Professional Documents
Culture Documents
The Use of Arthrocentesis in Patients With Temporomandibular Joint Disc Displacement Without Reduction
The Use of Arthrocentesis in Patients With Temporomandibular Joint Disc Displacement Without Reduction
Uploaded by
Angie CastilloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Use of Arthrocentesis in Patients With Temporomandibular Joint Disc Displacement Without Reduction
The Use of Arthrocentesis in Patients With Temporomandibular Joint Disc Displacement Without Reduction
Uploaded by
Angie CastilloCopyright:
Available Formats
RESEARCH ARTICLE
The use of arthrocentesis in patients with
temporomandibular joint disc displacement
without reduction
Eduardo Grossmann ID1☯*, Rodrigo Lorenzi Poluha2☯, Lilian Cristina Vessoni Iwaki2‡,
Rosângela Getirana Santana3‡, Liogi Iwaki Filho2‡
1 Department of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil,
2 Department of Dentistry, State University of Maringá, Maringá, Paraná, Brazil, 3 Department of Statistics,
State University of Maringá, Maringá, Paraná, Brazil
☯ These authors contributed equally to this work.
‡ These authors also contributed equally to this work.
* edugdor@gmail.com, grossmanneduardo@gmail.com
a1111111111
a1111111111
a1111111111 Abstract
a1111111111
a1111111111 The aim of this study was to evaluate the efficacy of the use of the arthrocentesis in patients
with disc displacement without reduction (DDWOR). Two hundred and thirty-four (234)
patients with DDWOR were evaluated and the following data collected: gender; affected
side; age (years); duration of the pain (months); patient’s perception of pain (measured by
OPEN ACCESS Visual Analogue Scale [VAS 0–10]); maximal interincisal distance (MID) (mm); and joint
Citation: Grossmann E, Poluha RL, Iwaki LCV, disc position, determined by magnetic resonance imaging. Data were obtained in two differ-
Santana RG, Iwaki Filho L (2019) The use of ent moments: before the arthrocentesis (M1) and three or four months later (M2). Paired t-
arthrocentesis in patients with temporomandibular Student Test, Scores Test and Wilcoxon Test showed a statistical significant difference
joint disc displacement without reduction. PLoS
(p<0.0001) between the M1 and M2 for the variables VAS and MID. There was an alteration
ONE 14(2): e0212307. https://doi.org/10.1371/
journal.pone.0212307 in the joint disc position in 93.88% of the cases after arthrocentesis. There was no associa-
tion between the general characteristics of the patients on the M1 and the results of the
Editor: Fabian Huettig, Eberhard-Karls-Universitat
Tubingen Medizinische Fakultat, GERMANY arthrocentesis (p>0.05). It can be concluded that the arthrocentesis is efficient in reducing
the pain, in increasing interincisal distance, and altering the joint disc position in patients
Received: January 22, 2018
with DDWOR regardless gender, age side and pain duration.
Accepted: January 31, 2019
Published: February 13, 2019
Copyright: © 2019 Grossmann et al. This is an
open access article distributed under the terms of
the Creative Commons Attribution License, which
permits unrestricted use, distribution, and
reproduction in any medium, provided the original Introduction
author and source are credited.
Among the different kinds of temporomandibular joint (TMJ) disorders, the displacement of
Data Availability Statement: All relevant data are the disc without reduction (DDWOR) has a prevalence of 35.7% [1]. In this condition, either
within the manuscript.
with the mouth open or closed, the disc remains anteriorly displaced in relation to the condyle,
Funding: The authors received no specific funding being pain and mouth opening limitation the main clinical features [2–4]. The treatment for
for this work. DDWOR should, at first, be a reversible and conservative one (drugs, interocclusal devices and
Competing interests: The authors have declared physiotherapy) [5], however if these methods are not efficient, surgical procedures should be
that no competing interests exist. considered [6].
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 1 / 10
Arthrocentesis in TMJ disc displacement without reduction
Arthrocentesis is a minimally invasive joint surgery and it is effective for decreasing pain,
increasing maximal interincisal distance, eliminating joint effusion and improving the oral
health related to the quality of life of the patients with TMJ disorders [6, 7]. It consists in wash-
ing the superior compartment of the TMJ, which is performed without a direct visualization of
the performance. The washing procedure is done using a biocompatible substance, such as a
physiological solution, which dilutes the local algogenic substances and frees the joint disc by
removing the adhesions formed between the surfaces of it and the mandibular fossa, which is
free due to the hydraulic pressure generated by the irrigation process [6, 8–11].
The arthrocentesis technique was introduced at about 30 years ago [8] and it has been
largely used along with other treatments, such as infiltrations of sodium hyaluronate [12],
intra-articular analgesics [13], corticosteroids [14] and platelet rich plasm [15]. However, the
literature has showed that an investigation regarding the isolated effects of the arthrocentesis
over the DDWOR along with a clinical analysis performed with the aid of the Magnetic Reso-
nance Imaging (MRI) may elucidate some of the benefits of this therapy.
Therefore, the aim of this study is to evaluate the efficacy of the arthrocentesis, alone, in
patients with DDWOR. The null hypothesis to be tested says that the results of the variables
studied here will not show any difference before and after the arthrocentesis.
Materials and methods
The research was approved by the Ethics Committee for Research on Humans of the State
University of Maringá (N˚: 1.751.299). A retrospective observational study was conducted
based on the Helsinki Declaration and recommendations of the report entitled Strengthening
the Reporting of Observational Studies in Epidemiology (STROBE) [16]. Data were collected
from the medical records of 400 patients in an orofacial pain and deformity centre (CEN-
DDOR) in Porto Alegre, Brazil, between January 2006 and May 2018. Clinical examinations
and procedures were conducted by the same surgeon (E.G.).
The patients included in the study should be 18 years old or above, have clinical symptoms
compatible with DDWOR and joint pain that did not respond to a conservative treatment for
at least three months (occlusal splints, anti-inflammatory drugs, compresses, soft diet and
physiotherapy). The diagnosis of DDWOR were confirmed by a combination of a clinical
examination based on the axis I of the Research Diagnostic Criteria for Temporomandibular
Disorders (RDC/TMD) [2] and by MRI reports.
