Professional Documents
Culture Documents
44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)
44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)
Uploaded by
Jay GutierrezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)
44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)
Uploaded by
Jay GutierrezCopyright:
Available Formats
TYRON MASANGKAY
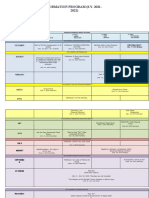
Author/s & Year Research Title Topic/ Problems Sample Data Major Findings Recommendati
Investigated (Participants in Collection on
(include the URL/link) the Study) Method
1. 44Albott, C. S., Battle buddies: rapid
Wozniak, J. R., deployment of a Significant and All of the Randomized The Psychological
McGlinch, B. P., psychological sustained efforts have participants in controlled Resilience
Wall, M. H., Gold, resilience focused on this study have a trials (RCT) Intervention
B. S., & intervention for mobilization of medical or with adaptive described here
health care workers personal protective mental health design are was developed
Vinogradov, S.
during the equipment, intensive issue and advised felt to be a contemporaneousl
(2020). coronavirus disease
https://www.ncbi.n care beds, and medical to have a priority y with the
2019 pandemic
lm.nih.gov/pmc/art equipment, while medication during an emerging
icles/PMC7199769 substantially less during the study. infectious COVID-19
/ attention has focused disease pandemic, was
on preserving the outbreak rapidly deployed,
psychological health of since they and is a work in
the medical workforce can progress at the
tasked with addressing iteratively time of this
the challenges of the accept or article. Level 1 of
pandemic. reject key the program—the
hypotheses Battle Buddy
related to the system—is highly
intervention scalable, has no
throughout cost, and requires
the trial while very few
also resources apart
considering from endorsement
power for on the part of unit
meaningful and department
TYRON MASANGKAY
clinical leaders. Early
outcomes. anecdotal
The current evidence
project will (including the
provide experience of the
important authors) suggests
data for that it is easy to
designing a implement and
subsequent very beneficial. It
RCT to be is our hope that
deployed this approach may
should there provide direction
be a second to others who
wave of the seek to implement
COVID-19 their own
pandemic. psychological
resilience
programs.
Ultimately, the
data collected as
part of this effort
will aid in
evaluating its
effectiveness in
addressing the
mental health
needs of a diverse
health care
workforce during
a large-scale
emergency.
TYRON MASANGKAY
Prevalence of post-
2. Qiu, D., Li, Y., Li, traumatic This review aimed at Studies were Systematic presents the main
L., He, J., Ouyang, stress symptoms am examining the pooled included if they searches of characteristics of
F., & Xiao, S. ong people prevalence of post- meet the databases the 76 included
(2021). influenced traumatic stress following were studies. Among
https://www.cambr by COVID-19 outbr symptoms among criteria: (a) the conducted for them, 66 were in
idge.org/core/journ eak: a meta-analysis people exposed to the study was literature English and 10
als/european- trauma resulting from observational published on were in Chinese.
psychiatry/article/p COVID-19 outbreak. study; (b) the PubMed, Most of the
revalence-of- participants were EMBASE, included studies
posttraumatic- adult aged ≥18; Web of were from Asia,
stress-symptoms- (c) information Science, the such as China,
among-people- about prevalence Cochrane Indian, and
influenced-by- of post-traumatic Library, Singapore.
covid19-outbreak- stress symptoms PsycArticle, See Table 1 for
a- among people and Chinese the details. From
metaanalysis/363B exposed to the National the 76 papers, 1
29C5A1617CE0C4 trauma resulting Knowledge (1.31%) study
DF943883B379C6 from COVID-19 Infrastructure was rated as high
outbreak was until October quality, 70
provided; (d) the 14, 2020. (92.11%) were
full article was Statistical rated as moderate,
written in analyses were and 5 (6.58%)
English or performed were rated as low
Chinese. Studies using R quality. The
were excluded if software reliability for the
(a) the report was (PROSPERO quality
a review, registration assessment
comments, meta- number: between the two
analysis, or CRD4202018 reviewers (J.H.
protocol and (b) 0309). and F.Y.O.Y.)
the participants was rated as good
TYRON MASANGKAY
with comorbid (Kappa = 0.73)
symptoms or [Reference Sands
chronic disease and Murphy105].
(such as mental
illness, cancer,
etc.).
