Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
3 viewsPharmacology: Gelianne Alba-Loquez, RN
Pharmacology: Gelianne Alba-Loquez, RN
Uploaded by
julinka beyla yanson1) Fluoroquinolones are a class of broad-spectrum antibacterial agents classified into generations based on their activity. First-generation drugs like norfloxacin are less active than second-generation ciprofloxacin and ofloxacin. Third-generation levofloxacin, gemifloxacin and moxifloxacin have even broader spectra.
2) They work by inhibiting bacterial DNA gyrase and topoisomerase IV, interfering with DNA replication. Resistance emerges rapidly in some pathogens.
3) Fluoroquinolones are used to treat infections in the GI, urinary and respiratory tracts, as well as pneumonia. They have gastrointestinal side effects and can prolong the
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Fluoroquinolone Antimicrobials in Animal HealthDocument17 pagesFluoroquinolone Antimicrobials in Animal HealthSunilNo ratings yet
- Select Projects, Infectious Disease MitigationDocument34 pagesSelect Projects, Infectious Disease MitigationTeoNo ratings yet
- NCLEX (Valerie) PDFDocument18 pagesNCLEX (Valerie) PDFValerie Orengo100% (1)
- Hot Stone Massage Manual-3Document56 pagesHot Stone Massage Manual-3Oana IftimieNo ratings yet
- Quinolone AntibioticsDocument21 pagesQuinolone Antibioticsergrt hdfhdhNo ratings yet
- Prepared By:-Ruchita V Bhavsar 1 Sem M.Pharm Guided By: - Mr. Samaresh Pal Roy HOD of Pharmacology, SDPC, KimDocument42 pagesPrepared By:-Ruchita V Bhavsar 1 Sem M.Pharm Guided By: - Mr. Samaresh Pal Roy HOD of Pharmacology, SDPC, KimHenry DanielNo ratings yet
- Pharmacokinetic/pharmacodynamic Modelling of Ciprofloxacin 250 mg/12 H Versus 500 mg/24 H For Urinary InfectionsDocument6 pagesPharmacokinetic/pharmacodynamic Modelling of Ciprofloxacin 250 mg/12 H Versus 500 mg/24 H For Urinary InfectionsLydia EvangelistNo ratings yet
- Group 9 - Bacteriology Reporting (Written Report)Document6 pagesGroup 9 - Bacteriology Reporting (Written Report)DENISE MARA�ANo ratings yet
- Flu Oro Quino L OnesDocument28 pagesFlu Oro Quino L Onesbushe_yhane23No ratings yet
- BY: Sonali Kanade Kaushik.N.Kuche Rucha.J.Kadmane Diksha KanojiyaDocument37 pagesBY: Sonali Kanade Kaushik.N.Kuche Rucha.J.Kadmane Diksha KanojiyaRaman KumarNo ratings yet
- PharmaDocument2 pagesPharmaPatrick MangilinNo ratings yet
- Project FinalDocument30 pagesProject FinalTinku BudhwarNo ratings yet
- Stahlmann-2002-Clinical Toxicological Aspects of FQ-Toxicology LettersDocument9 pagesStahlmann-2002-Clinical Toxicological Aspects of FQ-Toxicology LettersAndy KumarNo ratings yet
- Fluoroquinolones: QuinolonesDocument7 pagesFluoroquinolones: QuinolonesGhubaya CopNo ratings yet
- Group 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. JumuadDocument25 pagesGroup 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. Jumuadrakish16No ratings yet
- Drug Study-AntibacterialDocument6 pagesDrug Study-AntibacterialKyla Marie NabongNo ratings yet
- Antibiotics Simplified 1st Edition DR - Osama Ma3rofDocument57 pagesAntibiotics Simplified 1st Edition DR - Osama Ma3rofDark AngelNo ratings yet
- Fluoroquinolones PDFDocument1 pageFluoroquinolones PDFmariam ibrahimNo ratings yet
- MoxifloxacinDocument2 pagesMoxifloxacin1adie1907No ratings yet
- Antibacterial AgentsDocument24 pagesAntibacterial Agentsمصطفى أحمدNo ratings yet
- Handout Unit 7Document5 pagesHandout Unit 7Hillary FuentoantagioNo ratings yet
- Medicinal Chemistry: Lectures Note 8Document10 pagesMedicinal Chemistry: Lectures Note 8nosaybaNo ratings yet
- Anti-Inffective AgentsDocument2 pagesAnti-Inffective AgentsJamilah BanglanNo ratings yet
- Antibiotics PharmaDocument4 pagesAntibiotics PharmaJohn Dave V. VillarmenteNo ratings yet
- Vol3no3 8 PDFDocument5 pagesVol3no3 8 PDFMariayolanita PajangNo ratings yet
- Quinolones: Nucleic Acid Synthesis InhibitorsDocument21 pagesQuinolones: Nucleic Acid Synthesis InhibitorsShahid Iqbal100% (1)
- 24 05 2021 Floroquinolones DR - Syeda ZainDocument46 pages24 05 2021 Floroquinolones DR - Syeda ZaintehreemNo ratings yet
- Antimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette OpleidingDocument12 pagesAntimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette OpleidingYaserAbbasiNo ratings yet
- Therapeutic Advances of New PDFDocument23 pagesTherapeutic Advances of New PDFKevin ArechigaNo ratings yet