About the initial 400 patients, 20 had incomplete medical records were excluded; 59 present
rheumatoid arthritis; 2 presented agenesis, 2 hyperplasia, 2 hypoplasia e 1 had a malignant
neoplasm in the condyle; 5 presented bone ankylosis; 15 had previous TMJ surgery; 10
reported extreme fear for needles; and 50 no performed a MRI before the arthrocentesis and
were also excluded from the sample. A total of 234 patients (245 TMJs) fit into the research
criteria.
The following variables were registered: gender; side affected by joint pain; age (years); pain
duration (months); patient’s pain perception (measured by Visual Analogue Scale–VAS (0–
10)); maximal interincisal distance (MID) (mm), measured by a digital calliper (Mitutoyo,
Takatsu-ku, Kawasaki, Kanagawa, Japan); and joint disc position, determined by MRI. The
data were obtained in two different moments: before the arthrocentesis (M1) and three to four
months later (M2).
Magnetic resonance images
MRI scans were obtained in a Magnetic Resonance device at 1.5 Tesla (Signa HDxt; GE
Healthcare, Milwaukee, WI, USA). Series of T1 weighted images were performed with a
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 2 / 10
Arthrocentesis in TMJ disc displacement without reduction
repetition time (RT) of 567 milliseconds and time echo (TE) of 11.4 milliseconds. The Series of
T2 weighted images were performed with a RT of 5.200 milliseconds and a TE of 168.5, with
bilateral spherical surface coil of 9cm diameter. The matrix used for T1 was 288 x 192, with
numbers of excitation NEX = 3; and for T2, 288 x 160, with NEX = 4; and with a field of view
(FOV) of 11x11 cm.
The MRI images were all analysed by the same radiologist, who based his analysis on the
studies of Ahmad et al. (2009) [3]. The reports obtained in the second MRI were used to clas-
sify the final position of the articular disc in relation to the first MRI, in three categories: No
change (NC); the disc remained in the initial position, but there was anterior and inferior
movement of the condyle during mouth opening (IPAIC); and, there was a more anterior and
inferior movement of the set of the condyle/disc in relation to the articular tubercle (MAICD).
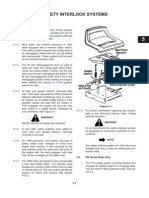
Arthrocentesis
The Arthrocentesis was performed once only in each of the indicated joint and the procedure
followed the technical references found in the literature [6,8, 10–15, 17] (Fig 1). A demo-
graphic pen was used to draw a straight line from the middle portion of the tragus to the cor-
ner side of the eyeball and two points were marked on this line for the insertion of the needles:
the first, the most posterior one, at a distance of 10 mm from the tragus and 2 mm below the
corner-tragus line; the second was inserted 20 mm anterior to the tragus and 10 mm inferior
to the corner-tragus line. Antisepsis was performed with 2% chlorhexidine solution that was
used all over the face, mainly in the preauricular area and ear. The next step was the auriculo-
temporal nerve block, followed by the anaesthesia of the posterior deep temporal and masseter
Fig 1. A: reference line and the two points for the insertion of the needles. B: first needle inserted. C: second needle
inserted. D: first needle connected with syringe and the second needle connected to a vacuum pump. The physiological
solution is administered in the first needle, get into the superior compartment of TMJ and got out by the second
needle.
https://doi.org/10.1371/journal.pone.0212307.g001
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 3 / 10
Arthrocentesis in TMJ disc displacement without reduction
nerves with lidocaine chloride without vasoconstrictor (Xylestesin 2%. Cristália, São Paulo,
São Paulo, Brazil), with a total volume of 3.6 mL. The patient was then requested to open the
mouth to the maximum, and a sterile mouth opener was placed on the contralateral side of the
procedure, allowing the displacement, down and forward, of the condyle, which enabled the
access to the posterior recess of the superior compartment of the temporomandibular joint
where the first needle 40x12 mm (18G) was introduced. The needle was then connected with a
5mL syringe and 4 mL physiological solution (PS), sodium chloride 0.9%, was administered in
order to distend the joint space. A second needle was introduced into the distended compart-
ment, at the point established before, and connected to a No˚ 20 long (60 cm) flexible and
transparent catheter connected to a vacuum pump (KaVo Vacuum, Kavo, Joinville, Santa
Catarina, Brazil), which allowed the visualization of the solution. Afterwards, an infusion
extender, 15C of 120 cm (Compojet Biomedica, Conceição do Jacuı́pe, Bahia, Brazil), was con-
nected to a 60 mL syringe to allow the joint lysis and lavage. A total of 300 mL of physiological
solution was used for the TMJ arthrocentesis. No other substance or drug was added to the
solution being injected. Once the procedure was completed, the needles were removed. Local
dressing was conducted with sterile gauze and micropore. After the procedure, the patients
were not recommended to use the occlusal splints or realized any other treatment, during the
follow-up period.
Statistical analysis
The individuals were considered as observational units; data were tabulated and submitted to a
descriptive analysis. The variables, VAS and MID, were evaluated before and after arthrocent-
esis (M1 and M2) and the results analysed by Paired Wilcoxon Test. In addition, univariate
analysis by logistic regression model was used to check if the characteristics of the patients col-
lected in the M1 (gender; affected side; age; pain duration) were responsible for the effects of
the arthrocentesis on the variables of interest (VAS and MID). All tests were performed with a
significance level of 5%. Data were analyzed using SAS version 9.3 (SAS Institute Inc., Cary,
NC, USA).
Results
The descriptive variables are shown in Table 1. The averages, standard deviation (±SD), mini-
mum, medium and maximum values of the VAS and MID variables are in Table 2.
The paired Wilcoxon test showed statistically significant differences (p < 0.0001) between
M1, before, and M2, after the arthrocentesis, for VAS and MID. The univariate analysis by
logistic regression model showed no association between the characteristics of the patients col-
lected in the M1 (gender; affected side; age; pain duration) with the results of VAS and MID
after the arthrocentesis (p>0.05).
