Professional Documents
Culture Documents
Ajprenal 00066 2019
Ajprenal 00066 2019
Uploaded by
Milbanur MazidahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajprenal 00066 2019
Ajprenal 00066 2019
Uploaded by
Milbanur MazidahCopyright:
Available Formats
Am J Physiol Renal Physiol 317: F65–F72, 2019.
First published April 24, 2019; doi:10.1152/ajprenal.00066.2019.
RESEARCH ARTICLE
Mechanisms for falling urine pH with age in stone formers
Cameron J. Menezes,1 Elaine M. Worcester,1 Fredric L. Coe,1 John Asplin,2 Kristin J. Bergsland,1
and Benjamin Ko1
1
Department of Medicine, University of Chicago Medicine, Chicago, Illinois; and 2Litholink, Laboratory Corporation of
America Holdings, Chicago, Illinois
Submitted 12 February 2019; accepted in final form 22 April 2019
Menezes CJ, Worcester EM, Coe FL, Asplin J, Bergsland KJ, falls while that of uric acid stones rises (4, 22). Given that
Ko B. Mechanisms for falling urine pH with age in stone formers. Am alkaline urine pH fosters the former and acid pH the latter,
J Physiol Renal Physiol 317: F65–F72, 2019. First published April 24, these epidemiological data suggest that urine pH falls with age.
2019; doi:10.1152/ajprenal.00066.2019.—One of the main functions Indeed, in a cohort of recurrent calcium oxalate stone formers,
of the kidney is to excrete an acid load derived from both dietary and
endogenous sources, thus maintaining the pH of other fluids in the
Otto et al. (28) found that urine pH fell with age, although this
body. Urine pH is also of particular interest in stone formers, since it has not been studied in other groups.
determines the presence of either calcium phosphate or uric acid Such a fall in pH could, in turn, reflect changes in systemic
content in stones. Others have noted in epidemiological studies a rise acid-base balance, renal acidification mechanisms, or both. It is
in incidence of low pH-dependent uric acid stones with age, coincid- known that urine pH falls with glomerular filtration rate (GFR);
ing with a decrease in the incidence of high pH-dependent phosphate however, phosphate stone prevalence falls between early adult-
stones. Taken together, these trends are suggestive of a longitudinal hood and young middle age (4, 22, 31) while GFR declines
decline in urine pH in stone-forming patients, and, if true, this could later in life (31), suggesting that the mechanism for falling
explain the observed trends in stone incidence. We studied 7,891 urine pH is not a decline in renal function. Obesity and diabetes
stone formers, all of whom collected a 24-h urine sample and also lower urine pH (3, 21), the prevalence of both rise with
matching serum. Multivariate modeling revealed that urine pH did
indeed fall with age and particularly between the ages of 20 and 50 yr
age, and both are higher among uric acid stone formers than
old in both men and women. We sought to explain this trend through other stone formers (39). Although diabetes and obesity cer-
the inclusion of traditionally understood determinants of urine pH tainly occur even in early middle age, one might have expected
such as urinary buffers, estimates of glomerular filtration, and dietary more effects from both a decade later. In other words, the
acid load, but these, taken together, accounted for but a small fraction mechanism for this presumed urine pH change is not apparent.
of the pH fall. Gastrointestinal anion absorption was the strongest Therefore, we undertook an analysis of urine pH, renal
predictor of urine pH in all age groups, as we have previously reported acidification, and dietary acid-base contribution with age
in middle-aged normal men and women. However, we found that, using cross-sectional 24-h urine data from a large popula-
despite a decreasing urine pH, gastrointestinal anion absorption in- tion of stone formers ranging from 18 to ⬎70 yr of age. In
creased monotonically with age. In fact, after adjustment for gastro- particular, we sought to determine the effects of body mass
intestinal anion absorption, urine pH declined more markedly, sug-
gesting that bicarbonate-producing anion absorption is regulated in a
index, GFR, ammonia production, and gastrointestinal anion
manner that offsets the decline of urine pH. absorption (27).
We found that urine pH fell with age and, indeed, most
acid base; kidney stones; urine pH rapidly in the years in which stone phosphate content falls most
steeply. As one might expect given their higher prevalence of
phosphate stones, women produced urine of higher pH than
INTRODUCTION men at all ages. Straightforward multivariable analysis re-
vealed that age itself, separate from body mass index, renal
Systemic acid-base balance and renal acid excretion have a function, and gastrointestinal anion absorption, had a large and
special importance among stone-forming patients. Urine pH independent association with urine pH. Gastrointestinal anion
governs whether the stone mineral will be calcium phosphate absorption had a strong positive correlation with urine pH, but
or uric acid as opposed to the most common calcium oxalate gastrointestinal anion excretion increased with age as if in
crystal, which forms independent of urine pH. Because both compensation as opposed to cause.
calcium phosphate and uric acid stone formers plug terminal
nephrons more than calcium oxalate stone formers do, the METHODS
stone mineral phase affects the potential for kidney tissue Subjects and Data
damage (5, 40).
Elsewhere, we have presented evidence for a higher urine We used a large United States national data set of stone former
pH in normal women versus men (42). With age, especially pretreatment collections (Litholink, a Division of LabCorp). Each
among women, the abundance of calcium phosphate stones patient contributed one set of serum and 24-h urine data. The data set
included 12,839 patients (5,586 women and 7,253 men) from which
we excluded 4,948 (1,981 women and 2,967 men) because of missing
Address for reprint requests and other correspondence: B. Ko, Univ. of height, weight, or serum data, ammonia excretion ⬎ 100 mmol/day,
Chicago Medicine, Nephrology Section/MC 5100, 5841 S. Maryland Ave., citrate excretion ⬍ 30 mg/day, or body surface area ⬍ 1 m2. The
Chicago, IL 60637 (e-mail: bko@uchicago.edu). remaining 7,891 cases were divided into hexiles by age (Table 1).
