H, Samet JM. Smoking and risk
of tuberculosis incidence, mortality, and recurrence in South Ko-
2010;10:156.
74 Int J High Risk Behav Addict. 2012; 1(2)
You might also like
- Tuberculosis, Smoking and Risk For Lung Cancer Incidence and MortalityDocument9 pagesTuberculosis, Smoking and Risk For Lung Cancer Incidence and MortalityarifahNo ratings yet
- Journal of Clinical Tuberculosis and Other Mycobacterial DiseasesDocument5 pagesJournal of Clinical Tuberculosis and Other Mycobacterial DiseasesputerinmNo ratings yet
- Jurnal Ke 2Document13 pagesJurnal Ke 2deroNo ratings yet
- Association Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalDocument5 pagesAssociation Between Smoking Habit and Pulmonary Tuberculosis at Dr. Soetomo General Academic HospitalairwanNo ratings yet
- Smoking Increases Risk of Recurrence After Successful Anti-Tuberculosis TreatmentDocument8 pagesSmoking Increases Risk of Recurrence After Successful Anti-Tuberculosis TreatmentRaditya Imam PratanaNo ratings yet
- Pulmonary Tuberculosis Specificities in Smokers: Egyptian Journal of Chest Diseases and TuberculosisDocument4 pagesPulmonary Tuberculosis Specificities in Smokers: Egyptian Journal of Chest Diseases and TuberculosisIntan TeraniaNo ratings yet
- Jurnal 10 HariantoDocument7 pagesJurnal 10 Hariantoaryzamelindah channelNo ratings yet
- JKMC, 2014 Issue2 (21-24)Document4 pagesJKMC, 2014 Issue2 (21-24)Jin SeonNo ratings yet
- Factors Associated With Mortality in Tuberculosis IranDocument4 pagesFactors Associated With Mortality in Tuberculosis IranMade NujitaNo ratings yet
- Mortality Among Tuberculosis Patients in The Democratic Republic of CongoDocument7 pagesMortality Among Tuberculosis Patients in The Democratic Republic of CongoGary Rios DionicioNo ratings yet
- Johanssen ReviewDocument16 pagesJohanssen Reviewsidra malikNo ratings yet
- Research On Prevalence of TB FinalDocument9 pagesResearch On Prevalence of TB FinalBontuNo ratings yet
- Which Patients Are Able To Adhere To Tuberculosis Treatment? A Study in A Rural Area in The Northwest Part of TurkeyDocument7 pagesWhich Patients Are Able To Adhere To Tuberculosis Treatment? A Study in A Rural Area in The Northwest Part of TurkeyAnonymous QPXAgjBwNo ratings yet
- Jact 12 I 2 P 142Document3 pagesJact 12 I 2 P 142Rosdiana Elizabeth Siburian0% (1)
- 1post-Class Quiz1 StudydesignsDocument14 pages1post-Class Quiz1 Studydesignssimplify8000No ratings yet
- Jurnal DR KrisDocument8 pagesJurnal DR KrisHiszom AsyhariNo ratings yet
- Bagi Retno Ariza Soeprihatini Soemarwoto (Inatime)Document6 pagesBagi Retno Ariza Soeprihatini Soemarwoto (Inatime)Dumora FatmaNo ratings yet
- Survival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorDocument10 pagesSurvival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorGetachew GemedaNo ratings yet
- Copd 2 263Document10 pagesCopd 2 263Vevi VarcetyNo ratings yet
- Title Subtle Presentation of Cryptic Tuberculosis in The ElderlyDocument25 pagesTitle Subtle Presentation of Cryptic Tuberculosis in The ElderlyHam FGNo ratings yet
- Diabetes Mellitus Among Tuberculosis Patients Admitted To The Pulmonarytuberculo PDFDocument5 pagesDiabetes Mellitus Among Tuberculosis Patients Admitted To The Pulmonarytuberculo PDFRinzyNo ratings yet
- EthiopiaDocument15 pagesEthiopiaVincentius Michael WilliantoNo ratings yet
- Boeck Ler 2009Document5 pagesBoeck Ler 2009l10n_assNo ratings yet
- Tuberculosis, Alcohol and Tobacco: Dangerous Liaisons: EditorialDocument2 pagesTuberculosis, Alcohol and Tobacco: Dangerous Liaisons: EditorialatikahanifahNo ratings yet