Table 1. Distribution of the frequency, average and standard deviation (±SD) of the descriptive variables.
Female Male Total Sample
Gender 208 (88.88%) 26 (11.12%) 234 (100%)
Side of the complaint Right 110 (52.88%) 10 (38.46%) 120 (51.28%)
Left 89 (42.78%) 14 (53.84%) 103 (44.01%)
Both 9 (4.34%) 2 (7.70%) 11 (4.71%)
Age (years) 32.84±8.19 33.21±7.49 33.02±7.84
Pain Duration (months) 10.40±4.85 11.70±4.86 11.05±4.85
https://doi.org/10.1371/journal.pone.0212307.t001
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 4 / 10
Arthrocentesis in TMJ disc displacement without reduction
Table 2. Descriptive measures of the variables VAS and MID.
Measures VAS (0–10) MID (mm)
M1 Average ±SD 7.20±1.37 31.04±1.68
Minimum 5 25.17
Medium 8 30.49
Maximum 10 35.00
M2 Average ±SD 0.43±0.44 42.50±4.09
Minimum 0 37.14
Medium 0 45.22
Maximum 1 54.05
VAS: visual analogue scale. MID: maximal interincisal distance. M1: before the arthrocentesis. M2: three or four
months after arthrocentesis.
https://doi.org/10.1371/journal.pone.0212307.t002
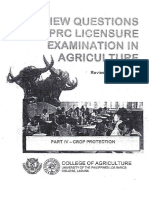
The results of the second MRI revealed that there was no change (NC, Fig 2) in 6.12% of the
cases; in 14.69% of the patients, the disc remained in the initial position, but there was an ante-
rior and inferior movement of the condyle during mouth opening (IPAIC, Fig 3); and in
79.19% of the cases there was a previous and inferior movement of the set of the condyle/disc
in relation to the articular tubercle (MAICD, Fig 4), suggesting a tendency towards this posi-
tion (Table 3).
Discussion
Although most DDWOR patients are asymptomatic, some individuals can experience pain
and reduced jaw mobility [18], being the arthrocentesis an effective treatment option for
DDWOR when conservative methods are no longer efficient [10]. The results of the present
study showed that DDWOR patients who underwent arthrocentesis had their VAS reduced
and MID increased (p<0.0001), which gave us support to reject the null hypothesis.
Pain is the most recurrent reason for patients to seek treatment for their TMJ [4], and
the earlier the patient undergoes treatment, the better the results are. Lately, arthrocentesis
Fig 2. NC example. A: before the arthrocentesis. B: four months after arthrocentesis.
https://doi.org/10.1371/journal.pone.0212307.g002
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 5 / 10
Arthrocentesis in TMJ disc displacement without reduction
Fig 3. IPAIC example. A: before the arthrocentesis. B: four months after arthrocentesis.
https://doi.org/10.1371/journal.pone.0212307.g003
has seemed to be more effective in treating pain [5], and some studies have also showed that
its cost-effectiveness has been superior to the more conservative approaches [19]. In the
present study, there was a significant reduction (p<0.0001) in the perception of pain after
arthrocentesis, with VAS values reducing from 7.20±1.37 to 0.43±0.44, being these values
similar to the ones found in other studies, from 8.7±1.1 to 1.13±1.16 [6] and from 6.45±1.17
to 1.12±0.42 [20].
The reduction of the pain is expected as the irrigation process, conducted with bio-compati-
ble substances, allows the removal of debris of the joint tissues in degeneration and eliminates
allogeneic substances, mainly inflammatory mediators [7, 10, 21]. The arthrocentesis is consid-
ered to be effective when there is a reduction of the levels of these mediators [22], being the
proper use of this technique highly important to achieve good results. In this study, was used
300 mL of physiological solution; however, recent literature has showed that smaller volumes
(50–200 mL) are equally effective to wash the upper compartment of the TMJ [23].
Despite reducing pain, the arthrocentesis performed under pressure may also present other
benefits to the patient, as it removes adherences, eliminates the negative pressure in the joint,
distends the joint space, recovering the space of the joint disc and fossa, changes the viscosity
of the synovial liquid, helps in the translation of the joint disc and condyle, and, consequently,
enlarges mouth opening [8, 24–27]. After arthrocentesis, our patients experienced an increase
in the maximum mouth opening, from 31.04±1.68 mm to 42.50±4.09 mm (p<0.0001), similar
to what has been found in other studies (from 23.7 ±2.91 mm to 41.05 ±2.91 mm) [20] and
(from 32.13±9.86 mm to 46.6±2.56) [6].
The proportion men: women were of 8:1, similar to the ones previously found in the litera-
ture [13, 28]. The higher incidence of DDWOR in women may be explained by some female
characteristics, such as a higher muscle laxity, higher intra-joint pressure and hormonal
changes [1, 29]. Regarding the side of the complaint, 95.29% of the patients presented unilat-
eral complaints, and 4.71% bilateral [1]. In agreement with previous studies [21, 23], the pres-
ent results showed no significant association between gender and the side of the joint in pain
with VAS and MID results (p>0.05). The average age of the patients was of 33.02±7.84, also
similar to the ones found in the literature [30]. However, there was no significant association
between the age and VAS and MID (p>0.05), as it would be predicted, as the literature has
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 6 / 10
Arthrocentesis in TMJ disc displacement without reduction
Fig 4. MAICD example. A: before the arthrocentesis. B: four months after arthrocentesis.
https://doi.org/10.1371/journal.pone.0212307.g004
showed that the rate of success of the arthrocentesis decreases as the age increases [31, 32].
Cases of DDWOR may be considered acute when the symptoms last for at least four months
[33]. In the present sample, the average time reported for pain duration was of 11.05±4.85
months and there was no association between pain duration and VAS and MID; however, the
literature has suggested that the arthrocentesis has more chance of being successful when
DDWOR patients have not been in pain for long [31].