http://www.ajprenal.org 1931-857X/19 Copyright © 2019 the American Physiological Society F65
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
F66 URINE pH AND GASTROINTESTINAL ANIONS WITH AGE
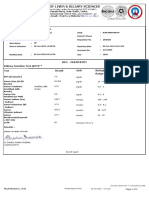
Table 1. Characteristics of age hexiles
Age Hexiles, yr
⬍33 33–42 42–49 49–56 56–64 ⬎64
Number
Women 821 681 559 568 525 452
Men 413 644 688 779 881 880
Age, yr
Women 26.0 ⫾ 0.2 37.0 ⫾ 0.1 45.2 ⫾ 0.1 51.9 ⫾ 0.1 59.2 ⫾ 0.1 70.4 ⫾ 0.3
Men 26.2 ⫾ 0.2 37.3 ⫾ 0.1 45.2 ⫾ 0.1 52.1 ⫾ 0.1 59.3 ⫾ 0.1 70.2 ⫾ 0.2
Weight, kg
Women 69.3 ⫾ 0.6 74.6 ⫾ 0.8 77.4 ⫾ 0.9 80.1 ⫾ 1.0 78.9 ⫾ 0.9 77.6 ⫾ 0.9
Men 83.9 ⫾ 0.8 91.8 ⫾ 0.8 93.6 ⫾ 0.7 93.8 ⫾ 0.7 94.6 ⫾ 0.7 88.9 ⫾ 0.6
Body mass index, kg/m2
Women* 25.9 ⫾ 0.2 27.9 ⫾ 0.3 28.7 ⫾ 0.3 30.1 ⫾ 0.3 29.8 ⫾ 0.3 29.8 ⫾ 0.3
Men* 26.4 ⫾ 0.2 29.1 ⫾ 0.8 29.2 ⫾ 0.2 29.5 ⫾ 0.2 29.7 ⫾ 0.2 28.2 ⫾ 0.2
Serum potassium
Women* 4.21 ⫾ 0.02 4.24 ⫾ 0.02 4.22 ⫾ 0.02 4.27 ⫾ 0.02 4.32 ⫾ 0.02 4.26 ⫾ 0.02
Men* 4.29 ⫾ 0.02 4.30 ⫾ 0.02 4.30 ⫾ 0.02 4.34 ⫾ 0.02 4.36 ⫾ 0.02 4.41 ⫾ 0.02
Serum total CO2
Women* 24.5 ⫾ 0.1 24.8 ⫾ 0.1 25.0 ⫾ 0.1 25.5 ⫾ 0.1† 25.7 ⫾ 0.1 25.7 ⫾ 0.1
Men 25.9 ⫾ 0.1 25.7 ⫾ 0.1 25.7 ⫾ 0.1 25.6 ⫾ 0.1 25.7 ⫾ 0.1 25.5 ⫾ 0.1
Values are means ⫾ SE. Trend analysis was undertaken for body mass index, potassium, and total CO2. *Significant linear trend, P ⬍ 0.001. Adjacent
difference analysis was undertaken only for serum analytes. †Significant difference (P ⬍ 0.001) from the previous hexile.
They were reasonably balanced with regard to sex ratio, age, weight, In the absence of urine total CO2 (TCO2), we were unable to
and body mass index. calculate net acid excretion (8). However, we performed some anal-
For each patient, we had available serum calcium, phosphorus, yses using the sum of ammonia and TA, which we termed “acid
magnesium, sodium, potassium, total CO2 content, chloride, uric acid, excretion” (AE).
and creatinine as well as the corresponding 24-h urine values for Creatinine clearance (CCr) was calculated as follows:
volume, pH, calcium, phosphorus, magnesium, sodium, potassium,
CCr ⫽ 共UC ⁄ serum creatinine兲 ⁄ 1, 440共ml · min⫺1 · 1.73 m2兲 (5)
uric acid, creatinine, oxalate, citrate, chloride, ammonium, and sulfate.
Analytes were measured using techniques previously described else- where UC ⫽ urine creatinine (mg/dl) ⫻ body surface area-adjusted
where (29, 30). volume [ml(1.73 m2) ⫻ body surface area].
Calculations Statistical Analysis
2
Urine excretions were calculated per 24 h per 1.73 m of body Comparisons across age hexiles by sex used fixed-effects multi-
surface. variable ANOVA, since each person had only one 24-h urine sample
We calculated titratable acidity (TA) as previously described (9). and paired serum. The significance of age effects was gauged using
Briefly, TA was calculated with the following equations derived from post hoc polynomial contrast testing of the ANOVA models (Systat
the Henderson-Hasselbalch relation, referring to the physiologically 13.2, San Jose, CA).
active pKa of the phosphate anion: Contrast testing assesses for the existence of a relationship across
antiph ⫽ 10共uph⫺6.8兲 (1) multiple levels of a variable with a specified polynomial form (linear,
quadratic, cubic, etc.) and returns an estimate of the coefficient of the
HP1 ⫽ 共antiph ⫻ p24M兲 ⁄ 共1 ⫹ antiph兲, highest-order polynomial of the equation defining the relationship
calculating the charge on phosphate at urine pH (2) between these levels. The null hypothesis is that the coefficient is
equal to zero, and a significant result demonstrates that the coefficient
HP2 ⫽ 共3.98 ⫻ p24M兲 ⁄ 4.98,
is nonzero. When adding adjusted variables to the ANOVA model, it
calculating the charge on phosphate at blood pH (3) is instructive to compare the magnitude of linear coefficients in
TA ⫹ HP2 ⫺ HP1 (4) particular, since these are a multivariate proxy of the slope of the
effect.
where antiph is the antilog of pH, uph is urine pH, and p24M is In our analysis, hexiles of age were ordered from youngest to
molality of phosphate in the 24-h urine collection. TA was expressed oldest, and variables of interest were tested with linear (order 1)
in millimoles per liter. polynomials with the exception of CCr, which was additionally tested
The value calculated from Eq. 4 is the concentration of titrated with a quadratic (order 2) polynomial.
protons, and multiplying by volume adjusted per 1.73 m2 body surface Figures 1– 6, displaying age hexiles, use dashed lines connecting
area returned the daily excretion of TA. adjacent hexile values for visual clarity.
Gastrointestinal anion levels were calculated as follows: 冱Na⫹ ⫹
K ⫹ Ca2⫹ ⫹ Mg2⫹ ⫺ 冱Cl⫺ ⫹ 1.8 ⫻ P, where all solutes were in
⫹
RESULTS
milliequivalents per liter except for P, which was in millimoles per
liter; multiplying by 1.8 converts P to milliequivalents per liter at Urine pH With Age
blood pH. Gastrointestinal anion levels in milliequivalents per liter
were then multiplied by the 24-h urine volume adjusted for body In men and women, urine pH fell with increasing age hexile
surface area. This composite variable represents gastrointestinal alkali (Fig. 1). pH decrements by hexile were significant (P ⬍ 0.01)
absorption and has been shown to correlate closely with anion ab- for all but the transitions between hexiles 3 and 4 and hexiles
sorptions measured in a total body balance study (27). 5 and 6 (men) as well as hexiles 4 and 5 and hexiles 5 and 6
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
URINE pH AND GASTROINTESTINAL ANIONS WITH AGE F67
Effect of Rising Body Mass Index
We (24) have previously shown the urine pH of stone-
forming patients falls with weight adjusted for urine creatinine,
a proxy for body mass index when height is not recorded. In
addition, Taylor and Curhan (38) have shown an inverse
association between urine pH and body mass index itself in
non-stone-forming patients. Therefore, increasing body mass
index with age could account for the fall in urine pH. Body
mass index rose with age (Fig. 2, top left, and Table 1) in both
men and women (linear contrast F ⫽ 146, both sexes com-
bined, P ⬍ 0.001). In ANOVA containing body mass index,
sex, and age hexile, all three factors were significant, but
adjusted urine pH fell with age with little change in the contrast
slope (Fig. 2, top right, and Table 2) compared with the
unadjusted slope for both sexes combined (Table 2).