- Hubungan Pola Merokok Dengan Kejadian AsmaDocument11 pagesHubungan Pola Merokok Dengan Kejadian AsmaLivilia MiftaNo ratings yet
- Risk Factors For Interstitial Lung Disease 2018Document7 pagesRisk Factors For Interstitial Lung Disease 2018Mary CogolloNo ratings yet
- Environmental Toxins Harm Fetal Auditory PathwaysDocument4 pagesEnvironmental Toxins Harm Fetal Auditory PathwaysDinah Marie CarinoNo ratings yet
- Attique Corrected Paper 1Document12 pagesAttique Corrected Paper 1Mobin Ur Rehman KhanNo ratings yet
- Antibiotic Use and The Risk of Lung CancerDocument8 pagesAntibiotic Use and The Risk of Lung CancerBelajarNo ratings yet
- An Exploratory Study To Assess The Knowledge Regarding Side Effects of Anti - Tubercular Drugs and Its Self-Care Management Adapted by Tuberculosis PatientsDocument8 pagesAn Exploratory Study To Assess The Knowledge Regarding Side Effects of Anti - Tubercular Drugs and Its Self-Care Management Adapted by Tuberculosis Patientssaurabh kumar guptaNo ratings yet
- CAP - PrinaDocument12 pagesCAP - PrinaSalNo ratings yet
- Tobacco Smoke, Indoor Air Pollution and Tuberculosis: A Systematic Review and Meta-AnalysisDocument2 pagesTobacco Smoke, Indoor Air Pollution and Tuberculosis: A Systematic Review and Meta-AnalysisPutri ClaraNo ratings yet
- Cigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasDocument9 pagesCigarette Smoking and Health-Promoting Behaviours Among Tuberculosis Patients in Rural AreasMaria FulgensiaNo ratings yet
- THT JurnalDocument4 pagesTHT JurnalanugerahNo ratings yet
- (2020) Treatment Outcome of Tuberculosis Treatment Regimens in Kandahar, AfghanistanDocument7 pages(2020) Treatment Outcome of Tuberculosis Treatment Regimens in Kandahar, AfghanistanBilal Ahmad RahimiNo ratings yet
- Predictors of Tuberculosis (TBDocument11 pagesPredictors of Tuberculosis (TBchikomuezza19No ratings yet
- Marzieh Shareizaei - Et.alDocument7 pagesMarzieh Shareizaei - Et.alkang.asep008No ratings yet
- Pone 0142607 PDFDocument9 pagesPone 0142607 PDFNurul Muqarribah Pratiwi IshaqNo ratings yet
- Healthmed 15 1 Damir SecicDocument6 pagesHealthmed 15 1 Damir SecicEdoHNo ratings yet
- Update in TBC and Non TBCDocument5 pagesUpdate in TBC and Non TBCReynaVG19No ratings yet
- Treatment Outcome and Mortality: Their Predictors Among HIV/TB Co-Infected Patients From IranDocument5 pagesTreatment Outcome and Mortality: Their Predictors Among HIV/TB Co-Infected Patients From Iranali aliNo ratings yet
- Avicenna JMedDocument5 pagesAvicenna JMedJehangir AllamNo ratings yet
- Tobacco ExposureDocument12 pagesTobacco ExposureHenny WijayaNo ratings yet
- Penjelasan JurnalDocument12 pagesPenjelasan JurnalPramestiNo ratings yet
- Never Smokers With Lung Cancer in Morocco: Epidemiology and Gender DifferencesDocument6 pagesNever Smokers With Lung Cancer in Morocco: Epidemiology and Gender DifferencesIJPHSNo ratings yet
- Tuberkulosis Paru Dan Analisis Faktor-Faktor Yang Mempenyaruhi Tingginya Angka Kejadiannya Di Indonesia Tahun 2007Document8 pagesTuberkulosis Paru Dan Analisis Faktor-Faktor Yang Mempenyaruhi Tingginya Angka Kejadiannya Di Indonesia Tahun 2007Bagus Ayu PurnamasariNo ratings yet
- Smoking: Effects On Multiple Sclerosis Susceptibility and Disease ProgressionDocument10 pagesSmoking: Effects On Multiple Sclerosis Susceptibility and Disease Progressionfarah maulida martaNo ratings yet
- Tuberculosis: A Global Health Problem: EditorialDocument3 pagesTuberculosis: A Global Health Problem: EditorialzihanNo ratings yet
- Pengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotoDocument8 pagesPengaruh Dinamika Kelompok Sosial Terhadap Angka Kejadian Dan Penyembuhan Penyakit Tuberkulosis Paru Di Wilayah Puskesmas MojorotohompalahompalaNo ratings yet
- Rujukan Peneltian Yag Menggunakan FisherDocument8 pagesRujukan Peneltian Yag Menggunakan FisherDwi YulNo ratings yet
- Inflammatory Potential of Diet and Risk of Laryngeal Cancer in A Case-Control Study From ItalyDocument8 pagesInflammatory Potential of Diet and Risk of Laryngeal Cancer in A Case-Control Study From ItalyFrizka ApriliaNo ratings yet
- A Randomized Controlled Trial of Smoking Cessation Methods in Patients Newly-Diagnosed With Pulmonary TuberculosisDocument9 pagesA Randomized Controlled Trial of Smoking Cessation Methods in Patients Newly-Diagnosed With Pulmonary TuberculosisAkhirul NuzulNo ratings yet
- Pulmonary Tuberculosis and Diabetes Mellitus: Co-Existence of Both Diseases in Patients Admitted in A Teaching Hospital in The Southwest of IranDocument4 pagesPulmonary Tuberculosis and Diabetes Mellitus: Co-Existence of Both Diseases in Patients Admitted in A Teaching Hospital in The Southwest of IranrutnomleniNo ratings yet
- Drug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaDocument16 pagesDrug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaaulianmediansyahNo ratings yet
- BBH 101h Written Report TBDocument11 pagesBBH 101h Written Report TBapi-608299493No ratings yet
- 2020 Article 63656Document10 pages2020 Article 63656SarmadNo ratings yet
- The Burden of Bacteriologically Negative TB DiagnosisDocument9 pagesThe Burden of Bacteriologically Negative TB DiagnosisMeiyanti MeiyantiNo ratings yet
- Jurnal TBC Inter 1Document5 pagesJurnal TBC Inter 1sekti lindaNo ratings yet
- Risk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewDocument11 pagesRisk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewKorwin TitlaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 2: RespiratoryFrom EverandComplementary and Alternative Medical Lab Testing Part 2: RespiratoryNo ratings yet
- Gsi Bioinfo Day1Document1 pageGsi Bioinfo Day1Ida NeniNo ratings yet
- Tips For A Reduction of False Positives in Manual RT-PCR Diagnostics of Sars-Cov-2Document7 pagesTips For A Reduction of False Positives in Manual RT-PCR Diagnostics of Sars-Cov-2Ida NeniNo ratings yet
- Tiket Garuda Rute Bengkulu - Jakarta 22 Oct 2021 (Ida)Document2 pagesTiket Garuda Rute Bengkulu - Jakarta 22 Oct 2021 (Ida)Ida NeniNo ratings yet
- Example Management ReviewDocument14 pagesExample Management ReviewIda NeniNo ratings yet
- Schedule Training QHSE 2021-Aljabar T&CDocument14 pagesSchedule Training QHSE 2021-Aljabar T&CIda NeniNo ratings yet
- Life-Cycle Environmental Impact Assessment of Mineral IndustriesDocument8 pagesLife-Cycle Environmental Impact Assessment of Mineral IndustriesIda NeniNo ratings yet
- Em Oranau: A Revision of The System of Nomenclature For Influenza Viruses: A WHO MemorandumDocument7 pagesEm Oranau: A Revision of The System of Nomenclature For Influenza Viruses: A WHO MemorandumIda NeniNo ratings yet
- Article WJPR 1438667348Document40 pagesArticle WJPR 1438667348Ida NeniNo ratings yet
- Interim Guidelines For Collecting & Handling of Clinical Specimens For COVID - Oct 25, 21Document9 pagesInterim Guidelines For Collecting & Handling of Clinical Specimens For COVID - Oct 25, 21Ida NeniNo ratings yet
- Intuitive Eating Is Associated With Glycemic Control in Type 2 DiabetesDocument12 pagesIntuitive Eating Is Associated With Glycemic Control in Type 2 DiabetesiaiafgdoNo ratings yet