- Antibioticos - CasasDocument14 pagesAntibioticos - Casashellenj.sancheznNo ratings yet
- Comparacion de Diferentes Tratamientos Antibióticos Focalizados Al Ciclio CelularDocument6 pagesComparacion de Diferentes Tratamientos Antibióticos Focalizados Al Ciclio CelularCamila LaraNo ratings yet
- The Quinolone Family From Antibacterial To Anticancer Agents - Sissi - 2003 PDFDocument12 pagesThe Quinolone Family From Antibacterial To Anticancer Agents - Sissi - 2003 PDFAndy KumarNo ratings yet
- New Classification and Update On The Quinolone AntibioticsDocument15 pagesNew Classification and Update On The Quinolone Antibioticssuvasish0068372No ratings yet
- Galang-D SDocument3 pagesGalang-D Sgalang.andrea.mNo ratings yet
- PRESENTED TO: Sir Zafar Iqbal Presented By: Group-EDocument31 pagesPRESENTED TO: Sir Zafar Iqbal Presented By: Group-EAdia MasooraNo ratings yet
- FluoroquinolonesDocument7 pagesFluoroquinolonesQambar abbasNo ratings yet
- Quino L OnesDocument1 pageQuino L OnesArnel Leonard TungbabanNo ratings yet
- Tetracyclines: Mechanism of ActionDocument16 pagesTetracyclines: Mechanism of Actionammar amerNo ratings yet
- Bayer 3rd Proc'99 - PAPICHDocument5 pagesBayer 3rd Proc'99 - PAPICHsergioNo ratings yet
- Oms MedsDocument21 pagesOms MedsJanine OpetingcoNo ratings yet
- Antibiotics in EndodonticsDocument74 pagesAntibiotics in EndodonticsdrishyaNo ratings yet
- Lactams Chemical Structure, Mode of Action And.2Document11 pagesLactams Chemical Structure, Mode of Action And.2asmanadjiNo ratings yet
- Antimikroba Untuk Infeksi Gastrointestinal: Oleh: Evi Sovia Lab. Farmakologi FK UNJANIDocument86 pagesAntimikroba Untuk Infeksi Gastrointestinal: Oleh: Evi Sovia Lab. Farmakologi FK UNJANIKresna Denta ElygioNo ratings yet
- Update Classification of Quinolone AntibioticDocument15 pagesUpdate Classification of Quinolone Antibioticsuvasish0068372No ratings yet
- Antimicrobial Drugs Lec 3 Cephalosporins Learning ObjectivesDocument2 pagesAntimicrobial Drugs Lec 3 Cephalosporins Learning ObjectivesNashat SaadiNo ratings yet
- Clase 1 Antibioticos AminoglucosidosDocument6 pagesClase 1 Antibioticos AminoglucosidosAndrés GarcíaNo ratings yet
- MICP LAB (WEEK - 5) Antimicrobial Agents in TherapydocDocument8 pagesMICP LAB (WEEK - 5) Antimicrobial Agents in Therapydoccaitie miracleNo ratings yet
- CH631-unit-3 Med Chem PDFDocument77 pagesCH631-unit-3 Med Chem PDFN Khadija BathoolNo ratings yet
- Flu Oro Quino LonasDocument8 pagesFlu Oro Quino LonasJESUS JAHIR MARTINEZ RAMIRONo ratings yet
- Perspectives: Where Will New Antibiotics Come From?Document6 pagesPerspectives: Where Will New Antibiotics Come From?nabilahNo ratings yet
- Banaag Antibacterial MedsDocument5 pagesBanaag Antibacterial MedsPrince JoaquinNo ratings yet
- Drug StudyDocument2 pagesDrug Studydev_ang23No ratings yet
- Drug Study Rle Final 1Document18 pagesDrug Study Rle Final 1YBH Construction SupplyNo ratings yet
- Anaerobic BacteriaDocument4 pagesAnaerobic BacteriaJesette KhoNo ratings yet
- Isolates With Concurrent Resistance To Ceftriaxone and Ciprofloxacin6Document6 pagesIsolates With Concurrent Resistance To Ceftriaxone and Ciprofloxacin6Talent.A. MangeyaNo ratings yet
- Antibacterial Drugs Cellwall and Protein Synthesis InhihibitorsDocument41 pagesAntibacterial Drugs Cellwall and Protein Synthesis InhihibitorsWezzyNo ratings yet
- Drug Study CepDocument10 pagesDrug Study CepPMG BrightNo ratings yet
- Drugsstudy Different ObDocument8 pagesDrugsstudy Different ObElvis DuotNo ratings yet
- ANTIBIOTICSDocument7 pagesANTIBIOTICSLutfi HakimNo ratings yet
- Anti-Leprosy Drugs: General InformationDocument12 pagesAnti-Leprosy Drugs: General InformationElla IlustreNo ratings yet
- Until Slide 799Document12 pagesUntil Slide 799Ella IlustreNo ratings yet
- Case2and3Q1Document6 pagesCase2and3Q1CO OK-Yim BoholNo ratings yet
- Comprehensive Exam Coverage First Sem SY 2022 2023Document5 pagesComprehensive Exam Coverage First Sem SY 2022 2023julinka beyla yansonNo ratings yet
- Jaha 121 025205Document32 pagesJaha 121 025205julinka beyla yansonNo ratings yet
- OIDP NCM3261 MS-2ndDocument2 pagesOIDP NCM3261 MS-2ndjulinka beyla yansonNo ratings yet
- Pharmacology: Ms. Gelianne Alba-LoquezDocument5 pagesPharmacology: Ms. Gelianne Alba-Loquezjulinka beyla yansonNo ratings yet