Fig. 1. Urine pH versus age hexiles in men and women. Triangles, men; circles,
women. Values are means ⫾ SE. pH fell progressively in both sexes (linear
contrast for pH over age, F ⫽ 144 and 71, men and women, respectively, P ⬍ Effect of Falling Glomerular Filtration
0.001 for both). Dashed lines are for visual clarity only and imply no
interposed information. As expected, CCr fell with age (Fig. 2, bottom left). Unlike
urine pH, decrements for both sexes were not significant
(women). In other words, the older age hexile transitions were between the youngest three hexiles, in which urine pH most
not generally significant for either sex. The linear contrast for markedly fell. Even so, the contrast trend was significant (F ⫽
pH versus age was highly significant (F ⫽ 145 and 71, men 114 and 58, men and women, respectively, order 2, and F ⫽
and women, respectively, and 208 for both sexes combined, 925 and 585, men and women, respectively, order 1, all P ⬍
P ⬍ 0.001 for both; linear slope ⫽ ⫺0.227 and ⫺0.170, men 0.001). When added to body mass index (Table 2), CCr had no
and women, respectively, and ⫺0.198 for both sexes com- significant effect on the fall of urine pH with age. The adjusted
bined). urine pH values were therefore practically identical with those
Fig. 2. Body mass index (BMI) versus age hexile,
BMI-adjusted (Adj) urine pH, creatinine clearance
(CCr) versus age hexile, and BMI ⫹ CCr-adjusted
urine pH. Triangles, men; circles, women. Dashed
lines are for visual clarity only and imply no inter-
posed information. Values are means ⫾ SE. Linear
contrast F ⫽ 146, both sexes combined, P ⬍ 0.001.
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
F68 URINE pH AND GASTROINTESTINAL ANIONS WITH AGE
Table 2. ANOVA models
Model 1 Model 2 Model 3 Model 4
F Effect F Effect F Effect F Effect
Constant 6.47 6.42 6.55 5.9
Body mass index, kg/m2 295* ⫺0.14 294* ⫺0.14 364* ⫺0.15 170* ⫺0.08
Sex 99* Men ⫽ ⫺0.054 102* Men ⫽ ⫺0.056 73* Men ⫽ ⫺0.045 8* Men ⫽ ⫺0.012
Age, yr 32* ⫺0.167 25* ⫺0.186 25* ⫺0.159 113* ⫺0.266
Creatinine clearance 4 186* 0.04 19* 0.01
Urine ammonia 659* ⫺0.12
Urine sulfate 839* ⫺0.1
Gastrointestinal anion 6,299* 0.16
Serum total CO2 25* 0.09
Age ⫻ sex 3 † 3 † 4 † 4* †
Multiple R2 0.084 0.085 0.156 0.498
*Significance at P ⬍ 0.01; all effects except age were per 10 units of the variable; effects for age were the linear contrast slope. †Many cross products use
sex, not shown for lack of important contribution to the model.
from model 1 in Table 2 and the unadjusted value (compare left) and then declined over the latter three hexiles. In both
Fig. 2, right, top and bottom, vs. Fig. 1). sexes, linear contrast tests showed a highly significant relation-
Estimated GFR (eGFR) falls consistently with age (data not ship between ammonia excretion and age (F ⫽ 191 and 173,
shown; changes between each hexile P ⬍ 0.001) because the men and women, respectively, order 1, all P ⬍ 0.001). When
CKD-Epi eGFR algorithm has 0.993age as a multiplier (20). added to the ANOVA (Table 2), urine ammonia excretion had
Likewise, by design, eGFR was nearly identical for the sexes a large effect, and its addition improved the significance of the
within a given hexile, as the equation demands. For this reason, model (multiple R2 ⫽ 0.156). Urine pH still fell significantly
we do not offer a formal trend analysis. with age, albeit with a reduced contrast slope (Table 2).
Renal Acid Excretion With Age Titratable acidity and acid excretion. TA rose and then fell
(Fig. 3, top right). The behavior of TA with age is complex
Ammonia. Urine ammonia excretion rose (in women) or was because falling urine pH would increase it, whereas falling
stable (in men) over the first three hexiles of age (Fig. 3, top urine phosphate excretion (Fig. 3, bottom left) would decrease
Fig. 3. Urine ammonia (NH4), urine titratable acid-
ity (TA), urine phosphate (Phos), and urine acid
excretion (AE), all versus age hexile. Triangles,
men; circles, women. Dashed lines are for visual
clarity only and imply no interposed information.
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
URINE pH AND GASTROINTESTINAL ANIONS WITH AGE F69
Fig. 4. Urine sulfate and urine gastrointestinal (GI)
anion levels versus age hexile. Triangles, men; cir-
cles, women. Dashed lines are for visual clarity only
and imply no interposed information.
it. Being the sum of ammonia and TA, AE (Fig. 3, bottom Gastrointestinal anion levels. Gastrointestinal anion levels
right) rose and then fell. We do not offer a formal analysis of (METHODS) rose with age (linear contrast, F ⫽ 42 and 23, men
urine pH as a function of TA or AE, since TA was calculated and women, respectively, P ⬍ 0.001; Fig. 4, right). Notably,
using urine pH as an exponent (METHODS). whereas the overall trend of increase was significant in both
sexes, in women there were no differences between adjacent
Dietary Acid-Base Contribution hexiles, whereas in men there was a significant increase (P ⬍
Urine sulfate. Urine sulfate, taken as the dietary acid load 0.001) between hexiles 3 and 4. Mean gastrointestinal anion
(8), rose in men and women between the first two hexiles (Fig. values for women exceeded those for men in the youngest
4, left) and then remained more or less stable until the last hexile (P ⫽ 0.007), but the difference disappeared with age
hexile, when it decreased significantly. Despite the modestness such that the sex difference in the second hexile was of
of changes between hexiles, there was a significant linear borderline significance (P ⫽ 0.015). In all other hexiles, the
relationship between age and sulfate excretion in both sexes sexes did not differ.
(F ⫽ 16 and 27, men and women, respectively, P ⬍ 0.001), Role of urine potassium. Notably, all of the constituents of
mainly because of the decline in the terminal hexiles. At all gastrointestinal anions (Fig. 5) were constant or decreased with
ages, values for men far exceed women despite normalization age with the exception of potassium, which increased with age
for body surface area. This is well known within the United (linear contrast, F ⫽ 84 and 53, contrast slope ⫽ 7.06 and 5.49,
States population (28a). men and women, respectively, P ⬍ 0.001 for all comparisons).
Fig. 5. Urine excretion of the components of gastrointestinal anion levels versus age hexile. Triangles, men; circles, women. Filled symbols are urinary sodium
(UNa), urinary phosphate (UPhos) ⫻ 1.8, and urinary calcium (UCa); open symbols are urinary chloride (UCl), urinary potassium (UK), and urinary magnesium
(UMg). All values are in meq·day⫺1·1.73 m⫺2 body surface area. Dashed lines are for visual clarity only and imply no interposed information.
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
F70 URINE pH AND GASTROINTESTINAL ANIONS WITH AGE
In men, there were increases between hexiles 1 and 2 and and CCr covary and thus are not independent predictors of
hexiles 3 and 4, whereas in women, there was an increase urine pH.
between hexiles 1 and 2 (all P ⬍ 0.001). It is this increase in
urine potassium that drives the increase in calculated gastro- DISCUSSION
intestinal anion values.
