Professional Documents
Culture Documents
Research Journal of Pharmaceutical, Biological and Chemical Sciences
Research Journal of Pharmaceutical, Biological and Chemical Sciences
Uploaded by
Indah GitaswariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Research Journal of Pharmaceutical, Biological and Chemical Sciences
Research Journal of Pharmaceutical, Biological and Chemical Sciences
Uploaded by
Indah GitaswariCopyright:
Available Formats
ISSN: 0975-8585
Research Journal of Pharmaceutical, Biological and Chemical
Sciences
Management of Mandibular Fractures with Conventional Miniplates - A
Review.
Saravana Kumar*, Balakrishnan, Abu Dakir, Muthumani, NP Prabu, and Waikhom Arvind.
Department of Oral and Maxillofacial Surgery, Sree Balaji Dental College And Hospital, Chennai, Tamil Nadu-600100, India.
ABSTRACT
The management of trauma has evolved greatly over the past many years. Various bone plating
have been introduced for stable fixation of mandibular fractures. The present concept of treating
mandibular fractures is with non-compression mini plates which relieves the patient from a hazardous
intermaxillary fixation with wires and gives better stability and osteosynthesis. When placed along the
Champy’s line of Osteosynthesis Miniplates gave maximum stability and Osteosynthesis. This article
presents an overview of management of mandibular fractures with mini plates.
Keywords: Mandibular Fractures, Miniplates, Champy`s line.
*Corresponding author
May – June 2015 RJPBCS 6(3) Page No. 120
ISSN: 0975-8585
INTRODUCTION
Mandibular fractures are more common than middle third fracture (anatomical factor). It could be
observed either alone or in combination with other facial fractures. Minor mandibular fracture may be
associated with head injury owing to the cranio-mandibular articulation. Mandibular fracture may compromise
the patency of the airway in particular with loss of consciousness. It has been found that fracture of mandible
can occur with frontal impact force as low as 425 lb (190 Kg) (Condylar fracture). Fracture of condyle is
regarded as a safety mechanism to the patient. Frontal force of 800-900 lb (350-400 Kg) is required to cause
symphysial fracture. Mandible is more sensitive to lateral impact than frontal one. Frontal impact is
substantially cushioned by opening and retrusion of the jaw (Nahum 1975). Long canine tooth and partially
erupted wisdom represent line of relatively weakness. The most significant advancements related to the
management of fractures of the mandible are based on specific technical refinements in the methods of
internal fixation. Recent mandibular fracture management techniques have allowed for decreased infection
rates and biological stable fixation of bone segments. The present concept of treating mandibular fractures is
with non compression mini plates which relieves the patient from a hazardous intermaxillary fixation with
wires and gives better stability and osteosynthesis. This review article presents an overview of management of
mandibular fractures with mini plates.
Literature review
History reveals that mandible fractures and treatment dates back as early as 1650 BC in papyrus by
Edwin Smith. Hippocrates described the treatment of fracture to be done with gold wirings and he himself did
circumferential dental wiring for mandibular fractures. In 1275 Salicetti first presented maxillomandibular
fixation as a treatment for fractures of the mandibles, [1, 2] After a decade it as Gilmer who revived Salicetti’s
technique and practiced it clinically more efficiently in 1887. [3] Mostly throughout the 20th century
intermaxillary fixation along with splints and bandages were the only modality of treatment for mandibular
fractures. Few unsuccessful reports of treating mandibular fractures by open reduction with silver wires or iron
loops had been reported [4, 5]. In 1976, Spiessl and others continued to advance techniques of open reduction
and internal fixation (ORIF) and developed the principles now advocated by the Arbeitsgemeinschaft fur
Osteosynthesefragen (Association for Osteosynthesis/ Association for the Study of Internal Fixation (AO/ ASIF)
[6]. These plates were heavy and bulky. However these plates did help to achieve better stability rather than
the conventional inter maxillary fixation by wirings. Even though these plating techniques had benefits of
avoiding maxillomandibular fixation by wiring, including comfort, return to normal mastication and normal oral
function, in reality, these heavy compression plates had a high morbidity. The neck scars were undesirable,
nerve damage to both the facial and inferior alveolar nerves was common and infection of the plates frequent;
a second operation to remove the plates was always necessary. The principles of heavy compression plating
could not be applied to the thin bones of the upper facial skeleton. Next came the system of lag screws where
big screws are attached through the fragmented segments and they are tightened to bring the fractured ends
together. This system didn`t show much promise and had limited use in mandibular fractures even though
intraoral surgical techniques were used.