- Moa PCMDocument32 pagesMoa PCMHinaRaviNo ratings yet
- Musculoskeletal Ultrasound For Interventional PhysiatryDocument15 pagesMusculoskeletal Ultrasound For Interventional PhysiatryHoussem BejaouiNo ratings yet
- Growth Hormone Deficiency - A Case ReportDocument3 pagesGrowth Hormone Deficiency - A Case ReportAyiek WicaksonoNo ratings yet
- Diagnosis Banding Kejang DemamDocument7 pagesDiagnosis Banding Kejang DemamCesaNo ratings yet
- Principles For Aseptic Technique - Information For Healthcare Workers - December 2021Document5 pagesPrinciples For Aseptic Technique - Information For Healthcare Workers - December 2021ebubechukwu echefuNo ratings yet
- Chap 118Document5 pagesChap 118theodoruskevinNo ratings yet
- CH 38 - Bowel EliminationDocument10 pagesCH 38 - Bowel EliminationJose GonzalezNo ratings yet
- Arf & CRFDocument55 pagesArf & CRFPramidi VarijaNo ratings yet
- 117 Picu Nursing Research Priorities in The Uk and IrelandDocument1 page117 Picu Nursing Research Priorities in The Uk and IrelandDaniella AwurumibeNo ratings yet
- Multimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoDocument11 pagesMultimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoIJAR JOURNALNo ratings yet
- NCM 107 Postpartum Assessment BenitezDocument2 pagesNCM 107 Postpartum Assessment BenitezJaye Aprile Adrianne KuizonNo ratings yet
- Discussion About Labor and DeliveryDocument3 pagesDiscussion About Labor and DeliveryStudent NurseNo ratings yet
- Questions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Document13 pagesQuestions and Answer Group 3 "Glaucoma" Nama: Gustin Ibrahim Umamah Kelas: A S1 FARMASI 2017 NIM: 821417021Afni YunitaNo ratings yet
- J Jds 2020 05 016Document5 pagesJ Jds 2020 05 016Kim Chi NguyễnNo ratings yet
- Sequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4Document6 pagesSequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4kingpintamNo ratings yet
- Haemostasis and Thrombosis: An Overview: H. RascheDocument5 pagesHaemostasis and Thrombosis: An Overview: H. Rascheshinichi kudoNo ratings yet
- Nootropil Injection SMPC 2016 02 04Document11 pagesNootropil Injection SMPC 2016 02 04MarkusNo ratings yet
- Acsms Resources For The Exercise Physiologist 2nd Edition Ebook PDFDocument61 pagesAcsms Resources For The Exercise Physiologist 2nd Edition Ebook PDFjames.keeter432100% (48)
- Restless Leg Syndrome ...Document5 pagesRestless Leg Syndrome ...RidaNo ratings yet
- 6.2 Lesson Plan DIPLOMA in OncologyDocument14 pages6.2 Lesson Plan DIPLOMA in OncologyedrinsneNo ratings yet
- Prosthetic Rehabilitation OF Maxillary Defects: A ReviewDocument12 pagesProsthetic Rehabilitation OF Maxillary Defects: A ReviewragulNo ratings yet
- Resume Charlie Castro 2Document13 pagesResume Charlie Castro 2JasonV.PanayNo ratings yet
- Reni-Infectious Disease 100 SoalDocument61 pagesReni-Infectious Disease 100 SoalNur akilaNo ratings yet
- Slide Rehab MedikDocument18 pagesSlide Rehab MedikElfan Mahfuzh SmavenNo ratings yet
- Routes of Drug AdministrationDocument23 pagesRoutes of Drug Administrationrosalyn sugayNo ratings yet
- Acute Calculous CholecystitisDocument9 pagesAcute Calculous CholecystitisNoel LoayzaNo ratings yet
- Optical Coherence Tomography (OCT) in Neurologic DiseasesDocument232 pagesOptical Coherence Tomography (OCT) in Neurologic DiseasesirodalexandraNo ratings yet
- Covid 19 AwarenessDocument13 pagesCovid 19 AwarenessAsorihm MhirosaNo ratings yet
- Examination of Peripheral Nerve InjuriesDocument9 pagesExamination of Peripheral Nerve InjuriessarandashoshiNo ratings yet