Urine pH Falls With Age
Serum Measurements In this study of 7,891 stone-forming individuals, urine pH
Serum potassium. In addition to the notable increases in fell with age, most dramatically between the ages of 18 and 55
urinary potassium excretion, serum potassium also increased yr old. The decline echoes that seen in calcium oxalate stone
with age (linear contrast, F ⫽ 28 and 17, men and women, formers in a cohort that includes calcium oxalate, calcium
respectively, P ⬍ 0.001; Table 1). There were no significant phosphate, and urine acid stone formers (28). This finding
differences between adjacent hexiles in either sex despite likely explains why phosphate content in kidney stones de-
highly significant overall trends. creases with age while uric acid content rises (4, 13). Indeed,
Serum TCO2. Serum TCO2 also displayed age-related the fall in kidney stone phosphate content occurred most
changes (Table 1). In women, there was a significant upward between the ages of 18 and 50 yr old, coinciding with the
trend (linear contrast, F ⫽ 128, P ⬍ 0.001) and an increase decline in urine pH we observed. Similarly, the higher urine pH
between hexiles 3 and 4 (P ⬍ 0.001). In men, no such changes of women throughout all age groups probably explains their
were seen (linear contrast, F ⫽ 6, P ⫽ not significant). higher kidney stone phosphate content versus men (22).
Final ANOVA Model of Urine pH Our Data Exclude Certain Potential Mechanisms
The addition of gastrointestinal anions, urine sulfate, and Body mass index, CCr, urine ammonia. While consistent
serum TCO2 (Table 2) almost fully accounted for the sex with our understanding of kidney stone formation, the physi-
difference (Fig. 6). The decline of urine pH with age remained ological mechanisms of the age decline in urine pH are less
highly significant. Indeed, after full adjustment, the fall in urine clear. We (24) have previously shown that, in two separate
pH with age was monotonic, and, except for the final hexile in stone centers, urine pH fell with body weight adjusted for urine
women, every hexile was significantly lower than the previous, creatinine. In the present study, body mass index indeed
and the contrast slope was higher than the unadjusted value correlated inversely with urine pH, but this explains only a
(Table 2, compare model 4 with the unadjusted value of small fraction of the pH decline with age. Although CCr and
⫺0.198, both sexes combined). The overall regression now urine ammonia excretion strongly correlate with urine pH,
accounted for a highly significant fraction of the total variation these measures accounted for only a small fraction of the age
of urine pH with age (multiple R2 ⫽ 0.498). The effect size of effect.
gastrointestinal anions was particularly notable. Diabetes lowers urine pH (10), and its prevalence rises with
age. Most of our pH decline occurred between the ages of 30
Interactions Between CCr and Urine Ammonia and 50 yr old, whereas one would expect diabetes prevalence
to rise continuously after 50 yr old, as well. We cannot explore
Ammonia was not included in model 4 because of its close this possibility further with the information available except to
correlation with CCr. Inclusion of ammonia drastically reduced mention that a defect of renal ammonia production has been
the value of the F statistic of CCr (19 – 0.1) and did not greatly identified as an important contributor to low urine pH in
improve the variance explained by the model (multiple R2 ⫽ diabetes (35) and was not important as an explanation for what
0.498 vs. 0.505). Taken together, this implies that ammonia we found here.
Urine sulfate and gastrointestinal anions. Although urine
sulfate excretion correlated negatively with urine pH, it rose
very little between the ages of 30 and 50 yr old and actually fell
thereafter. In our models, its addition accounted for little of the
fall in pH. Gastrointestinal anion levels had a preponderant and
powerful positive correlation with urine pH. However, gastro-
intestinal anion levels rose with age, and, as currently under-
stood, this increase would tend to offset a fall in urine pH. In
fact, adjusting for gastrointestinal anions and urine sulfate
caused pH to fall more steeply and consistently.
Sex differences. Adjusting for gastrointestinal anion and
sulfate removed the majority of the urine pH difference be-
tween sexes. A diet consisting of greater amounts of fruits and
vegetables could contribute to the higher urine pH in women.
However, the fraction of diet gastrointestinal alkali absorbed
might also differ between the sexes. We have previously
shown in nonstone formers that higher urine pH in women is
Fig. 6. Fully adjusted urine pH versus age hexiles from model 4. Triangles, entirely related to their higher urine gastrointestinal anion
men; circles, women. Dashed lines are for visual clarity only and imply no excretion even though both sexes ate identical diets (42). Here,
interposed information. the adjustment for sex differences arose from both the higher
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
URINE pH AND GASTROINTESTINAL ANIONS WITH AGE F71
gastrointestinal anion levels in women and higher sulfate in increase in steady-state acid serum H⫹ in older individuals (6).
men. A detailed examination of bicarbonate balance across multiple
data sets is necessary to explain this finding and is worthy of
Urine Potassium Rises With Age further study. Experiments targeted at explaining this phenom-
enon will need to include urine collections to preserve TCO2
This is the immediate arithmetic cause of the increase in and likewise direct measurement of total urine organic ions
gastrointestinal anion levels. All of the other constituents of the (33, 34).
urine charge difference from which gastrointestinal anion level
is calculated (Na⫹, Mg2⫹, Ca2⫹, Cl⫺, and PO1.8 ⫺
4 ) either
Potential Limitations of This Study
remained steady or declined with age. Although declines in the The study sample comes from a testing laboratory popula-
excretion of either Cl⫺ or PO1.8 4
⫺
could account for the change tion, so it is possible that uric acid stone formers are selectively
in calculated gastrointestinal anion levels, in our data set enriched in our data set. Their urine pH would be particularly
changes in urinary potassium excretion accounted for ⬎90% of low and would downweight the average urine pH with age.
the changes in gastrointestinal anion levels. In addition to the However, in a similar laboratory testing population (22), uric
increased urinary excretion of potassium, we also observed an acid stones were only ~8% in women and 12% in men from the
increase in serum potassium. Taken together, these phenomena ages of 50 –59 yr old, by which point most of the decline in
suggest that potassium intake, gastrointestinal potassium han- urine pH has occurred.
dling, or perhaps both are subject to aging effects. The decrease on average from a urine pH of 6.2–5.9 appears
Diet. The increasing urine potassium could perhaps be diet a clinically modest one, since the median pH of 24-h urine
driven, caused by a move away from meats and toward fruits collections is ~6. However, this decrease of 0.3 pH units
and vegetables, favoring increased potassium alkali absorption. represents approximately two times the concentration of free
However, while some dietary changes occur through adult- protons in urine, which likely arises from a combination of
hood, it is unlikely that shifts in diet could cause the monotonic decreased urinary buffers and increased proton excretion, since
and isolated increase of potassium (12a). Our data cannot allow AE only falls by 25% over the same time period. Although not
us to pursue this matter in more detail. of apparent clinical significance, these observations indepen-
Transport selectivity. Selective net absorption of potassium, dently could account for the clinical observations of decreasing
perhaps with food anions, rather than age-driven changes in calcium phosphate stone content in aging (2).
food intake might play a major role in raising gastrointestinal In our study, the gastrointestinal anion level was estimated
anion absorption with age. Absorption of potassium has long via Oh’s formula (27), which has been confirmed to match that
been known to occur primarily in the small intestine (1), and determined in total body balance studies. It is possible that
the colon is the principal site of potassium secretion (36). A Oh’s relationship does not hold with aging, since the original
large number of potassium channels have been identified in the paper introducing the concept is based on a review of Lemann
gut (12); however, regulation of the transmembrane potassium and Relman’s research performed largely on young men (7,
transport events leading to gut net potassium absorption is not 14 –18, 27, 32). However, Oh’s method is based on physical
well elucidated, nor are any potential effects of age. This chemistry, molar balance, and conservation, which are unlikely
represents an important area for future study. to vary with age.