- 03 Sympathomimetics-And-Blockers NCM206Document9 pages03 Sympathomimetics-And-Blockers NCM206julinka beyla yansonNo ratings yet
- Sympathetic Receptors and Their Responses: Nervous SystemDocument3 pagesSympathetic Receptors and Their Responses: Nervous Systemjulinka beyla yansonNo ratings yet
- Pharmacology: Ms. Gelianne Alba-Loquez, RNDocument6 pagesPharmacology: Ms. Gelianne Alba-Loquez, RNjulinka beyla yansonNo ratings yet
- LABREPORT1Document6 pagesLABREPORT1julinka beyla yansonNo ratings yet
- 06 - Tetracyclines and Other AntimicrobialsDocument6 pages06 - Tetracyclines and Other Antimicrobialsjulinka beyla yansonNo ratings yet
- 07 - Cardiac Glycosides Anti AnginaDocument5 pages07 - Cardiac Glycosides Anti Anginajulinka beyla yansonNo ratings yet
- Akong Tuo Na Kamot! Napaakan Man Gud Ko Ug Putsukan" AsDocument2 pagesAkong Tuo Na Kamot! Napaakan Man Gud Ko Ug Putsukan" Asjulinka beyla yansonNo ratings yet
- Pathophysiology of Acute Kidney InjuryDocument4 pagesPathophysiology of Acute Kidney InjuryJane Arian Berzabal0% (1)
- Tamwed - Mooligai Thottam Project Evaluation JANUARY 2012Document11 pagesTamwed - Mooligai Thottam Project Evaluation JANUARY 2012Manigandan BalajiNo ratings yet
- Physical Development in InfancyDocument31 pagesPhysical Development in InfancyJohn Ray SadgitapNo ratings yet
- Ack Your Bags and Move To The CountrysideDocument6 pagesAck Your Bags and Move To The CountrysidesarahNo ratings yet
- Acetylcysteine (EXFLEM)Document2 pagesAcetylcysteine (EXFLEM)Kristine YoungNo ratings yet
- Le Syndrome de Bardet Biedl Endocrino 2008Document9 pagesLe Syndrome de Bardet Biedl Endocrino 2008Talala tililiNo ratings yet
- Acute Phosphate NephropathyDocument12 pagesAcute Phosphate NephropathyOlga BabiiNo ratings yet
- Mtlaws LectureDocument6 pagesMtlaws LectureAhnorrei PavlaskaNo ratings yet
- AACE/ACE Disease State Clinical ReviewDocument11 pagesAACE/ACE Disease State Clinical ReviewDevi DaryaningsihNo ratings yet
- Social and Public HealthDocument54 pagesSocial and Public HealthMekuriya BeregaNo ratings yet
- What Is GKI, Glucose Ketone Index Calculate It KETO-MOJODocument1 pageWhat Is GKI, Glucose Ketone Index Calculate It KETO-MOJOsbtxbprm29No ratings yet
- Therapeutic Ultrasound in Soft Tissue Lesions: ReviewDocument6 pagesTherapeutic Ultrasound in Soft Tissue Lesions: ReviewNgoma FaithNo ratings yet
- Efficacy and Clinical Assessment of Varmam Theraphy in The Management of HeadacheDocument5 pagesEfficacy and Clinical Assessment of Varmam Theraphy in The Management of HeadacheMurali SmatNo ratings yet
- Fish DiseasesDocument38 pagesFish DiseasesSamia BasharatNo ratings yet
- 8 Important Facts About The COVID-19 Vaccine BoosterDocument1 page8 Important Facts About The COVID-19 Vaccine BoosterMT DevoteeNo ratings yet
- HOOKWORMSDocument47 pagesHOOKWORMSChipego ChiyaamaNo ratings yet
- Picornaviridae - CDocument9 pagesPicornaviridae - Cميمونه عبد الرحيم مصطفىNo ratings yet
- Day 1 - Alcohol and AnxietyDocument3 pagesDay 1 - Alcohol and AnxietyVictoria Castillo TamayoNo ratings yet
- Annual Work PlanDocument42 pagesAnnual Work Planpeter wanjohi100% (1)
- Precociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Document31 pagesPrecociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Priya RaviNo ratings yet
- Case Pre. (Ovarian Cyst)Document55 pagesCase Pre. (Ovarian Cyst)rebeljerome100% (3)
- POSTER Final PDFDocument1 pagePOSTER Final PDFpavani pNo ratings yet
- Book Notes: Runner's HandbookDocument3 pagesBook Notes: Runner's Handbookscribd532No ratings yet
- NCP (BPH)Document8 pagesNCP (BPH)NataCo50% (2)
- DAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourDocument3 pagesDAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourSHIVAM KUMAR SINGHNo ratings yet
- 05 Palmieri-VadalaDocument7 pages05 Palmieri-VadalaSantosNo ratings yet
- Lesson 1 Intro To BiochemDocument15 pagesLesson 1 Intro To BiochemJulius Memeg PanayoNo ratings yet
Pharmacology: Gelianne Alba-Loquez, RN
Pharmacology: Gelianne Alba-Loquez, RN
Uploaded by
julinka beyla yanson0 ratings0% found this document useful (0 votes)
3 views3 pages1) Fluoroquinolones are a class of broad-spectrum antibacterial agents classified into generations based on their activity. First-generation drugs like norfloxacin are less active than second-generation ciprofloxacin and ofloxacin. Third-generation levofloxacin, gemifloxacin and moxifloxacin have even broader spectra.