3. Cénat, J. M., Blais- Prevalence of We conducted a patients’, We searched A total of 2189
Rochette, C., symptoms of systematic review and colleagues’, and articles in articles were
Kokou-Kpolou, C. depression, anxiety, meta-analysis to family in their Medline, screened, 136
K., Noorishad, P. insomnia, estimate the pooled places around the Embase, full-text articles
G., Mukunzi, J. N., posttraumatic stress prevalence of globe. Different APA were assessed for
McIntee, S. E., ... disorder, and depression, anxiety, respondents, PsycInfo, eligibility. Fifty-
& Labelle, P. R. psychological insomnia, PTSD, and answer the CINAHL, five peer-
(2021) distress among Psychological distress survey or form Scopus, and reviewed studies
https://www.scienc populations affected (PD) related to for this Web of met inclusion
edirect.com/science by the COVID-19 COVID-19 among experiment or Science. criteria for the
/article/pii/S016517 pandemic: A affected populations. studies. Random- meta-analysis
8120332601 systematic review effects meta- (N=189,159). The
and meta-analysis analyses on prevalence of
the depression (k=46)
proportions was 15.97%
of individuals (95%CI, 13.24-
with 19.13). The
symptoms of prevalence of
depression, anxiety (k=54)
anxiety, was 15.15%
insomnia, (95%CI, 12.29-
PTSD, and 18.54). The
TYRON MASANGKAY
PD were prevalence of
generated and insomnia (k=14)
between- was 23.87%
group (95%CI, 15.74-
differences 34.48). The
for gender, prevalence of
healthcare PTSD (k=13) was
workers 21.94% (95%CI,
(HCWs), and 9.37-43.31).
regions where Finally, the
studies were prevalence of
conducted. psychological
distress (k=19)
was 13.29%
(95%CI, 8.80-
19.57). Between-
group differences
were only found
in HCWs
(z=2.69, p < 0.05)
who had a higher
prevalence of
insomnia than
others.
You might also like
- 44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)Document5 pages44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)Jay GutierrezNo ratings yet
- Coifman 2021Document3 pagesCoifman 2021Mădălina Liliana PopNo ratings yet
- Benefits of Psychological Preparation For Surgery: A Meta-AnalysisDocument13 pagesBenefits of Psychological Preparation For Surgery: A Meta-AnalysisPsic. Diego ZaizarNo ratings yet
- Pfefferbaum Jacobs Houston 2012 ChildrenDisastersFrameworkDocument11 pagesPfefferbaum Jacobs Houston 2012 ChildrenDisastersFrameworkSudar MonoNo ratings yet
- Untitled DocumentDocument2 pagesUntitled DocumentJasmin grace BustamanteNo ratings yet
- 539 FullDocument4 pages539 FullAymen BekirNo ratings yet
- Resiliencia SD BornoutDocument8 pagesResiliencia SD BornoutAlan Calderón BerrioNo ratings yet
- Trust and Public Health Emergency Events A Mixedmethods Systematic ReviewDocument21 pagesTrust and Public Health Emergency Events A Mixedmethods Systematic ReviewPutriNo ratings yet
- 1 s2.0 S2215036618302621 MainDocument2 pages1 s2.0 S2215036618302621 Mainstevenburrow06No ratings yet
- Suci Fitriani Po71241230266 Uas Evidence Based Kelas MeranginDocument2 pagesSuci Fitriani Po71241230266 Uas Evidence Based Kelas MeranginSoraya Shaqia RahayuNo ratings yet
- NR201 ReportDocument10 pagesNR201 ReportSeradallab Ch RishNo ratings yet
- Intensive & Critical Care Nursing: Ziad Alostaz, Louise Rose, Sangeeta Mehta, Linda Johnston, Craig DaleDocument11 pagesIntensive & Critical Care Nursing: Ziad Alostaz, Louise Rose, Sangeeta Mehta, Linda Johnston, Craig DalecindyNo ratings yet
- Activity 2Document5 pagesActivity 2Honey Bee S. PlatolonNo ratings yet
- Kepatuhan MaskerDocument8 pagesKepatuhan MaskerKhairul AsriNo ratings yet
- Devlin2020 PDFDocument8 pagesDevlin2020 PDFMatias FlammNo ratings yet