Although our work does not elucidate the mechanisms for
Anion Absorption the fall in urine pH with age, even in this selected population,
Gastrointestinal potassium and alkali absorption could be it does falsify the leading hypotheses concerning these mech-
coupled or could occur independent of each other. Although anisms based on present knowledge of acid-base physiology.
our data cannot test the possibility, gastrointestinal anion absorp- This was our intent, since it offers to other investigators
tion might increase in compensation for the factors reflected by opportunities for experiments concerning alternatives such as
a falling urine pH. In other words, gastrointestinal alkali abnormal conversion of diet anion to bicarbonate or perhaps
absorption might be regulated in response to rising systemic inadequacies of contemporary calculations of gastrointestinal
acid retention, for example. Such potential renal-gastrointesti- anions.
nal cross talk could act to offset increasing acid loads and Finally, and importantly, this data set is limited to a stone-
prevent metabolic acidosis. Such regulation could be because forming population. Therefore, it is unclear whether this phe-
of increased gastrointestinal transporter in situ activity or nomenon is limited to stone formers or is more generalizable to
abundance, as is seen with organic anion transporters (19). a larger population.
Alternatively, age-related changes in the microbiome could Summary
affect gastrointestinal alkali absorption, as has been proposed
by Maalouf et al. (11, 23). In conclusion, this work provides an explanation for the
decreasing prevalence of phosphate-based kidney stones seen
The Fall of Urine pH With Age Is Not Fully Accounted For in aging by demonstrating a progressive decline in urine pH in
stone-forming individuals. This decline seems ameliorated by
Multiple potential mechanisms exist that may explain the an increase in gastrointestinal alkali absorption with age. Both
remaining decline in urine pH with age. For instance, endo- of these findings need further investigation in the form of direct
thelin-1 levels rise with age (37), and Wesson and Dolson (41) experiments to fully elucidate the underlying mechanisms.
have demonstrated that endothelin-1 stimulates proton secre-
tion in the collecting duct. Alternatively, the fall of urine pH DISCLOSURES
may represent a consequence of the previously described No conflicts of interest, financial or otherwise, are declared by the authors.
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
F72 URINE pH AND GASTROINTESTINAL ANIONS WITH AGE
AUTHOR CONTRIBUTIONS polypeptide transporters. Am J Physiol Cell Physiol 296: C570 –C582,
2009. doi:10.1152/ajpcell.00436.2008.
C.J.M., E.M.W., F.L.C., K.J.B., and B.K. analyzed data; C.J.M., E.M.W.,
20. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd,
F.L.C., and B.K. interpreted results of experiments; C.J.M., E.M.W., F.L.C.,
Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J;
and K.J.B. prepared figures; C.J.M., E.M.W., F.L.C., and B.K. drafted man-
CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A
uscript; C.J.M., E.M.W., F.L.C., J.A., and B.K. edited and revised manuscript;
new equation to estimate glomerular filtration rate. Ann Intern Med 150:
C.J.M., E.M.W., F.L.C., J.A., K.J.B., and B.K. approved final version of
manuscript; E.M.W. and F.L.C. conceived and designed research. 604 –612, 2009. doi:10.7326/0003-4819-150-9-200905050-00006.
21. Li WM, Chou YH, Li CC, Liu CC, Huang SP, Wu WJ, Chen CW, Su
REFERENCES CY, Lee MH, Wei YC, Huang CH. Association of body mass index and
urine pH in patients with urolithiasis. Urol Res 37: 193–196, 2009.
1. Agarwal R, Afzalpurkar R, Fordtran JS. Pathophysiology of potassium doi:10.1007/s00240-009-0194-4.
absorption and secretion by the human intestine. Gastroenterology 107: 22. Lieske JC, Rule AD, Krambeck AE, Williams JC, Bergstralh EJ,
548 –571, 1994. doi:10.1016/0016-5085(94)90184-8. Mehta RA, Moyer TP. Stone composition as a function of age and sex.
2. Bergsland KJ, Coe FL, Parks JH, Asplin JR, Worcester EM. Evidence Clin J Am Soc Nephrol 9: 2141–2146, 2014. doi:10.2215/CJN.05660614.
for a role of PDZ domain-containing proteins to mediate hypophos- 23. Maalouf NM, Cameron MA, Moe OW, Sakhaee K. Metabolic basis for
phatemia in calcium stone formers. Nephrol Dial Transplant 33: 759 –770, low urine pH in type 2 diabetes. Clin J Am Soc Nephrol 5: 1277–1281,
2018. doi:10.1093/ndt/gfx284. 2010. doi:10.2215/CJN.08331109.
3. Carbone A, Al Salhi Y, Tasca A, Palleschi G, Fuschi A, De Nunzio C, 24. Maalouf NM, Sakhaee K, Parks JH, Coe FL, Adams-Huet B, Pak CY.
Bozzini G, Mazzaferro S, Pastore AL. Obesity and kidney stone disease: Association of urinary pH with body weight in nephrolithiasis. Kidney Int
a systematic review. Minerva Urol Nefrol 70: 393–400, 2018. doi:10. 65: 1422–1425, 2004. doi:10.1111/j.1523-1755.2004.00522.x.
23736/S0393-2249.18.03113-2. 27. Oh MS. A new method for estimating G-I absorption of alkali. Kidney Int
4. Daudon M, Doré JC, Jungers P, Lacour B. Changes in stone composition 36: 915–917, 1989. doi:10.1038/ki.1989.280.
according to age and gender of patients: a multivariate epidemiological 28. Otto BJ, Bozorgmehri S, Kuo J, Canales M, Bird VG, Canales B. Age,
approach. Urol Res 32: 241–247, 2004. doi:10.1007/s00240-004-0421-y. body mass index, and gender predict 24-hour urine parameters in recurrent
5. Evan AP, Lingeman JE, Worcester EM, Sommer AJ, Phillips CL, idiopathic calcium oxalate stone formers. J Endourol 31: 1335–1341,
Williams JC, Coe FL. Contrasting histopathology and crystal deposits in 2017. doi:10.1089/end.2017.0352.
kidneys of idiopathic stone formers who produce hydroxy apatite, brush- 28a.Panel on Dietary Reference Intakes for Electrolytes and Water;
ite, or calcium oxalate stones. Anat Rec (Hoboken) 297: 731–748, 2014. Standing Committee on the Scientific Evaluation of Dietary Reference
doi:10.1002/ar.22881. Intakes; Food and Nutrition Board. Dietary Reference Intakes for
6. Frassetto L, Sebastian A. Age and systemic acid-base equilibrium: Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: Na-
analysis of published data. J Gerontol A Biol Sci Med Sci 51: B91–B99, tional Academies, 2005.
1996. doi:10.1093/gerona/51A.1.B91. 29. Parks JH, Coe FL. A urinary calcium-citrate index for the evaluation of
7. Goodman AD, Lemann J Jr, Lennon EJ, Relman AS. Production, nephrolithiasis. Kidney Int 30: 85–90, 1986. doi:10.1038/ki.1986.155.
excretion, and net balance of fixed acid in patients with renal acidosis. J 30. Parks JH, Goldfischer ER, Coe FL. Changes in urine volume accom-
Clin Invest 44: 495–506, 1965. doi:10.1172/JCI105163. plished by physicians treating nephrolithiasis. J Urol 169: 863–866, 2003.