MANDIBULAR FRACTURES
May – June 2015 RJPBCS 6(3) Page No. 121
ISSN: 0975-8585
Michelet and his colleagues introduced the concept of internal fixation with small miniplates for fixing
and stabilizing mandibular fractures in 1970 [7]. Champy and his co workers in 1978 modified this technique
to use small, bendable and noncompression mini plates along the ideal line of osteosynthesis(8) for treating
mandibular fractures. These plates were fixed with monocortical mini screws. They were not heavy. When
placed along the Champy’s line of osteosynthesis they gave maximum stability and osteosynthesis. Last but not
least the use of small miniplates was successfully integrated into the rest of the facial skeleton, being refined
and miniaturized for the periorbital and cranial non-load bearing areas.
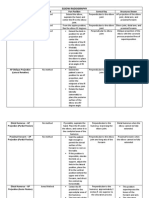
It is very important to know the classification of mandibular fractures. The mandible fractures can be
classified by Dingman and Natvig [9] on the basis of anatomy as - midline (Fractures between central incisors),
symphysis fractures (Bounded by vertical lines distal to canine teeth), parasymphysis fractures (Fractures
occuring in the area of symphysis), body of mandible fractures (From the distal symphysis to a line coinciding
with the alveolar border of the masseter muscles), angle fractures (Triangular region bounded by the anterior
border of the masseter muscle to the posterosuperior attachment of the masseter muscles), ramus (fractures
bounded by the superior aspect of the angle to two lines forming an apex at the sigmoid notch), coronoid(
includes the coronoid process of the mandible superior to the ramus region) and condylar( Area of the
condylar process superior to the ramus region) fractures. There are several other classifications of mandibular
fractures in literature. Second most important thing is to know about the biomechanics of mandibular
fractures.
Biomechanics of the mandible is a complex topic. Forces applied to the mandible cause varying zones
of tension and compression, depending on where the bite force is located. The superior portion of the
mandible is designated as the tension zone and the inferior portion is designated as the compression zone.
The mandible is a hoop of bone that deforms with movement based on the origin and insertion of the
muscles of mastication viz masseter, temporalis, medial and lateral pterygoid muscles.
May – June 2015 RJPBCS 6(3) Page No. 122
ISSN: 0975-8585
The superior border of the mandible is the tension zone and the inferior border is the compression
zone.
The mandible is similar to a hunting bow in shape, strongest in the midline (symphysis) and weakest
at both ends (condyles). The most common area of fracture in the mandible is therefore the condylar region. A
blow to the anterior mandibular body is the most common reason for condylar fracture. The force is
transmitted from the body of the mandible to the condyle. The condyle is trapped in the glenoid fossa.
Commonly, a blow to the ipsilateral mandible causes a contralateral fracture in the condylar region. If the
impact is in the midline of the mandible, fractures of the bilateral condylar region are very common.
Champy popularized the treatment of mandible fractures with miniplate fixation along the ideal lines
of osteosynthesis. This is a form of load-sharing osteosynthesis to be applied in simple fracture patterns having
an acceptable amount of bone stock.