Within time, the displaced joint disc becomes significantly deformed, and the retrodiscal
tissue becomes less flexible and more fibrous, which does not allow it to reposition itself along
the condyle, both in open and closed mouth [18, 22]. Our data showed an alteration in the
joint disc position in 93.88% of the cases after arthrocentesis (Table 3). From those, in 14.69%
of the patients the disc remained in the initial position, but there was an anterior and inferior
movement of the condyle during mouth opening; and in 79.19% of the cases there was a more
anterior and inferior movement of the set of the condyle/disc in relation to the articular tuber-
cle, being these changes probably due to combination of the following factors: distension of
the upper compartment, joint washing under certain pressure and joint manipulation. The
change in the position of the disc in DDWOR patients after arthrocentesis can be observed in
the techniques where one or two needles were used [34]. It was not possible to observe the full
return of the disc to its correct position in our sample, both with the mouth open and closed.
However, this is not necessary to relieve the pain and restore the proper function of the joint
Table 3. Distribution of the position of the TMJ disc according to the second MRI.
Position of the joint disc–MRI Female Male Total
(217 TMJs) (28 TMJs) (245 TMJs)
NC 13 (6%) 2 (7.14%) 15 (6.12%)
IPAIC 30 (13.82%) 6 (21.42%) 36 (14.69%)
MAICD 174 (80.18%) 20 (71.44%) 194 (79.19%)
NC: no change. IPAIC: the disc remained in the initial position, but there was anterior and inferior movement of the
condyle during mouth opening. MAICD: there was a more anterior and inferior movement of the set of the condyle/
disc in relation to the articular tubercle.
https://doi.org/10.1371/journal.pone.0212307.t003
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 7 / 10
Arthrocentesis in TMJ disc displacement without reduction
in patients with DDWOR [22, 27, 35], being the normalization of the functionality more
important than the re-establishment of the joint anatomy.
The minimally invasive character of the arthrocentesis produces less post-operative mor-
bidity if compared with other surgical techniques for the TMJ. The main disadvantages in rela-
tion to the arthroscopy is that: it is not possible to visualise the intra-joint pathology; there are
limitations for performing biopsies; and it is more difficult to eliminate adherences or adhe-
sions in more advanced stages [7, 10]. Although there was no complication associated to the
arthrocentesis in this study, the literature has reported some risks, such as: extravasation of liq-
uid to the surrounding tissue, lesion of the facial nerve, optical lesion, pre-auricular haema-
toma, arteriovenous fistula, trans articular perforation, intracranial perforation, extradural
haematoma and intra-articular problems [36].
This study was conducted in only one place and within a restricted population, so the
results should be carefully analysed, as there were some limitations. No control group was
used, as all the patients suffered from pain and restrictions to open the mouth and a control
group could have their disorders aggravated. Placebo was also not used due to ethical conflicts,
as we would have to perform the anaesthetic blocks and insert the needles without injecting
any substance. After the procedure, the patients were not recommended to use the occlusal
splints or realized any other treatment, during the follow-up period, so that there would be no
interference in the interpretation of the results. Although the follow-up period in the present
study ranged from 3 to 4 for months, the results tend to be long-lasting, once the literature has
shown good results for pain and jaw motion even after one year after the arthrocentesis [23].
Considering the results and the limitations of the present study, it can be concluded that
the arthrocentesis is efficient in reducing the pain, in increasing interincisal distance, and alter-
ing the joint disc position in patients with DDWOR regardless gender, age side and pain
duration.
Author Contributions
Conceptualization: Lilian Cristina Vessoni Iwaki.
Data curation: Eduardo Grossmann, Rosângela Getirana Santana.
Formal analysis: Rosângela Getirana Santana.
Investigation: Eduardo Grossmann, Rodrigo Lorenzi Poluha, Liogi Iwaki Filho.
Methodology: Eduardo Grossmann, Rodrigo Lorenzi Poluha.
Project administration: Eduardo Grossmann, Rodrigo Lorenzi Poluha.
Writing – original draft: Eduardo Grossmann, Rodrigo Lorenzi Poluha.
Writing – review & editing: Eduardo Grossmann, Lilian Cristina Vessoni Iwaki, Liogi Iwaki
Filho.
References
1. Lazarin RD, Previdelli IT, Silva RD, Iwaki LC, Grossmann E, Filho LI. Correlation of gender and age
with magnetic resonance imaging findings in patients with arthrogenic temporomandibular disorders: a
cross-sectional study. Int J Oral Maxillofac Surg. 2016; 45:1222–1228. https://doi.org/10.1016/j.ijom.
2016.04.016 PMID: 27197784
2. Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review criteria,
examinations and specifications, critique. J Craniomandib Disord. 1992; 6(4):301–350. PMID: 1298767
3. Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic cri-
teria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 8 / 10
Arthrocentesis in TMJ disc displacement without reduction
examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;
107:844–60. https://doi.org/10.1016/j.tripleo.2009.02.023 PMID: 19464658
4. Young AL. Internal derangements of the temporomandibular joint: a review of the anatomy, diagnosis,
and management. J Indian Prosthodont Soc. 2015; 15:2–7. https://doi.org/10.4103/0972-4052.156998
PMID: 26929478
5. Bouchard C, Goulet JP, El-Ouazzani M, Turgeon AF. Temporomandibular Lavage Versus Nonsurgical
Treatments for Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J Oral Maxillo-
fac Surg. 2017; 75(7):1352–1362. https://doi.org/10.1016/j.joms.2016.12.027 PMID: 28132759
6. Chandrashekhar VK, Kenchappa U, Chinnannavar SN, Singh S. Arthrocentesis a minimally invasive
method for TMJ disc disorders—A prospective study. J Clin Diagn Res. 2015; 9:59–62.
7. Song YL, Yap AU. Outcomes of therapeutic TMD interventions on oral health related quality of life: A
qualitative systematic review. Quintessence Int. 2018; 49(6):487–496. https://doi.org/10.3290/j.qi.
a40340 PMID: 29700502
8. Nitzan DW. Arthrocentesis-incentives for using this minimally invasive approach for temporomandibular
disorders. Oral Maxillofac Surg Clin North Am. 2006; 18:311–328. https://doi.org/10.1016/j.coms.2006.