- Shekelle The TopDocument5 pagesShekelle The TopMatias MedelesNo ratings yet
- Module 6 - Safety Events - Planning The Immediate Media ResponseDocument4 pagesModule 6 - Safety Events - Planning The Immediate Media ResponseTjut Fiora Tsania OebitNo ratings yet
- 22 STS859Document8 pages22 STS859Raul VerasteguiNo ratings yet
- Managing The Risks and BenefitDocument8 pagesManaging The Risks and BenefitcacaNo ratings yet
- Group 2 - Class C - Critical ReviewDocument8 pagesGroup 2 - Class C - Critical ReviewSanti AsihNo ratings yet
- Malkin CH1 PDFDocument11 pagesMalkin CH1 PDFPatriciaMariaNo ratings yet
- Methodological_and_Ethical_Considerations_when_Con (1)Document11 pagesMethodological_and_Ethical_Considerations_when_Con (1)Lavinia BaleaNo ratings yet
- Rapid Need Assessment JournalDocument16 pagesRapid Need Assessment Journalzubaidah muizNo ratings yet
- 7 1 7 An Organising Principle, Target, and AccounDocument3 pages7 1 7 An Organising Principle, Target, and AccounCláudia SilvaNo ratings yet
- Triaging Spine Surgery in The COVID 19 Era.1Document2 pagesTriaging Spine Surgery in The COVID 19 Era.1Hesbon MomanyiNo ratings yet
- How To Write A Systematic Review A Step by Step GuideDocument6 pagesHow To Write A Systematic Review A Step by Step GuideWikeUlfianiAresa100% (2)
- Zhuang Et Al 2021 Interprofessional Collaboration During Covid 19 A Case Study of A Shanghai Quarantine Center ForDocument3 pagesZhuang Et Al 2021 Interprofessional Collaboration During Covid 19 A Case Study of A Shanghai Quarantine Center Formariajesica lindsenNo ratings yet
- 2020 - Which Psychotherapy Is Effective inDocument9 pages2020 - Which Psychotherapy Is Effective inadelacrovara.seoNo ratings yet
- Avanzando La Investigacion Academica de Covid 19Document4 pagesAvanzando La Investigacion Academica de Covid 19Sarita CadenaNo ratings yet
- Public Health Emergency Decisionmaking and Management System Sound Research Using Rough Set Attribute Reduction and Blockchainscientific ReportsDocument11 pagesPublic Health Emergency Decisionmaking and Management System Sound Research Using Rough Set Attribute Reduction and Blockchainscientific ReportsPradana Ananda RaharjaNo ratings yet
- Sierra Rui 2022 DACDocument10 pagesSierra Rui 2022 DACDiazAlejoPhierinaNo ratings yet
- Acm 2020 0177Document10 pagesAcm 2020 0177Ragavendrasamy BNo ratings yet
- Brain, Behavior, and Immunity: SciencedirectDocument7 pagesBrain, Behavior, and Immunity: SciencedirectMarinela MeliszekNo ratings yet
- Chap 7Document10 pagesChap 7Pamela Monique RuizNo ratings yet
- DNP 801A RS6 LiteratureEvaluationTableDocument5 pagesDNP 801A RS6 LiteratureEvaluationTableStephen ManjeNo ratings yet
- 2016 - Observational Research Methods. Research Design II Cohort, Cross Sectional, and Case-Control StudiesDocument8 pages2016 - Observational Research Methods. Research Design II Cohort, Cross Sectional, and Case-Control StudiesamarillonoexpectaNo ratings yet
- What de Fines Mindfulness-Based Programs? The Warp and The WeftDocument10 pagesWhat de Fines Mindfulness-Based Programs? The Warp and The Weft290971No ratings yet
- Roots, Not ParachutesDocument4 pagesRoots, Not ParachutescesiahdezNo ratings yet
- Wearable Systems For Unveiling Collective Intelligence in Clinical SettingsDocument29 pagesWearable Systems For Unveiling Collective Intelligence in Clinical SettingsjjNo ratings yet
- E100046 FullDocument8 pagesE100046 FullweloveyouverymuchNo ratings yet
- Suporte Avançado de Vida - SAVDocument63 pagesSuporte Avançado de Vida - SAVAna Luísa MenezesNo ratings yet
- J of Nursing Scholarship - 2021 - Sim - Contextualization of Psychological First Aid An Integrative Literature ReviewDocument9 pagesJ of Nursing Scholarship - 2021 - Sim - Contextualization of Psychological First Aid An Integrative Literature ReviewJoelNo ratings yet