The ideal line of osteosynthesis in the body region runs at the vertical height of the tooth apices from
the canine region to the oblique line. This carries into the oblique ridge which turns into the anterior outer rim
of the ramus. All biomechanical models developed to date have shown that two points of fixation (ie, two
plates) provide much more stability than a single one. The basal triangle decreases the bone buttressing and
interfragmentary support. This condition demands a degree of stability beyond pure load sharing. The superior
border plate is positioned on the ideal line of osteosynthesis. The inferior border plate is located at the base of
the mandibular body in a longitudinal field below the course of the mandibular canal.
May – June 2015 RJPBCS 6(3) Page No. 123
ISSN: 0975-8585
It is Champy and his coworkers who started the system of semi rigid fixation with mini plates and
screws. This form of load-sharing osteosynthesis with the miniplate fixation technique popularized by Champy
suggests that when the plates are placed along the ideal line of osteosynthesis they give maximum stability
and proper osteosynthesis.
MINIPLATES (SEMI RIGID FIXATION)
Champy et al., defined the "ideal lines of osteosynthesis" based on experiments of GEBOAS (Group of
Research in Bones and Joint Biomechanics of Strasbourg) [10]. It is Champy and his coworkers who
revolutionised the system of semi rigid fixation with mini plates and screws. This form of load-sharing
osteosynthesis with the miniplate fixation technique popularized by Champy suggests that when the plates are
placed along the ideal line of osteosynthesis they give maximum stability and proper osteosynthesis.. These
plates were first introduced as stainless steel plates. It consisted of mono-cortical, juxta alveolar, and subapical
osteosynthesis without compression and intermaxillary fixation using miniaturized malleable plates. Small size
of the plate(thickness - 2mm), easy adaptability, easy placement, and use of intraoral approach led to
increased use of mono-cortical plates in maxillofacial surgery. [11]
Introduced by Champy and his coworkers this method has been successfully used since then and
underwent several modifications. However these plates can be placed by intraoral surgical approaches. The
May – June 2015 RJPBCS 6(3) Page No. 124
ISSN: 0975-8585
technique suggests placing a single miniplate in the subapical region or along the external oblique ridge when
fractures are posterior to the mental foramen. Anterior to the foramen 2 miniplates are used to resist the
forces of torsion. In mandible fracture, an arch bar is preferred for MMF. This equates to a second line of
resistance in particular with biting load anterior to the fracture line. The superior plate is inserted first in order
to achieve preliminary fixation. This will prevent inadvertent displacement of the fragments during subsequent
contouring and the insertion of the inferior border plate. The 1st miniplate is placed in the subapical region
and the 2nd plate 5mm inferior to the first plate and fixed with monocortical mini screws of 2mm diameter.
These screws are generally self tapping which comes in several lengths such as 2mm, 4mm, 6mm, 8mm and
10mm. Usually in mandible for fixing the miniplates (2 or 2.5) x 8mm or (2 or 2.5) x 10mm screws are used.
These mini plates are used to stress shield the forces of tension and torsion. At the same time it allows the
biomechanical forces of compression to work which is the advantage of this technique.
DISCUSSION
Several factors guide the management of mandibular fractures like dental and orthopaedic principles
like reduction of the fracture site to its correct anatomical position, restoration of pre morbid occlusion and
rigid immobilization of the fractures which facilitates healing, optimal and early restoration of function,
prevention of infection, malunion or nonunion of fracture [12]. Management of mandibular fractures started
with maxillary mandibular fixation with stainless steel wires. After that decade has passed and the treatment
modality advanced from wiring to lag screws to miniplates. Champy et al first introduced the semi rigid mini
plates. Michelet et al (1973) began experimenting with monocortical non- compression miniplates. Using a
simple cantilever beam model, Champy et al showed that the superior mandibular border was subjected to
tension and splaying, and the inferior border was subjected to compression. The transition zone between the
areas of tension and compression has been referred to as a “line of zero force” running along the inferior
alveolar nerve. Champy‟s experiment with miniplates further delineated the “ideal line of osteosynthesis”
within the mandible. The miniplate uses the tension-banding principle as described by Champy et al [8] A
single miniplate seemed to be more successful (overall complication rate, 7%) than the lag screws (14%) in the
management of mandibular angle fracture. However, Luhr and AO/ASIF advocates felt that miniplates did not
offer adequate stabilization of the fractures, thereby necessitating the need of further inter-maxillary fixation.