03.005 PMID: 18088835
9. Vos LM, Stegenga B, Stant AD, Quik EH, Huddleston Slater JJ. Cost Effectiveness of Arthrocentesis
Compared to Conservative Therapy for Arthralgia of the Temporomandibular Joint: A Randomized Con-
trolled Trial. J Oral Facial Pain Headache. 2018; 32(2):198–207. https://doi.org/10.11607/ofph.1457
PMID: 29466475
10. Tatli U, Benlidayi ME, Ekren O, Salimov F. Comparison of the effectiveness of three different treatment
methods for temporomandibular joint disc displacement without reduction. Int J Oral Maxillofac Surg.
2017; 46(5):603–609. https://doi.org/10.1016/j.ijom.2017.01.018 PMID: 28222947
11. Tuz HH, Baslarli O, Adiloglu S, Gokturk T, Meral SE. Comparison of local and general anaesthesia for
arthrocentesis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2016; 54:946–949. https://doi.
org/10.1016/j.bjoms.2016.06.026 PMID: 27435500
12. Gurung T, Singh RK, Mohammad S, Pal US, Mahdi AA, Kumar M. Efficacy of arthrocentesis versus
arthrocentesis with sodium hyaluronic acid in temporomandibular joint osteoarthritis: A comparison.
Natl J Maxillofac Surg. 2017; 8(1):41–49. https://doi.org/10.4103/njms.NJMS_84_16 PMID: 28761275
13. Gopalakrishnan V, Nagori SA, Roy Chowdhury SK, Saxena V. The use of intra-articular analgesics to
improve outcomes after temporomandibular joint arthrocentesis: a review. Oral Maxillofac Surg. 2018;
22(4):357–364. https://doi.org/10.1007/s10006-018-0720-z PMID: 30196484
14. Davoudi A, Khaki H, Mohammadi I, Daneshmand M, Tamizifar A, Bigdelou M, et al. Is arthrocentesis of
temporomandibular joint with corticosteroids beneficial? A systematic review. Med Oral Patol Oral Cir
Bucal. 2018; 23(3):e367–e375. https://doi.org/10.4317/medoral.21925 PMID: 29680840
15. Lin SL, Tsai CC, Wu SL, Ko SY, Chiang WF, Yang JW. Effect of arthrocentesis plus platelet-rich plasma
and platelet-rich plasma alone in the treatment of temporomandibular joint osteoarthritis: A retrospec-
tive matched cohort study (A STROBE-compliant article). Medicine (Baltimore). 2018; 97(16):e0477.
16. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement:
guidelines for reporting observational studies. Int J Surg. 2014; 12(12):1495–9. https://doi.org/10.1016/
j.ijsu.2014.07.013 PMID: 25046131
17. Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint: an autopsy study. Int J Oral Surg.
1985; 14:169–175. PMID: 3920161
18. Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptom-
atic temporomandibular joint disc displacement without reduction. J Dent Res. 1998; 77:361–365.
https://doi.org/10.1177/00220345980770020401 PMID: 9465168
19. Vos LM, Stegenga B, Stant AD, Quik EH, Huddleston Slater JJ. Cost Effectiveness of Arthrocentesis
Compared to Conservative Therapy for Arthralgia of the Temporomandibular Joint: A Randomized Con-
trolled Trial. J Oral Facial Pain Headache. 2018; 32(2):198–207. https://doi.org/10.11607/ofph.1457
PMID: 29466475
20. Malik AH, Shah AA. Efficacy of temporomandibular joint arthrocentesis on mouth opening and pain in
the treatment of internal derangement of TMJ—A clinical study. J Oral Maxillofac Surg. 2014; 13:244–
248.
21. Grossmann E, Poluha RL, Iwaki LCV, Santana RG, Filho LI. Predictors of arthrocentesis outcome on
joint effusion in patients with disk displacement without reduction. Oral Surg Oral Med Oral Pathol Oral
Radiol. 2018; 125(4):382–388. https://doi.org/10.1016/j.oooo.2017.12.021 PMID: 29422400
22. Tvrdy P, Heinz P, Pink R. Arthrocentesis of the temporomandibular joint: a review. Biomed Pap Med
Fac Univ Palacky Olomouc Czech Repub. 2015; 59:31–34.
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 9 / 10
Arthrocentesis in TMJ disc displacement without reduction
23. Grossmann E, Poluha RL, Iwaki LCV, Iwaki Filho L. Arthrocentesis with different irrigation volumes in
patients with disc displacement without reduction: One-year follow-up. Cranio. 2018; 26:1–6.
24. Yura S, Totsuka Y, Yoshikawa T, Inoue N. Can arthrocentesis release intracapsular adhesions? Arthro-
scopic findings before and after irrigation under sufficient hydraulic pressure. J Oral Maxillofac Surg.
2003; 61:1253–1256. PMID: 14613079
25. Yura S, Totsuka Y. Relationship between effectiveness of arthrocentesis under sufficient pressure and
conditions of the temporomandibular joint. J Oral Maxillofac Surg. 2005; 63:225–228. https://doi.org/
10.1016/j.joms.2004.06.053 PMID: 15690292
26. Ohnuki T, Fukuda M, Nakata A, Nagai H, Takahashi T, Sasano T, et al. Evaluation of the position,
mobility, and morphology of the disc by MRI before and after four different treatments for temporoman-
dibular joint disorders. Dentomaxillofac Radiol. 2006; 35:103–109. https://doi.org/10.1259/dmfr/
25020275 PMID: 16549437
27. Sembronio S, Albiero AM, Toro C, Robiony M, Politi M. Is there a role for arthrocentesis in recapturing
the displaced disc in patients with closed lock of the temporomandibular joint? Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 2008; 105:274–280. https://doi.org/10.1016/j.tripleo.2007.07.003 PMID:
18061492
28. De Riu G, Stimolo M, Meloni SM, Soma D, Pisano M, Sembronio S, et al. Arthrocentesis and temporo-
mandibular joint disorders: clinical and radiological results of a prospective study. Int J Dent. 2013;
4:790648.