2) They work by inhibiting bacterial DNA gyrase and topoisomerase IV, interfering with DNA replication. Resistance emerges rapidly in some pathogens.
3) Fluoroquinolones are used to treat infections in the GI, urinary and respiratory tracts, as well as pneumonia. They have gastrointestinal side effects and can prolong the
Original Description:
Original Title
01_ANTI-BACTERIALS-II_PCOL
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1) Fluoroquinolones are a class of broad-spectrum antibacterial agents classified into generations based on their activity. First-generation drugs like norfloxacin are less active than second-generation ciprofloxacin and ofloxacin. Third-generation levofloxacin, gemifloxacin and moxifloxacin have even broader spectra.
2) They work by inhibiting bacterial DNA gyrase and topoisomerase IV, interfering with DNA replication. Resistance emerges rapidly in some pathogens.
3) Fluoroquinolones are used to treat infections in the GI, urinary and respiratory tracts, as well as pneumonia. They have gastrointestinal side effects and can prolong the
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
3 views3 pagesPharmacology: Gelianne Alba-Loquez, RN
Pharmacology: Gelianne Alba-Loquez, RN
Uploaded by
julinka beyla yanson1) Fluoroquinolones are a class of broad-spectrum antibacterial agents classified into generations based on their activity. First-generation drugs like norfloxacin are less active than second-generation ciprofloxacin and ofloxacin. Third-generation levofloxacin, gemifloxacin and moxifloxacin have even broader spectra.
2) They work by inhibiting bacterial DNA gyrase and topoisomerase IV, interfering with DNA replication. Resistance emerges rapidly in some pathogens.
3) Fluoroquinolones are used to treat infections in the GI, urinary and respiratory tracts, as well as pneumonia. They have gastrointestinal side effects and can prolong the
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 3
10 L E C
Pharmacology
01
08
GELIANNE ALBA-LOQUEZ, RN 21
ANTI - BACTERIALS II
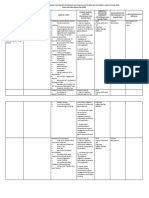
OUTLINE 1st gen: Norfloxacin
I. FLUOROQUINOLONES derived from nalidixic acid
a. Classification has an activity against common
pathogens that cause urinary tract
1st Generation
infections
2nd Generation 2nd gen: Ciprofloxacin and Ofloxacin
3rd Generation greater activity against gram-negative
b. Pharmacokinetics bacteria
c. Mechanism of action Also active against: gonococcus, many
d. Resistance gram-positive cocci, myvobacteria,
atypical pneumonia
e. Clinical uses
3rd gen: Levofloxacin, Gemifloxacin, and
f. Toxicity
Moxifloxacin
II. ANTI - METABOLITE slightly less active against gram-
a. Sulfonamides negative bacteria (versus 2nd gen)
Classification greater activity against grem-positive
Resistance cocci (S. pneumoniae, some strains of
Clinical Uses enterococci, and MRSA)
also known as respiratory
b. Trimethoprim
fluoroquinolones
Classification and Pharmacokinetics note: you will no that they are part of
Resistance fluoroquinolons because of the word flo present
Clinical Uses om each names.
c. Toxicity of Sulfonamides and
Trimethoprim PHARMACOKINETICS
all generations have good oral bioavailability
antacids may interfere
Note: before you administer fluoroquinolones
make sure that they are not also taking antacids
because those anticids would culture the
effectivity of the fluorquinolones
penetrate most body tissues
Elimination is through urinary excretion
can be blocked by probenecid
Note: if you don't want to prolong the antibiotic
inside the patients body then make sure the pt. is
not taking probenecid cause that will block the
urinary excretion of your fluoroquinolones
dosage production necessary in renal
failure because they are excreted
through the urine except moxifloxacin
which is excreted via biliary excretion.
FLUOROQUINOLONES its use in urinary tract infection is
CLASSIFICATION not recommended
According to "generations"- based on their
antimicrobial spectrum of activity
per generation it has different spectrum of
activity
BSN 2B TRANSCRIBED BY GROUP 3 1
MECHANISM OF ACTION Ofloxacin is possibly used for chlamydia
Interfere with bacterial DNA synthesis by trachomatis (but requires 7-day course of
inhibiting these enzymes: treatment)
Topoisomerase II (DNA gyrase) in gram Levofloxacin is for community acquired
negative bacteria pneumonia
Topoisomerase IV in gram positive Gemofloxacin and Moxifloxacin
bacteria have widest spectrum of activity against:
Similar to aminoglycosides, they also exhibit gram positive and gram negative
post-antibiotic effect microbes
bactericidal effect continues after drug Atypical pneumonia agents
levels fall below minimum inhibitory some anaerobic bacteria
concentration Fluoroquinolones may also be used in cases
note: meaning kahit daw bumaba na sa minimum of:
inhibitory concentration ang gamot inside the meningicoccal carrier state (carriers
body of the patient then it will still exhibit might not exhibit symptoms for
antibiotic effect meningicoccal)
Pulmonary tuberculosis
RESISTANCE Neutropenic patients (prophylaxis)
rapid emergence in the case of 2nd
generation fluoroquinolones, especially in: TOXICITY
campylobacter jejuni Gastrointestinal distress mosy common
Gonococci adverse effect
MRSA Others: rash, headache, abnormal liver
Pseudomonas spp function tests, ptototoxicty, tendinitis, and
note: ito iyong mga bacteria that are mostly tendon rupture
resistant to your 2nd generation fluoroquinolones not recommended for children and the
Bacteria are able to resist due to their ability pregnant due to possible damage to
to: growing cartilage ( anthropathy)
decrease intracellular accumulation of not recommended to pregnant women
the drug (by developing efflux pumps) kasi nagkakaproblema sa growth ng
note: example a bacteria developing pumps to bata or baby sa loob ng tiyan.