- RRR Model ResilienceDocument12 pagesRRR Model Resiliencelorraine kate umaliNo ratings yet
- Di Mid Jian 2015Document28 pagesDi Mid Jian 2015NeilermindNo ratings yet
- E053043 FullDocument12 pagesE053043 FullU of T MedicineNo ratings yet
- A Review of The Transdiagnostic Road Map To Case Formulation and Treatment Planning: Practical Guidance For Clinical Decision MakingDocument2 pagesA Review of The Transdiagnostic Road Map To Case Formulation and Treatment Planning: Practical Guidance For Clinical Decision Makingbeatrizmachado6No ratings yet
- Part 2.3 Sample Multi - and Inter - Disciplinary PTs - Docx (6) 2Document3 pagesPart 2.3 Sample Multi - and Inter - Disciplinary PTs - Docx (6) 2Andremae LorenoNo ratings yet
- A Review of The Transdiagnostic Road Map To Case Formulation and Treatment Planning: Practical Guidance For Clinical Decision MakingDocument2 pagesA Review of The Transdiagnostic Road Map To Case Formulation and Treatment Planning: Practical Guidance For Clinical Decision MakingKAROL GUISELL PATIÑO ATEHORTUANo ratings yet
- 6 Journal-of-Physics-Serie-de-conferenciasDocument11 pages6 Journal-of-Physics-Serie-de-conferenciaslauraNo ratings yet
- EconomicsDocument5 pagesEconomicsLaras SartikaNo ratings yet
- What Is The Role of The Social Sciences in The Response To COVIDDocument5 pagesWhat Is The Role of The Social Sciences in The Response To COVIDJack MonterNo ratings yet
- Assignment Evidence-Based Project, Part 1 - Identifying Research MethodologiesDocument6 pagesAssignment Evidence-Based Project, Part 1 - Identifying Research MethodologiesJoseph AkitongaNo ratings yet
- Artikel 1Document8 pagesArtikel 1Johansen HutajuluNo ratings yet
- Pi Is 0140673620307297Document2 pagesPi Is 0140673620307297Koushik MajumderNo ratings yet
- Designing A Research Project: Randomised Controlled Trials and Their PrinciplesDocument6 pagesDesigning A Research Project: Randomised Controlled Trials and Their PrinciplesErik GarNo ratings yet
- MEDICAL Rehabilitation IN DISASTER RELIEF TOWARDS A NEW PERSPECTIVEDocument9 pagesMEDICAL Rehabilitation IN DISASTER RELIEF TOWARDS A NEW PERSPECTIVEjaymarmandiaNo ratings yet
- The Toughest Triage - Allocating Ventilators in A Pandemic: PerspectiveDocument3 pagesThe Toughest Triage - Allocating Ventilators in A Pandemic: Perspectiveskyyblue10No ratings yet
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- Particle emission concept and probabilistic consideration of the development of infections in systems: Dynamics from logarithm and exponent in the infection process, percolation effectsFrom EverandParticle emission concept and probabilistic consideration of the development of infections in systems: Dynamics from logarithm and exponent in the infection process, percolation effectsNo ratings yet
- Formation Program (S.Y. 2021-2022) : AssociationDocument3 pagesFormation Program (S.Y. 2021-2022) : AssociationJay GutierrezNo ratings yet
- Ecology Ministry & Plastic Bank Project/Proposal: JanuaryDocument5 pagesEcology Ministry & Plastic Bank Project/Proposal: JanuaryJay GutierrezNo ratings yet
- Activity For Balance of PaymentDocument2 pagesActivity For Balance of PaymentJay GutierrezNo ratings yet
- Human Resource ManagementDocument3 pagesHuman Resource ManagementJay GutierrezNo ratings yet
- Adaptive Community For The Continuity of Education and Student Services National Teachers CollegeDocument7 pagesAdaptive Community For The Continuity of Education and Student Services National Teachers CollegeJay GutierrezNo ratings yet