29. McCarroll RS, Hesse JR, Naeije M, Yoon CK, Hansson TL. Mandibular border positions and their rela-
tionships with peripheral joint mobility. J Oral Rehabil. 1987; 14:125–131. PMID: 3470462
30. Alajbeg IZ, Gikić M, Valentić-Peruzović M. Mandibular range of movement and pain intensity in patients
with anterior disc displacement without reduction. Acta Stomatol Croat. 2015; 49:119–27. https://doi.
org/10.15644/asc49/2/5 PMID: 27688394
31. Attia HS, Mosleh MI, Jan AM, Shawky MM, Jadu FM. Age, gender and parafunctional habits as prog-
nostic factors for temporomandibular joint arthrocentesis. Cranio. 2018; 36(2):121–127. https://doi.org/
10.1080/08869634.2017.1292175 PMID: 28266224
32. Kim YH, Jeong TM, Pang KM, Song SI. Influencing factor on the prognosis of arthrocentesis. J Korean
Assoc Oral Maxillofac Surg. 2014; 40:155–159. https://doi.org/10.5125/jkaoms.2014.40.4.155 PMID:
25247144
33. Ness GM: Temporomandibular joint arthrocentesis for acute or chronic closed lock. J Oral Maxillofac
Surg. 1996; 54:112–120.
34. Pasqual PGV, Poluha RL, Setogutti ÊT, Grossmann E. Evaluation of effusion and articular disc position-
ing after two different arthrocentesis techniques in patients with temporomandibular joint disc displace-
ment without reduction. Cranio. 2018; 30:1–8.
35. Moses JJ, Sartoris D, Glass R, Tanaka T, Poker I. The effect of arthroscopic surgical lysis and lavage of
the superior joint space on TMJ disc position and mobility. J Oral Maxillofac Surg. 1989; 47:674–678.
PMID: 2732826
36. Vaira LA, Raho MT, Soma D, Salzano G, Dell’aversana Orabona G, Piombino, De Riu G. Complications
and post-operative sequelae of temporomandibular joint arthrocentesis. Cranio. 2018; 36(4):264–267.
https://doi.org/10.1080/08869634.2017.1341138 PMID: 28618979
PLOS ONE | https://doi.org/10.1371/journal.pone.0212307 February 13, 2019 10 / 10
You might also like
- Full Download Ebook Ebook PDF Microbiology With Diseases by Taxonomy 5th Edition PDFDocument40 pagesFull Download Ebook Ebook PDF Microbiology With Diseases by Taxonomy 5th Edition PDFmicheal.cooper97498% (42)
- Bolens Lawn Tractor RepairDocument46 pagesBolens Lawn Tractor Repairdakehi1188342157% (7)
- Design Calculation of Working Platform-1Document26 pagesDesign Calculation of Working Platform-1Khandaker Khairul Alam100% (1)
- DD-110 110HFDocument290 pagesDD-110 110HFsergioNo ratings yet
- New American Paintings - December-January, 2019Document180 pagesNew American Paintings - December-January, 2019Fabio Nagual100% (2)
- Maptek I-Site Studio Geotechnical ModuleDocument4 pagesMaptek I-Site Studio Geotechnical ModulekennycasillaNo ratings yet
- Article IN Press: Pain Management NursingDocument8 pagesArticle IN Press: Pain Management NursingWahyu HidayatiNo ratings yet
- Article Double Puncture Versus Single Puncture Arthrocentesis For The 2018Document5 pagesArticle Double Puncture Versus Single Puncture Arthrocentesis For The 2018pedrofar-1No ratings yet
- BBRC Vol 14 No 04 2021-80Document5 pagesBBRC Vol 14 No 04 2021-80Dr Sharique AliNo ratings yet
- Distraction of The Temporomandibular Joint Condyle in Patients With Unilateral Non-Reducing Disc Displacement: Fact or Fiction?Document7 pagesDistraction of The Temporomandibular Joint Condyle in Patients With Unilateral Non-Reducing Disc Displacement: Fact or Fiction?Ana VelezNo ratings yet
- Fisioterapia Pós Artrocentese Bas2018Document18 pagesFisioterapia Pós Artrocentese Bas2018Wanniely KussNo ratings yet
- Joint Clicking With Oral Splints: A Randomized The Treatment of Painful TemporomandibularDocument8 pagesJoint Clicking With Oral Splints: A Randomized The Treatment of Painful TemporomandibularCaioSelaimenNo ratings yet
- 5509 19744 1 PBDocument5 pages5509 19744 1 PBCaioSelaimenNo ratings yet
- Efeoglu 2018Document7 pagesEfeoglu 2018Sree BanNo ratings yet
- Férula de Estabilización Oclusal para Pacientes Con Trastornos Temporomandibulares: Metanálisis de Los Efectos A Corto y Largo PlazoDocument21 pagesFérula de Estabilización Oclusal para Pacientes Con Trastornos Temporomandibulares: Metanálisis de Los Efectos A Corto y Largo PlazoMaritza AulestiaNo ratings yet
- Surgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialDocument10 pagesSurgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialFabian SanabriaNo ratings yet
- Splint Ont MuscleDocument6 pagesSplint Ont MuscleHồ TiênNo ratings yet
- Pinto 2019Document7 pagesPinto 2019Marcela RibeiroNo ratings yet
- Cohrt After Knee ArthoDocument8 pagesCohrt After Knee Arthoد.أحمد حسن جبريلNo ratings yet
- THA Polyethylene SurvivalDocument5 pagesTHA Polyethylene SurvivalCleff FlowersNo ratings yet
- BLL 2020 05 352Document6 pagesBLL 2020 05 352Benjamin O. ZuñigaNo ratings yet
- Jurnal Total Knee ArthroplastyDocument9 pagesJurnal Total Knee ArthroplastykiranaNo ratings yet
- Parker 2020Document6 pagesParker 2020QuiroprácticaParaTodosNo ratings yet
- Operative Treatment of Terrible Triad of TheDocument8 pagesOperative Treatment of Terrible Triad of TheAndrea OsborneNo ratings yet