push the drug outside or away resulting na konti Opportunistic infections by Candida albicans
nalang ang drug na nasa loob ng bacteria. The and streptococci
concentration of the drug is so small or low that Can prolong QT interval: 3rd generation
does not make any effect in the bacteria that is fluoroquinolones
why nagkakaroon ng resistance ang bacteria not for patients on medications for
point mutations in binding regions of antiarrythmic medications
the antibiotics
note: example if your drug is suppose to bind at a
ANTI - METABOLITE
certain receptor of a bacteria. Your bacteria
causes mutation or a change in those binding Drug that is able to interfere wIth the role of an
sites therefore rendering the binding of the drug endogenous compound in cellular metabolism
ineffective. Hindi na nakakabind iyong gamot sa note: they interfere with the role of a specific enzyme
kung saan siya dapat magbind kasi nagmutate or or compound that is important for the bacteria to
nagchange na iyong binding site. metabolize or to be able to undergo cellular
metabolism
CLINICAL USES Examples are sulfonamides, Trimethoprim, TMP-
Effective for treatment of infections in the: SMX
gastrointestinal tract
urogenital tract SULFONAMIDES
Respiratory weakly acidic compounds that have a common
integumentary (and soft tissue) chemical nucleus resemblung p-aminobezoic
Ciprofloxacin and Ofloxacin Clinical Uses acud (PABA)
single oral doses for gonorrhea (as note: PABA is important in folic acid synthesis. Folic
alternatives to cetriaxone and cefixime) acid is very important in DNA and nucleic acid
still not recommneded to increased development or synthesis of the bacteria. PABA is
patterns of antimicrobial resistance important to the bacteria to be able to synthesize folic
BSN 2B TRANSCRIBED BY GROUP 3 2
acid. Sulfonamides look like PABA, paginiinom ng tao reaches high concentrations in prostatic and
the drug will in way will trick the bacteria na PABA vaginal fluids
iyan iyon pala sulfonamide siya so there is an large percentage is excreted unchanged in
alteration of the folic acid synthesis which makes the the urine
folic acid synthesis ineffective for the bacteria selective inhibitor of bacterial diydrofolate
Members differ mainly in their pharmacokinetic reductase (prevents formation of active form
properties and uses of folic acid)
modest tissue penetration, hepatic metabolism, bacterial dihydrofolate reductase is 4-5
and renal excretion times more sensitive than the
mammalian version of the enzyme
CLASSIFICATION: note: your trimetophrim can easily inhibit
short acting (sulfisoxazole) bacterial dihydrofolate reductase because it
Intermediate acting (sulfamethoxazole) is 4-5 times more sensitive than the
Long acting (sulfadoxine) mammalian version
MECHANISM OF ACTION: RESISTANCE
bacteriostatic inhibitors of folic acid production of dihydrofolate reductase (but
synthesis with reduced affinity for the drug)
competitive inhibitors of dihydropteroate note that this is the exact same enzyme
synthase (also acts as subtrates which which is targeted by trimethoprim
produces non functioning forms of folic acid) Note: bacteria is able to produce dihydrofolate
note: dihydropteroate synthase triggers your enzyme but not that much affected by the
PABA or lets PABA work so that there will be folic trimethoprim drug
acid synthesis then sulfonamides targets
dihydropteroate synthase so that there is an CLINICAL USES:
interference in the synthesis of folic acid. So ang as TMP-SMX (trimetophrim/
nangyayari when sulfonamides come in there will sulfamethoxazole, also known as
be production of non functioning form of folic Cotrimoxazole)
acid making the folic acid synthesize by the UTI, respiratory, ear, and sinud infections (H.