- 44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)Document5 pages44albott, C. S., Wozniak, J. R., Mcglinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020)Jay GutierrezNo ratings yet
- 2016 SSHD Research ContributionsDocument3 pages2016 SSHD Research ContributionsJay GutierrezNo ratings yet
- Reflection About BioethicsDocument1 pageReflection About BioethicsJay GutierrezNo ratings yet
- Episkleritis Dan SkleritisDocument41 pagesEpiskleritis Dan SkleritisSuryana AdityaNo ratings yet
- Pathology: Fajar L. Gultom Departemen Patologi Anatomik FK UKI April 2019Document39 pagesPathology: Fajar L. Gultom Departemen Patologi Anatomik FK UKI April 2019ErniNo ratings yet
- A Guide To Aspen Healthcare BrochureDocument8 pagesA Guide To Aspen Healthcare BrochureAntonio LoscialeNo ratings yet
- Nursing Care of Patients With Ventilation DisordersDocument33 pagesNursing Care of Patients With Ventilation DisordersYAMINIPRIYANNo ratings yet
- Physical Activity For HealthDocument7 pagesPhysical Activity For Healthshd9617No ratings yet
- 2.nutrition Guide For Physicians PDFDocument444 pages2.nutrition Guide For Physicians PDFMauro Lopez100% (2)
- Mental Retardation 1Document4 pagesMental Retardation 1Aizah Lazo LuzonNo ratings yet
- CPDprogram NURSE91917Document100 pagesCPDprogram NURSE91917PRC Board100% (1)
- Urolithiasis - Final Case StudyDocument63 pagesUrolithiasis - Final Case StudyLovely Grace PoreNo ratings yet
- Leukoplakia 201119144109Document24 pagesLeukoplakia 201119144109saldy meirisandyNo ratings yet
- Revised-Chapter 6 Case Study BDocument2 pagesRevised-Chapter 6 Case Study BAngelica PerezNo ratings yet
- NCP For Bronchopneumonia With 7 Nursing DiagnosisDocument4 pagesNCP For Bronchopneumonia With 7 Nursing DiagnosisBeng AlontoNo ratings yet
- Kashif-Zaman 1001692787Document1 pageKashif-Zaman 1001692787Mithun KumarNo ratings yet
- Ateletaksis Case ReportDocument17 pagesAteletaksis Case Reportnina purnamasariNo ratings yet
- Clinical Teaching ON Geriatric AssessmentDocument9 pagesClinical Teaching ON Geriatric AssessmentANITTA SNo ratings yet
- Acute AppendicitisDocument63 pagesAcute AppendicitisIsis Elektra100% (1)
- GFSDGSDGFSDGDocument2 pagesGFSDGSDGFSDGMA IZNo ratings yet
- Case Synthesis: MEDICAL MALPRACTICEDocument5 pagesCase Synthesis: MEDICAL MALPRACTICERegina Via G. Garcia0% (1)
- Fasting EnemaDocument108 pagesFasting Enemavskliris1100% (2)
- Thoracic Outlet Syndrome Exercises IIDocument2 pagesThoracic Outlet Syndrome Exercises IIRiaz KhanNo ratings yet
- Infection Control in Burns PatietnsDocument41 pagesInfection Control in Burns Patietnstummalapalli venkateswara raoNo ratings yet
- Vaccines 08 00321Document17 pagesVaccines 08 00321Kshitiz Raj ShresthaNo ratings yet
- 6 - Immune Deficiency Diseases 2Document8 pages6 - Immune Deficiency Diseases 2Belle Galao GepteNo ratings yet
- Management of C Shaped Canals: 3 Case ReportsDocument3 pagesManagement of C Shaped Canals: 3 Case ReportsTaufiqurrahman Abdul Djabbar100% (1)
- (EPI) 1.04 Accuracy of Observations and Measurements (Dr. Zulueta)Document5 pages(EPI) 1.04 Accuracy of Observations and Measurements (Dr. Zulueta)pasambalyrradjohndarNo ratings yet
- Eosinophilic Ulcer of The Oral MucosaDocument4 pagesEosinophilic Ulcer of The Oral MucosaKhairunnisa Indah NurfaizahNo ratings yet
- Kidney Stones: Kim Applebee Alex KaullenDocument26 pagesKidney Stones: Kim Applebee Alex KaullenPatrascu CristiNo ratings yet
- Micro paraDocument9 pagesMicro paraRaph GadianaNo ratings yet
- Lab Manual CSI103Document30 pagesLab Manual CSI103Nurul AinNo ratings yet
- Physiology of The Cerebrospinal FluidDocument6 pagesPhysiology of The Cerebrospinal FluidShereen Al-ObinayNo ratings yet