- Farias 2016Document6 pagesFarias 2016Suli M ENo ratings yet
- Bone Reports: Case ReportDocument8 pagesBone Reports: Case ReportDaniella NúñezNo ratings yet
- Assessment of Occlusal Appliance For The Reposition of Temporomandibular Joint Anterior Disc Displacement With ReductionDocument4 pagesAssessment of Occlusal Appliance For The Reposition of Temporomandibular Joint Anterior Disc Displacement With ReductionSTEPHANIE JARAMILLONo ratings yet
- The Rationale of Surgical Treatment in Pediatric Spine TuberculosisDocument6 pagesThe Rationale of Surgical Treatment in Pediatric Spine TuberculosisSpica KentNo ratings yet
- Use of Transcutaneous Electrical Nerve Stimulation Device in Early Osteoarthritis of The KneeDocument7 pagesUse of Transcutaneous Electrical Nerve Stimulation Device in Early Osteoarthritis of The KneeAlifah Nisrina Rihadatul AisyNo ratings yet
- Ijss Aug Oa12Document5 pagesIjss Aug Oa12Herry HendrayadiNo ratings yet
- Comparative Assessment Between Ibuprofen, Chewing Gum, and Bite Wafers. SaudiDocument5 pagesComparative Assessment Between Ibuprofen, Chewing Gum, and Bite Wafers. SaudiTarif HamshoNo ratings yet
- AJODO-2013 Bradley 143 5 599Document3 pagesAJODO-2013 Bradley 143 5 599player osamaNo ratings yet
- Kjim 2017 304Document10 pagesKjim 2017 304edo adimastaNo ratings yet
- Jcpe 13246Document17 pagesJcpe 13246Dr. Pragyan SwainNo ratings yet
- Management of Infantile Blount'S Disease With Molded Orthoses: A New PerspectiveDocument5 pagesManagement of Infantile Blount'S Disease With Molded Orthoses: A New PerspectiveKrinta AlisaNo ratings yet
- Forgotten Joint Score PDFDocument8 pagesForgotten Joint Score PDFdeepakNo ratings yet
- Manual Therapy: Systematic ReviewDocument8 pagesManual Therapy: Systematic ReviewArlen EvelyNo ratings yet
- Advantages of Ultrasound Guidance For TMJ Arthrocentesis and Intra-Articular Injection: A Narrative ReviewDocument10 pagesAdvantages of Ultrasound Guidance For TMJ Arthrocentesis and Intra-Articular Injection: A Narrative Reviewnajimohammed020113No ratings yet
- Myofascial Trigger Points in Patients With Temporomandibular Joint Disc Displacement With Reduction: A Cross-Sectional StudyDocument7 pagesMyofascial Trigger Points in Patients With Temporomandibular Joint Disc Displacement With Reduction: A Cross-Sectional StudyfilzahNo ratings yet
- Comparison Between Outcomes of Dry Needling With Conventional Protocol and Rood's Approach With Conventional Protocol On Pain, Strength and Balance in Knee OsteoarthritisDocument29 pagesComparison Between Outcomes of Dry Needling With Conventional Protocol and Rood's Approach With Conventional Protocol On Pain, Strength and Balance in Knee OsteoarthritisDrPratibha SinghNo ratings yet
- 10 1016@j Jcms 2020 09 007Document6 pages10 1016@j Jcms 2020 09 007Sathyla Lander SelomNo ratings yet
- 4 03000605221103974Document13 pages4 03000605221103974Teuku FadhliNo ratings yet
- Osteoarthritis of The Temporomandibular Joint An Evaluation of The Effects and Complications of Corticosteroid Injection Compared With Injection With Sodium Hyaluronate PDFDocument7 pagesOsteoarthritis of The Temporomandibular Joint An Evaluation of The Effects and Complications of Corticosteroid Injection Compared With Injection With Sodium Hyaluronate PDFNado CuiabáNo ratings yet
- Post-Operative Clinical Outcomes in Patients With or Without The Use of Tourniquet in Total Knee Replacement SurgeryDocument3 pagesPost-Operative Clinical Outcomes in Patients With or Without The Use of Tourniquet in Total Knee Replacement SurgerymunazilatulchasanahNo ratings yet
- 1 s2.0 S1607551X11000805 MainDocument7 pages1 s2.0 S1607551X11000805 MainUlip KusumaNo ratings yet
- Hyaluronic Acid Injections For Pain Relief and Functional Improvement in Patients With Temporomandibular DisordersDocument17 pagesHyaluronic Acid Injections For Pain Relief and Functional Improvement in Patients With Temporomandibular Disorders林廷叡No ratings yet
- Piezosurgery Vs ConventionalDocument5 pagesPiezosurgery Vs ConventionalSaskia ParamitaNo ratings yet
- Piezosurgery Versus Rotatory Osteotomy in Mandibular Impacted Third Molar ExtractionDocument17 pagesPiezosurgery Versus Rotatory Osteotomy in Mandibular Impacted Third Molar ExtractionHUYNH TRINHNo ratings yet
- Full TextDocument7 pagesFull TextJuan Pablo Casanova AnguloNo ratings yet
- JCM 11 01202Document9 pagesJCM 11 01202anca_adam_26No ratings yet
- 190 Disc Repositioning Does It Really WorkDocument23 pages190 Disc Repositioning Does It Really WorkAngélica Valenzuela AndrighiNo ratings yet
- Overcoming Temporomandibular Joint Clicking and PainDocument4 pagesOvercoming Temporomandibular Joint Clicking and PainNatalie SalazarNo ratings yet
- Prolotherapy For Osteoarthritis and Tendinopathy: A Descriptive ReviewDocument8 pagesProlotherapy For Osteoarthritis and Tendinopathy: A Descriptive ReviewFisiatria UNNo ratings yet