bacteria ineffective influenza and M. catarrhalis)
DOC (Drug of Choice) for Pneumocystis
RESISTANCE: pneumonia (immunocompromised patients)
plasmid-mediated (overproduction of PABA, Backup drug for cholera, typhoid fever, and
folic acid synthesizing enzyme woth low shigellosis
affinity for sulfonamides, impair
permeability to sulfonamide) TOXICITY OF SULFONAMIDES AND
note: di na nagiging effective si sulfonamide kasi TRIMETHOPRIM
na over power na ng PABA
decreased intracellular accumulation of the Sulfonamides
drug Hyoersensitivity (allergic reactions, fever,
note: low concentration of drug in the bacteria exfoliative dermatitis, and Steven-Johnsons
for it to take its effect. syndrome)
GI irritation (nausea, vomiting, and diarrhea)
CLINICAL USES: Hematoxicity (granulocytopenia,
Simple UTI (oral; sulfisoxazole) thrombocytopenia, and apalstic anemia)
Ocular infections (topical; sulfacetamide) Nephtotoxicity (crystalluria, and hematura)
Burns (topical; silver sukfadiazine, mafenide)
Ulcerative colitis (oral; sulfasalazine) Trimethoprim
Toxoplasmosis (oral; sulfadiazine) Hematoxicity (megaloblastic anemia,
leukopenia, and granulocytopenia)
TRIMETHOPRIM
REFERENCES
CLASSIFICATION AND PHARMACOKINETICS:
“PROF’S PPT ON QUIPPER AND LECTURE”
structurally similar to folic acid
weak acid
BSN 2B TRANSCRIBED BY GROUP 3 3
You might also like
- Fluoroquinolone Antimicrobials in Animal HealthDocument17 pagesFluoroquinolone Antimicrobials in Animal HealthSunilNo ratings yet
- Select Projects, Infectious Disease MitigationDocument34 pagesSelect Projects, Infectious Disease MitigationTeoNo ratings yet
- NCLEX (Valerie) PDFDocument18 pagesNCLEX (Valerie) PDFValerie Orengo100% (1)
- Hot Stone Massage Manual-3Document56 pagesHot Stone Massage Manual-3Oana IftimieNo ratings yet
- Quinolone AntibioticsDocument21 pagesQuinolone Antibioticsergrt hdfhdhNo ratings yet
- Prepared By:-Ruchita V Bhavsar 1 Sem M.Pharm Guided By: - Mr. Samaresh Pal Roy HOD of Pharmacology, SDPC, KimDocument42 pagesPrepared By:-Ruchita V Bhavsar 1 Sem M.Pharm Guided By: - Mr. Samaresh Pal Roy HOD of Pharmacology, SDPC, KimHenry DanielNo ratings yet
- Pharmacokinetic/pharmacodynamic Modelling of Ciprofloxacin 250 mg/12 H Versus 500 mg/24 H For Urinary InfectionsDocument6 pagesPharmacokinetic/pharmacodynamic Modelling of Ciprofloxacin 250 mg/12 H Versus 500 mg/24 H For Urinary InfectionsLydia EvangelistNo ratings yet
- Group 9 - Bacteriology Reporting (Written Report)Document6 pagesGroup 9 - Bacteriology Reporting (Written Report)DENISE MARA�ANo ratings yet
- Flu Oro Quino L OnesDocument28 pagesFlu Oro Quino L Onesbushe_yhane23No ratings yet
- BY: Sonali Kanade Kaushik.N.Kuche Rucha.J.Kadmane Diksha KanojiyaDocument37 pagesBY: Sonali Kanade Kaushik.N.Kuche Rucha.J.Kadmane Diksha KanojiyaRaman KumarNo ratings yet
- PharmaDocument2 pagesPharmaPatrick MangilinNo ratings yet
- Project FinalDocument30 pagesProject FinalTinku BudhwarNo ratings yet
- Stahlmann-2002-Clinical Toxicological Aspects of FQ-Toxicology LettersDocument9 pagesStahlmann-2002-Clinical Toxicological Aspects of FQ-Toxicology LettersAndy KumarNo ratings yet
- Fluoroquinolones: QuinolonesDocument7 pagesFluoroquinolones: QuinolonesGhubaya CopNo ratings yet
- Group 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. JumuadDocument25 pagesGroup 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. Jumuadrakish16No ratings yet
- Drug Study-AntibacterialDocument6 pagesDrug Study-AntibacterialKyla Marie NabongNo ratings yet
- Antibiotics Simplified 1st Edition DR - Osama Ma3rofDocument57 pagesAntibiotics Simplified 1st Edition DR - Osama Ma3rofDark AngelNo ratings yet
- Fluoroquinolones PDFDocument1 pageFluoroquinolones PDFmariam ibrahimNo ratings yet
- MoxifloxacinDocument2 pagesMoxifloxacin1adie1907No ratings yet
- Antibacterial AgentsDocument24 pagesAntibacterial Agentsمصطفى أحمدNo ratings yet
- Handout Unit 7Document5 pagesHandout Unit 7Hillary FuentoantagioNo ratings yet
- Medicinal Chemistry: Lectures Note 8Document10 pagesMedicinal Chemistry: Lectures Note 8nosaybaNo ratings yet
- Anti-Inffective AgentsDocument2 pagesAnti-Inffective AgentsJamilah BanglanNo ratings yet
- Antibiotics PharmaDocument4 pagesAntibiotics PharmaJohn Dave V. VillarmenteNo ratings yet
- Vol3no3 8 PDFDocument5 pagesVol3no3 8 PDFMariayolanita PajangNo ratings yet