[13] Farmand and Dupoirieux presented 3-D plates with quadrangular shape formed by joining two mini-
plates with interconnecting crossbars [13]. Because of the quadrangular configuration of the plates, they
provided good stability and resistance to torsional forces. Easy use, good resistance against torque forces, and
compact form of the plates were some of their advantages. The author in Sree Balaji Dental College And
Hospital studied 100 cases of mandibular fractures for past 1 year consisting of 41 parasymphysis fractures, 35
body fractures, 17 angle fractures and 7 symphysis fractures and all were treated with conventional mini plate
fixation. As per Champys ideal line of osteosynthesis two plates were placed in symphysis and parasymphysis
fracture region and single mini plate in the body and angle fracture. 5% of total patients underwent for
infection followed by plate removal and 2% suffered parasthesia which was present for 5 and 6 months
respectively after which the patients regained the sense.
May – June 2015 RJPBCS 6(3) Page No. 125
ISSN: 0975-8585
REFERENCES
[1] Salicetti G. Cyrurgia 1275.
[2] Prevost N. Translation of Salicetti's Cyrurgia. Lyons, France 1492
[3] Gilmer TL. Arch Dentistr 1887; 4: 388
[4] Buck G. Annalist NY 1846; 1:245.
[5] Dorrance GM, Bransfield JW. The History of Treatment of Fractured Jaws, vols 1 and 2 Washington,
DC, 1941.
[6] Spiessl B. New concepts in maxillofacial bone surgery. Springer-Verlag, Berlin 1976
[7] Michelet FX, Deymes J. Dessus B. J Maxillofac Surg 1973; 1: 79.
[8] Champy M, Lodde JP, Schmitt R, et al. J Maxillofac Surg 1978;6: 14.
[9] Dingman RO , Natvig P. Surgery of facial fractures, Philadelphia,1964, WB Saunders.
[10] Champy M, Pape HD. The strasbourg miniplate osteosynthesis. In: Kruger E, Schilli W, editors. Oral
and Maxillofacial Traumotology. vol. 2. Berlin: Quintessence; 1986. p. 19-43.
[11] Cawood JI. Br J Oral Maxillofac Surg 1985;23:77- 91.
[12] Harold Kai Tu, David Tenhulza. J Oral Maxillof Surg 1985; 43: 585-589
[13] Luhr HG. Otolaryngol Clin North Am 1987; 20:573-606.
[14] Farmand M, Dupoirieux L. Rev Stomatol Chir Maxillofac 1992; 93: 353-7.