- Efficacy of Musculoeskeletal Manual Approach in The Treatment of Temporomandibulaar Joint DisorderDocument8 pagesEfficacy of Musculoeskeletal Manual Approach in The Treatment of Temporomandibulaar Joint DisorderLaura Espejo SalamancaNo ratings yet
- 4 FQB GN 7 C YTf 5 GM FJJ PRs DZyDocument8 pages4 FQB GN 7 C YTf 5 GM FJJ PRs DZygck85fj8pnNo ratings yet
- Prolo TherapyDocument32 pagesProlo TherapySASIKALANo ratings yet
- TriggerfingerarticleDocument9 pagesTriggerfingerarticleRaviKumarNo ratings yet
- The Study To Assess The Effect of Prehabilitation On Postoperative Outcome of The Patients On Total Knee Arthroplasty at Selected HospitalDocument4 pagesThe Study To Assess The Effect of Prehabilitation On Postoperative Outcome of The Patients On Total Knee Arthroplasty at Selected HospitalEditor IJTSRDNo ratings yet
- ARS Part Time Use 2005Document6 pagesARS Part Time Use 2005Hồ TiênNo ratings yet
- 2021 Dextrose Prolotherapy in Knee Osteoarthritis A Systematic Review and Meta-AnalysisDocument10 pages2021 Dextrose Prolotherapy in Knee Osteoarthritis A Systematic Review and Meta-AnalysiswanhsiorthopedicsNo ratings yet
- Effectiveness of High Intensity Laser Therapy For Reduction of Pain in Knee OsteoarthritisDocument12 pagesEffectiveness of High Intensity Laser Therapy For Reduction of Pain in Knee OsteoarthritisGading Aurora100% (1)
- Measurement of Mandibular Movements in Patients With Temporomandibular Disorders and in Asymptomatic SubjectsDocument7 pagesMeasurement of Mandibular Movements in Patients With Temporomandibular Disorders and in Asymptomatic SubjectsMohammed FeroNo ratings yet
- 3 Febrero 2020 Is The Application of PlateletDocument18 pages3 Febrero 2020 Is The Application of PlateletFacundo Antonio AcevedoNo ratings yet
- Medicina: Fferent Treatments in Patients WithDocument10 pagesMedicina: Fferent Treatments in Patients WithDwi ApriyantiNo ratings yet
- 2012 Article 220Document5 pages2012 Article 220Ines Riera MoyaNo ratings yet
- Graftless Solutions for the Edentulous PatientFrom EverandGraftless Solutions for the Edentulous PatientSaj JivrajNo ratings yet
- Uwex 722 C Underwater Metal Detector: Operating InstructionsDocument20 pagesUwex 722 C Underwater Metal Detector: Operating InstructionsutvrdaNo ratings yet
- Part 4 Crop Protection Q ADocument54 pagesPart 4 Crop Protection Q AEleven HopperNo ratings yet
- United International University: EEE 424: Microprocessor and Interfacing Laboratory Experiment#5Document7 pagesUnited International University: EEE 424: Microprocessor and Interfacing Laboratory Experiment#5Nura Alam ProtikNo ratings yet
- Modül 17 Pervane Ders Notu (Sezai Turpçu) : PropellersDocument4 pagesModül 17 Pervane Ders Notu (Sezai Turpçu) : Propellersmevlüt said çalgınNo ratings yet
- MODULE-VIII Processing Seledted Food ItemDocument8 pagesMODULE-VIII Processing Seledted Food ItemKyla Gaile MendozaNo ratings yet
- EgyptDocument5 pagesEgyptLorenz Jedd GuañizoNo ratings yet
- Design of Hydraulic Structure - 1Document16 pagesDesign of Hydraulic Structure - 1aland pshtiwanNo ratings yet
- To Be Head Over All Things To The Church,: Ephesians 1 17-23 - 17Document4 pagesTo Be Head Over All Things To The Church,: Ephesians 1 17-23 - 17Niyi FunminiyiNo ratings yet
- Factores de Virulencia Del Streptococcus PneumoniaeDocument7 pagesFactores de Virulencia Del Streptococcus PneumoniaeFranklin ArandaNo ratings yet
- Microscopy and Differential Staining of BacteriaDocument9 pagesMicroscopy and Differential Staining of BacteriaSasha100% (2)
- Unit 5Document44 pagesUnit 5bereket gashuNo ratings yet
- Analog Communication W3Document9 pagesAnalog Communication W3Subhajit BhattacharyyaNo ratings yet
- TECHNOLOGY1 Answer-1Document6 pagesTECHNOLOGY1 Answer-1JlkKumarNo ratings yet
- The Legend of Lake TobaDocument2 pagesThe Legend of Lake Tobamesin cuci15No ratings yet
- Pallas Athena in AstrologyDocument1 pagePallas Athena in AstrologyMoraru Mariana0% (1)
- Cement - Quality Types & UsesDocument13 pagesCement - Quality Types & UsesRundhuNo ratings yet
- 5064 (UK) P392 BHL Product Brochure Issue6Document12 pages5064 (UK) P392 BHL Product Brochure Issue6Pawan SharmaNo ratings yet
- Tabatana 2023 ReportDocument15 pagesTabatana 2023 ReportKudakwashe Pride ChirendaNo ratings yet
- Standard Test Method For Relative Density (Specific Gravity) and Absorption of Coarse Aggregate (ASTM C127-15)Document2 pagesStandard Test Method For Relative Density (Specific Gravity) and Absorption of Coarse Aggregate (ASTM C127-15)culminasclairemaryNo ratings yet
- LabVentMgmt RPDocument100 pagesLabVentMgmt RPGanesh.MahendraNo ratings yet
- Certified Energy Manager ® Training Program: Outline & Study Guide (SI Units)Document11 pagesCertified Energy Manager ® Training Program: Outline & Study Guide (SI Units)EngSafwanQadousNo ratings yet
- Worksheet 1Document7 pagesWorksheet 1ndtitcNo ratings yet
- 2022 K 1600 Grand AmericaDocument8 pages2022 K 1600 Grand AmericaRashith TorresNo ratings yet
- Cambridge Primary Science Skills Builder 6 SampleDocument31 pagesCambridge Primary Science Skills Builder 6 SampleRuxandra Samaila75% (4)