8. Hamm LL, Nakhoul N, Hering-Smith KS. Acid-base homeostasis. Clin doi:10.1097/01.ju.0000044922.22478.32.
J Am Soc Nephrol 10: 2232–2242, 2015. doi:10.2215/CJN.07400715. 31. Poggio ED, Rule AD, Tanchanco R, Arrigain S, Butler RS, Srinivas T,
9. Hamm LL, Simon EE. Roles and mechanisms of urinary buffer excre- Stephany BR, Meyer KH, Nurko S, Fatica RA, Shoskes DA, Krish-
tion. Am J Physiol 253: F595–F605, 1987. doi:10.1152/ajprenal.1987.253. namurthi V, Goldfarb DA, Gill I, Schreiber MJ Jr. Demographic and
4.F595. clinical characteristics associated with glomerular filtration rates in living
10. Hartman C, Friedlander JI, Moreira DM, Elsamra SE, Smith AD, kidney donors. Kidney Int 75: 1079 –1087, 2009. doi:10.1038/ki.2009.11.
Okeke Z. Differences in 24-h urine composition between nephrolithiasis
32. Relman AS, Lennon EJ, Lemann J Jr. Endogenous production of fixed
patients with and without diabetes mellitus. BJU Int 115: 619 –624, 2015.
acid and the measurement of the net balance of acid in normal subjects. J
doi:10.1111/bju.12807.
Clin Invest 40: 1621–1630, 1961. doi:10.1172/JCI104384.
11. Heintz C, Mair W. You are what you host: microbiome modulation of the
33. Ring T. Modeling amount of acid. Kidney Int 91: 1519 –1520, 2017.
aging process. Cell 156: 408 –411, 2014. doi:10.1016/j.cell.2014.01.025.
doi:10.1016/j.kint.2017.01.036.
12. Heitzmann D, Warth R. Physiology and pathophysiology of potassium
34. Ring T, Nielsen S. Whole body acid-base modeling revisited. Am J Physiol
channels in gastrointestinal epithelia. Physiol Rev 88: 1119 –1182, 2008.
doi:10.1152/physrev.00020.2007. Renal Physiol 312: F647–F653, 2017. doi:10.1152/ajprenal.00560.2016.
12a.Hoy MK, Goldman JD. Potassium Intake of the U.S. Population. What 35. Sakhaee K, Adams-Huet B, Moe OW, Pak CY. Pathophysiologic basis
We Eat in America, NHANES 2009 –2010. Beltsville, MD: United States for normouricosuric uric acid nephrolithiasis. Kidney Int 62: 971–979,
Department of Agriculture, 2012. 2002. doi:10.1046/j.1523-1755.2002.00508.x.
13. Knoll T, Schubert AB, Fahlenkamp D, Leusmann DB, Wendt-Nor- 36. Sorensen MV, Matos JE, Praetorius HA, Leipziger J. Colonic potas-
dahl G, Schubert G. Urolithiasis through the ages: data on more than sium handling. Pflugers Arch 459: 645–656, 2010. doi:10.1007/s00424-
200,000 urinary stone analyses. J Urol 185: 1304 –1311, 2011. doi:10. 009-0781-9.
1016/j.juro.2010.11.073. 37. Stauffer BL, Westby CM, DeSouza CA. Endothelin-1, aging and
14. Lemann J Jr, Lennon EJ, Goodman AD, Litzow JR, Relman AS. The hypertension. Curr Opin Cardiol 23: 350 –355, 2008. doi:10.1097/HCO.
net balance of acid in subjects given large loads of acid or alkali. J Clin 0b013e328302f3c6.
Invest 44: 507–517, 1965. doi:10.1172/JCI105164. 38. Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am
15. Lemann J Jr, Litzow JR, Lennon EJ. The effects of chronic acid loads J Kidney Dis 48: 905–915, 2006. doi:10.1053/j.ajkd.2006.09.004.
in normal man: further evidence for the participation of bone mineral in 39. Trinchieri A, Montanari E. Biochemical and dietary factors of uric acid
the defense against chronic metabolic acidosis. J Clin Invest 45: 1608 – stone formation. Urolithiasis 46: 167–172, 2018. doi:10.1007/s00240-017-
1614, 1966. doi:10.1172/JCI105467. 0965-2.
16. Lemann J Jr, Relman AS. The relation of sulfur metabolism to acid-base 40. Viers BR, Lieske JC, Vrtiska TJ, Herrera Hernandez LP, Vaughan
balance and electrolyte excretion: the effects of DL-methionine in normal LE, Mehta RA, Bergstralh EJ, Rule AD, Holmes DR III, Krambeck
man. J Clin Invest 38: 2215–2223, 1959. doi:10.1172/JCI104001. AE. Endoscopic and histologic findings in a cohort of uric acid and
17. Lennon EJ, Lemann J Jr, Litzow JR. The effects of diet and stool calcium oxalate stone formers. Urology 85: 771–776, 2015. doi:10.1016/
composition on the net external acid balance of normal subjects. J Clin j.urology.2014.12.036.
Invest 45: 1601–1607, 1966. doi:10.1172/JCI105466. 41. Wesson DE, Dolson GM. Endothelin-1 increases rat distal tubule acid-
18. Lennon EJ, Lemann J Jr, Relman AS. The effects of phosphoproteins ification in vivo. Am J Physiol 273: F586 –F594, 1997. doi:10.1152/
on acid balance in normal subjects. J Clin Invest 41: 637–645, 1962. ajprenal.1997.273.4.F586.
doi:10.1172/JCI104519. 42. Worcester EM, Bergsland KJ, Gillen DL, Coe FL. Mechanism for higher
19. Leuthold S, Hagenbuch B, Mohebbi N, Wagner CA, Meier PJ, Stieger urine pH in normal women compared with men. Am J Physiol Renal
B. Mechanisms of pH-gradient driven transport mediated by organic anion Physiol 314: F623–F629, 2018. doi:10.1152/ajprenal.00494.2017.
AJP-Renal Physiol • doi:10.1152/ajprenal.00066.2019 • www.ajprenal.org
Downloaded from journals.physiology.org/journal/ajprenal (114.125.205.057) on November 20, 2021.