May – June 2015 RJPBCS 6(3) Page No. 126
You might also like
- NASM 6th Edition Study GuideDocument44 pagesNASM 6th Edition Study GuideRyanClancy100% (3)
- First Impressions Count: RestorativeDocument12 pagesFirst Impressions Count: RestorativeMasitah GraceNo ratings yet
- Rockwood and Matsen S The Shoulder 4th EditionDocument1,616 pagesRockwood and Matsen S The Shoulder 4th EditionCristina Maria67% (6)
- Shoulderless Preliminary DraftDocument29 pagesShoulderless Preliminary Draftvrana23-1100% (2)
- Fractures of The Middle Third of The Facial SkeletonDocument7 pagesFractures of The Middle Third of The Facial SkeletonMahendra Perumal50% (2)
- TMJ Splints SaherDocument94 pagesTMJ Splints SaherAnkita AgarwallNo ratings yet
- Mandibular FrakturDocument17 pagesMandibular Frakturmuhammad rezky juniNo ratings yet
- Oral Surgery - Dr. Labeed SamiDocument22 pagesOral Surgery - Dr. Labeed SamiMohammed TarekNo ratings yet
- Intramedullary Nailing of The Proximal Humerus: Evolution, Technique, and ResultsDocument9 pagesIntramedullary Nailing of The Proximal Humerus: Evolution, Technique, and ResultsAna MariaNo ratings yet
- Comparison of 3-D Locking Miniplates Versus Conventional Miniplates in Anterior Mandibular FracturesDocument9 pagesComparison of 3-D Locking Miniplates Versus Conventional Miniplates in Anterior Mandibular FracturesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Eyelets Vs Arch Bar 2017Document12 pagesEyelets Vs Arch Bar 20176hd6mnrzw2No ratings yet
- Evaluation of Titanium Lag Screw Osteosynthesis in The Management of Mandibular FracturesDocument6 pagesEvaluation of Titanium Lag Screw Osteosynthesis in The Management of Mandibular Fracturesleslie kalathilNo ratings yet
- Goyal 2012Document9 pagesGoyal 2012rahulNo ratings yet
- J Jds 2019 12 003Document6 pagesJ Jds 2019 12 003aDITYA GUJARENo ratings yet
- Management of Fracture of The Edentulous Mandible Oral SurgeryDocument27 pagesManagement of Fracture of The Edentulous Mandible Oral SurgeryFourthMolar.comNo ratings yet
- MANAGEMENT OF MANDIBULAR FRACTURES - Ghiffar Oka Prihardian - 18700062Document22 pagesMANAGEMENT OF MANDIBULAR FRACTURES - Ghiffar Oka Prihardian - 18700062fransiscaNo ratings yet
- TestoriDocument7 pagesTestoriGgNo ratings yet
- Humeral FractureDocument9 pagesHumeral FractureAustine Osawe100% (1)
- Principles of Fixation For Maxillofacial Trauma PatientsDocument69 pagesPrinciples of Fixation For Maxillofacial Trauma PatientsSiyum MathewosNo ratings yet
- Menisco Current ConceptDocument7 pagesMenisco Current ConceptJulio Cesar Guillen MoralesNo ratings yet
- Diaphyseal Femur FracturesDocument9 pagesDiaphyseal Femur FracturesSoulmates1No ratings yet
- Pi Is 1043181008000225Document5 pagesPi Is 1043181008000225drbhaskar128No ratings yet
- Oh 2010Document5 pagesOh 2010gbaez.88No ratings yet
- El Tratamiento de Las Fracturas Del Ángulo MandibularDocument8 pagesEl Tratamiento de Las Fracturas Del Ángulo MandibularCristhian ChanaméNo ratings yet
- Subtrochanteric Fracture Non-Unions With Implant Failure Managed With The "Diamond" ConceptDocument6 pagesSubtrochanteric Fracture Non-Unions With Implant Failure Managed With The "Diamond" ConceptsaimanojkosuriNo ratings yet
- Mandibular Condylar and Subcondylar Fractures PDFDocument16 pagesMandibular Condylar and Subcondylar Fractures PDFWayan Sutresna YasaNo ratings yet