- Quinolones: Nucleic Acid Synthesis InhibitorsDocument21 pagesQuinolones: Nucleic Acid Synthesis InhibitorsShahid Iqbal100% (1)
- 24 05 2021 Floroquinolones DR - Syeda ZainDocument46 pages24 05 2021 Floroquinolones DR - Syeda ZaintehreemNo ratings yet
- Antimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette OpleidingDocument12 pagesAntimicrobial Selection, Administration and Dosage: Continuing Education - Voortgesette OpleidingYaserAbbasiNo ratings yet
- Therapeutic Advances of New PDFDocument23 pagesTherapeutic Advances of New PDFKevin ArechigaNo ratings yet
- Antibioticos - CasasDocument14 pagesAntibioticos - Casashellenj.sancheznNo ratings yet
- Comparacion de Diferentes Tratamientos Antibióticos Focalizados Al Ciclio CelularDocument6 pagesComparacion de Diferentes Tratamientos Antibióticos Focalizados Al Ciclio CelularCamila LaraNo ratings yet
- The Quinolone Family From Antibacterial To Anticancer Agents - Sissi - 2003 PDFDocument12 pagesThe Quinolone Family From Antibacterial To Anticancer Agents - Sissi - 2003 PDFAndy KumarNo ratings yet
- New Classification and Update On The Quinolone AntibioticsDocument15 pagesNew Classification and Update On The Quinolone Antibioticssuvasish0068372No ratings yet
- Galang-D SDocument3 pagesGalang-D Sgalang.andrea.mNo ratings yet
- PRESENTED TO: Sir Zafar Iqbal Presented By: Group-EDocument31 pagesPRESENTED TO: Sir Zafar Iqbal Presented By: Group-EAdia MasooraNo ratings yet
- FluoroquinolonesDocument7 pagesFluoroquinolonesQambar abbasNo ratings yet
- Quino L OnesDocument1 pageQuino L OnesArnel Leonard TungbabanNo ratings yet
- Tetracyclines: Mechanism of ActionDocument16 pagesTetracyclines: Mechanism of Actionammar amerNo ratings yet
- Bayer 3rd Proc'99 - PAPICHDocument5 pagesBayer 3rd Proc'99 - PAPICHsergioNo ratings yet
- Oms MedsDocument21 pagesOms MedsJanine OpetingcoNo ratings yet
- Antibiotics in EndodonticsDocument74 pagesAntibiotics in EndodonticsdrishyaNo ratings yet
- Lactams Chemical Structure, Mode of Action And.2Document11 pagesLactams Chemical Structure, Mode of Action And.2asmanadjiNo ratings yet
- Antimikroba Untuk Infeksi Gastrointestinal: Oleh: Evi Sovia Lab. Farmakologi FK UNJANIDocument86 pagesAntimikroba Untuk Infeksi Gastrointestinal: Oleh: Evi Sovia Lab. Farmakologi FK UNJANIKresna Denta ElygioNo ratings yet
- Update Classification of Quinolone AntibioticDocument15 pagesUpdate Classification of Quinolone Antibioticsuvasish0068372No ratings yet
- Antimicrobial Drugs Lec 3 Cephalosporins Learning ObjectivesDocument2 pagesAntimicrobial Drugs Lec 3 Cephalosporins Learning ObjectivesNashat SaadiNo ratings yet
- Clase 1 Antibioticos AminoglucosidosDocument6 pagesClase 1 Antibioticos AminoglucosidosAndrés GarcíaNo ratings yet
- MICP LAB (WEEK - 5) Antimicrobial Agents in TherapydocDocument8 pagesMICP LAB (WEEK - 5) Antimicrobial Agents in Therapydoccaitie miracleNo ratings yet
- CH631-unit-3 Med Chem PDFDocument77 pagesCH631-unit-3 Med Chem PDFN Khadija BathoolNo ratings yet
- Flu Oro Quino LonasDocument8 pagesFlu Oro Quino LonasJESUS JAHIR MARTINEZ RAMIRONo ratings yet
- Perspectives: Where Will New Antibiotics Come From?Document6 pagesPerspectives: Where Will New Antibiotics Come From?nabilahNo ratings yet
- Banaag Antibacterial MedsDocument5 pagesBanaag Antibacterial MedsPrince JoaquinNo ratings yet
- Drug StudyDocument2 pagesDrug Studydev_ang23No ratings yet
- Drug Study Rle Final 1Document18 pagesDrug Study Rle Final 1YBH Construction SupplyNo ratings yet
- Anaerobic BacteriaDocument4 pagesAnaerobic BacteriaJesette KhoNo ratings yet
- Isolates With Concurrent Resistance To Ceftriaxone and Ciprofloxacin6Document6 pagesIsolates With Concurrent Resistance To Ceftriaxone and Ciprofloxacin6Talent.A. MangeyaNo ratings yet
- Antibacterial Drugs Cellwall and Protein Synthesis InhihibitorsDocument41 pagesAntibacterial Drugs Cellwall and Protein Synthesis InhihibitorsWezzyNo ratings yet
- Drug Study CepDocument10 pagesDrug Study CepPMG BrightNo ratings yet
- Drugsstudy Different ObDocument8 pagesDrugsstudy Different ObElvis DuotNo ratings yet
- ANTIBIOTICSDocument7 pagesANTIBIOTICSLutfi HakimNo ratings yet
- Anti-Leprosy Drugs: General InformationDocument12 pagesAnti-Leprosy Drugs: General InformationElla IlustreNo ratings yet
- Until Slide 799Document12 pagesUntil Slide 799Ella IlustreNo ratings yet
- Case2and3Q1Document6 pagesCase2and3Q1CO OK-Yim BoholNo ratings yet