You might also like
- Test Bank Radiographic Pathology For Technologists 8th Edition KowalczykDocument51 pagesTest Bank Radiographic Pathology For Technologists 8th Edition Kowalczykmarcuskenyatta275No ratings yet
- Complete Nephrology Revision - c25f1267 7e5b 4cbf b13f 699a5696711aDocument114 pagesComplete Nephrology Revision - c25f1267 7e5b 4cbf b13f 699a5696711aKumarNo ratings yet
- Acid Induced OsteoporosisDocument6 pagesAcid Induced OsteoporosisJosephine RobinsonNo ratings yet
- Assessment of Kidney Stone and Prevalence of Its Chemical CompositionsDocument3 pagesAssessment of Kidney Stone and Prevalence of Its Chemical CompositionsAnjan khadkaNo ratings yet
- En A Gic StudiesDocument116 pagesEn A Gic StudiessbivekNo ratings yet
- Sprague Dawley Rats Fed With SoymealDocument9 pagesSprague Dawley Rats Fed With SoymealFirdaus FirdausNo ratings yet
- World's Largest Science, Technology & Medicine Open Access Book PublisherDocument20 pagesWorld's Largest Science, Technology & Medicine Open Access Book PublisherraynanthaNo ratings yet
- Consenso Saha 2Document12 pagesConsenso Saha 2RobertoNo ratings yet
- Alkaline Water StudyDocument5 pagesAlkaline Water StudyKENS 5No ratings yet
- Stones in KidneyDocument7 pagesStones in Kidneygujji111No ratings yet
- Thesis Einddocument Sanne LeveringcopPDFDocument42 pagesThesis Einddocument Sanne LeveringcopPDFMartin WiniarskiNo ratings yet
- Jenis Batu TerbanyakDocument4 pagesJenis Batu TerbanyakNovita Anggun Permata SariNo ratings yet
- Calcium Oxalate Nephrolithiasis: An Easy Way To Detect An Imbalance Between Promoting and Inhibiting FactorsDocument7 pagesCalcium Oxalate Nephrolithiasis: An Easy Way To Detect An Imbalance Between Promoting and Inhibiting FactorsJames TerryNo ratings yet
- Uric Acid and Renal Function: Guilherme Ambrosio Albertoni, Fernanda Teixeira Borges and Nestor SchorDocument19 pagesUric Acid and Renal Function: Guilherme Ambrosio Albertoni, Fernanda Teixeira Borges and Nestor SchorYosuairvanNo ratings yet
- Pizzorno AcidosisDocument106 pagesPizzorno AcidosisAmber ChenNo ratings yet
- Pshychilogical JournalDocument7 pagesPshychilogical JournalHubbyNo ratings yet
- 10.1177 1756287210369121 PDFDocument7 pages10.1177 1756287210369121 PDFasfwegereNo ratings yet
- Validation of A Novel Diagnostic Test For Assessing The Risk of Urinary Uric ACID CRYSTALLIZACIONDocument6 pagesValidation of A Novel Diagnostic Test For Assessing The Risk of Urinary Uric ACID CRYSTALLIZACIONMARIANNE CASTILLO ESCOBARNo ratings yet
- Fras Set To 2018Document9 pagesFras Set To 2018Sanita AurinNo ratings yet
- Cejph - Cjp-Faktor Penyebab UrolithiasisDocument6 pagesCejph - Cjp-Faktor Penyebab UrolithiasisCDKadrianNo ratings yet
- 1223 Full-2Document15 pages1223 Full-26pb4rwpk45No ratings yet
- Protein Intake Calcium Balance and Health ConsequeDocument16 pagesProtein Intake Calcium Balance and Health ConsequeJoel LopezNo ratings yet
- The Role of Dietary Protein in The Pathogenesis of OsteoporosisDocument5 pagesThe Role of Dietary Protein in The Pathogenesis of OsteoporosisJoel LopezNo ratings yet
- Lifestyle Recommendations To Reduce The Risk of Kidney StonesDocument8 pagesLifestyle Recommendations To Reduce The Risk of Kidney Stonesjsali9210No ratings yet
- Pathophysiology-Based Treatment of UrolithiasisDocument7 pagesPathophysiology-Based Treatment of UrolithiasisLea Bali Ulina SinurayaNo ratings yet
- I R C U (Ircu) : V F U P W P S C R S ?Document15 pagesI R C U (Ircu) : V F U P W P S C R S ?Riot Riot AdjaNo ratings yet
- Caffeine Bone CalciumDocument8 pagesCaffeine Bone CalciumHerpika DianaNo ratings yet
- Batu EmepeduDocument9 pagesBatu Emepeduinneke sitompulNo ratings yet
- Acidosis Ruminal SubagudaDocument11 pagesAcidosis Ruminal SubagudaGabriela RiosNo ratings yet
- Dietary Oxalate and Kidney Stone Formation - PMCDocument12 pagesDietary Oxalate and Kidney Stone Formation - PMCRonNo ratings yet
- A Role For Uric Acid in The Progression of Renal DiseaseDocument10 pagesA Role For Uric Acid in The Progression of Renal DiseaseFausiah Ulva MNo ratings yet
- THE Composition OF Urinary Stones IN Central Sindh: Original ArticleDocument5 pagesTHE Composition OF Urinary Stones IN Central Sindh: Original ArticleShaheryar HasanNo ratings yet
- Protein & BoneDocument3 pagesProtein & BoneJoel LopezNo ratings yet
- Effects of Lactulose and Neomycin On Urea Metabolism in Cirrhotic SubjectsDocument5 pagesEffects of Lactulose and Neomycin On Urea Metabolism in Cirrhotic Subjectsnova adiNo ratings yet
- Toksik 2Document3 pagesToksik 2な ーNo ratings yet
- Coltherd Et Al 2021 BJN NOAEL P Sources Feline DietsDocument16 pagesColtherd Et Al 2021 BJN NOAEL P Sources Feline DietsannemabNo ratings yet
- Comparitive Study of Biochemical Bone Turnover Markers in Pre & Post-Menopausal WomenDocument3 pagesComparitive Study of Biochemical Bone Turnover Markers in Pre & Post-Menopausal Womenvenkateswarlu25No ratings yet
- Hypercalcemia and Calcium Oxalate Urolithiasis in Cats: A Report of Five CasesDocument5 pagesHypercalcemia and Calcium Oxalate Urolithiasis in Cats: A Report of Five CasesJean AmorinNo ratings yet
- Article Wjpps 1430385039Document7 pagesArticle Wjpps 1430385039Maipha DeapatiNo ratings yet
- Short-Chain Fatty Acids and Human Colonic Function: Roles of Resistant Starch and Nonstarch PolysaccharidesDocument34 pagesShort-Chain Fatty Acids and Human Colonic Function: Roles of Resistant Starch and Nonstarch Polysaccharidesbdalcin5512No ratings yet
- Original ArticleDocument6 pagesOriginal ArticleShwethaNo ratings yet
- Use of Non-Collagen Markers in Osteoporosis Studies: Calcified Tissue InternationalDocument5 pagesUse of Non-Collagen Markers in Osteoporosis Studies: Calcified Tissue InternationalDaniel SilvaNo ratings yet
- A Diet High in Meat Protein and Potential Renal Acid Load Increases Fractional Calcium Absorption and Urinary Calcium Excretion Without AffectingDocument7 pagesA Diet High in Meat Protein and Potential Renal Acid Load Increases Fractional Calcium Absorption and Urinary Calcium Excretion Without AffectingBruno CavicchioNo ratings yet