- Risks and Complications of Orthodontic MiniscrewsDocument51 pagesRisks and Complications of Orthodontic MiniscrewsutokaNo ratings yet
- 1 s2.0 S0901502715013521 MainDocument7 pages1 s2.0 S0901502715013521 MainGabriellaMariaNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument31 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsmustafasacarNo ratings yet
- Cous Ley 2015Document6 pagesCous Ley 2015druzair007No ratings yet
- Trauma ZygomaDocument9 pagesTrauma ZygomarezaaamuhammadNo ratings yet
- Aosm004 01 01Document12 pagesAosm004 01 01elhadidimahmoudNo ratings yet
- 2019 - From Rigid Bone Plate Fixation To Stable Dynamic Osteosynthesis in Mandibular and Craniomaxillo-Facial Surgery: Historical Evolution of Concepts and Technical DevelopmentsDocument5 pages2019 - From Rigid Bone Plate Fixation To Stable Dynamic Osteosynthesis in Mandibular and Craniomaxillo-Facial Surgery: Historical Evolution of Concepts and Technical DevelopmentsLeandro Nascimento Rodrigues dos santosNo ratings yet
- Locked Plating Biomechanics and Biology - 2007Document6 pagesLocked Plating Biomechanics and Biology - 2007VadymNo ratings yet
- Mandible FracturesDocument17 pagesMandible FracturesYaser JasNo ratings yet
- 2 Anatomy of TMJDocument117 pages2 Anatomy of TMJSugandhi Pidaparthi100% (1)
- The Shoulderless Approach by TTDocument19 pagesThe Shoulderless Approach by TTMahmoud HeshamNo ratings yet
- Im NailsDocument94 pagesIm NailsYasmina Qabbani100% (1)
- Osseous Resective Surgery: G C & W B. KDocument29 pagesOsseous Resective Surgery: G C & W B. KYashNo ratings yet
- Preliminary Report On A Staged Ridge Splitting Technique For Implant Placement in The Mandible: A Technical NoteDocument5 pagesPreliminary Report On A Staged Ridge Splitting Technique For Implant Placement in The Mandible: A Technical NoteSaurabh SatheNo ratings yet
- UntitledDocument35 pagesUntitledGiselmar Soto DíazNo ratings yet
- TMJ Osteoarthritis Case Report Lubna M. QanberDocument6 pagesTMJ Osteoarthritis Case Report Lubna M. QanberLubna QanberNo ratings yet
- JC TMJDocument59 pagesJC TMJGowda Sharad SureshNo ratings yet
- 1 s2.0 S1991790219308700 MainDocument6 pages1 s2.0 S1991790219308700 MainRonin ZxxNo ratings yet
- OAJSM 7753 Meniscal Tears - 042110Document10 pagesOAJSM 7753 Meniscal Tears - 042110Chrysi TsiouriNo ratings yet
- Degenerative Meniscus - Pathogenesis, Diagnosis, and Treatment Options - PMCDocument10 pagesDegenerative Meniscus - Pathogenesis, Diagnosis, and Treatment Options - PMCAhmedNo ratings yet
- Mandibular FracturesDocument33 pagesMandibular FracturesDrMuskan AroraNo ratings yet
- Titanium Lag Screw Versus Miniplate Fixation in The Treatment of AnteriorDocument31 pagesTitanium Lag Screw Versus Miniplate Fixation in The Treatment of Anterioranusha guptaNo ratings yet
- Os Finals ReviewerDocument33 pagesOs Finals ReviewerGuen ColisNo ratings yet
- Jaw Surgery: Robert M. Menard, Nikhil K. DesaiDocument10 pagesJaw Surgery: Robert M. Menard, Nikhil K. DesaiAlain AguirreNo ratings yet
- 8 Surgical Anatomy of TMJDocument11 pages8 Surgical Anatomy of TMJArchanaShenoyNo ratings yet
- Comparative Evaluation of Various Miniplate Systems For The Repair of Mandibular Corpus FracturesDocument5 pagesComparative Evaluation of Various Miniplate Systems For The Repair of Mandibular Corpus Fracturesmehak malhotraNo ratings yet