- Comprehensive Exam Coverage First Sem SY 2022 2023Document5 pagesComprehensive Exam Coverage First Sem SY 2022 2023julinka beyla yansonNo ratings yet
- Jaha 121 025205Document32 pagesJaha 121 025205julinka beyla yansonNo ratings yet
- OIDP NCM3261 MS-2ndDocument2 pagesOIDP NCM3261 MS-2ndjulinka beyla yansonNo ratings yet
- Pharmacology: Ms. Gelianne Alba-LoquezDocument5 pagesPharmacology: Ms. Gelianne Alba-Loquezjulinka beyla yansonNo ratings yet
- 03 Sympathomimetics-And-Blockers NCM206Document9 pages03 Sympathomimetics-And-Blockers NCM206julinka beyla yansonNo ratings yet
- Sympathetic Receptors and Their Responses: Nervous SystemDocument3 pagesSympathetic Receptors and Their Responses: Nervous Systemjulinka beyla yansonNo ratings yet
- Pharmacology: Ms. Gelianne Alba-Loquez, RNDocument6 pagesPharmacology: Ms. Gelianne Alba-Loquez, RNjulinka beyla yansonNo ratings yet
- LABREPORT1Document6 pagesLABREPORT1julinka beyla yansonNo ratings yet
- 06 - Tetracyclines and Other AntimicrobialsDocument6 pages06 - Tetracyclines and Other Antimicrobialsjulinka beyla yansonNo ratings yet
- 07 - Cardiac Glycosides Anti AnginaDocument5 pages07 - Cardiac Glycosides Anti Anginajulinka beyla yansonNo ratings yet
- Akong Tuo Na Kamot! Napaakan Man Gud Ko Ug Putsukan" AsDocument2 pagesAkong Tuo Na Kamot! Napaakan Man Gud Ko Ug Putsukan" Asjulinka beyla yansonNo ratings yet
- Pathophysiology of Acute Kidney InjuryDocument4 pagesPathophysiology of Acute Kidney InjuryJane Arian Berzabal0% (1)
- Tamwed - Mooligai Thottam Project Evaluation JANUARY 2012Document11 pagesTamwed - Mooligai Thottam Project Evaluation JANUARY 2012Manigandan BalajiNo ratings yet
- Physical Development in InfancyDocument31 pagesPhysical Development in InfancyJohn Ray SadgitapNo ratings yet
- Ack Your Bags and Move To The CountrysideDocument6 pagesAck Your Bags and Move To The CountrysidesarahNo ratings yet
- Acetylcysteine (EXFLEM)Document2 pagesAcetylcysteine (EXFLEM)Kristine YoungNo ratings yet
- Le Syndrome de Bardet Biedl Endocrino 2008Document9 pagesLe Syndrome de Bardet Biedl Endocrino 2008Talala tililiNo ratings yet
- Acute Phosphate NephropathyDocument12 pagesAcute Phosphate NephropathyOlga BabiiNo ratings yet
- Mtlaws LectureDocument6 pagesMtlaws LectureAhnorrei PavlaskaNo ratings yet
- AACE/ACE Disease State Clinical ReviewDocument11 pagesAACE/ACE Disease State Clinical ReviewDevi DaryaningsihNo ratings yet
- Social and Public HealthDocument54 pagesSocial and Public HealthMekuriya BeregaNo ratings yet
- What Is GKI, Glucose Ketone Index Calculate It KETO-MOJODocument1 pageWhat Is GKI, Glucose Ketone Index Calculate It KETO-MOJOsbtxbprm29No ratings yet
- Therapeutic Ultrasound in Soft Tissue Lesions: ReviewDocument6 pagesTherapeutic Ultrasound in Soft Tissue Lesions: ReviewNgoma FaithNo ratings yet
- Efficacy and Clinical Assessment of Varmam Theraphy in The Management of HeadacheDocument5 pagesEfficacy and Clinical Assessment of Varmam Theraphy in The Management of HeadacheMurali SmatNo ratings yet
- Fish DiseasesDocument38 pagesFish DiseasesSamia BasharatNo ratings yet
- 8 Important Facts About The COVID-19 Vaccine BoosterDocument1 page8 Important Facts About The COVID-19 Vaccine BoosterMT DevoteeNo ratings yet
- HOOKWORMSDocument47 pagesHOOKWORMSChipego ChiyaamaNo ratings yet
- Picornaviridae - CDocument9 pagesPicornaviridae - Cميمونه عبد الرحيم مصطفىNo ratings yet
- Day 1 - Alcohol and AnxietyDocument3 pagesDay 1 - Alcohol and AnxietyVictoria Castillo TamayoNo ratings yet
- Annual Work PlanDocument42 pagesAnnual Work Planpeter wanjohi100% (1)
- Precociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Document31 pagesPrecociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Priya RaviNo ratings yet
- Case Pre. (Ovarian Cyst)Document55 pagesCase Pre. (Ovarian Cyst)rebeljerome100% (3)
- POSTER Final PDFDocument1 pagePOSTER Final PDFpavani pNo ratings yet
- Book Notes: Runner's HandbookDocument3 pagesBook Notes: Runner's Handbookscribd532No ratings yet
- NCP (BPH)Document8 pagesNCP (BPH)NataCo50% (2)
- DAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourDocument3 pagesDAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourSHIVAM KUMAR SINGHNo ratings yet
- 05 Palmieri-VadalaDocument7 pages05 Palmieri-VadalaSantosNo ratings yet
- Lesson 1 Intro To BiochemDocument15 pagesLesson 1 Intro To BiochemJulius Memeg PanayoNo ratings yet