- 333 FullDocument6 pages333 FullHussein FaresNo ratings yet
- Whit FordDocument8 pagesWhit FordlarissatgrizzotNo ratings yet
- Treatment of Asymptomatic Hyperuricemia in Chronic Kidney DiseaseDocument4 pagesTreatment of Asymptomatic Hyperuricemia in Chronic Kidney DiseaseRonald Ariyanto WiradirnataNo ratings yet
- Current Concepts of And: Hyperuricemia GoutDocument13 pagesCurrent Concepts of And: Hyperuricemia GoutAnonymous h0XxWy8SNo ratings yet
- Dietary Carbohydrates and Lipid Metabolism PDFDocument5 pagesDietary Carbohydrates and Lipid Metabolism PDFNurmaNo ratings yet
- Nutrients: Calcium Oxalate Nephrolithiasis and Gut Microbiota: Not Just A Gut-Kidney Axis. A Nutritional PerspectiveDocument21 pagesNutrients: Calcium Oxalate Nephrolithiasis and Gut Microbiota: Not Just A Gut-Kidney Axis. A Nutritional PerspectiveVera VuchkovaNo ratings yet
- Bone Disease in Idiopathic Hypercalciuria: Ita P. Heilberg and Jose R. WeisingerDocument9 pagesBone Disease in Idiopathic Hypercalciuria: Ita P. Heilberg and Jose R. WeisingerRafael CastellarNo ratings yet
- Nurul Nabilah Azra Binti Nor A'zlan c11112863Document8 pagesNurul Nabilah Azra Binti Nor A'zlan c11112863tomeyttoNo ratings yet
- The Alkaline Diet: Is There Evidence That An Alkaline PH Diet Benefits Health?Document8 pagesThe Alkaline Diet: Is There Evidence That An Alkaline PH Diet Benefits Health?a3llamNo ratings yet
- Bexiga 2Document3 pagesBexiga 2ana claraNo ratings yet
- 10 1111@eve 13373Document10 pages10 1111@eve 13373ccamachoNo ratings yet
- Mineral: Lecturer: Puspa Julistia AssistantDocument7 pagesMineral: Lecturer: Puspa Julistia AssistantNatashaAnneNo ratings yet
- Jurnal UrologyDocument6 pagesJurnal UrologyFerryGoNo ratings yet
- Emma Wynn, Marc-Antoine Krieg, Jean-Marc Aeschlimann, Peter BurckhardtDocument5 pagesEmma Wynn, Marc-Antoine Krieg, Jean-Marc Aeschlimann, Peter BurckhardtMihai MishuNo ratings yet
- Journal BiochemistryDocument6 pagesJournal BiochemistrySofiNo ratings yet
- 1 s2.0 S2314808X16300033 MainDocument8 pages1 s2.0 S2314808X16300033 MainnisceNo ratings yet
- Urinary Stones: Medical and Surgical ManagementFrom EverandUrinary Stones: Medical and Surgical ManagementMichael GrassoNo ratings yet
- Assessment and Management of Heart Failure in Patients With Chronic Kidney DiseaseDocument16 pagesAssessment and Management of Heart Failure in Patients With Chronic Kidney DiseaseElian BenjaminNo ratings yet
- Renal Dose Adjustment: Robert W. Schrier. Manual of Nephrology, 6 Ed. LWW. 2005: p269-86Document7 pagesRenal Dose Adjustment: Robert W. Schrier. Manual of Nephrology, 6 Ed. LWW. 2005: p269-86octaNo ratings yet
- GOCABR ProtocolDocument5 pagesGOCABR Protocolnunuk wijayantiNo ratings yet
- Common OstrichDocument165 pagesCommon OstrichHarish BhatNo ratings yet
- Institute of Liver & Biliary Sciences: Bio - ChemistryDocument1 pageInstitute of Liver & Biliary Sciences: Bio - ChemistryNeeraj NegiNo ratings yet
- Physiology HhsDocument7 pagesPhysiology HhszeeshanNo ratings yet
- Research Paper On Chronic Renal FailureDocument4 pagesResearch Paper On Chronic Renal Failuretxdpmcbkf100% (1)
- MARCH MTLE 2023 Recalls: Clinical ChemistryDocument8 pagesMARCH MTLE 2023 Recalls: Clinical ChemistryJeanly DoctorNo ratings yet
- Nutrition Therapy For Renal Disorders Case QuestionsDocument9 pagesNutrition Therapy For Renal Disorders Case QuestionspeytonNo ratings yet
- 2017 KDIGO CKD MBD GL Update (20 25)Document6 pages2017 KDIGO CKD MBD GL Update (20 25)SMA N 1 TOROHNo ratings yet
- DR Ara Khan Marwat: Join My Watssap Group For Part-1 Books, Papers and UpdatesDocument25 pagesDR Ara Khan Marwat: Join My Watssap Group For Part-1 Books, Papers and UpdatesmisdduaaNo ratings yet
- Renal SystemDocument14 pagesRenal SystemFrances RebeccaNo ratings yet
- Clinical Biochemistry - Fifth YearDocument176 pagesClinical Biochemistry - Fifth YearBayan AlsaadiNo ratings yet
- Use of Diuretics in Patients With Heart Failure - UpToDateDocument11 pagesUse of Diuretics in Patients With Heart Failure - UpToDateAFA.BLSNo ratings yet
- Revisiting Diuretic Choice in Chronic Kidney.4Document8 pagesRevisiting Diuretic Choice in Chronic Kidney.4FABIO JAVIER BRAVO SALDARRIAGANo ratings yet
- A Machine Learning Analysis of Health Records of Patients With Chronic Kidney Disease at Risk of Cardiovascular DiseaseDocument14 pagesA Machine Learning Analysis of Health Records of Patients With Chronic Kidney Disease at Risk of Cardiovascular DiseaseMortimer SmithNo ratings yet
- Yoshio Terada Takashi Wada Kent Doi Acute Kidney Injury and Regenerative Medicine Springer Singapore Springer 2020Document390 pagesYoshio Terada Takashi Wada Kent Doi Acute Kidney Injury and Regenerative Medicine Springer Singapore Springer 2020XtineNo ratings yet
- Quick Reference DMARDsDocument12 pagesQuick Reference DMARDsEman MohamedNo ratings yet
- Full FileDocument105 pagesFull Filekrishan kumarNo ratings yet
- Strasinger AUBFDocument44 pagesStrasinger AUBFangela tanteoNo ratings yet
- Drug Use in Special Conditions - CLD and CKDDocument93 pagesDrug Use in Special Conditions - CLD and CKDadamu mohammadNo ratings yet
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916srirampharmNo ratings yet
- Report - SIDDHANT CHOUDHARY (231013056)Document17 pagesReport - SIDDHANT CHOUDHARY (231013056)Siddhant choudharyNo ratings yet
- Feline Acute Kidney Injury. 1. Pathophysiology, Etiology and Etiology-Specific Management ConsiderationsDocument11 pagesFeline Acute Kidney Injury. 1. Pathophysiology, Etiology and Etiology-Specific Management ConsiderationsMartín QuirogaNo ratings yet
- MTLE - ASCPI Final CoachingDocument57 pagesMTLE - ASCPI Final CoachingbambasanlyNo ratings yet
- Renal Failure and ItsDocument8 pagesRenal Failure and ItsSandra CalderonNo ratings yet
- Nejmoa 2206038Document12 pagesNejmoa 2206038Juan David Arboleda LopezNo ratings yet
- Yosefin Eka Pembimbing: Dr. Anik W., Sp. PK (K)Document33 pagesYosefin Eka Pembimbing: Dr. Anik W., Sp. PK (K)Yosefin EkaNo ratings yet