- 10 11607@jomi 8122Document8 pages10 11607@jomi 8122Marlene Kasumi Gantier TakanoNo ratings yet
- Edent DistDocument70 pagesEdent Distminatta100% (1)
- Iliac Crest Grafting For Mandibular ReconstructionDocument10 pagesIliac Crest Grafting For Mandibular Reconstructiontanvi vijayNo ratings yet
- The Composite Spreader FlapDocument11 pagesThe Composite Spreader FlapameliNo ratings yet
- 1.a) Structure:: Fibrocartilaginous Knee Tibia Femur Fossae CondylesDocument11 pages1.a) Structure:: Fibrocartilaginous Knee Tibia Femur Fossae CondylesWaiKheongNo ratings yet
- Interlocking Nailining Minimally Invasive OsteosynthesisDocument28 pagesInterlocking Nailining Minimally Invasive Osteosynthesistvm1018No ratings yet
- Rapid Maxillary Expansion A ReviewDocument6 pagesRapid Maxillary Expansion A ReviewInternational Journal of Innovative Science and Research Technology100% (1)
- Meniscal Tear: Presentation, Diagnosis and Management: Australian Family Physician April 2012Document6 pagesMeniscal Tear: Presentation, Diagnosis and Management: Australian Family Physician April 2012raditya kusumaNo ratings yet
- Carlino 2019Document9 pagesCarlino 2019Isabella WilkeNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- An 385Document8 pagesAn 385Indah GitaswariNo ratings yet
- 10 1016@j Oraloncology 2020 104804Document5 pages10 1016@j Oraloncology 2020 104804Indah GitaswariNo ratings yet
- Review Article: Recent Advances of Hemorrhage Management in Severe TraumaDocument6 pagesReview Article: Recent Advances of Hemorrhage Management in Severe TraumaIndah GitaswariNo ratings yet
- Stress Distribution in Mandible and Temporomandibular Joint by Mandibular Distraction: A 3-Dimensional Finite-Element AnalysisDocument10 pagesStress Distribution in Mandible and Temporomandibular Joint by Mandibular Distraction: A 3-Dimensional Finite-Element AnalysisIndah GitaswariNo ratings yet
- Positioning The Instillation of Contrast Cystography: Does It Provide Any Clinical Benefit?Document17 pagesPositioning The Instillation of Contrast Cystography: Does It Provide Any Clinical Benefit?Indah GitaswariNo ratings yet
- Journal Pre-Proof: Acta BiomaterialiaDocument45 pagesJournal Pre-Proof: Acta BiomaterialiaIndah GitaswariNo ratings yet
- Management of The Injured Hand - Basic PrinciplesDocument6 pagesManagement of The Injured Hand - Basic PrinciplesIndah GitaswariNo ratings yet
- The Role of Brain-Derived Neurotrophic Factor (BDNF) in Cognitive FunctionsDocument8 pagesThe Role of Brain-Derived Neurotrophic Factor (BDNF) in Cognitive FunctionsIndah GitaswariNo ratings yet
- Accepted Manuscript: NeuroscienceDocument40 pagesAccepted Manuscript: NeuroscienceIndah GitaswariNo ratings yet
- Gordon 2016Document16 pagesGordon 2016Indah GitaswariNo ratings yet
- Reconstruction of The Nasal ColumellaDocument5 pagesReconstruction of The Nasal ColumellaIndah GitaswariNo ratings yet
- Static Stretching ExercisesDocument6 pagesStatic Stretching ExercisesJai Seng100% (1)
- Wang 2016 JSES Trends Associated With Distal Biceps Tendon Repair in The U.S, 2007 To 2011Document5 pagesWang 2016 JSES Trends Associated With Distal Biceps Tendon Repair in The U.S, 2007 To 2011Kuozram No MasNo ratings yet
- (1893) Spalding's Athletic Library: BoxingDocument56 pages(1893) Spalding's Athletic Library: BoxingHerbert Hillary Booker 2nd75% (4)
- A Pattern Recognition Approach To Myopathy.15Document24 pagesA Pattern Recognition Approach To Myopathy.15Maryam NabNo ratings yet
- Pe 1 Task 4Document9 pagesPe 1 Task 4Rex Lander BlanzaNo ratings yet
- Neurologic Examination of Newborn and InfantsDocument6 pagesNeurologic Examination of Newborn and InfantsRem AlfelorNo ratings yet
- Frozen Shoulder Phase 2ExorLive-WorkoutDocument2 pagesFrozen Shoulder Phase 2ExorLive-WorkoutJomari ServanoNo ratings yet
- Li 3 Muscles and MovementsDocument3 pagesLi 3 Muscles and MovementsMei BejeranoNo ratings yet
- Zimmer Nexgen Tibial Stem Extension Augmentation Surgical TechniqueDocument16 pagesZimmer Nexgen Tibial Stem Extension Augmentation Surgical TechniqueTudor MadalinaNo ratings yet
- Anatomy Decoded - Q & A 1 To 7 Upper Limb - WhatsApp Premium Group PDFDocument43 pagesAnatomy Decoded - Q & A 1 To 7 Upper Limb - WhatsApp Premium Group PDFNijam Udeen100% (1)
- Validity of The Lateral Gliding Test As Tool ForDocument7 pagesValidity of The Lateral Gliding Test As Tool ForFelippe GuarigliaNo ratings yet
- MCQ Rheumatology ReviewDocument70 pagesMCQ Rheumatology ReviewM100% (4)
- Effect of Static Knee Joint Flexion On Vastus Medialis Obliquus Fiber Angle in Patellofemoral Pain Syndrome - An Ultrasonographic StudyDocument9 pagesEffect of Static Knee Joint Flexion On Vastus Medialis Obliquus Fiber Angle in Patellofemoral Pain Syndrome - An Ultrasonographic Studycris weeNo ratings yet
- Material Mini NetterDocument21 pagesMaterial Mini NetterVALENTINA ALBORNOZ BASTÍASNo ratings yet
- Fractura Columnae VertebralisDocument4 pagesFractura Columnae VertebralisTheo DapamedeNo ratings yet
- Muscle Tissue: Matthew Velkey, PH.DDocument40 pagesMuscle Tissue: Matthew Velkey, PH.DREMAN ALINGASANo ratings yet
- Orthopedic One Liners Mci ImpDocument15 pagesOrthopedic One Liners Mci ImpadiNo ratings yet
- Cartilage FactsDocument4 pagesCartilage FactsMJ BotorNo ratings yet
- Untamed MDMW Home 1-2Document5 pagesUntamed MDMW Home 1-2Leena FranklinNo ratings yet
- Review Jurnal: Poltekkes Kemenkes Semarang Jurusan Keperawatan Prodi Ners 2018Document7 pagesReview Jurnal: Poltekkes Kemenkes Semarang Jurusan Keperawatan Prodi Ners 2018Muslikah Ida Mugi RahayuNo ratings yet
- The Warm-Up: Sabina Rubio SánchezDocument19 pagesThe Warm-Up: Sabina Rubio Sánchezsabirubiosa5741No ratings yet
- BPE 105 - Movement Education - Final ExamDocument5 pagesBPE 105 - Movement Education - Final ExamJoseph Bernard Marcelo100% (2)
- Osteoarthritis (Oa) : Prakash Thakulla InternDocument48 pagesOsteoarthritis (Oa) : Prakash Thakulla InternPrakash ThakullaNo ratings yet
- 2.introduction To MovementsDocument36 pages2.introduction To MovementsZuhaib AhmedNo ratings yet
- Incidental Complex Repetitive Discharges On Needle ElectromyographyDocument4 pagesIncidental Complex Repetitive Discharges On Needle Electromyographyfulgencio garciaNo ratings yet
- Elbow Radiography: Projection Method Part Position Central Ray Structures Shown AP ProjectionDocument14 pagesElbow Radiography: Projection Method Part Position Central Ray Structures Shown AP ProjectionAndrei YabutNo ratings yet
- Catalogo COMFORSIL SiliconasDocument51 pagesCatalogo COMFORSIL SiliconasTalquipen DbzapNo ratings yet